Abstract
Aims
The choice of resynchronization therapy between with (CRT-D) and without (CRT-P) a defibrillator remains a contentious issue. Cause-of-death analysis among CRT-P, compared with CRT-D, patients could help evaluate the extent to which CRT-P patients would have additionally benefited from a defibrillator in a daily clinical practice.
Methods and results
A total of 1705 consecutive patients implanted with a CRT (CRT-P: 535 and CRT-D: 1170) between 2008 and 2010 were enrolled in CeRtiTuDe, a multicentric prospective follow-up cohort study, with specific adjudication for causes of death at 2 years. Patients with CRT-P compared with CRT-D were older (P < 0.0001), less often male (P < 0.0001), more symptomatic (P = 0.0005), with less coronary artery disease (P = 0.003), wider QRS (P = 0.002), more atrial fibrillation (P < 0.0001), and more co-morbidities (P = 0.04). At 2-year follow-up, the annual overall mortality rate was 83.80 [95% confidence interval (CI) 73.41–94.19] per 1000 person-years. The crude mortality rate among CRT-P patients was double compared with CRT-D (relative risk 2.01, 95% CI 1.56–2.58). In a Cox proportional hazards regression analysis, CRT-P remained associated with increased mortality (hazard ratio 1.54, 95% CI 1.07–2.21, P = 0.0209), although other potential confounders may persist. By cause-of-death analysis, 95% of the excess mortality among CRT-P subjects was related to an increase in non-sudden death.
Conclusion
When compared with CRT-D patients, excess mortality in CRT-P recipients was mainly due to non-sudden death. Our findings suggest that CRT-P patients, as currently selected in routine clinical practice, would not potentially benefit with the addition of a defibrillator.
Keywords: Heart failure, Sudden death, Cardioverter defibrillator, Competing risk, Cardiac resynchronization
See page 2777 for the editorial comment on this article (doi:10.1093/eurheartj/ehv474)
Introduction
Patients with congestive heart failure (HF) are at high risk of dying from its progression as well from sudden cardiac death related to ventricular tachyarrhythmia.1 Over the last decade, cardiac resynchronization therapy (CRT) and implantable cardioverter defibrillators (ICDs) have markedly improved the prognosis of HF patients, with prolongation of survival over and above that conferred by medical therapy alone.2–5 It has been well established in trials that in patients with severe left ventricular (LV) systolic dysfunction, New York Heart Association (NYHA) class III/IV symptoms, and wide QRS, CRT improves symptoms/quality of life and also reduces mortality.3,6 Additionally, more recent trials have shown beneficial reverse LV remodelling even in patients with milder symptoms.5,7–11 This has resulted in a class I recommendation for CRT in appropriately selected candidates in guidelines framed on both sides of the Atlantic.12,13
Since most patients who are candidates for CRT will have a LV ejection fraction (EF) of ≤35%, this ‘automatically’ makes them candidates for an ICD as well by the current guidelines, which makes the assumption that there is universally significant excess mortality due to sudden cardiac death (SCD) among CRT-P patients who can therefore definitively benefit from the added defibrillator.13 However, concrete evidence for such a premise in a contemporary CRT-P population is lacking and in any population of this kind; competing risks for mortality need to be carefully considered. A few studies have attempted to directly compare outcomes between CRT-P vs. CRT-D subjects.14,15 Furthermore, such outcome comparisons based on observational studies have methodological limitations and may be biased. Current guidelines do not make firm recommendations in terms of the choice between CRT-P vs. CRT-D, leaving room for physician discretion. This has resulted in wide variation in the rates of implantation worldwide. For instance, the proportion of CRT implantations, which are CRT-D, reaches >90% in most practices in the USA,16 whereas it is relatively lesser across Europe.17 The use of CRT-D or CRT-P in clinical practice is an important question with significant implications in terms of costs,18 as well as device-related complications.19,20
In this context, a better understanding of the relative contribution of SCD as opposed to other competing causes of mortality in the CRT population can be very informative. A cause-of-death analysis among CRT-P vs. CRT-D patients, may represent a novel approach to this problem. Using a large, multicentre study with prospective follow-up, we evaluated the characteristics of CRT-P vs. CRT-D patients in a real-world scenario and analysed to what extent CRT-P subjects, as currently chosen in clinical practice, would have potentially additionally benefited from the presence of a back-up defibrillator.
