Abstract
Background
Increasing the value of healthcare delivery is a national priority, and providers face growing pressure to reduce cost while improving quality. Ample opportunity exists to increase efficiency and quality simultaneously through the application of systems engineering science.
Objective
We examined the hypothesis that Lean-based reorganization of laboratory process flow would improve laboratory turnaround times (TAT) and reduce waste in the system.
Methods
This study was a prospective, before-after analysis of laboratory process improvement in a teaching hospital Emergency Department (ED). The intervention included a reorganization of laboratory sample flow based in systems engineering science and Lean methodologies, with no additional resources. The primary outcome was the median TAT from sample collection to result for six tests previously performed in an ED kiosk.
Results
Following the intervention, median laboratory TAT decreased across most tests. The greatest decreases were found in “reflex tests” performed after an initial screening test: troponin T TAT was reduced by 33 minutes (86 to 53 min, 99%CI 30–35 min) and urine sedimentation TAT by 88 minutes (117 to 29 min, 99% CI 87–90 min). In addition, troponin I TAT was reduced by 12 minutes, urinalysis by 9 minutes, and urine HCG by 10 minutes. Microbiology rapid testing TAT, a ‘control’, did not change.
Conclusions
In this study, Lean-based reorganization of laboratory process flow significantly increased process efficiency. Broader application of systems engineering science might further improve healthcare quality and capacity, while reducing waste and cost.
Keywords: Lean, Process Improvement, Systems Engineering, ED Performance, Laboratory Testing
1. INTRODUCTION
Healthcare costs continue to increase in the U.S., and average per capita expenditures represent approximately twice that of other developed nations [1]. Thus, increasing the value of healthcare delivery is a national priority, and providers are facing growing pressure to reduce cost while improving quality [2,3]. However, while multiple studies and governing bodies have suggested increased utilization of systems engineering science as a potential solution, it is not abundantly clear which tools are the most effective for application in healthcare [2].
Although this problem is ubiquitous in most areas of medicine, some of the present challenges are of particular importance in emergency medicine. For example, emergency department (ED) crowding remains a national crisis, with myriad and well-documented negative effects on patient care efficiency, quality, and safety, including increased cost, delayed care, and even increased mortality [4–6]. Moreover, the burden of capacity constraints on U.S. EDs is predicted to worsen in the future, likely exacerbating the most destructive current barrier to effective, high-quality care for ED patients in the U.S. [1,7,8] and underscoring the importance of targeting throughput as an approach to increasing functional capacity. In their 2006 report detailing these challenges, “Hospital Based Emergency Care: At the Breaking Point,” the Institute of Medicine (IOM) recommended that proven innovations in systems science and industrial engineering, which have largely not yet taken hold in the healthcare delivery sector, be broadly applied to improve the quality and efficiency of emergency care [7]. As a model for further investigation, emergency medicine represents a valuable crucible in which to test theories that may be more broadly applicable.
1.2 Theoretical Framework
In terms of systems improvement opportunities, emergency medicine is also an excellent example of an area in healthcare in which increased patient care efficiency not only decreases waste and cost, but also improves quality. This occurs through effects on the quality domains of timeliness, efficiency, effectiveness, and safety. However, only recently has the emergency medicine literature started to demonstrate the successes that many similarly complex industries, such as the auto, airline, and service industries, discovered long ago [9–11]. As such, there remains significant opportunity to refine the use and application of these tools across EDs in an ongoing effort to optimize care, especially with respect to modeling and streamlining processes and improving throughput, reducing waste and creating much needed capacity [12–14].
For example, Lean methodologies, originally designed for use in process improvement in the manufacturing industry, represents a potential tool for improving systems of care and throughput in the ED [15–17]. However, these tools have only minimally been studied in health care as a whole, and less so in the ED specifically [18–20].
