Abstract
A wide variety of fat-containing entities occur in and near the heart. These findings are often encountered by radiologists and may be incidental or the reason for the patient's clinical presentation. Cross-sectional imaging helps to characterize the extent of these lesions and to formulate a differential diagnosis, which varies by lesion location, imaging features and patient demographics. The purpose of this pictorial essay is to familiarize radiologists with these fat-containing lesions and to help avoid misdiagnosis and errors in management. This pictorial review will discuss the normal fatty structures in and around the heart. A range of common and uncommon fat-containing lesions will then be reviewed based upon lesion location.
There is a wide range of fat-containing lesions that can occur in and around the heart (Figure 1).1–5 Clinical findings of such lesions are frequently non-specific with many found incidentally on imaging studies performed for other reasons. Some may be detected on chest radiography or echocardiography; however, CT and MR are the preferred modalities for more definitive characterization. Awareness of the different causes and appearances of these lesions will aid in formulating a differential diagnosis, help to guide additional evaluation and potentially avoid unnecessary work-up for some lesions.
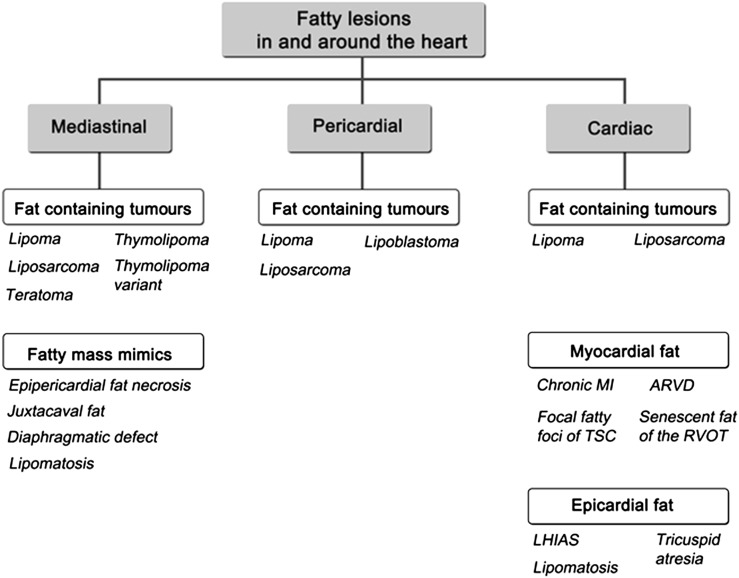
Figure 1.
Flow chart providing an overview fat-containing lesions encountered in and near the heart, organized by location. ARVD, arrhythmogenic right ventricular dysplasia; LHIAS, lipomatous hypertrophy of the interatrial septum; MI, myocardial infract; RVOT, right ventricular outflow tract; TSC, tuberous sclerosis complex.
NORMAL APPEARANCE OF FAT IN AND AROUND THE HEART
The heart is positioned in the inferior middle mediastinum and is surrounded by fat. The pericardium, which surrounds the heart and roots of the great vessels, separates the epicardial fat (which directly encases the myocardium and coronary vessels) from mediastinal or epipericardial fat (located outside of the pericardium). The amount of epicardial fat has been linked to obesity. On occasion, mediastinal fat can mimic a mass on the chest radiograph.4 Within the heart itself, there is a small amount of fat within the atrioventricular groove and inferior right ventricle.6
MEDIASTINAL AND EPIPERICARDIAL FATTY LESIONS
These lesions can be separated into fat-containing tumours and fatty tumour mimics that are confined to the mediastinal fat. Symptoms vary and, when present, are likely related to mass effect upon surrounding structures.
Fat-containing neoplasms
Germ cell tumours are composed of a heterogeneous mixture of tissue from at least two of three germ cell layers. They present most often as a mature teratoma appearing as a well-defined, fat-containing mass in the anterior mediastinum often admixed with cystic areas and irregular calcifications.1 On CT and MR, they have characteristics that reflect their heterogeneous components (Figure 2). While often benign, a teratoma may contain malignant components (teratocarcinoma) or have mixed aggressive features (mixed germ cell tumour with immature teratoma). These forms are often less well defined and may show signs of invasion.1
Figure 2.
Mediastinal teratoma. Coronal contrast-enhanced CT image demonstrates a large, encapsulated mass in the right paracardiac region resulting in mass effect upon the right atrium and right superior pulmonary vein. Attenuation characteristics of this mass are consistent with a mature teratoma with foci of coarse calcification and a significant amount of fatty tissue.