Methods
Setting and design of the study
CeRtiTuDe, a 2-year, prospective, multicentre registry launched in January 2008 and held under the direction of the Working Group on Pacing and Arrhythmias of the French Society of Cardiology, was funded and coordinated by the French Society of Cardiology. Its primary objective was to define the baseline characteristics and clinical outcomes of French patients who undergo implantation of CRT systems. An analysis of the precise causes of death was planned at 2 years after device implantation.
The 41 medical centres participating in the study (Appendix) enrolled consecutive patients who, between 1 January 2008 and 31 December 2010, had undergone CRT device implantations. The criteria for CRT implantation were as per the 2007 guidelines of the European Society of Cardiology and European Heart Rhythm Association, updated in 2010. However, all CRT recipients were enrolled, in order for the registry to reflect ‘real-world’ medical practice. Each patient was then enrolled in a specific follow-up programme with clinical, ECG, echocardiographic, and device interrogation data collected every 6 months over the following 2 years (up to 1 January 2013).
The study was conducted in accordance with Good Clinical Practice, French Law, and the French data protection law. The protocol was reviewed by the Committee for the Protection of Human Subjects in Biomedical Research (CCTIRS #08-522) and the data file was reported to, and authorized by, the Commission Nationale Informatique et des Libertés (French Data Protection Committee, CNIL #909048).
Baseline characteristics at implant
Individual patient data were collected, using an electronic case report form created by the Scientific Committee to record, at each participating medical centre, the demographic and baseline clinical characteristics, and the implantation procedures and techniques. These data were regularly transferred (every 3 months) via an internet-based system to a central database created at the data management centre of the French Society of Cardiology in collaboration with the Paris Cardiovascular Research Center, European Georges Pompidou Hospital, Paris (INSERM Unit 970).
All variables recorded before device implantation were defined and classified using standard clinical terminology, including gender, age (stratified as <60, 60–74, and ≥75 years), and underlying heart disease (ischaemic vs. non-ischaemic). Renal clearance was estimated using the Cockroft and Gault's formula, and defined as severe renal insufficiency if <30 mL/min/1.73 m2, and QRS duration was classified as ≤120, 121–149, and ≥150 ms. Left ventricular ejection fraction was measured on transthoracic echocardiograms, using Simpson's method, and recorded as a continuous variable and also stratified as ≤20, 21–35, and >35%. A history of atrial fibrillation (AF) was based on medical records, and classified as paroxysmal or permanent. In addition to AF and renal failure, other co-morbidities were systematically recorded, including cancer, chronic obstructive pulmonary disease, liver disease, diabetes mellitus, and cerebral vascular disease.
Device implant, hospital discharge, and follow-up
The type of CRT (CRT-P or CRT-D) implanted was recorded without the manufacturer's information. The complications recorded included infections, changes in capture threshold, lead dislodgement, haematomas, HF, fever, arrhythmias, pneumothorax, phrenic nerve stimulation, and death. Finally, drug regimens prescribed at the time of hospital discharge including beta-adrenergic blockers, anti-arrhythmics, digoxin, calcium antagonists, angiotensin-converting enzyme inhibitors or angiotensin II receptor blockers, mineralocorticoid receptor antagonists, diuretics, and anticoagulants were recorded. Device programming was left to the discretion of the investigators at each centre, with the guiding principle being achievement of maximal biventricular pacing.
All patients were followed at 6-month intervals for 2 years by the implanting centre till the close of study on 1 January 2013. At each follow-up, the patients underwent clinical examination, ECG, transthoracic echocardiogram, and device interrogation. In addition, information on any intercurrent events (such as hospitalization) was also recorded in the file. The above data were systematically gathered at each follow-up visit from the date of device implantation to study closure or death or heart transplantation.