While previous observational research has demonstrated the potential for Lean methodologies to reduce hospital ED laboratory TAT [21,22], we hoped to expand the extant literature, especially given the link between laboratory and other ancillary testing and ED length-of-stay (LOS) and capacity [23]. In this study, we utilized Lean-based systems engineering tools to reorganize laboratory sample flow based in systems engineering science and modeling, with associated reallocation of resources; no resources were added. We sought to optimize the laboratory testing processes, reduce TAT to the extent possible, decrease waste, and begin to quantify the value of such an intervention.
2. Methods
2.1 Study Design
This study was a prospective, before-after analysis of laboratory process improvements in a hospital ED and main laboratory. We included all adult patients seen during the study periods of 9/2012–2/2013 (before) and 3/2013–2/2014 (after). Data were extracted from the laboratory information system. A period of 1-year post intervention was chosen to provide an adequate sample size and to assess the sustainability of any observed effects. The intervention occurred on 3/4/2013. IRB approval was obtained for the final data analysis so that de-identified data could be retrospectively evaluated in the context of a hypothesis-driven study.
2.2 Study Setting and Population
The study was performed in a large, urban, teaching hospital ED with an annual census of approximately 102,000. The ED serves as a Level I trauma center for adult and pediatric patients as well as a regional burn center. The admission rate is approximately 26% and approximately 31% of all visits arrive by ambulance. Patient flow in the ED follows a relatively standard course with triage, registration, evaluation in a care area, and disposition. Laboratory studies are ordered following initial patient evaluation, and samples are then drawn by nursing and nursing assistant staff. Samples are labeled, a laboratory requisition sheet is completed, and the sample is sent for laboratory testing as described in more detail below.
