Abstract
Background
The literature describing the health services individuals receive prior to and following self-directed violence is limited.
Objectives
This study examines services received for the six months preceding admission to an urban county medical center emergency department for self-directed violence. We predicted that individuals with at least one prior act of self-directed violence in the past six months would have received more services than those for whom the index admission was their only recent act.
Method
Participants were recruited from emergency department admissions during shifts selected to maximize representativeness. Participants (n=202) were interviewed using the Suicide Attempt Self-Injury Interview, Suicide Attempt Self-Injury Count, Treatment History Interview, MINI, Brief Symptom Index, and SF-12.
Results
The majority of index acts of self-directed violence (79%) were suicide attempts. The participants were characterized by low socio-economic status, substantial symptomatology, low physical and mental health functioning, and multiple psychiatric diagnoses. In the preceding six months, 34% were admitted to a hospital and 56% received crisis services (including 44% in the ED). While three quarters (76%) had seen an outpatient medical provider and most (70%) received psychotropic medications, less than half of the sample received psychiatric services (40%) or outpatient psychosocial treatment (48%). As predicted, utilization for most types of usual care was higher for those engaging in self-directed violence in the six months preceding the index admission.
Conclusions
Individuals admitted to this emergency department for self-directed violence received inadequate outpatient psychosocial and psychiatric services despite severe illness and disability.
Keywords: suicide attempt, self-directed violence, emergency, health services, quality of care
Suicide remains a staggering public health burden in the US. In 2010, over 38,000 deaths by suicide occurred – one suicide every 14 minutes and more than two suicides for every homicide1. Self-directed violence (SDV), as defined by the Centers for Disease Control and Prevention2 and utilized by the Departments of Defense and Veterans Affairs3,4, incorporates suicide attempts and non-suicidal self-directed violence as well as death by suicide. In 2012, 483,596 people were treated in emergency departments (EDs) for SDV (primarily suicide attempts); 68.8% of whom were hospitalized due to SDV5. In 2000, the cost of SDV was $33 billion, including $1 billion for medical treatment and $32 billion in lost productivity6. While suicide prevention efforts have focused on youth and older adults, the most recent CDC mortality data from 1999-2010 in the US show a 28% increase in suicide rates among middle-aged adults7.
For all these reasons, reducing death by suicide and SDV more generally is a health care priority.8,9 Yet very little is known about the type and quantity of usual care suicidal individuals receive – particularly those admitted to the Emergency Department (ED). Admission to the ED is a strong predictor of future suicide death10,11 and suicidal individuals represented 1.7% of all ED admissions in a recent survey12. From 1993-2008, the average number of ED visits for SDV more than doubled and the rate per 1,000 people almost doubled for males, females, whites, and blacks13. Individuals admitted to the ED due to SDV have higher rates of return ED visits (232.7 visits per 100 person-years) than individuals presenting with asthma (117.6 visits) and other health concerns (83.0 visits)14 with a third admitted to the hospital, and a quarter transferred to another facility14. Thus, the ED is a critical entry point for suicidal individuals with the healthcare system, though little is known about the health services these individuals receive.
Most research has evaluated services received prior to suicide deaths. A review of 40 studies15 found 45% and 77% of individuals who died by suicide attended primary care in the month and year before their deaths. However, only 19% received inpatient or outpatient mental health services in the prior month, 32% in the prior year, and 53% lifetime15. Little research has examined services leading to or following ED admission for self-directed violence (SDV)16. ED directors surveyed in California found their main concern for their suicidal patients was the lack of available community services12. Only one study in Finland evaluated the quality of care for SDV and found inadequate depression pharmacotherapy, psychotherapy, and ECT17 and inadequate alcohol treatment18 in the month prior and following an ED admission. Studies of individuals with multiple compared to single episodes of SDV find multiple episodes are associated with more use of services including inpatient psychiatric admission, inpatient length-of-stay, outpatient psychiatric services, outpatient psychotherapy, and psychiatric medications19–22.
Thus, health services studies of usual care for suicidal individuals admitted to the ED have been limited in both detail and scope and present a complex picture. The present study was designed as a detailed, descriptive examination of multiple types of usual medical, psychosocial, and pharmacotherapy services received in the six months prior to an ED admission for SDV. Based on previous research, we predicted that individuals reporting SDV in the six months preceding the ED admission would have received more inpatient, crisis, and outpatient health services than those for whom the index ED admission was the only six-month episode of SDV.
Methods
Participants
Participants were consecutively recruited from all admissions to the medical/surgical and psychiatric emergency services of XXX (HMC) between 2003 and 2005 during assessment periods selected to maximize representativeness. HMC is the county-owned hospital serving XXX and XXX and is the medical center that receives patients from law enforcement and emergency dispatch as well as those without means to pay.
Study interviewers were extensively trained on all measures as well as on suicide risk management and the ethics of research with high-risk patients in the ED setting. Interviewers were scheduled for recruitment periods from 12:00am to 8:00am, 8:00am to 4:00pm, and 4:00pm to 12:00am. Recruitment periods were selected to equally represent times of day, days of the week, and months of the year, although, we replaced the overnight shift with a second 4:00pm to 12:00am shift, because almost all patients were intoxicated, sleeping, or unwilling to be interviewed overnight.
During each recruitment period, all injuries likely to be self-directed violence (e.g., motor vehicle accidents, falls, lacerations, overdoses) were reviewed with clinical staff to determine if it was possible they were self-inflicted. Medical/surgical patients with injuries that were possibly SDV and all patients in the psychiatric emergency department were considered for the study if they were between 18-60 years of age. Potential participants with any of the following criteria were excluded: (a) not from local county, (b) did not speak English sufficiently to consent or be interviewed, (c) symptoms of psychosis, dementia, confusion, or other cognitive impairment were too severe for informed consent or to be interviewed, (d) was an inmate or under arrest, (e) was too aggressive to be interviewed, or (f) determined clinically inappropriate by an ED clinician.
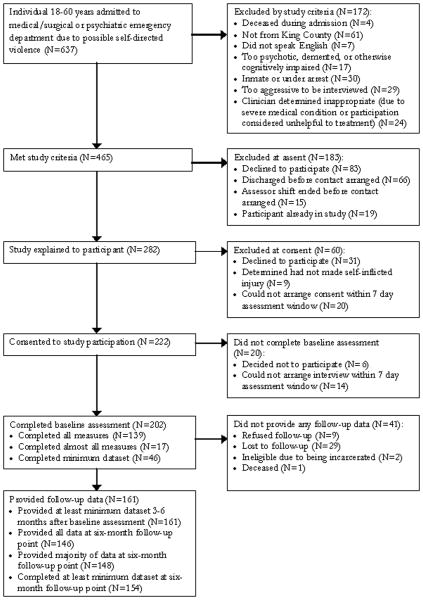
Following informed consent, a screening interview included the Suicide Attempt Self-Injury Interview (SASII)23 to standardize determination of SDV generally and whether the participant had intended to die. Of the 202 study participants, the index admission of 160 (79%) was for a suicide attempt; the remaining 42 (21%) was for non-suicidal SDV (See Figure 1 Flowchart of Study Recruitment and Completion).
