Abstract
The current study examined parent perceptions of communication, the focus of early intervention goals and strategies, and factors predicting the implementation of augmentative and alternative communication (AAC) for 26, 2-year-old children with cerebral palsy. Parents completed a communication questionnaire and provided early intervention plans detailing child speech and language goals. Results indicated that receptive language had the strongest association with parent perceptions of communication. Children who were not talking received a greater number of intervention goals, had a greater variety of goals, and had more AAC goals than children who were emerging and established talkers. Finally, expressive language had the strongest influence on AAC decisions. Results are discussed in terms of the relationship between parent perceptions and language skills, communication as an emphasis in early intervention, AAC intervention decisions, and the importance of receptive language.
Keywords: Cerebral palsy, Parent perceptions, Early language intervention, Augmentative and alternative communication
Cerebral palsy is a complex and heterogeneous disorder that places children at increased risk for a variety of speech and language problems. Although motor impairment is a defining feature of cerebral palsy, difficulties with communication are also a key feature of the disorder. Children with cerebral palsy present with a variety of speech and language profiles. They may have no speech motor involvement and typical language/cognition or may be unable to speak, with a wide range in between (Hustad, Gorton, & Lee, 2010). Estimates from a large study of European children with cerebral palsy indicate that 60% exhibit some type of communication difficulty (Bax, Tydeman, & Flodmark, 2006). In a recent study of 2-year-old children with cerebral palsy from the United States, Hustad, Allison, McFadd, and Riehle (2014) found that 85% of the children in their cohort had clear and significant speech and language impairments. In this study, Hustad et al. (2014) identified three distinct speech and language profile groups among 2-year olds: not yet talking, emerging talkers, and established talkers. Children in these three profile groups showed consistent differences on expressive language measures but receptive language was not a significant differentiating variable among the groups.
What is unknown from the Hustad et al. (2014) study is how parents perceived their children’s communication skills and what types of speech and language intervention services they received, particularly whether children received intervention supporting Augmentative and Alternative Communication (AAC). This is especially important given the role parents can play in a child’s language development. In the United States, a key focus of early intervention services is on promoting parental competence in fostering children’s learning and development. Additionally, the combination of motor impairment and communication difficulties that often co-occur in children with cerebral palsy puts them at risk for being unable to meet all of their communication needs using speech. For these young children the introduction of AAC in early intervention is an important and essential part of facilitating speech and language development as well as providing a modality for successful communication (Cress & Marvin, 2003; Light & McNaughton, 2012b; Romski & Sevcik, 1993). Using the same sample of 2-year-old children from the Hustad et al. (2014) study, the primary aims of the current study were to (a) examine parent perceptions of their children’s communication skills and the relationship of parent perceptions to children’s observed language skills; and (b) examine the focus of children’s early intervention plans, including factors that influenced the likelihood of implementing AAC in early intervention.
Parent Perceptions of Communication
Parents can provide important information about their children’s communication skills that can both supplement and expand on formal testing. Despite evidence regarding the role that parents can play in fostering their child’s language development (Vygotsky, 1978; Yoder & Warren, 2002; Romski et al., 2011), only a few studies have examined how parents perceive their children’s communication skills. Smith, Romski, Sevcik, Adamson, and Bakeman (2011) found that for young children with disabilities who produced fewer than ten words, parent perceptions about the severity of their children’s communication difficulties had a stronger relationship with expressive than receptive language. The few other studies examining parent perceptions of children’s communication skills have been qualitative. Brady, Skinner, Roberts, and Hennon (2006) found that parents described challenges surrounding their children’s communication that were primarily related to difficulty understanding their wants and needs, and frustrations related to obtaining speech and language services for their children. Marshall and Goldbart (2008) interviewed parents of children with significant communication difficulties in England and found that they expressed a high level of knowledge about their children and also found successful ways to communicate with their children.
Early Speech and Language Intervention for Children with Cerebral Palsy
The literature on early intervention speech and language services received by children with cerebral palsy is extremely limited. Children with cerebral palsy experience a range of difficulties and routinely participate in a variety of therapies in early intervention including physical therapy, occupational therapy. They also often undergo other medical or surgical procedures beginning early in the first year of life (Palisano et al., 2012; McLellan, Cipparone, Giancola, Armstrong, & Bartlett, 2012). Because speech and language impairments may not be readily observable until the beginning of the second year of life, parents and professionals may prioritize other therapies and procedures aimed at improving children’s gross motor skills over communication intervention. Chiarello et al. (2010) conducted a large study at various sites around the United States to examine family priorities in intervention for children with cerebral palsy. The authors found that in terms of daily activities, families reported the lowest number of priorities for communication, which was ranked third (n=14) behind self-care (n=132) and mobility (n=52). Qualitative research in this area allows for more detailed information regarding emphasis for intervention. Marshall and Goldbart (2008) found that parents in England varied in how much they emphasized communication over other issues their children were facing. Pennington and Noble (2010) interviewed parents of pre-school children with motor disorders who participated in a parent training program for communication in England and found that some parents were not ready to make communication a priority. Instead, they preferred to wait and see if communication and language developed without intervention. Conversely, other parents felt that through the program their own views evolved and they came to realize that in addition to focusing on physical skills such as walking, communication also needed to be a top priority. Additionally, although parents were positive about the outcomes of communication intervention, they found it demanding in terms of time and organization. The authors suggested that parents participating in language interventions should be at a point where they are ready to prioritize communication rather than focusing on other skills and turning to communication later in the intervention process. This underscores the importance of understanding how parents view the communication skills of their children and examining the specific types of early intervention speech and language services that children with cerebral palsy receive. Such information will allow for a better understanding of how parents as well as therapists emphasize communication.
AAC for Children with Cerebral Palsy
For children with cerebral palsy, the incorporation of AAC is one aspect of a larger focus on supporting and developing a child’s full range of communication skills (Pennington, 2008; Clarke & Price, 2012). However, very few studies have specifically examined the types of AAC services utilized by children with cerebral palsy. As a whole, these few studies highlight that a significant number of children with cerebral palsy who could benefit from AAC were either not receiving any AAC services, did not have access to high quality types of AAC, or did not receive services at an early age due to difficulties with identification of speech and language problems (Andersen, Mjøen, & Vik, 2010; Cockerill et al., 2014; Sigurdardottir & Vik, 2011). These studies took place outside of the United States (Norway, United Kingdom, and Iceland), primarily examined AAC use in older children and adolescents, and suggested that AAC use was based on the expressive skills of the children with cerebral palsy. Findings from another study in the United States suggest that children with cerebral palsy may be underserved with respect to receiving AAC interventions. Hustad and Miles (2010) examined speech and language services among 4-year-old children with cerebral palsy and found that just over half of the children who needed AAC actually had AAC-focused objectives in their Individual Education Plans (Hustad & Miles, 2010). This is particularly concerning given that the majority of children with cerebral palsy are likely to have speech and/or language impairments (Bax et al., 2006; Hustad et al., 2014). By the time delays become clearly observable around age 2, there may be missed opportunities for early intervention to reduce deficits. Taking a “wait and see” approach does not give children access to alternative modes of communication that can support later language learning (Cress & Marvin, 2003, p. 255).
Researchers acknowledge that introducing AAC to children with cerebral palsy at an early age is challenging, but necessary to optimize communication and language skills (Geytenbeek, 2011). Some parents whose older children with cerebral palsy were using AAC even reported that they wished AAC had been introduced to their children earlier (Marshall & Goldbart, 2008). Current recommendations from the larger disability literature suggest introducing AAC as early as possible and involving parents in the process (Cress, 2004; Light & Drager, 2012; Light & McNaughton, 2012a, 2012b). Interventions utilizing AAC approaches allow young children to develop functional communication skills and promote the development of both receptive and expressive language skills (Drager, Light, & McNaughton, 2010; Romski & Sevcik, 2003). Importantly, research shows that introducing AAC at an early age does not seem to hinder the development of speech (Romski et al., 2010; Millar, Light, & Schlosser, 2006; Schlosser & Wendt, 2008). Therefore, it is important to examine AAC experience in very young children with cerebral palsy to determine whether they are receiving AAC services and to examine child factors that may influence the likelihood that AAC strategies were incorporated into a child’s early intervention plan.
