Abstract
Objective
To compare the risks and benefits of lumbar puncture (LP) to evaluate for subarachnoid hemorrhage (SAH) after a normal head computed tomography (CT) scan.
Methods
This was an observational study of adult emergency department (ED) patients at a single hospital who presented with headache and underwent LP after a normal head CT to evaluate for SAH. LP results classified as indicating a SAH included: xanthochromia in cerebrospinal fluid (CSF); or red blood cells in the final tube of CSF with an aneurysm or arteriovenous malformation on cerebral angiography. An LP-related complication was defined as hospitalization or a return visit due to symptoms attributed to the LP. Proportions of the study patients who had SAH diagnosed by LP and who experienced an LP-related complication were compared.
Results
The study included 302 patients, including 2 (0.66%) who were diagnosed with SAH based on LP (number-needed-to diagnose: 151); both of these patients had a known intracranial aneurysm. Eighteen (5.96%) patients experienced a LP-related complication (p<0.01 compared to number with SAH diagnosed; number-needed-to-harm: 17). Complications included 12 patients with low-pressure headaches, 4 with pain at the LP site, and 2 with contaminated CSF cultures.
Conclusion
The yield of LP for diagnosing SAH in adults with nontraumatic headache after a normal head CT was very low. The severity of LP-related complications was low, but complications were more common than SAH diagnoses. LP may not be advisable after a normal head CT to evaluate for SAH, particularly in patients with low-risk clinical features for SAH.
Keywords: subarachnoid hemorrhage, lumbar puncture, risk-benefit analysis, diagnostic testing
1. Introduction
Headache is the chief complaint for approximately 2.2% of emergency department (ED) visits in the United States, representing over 2 million visits annually.1 Subarachnoid hemorrhage (SAH) is a rare cause of these headaches, accounting for only about 0.6% of headaches evaluated in the ED.1 Even among adult ED patients with a severe nontraumatic headache instantly peaking in pain intensity (a so-called “thunderclap headache”), only approximately 6.2% of patients have SAH.2
A non-contrast computed tomography (CT) scan of the head is the initial diagnostic test of choice to evaluate for SAH.3 Historically, the sensitivity of head CT for SAH was 92-98% with third-generation scanners from the 1980s and 1990s, with lower sensitivity if the CT scan was delayed > 12 hours after headache onset.4,5 Due to this imperfect sensitivity of head CT for SAH, current practice guidelines recommend a lumbar puncture (LP) to directly evaluate the cerebrospinal fluid (CSF) for signs of SAH after a normal head CT in patients with a clinical presentation suggestive of SAH.3,6
More recent studies suggest the sensitivity of head CT for SAH has improved with updated CT technology. 7, 8, 9 As the sensitivity of CT improves, the potential benefit of performing a LP after a normal CT to evaluate for SAH diminishes. Considering both the risks and benefits of LP is important for informed decision-making about whether to perform this invasive procedure. Historically, the benefits of LP to evaluate for SAH have been emphasized, but the risks of the procedure have not been well characterized in the literature. Given the complexity of weighing the risks and benefits of LP after a normal head CT and the paucity of data in the literature regarding these risks, we compared the beneficial and adverse effects of LP in a cohort of adults who underwent LP to evaluate for SAH in an ED.
2. Methods
2.1. Study Design and Setting
This was a retrospective observational study of adult ED patients presenting with a nontraumatic headache who underwent LP to evaluate for SAH after a normal head CT at a single academic hospital in the United States from July 1, 2010 to June 30, 2013. The study hospital had approximately 65,000 adult ED visits per year. CT scans were obtained with a 64-slice CT scanner (Philips Brilliance CT 64-channel scanner; Philips Healthcare, Andover, MA). CT images were interpreted in real-time for clinical care by board-certified radiologists. The study was approved by the local Institutional Review Board with waiver of informed consent.
2.2. Study Population
Patients meeting the following criteria were included: 1) age ≥ 18 years old; 2) presentation to the study ED between July 1, 2010 and June 30, 2013; 3) chief complaint of nontraumatic headache of < 7 days duration; 4) non-contrasted head CT performed prior to LP; 5) CT results did not reveal an explanation for the patient's headache; 6) CSF collected from a LP (not from a shunt); and 7) LP performed to evaluate for SAH, which was operationalized as a description in the medical record of “the worse headache of life” or “thunderclap headache,” or specific documentation that the LP was performed to assess for SAH.