Figure 1. Flowchart of Study Recruitment and Completion.
Measures
The SASII23 assesses a single act of SDV in detail, in this case the act resulting in ED admission. The SASII was used to determine whether the SDV was a suicide attempt or non-suicidal SDV. Excellent inter-rater reliability (ICCs .871–.978) and validity compared to medical records, therapist notes, and patient self-monitoring has been demonstrated for the SASII26. The Suicide Attempt and Self-Injury Count (SASI-Count24,25) is a short form of the SASII that efficiently assesses all SDV acts during a specified time period, in this case, the past six months and lifetime. The SASI-Count determines method, suicide intent, lethality, and medical treatment received for suicide attempts and non-suicidal SDV. The Mini International Neuropsychiatric Interview (MINI26–28) was used as a brief diagnostic measure because the context of the ED precluded the use of a full diagnostic measure like the SCID-P. The MINI has excellent inter-rater reliability26,27 but only moderate concordance with the SCID-P27 and CIDI28. The MINI assesses current mood episodes, current anxiety and eating disorders, current psychotic disorder (MINI does not differentiate between psychotic diagnoses), current psychoactive substance use disorders (past 12 months), and lifetime antisocial personality disorder. The presence or absence of lifetime borderline personality disorder was determined via the Structured Clinical Interview for DSM-IV, Axis II (SCID-II29–31). Overall adjustment and symptomatology was measured by the Brief Symptom Inventory (BSI32–34). The Short-Form Health Survey (SF-1235–37) assessed functional status.
The Treatment History Interview (THI38) describes (1) the participant's involvement with professional psychotherapy, comprehensive treatment programs, substance abuse programs, case management, self-help groups, and other non-professional forms of treatment; (2) involvement with inpatient units, crisis services, and outpatient psychiatric and medical treatment, and (3) medications prescribed, dates of use, and estimates of compliance.
Analyses of previous THI data have demonstrated its validity38. Participant self-report of psychiatric admissions and days were compared with medical records, revealing 90% agreement between participant report and hospital records for number of admissions per participant and 80% agreement for number of days per participant. In a clinical trial of Dialectical Behavior Therapy, all reports of individual psychotherapy were verified by calling psychotherapists for interviews. There were no false positives. Comparison between therapists' records of therapy hours and self-reported therapy hours yielded no significant difference. To maximize validity in the study described here, releases of information were obtained for all self-reported health services and these medical records sought. Available records were used to clarify and supplement unclear or missing participant responses.
Procedure
Participants were interviewed during the hospital admission – either in the ED or on a medical, surgical, or psychiatric unit. Interviews were divided into sessions if participants were distressed or fatigued, to assure treatment was provided without delay, and for transfers to other units. If discharged prior to completion of the interview, participants were interviewed up to one week following discharge. Assessments were prioritized so critical measures of suicidal behavior and health services occurred first with diagnostic and self-report measures last in case the full interview could not be completed. Participants were compensated $25 for the interview, which took a median of 1 hour (IQR=1-2). The University of Washington Risk Assessment Protocol (UWRAP) was utilized to manage risk during the assessments. This protocol has been recommended by NIMH39 and has been used successfully in over 20 years of research by the PI and others40,41. All measures were checked by lead research staff for accuracy, reliability of ratings, and consistency within and between measures. All procedures were reviewed and approved by the XXX Institutional Review Board.
Statistical Analysis
To describe health services use, descriptive statistics were tabulated for the type and quantity of medical, crisis, outpatient, and pharmacotherapy services and compared by six-month SDV status (single versus multiple SDV episodes). Logistic, negative binomial, or linear regression models were used, for binary, count, or continuous outcomes, respectively. For several count outcomes, a two-part hurdle model was used due to large presence of zeroes42. Some logistic regression models had very small cell sizes, leading to a problem known as partial separation in logistic regression43 in which odds ratios and 95% CI become extreme and biased. Accordingly, we utilized a Bayesian approach to logistic regression in which a prior distribution is placed on the coefficients, restricting them from going to extreme values44. R software (version 3.0.045) was used for all analyses, and the bayesglm function in the arm package46 was used for the Bayesian analyses.
Results
Table 1 provides the demographic and clinical description of the full sample categorized by six-month SDV status. Participants were in mid-adulthood, roughly equal in gender, predominantly Caucasian, largely single, and evenly divided between those with a high school education or less and those with at least some college education. Most were unemployed and low-income, and a quarter were homeless. Compared to a representative sample of patients (SDV and non-SDV) in the XX psychiatric emergency service (PES)47, this sample was almost exactly the same for gender, age, ethnicity and homelessness. However, compared to [City] census data the study sample has a lower percentage of African-Americans (7.9%), and mixed race (5.1%) and a higher percentage Asian and Pacific Islander (14.2%).48 Median household income in [City] is $63,470, whereas 75% of the study sample reported incomes below $20,000. City homelessness is 1.4% compared to the 25% in this sample.49 Those who refused assent (n=83) were slightly yet significantly younger (M=32.3 years, SD=10.0) than those who assented (M=36.2 years, SD=10.9; n=282, t(362)=2.91, p=.004). Those who refused did not differ in gender, the presence of suicidal ideation, positive blood alcohol or urine toxicology screen, or being restrained during their admission.