Mediastinal lipomas are similar to lipomas elsewhere appearing as a slow growing, encapsulated mass with homogeneous fat attenuation. These lesions occur most commonly in the anterior mediastinum.1,4 If excessive, unencapsulated fat is noted in the mediastinum, the term mediastinal lipomatosis is favoured. Both obesity and steroid use have been linked to this finding.1,4 Inhomogeneous appearance and location help differentiate lipoma from liposarcoma, which tends to have areas of enhancing soft tissue and occur most commonly in the posterior mediastinum.3,4
Thymolipoma arises from thymic tissue and may be associated with myasthenia gravis. Differentiating it from a teratoma is challenging as they share many of the same imaging features. The absence of cystic changes and an origin from the thymic bed is helpful in suggesting thymolipoma.1 Rarely, a malignant variant termed thymoliposarcoma has been reported,7 presenting with liposarcoma-like features within the thymus (Figure 3).
Figure 3.
Thymoliposarcoma. Transaxial contrast-enhanced CT image of the chest reveals a very large, predominantly fatty mass throughout the anterior mediastinum and extending along the cardiophrenic angles. There are several enhancing septa (arrow) as well as solid components. The mass results in posterior displacement of the mediastinal structures.
Fatty mass mimics
Epipericardial fat necrosis is a benign condition of uncertain aetiology. It often presents as acute chest pain with features similar to fat necrosis found elsewhere.4 On CT, this process appears as an encapsulated fat-containing paracardiac mass centred in the epipericardial fat, which may or may not have adjacent inflammatory changes depending on the timing of imaging (Figure 4). It is a benign, self-limiting process and warrants no further work-up.4
Figure 4.
Epipericardial fat necrosis. Transaxial contrast-enhanced CT images of the chest demonstrate a lobulated low attenuation mass in the right anterior pericardiophrenic angle with intrinsic inflammatory stranding (arrows) consistent with epipericardial fat necrosis.
Juxtacaval fat is a normal variant with a characteristic location and appearance. It is typically observed as a focus of fat in the medial lumen of the inferior vena cava just superior to the hepatic venous confluence and is contiguous with the fat surrounding the subdiaphragmatic oesophagus.1 It is important not to mistake this benign finding for intracaval tumour or thrombus.
Defects in the diaphragm can be congenital or acquired and are a common source of diagnostic challenges. Multiplanar reformations assist in characterizing the defect and the relationship of the herniated structures (Figure 5). In cases where only omental fat has herniated, the presence of vessels originating in the abdomen helps differentiate hernia from a fat-containing mass.1,4
Figure 5.
Fat-containing Morgagni hernia. Axial contrast-enhanced CT image shows a large amount of omental fat herniating through an anterior diaphragmatic defect along with loops of both small and large bowel. Reformatted images (not shown) depicted mesenteric vessels herniating through the defect as well.
FAT-CONTAINING LESIONS IN THE PERICARDIUM
There are very few fat-containing masses that may arise in the pericardium, making their distinction relatively straightforward. These masses can be classified as benign and malignant.
Benign fatty pericardial masses