Vital status, specific causes of death, and adjudication process
The investigators at each enrolling centre recorded major clinical events, using a standardized form, and a Clinical Events Committee verified their accuracy by contacting the attending physicians or the patients as required, on a yearly basis, focusing on the vital status and on the specific modes and causes of death and on major clinical events or interventions during follow-up, including changes in drug regimens, as well as interim hospitalizations. Sources to ascertain the vital status also included registries of the patients' birthplaces, the French National Institute of Health and Medical Research (INSERM CépiDc Unit—Le Kremlin-Bicêtre, France), and the French National Institute of Statistics and Economical Studies.
The cause-of-death were classified as sudden if the patient (i) died suddenly and unexpectedly within 1 h of symptoms in the absence of progressive cardiac deterioration, (ii) died unexpectedly in sleep, or (iii) died unexpectedly within 24 h after last being seen alive and in the usual state of health. Other cardiovascular deaths included myocardial infarction, HF, acute aortic syndrome, stroke, and pulmonary embolism. Fatal arrhythmias associated with end-stage HF were classified as non-sudden cardiovascular deaths. Deaths attributable to causes, such as cancer, infectious disease, or renal or respiratory failure, were classified as non-cardiovascular. When inadequate or no data were available, the cause of death was classified as unknown or unidentifiable. We used multiple sources to assess and finally adjudicate the cause of death, which included medical data obtained by the regional investigators, pathology report, Emergency Medical Services report, as well as data from the French Center on Medical Causes of Death (INSERM CépiDc unit), which is able to provide the causes of death occurring in France.
Statistical analysis
This report was prepared in compliance with the STROBE checklist for observational studies.21 Continuous variables are presented as mean ± standard deviation and categorical variables are presented as numbers and percentages. Comparisons between groups (patients with CRT-P vs. patients with CRT-D) were made, using the χ2 or Fisher's exact tests for discrete variables and with unpaired t-tests, Wilcoxon signed-rank tests, or one-way analysis of variance for continuous variables. Factors associated with the implantation of CRT-P were identified, using a multiple variable, stepwise, logistic regression analysis.
Kaplan–Meier curves were constructed to estimate the 2-year survival, and CRT-P and CRT-D groups were compared using the log-rank test. For the cause-specific mortality, we used a competing risk analysis and estimated the cumulative incidence function. We then used Gray tests to assess the difference between the CRT-P and CRT-D groups.22 A Cox proportional hazards regression analysis was used to identify variables independently associated with overall mortality. The proportional hazard assumptions were tested. The crude associations between mortality and different variables (listed in Table 1) were first quantified by univariate Cox regression. All covariates that reached a significance level of P < 15% were then included in an initial multivariate regression model. A stepwise selection was applied to obtain a final model that included covariates with P < 5%. Given the observational design of the study and minimization of indication bias for device implantation, propensity score analyses were conducted. We estimated the propensity score of receiving a CRT-P therapy by fitting a logistic regression model using age, sex, AF, LVEF, aetiology of HF, NYHA, and beta-adrenergic blockers as covariates. We then matched patients who received CRT-D therapy with those who received CRT-P in an 1 : 1 ratio using a greedy matching algorithm with a maximum allowable difference of 0.05 (see Supplementary material online, Table S1 and Figure S1). Patients who could not be matched using these criteria were removed from the analysis. Then, the association between device type and mortality was repeated after propensity score matching (462 patients). All data were analysed at INSERM, Unit 970, Cardiovascular Epidemiology and Sudden Death, Paris, using SAS version 9.4 (SAS Institute, Inc., Cary, NC, USA).
Table 1.