Table 1. Demographic and Clinical Characteristics.
| Full Sample | Single SDV episode | Multiple SDV episodes | Odds Ratioa (95% CI) | |
|---|---|---|---|---|
|
| ||||
| N (% of Total) | 202 (100.0) | 109 (54.0) | 93 (46.0) | |
|
| ||||
| % Male | 105 (52.0) | 56 (51.4) | 49 (52.7) | 1.05 (0.61-1.82) |
|
| ||||
| Age | ||||
| Mean (Standard Deviation) | 36.4 (10.6) | 38.2 (10.4) | 34.4 (10.4) | 0.97 (0.94-0.99)1 |
|
| ||||
| Racial Ethnicity | ||||
| %Caucasian | 143 (70.8) | 78 (71.6) | 65 (69.9) | Ref |
| %African-American | 21 (10.4) | 11 (10.1) | 10 (10.8) | 1.08 (0.45-2.63) |
| %Asian | 4 (2.0) | 0 (0.0) | 4 (4.3) | 12.93 (0.67-248.11) |
| %Native American | 5 (2.5) | 4 (3.7) | 1 (1.1) | 0.39 (0.06-2.43) |
| %Latino/a | 5 (2.5) | 3 (2.8) | 2 (2.2) | 0.83 (0.16-4.23) |
| %Other (primarily multiracial) | 24 (11.9) | 13 (11.9) | 11 (11.8) | 1.01 (0.44-2.35) |
|
| ||||
| Marital Status | ||||
| % Single, never married | 104 (51.7) | 46 (42.6) | 58 (62.4) | Ref |
| % Widowed | 5 (2.5) | 3 (2.8) | 2 (2.2) | 0.61 (0.12-3.11) |
| % Separated | 20 (10.0) | 13 (12.0) | 7 (7.5) | 0.46 (0.18-1.20) |
| % Divorced | 41 (20.4) | 22 (20.4) | 19 (20.4) | 0.71 (0.35-1.45) |
| % Married | 31 (15.4) | 24 (22.2) | 7 (7.5) | 0.25 (0.10-0.62) |
|
| ||||
| Educational level | ||||
| % Some high school/GED not completed | 28 (14.3) | 16 (15.1) | 12 (13.3) | Ref |
| % High school diploma or GED | 61 (31.1) | 26 (24.5) | 35 (38.9) | 1.77 (0.75-4.15) |
| % Some college or business/technical training | 79 (40.3) | 45 (42.5) | 34 (37.8) | 1.00 (0.44-2.28) |
| % College graduate and beyond | 28 (14.3) | 19 (17.9) | 9 (10.0) | 0.64 (0.37-1.79) |
|
| ||||
| Income in past year | ||||
| % Making less than $10,000 | 80 (58.4) | 40 (51.3) | 40 (67.8) | Ref |
| % Making $10,000 - $24,999 | 30 (21.9) | 22 (28.2) | 8 (13.6) | 0.39 (0.16-0.94) |
| % Making $25,000 - $49,999 | 18 (13.1) | 9 (11.5) | 9 (15.3) | 1.02 (0.38-2.73) |
| % Making $50,000 and higher | 9 (4.5) | 7 (9.0) | 2 (2.2) | 0.35 (0.08-1.48) |
|
| ||||
| % Homeless | 50 (24.8) | 20 (18.3) | 30 (32.3) | 2.07 (1.09-3.93) |
|
| ||||
| Lifetime suicide attempts | ||||
| Median (IQR2) | 2 (0-7) | 1 (0-3) | 6 (3-16) | 3.42 (2.30-5.10)3 |
|
| ||||
| Lifetime non-suicidal SDV | ||||
| Any N (%) | 76 (46%) | 28 (30%) | 48 (66%) | |
| If any, Median (IQR) | 11 (3-68) | 4 (1-30) | 23 (7-117) | 1.66 (1.35-2.05)2 |
|
| ||||
| Psychiatric Conditions4 | N (%) | N (%) | N (%) | |
|
| ||||
| % Major depressive episode | 118 (80.8) | 67 (79.8) | 51 (82.3) | |
| % Dysthymia | 40 (27.6) | 18 (21.4) | 22 (36.1) | |
| % Manic episode | 14 (9.7) | 4 (4.8) | 10 (16.4) | |
| % Hypomanic episode | 2 (1.4) | 1 (1.2) | 1 (1.6) | |
| % Panic disorder | 28 (19.3) | 13 (15.5) | 15 (24.6) | |
| % Agoraphobia | 61 (42.4) | 32 (38.1) | 29 (48.3) | |
| % Social phobia | 36 (25.0) | 18 (21.4) | 18 (30.0) | |
| % OCD | 31 (21.5) | 15 (17.9) | 16 (26.7) | |
| % PTSD | 38 (26.8) | 21 (25.0) | 17 (29.3) | |
| % Alcohol dependence | 61 (40.4) | 36 (40.9) | 25 (39.7) | |
| % Alcohol abuse | 12 (7.9) | 7 (8.0) | 5 (7.9) | |
| % Substance dependence | 48 (31.6) | 23 (25.8) | 25 (39.7) | |
| % Substance abuse | 11 (7.2) | 9 (10.1) | 2 (3.2) | |
| % Psychotic symptoms | 43 (30.1) | 18 (21.4) | 25 (42.4) | |
| % Anorexia nervosa | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| % Bulimia nervosa | 8 (5.6) | 3 (3.6) | 5 (8.3) | |
| % Generalized anxiety | 57 (39.6) | 35 (41.7) | 22 (36.7) | |
| % Any Affective Episode5 | 130 (90.9) | 74 (89.2) | 56 (93.3) | 1.61 (0.51-5.11) |
| % Any Anxiety Disorder6 | 114 (80.3) | 64 (76.2) | 50 (86.2) | 1.88 (0.79-4.47) |
| % Substance Use Disorder7 | 92 (60.9) | 52 (59.1) | 40 (63.5) | 0.84 (0.43-1.61) |
| % Anti-social personality | 34 (23.8) | 16 (19.0) | 18 (30.5) | 1.81 (0.85-3.88) |
| % Borderline personality | 41 (29.3) | 20 (24.7) | 21 (35.6) | 1.65 (0.80-3.39) |
|
| ||||
| Symptom Scales8 | Mean (SD) | Mean (SD) | Mean (SD) | |
|
| ||||
| Brief Symptom Inventory | ||||
| Global Severity Index | 2.12 (.69) | 1.94 (.71) | 2.34 (.60) | 2.48 (1.47-4.20) |
|
| ||||
| SF-129 | ||||
| Physical Component Score | 48.61 (11.55) | 48.36 (11.25) | 48.93 (12.01) | 1.00 (0.98-1.03) |
| Mental Component Score | 27.45 (10.72) | 28.75 (11.98) | 25.77 (8.63) | 0.97 (0.94-1.01) |
Bayesian logistic regression of predictors on the outcome of single vs. multiple SII episodes
Boldface type indicates statistically significant result
Interquartile Range
Outliers included in the analysis presented. Results excluding outliers comparable.