2.2.1. Subgroup Population: Low-risk clinical features
We also analyzed a subgroup of the study population with low-risk clinical features for SAH.2, 8 Patients were included in this low-risk subgroup if they exhibited all of the following features in addition to the eligibility criteria listed above: 1) normal mental status in the ED; 2) no known intracranial aneurysm at the time of LP; and 3) no known prior SAH.
2.3. Study Protocol
A list of all patients who had CSF collected in the adult ED of the study hospital from July 1, 2010 to June 30, 2013 was generated using the institution's electronic database warehouse. One of three investigators (VLM, WKW, DL) reviewed the medical record of each patient who had CSF collected to ascertain if the patient met eligibility criteria for the study, and if so, to collect study data. The medical records review included all documentation for one month, starting with the index ED visit during which an LP was performed. Data collection was performed according to standards for emergency medicine chart review studies. 10, 11 All investigators were trained on the study protocol and all variables were defined prior to initiation of the chart reviews. Data were abstracted using a standardized electronic data collection instrument. Investigators held routine meetings during the data abstraction phase to ensure standardization of methods. The senior investigator (WHS) reviewed a random 10% sample of the charts and inter-rater agreement between the initial review and the senior investigator review was calculated for key variables (see Data Analysis below for details).
2.4. Outcomes
The primary outcome was a diagnosis of SAH based on LP results, defined as: 1) xanthochromia in the CSF; or 2) red blood cells (>1 × 106/mm3) in the final tube of CSF with an aneurysm or arteriovenous malformation subsequently identified on cerebral angiography.2
Additionally, we also identified alternative diagnoses revealed by LP results. These included: bacterial meningitis, defined as a positive CSF culture for pathogenic bacteria (all bacteria except common skin contaminants defined below); viral meningitis, defined as lymphocyte predominate CSF pleocytosis (>5 × 106 WBC/mm3) with negative bacterial cultures and no meningeal exposure to chemical irritants; chemical meningitis, defined as CSF pleocytosis after exposure to a known meningeal chemical irritant and negative CSF cultures; and intracranial hypertension, defined as an opening CSF pressure > 25 cm H20 in the absence of intracranial infection or hemorrhage.
We also identified complications related to LP that resulted in a return visit to the ED or clinic or hospitalization. Complications were classified into the following groups: 1) low-pressure headache, defined as headache within 5 days of an LP that worsened with upright position and improved with supine position12; 2) contaminated CSF, defined as a CSF culture that grew a common skin contaminant, including Aerococcus species, α-hemolytic Streptococcus, Bacillus species except anthracis, coagulase negative Staphylococcus species except lugdunensis, Corynebacterium species, Micrococcus species, diphtheroids, and Propionibacterium species; 3) hemorrhage at the LP site; 4) infection at LP site, which included cellulitis (clinical diagnosis) and deep space infection (radiographic diagnosis); 5) pain related the LP, including both localized pain and neuropathic pain; and 6) additional invasive testing due to equivocal or false-positive LP results.
2.5. Data Analysis
Inter-rater agreement between the initial medical records review and the senior investigator review was calculated with Cohen's kappa13 for the following variables: diagnosis of SAH based on LP results, and presence of an LP-related complication.
Proportions of the study population who had SAH and each of the alternative diagnoses identified by LP results were calculated. The proportion of patients who experience an LP-related complication resulting in a return visit or hospitalization was also calculated. Proportions with SAH diagnosed and an LP-related complication were compared with Fisher's exact test.
The number of LPs needed to diagnose one SAH (number-needed-to-diagnose) was calculated by dividing the total number of patients who underwent LP by the number of SAH diagnosed. Similarly, number-needed-to-harm was calculated by dividing the total number of LPs by the number of patients who experienced a LP-related complication. Binomial exact confidence intervals were calculated for number-needed-to-diagnose and number-needed-to-harm.
These calculations were also performed after limiting the study population to the subgroup with low risk-clinical features (normal mental status, no known history of intracranial aneurysm, and no known prior SAH).