2.3 Selection of Participants
All adult patients seen in the ED on whom applicable laboratory testing was performed were included in the analysis.
2.4 Intervention
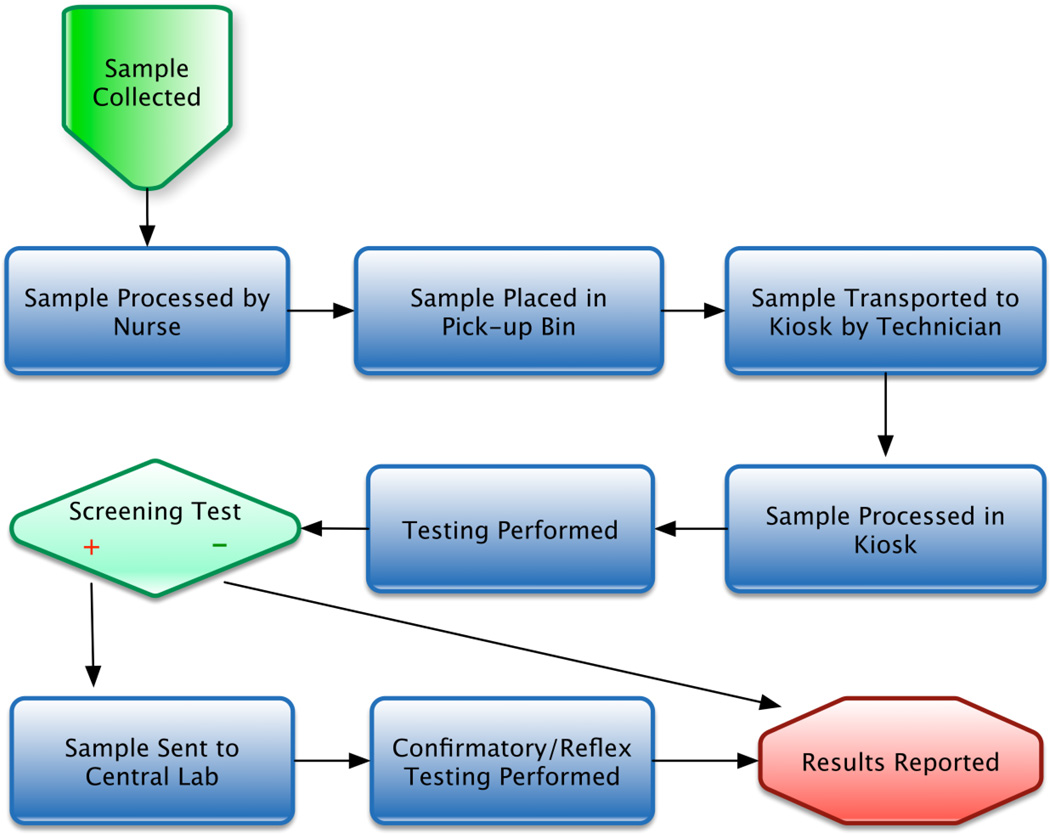
The intervention was a focused Lean-based reorganization of laboratory process flow. Pre-intervention, selected point-of-care laboratory tests (troponin I, urinalysis, urine HCG) were processed and performed in a laboratory located within the ED (the “Kiosk”), and results distributed through the electronic medical record (EMR). More specifically with regard to process flow, laboratory samples were either hand-carried to the Kiosk, or placed in specified bins in order to be collected by the Kiosk laboratory technician (Figure 1).
Figure 1.
Pre-Intervention Laboratory Process Flow
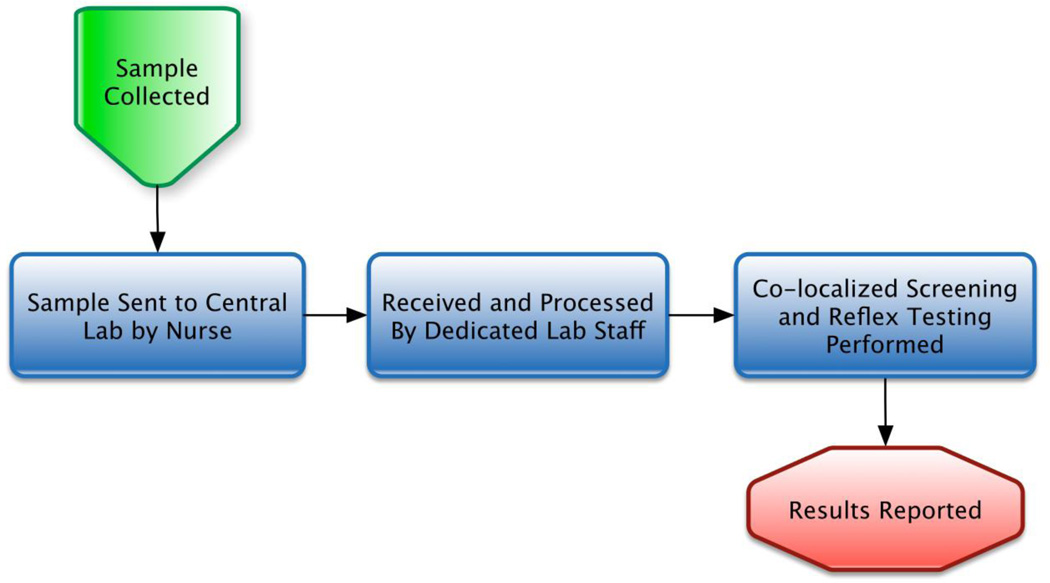
In the future state intervention, it was determined that all samples would be sent via an existing pneumatic tube system to a reorganized section within the central laboratory of the hospital (Figure 2). In the re-organized laboratory section the screening and confirmatory testing platforms were co-localized to facilitate improved reflex testing and communication. Microbiology rapid testing flow did not change significantly in terms of process re-engineering intervention, and thus was considered a “control” test.
Figure 2.
Post Intervention Lean-based Laboratory Process Flow
There were no additions to staffing, nor added resources, during this intervention. In addition, there were no other significant and identifiable operations changes effecting laboratory process flow metrics in either the ED or the main laboratory between the two study periods.