Research Questions
In the present study, we examined parents’ perceptions about their children’s communication, the focus of early intervention services, and AAC decisions, for the cohort of young children with cerebral palsy who are described in Hustad et al. (2014). We addressed two broad research questions that focused on parental perceptions of communication and early intervention supports. The questions were:
What were parents’ perceptions of their children’s communication skills and were perceptions different for children in the three profile groups identified by Hustad et al. (2014)? Was there an association between expressive and receptive language of the children with cerebral palsy and how parents perceived their children’s communication skills?
How many 2-year-old children with a diagnosis of cerebral palsy received early intervention services that targeted speech and language skills? Specifically, among profile groups described by Hustad et al. (2014), what was the nature of the interventions these children received? How many received intervention incorporating AAC goals and strategies? What was the impact of receptive and expressive language on the likelihood that a child would be recommended for AAC goals and strategies?
Method
Participants
Participants for the current study were the same sample of children with cerebral palsy and their parents as described in Hustad et al. (2014). In that study, three different profile groups were identified within a cohort of 27, 2-year-old children with cerebral palsy, based on their performance on a variety of speech and language measures. The profile groups were: not yet talking (n =12), emerging talkers (n =11), and established talkers (n =4). Children in these profile groups showed consistent differences on expressive language measures. Specifically, all three groups differed significantly on number of words produced, percent intelligible utterances, and number of different words. Children in the emerging and established talker group did not differ significantly on MLUm or number of vocal utterances. Receptive language was more variable and did not differ significantly among the groups. Further information and analyses about profile group formation can be found in Hustad et al. (2014). One child from the emerging talker group in the original sample of 27 children was omitted from the current study because his parents did not complete questionnaires or provide documentation regarding therapy services. Therefore, data from 26 children (n =10 in the emerging talker group) and their parents were used for the current study. The children were also part of a larger prospective longitudinal study of communication development in children with cerebral palsy. Participants were recruited throughout the upper Midwestern region of the United States via local and regional neurology and physical medicine and rehabilitation clinics. They were a heterogeneous sample of children with cerebral palsy representing the full range of speech and language skills. Inclusion criteria for the larger study required that children have a medical diagnosis of cerebral palsy as well as hearing within normal limits.
The current study expands on the findings of Hustad et al., (2014) by adding data provided by parents regarding their perceptions of their children’s communication, and chart data examining early intervention speech and language services (including AAC) received by children with cerebral palsy. The sample consisted of 13 boys and 13 girls between the ages of 24 and 29.5 months (M CA = 27.11, SD=1.75). Table 1 presents demographic characteristics for all children, including age, adjusted age (for children born prematurely), Gross Motor Function Classification System Rating (Palisano et al., 1997), and receptive and expressive language skills. Other developmental levels beyond speech and language were not directly assessed because of time and behavioral constraints associated with the length of the protocol designed to characterize speech motor and language development. Within the group, 24 of the parents and their children were Caucasian and two were African-American. Ten of the parents in the sample reported that they had received a high school degree, four parents had received a 2-year associates degree, seven parents had received a 4-year bachelors degree, and five parents had received an advanced degree. All children spoke English as their first language.
Table 1.
Demographic Characteristics of Children with CP by Profile Group
| Profile | Child | CA | Adj Age | Sex | GMFCS | PLS SS | PLS Raw | MLUm |
|---|---|---|---|---|---|---|---|---|
| Not yet talking | 1 | 25.5 | NA | F | 5 | 50 | 10 | 0 |
| 2 | 27.9 | NA | M | 4 | 71 | 21 | 0 | |
| 3 | 26.5 | NA | M | 5 | 50 | 13 | 0 | |
| 4 | 24.5 | 22.1 | F | 5 | 53 | 10 | 0 | |
| 5 | 28.7 | 25.3 | F | 4 | 55 | 16 | 0 | |
| 6 | 26.8 | 22.9 | M | 4 | 74 | 19 | 0 | |
| 7 | 24.3 | NA | F | 5 | 111 | 34 | 0 | |
| 8 | 27.6 | 26.4 | M | 5 | 53 | 15 | 0 | |
| 9 | 24.8 | NA | F | 5 | 50 | 9 | 0 | |
| 10 | 26.6 | NA | M | 1 | 81 | 25 | 0 | |
| 11 | 29.3 | NA | M | 5 | 50 | 11 | 0 | |
| 12 | 29.9 | NA | M | 5 | 50 | 12 | 0 | |
|
| ||||||||
| Emerging talkers | 13 | 27.6 | 23.6 | F | 2 | 118 | 30 | 1.22 |
| 14 | 26.9 | 22.9 | M | 1 | 66 | 16 | 1.40 | |
| 15 | 28.4 | 26.0 | M | 3 | 111 | 34 | 1.16 | |
| 16 | 27.6 | NA | F | 3 | 75 | 22 | 1.05 | |
| 17 | 28.8 | NA | F | 2 | 57 | 17 | 1.00 | |
| 18 | 26.9 | NA | F | 1 | 84 | 24 | 1.28 | |
| 19 | 29.6 | 27.8 | F | 4 | 114 | 35 | 1.00 | |
| 20 | 24.6 | NA | F | 2 | 108 | 27 | 1.40 | |
| 21 | 26.9 | NA | M | 1 | 61 | 19 | 1.00 | |
| 22 | 29.4 | 26.5 | M | 5 | 71 | 21 | 1.03 | |
|
| ||||||||
| Established talkers | 23 | 29.6 | 27.0 | M | 4 | 77 | 23 | 2.24 |
| 24 | 24.5 | 22.4 | F | 3 | 106 | 24 | 1.23 | |
| 25 | 27.5 | NA | F | 1 | 87 | 27 | 1.41 | |
| 26 | 25.0 | NA | M | 1 | 87 | 27 | 1.40 | |
Note. Adj age = age adjusted for prematurity. GMFCS = Gross Motor Function Classification System. PLS SS = Preschool Language Scale (4th ed.) Standard Score. MLUm = mean length of utterance in morphemes.
Procedure
As part of the larger longitudinal study, each child participated in a data collection session between the ages of 24 and 29 months. The session lasted approximately 2 hr and was conducted by a certified speech-language pathologist (SLP). Child language scores for the current study were obtained as part of this data collection session and are also reported in the paper describing profile groups (Hustad et al., 2014). Additional questionnaires were mailed to parents to be completed prior to the data collection session. These measures collected information about the children’s communication skills, therapies, gross and fine motor skills, and feeding. Parents also provided information about the intervention services their children received. This included copies of the Individual Family Service Plan (IFSP). This is a document that was developed in accordance with the Individuals with Disabilities Act (IDEA), a federally mandated statute in the United States that entitles each student with a disability to a free and appropriate public education to meet his or her unique needs. The IFSP is specifically targeted to infants and toddlers and is a collaborative document between the child’s early interventionist and the parent where they work together to determine appropriate goals and strategies for the child (Hebbeler et al., 2007). Parents also provided any other reports written by the child’s SLP, physical therapist, and occupational therapist.
Materials
Child measures
Two speech and language measures were used for the current study. Both of these language measures were collected and used to create the speech and language profile groups identified in the previous study by Hustad et al., (2014).
Receptive language was measured using the auditory comprehension subscale of the Preschool Language Scale-Fourth Edition (PLS-4; Zimmerman, Steiner, & Pond, 2002). The PLS-4 was designed to measure early language skills for children between the ages of 2 days to 6;11 (years; months). Because several of the children in this study had significant motor impairments, standard administration procedures for the PLS-4 were adapted to enable participation in testing for items involving manual manipulation on a child-by-child and item-by-item basis. This measure yields raw scores, standard scores, and age equivalents. Raw scores were used for analyses in the current study for two main reasons. First, a significant number of children scored in the low range on this measure and raw scores allow for a greater amount of variability in scores; second, converting raw scores to standard scores is problematic if administration procedures have been adapted.