Characteristics of the entire registry sample and of the CRT-P vs. CRT-D recipients
| Total (N = 1705) | CRT-D (N = 1170) | CRT-P (N = 535) | P-value | |
|---|---|---|---|---|
| Age (years) | 68.8 ± 11.1 | 65.6 ± 10.4 | 75.9 ± 9.0 | <0.0001 |
| Men | 1317 (77.2) | 945 (80.8) | 372 (69.5) | <0.0001 |
| Heart disease | ||||
| Ischaemic | 724 (47.0) | 556 (49.3) | 168 (40.7) | 0.0026 |
| Non-ischaemic | 816 (53.0) | 571 (50.7) | 245 (59.3) | |
| QRS duration | ||||
| Mean (ms) | 157.7 ± 27.1 | 155.0 ± 26.2 | 160.8 ± 29.0 | 0.0018 |
| Left ventricular ejection fraction | ||||
| Median, % | 25.5 (10.0) | 25.5 (10.0) | 25.5 (10.0) | 0.084 |
| ≤20% | 484 (29.3) | 333 (29.2) | 151 (29.6) | <0.0001 |
| 21–35% | 1078 (65.3) | 764 (67.1) | 314 (61.5) | |
| >35% | 88 (5.3) | 42 (3.7) | 46 (9.0) | |
| New York Heart Association functional class | ||||
| I | 16 (1.0) | 14 (1.3) | 2 (0.4) | <0.0001 |
| II | 250 (16.0) | 194 (18.0) | 56 (11.7) | |
| III | 1188 (76.2) | 824 (76.2) | 364 (76.0) | |
| IV | 106 (6.8) | 49 (4.5) | 57 (11.9) | |
| History of: | ||||
| Atrial fibrillation | 445 (27.3) | 248 (22.1) | 197 (38.7) | <0.0001 |
| Renal insufficiency | 211 (14.4) | 138 (13.0) | 73 (18.2) | 0.0128 |
| COPD | 264 (18.1) | 198 (18.7) | 66 (16.4) | 0.3120 |
| Cancer | 122 (8.4) | 88 (8.3) | 34 (8.5) | 0.9272 |
| Miscellaneous disorders | 266 (18.2) | 174 (16.4) | 92 (22.9) | 0.0043 |
| Drug therapy at the time of implantation | ||||
| Diuretics | 1045 (66.2) | 752 (69.2) | 293 (59.6) | 0.0002 |
| ACE inhibitors/ARB | 1057 (66.9) | 792 (72.9) | 265 (53.9) | <0.0001 |
| MRA | 404 (25.6) | 331 (30.5) | 73 (14.8) | <0.0001 |
| Beta-adrenergic blockers | 945 (59.9) | 732 (67.3) | 213 (43.3) | <0.0001 |
| Oral anticoagulant agent | 658 (41.7) | 438 (40.3) | 220 (44.7) | 0.0989 |
| Antiplatelet agents | 693 (43.9) | 512 (47.1) | 181 (36.8) | 0.0001 |
Values are means ± SD, median (IQR), or numbers (%) of observations.
ACE, angiotensin-converting enzyme; ARB, angiotensin receptor blocker; COPD, chronic obstructive pulmonary disease; MRA, mineralocorticoid receptor antagonist; CRT-D: cardiac resynchronization therapy with defibrillator; CRT-P: cardiac resynchronization therapy without defibrillator.
Results
Baseline characteristics and device implantation
Overall, a total of 1705 consecutive patients were enrolled in the study and received CRT devices. The mean age of the overall population was 68.8 ± 11.1 years, 33% were >75 years of age, and 77% were men. Nearly 20% had been hospitalized for decompensated HF within the previous 6 months. The heart disease was ischaemic in 47% of patients and related to non-ischaemic dilated cardiomyopathy in 53%. Overall, 29% of patients presented with a LVEF of ≤20% at the time of implantation.