2.5 Methods of measurement
The primary outcomes measured were laboratory TAT for individual testing modalities, defined as the time interval between sample collection and final result.
2.6 Data Collection and Analysis
Data were extracted from the Sunquest laboratory information system (LIS; Tucson, AZ) for both the pre-intervention and the post-intervention periods. Tests were included in the analysis if accessioned at the dedicated ED kiosk computer terminal by the dedicated technologist (identified by a unique LIS location code); as noted, this “virtual” location and terminal was physically within the ED during the pre period and within the central lab during the post period. ED testing during the pre and post period not routed through the dedicated ED kiosk location and workflow was excluded from the analysis. These excluded tests include those not offered by the kiosk and tests not sent using special kiosk requisitions. In addition, testing sent in the pre and post periods using requisitions improperly completed and lacking collection times were excluded from the analysis.
Statistics were performed using the R statistical scripting language [24]. Since turnaround times were not normally distributed, and follow a skewed distribution, medians were used as a measure of central tendency to summarize the distributions. To adjust for multiple testing, Bootstrap resampling was used to calculate empiric 99% confidence intervals around the median turn around time for each test category before and after the intervention as well as the change in median turn around time for each test category. Bootstrap confidence intervals were calculated using the “basic” approach within the R package Boot [25]. 2,500 bootstrap replicates were used to calculate each interval. Bar graphs were generated using the R package ggplots [26].
3. Results
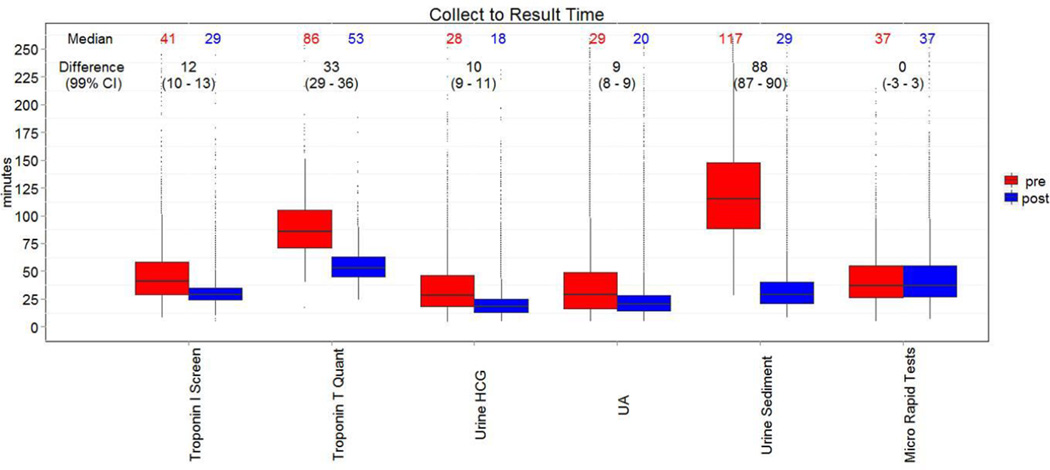
Following the intervention, median laboratory TAT decreased significantly across most tests studied (Figure 3). The greatest decreases were found in reflex tests performed after an initial screening test: troponin T (reflex test for a positive or borderline troponin I test) TAT was reduced by 33 minutes (86 to 53 min, 99%CI 30–35 min, N=722 pre and 844 post) and urine sedimentation (reflex test for a positive chemical urinalysis test) TAT by 88 minutes (117 to 29 min, 99% CI 87–90 min, N=6,396 pre and 13,155 post). In addition, troponin I TAT was reduced by 12 minutes (41 to 29 min, 99%CI 10–13 min, N=3,656 pre and 4,698 post), urinalysis TAT by 9 minutes (29 to 20 min, 99%CI 8–9 min, N=11,470 pre and 24,018 post), and urine HCG TAT by 10 minutes (28 to 18 min, 99%CI 9–11 min, N=3,294 pre and 7,005 post). Microbiology rapid testing TAT did not change (37 to 37 min, 99%CI ±3 min, N=1,193 pre and 2,436 post).