Diagnoses and conditions are current (past month) except substance abuse which his past 12 months and personality disorders which are lifetime; N=146 for diagnostic data as 56 participants did not complete the entire interview due to lack of time, fatigue, or because they were a poor historian. Representativeness analysis did not show differences in demographic or SII data between those with and without diagnostic data
Any affective episode included major depression, bipolar disorder, and dysthymia
Any anxiety disorders included panic, agoraphobia without panic, social phobia, obsessive-compulsive disorder, and post-traumatic stress disorder.
Substance use disorder included any type of substance including alcohol and abuse as well as dependence
N=146 for symptom scales data as 56 participants did not complete the entire interview because of lack of time or fatigue.
Lower scores are more severe on the SF-12
As seen in Table 1, participants with multiple SDV episodes were generally comparable to those with a single SDV in the previous six months, but were younger and more likely to be single and homeless. The sample as a whole had a median of two previous suicide attempts (lifetime), but among those with multiple SDV episodes, there was a median of six previous lifetime suicide attempts. Non-suicidal SDV differed between groups with a median of zero in the full sample and one among those with multiple SDV episodes.
Also shown in Table 1, the sample screened positive for multiple psychiatric diagnoses with over 90% reporting an affective episode and over 80% reporting at least one current anxiety disorder. Over 40% met criteria for a substance use disorder and 30% reported psychotic symptoms. Almost a quarter met criteria on the MINI for antisocial personality disorder and 29% met criteria for borderline personality disorder on the SCID-II. Global severity index (GSI) scores on the BSI questionnaire indicated substantial symptomatology. Both physical and mental health functioning scores on the SF-12 were not only well below their age norms, but also below a sample of those with clinical depression35,36. However, only the GSI measure of symptomatology was associated with SDV subgroups – with greater psychiatric symptomatology in those with multiple SDV in the past six months.
Table 2 illustrates the range of inpatient and crisis services received for behavioral health reasons in the six months preceding index ED admission. A third (34%) had at least one medical, psychiatric, or substance abuse inpatient admission, with a quarter admitted to an inpatient psychiatric unit—largely voluntarily. Fifty-six percent had received a crisis service: almost half in an ED for behavioral health reasons, and over a quarter from paramedics. As expected, those with multiple SDV episodes used significantly more inpatient and crisis services.
Table 2. Inpatient and Crisis Services Received in the Six Months Prior to ED Admission.
| Full Sample | Single SII episode | Multiple SII episodes | Odds Ratio (95% CI) | ||||
|---|---|---|---|---|---|---|---|
| Any N (%) | If any, Median (IQR1) | Any N (%) | If any, Median (IQR) | Any N (%) | If any, Median (IQR) | ||
| 1982 (100.0) | 107 (54.0) | 91 (46.0) | |||||
| Inpatient Treatment | |||||||
| Medical/surgical inpatient admission | 10 (5%) | 1 (1-1) | 2 (2%) | 1 (1-1) | 8 (9%) | 1 (1-2) | 1.07 (1.01-1.14)a |
| Psychiatric inpatient | 52 (26%) | 1 (1-2) | 10 (9%) | 1 (1-2) | 42 (46%) | 1 (1-2) | 6.15 (3.24-11.67)b |
| Voluntary admission | 48 (24%) | 1 (1-2) | 10 (9%) | 1 (1-1) | 38 (41%) | 1 (1-2) | |
| Involuntary admission | 16 (8%) | 1 (1-1) | 3 (3%) | 1 (1-1) | 13 (14%) | 1 (1-1) | |
| Residential chemical dependency treatment | 18 (9%) | 1 (1-1) | 8 (8%) | 1 (1-1) | 10 (11%) | 1 (1-2) | 1.03 (0.96-1.12)a |
| Crisis Services | |||||||
| Emergency Department | 88 (44%) | 1 (1-3) | 22 (21%) | 1 (1-2) | 66 (73%) | 2 (1-3) | 4.22(2.67-6.65)b |
| Paramedics responded | 55 (28%) | 1 (1-3) | 13 (12%) | 1 (1-3) | 42 (46%) | 1 (1-3) | 1.40 (1.25-1.58)a |
| Police made wellness check | 15 (8%) | 1 (1-2) | 4 (4%) | 2 (1-2) | 11 (12%) | 1 (1-2) | 1.09 (1.01-1.17)a |
| Evaluated for involuntary admission | 22 (11%) | 1 (1-2) | 4 (4%) | 2 (1-2) | 18 (20%) | 2 (1-2) | 1.17 (1.08-1.28)a |
| Detox | 21 (11%) | 1 (1-1) | 6 (5.6%) | 1 (1-2) | 15 (17%) | 1 (1-1) | 1.14 (1.04-1.24)a |
| Contacted a Crisis Line | 31 (16%) | 2 (1-6) | 10 (9%) | 2 (2-5) | 21 (23%) | 1 (1-7) | 1.14 (1.04-1.26)a |
Bayesian logistic regression of whether low base rate service occurred or not predicted by single vs. multiple SII episodes
Negative binomial regression of rate of service utilization predicted by single vs. multiple SII episodes
Interquartile Range
Three participants did not complete the interview due to discharge or other interference and one participant refused this part of the interview
Table 3 presents medical and pharmacotherapy visits. Less than half the participants (41%) received at least one outpatient visit with a medical or psychiatric professional for behavioral health reasons, i.e., for suicidality, psychiatric symptoms, substance abuse, or psychiatric medications. This did not differ between groups. Over two-thirds of the sample were prescribed, and took, a psychotropic medication with those with a single SDV episode less likely to take any medication than those with multiple SDV episodes (60% vs. 80%). Moreover, there were significantly more medications taken by individuals with multiple SDV episodes (Mdn = 3) vs. those with a single SDV episode (Mdn = 2).