Sample size calculations were based on the projected difference in the proportion who had SAH diagnosed based on LP results and the proportion who experienced an LP-related complication. We projected 0.5% would have SAH diagnosed by LP and 4% would have an LP-related complication. Using these estimates, at least 281 patients were required for 80% power to detect the difference in these proportions with a type I error of 0.05.
Analyses were performed with Stata 12.0 (Stata Corp, College Station, TX) and PS Power and Sample Size Calculations. 14
3. Results
3.1 Study Population
A total of 1,700 patients had CSF collected during the 3-year study period in the participating ED; 302 (17.8%) patients met all study eligibility criteria and were included in the primary analysis (Figure). The most common exclusion criteria were: LP performed to evaluate for conditions other than SAH (1,355); CSF collected from a shunt (407); and headache not the presenting symptom (341). Median age of included patients was 40 years [interquartile range (IQR): 30, 55 years]; 22 (7.3%) patients presented with altered mental status, 34 (11.3%) had a known intracranial aneurysm, and 13 (4.3%) had a prior SAH (Table 1).
Figure.
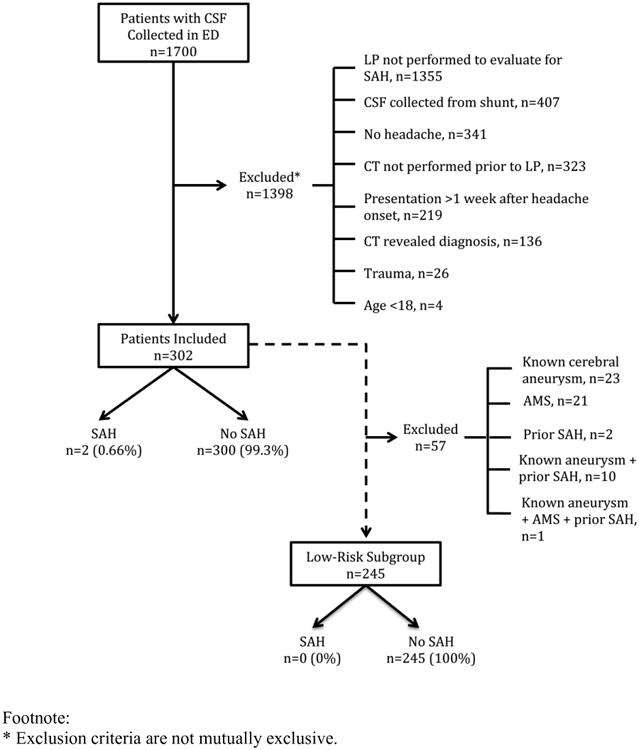
Flow diagram of patient participation.
Table 1.
Patient characteristics.
| Characteristic | Patients with LP to evaluate for SAH (n = 302) |
|---|---|
| Median age, years (IQR) | 40 (30, 55) |
| Female, n (%) | 200 (66.2) |
| Race, n (%) | |
| White | 216 (71.5) |
| Black | 60 (19.9) |
| Other | 26 (8.6) |
| Chronic Medical Conditions, n (%) | |
| Migraine headaches | 65 (21.5) |
| Other chronic headaches | 31 (10.3) |
| Hypertension | 103 (34.1) |
| Known cerebral aneurysm | 34 (11.3) |
| Known cerebral artiovenous malformation | 2 (0.7) |
| Prior stroke | 11 (3.7) |
| Polycystic kidney disease | 1 (0.3) |
| Known family history of aneurysms | 12 (4.0) |
| Current anticoagulation medication | 10 (3.3) |
| Prior subarachnoid hemorrhage | 13 (4.3) |
| Current pregnancy | 2 (0.7) |
| Coarctation of the aorta | 2 (0.7) |
| Sympathomimetic drug use | 7 (2.3) |
| Prior or current tobacco use | 118 (39.0) |
| Presenting Signs and Symptoms Accompanying Headache, n (%) | |
| Reported worst headache of life | 126 (41.7) |
| Neck pain/stiffness | 96 (31.8) |
| Nausea | 157 (51.0) |
| Vomiting | 102 (33.8) |
| Altered mental status | 22 (7.3) |
| Change in vision | 53 (17.6) |
| Unable to ambulate | 7 (2.3) |
| Seizure | 3 (1.0) |
The inter-rater agreement between the original review and senior investigator review was 100% (Kappa: 1.00; standard error: 0.18) for both the diagnosis of SAH and presence of an LP-related complication.