Lipomas can occur in the pericardium with features of lipomas that present elsewhere (Figure 6). Pericardial lipomas are encapsulated. Unlike subcutaneous lipomas, pericardial lipomas are less circumscribed with their contours conforming to the space they occupy.5
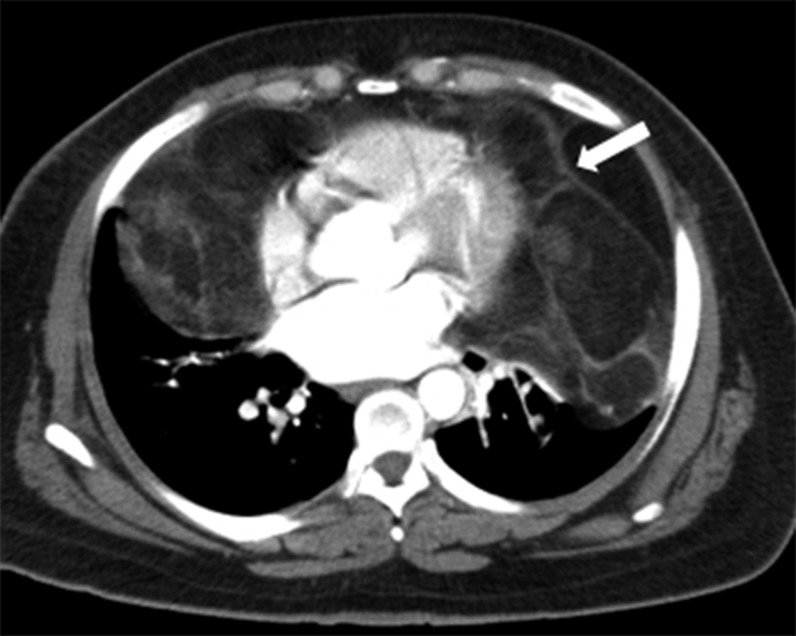
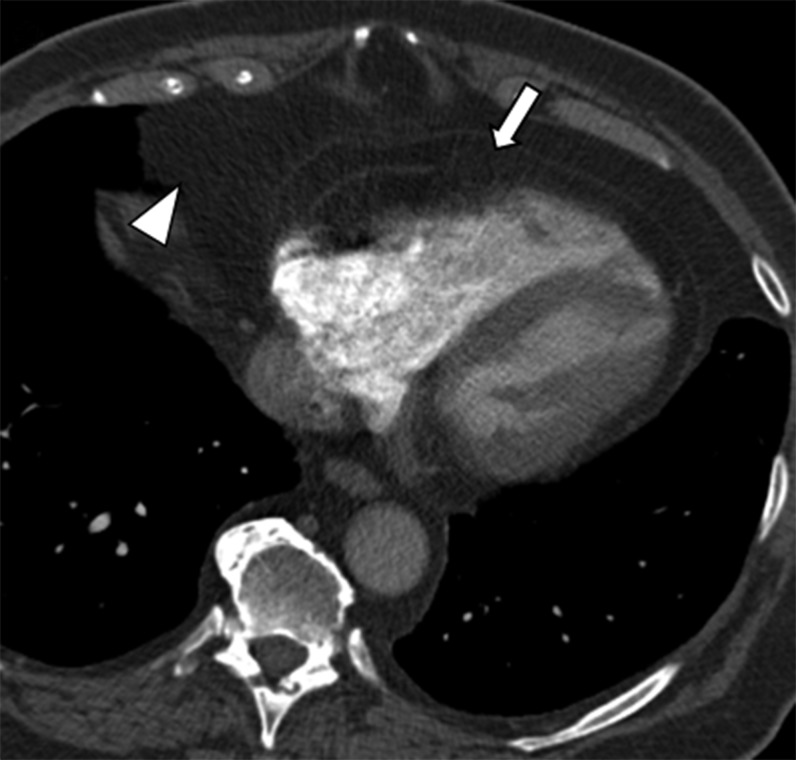
Figure 6.
Pericardial lipoma. Transaxial contrast-enhanced CT images at the level of the heart reveal a large low attenuating mass confined within the pericardium consistent with pericardial lipoma. Note how the lesion insinuates throughout the space it occupies. Also note the significant mass effect upon the superior vena cava (arrowhead) and pulmonary veins (arrow).
Pericardial lipoblastoma is an unusual mesenchymal tumour that presents in the paediatric age group, frequently before 3 years of age. The term lipoblastoma refers to its superficial, well-defined form, whereas lipoblastomatosis is reserved for the deep, infiltrating form.5 Regardless of the type, the mass is characterized by intrinsic tumoral stranding on CT and intrinsic streaks and swirls on MR, corresponding to its known fibrovascular network (Figure 7). It lacks calcifications and fluid, often seen with teratomas, and usually presents at an earlier age than liposarcoma.1,5 Age and clinical history will help to differentiate this tumour from other similar appearing fatty neoplasms.
Figure 7.
(a, b) Pericardial lipoblastoma in a young child. Coronal (a) and sagittal (b) T1 weighted images show a large fatty pericardial mass occupying the left hemithorax. Note the characteristic intratumoral streaks consistent with the internal septa (arrows). The imaging appearance appearance as well as the patient's age at presentation favoured a diagnosis of lipoblastoma over liposarcoma. Reproduced from Restrepo et al.5
Malignant fat-containing pericardial mass
Primary pericardial liposarcomas are exceedingly rare tumours with no more than 15 cases reported to date. They are often large at presentation with invasive features and symptoms related to mass effect.5 Imaging features are similar to liposarcomas found elsewhere, appearing as a large heterogeneous predominantly fatty mass with areas of soft-tissue enhancement.
FAT-CONTAINING CARDIAC LESIONS
These lesions are characterized by fat contained within one of the three cardiac layers.
Similar to lipomatosis in the mediastinum, epicardial lipomatosis appears as unencapsulated redundant adipose tissue confined to the epicardium (Figure 8).5
Figure 8.
Epicardial lipomatosis. Axial contrast image of the chest demonstrates prominent epicardial (arrow) and mediastinal fat (arrowhead).
Lipomatous hypertrophy of the interatrial septum refers to the accumulation of adipose tissue in the interatrial septum. It is most commonly seen in older patients. Histologically, this accumulation of tissue includes faetal fat, myocardial fibres, myocytes and fibrosis. Although typically asymptomatic, it can be potentially arrhythmogenic or produce symptoms related to mass effect on the superior vena cava or right atrium.1 On fluorine-18 fludeoxyglucose imaging positron emission tomography, it may be hypermetabolic, simulating a neoplastic process. The characteristic imaging appearance is that of a dumbbell-shaped fat-containing lesion that spans the interatrial septum but spares the fossa ovalis (Figures 9 and 10).
Figure 9.