Table 3. Medical Visits and Pharmacotherapy Received in the Six Months Prior to ED Admission.
| Full Sample | Single SII episode | Multiple SII episodes | Odds Ratio (95% CI) | ||||
|---|---|---|---|---|---|---|---|
| Any N (%) | If any, Median (IQR1) | Any N (%) | If any, Median (IQR) | Any N (%) | If any, Median (IQR) | ||
| 1982 (100.0) | 107 (54.0) | 91 (46.0) | |||||
| Pharmacotherapy Services3 | |||||||
| Had behavioral health related medical visit | 80 (41.2%) | 3 (1.3-6) | 42 (40%) | 4 (1.8-6) | 38 (42.7%) | 2 (1-5) | 1.05 (0.60 -1.83)b |
| N (% of Total) | 155 (100.0)4 | 84 (54.0) | 71 (46.0) | ||||
| Received psychotropic medication | 107 (69.5%) | 2 (1-4) | 51 (60.7%) | 2 (1-3) | 56 (80%) | 3 (2-4) | 1.63 (1.20-2.22)b |
| Prescribed psychotropic medication and never filled prescription | 25 (16.2%) | 1 (1-2) | 10 (11.9%) | 1 (1-2.8) | 15 (21.4%) | 1 (1-2) | 1.10 (0.98-1.23)a |
| Received non-psychotropic medication | 84 (54.2%) | 2 (1-2) | 43 (51.2%) | 2 (1-2) | 41 (57.7%) | 2 (1-2) | 1.06 (0.68-1.64)b |
| Took complimentary/ alternative medication | 17 (11%) | 0 (0-0) | 10 (12%) | 0 (0-0) | 7 (10%) | 0 (0-0) | 0.98 (0.89-1.08)a |
Bayesian logistic regression of whether low base rate service occurred or not predicted by single vs. multiple SII episodes
Negative binomial regression of rate of service utilization predicted by single vs. multiple SII episodes
Interquartile Range
Three participants did not complete the interview due to discharge or other interference and one participant refused this part of the interview
Note that 2 participants did not know which services they had and 6 did not complete this section of the interview.
Note that 39 participants did not complete this section of the interview
Table 4 shows the frequency and types of outpatient psychosocial services received by participants in the previous six months. Less than half had received outpatient psychosocial services, with large variation in the number of sessions received. Modal services received were individual therapy and case management. Few (10%) reported formal substance abuse treatment and slightly less than a quarter reported attending twelve-step meetings (although 40% met substance abuse or dependence in past 12 months). Average satisfaction with psychosocial services was almost 4 on a 5-point scale. As expected, the participants with multiple SDV episodes were twice as likely to have received outpatient psychosocial services than those for whom the ED admission was the single SDV episode. However, among those who received these services, there was not a significant difference in the amount of services received and the only treatment modality that differed was that case management was received by more of the multiple SDV participants.
Table 4. Psychosocial Outpatient Interventions Received in the Six Months Prior to Emergency Department Admission.
| Full Sample | Single SII episode | Multiple SII episodes | OR (95% CI) / RR (95% CI) | |
|---|---|---|---|---|
|
| ||||
| N (% of Total) | 174 (100.0) | 99 (56.9) | 75 (43.1) | |
|
| ||||
| Outpatient psychosocial visits | Zero: 2.38 (1.28- 4.43)c Count: 0.97 (0.88-1.06) | |||
| % None | 90 (51.7) | 61 (61.6) | 29 (38.7) | |
| % 1-5 visits | 12 (6.9) | 3 (3.0) | 9 (12.0) | |
| % 6-11 visits | 6 (3.4) | 5 (5.1) | 1 (1.3) | |
| % 12 or more visits | 66 (37.9) | 30 (30.3) | 36 (48.0) | |
|
| ||||
| Persons receiving at least one visit of following services1 N (%) | ||||
|
| ||||
| Individual therapy | 61 (30.0) | 29 (26.6) | 32 (34.4) | 1.08 (0.95-1.23)a |
|
| ||||
| Group therapy | 19 (9.4) | 6 (5.5) | 13 (14.0) | 1.09 (1-1.18)a |
|
| ||||
| Case management | 50 (24.8) | 16 (14.7) | 34 (36.6) | 1.24 (1.11-1.40)a |
|
| ||||
| Substance abuse treatment program | 20 (9.9) | 9 (8.3) | 11 (11.8) | 1.04 (0.95-1.13)a |
|
| ||||
| Twelve-step program | 36 (22.8) | 16 (18.2) | 20 (28.6) | 1.11 (0.97-1.26)a |
|
| ||||
| Satisfaction with provider | Mean (SD) | Mean (SD) | Mean (SD) | |
| (0=not at all to 5=very helpful) | 3.95 (1.26) | 4.03 (1.27) | 3.88 (1.27) | 0.85 (0.60-1.21)a |
Bayesian logistic regression of whether low base rate service occurred or not predicted by single vs. multiple SII episodes
Hurdle model with negative binomial regression of rate of service utilization predicted by single vs. multiple SII episodes
Services received by less than 5% of the participants are excluded. These included couple or family counseling, spiritual counseling, free standing skills training class, vocational training, and intake assessment alone.
Discussion
This examination of usual care medical, psychosocial, and pharmacotherapy services received in the six months prior to an ED admission for SDV paints a sobering picture of the physical and mental health of patients and the services they receive. The participants in this sample were quite ill, with substantial symptomatology, poor physical and mental health, and multiple diagnoses. Despite this, the majority never received outpatient psychosocial or psychiatric services in the six months prior to the index ED admission for SDV. Despite diagnoses of affective disorder in 90% and anxiety disorder in 80%, a third had not received any psychotropic medication and none had received ECT or rTMS. While two thirds were taking psychotropic medication, in the previous six months less than half reported a visit with a psychiatric or medical provider in which any behavioral health concern was addressed. Thus, as seen in Suominen's quality of care studies17,18, these patients were under-treated.
Consistent with previous studies, approximately a quarter had been admitted to a psychiatric unit in the previous six months – slightly more than the 20% found by Runeson & Wasserman16 in Sweden, the only other study examining a six-month window. Almost half (48%) received at least one outpatient psychosocial service and 41% at least one behavioral health medical visit in the previous six months, also similar to the 43% found by Runeson & Wasserman. Three quarters (76%) had seen a physician, nurse, or other outpatient medical provider in the previous six months, twice the rate reported by Runeson & Wasserman16.
We hypothesized that the quantity of health services would be higher for those who had harmed themselves multiple times because this may have led them to seek services or be recommended for them (although not all SDV episodes were treated)19–22. Higher utilization among participants with multiple SDV episodes was seen for almost every crisis service including inpatient and ED admissions, as well as whether they received outpatient psychosocial treatment or were taking psychotropic medications. However, multiple SDV episodes were not associated with amount of psychosocial treatment nor rates of medical or psychiatric visits, individual therapy, group therapy, or any type of substance abuse treatment. However, multiple episodes were associated with higher use of case management services. This may reflect a bias in publicly funded services in XX state toward psychotropic medications and case management over other forms of treatment.
While almost two-thirds of the sample had an alcohol or substance abuse or dependence diagnosis on the MINI, very few had received appropriate services. Ten percent had been to a residential drug or alcohol program and 10% to outpatient substance abuse treatment – comparable with the 11% who went to a detoxification center, which is a very short-term crisis response to substance dependence. Only one in seven participants received any of these three types of substance abuse treatment, and less than a quarter had attended a twelve-step meeting during the previous six months. Thus, substance abuse was drastically under-treated in this sample as was found in the previous study by Suominen18.