A CRT-D was implanted in 1170 patients (69%). Overall, 13% of the CRT-D group was implanted in the secondary prevention, following symptomatic ventricular tachycardia or sudden cardiac arrest. Patients with CRT-P compared with CRT-D were older (75.9 vs. 65.6 years, P < 0.0001), less often male (69.5 vs. 80.8%, P < 0.0001), more symptomatic (proportion of NYHA class III/IV, 87.9 vs. 80.8%, P = 0.0005), with less coronary artery disease (40.7 vs. 49.3%, P = 0.003), wider QRS (160.8 vs. 154.9 ms, P = 0.002), more AF (38.7 vs. 22.1%, P < 0.0001), and more co-morbidities (≥2 comorbidities, 16.9 vs. 12.9%, P = 0.04; Table 1). Independent variables associated with CRT-P (vs. CRT-D) implantation are depicted in Table 2.
Table 2.
Independent variables associated with CRT-P (vs. CRT-D) implantation
| Variables | OR | 95% CI | P-value |
|---|---|---|---|
| Age | 1.17 | 1.14–1.19 | <0.0001 |
| Female | 1.78 | 1.24–2.55 | 0.0018 |
| Dilated non-ischaemic cardiomyopathy | 1.75 | 1.28–2.40 | 0.0005 |
| Atrial fibrillation | 1.58 | 1.14–2.20 | 0.0062 |
| LVEF <25% | 1.05 | 1.02–1.07 | 0.0001 |
| NYHA IV | 2.82 | 1.61–4.92 | 0.0003 |
| No beta-adrenergic blockers | 2.40 | 1.76–3.26 | <0.0001 |
LVEF, left ventricular ejection fraction; NYHA, New York Heart Association; CRT-D: cardiac resynchronization therapy with defibrillator; CRT-P: cardiac resynchronization therapy without defibrillator.
Fatal periprocedural complications occurred in one patient, and death occurred before hospital discharge in five others (0.3%), due to severe cardiogenic shock. Overall, significant perioperative complications occurred in 133 subjects (7.8%) without significant difference between CRT-D and CRT-P (8.9 vs. 6.7%, P = 0.20). Pulse generator pocket haematoma (2.5%), lead dislodgment (1.6%), and phrenic nerve stimulation (1.6%) were the most frequent complications, and the need for new intervention during the same hospital stay was observed in 40 patients (2.3%).