Lipomatous hypertrophy of the interatrial septum. Contrast-enhanced transaxial CT image of the heart shows invaginated fatty tissue in the interatrial septum and mildly encasing the superior vena cava. Note how the fossa ovalis is characteristically spared (arrow).
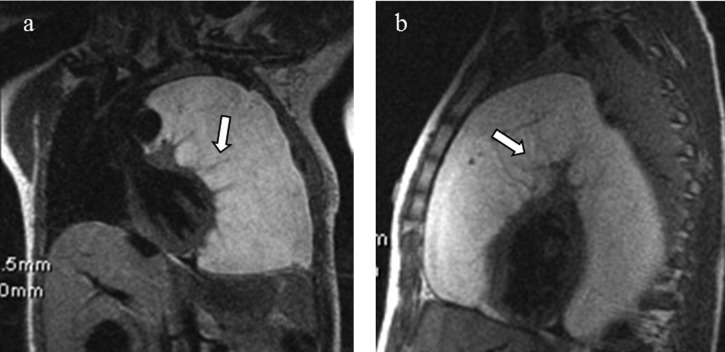
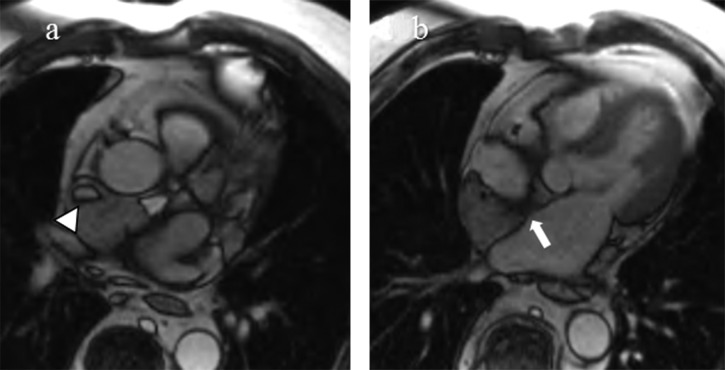
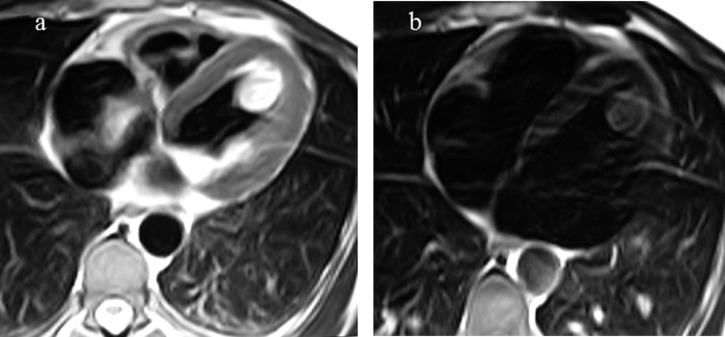
Figure 10.
(a, b) Lipomatous hypertrophy of the interatrial septum in a 63-year-old male with history of right atrial mass seen on echocardiography. Balanced steady-state free precession MR images demonstrate a large amount of tissue in the interatrial septum. This tissue follows signal characteristics of fat on all sequences with signal loss on fat saturated sequences (not shown). Note narrowing of the superior vena cava (arrowhead) and sparing of the fossa ovalis (arrow).
In patients with classic tricuspid atresia, epicardial fat is often noted in the deep atrioventricular sulcus. This “fatty bar” serves as a useful landmark in differentiating it from other types of right atrioventricular valve atresias (Figure 11).8
Figure 11.
Tricuspid atresia. Horizontal long axis reformat from a contrast-enhanced CT of the heart demonstrating a deep fatty bar in the region of the right atrioventricular groove and associated absence of tricuspid valvular tissue (arrow). As a result, the right ventricle is diminutive. A small ventricular septal defect is present (arrowhead).
Intracardiac lipoma has features similar to lipomas elsewhere and is distinguished from other causes of cardiac fat based on its encapsulated appearance (Figure 12). It is distinguished from a cardiac liposarcoma, lacking aggressive features such as local invasion and metastases.1
Figure 12.
(a, b) Cardiac lipoma. Transaxial T2 weighted fast turbo spin echo MR image (a) shows an encapsulated, hyperintense mass along the left ventricular wall. Fat saturated T1 weighted image (b) confirms the fatty content of the mass consistent with an intracardiac lipoma.
Fatty myocardial foci have been described in patients with tuberous sclerosis complex. The origin of these fatty deposits is unclear. While some authors favoured these to represent sequelae of regressed rhabdomyomas, recent evidence suggests origin from perivascular epithelioid cells. These lesions are unique in location and appearance, occurring as unencapsulated deposits of mid-myocardial fat often within the interventricular septum or left ventricular wall (Figure 13).9 This differentiates them from true intramyocardial lipomas that tend to be irregular and capsulated, and arrhythmogenic right ventricular dysplasia (ARVD) that tends to show more diffuse fatty infiltration of the ventricles.