3.2. Subarachnoid Hemorrhage Diagnoses and Complications from Lumbar Puncture
Of the 302 included patients, 2 (0.66%) had SAH diagnosed based on LP results (Table 2). Both of these patients had high-risk clinical features for SAH. One patient presented with acute altered mental status and gait ataxia and was found to have a 3×6mm intracranial aneurysm on CT-angiogram (CTA) prior to LP. Non-contrast head CT showed no signs of intracranial hemorrhage. CSF had xanthochromia and 251,600 red cells in tube 4. This patient underwent embolization of the aneurysm and made a neurologic recovery back to her baseline.
Table 2.
Lumbar puncture (LP) outcomes for 302 patients who underwent LP to evaluate for subarachnoid hemorrhage.
| Diagnoses resulting from LP | n (%) | LP-related complications | n (%) |
|---|---|---|---|
|
|
|
||
| None | 268 (88.7) | None | 284 (94.0) |
| Subarachnoid hemorrhage | 2 (0.66) | Any complication | 18 (5.96) |
| Any alternative diagnosis | 32 (10.6) | Specific complications | |
| Specific alternative diagnoses | Low pressure headache | 12 (3.97) | |
| Bacterial meningitis | 5 (1.66) | Pain related to LP | 4 (1.32) |
| Viral meningitis | 19 (6.29) | Contaminated CSF culture | 2 (0.66) |
| Chemical meningitis | 1 (0.33) | ||
| Intracranial hypertension | 6 (1.99) | ||
| Intrathecal hematoma | 1 (0.33) | ||
The second patient diagnosed with a SAH based on LP results presented to the ED with headache and neck stiffness. This patient had a known basilar artery aneurysm that had undergone coil embolization 10 days prior to presenting to the ED. Head CT revealed no signs of hemorrhage. CSF had xanthochromia and 43,725 red cells in tube 4. A subsequent angiogram confirmed the known aneurysm and showed no changes in the coil embolization. No further intervention was completed.
Of 302 included patients, 18 (5.96%) had a LP-related complication resulting in a return visit or hospitalization (p<0.01 compared to the proportion with SAH diagnosed by LP results) (Table 2). Twelve (3.97%) of these patients returned to the ED with low-pressure headaches, including four patients treated with a blood patch. Four (1.32%) patients had severe pain at the LP site and two (0.66%) had contaminated CSF cultures leading to return visits and additional cultures. None of the patients had an infectious or hemorrhagic complication from LP.
Based on these results, the number of LPs needed to diagnose one SAH in our population was 151 (95% CI: 42, 1245). The number of LPs needed to harm one patient was 17 (95% CI: 11, 28).
3.3 Alternative Diagnoses
Among the 302 included patients, 32 (10.6%) had an alternative diagnosis other than SAH identify from LP (Table 1), including 19 (6.29%) with viral meningitis, 5 (1.66%) with bacterial meningitis, and 1 (0.33%) with chemical meningitis from recent contrast exposure (Table 2). Of note, all 5 patients diagnosed with bacterial meningitis had clinical features of infectious meningitis in the ED. Two of these patients had rapid and profound decline in mental status. One patient presented with a fever, headache and neck stiffness. Another patient had a fever and known sinusitis. The final patient had a headache similar to a prior episode of bacterial meningitis.
3.4. CT-angiogram results
Head CT angiography (CTA) was performed on 100 (33.1%) of the 302 included patients as part of routine ED care. Twenty-two (7.28%) of these patients had an aneurysm visualized on CTA. Of the 22 patients with an aneurysm, 2 (9.09%) patients had a SAH diagnosed based on LP results.
3.5. Subgroup Population with low-risk clinical features
Two hundred forty-five (81.1%) of the included patients had low-risk clinical features for SAH, defined as a normal mental status and no known history of aneurysm or prior SAH. The following patients included in the full study population were excluded from this low risk group: 21 with acute altered mental status; 23 with a known intracranial aneurysm; 2 with a prior SAH; 10 with a known aneurysm and prior SAH; and 1 with altered mental status, a known aneurysm and prior SAH (Figure). Within this low risk population, none of the patients were found to have SAH and 13 (5.31%) had LP-related complications.