Figure 3.
Median Laboratory Collect to Result Time
A boxplot demonstrating median pre- and post-intervention median TATs, and 99%CI whiskers. Median laboratory TAT decreased across all tests with the exception of Microbiology rapid testing, in which no significant process flow intervention took place.
4. Discussion
In this single center before-after study, a Lean-based reorganization of ED laboratory process flow decreased TAT without added expense. Reflex testing TATs were reduced by 75 % for urine sedimentation testing, and 38 % for troponin T testing.
Lean methodologies are based on elimination of non-value added waste within a system; that is, actions and activities which do not add value to the consumer. In the case of laboratory testing processes, there are many possible foci of waste, many of which are manifested in the form of waiting for one process step to transition to the next process step. As such, there are many potential contributing factors which may have played a role in the success of the Lean intervention. First, in our prior system, the laboratory technician was responsible for gathering samples from multiple ED areas, and collected samples might wait for many minutes prior to being processed. In addition, the act of gathering samples distracted the laboratory technician from their primary role, and in the setting of a single-server system, directly contributed to longer cycle times, as would be explained by queuing theory. Focusing the technologists effort on testing allowed for increased efficiency and improved demand-capacity matching. Further downstream, the co-localization of screening and reflex testing devices for troponin and urinalysis testing allowed for immediate transfer between devices, and eliminated handoffs, sample transport, and associated delays. Regarding urinalysis alone, moving testing devices closer to the sample delivery tube system, and leveraging existing automated testing platforms allowed for decreased technologist involvement.
Regarding cost/benefit implications, the operational benefits gained from this intervention far outweighed the resources (i.e. time and effort) spent to implement this project. As an example, during the intervention, no resources were added, and yet significant reductions in laboratory testing TAT were realized. In addition, as a result of improved efficiency (largely secondary to reduced technician rounding time and simplification of workflows) and pooling servers, 1.2 FTEs of clinical lab assistant time were re-deployed and eliminated from the prior Kiosk testing process. Given an average salary of $52,000 (including benefits), this equates to $62,400 in reduced staffing cost per year.
These results exemplify the potential value of applying systems engineering in order improve efficiency in ED processes. In addition, this work might inform decisions regarding hospital main laboratory design and instrumentation, and demonstrates the importance of flexibility and modularity in order to adapt to changing workflows and maintain the ability to accommodate the needs for both “high throughput, routine testing” and “low volume, turnaround intensive testing”. This work also has implications for the trade-offs inherent in a 2-phase testing approach, as is present in many EDs, with point-of-care screening testing being performed in the ED, and reflex and confirmatory testing in a main lab.
Finally, in an era of increasing focus on healthcare value nationwide, interventions aimed at increasing quality, process efficiency, and capacity, while also reducing waste and extraneous cost, may represent the most powerful approach for hospital, laboratory, and emergency medicine administrators to continue to improve healthcare value.
4.1 Limitations
There are potential limitations with this study. Most importantly, as with any before-after study, while the outcomes measured may have demonstrated a change, they do not prove causality. The observed changes may have been due to some other contributing factor that occurred over the study period which cannot be fully excluded, such as differences in individual productivity, or subtle differences across the patient population studied. However, we were unable to identify any other significant systems or operations changes in the ED or laboratory process flow during this time period, and other known contributors to prolonging laboratory TAT, such as testing volume, did not change significantly in the intervention group during the period studied. In addition, there was no change in the TAT of the rapid microbiology tests in which there were no significant process changes before and after the intervention. Thus, we feel confident that the intervention was associated with the outcomes measured.