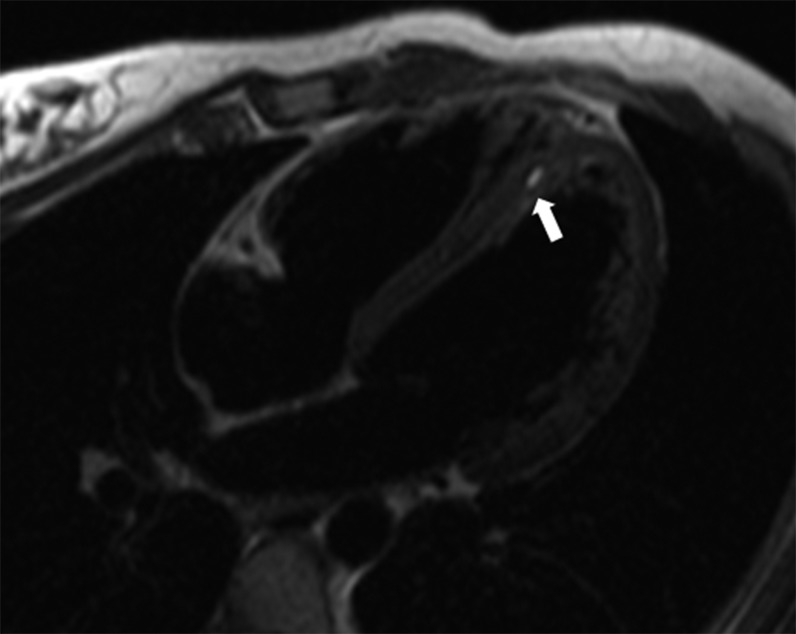
Figure 13.
Intramyocardial fat deposits in tuberous sclerosis complex. Transaxial T2 weighted dark blood image in a patient with history of tuberous sclerosis reveals a small intramyocardial focus of fat (arrow).
Intramyocardial fat has been correlated with various cardiomyopathies, serving as a substrate for arrhythmias, but it is also present to some degree in the normal myocardium. Pathologies associated with fatty infiltration of the myocardium include ARVD and ischaemic cardiomyopathy.6
ARVD is defined by fatty or fibrofatty replacement of the normal right ventricular myocardium. The fatty replacement characteristically affects the right ventricle; however, fibrofatty replacement has been shown to affect the left ventricle as well.10 The typical patient is a young adult presenting with ventricular arrhythmia. MR is useful in evaluating these patients, as it depicts right ventricular enlargement, poor right ventricular function, wall motion abnormalities, and the presence and extent of fatty or fibrofatty myocardial replacement (Figure 14).10 Current diagnosis of ARVD depends on meeting major and minor criteria set forth by an International Task Force that incorporates electrocardiographic, arrhythmic, genetic, histological and structural factors. Recent revision of the structural criteria as seen by cardiac MR include right ventricular dysfunction with either an increase in right ventricular end-diastolic volume index or decrease in right ventricular ejection fraction.11
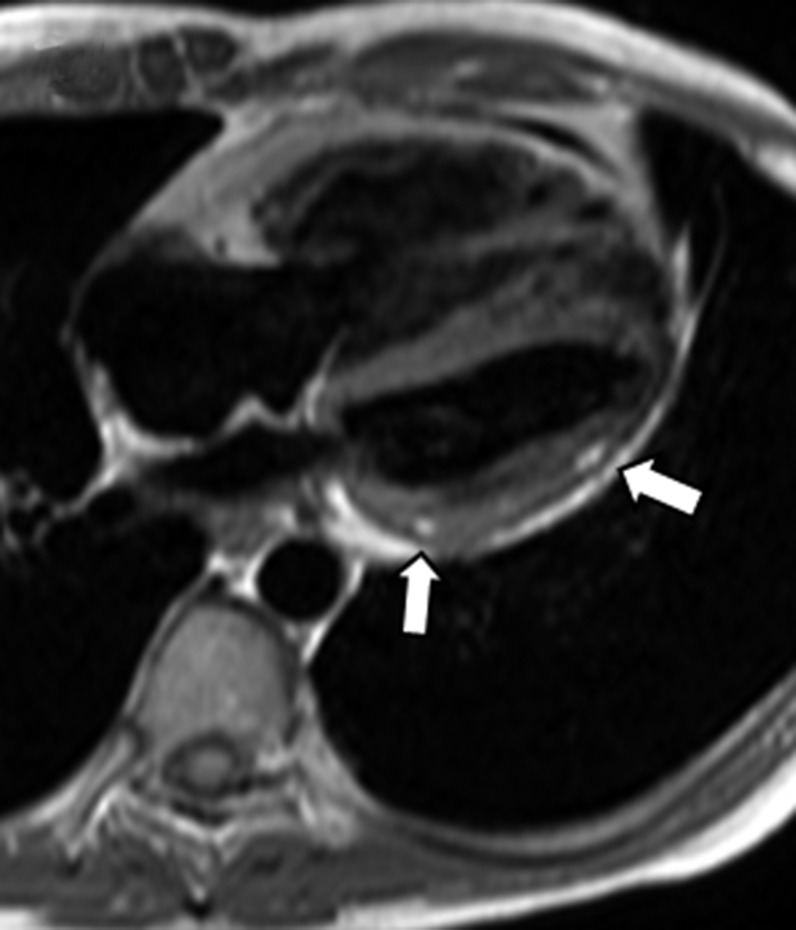
Figure 14.