Expressive language was measured using mean length of utterance in morphemes (MLUm). Due to sample size considerations we were only able to choose one expressive language variable for use in the current study. Although MLUm was not significantly different between the emerging and established talker group, we chose it as our expressive language variable for two reasons. First, as outlined in Hustad et al. (2014), MLUm was the expressive language variable that made the strongest contribution to profile group membership for these children; second, it had the lowest amount of overall variability compared to the other measures. Additionally, MLU is one of the most robust indices of young children’s language acquisition and is particularly valuable when studying children with language impairments (Rice et al., 2010). MLUm was obtained from a 10-min parent-child interaction sample that was completed during the assessment battery and transcribed using the Systematic Analysis of Language Transcripts (SALT; Miller & Chapman, 1985).
Parent measures
To examine parent perceptions of communication skills, we used a communication questionnaire parents completed prior to the data collection session that was designed to elicit information about children’s communication skills. We chose two questions from this measure for the current study: How well is your child able to communicate familiar information using any mode of communication; and How well is your child able to communicate wants and needs using any mode of communication? These questions were scored on an ordinal 7-point Likert scale ranging from 0 (completely unable) to 6 (very well). Lower scores indicated that children had more difficulty with communication while higher scores indicated that children had less difficulty with communication.
Characterizing speech and language services
To determine the types of early intervention speech and language services each child received, we utilized each child’s IFSP or private therapy reports if the IFSP was not available. Twenty-one children had an IFSP on file, four children had private therapy reports, and one child had both an IFSP and a private therapy report. In these reports, we located all goals written by the children’s SLP. The categories derived by Hustad and Miles (2010) in their study of 4-year-old children with cerebral palsy were used as a guide for the current study. In that study, the authors categorized speech and language goals that characterized each child’s Individual Education Plan, (an educational document in the US for children between the ages of 4–21 years). The current study utilized IFSP data because children were younger and did not yet have an Individual Education Plan. Although these two documents share similar features, they are fundamentally different in terms of goals and settings where they apply. IFSPs typically include goals that focus on foundational skills to reduce the underlying impairment (feeding and oral motor skills), and goals that are specifically focused on communication. Therefore, the categories obtained by Hustad and Miles (2010) were used as a guide and categories were modified as appropriate for younger children. For example, goals targeting AAC might be similar on both an IEP and an IPSP but goals that focus on feeding and parent education might only be seen on an IFSP. Categories and operational definitions are provided in Table 2.
Table 2.
Operational Definitions of Speech and Language Goals
| Goal area | Operational definition |
|---|---|
| Receptive language | Goals/objectives targeting the ability to understand or express spoken language using a verbal (speech) modality. This category includes goals related to expressive or receptive vocabulary, semantics, and morphology; concepts (e.g., under, more, big); questions, directives, comprehension; and production of objects/labels, and classification. Examples include increasing vocabulary (including vocalizations and/or vocal play), combining words, and identifying objects and pictures. Use of aided or unaided AAC is excluded from this category. All goals in this category imply or directly state that speech is the target modality of expression. |
| Social communication | Goals/objectives targeting the ability to use language (appropriately and functionally) in multiple settings and with a variety of communication partners. This category includes goals that address social communication in some type of meaningful context. Examples include using music, singing, and social games to participate in group activities; responding appropriately to others; participating in cooperative or parallel play; and attending to communication partners. Use of aided or unaided AAC is excluded from this category. |
| Cognitive development | Goals/objectives targeting the ability to coordinate and use attention, problem-solving and executive functioning skills in various aspects of communication. This category includes goals related to object awareness, object discrimination, development of cause and effect, visual tracking, appropriate play with objects, and consistent response to stimuli and/or communication partners. Use of aided or unaided AAC is excluded from this category. |
| Phonology/articulation | Goals/objectives targeting the ability to produce speech sounds either in isolation or in spoken words or utterances. This category includes goals related to improvement in speech production at the phoneme, syllable, or word level. This category may include goals related to increasing the number of phonemes in a repertoire, correct placement of articulators during speech production, and/or correct production/approximation of target phonemes in the repertoire. Goals related to speech intelligibility are excluded from this category. |
| Intelligibility | Goals/objectives targeting the ability to produce intelligible speech. Goals related to improving overall understandability of speech and those related to consistent production and/or approximations of expressive vocabulary (not target phonemes) are included in this category. |
| Aided AAC | Goals/objectives targeting the ability to use alternative and/or supplemental communication systems to advance functional communication abilities or support language development. The use of aided communication modalities other than speech automatically qualifies as a goal for inclusion in this category. Examples include low-technology boards, switches, high-technology devices, and other aided communication modalities. Any mention of specific AAC devices or strategies qualifies as a goal for inclusion in this category. |
| Unaided AAC | Goals/objectives targeting the ability to use alternative and/or supplemental communication systems to advance functional communication abilities or support language development. The use of unaided communication modalities other than speech qualifies as a goal for inclusion in this category. Examples include facial expression, sign, eye gaze, and gestures. Any mention of an AAC device is excluded from this category. |
| Oral-motor skills | Goals/objectives targeting the ability to develop and/or increase strength, range of motion, sensation or coordination of oral muscles using non-speech tasks (tongue/blowing exercises, passive stimulation activities). Goals that mention the use of oral-motor exercises or tolerating different kinds of oral stimulation are included here. Also goals that address blowing and sucking (for non-nutritive purposes) are included here. |
| Feeding | Goals/objectives targeting the ability to acquire food for nutritional purposes. Includes goals related to sucking, chewing, or swallowing. |
| Parent education | Goals included those that are specifically targeted towards giving parents strategies that they can use at home to facilitate their child’s communication and language skills. |
| Miscellaneous | Goals that are not directly related to any of the other categories but are included in the IFSP. Examples include behavioral management, medical management, etc. |
Note. Adapted from Hustad and Miles (2010).
Analysis Plan
The analysis approach for this study was two-fold. To address the first set of research questions, we utilized the non-parametric Kruskal-Wallis test to analyze differences in parent perceptions among profile groups. The non-parametric statistic was used due to the small and unequal group sizes and violations of homogeneity of variance. We also examined correlations between parent perceptions of communication and expressive language as measured by MLUm, and receptive language as measured by the raw score from the auditory comprehension subscale of the PLS-4. Based on these correlations we used standard multiple regression to determine if expressive or receptive language skills were associated with parent perceptions of their children’s communication skills. MLUm and the raw score of the PLS were significantly positively correlated, r = .51, p =.007, but the magnitude of the correlation was not indicative of multicollinearity. The dependent variables were parent responses to the questions, How well is your child able to communicate familiar information using any mode? and How well can your child communicate wants and needs using any mode? Although parent perception data were ordinal and the language measures were interval in nature, research suggests that correlation and regression are robust with respect to departure from linear, normal distributions (Carifio & Perla, 2008; Norman, 2010). Because of the exploratory nature of this study, an alpha level of .05 was assigned to each regression analysis.
To address the second set of research questions we used thematic analysis (Bogden & Biklen, 1992; Cresswell, 2003) to characterize the specific types of speech and language services received by children. This qualitative methodology allowed us to examine the types of speech and language intervention goals and strategies that children received and how this related to their specific communication profiles. This was particularly important for examining the AAC goals and strategies that children received and if children who could benefit from AAC received those services as part of their early intervention plans. First, all speech and language goals written by the child’s SLP were located in the child’s IFSP or private therapy reports. All goals and objectives were then transcribed, verbatim, into a database and organized using the qualitative software package NVivo (QSR International, 2012).
Using the operational definitions, the first author placed each early intervention speech and language goal into one of the mutually exclusive categories. An undergraduate research assistant with experience observing children with cerebral palsy was also trained to code the goals and objectives. The training involved giving the research assistant access to the categories and operational definitions and discussing each one to ensure that the differences between each category were understood. That individual then coded all goals and objectives into the operationally defined categories. Finally, the first author and research assistant discussed the results, and agreement between these raters was 86.2% (as determined by the number of codes agreed upon divided by total number of codes). Discrepancies between the raters on coded responses were resolved through discussion and consensus.