These results have several clinical implications. Few SDV patients are receiving outpatient behavioral health treatment, particularly psychotherapy, which has the strongest empirical support in preventing future suicide attempts.50–55 Conversely, pharmacotherapy and case management, which have little empirical support in preventing suicidal behavior54,55, were much more common. These results emphasize the need for medical/surgical services to screen for SDV and suicidal ideation and make clear discharge referrals for appropriate behavioral health care. While access to care is often limited12, a clear referral for a type of service (e.g., psychotherapy), increases the chances it will be followed by the patient, family, or primary care clinician.
This study also highlights the lack of substance abuse treatment for those with addictions. It is also imperative that suicidal individuals with substance abuse and dependence have access to treatment – both substance abuse and mental health services.56,57 Substance abuse treatment providers are often not credentialed to address suicidal behavior and therefore refer patients to the ED. Since addiction is such a critical risk factor for suicide, integration of mental health resources for suicide risk, management, and treatment into outpatient services rather than relying on the ED is critical.57
There were important limitations to this study. First, this study was conducted at one publicly funded medical center in an urban XXX community, which will not be representative of all suicidal ED patients – especially in XXX county where the median income is $70,000, high school and college graduation rates are 92% and 46% respectively, and only 11% of the population is below the poverty line. In this sample, 85% graduated high school but only 14% graduated college and over half were under the poverty line of $10,000/year. Thus, this sample represents a very low-income subgroup. It is unclear whether they were always in this situation or whether their illness(es) led to social drift to poverty and disadvantage.
Second, not all participants approached by the study participated or completed the entire interview as shown in Figure 1. However, all admissions in the assessment windows chosen to maximize representativeness were tracked for recruitment. Third, information was provided retrospectively by participant report. Services and especially diagnostic information may have been missed or reported inaccurately. Standardized measures with demonstrated validity, well-trained interviewers, and clarification with medical records (when available) were used to mitigate this limitation. Finally, the lack of previous research on health service utilization among suicidal individuals limited hypotheses to guide study predictions, which therefore were made by univariate relationships with outcomes. Thus, these results should be considered exploratory to determine factors that might be considered in the design of future studies.
In conclusion, more than half of patients who were admitted to the ED of a large county medical center due to SDV had not received outpatient psychosocial or psychiatric services in the previous six months and almost a third had not received psychotropic medications despite severe symptoms and impaired functioning. While our hypothesis that multiple episodes of self-directed violence would predict more utilization was largely supported, a number of key services were no more likely or frequent. This is one of the only studies of usual care services for suicidal individuals admitted to the ED and helps to illuminate areas that need to be improved to prevent suicide. Further research is clearly needed to determine the generalizability of these findings to other subgroups of suicidal individuals.
Acknowledgments
Funding for this project was provided by the National Institute of Mental Health 1K01-MH1933-01A1.
Contributor Information
Amanda H. Kerbrat, Email: ahm2@uw.edu, Department of Psychiatry & Behavioral Sciences, Harborview Medical Center, Box 359911, 325 9th Ave, Seattle, WA 98104, 206-744-1716 (office) 206-744-9939 (fax).
David C. Atkins, Email: datkins@uw.edu, Center for the Study of Health and Risk Behaviors, Department of Psychiatry and Behavioral Sciences, University of Washington, 1100 NE 45th Street, Suite 300, Seattle, WA 98105, 206-616-3879 (office) 206-744-3231 (fax).
Peter Roy-Byrne, Email: roybyrne@uw.edu, Department of Psychiatry & Behavioral Sciences, Harborview Medical Center, Box 359911, 325 9th Ave, Seattle, WA 98104, 206-897-4201 (office) 206-744-3231 (fax).
Wayne J. Katon, Email: wkaton@uw.edu, Department of Psychiatry & Behavioral Sciences, University of Washington, Box 356560, Seattle, WA 98195, 206-543-7177 (office) 206-221-5414 (fax).
References
- 1.McIntosh J, Drapeau C. U S A Suicide 2010 Official Final Data [Internet] Washington DC: American Association of Suicidology; 2012. [cited 2014 Jan 8]. Available from: http://www.suicidology.org/c/document_library/get_file?folderId=262&name=DLFE-635.pdf. [Google Scholar]
- 2.Crosby A, Ortega L, Melanson C. Self-directed Violence Surveillance: Uniform Definitions and Recommended Data Elements, Version 1.0 [Internet] Atlanta, GA: Centers for Disease Control and Prevention, National Center for Injury Prevention and Control; 2011. Available from: http://www.cdc.gov/violenceprevention/pdf/self-directed-violence-a.pdf. [Google Scholar]
- 3.Brenner LA, Breshears RE, Betthauser LM, et al. Implementation of a Suicide Nomenclature within Two VA Healthcare Settings. J Clin Psychol Med Settings. 2011;18(2):116–28. doi: 10.1007/s10880-011-9240-9. [DOI] [PubMed] [Google Scholar]
- 4.Matarazzo BB, Clemans TA, Silverman MM, Brenner LA. The Self-Directed Violence Classification System and the Columbia Classification Algorithm for Suicide Assessment: A Crosswalk. Suicide Life Threat Behav. 2013;43(3):235–49. doi: 10.1111/j.1943-278x.2012.00131.x. [DOI] [PubMed] [Google Scholar]
- 5.Rockett IRH, Regier MD, Kapusta ND, et al. Leading causes of unintentional and intentional injury mortality: United States, 2000-2009. Am J Public Health. 2012;102(11):e84–92. doi: 10.2105/AJPH.2012.300960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Corso PS, Mercy JA, Simon TR, Finkelstein EA, Miller TR. Medical costs and productivity losses due to interpersonal and self-directed violence in the United States. Am J Prev Med. 2007;32(6):474–82. doi: 10.1016/j.amepre.2007.02.010. [DOI] [PubMed] [Google Scholar]
- 7.Centers for Disease Control and Prevention (CDC) Suicide among adults aged 35-64 years--United States, 1999-2010. MMWR Morb Mortal Wkly Rep. 2013;62(17):321–5. [PMC free article] [PubMed] [Google Scholar]
- 8.World Health Organization. Health21: the health for all policy framework for the WHO European Region. Copenhagen: World Health Organization, Regional Office for Europe; 1999. [Google Scholar]