Arrhythmogenic right ventricular dysplasia. Horizontal long axis T1 weighted image shows foci of intramyocardial high signal in the lateral wall of the left ventricle (arrows). Fat-suppressed images revealed nulling of signal in these foci with diffuse delayed enhancement of the right ventricle (not shown) characteristic of arrhythmogenic right ventricular dysplasia.
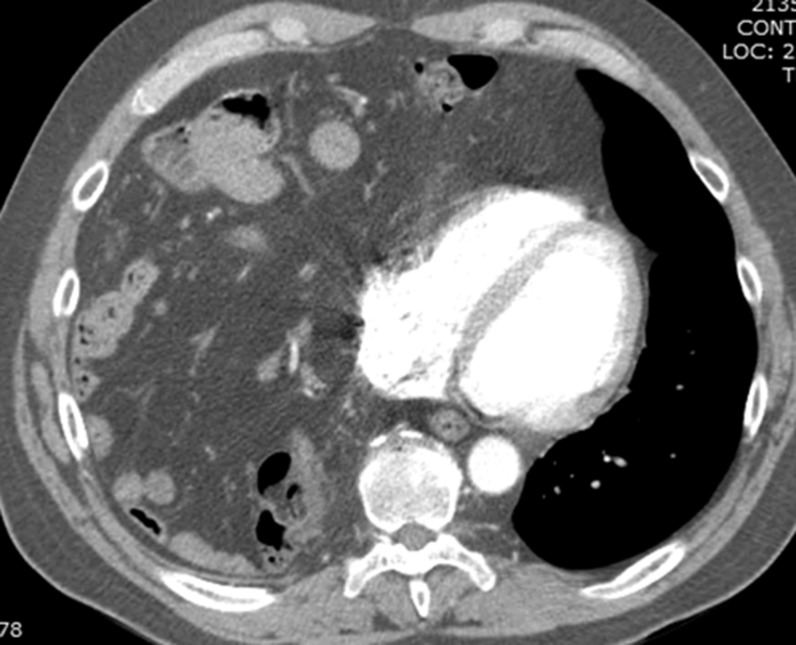
In chronic myocardial infarct, it is not uncommon to see curvilinear fatty deposition in a subendocardial or transmural vascular distribution highlighting the ischaemic event (Figure 15).6 It is important for the radiologist to recognize this finding, as it may significantly impact the patient's management.
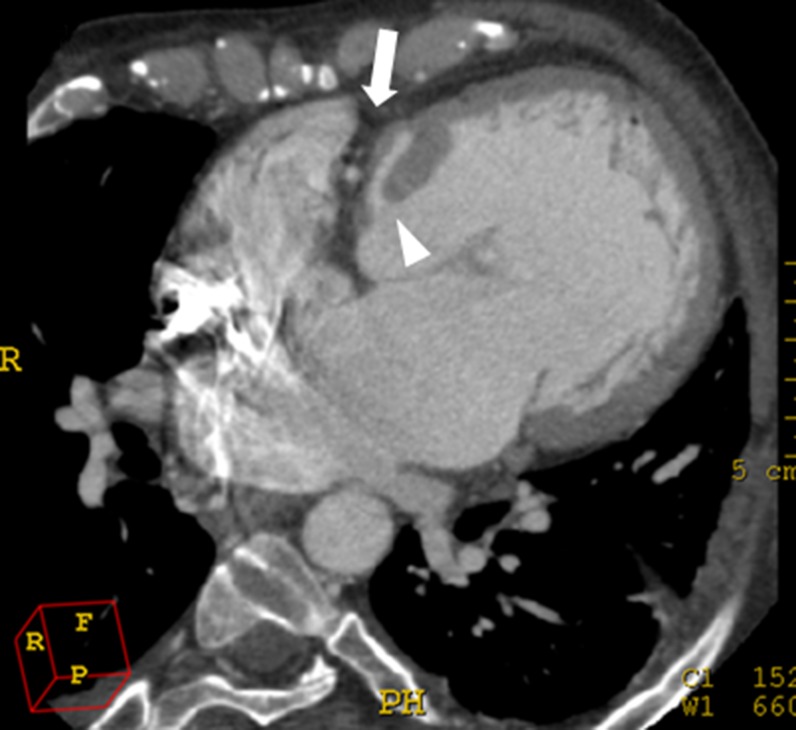
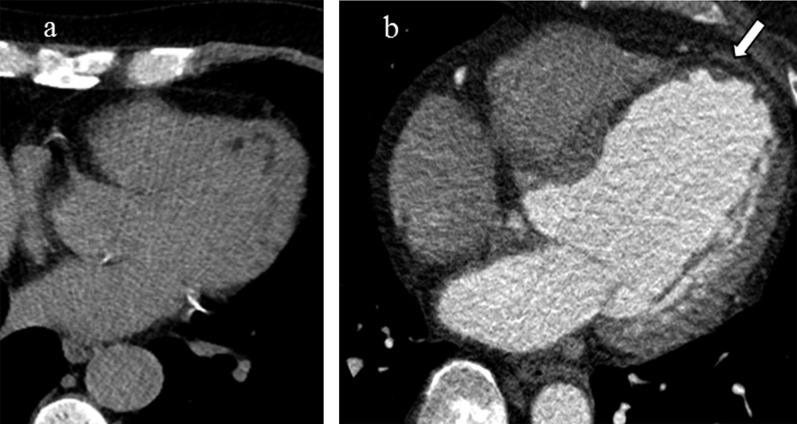