For the last analysis examining AAC intervention decisions, we used a univariate binary logistic regression model to assess the impact of receptive and expressive language on the likelihood that a child would be recommended for AAC. The independent variables were expressive language as measured by MLUm, and receptive language as measured by the raw score from the auditory comprehension subscale of the PLS-4. The dependent variable was whether the child received AAC goals and strategies as part of his or her early intervention plan. There were two possible responses: No (coded as 0) and Yes (coded as 1).
Results
Parent Perceptions of Communication
Descriptive results for study variables are presented in Table 3. Parents of children in the not talking group reported that their children had more difficulty communicating familiar information as well as wants and needs than parents of children who were emerging talkers, who in turn, had more difficulty than established talkers. However, results of the Kruskal-Wallis test indicated that the differences among profile groups were not statistically significant for how well children communicated familiar information, χ2 (2, N = 26) = 3.98, p= .14, or how well children communicated wants and needs, χ2 (2, N = 26) = 2.87, p= .24.
Table 3.
Descriptive Results for Study Variables by Profile Group
| Not talking (n = 12) | Emerging talkers (n = 10) | Established talkers (n=4) | |
|---|---|---|---|
|
|
|||
| Variable | M (SD) | M (SD) | M (SD) |
| MLUm | 0 | 1.15 (.16) | 1.57(.45) |
| PLS Raw | 16.25 (7.45) | 24.50 (6.79) | 25.25 (2.06) |
| Familiar information | 2.92 (2.64) | 4.60 (1.90) | 5.75 (.50) |
| Wants and needs | 3.17 (2.29) | 4 (1.83) | 5.25 (.50) |
Note. PLS Raw = Preschool Language Scale (4th ed.) Raw Score; MLUm = mean length of utterance in morphemes; Familiar information = How well does your child communicate familiar information using any mode? Wants and Needs = How well does your child communicate wants and needs using any mode?
There were, however, significant correlations indicating a relationship between parent perceptions and language measures. Specifically, parent perceptions about how well their children could communicate familiar information was significantly positively correlated with both MLUm, r = .45, p = .02, and PLS raw score, r = .66, p <.001. Parent perceptions about how well their children were able to communicate wants and needs were significantly positively correlated with PLS raw score, r = .59, p = .002, but not MLUm, r = .36, p = .07. Multiple regression was used to further explore these relationships and determine which language variables had the strongest association with parent perceptions. Although the relationship with MLUm for wants and needs did not reach a conventional level of significance, the moderate size of the correlation indicated its appropriateness for use in the regression analyses.
Results of the two standard multiple regression models to determine if expressive and/or receptive language were associated with parent perceptions of their children’s communication skills are presented in Table 4. For the first communication question, How well is your child able to communicate familiar information using any mode?, results indicated that the linear combination of receptive and expressive language was significantly associated with how well parents perceived their children were able to communicate familiar information, F(2, 24) = 7.58, p = .003, R2 = .65. Receptive language had the strongest and only significant association, β = 0.62, p = .004, with how well parents reported their children were able to communicate familiar information using any mode. Expressive language was not significantly associated, β = −0.06, p = .81.
Table 4.
Summary of Simultaneous Regression Analyses for Variables Predicting Parent Perceptions
| Familiar information | Wants and needs | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| B | SE B | β | B | SE B | β | |
| PLS Raw Score | 0.17 | 0.05 | 0.62** | 0.12 | 0.05 | 0.48* |
| MLU M | 0.15 | 0.62 | −0.06 | 0.36 | 0.58 | 0.13 |
| R2 | .65 | .56 | ||||
| F | 7.58** | 4.89** | ||||
p < .05.
p < .01
For the second communication question, How well can your child communicate wants and needs using any mode?, there was a similar pattern of results. The linear combination of receptive and expressive language was significantly associated with how well parents perceived their children were able to communicate their wants and needs, F(2, 24) = 4.89, p = .02, R2 = .56. Again, receptive language had the strongest and only significant association, β = 0.48, p = .03, with how well parents reported their children were able to communicate their wants and needs. Expressive language was not significantly associated, β = 0.13, p = .54.
Early Intervention and AAC Experience
Of the 26 children enrolled in this study, 77% (n = 20) received early intervention services that included speech and language therapy. Although six children were not receiving speech and language therapy services, they did receive other early intervention services including physical and/or occupational therapy. Two of these children were in the not talking group, two were in the emerging talker group, and two were in the established talker group. Of the six children not receiving therapy, three exhibited lower receptive and expressive language skills (M MLU = 0.69; M PLS SS = 72) and had a recommendation for a speech and language assessment, and three exhibited higher receptive and expressive language (M MLU = 1.12; M PLS SS = 110) and did not have a recommendation for a speech and language assessment.
Figure 1 displays the percentage of goals by each specified goal area for children in each profile group. Because of the difference in sample sizes, the total number of goals in each goal area was converted into a percentage based on the total number of goals for each group. Table 5 gives specific examples of goals from the IFSPs for children in each profile group. Children in all three groups had an equal percentage of goals that incorporated parent education and suggestions for strategies parents could use at home with their children.
Figure 1.
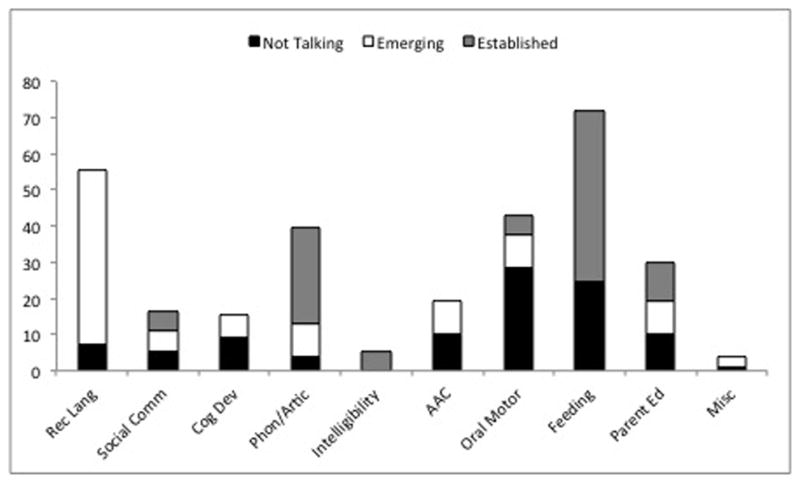
Percentage of goals received by children in each area by profile group.
Table 5.
Examples of Specific Goals on the IFSP by Profile Group
| Profile group | Goal area | Example of specific goal |
|---|---|---|
| Not yet talking | Oral-Motor | Offer teething toys to stimulate him to explore orally |
| Feeding | Slowly introduce foods with more texture – small amounts at a time | |
| Cognitive development | Understanding cause and effect; anticipate routines | |
| Aided AAC | Work on alternative communication using picture books and BIGmack1™ | |
| Unaided AAC | The team will use hand over hand assistance to help him perform signs and gestures | |
| Receptive language | Demonstrate big and little concepts | |
| Parent education | Almost every interaction throughout the day provides opportunities to model sounds, and words to label objects, people, and actions | |
| Phonology/articulation | Work on specific sounds we want him to produce using spoken language: ma, b, d, p | |
| Social communication | Use music, singing, and social games to help engage him | |
|
| ||
| Emerging talkers | Receptive language | Show an understanding of “just 1”, attributes, position words, size, etc. |
| Phonology/articulation | Visual cues for target sounds – show on face how to make the sounds | |
| Social communication | Continue modeling social language and demonstrate verbal turn-taking | |
| Cognitive development | Understanding cause and effect | |
| Aided AAC | Use picture cards to help her make choices | |
| Oral-Motor | She will participate in oral motor activities and games | |
| Parent education | Encourage him to engage in imitation | |
|
| ||
| Established talkers | Oral-Motor | Continue to offer her oral motor tools – vibrating toys and have her use it on both sides |
| Feeding | Provide hand over hand assistance when he is drinking and fade assistance over time | |
| Phonology/articulation | Reinforce her vocalization by repeating what she says and give her the correct model | |
| Social communication | Use lots of songs and finger plays to encourage socialization | |
| Intelligibility | Increase intelligibility of conversational speech milestones | |
| Parent education | Education on typical sound development and language | |
In the not yet talking group, 10 of the 12 children had goals written by an SLP. These 10 children received an average of 10 goals each as part of their early intervention plan, with a range of one to 16 goals per child. In the not yet talking group, seven of the 12 children had communication-focused goals that incorporated aided or unaided AAC. Examples of specific goals from the IFSPs include, “Work on vocal play and alternative communication (e.g., picture books, big Mac)”, “Investigate alternative communication methods to master strategies”, and “The therapist and family will come up with picture cards and start implementing communication devised to help XX communicate his needs.” As shown in Figure 1, children in this group had the highest percentage of goals focused on oral motor skills (29%) and feeding (24%). These goals target foundational skills to reduce the underlying motor impairment rather than targeting communication directly. Goals specifically related to communication primarily focused on AAC (10%), cognitive development (9%), and receptive language (7%). Children in this group had the lowest percentage of goals related to social communication (5%), and phonology/articulation (4%).