- 9.U.S. Department of Health and Human Services (HHS) Office of the Surgeon General and National Action Alliance for Suicide Prevention. 2012 National Strategy for Suicide Prevention: Goals and Objectives for Action [Internet] 2012 Available from: http://www.surgeongeneral.gov/library/reports/national-strategy-suicide-prevention/ [PubMed]
- 10.Ryan J, Rushdy A, Perez-Avila CA, Allison R. Suicide rate following attendance at an accident and emergency department with deliberate self harm. J Accid Emerg Med. 1996;13(2):101–4. doi: 10.1136/emj.13.2.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cooper J, Kapur N, Webb R, et al. Suicide after deliberate self-harm: a 4-year cohort study. Am J Psychiatry. 2005;162(2):297–303. doi: 10.1176/appi.ajp.162.2.297. [DOI] [PubMed] [Google Scholar]
- 12.Baraff LJ, Janowicz N, Asarnow JR. Survey of California Emergency Departments About Practices for Management of Suicidal Patients and Resources Available for Their Care. Ann Emerg Med. 2006;48(4):452–458.e2. doi: 10.1016/j.annemergmed.2006.06.026. [DOI] [PubMed] [Google Scholar]
- 13.Ting SA, Sullivan AF, Boudreaux ED, Miller I, Camargo CA., Jr Trends in US emergency department visits for attempted suicide and self-inflicted injury, 1993-2008. Gen Hosp Psychiatry. 2012;34(5):557–65. doi: 10.1016/j.genhosppsych.2012.03.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Colman I, Dryden DM, Thompson AH, et al. Utilization of the emergency department after self-inflicted injury. Acad Emerg Med Off J Soc Acad Emerg Med. 2004;11(2):136–42. [PubMed] [Google Scholar]
- 15.Luoma JB, Martin CE, Pearson JL. Contact with mental health and primary care providers before suicide: a review of the evidence. Am J Psychiatry. 2002;159(6):909–16. doi: 10.1176/appi.ajp.159.6.909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Runeson B, Wasserman D. Management of suicide attempters: what are the routines and the costs? Acta Psychiatr Scand. 1994;90(3):222–8. doi: 10.1111/j.1600-0447.1994.tb01581.x. [DOI] [PubMed] [Google Scholar]
- 17.Suominen KH, Isometsä ET, Henriksson MM, Ostamo AI, Lönnqvist JK. Inadequate treatment for major depression both before and after attempted suicide. Am J Psychiatry. 1998;155(12):1778–80. doi: 10.1176/ajp.155.12.1778. [DOI] [PubMed] [Google Scholar]
- 18.Suominen KH, Isometsä ET, Henriksson MM, Ostamo AI, Lönnqvist JK. Treatment received by alcohol-dependent suicide attempters. Acta Psychiatr Scand. 1999;99(3):214–9. doi: 10.1111/j.1600-0447.1999.tb00978.x. [DOI] [PubMed] [Google Scholar]
- 19.Pérez E, Minoletti A, Blouin J, Blouin A. Repeated users of a psychiatric emergency service in a Canadian general hospital. Psychiatr Q. 1986;58(3):189–201. doi: 10.1007/BF01064733. [DOI] [PubMed] [Google Scholar]
- 20.Ellison JM, Blum NR, Barsky AJ. Frequent repeaters in a psychiatric emergency service. Hosp Community Psychiatry. 1989;40(9):958–60. doi: 10.1176/ps.40.9.958. [DOI] [PubMed] [Google Scholar]
- 21.Stocks R, Scott AI. What happens to patients who frequently harm themselves? A retrospective one-year outcome study. Br J Psychiatry J Ment Sci. 1991;158:375–8. doi: 10.1192/bjp.158.3.375. [DOI] [PubMed] [Google Scholar]
- 22.O'Sullivan M, Lawlor M, Corcoran P, Kelleher MJ. The cost of hospital care in the year before and after parasuicide. Crisis. 1999;20(4):178–83. doi: 10.1027//0227-5910.20.4.178. [DOI] [PubMed] [Google Scholar]
- 23.Linehan MM, Comtois KA, Brown MZ, Heard HL, Wagner A. Suicide Attempt Self-Injury Interview (SASII): development, reliability, and validity of a scale to assess suicide attempts and intentional self-injury. Psychol Assess. 2006;18(3):303–12. doi: 10.1037/1040-3590.18.3.303. [DOI] [PubMed] [Google Scholar]
- 24.Linehan M, Comtois KA. Suicide Attempt and Self-Injury Count (SASI-Count) (formerly Lifetime Parasuicide History) [Internet] 1996 Available from: http://depts.washington.edu/brtc/files/L-SASI%20Count.pdf.
- 25.Linehan MM, Comtois KA, Lungu A. Brief or In Depth Interview in Assessing Self-Injury: Balancing Assessment Effort and Results. Seattle, WA: 2011. [Google Scholar]
- 26.Sheehan DV, Lecrubier Y, Sheehan KH, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59(Suppl 20):22–33. quiz 34–57. [PubMed] [Google Scholar]
- 27.Sheehan D, Lecrubier Y, Harnett Sheehan K, et al. The validity of the Mini International Neuropsychiatric Interview (MINI) according to the SCID-P and its reliability. Eur Psychiatry. 1997;12(5):232–41. [Google Scholar]
- 28.Amorim P, Lecrubier Y, Weiller E, Hergueta T, Sheehan D. DSM-IH-R Psychotic Disorders: procedural validity of the Mini International Neuropsychiatric Interview (MINI). Concordance and causes for discordance with the CIDI. Eur Psychiatry. 1998;13(1):26–34. doi: 10.1016/S0924-9338(97)86748-X. [DOI] [PubMed] [Google Scholar]
- 29.First MB. User's guide for the structured clinical interview for DSM-IV axis II personality disorders: SCID-II. Washington, DC: American Psychiatric Press; 1997. [Google Scholar]
- 30.First MB, Spitzer RL, Gibbon M, Williams JBW. The Structured Clinical Interview for DSM-III-R Personality Disorders (SCID-II). Part I: Description. J Personal Disord. 1995;9(2):83–91. [Google Scholar]
- 31.First MB, Spitzer RL, Gibbon M, et al. The Structured Clinical Interview for DSM-III-R Personality Disorders (SCID-II). Part II: Multi-Site Test-Retest Reliability Study. J Personal Disord. 1995;9(2):92–104. [Google Scholar]
- 32.Derogatis L. The Brief Symptom Inventory: Administration, Scoring, and Procedures Manual. Fourth. Minneapolis, MN: National Computer Systems; 1993. [Google Scholar]
- 33.Prinz U, Nutzinger DO, Schulz H, Petermann F, Braukhaus C, Andreas S. Comparative psychometric analyses of the SCL-90-R and its short versions in patients with affective disorders. BMC Psychiatry. 2013;13:104. doi: 10.1186/1471-244X-13-104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tarescavage AM, Ben-Porath YS. Psychotherapeutic Outcomes Measures: A Critical Review for Practitioners: Evaluating Outcome Measures. J Clin Psychol. 2014:n/a–n/a. doi: 10.1002/jclp.22080. [DOI] [PubMed] [Google Scholar]
- 35.Ware J, Jr, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34(3):220–33. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 36.Larson CO. Use of the SF-12 instrument for measuring the health of homeless persons. Health Serv Res. 2002;37(3):733–50. doi: 10.1111/1475-6773.00046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Salyers MP, Bosworth HB, Swanson JW, Lamb-Pagone J, Osher FC. Reliability and validity of the SF-12 health survey among people with severe mental illness. Med Care. 2000;38(11):1141–50. doi: 10.1097/00005650-200011000-00008. [DOI] [PubMed] [Google Scholar]
- 38.Linehan MM, Heard HL. Treatment History Interview (THI) [Internet] 1987 Available from: http://depts.washington.edu/brtc/files/THI%204.pdf.