4. Discussion
In our three-year study in one ED with approximately 65,000 adult ED visits per year, 302 patients underwent a LP during routine clinical care to evaluate for SAH after a head CT scan showed no evidence of SAH. The yield of LP for diagnosing SAH in this population was very low, with only 2 (0.66%) patients being diagnosed with SAH based on LP results. Both of these patients had high-risk clinical features for SAH, defined a priori as altered mental status, known intracranial aneurysm, or prior SAH. None of the 245 patients without high-risk features had SAH. LP-related complications resulting in repeat healthcare visits, which occurred in 18 (5.96%) patients, were more common than SAH diagnoses, but were relatively mild in severity. The majority of complications were low pressure headaches, and none of the patients experienced a hemorrhagic or infectious complication. These results suggest LP is a reasonably safe procedure in the ED, but the yield for diagnosing SAH after a normal head CT is very low, especially for patients without major risk factors for SAH, including altered mental status, known aneurysms or prior SAH.
The current clinical policy on the evaluation of headaches published by the American College of Emergency Physicians (ACEP) provides a level B recommendation (moderate clinical certainty) for performing LP to evaluate for SAH after a normal head CT in patients with a sudden onset, severe headache.3 Accumulating evidence from this and other studies suggests that a low-risk group of patients with severe headache may be identified in which LP can be safely omitted from the diagnostic workup. Similar to our findings, Perry et al8 found non-contrast head CT using a modern third-generation scanner had 100% sensitivity and specificity for SAH among 953 patients who were awake and alert in the ED and underwent CT within six hours of headache onset. Boesiger and Shiber9 found that none of the 177 patients who underwent LP after a normal head CT during one year in their ED had SAH diagnosed based on LP results. Using a systematic review of the available literature and mathematical modeling, McCormack and Hutson15 estimated that the combination of a non-contrast head CT showing no evidence intracranial hemorrhage and CT-angiogram showing no intracranial aneurysm or AVM resulted in 99.4% post-test probability of no SAH in patients presenting with a headache and intact neurologic exam.
Historically, the potential benefits of LP in the diagnostic evaluation of SAH have been emphasized due to the high risk of morbidity and mortality associated with a missed diagnosis. The mortality rate of SAH in the United States is approximately 32% and 20% of survivors have persistent cognitive impairment .16 Failure to diagnosis SAH at the first evaluation and delayed treatment are associated with increased morbidity and mortality.17,18 However, while acknowledging the gravity of a missed SAH diagnosis, informed conversations with patients about the utility of LP require consideration of potential risks associated with the procedure as well as potential benefits. 19-22 Some potential complications include infection and hemorrhage at the puncture site, low pressure headache, pain associated with the puncture, damage to surrounding structures, and equivocal LP results leading to further unnecessary testing. In our series of 302 patients undergoing LP to evaluate for SAH, no patients were discovered to have an infectious or hemorrhagic complication from the procedure. LP-related complications, which included low pressure headaches, localized pain and contaminated CSF cultures, led to repeat visits for 5.96% of patients in our study.
Interestingly, LP led to several alternative diagnoses other than SAH in patients included in our study, including five cases of bacterial meningitis. Detailed review revealed each of these five patients presented with signs and symptoms suggestive of a central nervous system infection. These infectious signs and symptoms would likely to have led clinicians to LP even if they were not concerned about SAH. However, this is an important reminder that even if the number of LPs can be reduced in the ED without missing more cases of SAH, alternative etiologies of headache that depend on LP for diagnosis should be carefully considered before electing not to pursue LP.
4.1 Limitations and future directions
The retrospective design of our study introduced several limitations. We systematically evaluated the electronic medical record to identify ED patients with clear documentation showing LP was performed to evaluate for SAH. Additional patients who underwent LP to evaluate for SAH may have not been included in our study due to lack of specific documentation in the medical record regarding the indication for LP. Complications leading to repeat visits at our medical center were captured, but LP-related complications resulting in visits to other hospitals were not systematically captured. While local healthcare access patterns suggest patients with a complication related to a LP performed at our hospital would likely have returned to the same hospital, we cannot exclude the possibility of complications being treated at other facilities. We did not evaluate patients who underwent a head CT without an LP. Therefore, we cannot comment on the accuracy of CT to identify SAH, but only the yield of LP for SAH in our study population, which was limited to patients who had both a CT and LP completed. The study was conducted in a single academic hospital in the United States with real-time interpretation of head CT scans by board-certified radiologists; evaluation in other clinical settings is also needed.