In the emerging talker group, eight of the 10 children had goals written by a speech-language pathologist. These eight children received an average of four goals each as part of their early intervention plan, with a range of one to nine goals per child. Although the percentage of goals focused on AAC was equal across the emerging and not talking group, descriptively fewer children in the emerging talker group had goals that incorporated AAC. Only one of the eight children had a goal that incorporated an aided AAC strategy. This goal read, “Use pictures to help XX make choices.” As shown in Figure 1, children in this group had goals primarily related to receptive language with other goals spread out evenly among the remaining areas.
In the established talker group, two of the four children were receiving services from a speech-language pathologist, and none of the targeted goals incorporated aided or unaided AAC strategies. As shown in Figure 1, these two children had goals that were spread out among the communication-focused goals of intelligibility, phonology/articulation, and social communication, as well as goals addressing feeding and oral motor skills. One child received eight goals that were all focused on feeding. One child received 10 goals, five of which were communication-focused (phonology, articulation, and social communication), with the rest addressing skills of feeding and oral motor skills.
AAC Intervention Decisions
Results of the univariate binary logistic regression to assess the impact of receptive and expressive language on the likelihood that a child would be recommended for AAC are presented in Table 6. The full model containing both predictor variables was statistically significant, χ2(2, N = 26) = 8.45, p =.02, indicating that the model was able to distinguish between children who were and were not recommended for AAC. The model as a whole explained between 30% (Cox and Snell R squared) and 40% (Nagelkerke R squared) of the variance in AAC intervention decisions and correctly classified 77% of the cases. As shown in Table 6, only MLUm made a unique, statistically significant contribution to the model, and was the strongest and only significant predictor of whether a child was likely to receive AAC, recording an odds ratio of 14.3. This indicated that children were 14 times more likely to receive speech and language goals involving AAC when they had a lower MLUm, controlling for receptive language.
Table 6.
Summary of Logistic Regression Analyses for Variables Predicting AAC Intervention Decisions
| Variable | B | SE B | Wald | df | p | OR | 95% CI
|
|
|---|---|---|---|---|---|---|---|---|
| Lower | Upper | |||||||
| PLS raw score | 0.43 | 0.80 | 0.28 | 1 | 0.60 | 1.04 | 0.89 | 1.22 |
| MLU M | −2.60* | 1.19 | 4.74 | 1 | 0.03 | 14.3 | 0.01 | 0.77 |
| Constant | −0.23 | 1.45 | 0.02 | 1 | 0.80 | |||
p < .05
Discussion
In the present study, we examined parents’ perceptions about their children’s communication, the focus of early intervention speech and language services, and AAC decisions for 26 young children with cerebral palsy who were at risk for expressive communication impairments. Results indicated that receptive language had the strongest association with how parents perceived their children’s ability to communicate familiar information as well as wants and needs. Children in the not talking group received a greater number of speech and language intervention goals on average, had a greater variety of goals, and had more AAC goals compared to children in the emerging talker and established talker group. Finally, expressive language was the only significant predictor of AAC intervention decisions. These findings and their implications are discussed in terms of the relationship between parent perceptions and language skills, communication as an emphasis in early intervention for children with cerebral palsy, predictors of AAC intervention decisions, and the importance of receptive language for parent perceptions and AAC.
Relationship Between Parent Perceptions and Language Skills
We found moderate to strong associations between child language skills (both receptive and expressive) and parent perceptions of communication skills, indicating that parent perceptions were accurate indicators of language skills. However, receptive language had the strongest association with how well parents reported that their children were able to communicate familiar information as well as their wants and needs. This is particularly noteworthy, given that parents responded to questions that were targeted towards expressive communication (any mode), yet it was receptive language skills that best predicted their response. Although parents were not asked to indicate in what mode their children were best able to communicate familiar information or wants and needs, it may suggest that attuning to receptive language skills provides a broader base for interpreting a variety of communicative behaviors. This finding is in contrast to the finding by Smith et al. (2011), which showed that expressive language had the strongest relationship with parent perceptions about their child’s difficulty with communication. A possible explanation for this difference is that the finding from the current study may reflect unique challenges specifically associated with cerebral palsy. Although all of the children in the Smith et al. (2011) study had significant difficulty with communication, the sample was comprised of children with a wide range of developmental disabilities, where significant delays in both receptive and expressive language are common. Children in the current study exhibited considerable variability in receptive language skills, which is not uncommon for children with cerebral palsy. Specifically, children with cerebral palsy may exhibit a more uneven profile of receptive and expressive language, with greater challenges with expressive communication secondary to speech motor impairment, as compared to receptive language (Hustad et al., 2014). Therefore, this finding may suggest that children with cerebral palsy who have better receptive language skills were able to find functional ways to communicate that parents were able to understand.
Communication as an Emphasis in Early Intervention
Findings regarding the focus of early speech and language services for young children with cerebral palsy indicate that although most children received speech and language services, the vast majority of goals were focused primarily on reducing the underlying impairment (feeding and oral-motor skills) rather than facilitating functional communication, especially for children who were not talking. The IFSP analysis indicated that children in the not talking group had the highest percentage of goals focused on improving oral motor skills and feeding. From there, a much smaller percentage of goals focused on AAC, cognitive development, receptive language, social communication, and phonology/articulation, in that order. Although it is not possible to directly infer that the percentage of goals correlates to the priority they were given by speech language pathologists, it is possible that parents and professionals may not be emphasizing communication at this early age. Rather they may be emphasizing interventions that are focused on issues seen as more immediate such as feeding and facilitating physical development. This suggestion is in line with previous research findings indicating that parents vary in how much they prioritize communication at an early age (Marshall & Goldbart, 2010), and may initially focus on intervention goals related to walking and improving their child’s physical and self-care skills rather than communication (Chiarello et al., 2010; Pennington & Noble, 2010). Additionally, parents of young children with cerebral palsy may prefer to simply wait to see if communication skills develop (Pennington & Noble, 2010).
Other findings from the IFSP analysis suggest that, although goals related to functional communication development may not have been emphasized in terms of the percentage of goals, 64% (seven of 12) of children in the not talking group did have goals that targeted AAC strategies as part of their early intervention plans. Although we only had information from the IFSP and did not speak with the SLPs directly, this finding supports previous research. Results may suggest that SLPs working with children in this study recognized the importance of AAC and were following recommendations from research for incorporating AAC at an early age for children who are exhibiting the most significant difficulties with communication (ASHA, 2004; Light & Drager, 2012; Light & McNaughton, 2012a, 2012b). In addition, findings may also suggest that professionals are listening to parents who indicate their desire for AAC to be introduced earlier (Marshall & Goldbart, 2008) and to be involved in the AAC intervention process (Granlund, Björck-Åkesson, Wilder, & Ylvén, 2008).
AAC Intervention Decisions
In this study, expressive language skills of the children with cerebral palsy predicted whether a child received early intervention that included AAC goals and strategies. Children who exhibited the most difficulty with expressive language, as measured by MLUm, were more likely to receive early intervention services that included AAC goals and strategies, which is in line with findings from previous research with older children with cerebral palsy (Cockerill et al., 2014; Sigurdardottir & Vik, 2011). This finding is not surprising and generally follows accepted clinical practice in which AAC is provided for children who are unable to use natural speech to communicate.