Another potential limitation is that this study was performed at a single institution, and thus the findings might not be generalizable to EDs with markedly different demographics, or markedly different laboratory process flows. However, given that improvement science is, by definition, broadly applicable, our findings should be of value to most ED and hospital laboratory administrators on some level.
Also, participants were not blinded to the intervention, and this raises the possible contribution of the Hawthorne effect (i.e. the phenomenon in which individuals modify their behavior in response to being observed). However, the fact that the post-intervention study period occurred for a full year after the intervention was initiated should serve to mitigate this effect, in that study participants had ample time to become familiar with the new system, and were unlikely to alter their actions due to the Hawthorne effect for an entire year. In addition, there was no identifiable incentive to alter behavior following the intervention.
Finally, the intervention studied actually consisted of a number of smaller systems improvements grouped into a single process change. While this is more practically feasible and frequently the case with systems engineering and redesign, our study design does not permit interpretation of each component’s individual contribution to the results.
5. Conclusion
In this study, Lean-based reorganization of laboratory process flow significantly increased process efficiency. Broader application of systems engineering science might further improve healthcare quality and capacity, while reducing waste and cost.
Acknowledgments
This work was supported by a Loan Repayment Program (LRP) grant from the National Institutes of Health (NIH).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
A subset of these data were presented at the American College of Emergency Medicine (ACEP) national meeting in Chicago, IL, on October 27th, 2014.
As noted in the Methods section, Institutional Review Board approval was obtained for this study.
REFERENCES
- 1. [Retrieved November 28, 2014];AHA Trendwatch Chartbook. 2014 from www.aha.org/research/reports. [Google Scholar]
- 2.Yong PL, Saunders RS, Olsen L. The Healthcare Imperative. National Academies Press (US); 2010. [PubMed] [Google Scholar]
- 3.Martin L, CW N, Mountford J, Bisognano M, Nolan T. Increasing Efficiency and Enhancing Value in Health Care. Cambridge: Massachusetts; 2009. [Google Scholar]
- 4.Bernstein SL, Aronsky D, Duseja R, Epstein S, Handel D, Hwang U, et al. The effect of emergency department crowding on clinically oriented outcomes. Acad Emerg Med. 2009;16:1–10. doi: 10.1111/j.1553-2712.2008.00295.x. [DOI] [PubMed] [Google Scholar]
- 5.Miro O, Antonio MT, Jimenez S, De Dios A, Sanchez M, Borras A, et al. Decreased health care quality associated with emergency department overcrowding. Eur J Emerg Med. 1999;6:105–107. doi: 10.1097/00063110-199906000-00003. [DOI] [PubMed] [Google Scholar]
- 6.Sprivulis PC, Da Silva JA, Jacobs IG, Frazer AR, Jelinek GA. The association between hospital overcrowding and mortality among patients admitted via Western Australian emergency departments. Med J Aust. 2006;184:208–212. doi: 10.5694/j.1326-5377.2006.tb00416.x. [DOI] [PubMed] [Google Scholar]
- 7.Institute of Medicine. Washington, DC: National Academy Press; 2006. Hospital-Based Emergency Care: At the Breaking Point. [Google Scholar]
- 8.Pines JM, McCarthy ML. The crowding-effectiveness link: it doesn’t matter how fast we deliver care if we don't deliver it right. Ann Emerg Med. 2011;57:201–202. doi: 10.1016/j.annemergmed.2010.12.005. [DOI] [PubMed] [Google Scholar]