Future work should include continuous re-assessment of the utility of LP to evaluate for SAH as the sensitivity of CT for SAH continues to improve.23 Additionally, development of an informed consent template could help clinicians discuss the risks and benefits of LP with patients in an evidence-based manner when obtaining consent for the procedure.
4.2 Conclusions
The yield of LP for diagnosing SAH after a normal head CT in ED patients presenting with headache is very low, particularly for patients without a major risk factor for SAH, such as altered mental status, known intracranial aneurysm or prior SAH. LP remains an important procedure to evaluate for other causes of headache, including meningitis and elevated intracranial pressure, but routine use of LP after CT scanning to assess for SAH in patients presenting with headache may not be advisable.
Acknowledgments
W.H.S is partially funded by a grant from the National Institute of General Medical Sciences (K23GM110469). C.D.M and M.J.W are partially funded by a grant from the National Heart, Lung, and Blood Institute (K12HL109019).
Funding: Dr. Self is partially supported by a grant from the National Institute of General Medical Sciences (K23GM110469 to WHS). Drs. McNaughton and Ward are supported by a grant from the National Heart, Lung, and Blood Institute (K12HL109019).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Goldstein JN, Camargo CA, Pelletier AJ, Edlow JA. Headache in United States Emergency Departments: Demographics, Work-up and Frequency of Pathological Diagnoses. Cephalalgia. 2006;26:684–90. doi: 10.1111/j.1468-2982.2006.01093.x. [DOI] [PubMed] [Google Scholar]
- 2.Perry JI, Stiell IG, Sivilotti ML, Bullard MJ, et al. Clinical Decision Rules to Rule Out Subarachnoid Hemorrhage for Acute Headache. JAMA. 2013;310:1248–255. doi: 10.1001/jama.2013.278018. [DOI] [PubMed] [Google Scholar]
- 3.Edlow JA, Panagos PD, Godwin SA, Thomas TL, et al. Clinical Policy: Critical Issues in the Evaluation and Management of Adult Patients Presenting to the Emergency Department With Acute Headache. Ann Emerg Med. 2008;52:407–36. doi: 10.1016/j.annemergmed.2008.07.001. [DOI] [PubMed] [Google Scholar]
- 4.Sidman R, Connolly E, Lemke T. Subarachnoid Hemorrhage Diagnosis: Lumbar Puncture Is Still Needed When the Computed Tomography Scan Is Normal. Acad Emerg Med. 1996;3:827–31. doi: 10.1111/j.1553-2712.1996.tb03526.x. [DOI] [PubMed] [Google Scholar]
- 5.Byyny RL, Mower WR, Shum N, Gabayan GZ. Sensitivity of Noncontrast Cranial Computed Tomography for the Emergency Department Diagnosis of Subarachnoid Hemorrhage. Ann Emerg Med. 2008;51:697–703. doi: 10.1016/j.annemergmed.2007.10.007. [DOI] [PubMed] [Google Scholar]
- 6.Marx JA, Hockberger RS, Walls RM, et al. Chapter 20: Headache In Rosen's Emergency Medicine: Concepts and Clinical Practice. 8th. Philadelphia: Elsevier Saunders; 2014. pp. 170–75. [Google Scholar]
- 7.Backes D, Rinkel GJE, Kemperman H, Linn FHH, et al. Time-Dependent Test Characteristics of Head Computed Tomography in Patients Suspected of Nontraumatic Subarachnoid Hemorrhage. Stroke. 2012;43:2115–119. doi: 10.1161/STROKEAHA.112.658880. [DOI] [PubMed] [Google Scholar]