For the most part, this also corresponds to findings from the IFSP analysis regarding AAC for children in the not talking group, as discussed previously. However, for children in the emerging talker group, only 10% (one of 10) received any type of AAC support. This finding is consistent with previous research suggesting that there may be a systematic bias against providing AAC services to children who have any speech. Specifically, Hustad and Miles (2010) showed that fewer than half of 4-year-old children with CP who had speech in any capacity had IEPs that included AAC focused goals and objectives. It is important to emphasize that children in the present study were still significantly delayed expressively, exhibiting an average MLUm of 1.15, indicating that despite being emerging talkers, their expressive language skills were still lower than would be expected, based on their age. Rice et al. (2010) reported that 2-year-old children with typical development exhibited, on average, just over three morphemes in each of their spontaneous utterances. It is also important to note that despite considerable overlap between emerging and established talkers for MLUm, children in the established talker group were producing significantly more words according to parent report, had a greater percentage of intelligible utterances, and used a greater variety of words (Hustad et al., 2014). This indicates a greater need for the implementation of AAC goals and strategies for children in the emerging talker group. Clinically, speech-language pathologists may be inclined to focus primarily on what they can observe, that is, expressive language. In that sense, a child who is exhibiting more significant difficulty with expressive communication may be a more obvious choice to receive AAC interventions. It is possible that children in this group were more verbal overall or were meeting their communication needs in other functional ways such as pointing and gesturing, and therefore SLPs did not see the immediate need to introduce AAC strategies. However, children at 2 years of age are still in the beginning stages of language development. Even though children in this group were considered emerging talkers, they continue to be at-risk for pervasive speech and language difficulties. There is no way to predict whether these children will develop functional speech and language skills (Pennington, 2008; Hustad & Miles, 2010). Therefore it is important that therapists do not take a “wait and see approach” before introducing AAC systems and strategies (Cress & Marvin, 2003, p. 255).
Importance of Receptive Language for AAC and Parent Perceptions
Several findings from this study highlight the role that receptive language can play for both AAC and parent perceptions. First, the IFSP analysis indicated that for children in the not talking group, 36% (five of 12) were not receiving AAC services. Unifying variables among children not receiving AAC in this group were that all had significant receptive language delays, likely indicating significant developmental delay (age equivalent scores less than 10 months); all but two of the children had a significant visual impairment; and all of the children were classified at Gross Motor Function Classification (GMFCS) Levels IV or V (Palisano et al., 1997, 2000), indicating significant gross motor limitations. Children with this this type of profile can be extremely challenging to serve, and there are several possible explanations as to why they might not be receiving AAC services. First, clinicians may not know what to do to implement AAC, or where to begin, given the complex communication needs of the children. In addition, there may be a concern regarding “readiness” for communication, in spite of the well-established body of literature dispelling the myth that there are pre-requisites for AAC intervention (Cress & Marvin, 2003; Kangas & Lloyd, 1988; Light & Drager, 2012; Light & McNaughton, 2012b; Romski & Sevcik, 2005; Romski et al., 2010). For these children, it is important that speech-language pathologists and other service providers focus on supporting receptive language through AAC goals and strategies. Children exhibiting low receptive language skills can use AAC to learn meanings between symbols and their referents, which can set them on the path to producing AAC symbols and/or developing spoken language skills (Romski & Sevcik, 1996; Sevcik, 2006). It is also important to support receptive language skills in children with vision impairments. Clearly, vision issues make decision-making and intervention in AAC more difficult, especially in the presence of language and/or intellectual disability. Available literature suggests that the introduction of AAC in the form of tangible symbols for children with both visual and motor impairments can be successful for improving comprehension, communicating effectively, and act as a stepping stone to developing more sophisticated symbol systems (Roche et al., 2014).
The current study revealed contrasting findings regarding the associations between receptive and expressive language, parent perceptions, and AAC intervention decisions. The finding that receptive language had the strongest association with parent perceptions was in contrast to our finding that expressive language had the strongest influence on the likelihood that a child received early intervention that included AAC goals and strategies. These contrasting findings may suggest that therapists and parents are attuned to different aspects of children’s language skills. Therapists may be more focused on what a child is able to demonstrate expressively. Parents, on the other hand may be more attuned to what children are able to understand rather than what they are able to express. Parent responses on questions relating to expressive communication reflect an implicit knowledge of their child’s comprehension and that parents know their children very well at this age.
Implications
As a whole, results of this study have several important implications for clinical practice. First, given that receptive language skills as measured by the PLS-4 appear to have a stronger association with how well parents perceive their child is able to communicate, therapists should consider incorporating intervention strategies that focus on receptive language as well as expression. Intervention approaches such as aided language stimulation (Goossens’, 1989) and augmented input (Romski & Sevcik, 2003) include a receptive language component as part of the protocol. Both of these approaches use an input strategy whereby a picture symbol is paired with speech. In fact, early language intervention approaches such as these that foster comprehension as well as production, result in gains in both expressive and receptive communication skills (Brady, 2000; Millar et al., 2006; Dada & Alant, 2009) and can be implemented successfully with parents (Jonsson, Kristoffersson, Ferm, & Thunberg, 2011; Romski et al., 2010).
Additionally, these findings regarding receptive language underscore the important role of parents as communication partners with their children and the ability of parents to accurately interpret their children’s communication. The introduction of AAC strategies can be a complex and challenging process (Cress, 2004; Marshall & Goldbart, 2008), but parent involvement is critical for effective service delivery (Granlund et al., 2008). For AAC in particular, parents report wanting to be involved in all aspects of their children’s intervention and a desire to play a significant role in identifying their children’s AAC needs (Calculator & Black, 2010). Therapists should be cognizant of parent perceptions and how these can be effectively integrated into early intervention planning in order to maximize child outcomes.
Results of this study have clear implications for education and training regarding the different roles and various forms of AAC that are available for children with significant, multiple disabilities. It is true that the presence of a visual impairment in addition to significant motor and language impairments makes AAC assessment and intervention more challenging. There may be a significant number of therapists working with these children who do not have expertise regarding the ways that AAC can be effectively used for this population. Therefore, it will be important for graduate training programs and continuing education programs to focus on this aspect of AAC. Additionally, research is needed to determine more effective ways to approach the introduction of AAC for this population of children and ensure that those with the most significant disabilities are not overlooked in terms of providing them with a means to learn language and effectively communicate.
Limitations and Future Directions
One limitation of this study is the small sample size (N = 26). Future studies should determine if similar variables influence AAC intervention decisions and parent perceptions of communication for children with cerebral palsy. Due to the small sample size, we were unable to include other variables in our regression models that may influence AAC intervention decisions and parent perceptions, such as additional language variables that contributed to profile group membership, motor skills, and severity of disability. A second limitation was the demographic characteristics of the current sample. All of the IFSPs for this study were collected between 2006 and 2010 and were from the upper Midwest region of the United States. It is possible that services and trends might be different in other parts of the United States as well as other countries. A third limitation concerns the measures used for this study. First, MLUm as measured by parent interaction is limited by the quality of the interaction and the small number of utterances obtained in a relatively short time period (Eisenburg, Fersko, & Lundgren, 2001). It is possible that MLUm obtained for the children in this study was not a true reflection of their syntactic complexity, particularly for those in the emerging talker group. Additionally, the strong correlation between MLU and intelligibility can impact the reliability of MLU as a language measure (Rice et al., 2010). Second, the parent questions used for this study were limited by the young age of the children. For children at 2-years-old, parents may not have a clear understanding of what may be typical for that age, especially if there are no older siblings in the family. Parents may have also interpreted the questions in different ways. Both questions asked about expressive communication in any mode (which could have included signs, gestures, AAC, or speech), yet some parents’ answers may have reflected only their children’s speech. Future studies should ask parents more directly about their perceptions of children’s communication via specific modes of communication.