Figure 15.
(a, b) Lipomatous metaplasia in chronic myocardial infarct in two different patients. Transaxial non-contrast CT image of the heart demonstrates curvilinear low attenuation in a subendocardial distribution along the anterolateral and apical walls of the left ventricle. In a different patient, there is transmural fibrofatty replacement and thinning along the interventricular septum, anteroseptal wall and apex of the left ventricle (arrow) consistent with prior myocardial infarct in the left anterior descending distribution.
Senescent fatty infiltration of the right ventricular outflow tract refers to accumulation of fat within the wall of the right ventricular outflow tract and sometimes the right ventricular free wall (Figure 16).1
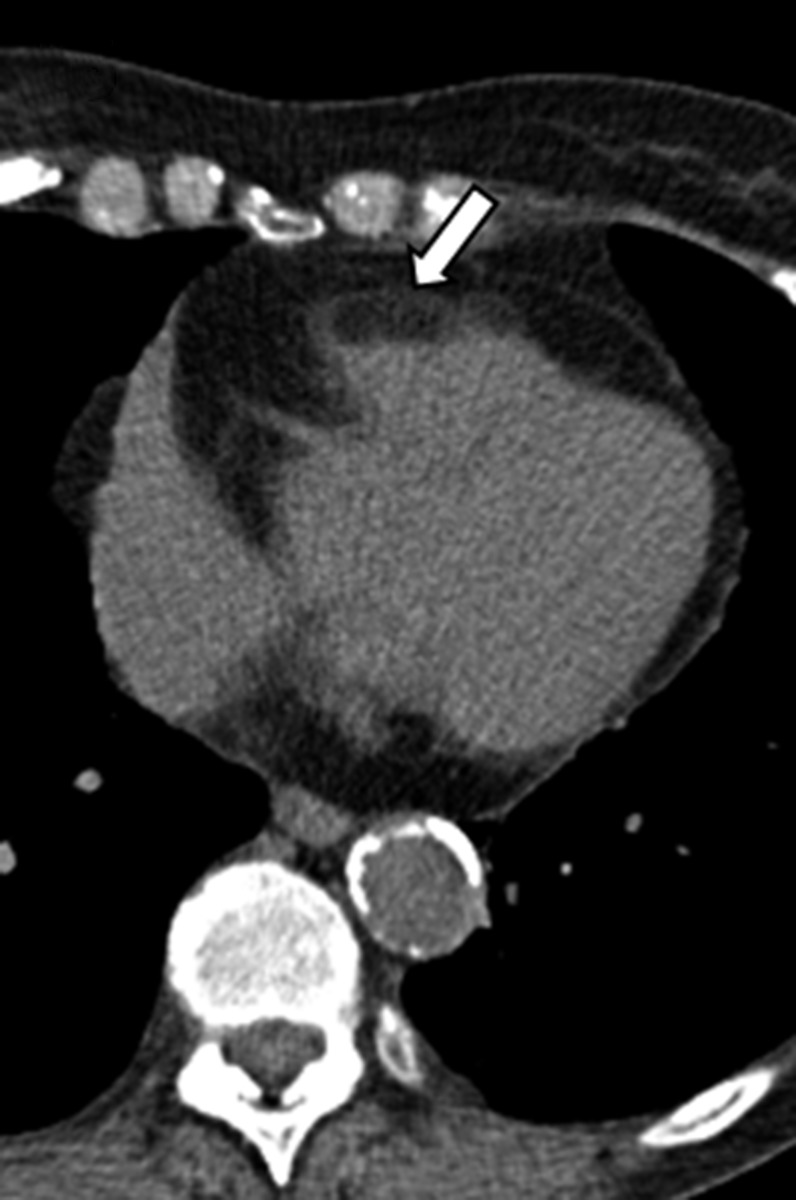
Figure 16.