- 8.Perry JJ, Stiell IG, Sivilotti MLA, Bullard MJ, et al. Sensitivity of Computed Tomography Performed within Six Hours of Onset of Headache for Diagnosis of Subarachnoid Haemorrhage: Prospective Cohort Study. BMJ. 2011;343:D4277. doi: 10.1136/bmj.d4277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Boesiger BM, Shiber JR. Subarachnoid Hemorrhage Diagnosis by Computed Tomography and Lumbar Puncture: Are Fifth Generation CT Scanners Better at Identifying Subarachnoid Hemorrhage? JEM. 2005;29:23–27. doi: 10.1016/j.jemermed.2005.02.002. [DOI] [PubMed] [Google Scholar]
- 10.Gilbert EH, Lowenstein SR, Kozio-McLain J, Barta DC, Steiner J. Chart reviews in emergency medicine research: Where are the methods? Ann Emerg Med. 1996;27:305–308. doi: 10.1016/s0196-0644(96)70264-0. [DOI] [PubMed] [Google Scholar]
- 11.Kaji AH, Schriger D, Green S. Looking through the retrospectoscope: Reducing bias in emergency medicine chart review studies. Ann Emerg Med. 2014;64:292–298. doi: 10.1016/j.annemergmed.2014.03.025. [DOI] [PubMed] [Google Scholar]
- 12.Olesen J, Bousser MG, Diener HC, et al. The International Classification of Headache Disorders. Headache Classification Subcommittee of the International Headache Society. (2nd) 2005:111–29. [Google Scholar]
- 13.Landis JR, Koch CG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–174. [PubMed] [Google Scholar]
- 14.Dupont WD, Plummer WD. Power and sample size calculations: A review and computer program. Controlled Clinical Trials. 1990;11:116–28. doi: 10.1016/0197-2456(90)90005-m. [DOI] [PubMed] [Google Scholar]
- 15.Mccormack RF, Hutson A. Can Computed Tomography Angiography of the Brain Replace Lumbar Puncture in the Evaluation of Acute-onset Headache After a Negative Noncontrast Cranial Computed Tomography Scan? Acad Emerg Med. 2010;17:444–51. doi: 10.1111/j.1553-2712.2010.00694.x. [DOI] [PubMed] [Google Scholar]
- 16.Connolly ES, Rabinstein AA, Carhuapoma JR, et al. Guidelines for the management of aneurysmal subarachnoid hemorrhage: A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2012;43:1711–1737. doi: 10.1161/STR.0b013e3182587839. [DOI] [PubMed] [Google Scholar]
- 17.Kowalski RG, Claassen J, Kreiter KT, et al. Initial misdiagnosis and outcome after subarachnoid hemorrhage. JAMA. 2004;291:866–9. doi: 10.1001/jama.291.7.866. [DOI] [PubMed] [Google Scholar]
- 18.Phillips TJ, Dowling RJ, Yan B, et al. Does treatment of ruptured intracranial aneurysms with 24 hours improve clinical outcome? Stroke. 2011;42:1936–45. doi: 10.1161/STROKEAHA.110.602888. [DOI] [PubMed] [Google Scholar]
- 19.Doherty CM, Forbes RB. Diagnostic Lumbar Puncture. Ulster Med J. 2014;83:93–102. [PMC free article] [PubMed] [Google Scholar]
- 20.Shah KH. Incidence of Traumatic Lumbar Puncture. Acad Emerg Med. 2003;10:151–54. doi: 10.1111/j.1553-2712.2003.tb00033.x. [DOI] [PubMed] [Google Scholar]
- 21.Perry JJ, Stiell I, Wells G, Spacek A. Diagnostic test utilization in the emergency department for alert headache patients with possible subarachnoid hemorrhage. Canadian Journal of Emergency Medicine. 2002;4:333–7. doi: 10.1017/s1481803500007739. [DOI] [PubMed] [Google Scholar]
- 22.Evans RW. Complications of lumbar puncture. Neurol Clin. 1998;16:83–105. doi: 10.1016/s0733-8619(05)70368-6. [DOI] [PubMed] [Google Scholar]
- 23.Ward MJ, Bonomo JB, Adeoye O, Raja AS, Pines JM. Cost-effectiveness of diagnostic strategies for evaluation of suspected subarachnoid hemorrhage in the emergency department. Acad Emerg Med. 2012;19:1134–44. doi: 10.1111/j.1553-2712.2012.01455.x. [DOI] [PubMed] [Google Scholar]