Finally, we did not directly measure parent perceptions of, or satisfaction with, the AAC services their children received or their child’s early intervention professionals. Parent views about their child’s communication are an important supplement to the assessment provided by early intervention professionals. Additionally, the congruence between parent and professional views could influence parents’ engagement with intervention. These are important variables that would add additional information about the parent-professional collaboration in early intervention. Future studies should directly examine early intervention experience for children with cerebral palsy as well as parents’ participation in the early intervention process. Parents may be more attuned to children’s receptive language as it pertains to how well they perceive their children are communicating functionally, whereas professionals may be more attuned to children’s expressive language, which determines AAC intervention decisions. This complementarity is especially important as it relates to beginning an AAC intervention. We have stressed the importance of the role that comprehension can play in an AAC intervention approach. If parents are more attuned to a child’s comprehension skills, this information could be useful to professionals who may be reticent or unsure about when to introduce AAC for very young children. Future studies should also focus on gaining information directly from speech-language therapists who provide early intervention services, in order to more fully understand the priority they place on intervention goals and their decision-making process when deciding to implement AAC goals and strategies with very young children.
Conclusion
In conclusion, this study indicated that, although the majority of young children with cerebral palsy received speech and language services, those in the not talking group and emerging talker group who could benefit from the incorporation of AAC goals and strategies did not universally receive them as part of their early intervention plans. Yet all could potentially benefit from AAC because of their speech and/or language delays and other risk factors associated with their diagnosis of cerebral palsy. Additionally, this study provides further support for the need to consider parent perceptions when determining early intervention AAC decisions. Parents are young children’s most frequent communication partners and if they are more attuned to what children understand, obtaining that information will be important for deciding where and when to begin AAC intervention services for young children with cerebral palsy.
Acknowledgments
This research was supported by National Institutes of Health grant R01DC009411 to Katherine C. Hustad as well as the post-doctoral training grant T32HD07489 and grant P30HD03352 to the Waisman Center from the National Institutes of Health.
Footnotes
BIGmack is a product of AbleNet, Inc. of Roseville, MN.
References
- American Speech-Language-Hearing Association. Technical Report. 2004. Roles and responsibilities of speech-language pathologists with respect to augmentative and alternative communication: Technical report. [Google Scholar]
- Andersen G, Mjøen TR, Vik T. Prevalence of speech problems and the use of augmentative and alternative communication in children with cerebral palsy: A registry-based study in Norway. Perspectives on Augmentative and Alternative Communication. 2010;19:12–20. doi: 10.1044/aac19.1.12. [DOI] [Google Scholar]
- Bax M, Tydeman C, Flodmark O. Clinical and MRI correlates of cerebral palsy: the European cerebral palsy study. Journal of the American Medical Association. 2006;296:1602–1608. doi: 10.1001/jama.296.13.1602. [DOI] [PubMed] [Google Scholar]
- Biklen SK, Bogdan R. Qualitative research for education: An introduction to theory and methods. Boston, MA: Allyn & Bacon; 1992. [Google Scholar]
- Brady N. Improved comprehension of object names following voice output communication aid use: Two case studies. Augmentative and Alternative Communication. 2000;16:197–204. doi: 10.1080/07434610012331279054. [DOI] [Google Scholar]
- Brady N, Skinner D, Roberts J, Hennon E. Communication in young children with Fragile X syndrome: A qualitative study of mothers’ perspectives. American Journal of Speech-Language Pathology. 2006;15:353–364. doi: 10.1044/1058-0360(2006/033). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calculator SN, Black T. Parents’ priorities for AAC and related instruction for their children with Angelman syndrome. Augmentative and Alternative Communication. 2010;26:30–40. doi: 10.3109/07434610903585406. [DOI] [PubMed] [Google Scholar]
- Carifio L, Perla R. Resolving the 50 year debate around using and misusing Likert scales. Medical Education. 2008;42:1150–1152. doi: 10.1111/j.1365-2923.2008.03172.x. [DOI] [PubMed] [Google Scholar]
- Chiarello LA, Palisano RJ, Maggs JM, Orlin MN, Almasri N, Kang L, Chang H. Family priorities for activity and participation of children and youth with cerebral palsy. Physical Therapy. 2010;90:1254–1264. doi: 10.2522/ptj.20090388. [DOI] [PubMed] [Google Scholar]
- Clarke M, Price K. Augmentative and alternative communication for children with cerebral palsy. Paediatrics and Child Health. 2012;22:367–371. doi: 10.1016/j.paed.2012.03.002. [DOI] [Google Scholar]
- Cockerill H, Elbourne D, Allen E, Scrutton D, Will E, McNee A, Baird G. Speech, communication and use of augmentative communication in young people with cerebral palsy: The SHAPE population study: Communication and AAC use in bilateral cerebral palsy. Child: Care, Health and Development. 2014;40:149–157. doi: 10.1111/cch.12066. [DOI] [PubMed] [Google Scholar]
- Cress CJ. Augmentative and alternative communication and language: understanding and responding to parents’ perspectives. Topics in Language Disorders. 2004;24:51–61. [Google Scholar]
- Cress CJ, Marvin CA. Common questions about AAC services in early intervention. Augmentative and Alternative Communication. 2003;19:254–272. doi: 10.1080/07434610310001598242. [DOI] [Google Scholar]
- Cress CJ. Augmentative and alternative communication and language: understanding and responding to parents’ perspectives. Topics in Language Disorders. 2004;24(1):51–61. [Google Scholar]
- Creswell JW. Research design: Qualitative, quantitative, and mixed methods approaches. Thousand Oaks, CA: Sage publications; 2013. [Google Scholar]
- Dada S, Alant E. The effect of aided language stimulation on vocabulary acquisition in children with little or no functional speech. American Journal of Speech-Language Pathology. 2009;18:50–64. doi: 10.1044/1058-0360(2008/07-0018). [DOI] [PubMed] [Google Scholar]
- Drager K, Light J, McNaughton D. Effects of AAC interventions on communication and language for young children with complex communication needs. Journal of Pediatric Rehabilitation Medicine: An Interdisciplinary Approach. 2010;3:303–310. doi: 10.3233/PRM-2010-0141. [DOI] [PubMed] [Google Scholar]
- Eisenberg SL, Fersko TM, Lundgren C. The use of MLU for identifying language impairment in preschool children: A review. American Journal of Speech-Language Pathology. 2001;10:323–342. doi: 10.1044/1058-0360(2001/028). [DOI] [Google Scholar]
- Geytenbeek J. Prevalence of speech and communication disorders in children with CP. Developmental Medicine and Child Neurology. 2011;53:10–11. doi: 10.1111/j.1469-8749.2010.03803.x. [DOI] [PubMed] [Google Scholar]
- Goossens’ C. Aided communication intervention before assessment: A case study of a child with cerebral palsy. Augmentative and Alternative Communication. 1989;5:14–26. doi: 10.1080/07434618912331274926. [DOI] [Google Scholar]
- Granlund M, Björck-Åkesson E, Wilder J, Ylvén R. AAC interventions for children in a family environment: Implementing evidence in practice. Augmentative and Alternative Communication. 2008;24:207–219. doi: 10.1080/08990220802387935. [DOI] [PubMed] [Google Scholar]
- Hebbeler K, Spiker D, Bailey D, Scarborough A, Mallik S, Simeonsson R, Nelson L. Early intervention for infants and toddlers with disabilities and their families: Participants, services, and outcomes. Final Report of the National Early Intervention Longitudinal Study (NEILS) 2007 Retrieved from http://sriinternational.mobi/sites/default/files/publications/neils_finalreport_200702.pdf.