Senescent fatty infiltration of the right ventricular outflow tract. Transaxial non-contrast CT image of the heart in an 81-year-old asymptomatic female shows extensive fatty infiltration of the right ventricular free wall extending into the right ventricular outflow tract (arrow).
CONCLUSION
Various fat-containing lesions may be encountered in and around the heart. While some of these lesions are incidental and of no consequence, others may require additional evaluation and management. This pictorial review illustrates both common and uncommon causes of these lesions and will help to increase awareness, avoid misdiagnosis and guide appropriate management.
Contributor Information
R Pruente, Email: pruenter@gmail.com.
C S Restrepo, Email: crestr@gmail.com.
D Ocazionez, Email: danielocazionez@gmail.com.
T Suby-Long, Email: thomas.suby-long@ucdenver.edu.
D Vargas, Email: daniel.vargas@ucdenver.edu.
REFERENCES
- 1.Gaerte SC, Meyer CA, Winer-Muram HT, Tarver RD, Conces DJ, Jr. Fat-containing lesions of the chest. Radiographics 2002; 22: S61–78. doi: 10.1148/radiographics.22.suppl_1.g02oc08s61 [DOI] [PubMed] [Google Scholar]
- 2.Lamba G, Frishman WH. Cardiac and pericardial tumors. Cardiol Rev 2012; 20: 237–52. doi: 10.1097/CRD.0b013e31825603e7 [DOI] [PubMed] [Google Scholar]
- 3.Molinari F, Bankier AA, Eisenberg RL. Fat-containing lesions in adult thoracic imaging. AJR Am J Roentgenol 2011; 197: W795–813. doi: 10.2214/AJR.11.6932 [DOI] [PubMed] [Google Scholar]
- 4.Pineda V, Andreu J, Cáceres J, Merino X, Varona D, Domínguez-Oronoz R. Lesions of the cardiophrenic space: findings at cross-sectional imaging. Radiographics 2007; 27: 19–32. doi: 10.1148/rg.271065089 [DOI] [PubMed] [Google Scholar]
- 5.Restrepo CS, Vargas D, Ocazionez D, Martínez-Jiménez S, Betancourt Cuellar SL, Gutierrez FR. Primary pericardial tumors. Radiographics 2013; 33: 1613–30. doi: 10.1148/rg.336135512 [DOI] [PubMed] [Google Scholar]
- 6.Kellman P, Hernando D, Arai AE. Myocardial fat imaging. Curr Cardiovasc Imaging Rep 2010; 3: 83–91. doi: 10.1007/s12410-010-9012-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Howling SJ, Flint JD, Müller NL. Thymoliposarcoma: CT and pathologic findings. Clin Radiol 1999; 54: 341. doi: 10.1016/S0009-9260(99)90571-8 [DOI] [PubMed] [Google Scholar]
- 8.Fletcher BD, Jacobstein MD, Abramowsky CR, Anderson RH. Right atrioventricular valve atresia: anatomic evaluation with MR imaging. AJR Am J Roentgenol 1987; 148: 671–4. doi: 10.2214/ajr.148.4.671 [DOI] [PubMed] [Google Scholar]
- 9.Adriaensen ME, Schaefer-Prokop CM, Duyndam DA, Zonnenberg BA, Prokop M. Fatty foci in the myocardium in patients with tuberous sclerosis complex: common finding at CT. Radiology 2009; 253: 359–63. doi: 10.1148/radiol.2533082118 [DOI] [PubMed] [Google Scholar]
- 10.Kayser HW, van der Wall EE, Sivananthan MU, Plein S, Bloomer TN, de Roos A. Diagnosis of arrhythmogenic right ventricular dysplasia: a review. Radiographics 2002; 22: 639–48; discussion 649–50. doi: 10.1148/radiographics.22.3.g02ma07639 [DOI] [PubMed] [Google Scholar]
- 11.Marcus FI, McKenna WJ, Sherrill D, Basso C, Bauce B, Bluemke DA, et al. Diagnosis of arrhythmogenic right ventricular cardiomyopathy/dysplasia: proposed modification of the task force criteria. Circulation 2010; 121: 1533–41. doi: 10.1161/CIRCULATIONAHA.108.840827 [DOI] [PMC free article] [PubMed] [Google Scholar]