- 39.Pearson J, Stanley B, King C, Fisher C NIMH. Issues to Consider in Intervention Research with Persons at High Risk for Suicidality [Internet] [cited 2013 Dec 17];Issues Consider Interv Res Pers High Risk Suicidality. 2001 Available from: http://www.nimh.nih.gov/health/topics/suicide-prevention/issues-to-consider-in-intervention-research-with-persons-at-high-risk-for-suicidality.shtml. [PubMed] [Google Scholar]
- 40.Reynolds SK, Lindenboim N, Comtois KA, Murray A, Linehan MM. Risky assessments: participant suicidality and distress associated with research assessments in a treatment study of suicidal behavior. Suicide Life Threat Behav. 2006;36(1):19–34. doi: 10.1521/suli.2006.36.1.19. [DOI] [PubMed] [Google Scholar]
- 41.Linehan MM, Comtois KA, Ward-Ciesielski EF. Assessing and managing risk with suicidal individuals. Cogn Behav Pract. 2012;19(2):218–32. [Google Scholar]
- 42.Hilbe JM. Negative binomial regression. 2nd. Cambridge, UK; New York: Cambridge University Press; 2011. [Google Scholar]
- 43.Lesaffre E, Albert A. Partial separation in logistic regression. J R Stat Soc Ser B Methodol. 1989;51(1):109–16. [Google Scholar]
- 44.Gelman A, Jakulin A, Pittau MG, Su YS. A weakly informative default prior distribution for logistic and other regression models. Ann Appl Stat. 2008;2(4):1360–83. [Google Scholar]
- 45.R Development Core Team. R Foundation for Statistical Computing [Internet] Vienna, Austria: R Foundation for Statistical Computing; 2013. R: A language and environment for statistical computing. Available from: http://www.R-project.org/ [Google Scholar]
- 46.Gelman A, Su YS. arm: Data Analysis Using Regression and Multilevel/Hierarchical Models. 2013 [Google Scholar]
- 47.Pasic J, Russo J, Roy-Byrne P. High utilizers of psychiatric emergency services. Psychiatr Serv Wash DC. 2005;56(6):678–84. doi: 10.1176/appi.ps.56.6.678. [DOI] [PubMed] [Google Scholar]
- 48.United States Census Bureau State and County QuickFacts [Internet] US Department of Commerce; 2010. [cited 2014 May 10]. Available from: http://quickfacts.census.gov/qfd/states/53/5363000.html. [Google Scholar]
- 49.Kim J, Kinney S. The Myths and Facts of Homelessness [Internet] Seattle, WA: Interfaith Task Force on Homelessness; 2013. Available from: http://greaterseattlecares.org/wp-content/uploads/Homelessness-Myths-and-facts.pdf. [Google Scholar]
- 50.Linehan MM, Comtois KA, Murray AM, et al. Two-year randomized controlled trial and follow-up of dialectical behavior therapy vs therapy by experts for suicidal behaviors and borderline personality disorder. Arch Gen Psychiatry. 2006;63(7):757–66. doi: 10.1001/archpsyc.63.7.757. [DOI] [PubMed] [Google Scholar]
- 51.Linehan MM, Armstrong HE, Suarez A, Allmon D, Heard HL. Cognitive-behavioral treatment of chronically parasuicidal borderline patients. Arch Gen Psychiatry. 1991;48(12):1060–4. doi: 10.1001/archpsyc.1991.01810360024003. [DOI] [PubMed] [Google Scholar]
- 52.Brown GK, Ten Have T, Henriques GR, Xie SX, Hollander JE, Beck AT. Cognitive therapy for the prevention of suicide attempts: a randomized controlled trial. JAMA J Am Med Assoc. 2005;294(5):563–70. doi: 10.1001/jama.294.5.563. [DOI] [PubMed] [Google Scholar]
- 53.Comtois KA, Linehan MM. Psychosocial treatments of suicidal behaviors: a practice-friendly review. J Clin Psychol. 2006;62(2):161–70. doi: 10.1002/jclp.20220. [DOI] [PubMed] [Google Scholar]
- 54.Hawton K, Townsend E, Arensman E, et al. Psychosocial versus pharmacological treatments for deliberate self harm. Cochrane Database Syst Rev. 2000;(2):CD001764. doi: 10.1002/14651858.CD001764. [DOI] [PubMed] [Google Scholar]
- 55.Mann JJ, Apter A, Bertolote J, et al. Suicide prevention strategies: a systematic review. JAMA J Am Med Assoc. 2005;294(16):2064–74. doi: 10.1001/jama.294.16.2064. [DOI] [PubMed] [Google Scholar]
- 56.Ries RK, Yuodelis-Flores C, Roy-Byrne PP, Nilssen O, Russo J. Addiction and suicidal behavior in acute psychiatric inpatients. Compr Psychiatry. 2009;50(2):93–9. doi: 10.1016/j.comppsych.2008.07.003. [DOI] [PubMed] [Google Scholar]
- 57.SAMHSA/CSAT. TIP 50: Addressing Suicidal Thoughts and Behaviors in Substance Abuse Treatment - Literature Review with Update [Internet] [cited 2014 May 25];2012 Available from: http://store.samhsa.gov/product/TIP-50-Addressing-Suicidal-Thoughts-and-Behaviors-in-Substance-Abuse-Treatment/SMA09-4381.