- Hustad KC, Allison K, McFadd E, Riehle K. Speech and language development in 2-year-old children with cerebral palsy. Developmental Neurorehabilitation. 2014;17:167–175. doi: 10.3109/17518423.2012.747009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hustad KC, Gorton K, Lee J. Classification of speech and language profiles in 4-year-old children with cerebral palsy: A prospective preliminary study. Journal of Speech, Language, and Hearing Research. 2010;53:1496–1513. doi: 10.1044/1092-4388(2010/09-0176). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hustad KC, Miles LK. Alignment between augmentative and alternative communication needs and school-based speech-language services provided to young children with cerebral palsy. Early Childhood Services. 2010;4:129–140. [PMC free article] [PubMed] [Google Scholar]
- Jonsson A, Kristoffersson L, Ferm U, Thunberg G. The ComAlong communication boards: Parents’ use and experiences of aided language stimulation. Augmentative and Alternative Communication. 2011;27:103–116. doi: 10.3109/07434618.2011.580780. [DOI] [PubMed] [Google Scholar]
- Kangas KA, Lloyd LL. Early cognitive skills as prerequisites to augmentative and alternative communication use: What are we waiting for? Augmentative and Alternative Communication. 1988;4:211–221. doi: 10.1080/07434618812331274817. [DOI] [Google Scholar]
- Light J, Drager K. Early intervention for young children with autism, cerebral palsy, Down syndrome, and other disabilities. 2012 Retrieved from http://aackids.psu.edu.
- Light J, McNaughton D. Supporting the communication, language, and literacy development of children with complex communication needs: State of the science and future research priorities. Assistive Technology. 2012a;24:34–44. doi: 10.1080/10400435.2011.648717. [DOI] [PubMed] [Google Scholar]
- Light J, McNaughton D. The changing face of augmentative and alternative communication: Past, present, and future challenges. Augmentative and Alternative Communication. 2012b;28:197–204. doi: 10.3109/07434618.2012.737024. [DOI] [PubMed] [Google Scholar]
- Marshall J, Goldbart J. Communication is everything I think.” Parenting a child who needs augmentative and alternative communication (AAC) International Journal of Language & Communication Disorders. 2008;43:77–98. doi: 10.1080/13682820701267444. [DOI] [PubMed] [Google Scholar]
- McLellan A, Cipparone C, Giancola D, Armstrong D, Bartlett D. Medical and surgical procedures experienced by young children with cerebral palsy. Pediatric Physical Therapy. 2012;24:268–277. doi: 10.1097/PEP.0b013e31825be2f6. [DOI] [PubMed] [Google Scholar]
- Millar DC, Light JC, Schlosser RW. The impact of augmentative and alternative communication intervention on the speech production of individuals with developmental disabilities: A research review. Journal of Speech, Language, and Hearing Research. 2006;49:248–264. doi: 10.1044/1092-4388(2006/021). [DOI] [PubMed] [Google Scholar]
- Miller J, Chapman R. Systematic analysis of language transcripts. Madison, WI: University of Wisconsin; 1985. [Google Scholar]
- Norman G. Likert scales, levels of measurement and the “laws” of statistics. Advances in Health Sciences Education. 2010;15:625–632. doi: 10.1007/s10459-010-9222-y. [DOI] [PubMed] [Google Scholar]
- Palisano RJ, Begnoche DM, Chiarello LA, Bartlett DJ, McCoy SW, Chang HJ. Amount and focus of physical therapy and occupational therapy for young children with cerebral palsy. Physical & Occupational Therapy in Pediatrics. 2012;32:368–382. doi: 10.3109/01942638.2012.715620. [DOI] [PubMed] [Google Scholar]
- Palisano RJ, Hanna SE, Rosenbaum PL, Russell DJ, Walter SD, Wood EP, Galuppi BE. Validation of a model of gross motor function for children with cerebral palsy. Physical Therapy. 2000;80:974–985. [PubMed] [Google Scholar]
- Palisano RJ, Rosenbaum P, Walter S, Russell D, Wood E, Galuppi B. Development and reliability of a system to classify gross motor function in children with cerebral palsy. Developmental Medicine & Child Neurology. 1997;39:214–223. doi: 10.1111/j.1469-8749.1997.tb07414.x. [DOI] [PubMed] [Google Scholar]
- Pennington L. Cerebral palsy and communication. Paediatrics and Child Health. 2008;18:405–409. doi: 10.1016/j.paed.2008.05.013. [DOI] [Google Scholar]
- Pennington L, Noble E. Acceptability and usefulness of the group interaction training program It Takes Two to Talk to parents of pre-school children with motor disorders. Child: Care, Health, and Development. 2010;36:285–296. doi: 10.1111/J.1365-2214.2009.01054.x. [DOI] [PubMed] [Google Scholar]
- QSR International. NVivo qualitative data analysis (Version 10) [Computer Software] 2012 [Google Scholar]
- Rice ML, Smolik F, Perpich D, Thompson T, Rytting N, Blossom M. Mean length of utterance levels in 6-month intervals for children 3 to 9 years with and without language impairments. Journal of Speech, Language, and Hearing Research. 2010;53:333. doi: 10.1044/1092-4388(2009/08-0183). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roche L, Sigafoos J, Lancioni GE, O’Reilly MF, Green VA, Sutherland D, Edrisinha CD. Tangible symbols as an AAC option for individuals with developmental disabilities: A systematic review of intervention studies. Augmentative and Alternative Communication. 2014;30:28–39. doi: 10.3109/07434618.2013.878958. [DOI] [PubMed] [Google Scholar]
- Romski MA, Sevcik RA. Language comprehension: Considerations for augmentative and alternative communication. Augmentative and Alternative Communication. 1993;9:281–285. doi: 10.1080/07434619312331276701. [DOI] [Google Scholar]
- Romski MA, Sevcik RA. Breaking the speech barrier. Baltimore, MD: Brookes; 1996. [Google Scholar]
- Romski MA, Sevcik RA. Augmented input: Enhancing communication development. In: Light JC, Beukelman DR, Reichle J, editors. Communicative competence for individuals who use AAC: From research to effective practice. Baltimore, MD: Paul H. Brookes; 2003. [Google Scholar]
- Romski MA, Sevcik RA. Augmentative communication and early intervention: Myths and realities. Infants & Young Children. 2005;18:174–185. [Google Scholar]
- Romski MA, Sevcik RA, Adamson LB, Cheslock M, Smith A, Barker RM, Bakeman R. Randomized comparison of augmented and nonaugmented language interventions for toddlers with developmental delays and their parents. Journal of Speech, Language, and Hearing Research. 2010;53:350–364. doi: 10.1044/1092-4388(2009/08-0156). [DOI] [PubMed] [Google Scholar]
- Romski MA, Sevcik RA, Adamson LB, Smith A, Cheslock M, Bakeman R. Parent perceptions of the language development of toddlers with developmental delays before and after participation in parent-coached language interventions. American Journal of Speech-Language Pathology. 2011;20:111–118. doi: 10.1044/1058-0360(2011/09-0087). [DOI] [PubMed] [Google Scholar]
- Schlosser RW, Wendt O. Effects of augmentative and alternative communication intervention on speech production in children with autism: A systematic review. American Journal of Speech-Language Pathology. 2008;17:212–230. doi: 10.1044/1058-0360(2008/021). doi:1058-0360/08/1703-0212. [DOI] [PubMed] [Google Scholar]
- Sevcik RA. Comprehension: An overlooked component in augmented language development. Disability & Rehabilitation. 2006;28:159–167. doi: 10.1080/09638280500077804. [DOI] [PubMed] [Google Scholar]
- Sigurdardottir S, Vik T. Speech, expressive language, and verbal cognition of preschool children with cerebral palsy in Iceland: Speech, language, and cognition in CP. Developmental Medicine & Child Neurology. 2011;53:74–80. doi: 10.1111/j.1469-8749.2010.03790.x. [DOI] [PubMed] [Google Scholar]
- Smith A, Romski MA, Sevcik RA, Adamson LB, Bakeman R. Parent stress and its relation to parent perceptions of communication following parent-coached language intervention. Journal of Early Intervention. 2011;33:135–150. doi: 10.1177/1053815111405526. [DOI] [Google Scholar]
- Vygotsky L. Mind in society. Cambridge, Massachusetts: Harvard University Press; 1978. [Google Scholar]
- Yoder PJ, Warren SF. Effects of prelinguistic milieu teaching and parent responsivity education on dyads involving children with intellectual disabilities. Journal of Speech, Language, and Hearing Research. 2002;45:1158–1174. doi: 10.1044/1092-4388(2002/094). [DOI] [PubMed] [Google Scholar]
- Zimmerman IL, Steiner VG, Pond RE. Preschool Language Scale. 4. San Antonio, TX: The Psychological Corporation; 2002. [Google Scholar]