- 9.Hogan B, Rasche C, von Reinersdorff AB. The First View Concept: introduction of industrial flow techniques into emergency medicine organization. Eur J Emerg Med. 2011 doi: 10.1097/MEJ.0b013e32834bbd93. [DOI] [PubMed] [Google Scholar]
- 10.Eitel DR, Rudkin SE, Malvehy MA, Killeen JP, Pines JM. Improving service quality by understanding emergency department flow: a White Paper and position statement prepared for the American Academy of Emergency Medicine. J Emerg Med. 2010;38:70–79. doi: 10.1016/j.jemermed.2008.03.038. [DOI] [PubMed] [Google Scholar]
- 11.Hoot NR, Aronsky D. Systematic review of emergency department crowding: causes, effects, and solutions. Ann Emerg Med. 2008;52:126–136. doi: 10.1016/j.annemergmed.2008.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Storrow AB, Zhou C, Gaddis G, Han JH, Miller K, Klubert D, et al. Decreasing lab turnaround time improves emergency department throughput and decreases emergency medical services diversion: a simulation model. Acad Emerg Med. 2008;15:1130–1135. doi: 10.1111/j.1553-2712.2008.00181.x. [DOI] [PubMed] [Google Scholar]
- 13.Asplin BR, Magid DJ, Rhodes KV, Solberg LI, Lurie N, Camargo CA., Jr A conceptual model of emergency department crowding. Ann Emerg Med. 2003;42:173–180. doi: 10.1067/mem.2003.302. [DOI] [PubMed] [Google Scholar]
- 14.Asaro PV, Lewis LM, Boxerman SB. The impact of input and output factors on emergency department throughput. Acad Emerg Med. 2007;14:235–242. doi: 10.1197/j.aem.2006.10.104. [DOI] [PubMed] [Google Scholar]
- 15.Graban M. Lean Hospitals: Improving Quality, Patient Safety, and Employee Satisfaction. New York: Productivity Press; 2008. [Google Scholar]
- 16.Dart RC. Can Lean Thinking Transform American Health Care? YMEM. 2011;57:279–281. doi: 10.1016/j.annemergmed.2010.11.027. [DOI] [PubMed] [Google Scholar]
- 17.Parks JK, Klein J, Frankel HL, Friese RS, Shafi S. Dissecting delays in trauma care using corporate lean six sigma methodology. J Trauma. 2008;65:1095–1098. doi: 10.1097/TA.0b013e318188e8ad. [DOI] [PubMed] [Google Scholar]
- 18.Holden RJ. Lean Thinking in Emergency Departments: A Critical Review. YMEM. 2011;57:265–278. doi: 10.1016/j.annemergmed.2010.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Decker WW, Stead LG. Application of lean thinking in health care: a role in emergency departments globally. Int J Emerg Med. 2008;1:161–162. doi: 10.1007/s12245-008-0057-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dickson EW, Singh S, Cheung DS, Wyatt CC, Nugent AS. Application of lean manufacturing techniques in the Emergency Department. J Emerg Med. 2009;37:177–182. doi: 10.1016/j.jemermed.2007.11.108. [DOI] [PubMed] [Google Scholar]
- 21.Hagg HW, Mapa L, Vanni C. Application of Lean Six Sigma techniques to optimize hospital laboratory Emergency Department Turnaround time across a multi-hospital system. Eng Educ. 2007:30. [Google Scholar]
- 22.Sullivan P, Cruise K, Callahan CD. Lean six sigma methods reduce and sustain troponin turnaround time (TAT) for emergency department patients. Am J Clin Pathol. 2013;140:A237. [Google Scholar]
- 23.Kocher KE, Meurer WJ, Desmond JS, Nallamothu BK. Effect of testing and treatment on emergency department length of stay using a national database. Acad Emerg Med. 2012;19:525–534. doi: 10.1111/j.1553-2712.2012.01353.x. [DOI] [PubMed] [Google Scholar]
- 24.R Core Team. R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2013. [Google Scholar]
- 25.Canty A, Ripley B. boot: Bootstrap R (S-Plus) Functions. R package version 1.3-9. 2013 [Google Scholar]
- 26.Wickham H SpringerLink (Online service) ggplot2 Elegant Graphics for Data Analysis. New York, NY: Springer-Verlag New York; 2009. [Google Scholar]