Follow-up, overall mortality, and specific causes of death
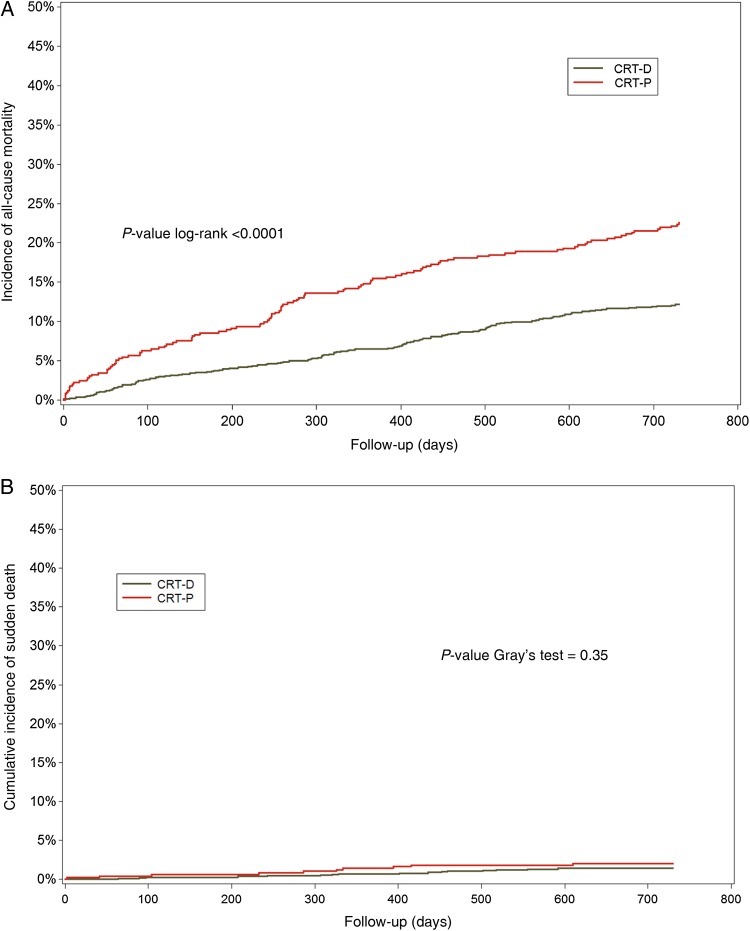
The 1705 consecutive patients enrolled in the study were followed for a mean of 665.6 ± 173.8 days (1.0–730.5 days). At 2-year follow-up (completed in 94.5% of subjects), 267 patients died, giving an overall annual mortality rate of 83.8% (95% CI 73.4–94.2) per 1000 person-years, with a higher rate among CRT-P, compared with CRT-D, patients [130.8 vs. 65.1 per 1000 year, respectively, relative risk (RR) 2.01, 95% CI 1.56–2.58, P < 0.0001; Figure 1A]. The incidence of SCD was not statistically higher in the CRT-P group compared with CRT-D (RR 1.57, 95% CI 0.71–3.46, P = 0.42) (Figure 1B). The rate of hospitalization for HF was not different between the CRT-D vs. CRT-P groups (19.6 vs. 22.0%, P = 0.28).
Figure 1.
Overall mortality incidence over time according to CRT-P and CRT-D groups. (A) Overall mortality and (B) sudden cardiac death. CRT-D: cardiac resynchronization therapy with defibrillator; CRT-P: cardiac resynchronization therapy without defibrillator.
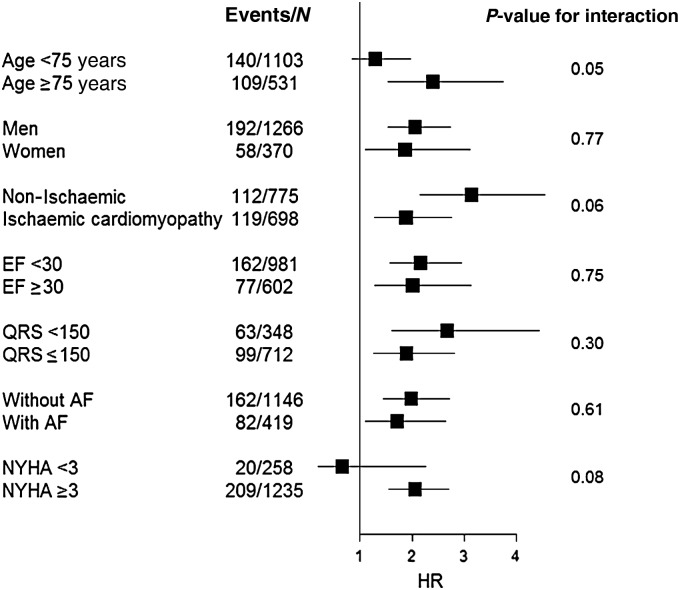
After considering potential confounding factors in a Cox proportional hazards regression analysis, CRT-P remained associated with increased mortality [hazard ratio (HR) 1.54, 95% CI 1.07–2.21, P = 0.0209], as well as the presence of co-morbidities (HR 1.98, 95% CI 1.34–2.92, P = 0.0006) and functional NYHA class IV (HR 1.85, 95% CI 1.10–3.11, P = 0.0207). Using the propensity-matched cohort, CRT-P was associated with increased mortality (RR 2.0, 95% CI 1.22–3.28, P = 0.01). Cardiac resynchronization therapy without defibrillator was not associated with a higher incidence of SCD (RR 1.21, 95% CI 0.45–3.29, P = 0.70). Forest plots showing hazard ratios of CRT-P vs. CRT-D for mortality by different subgroups were represented in Figure 2.
Figure 2.
Forest plots showing unadjusted hazard ratios of CRT-P vs. CRT-D for mortality by different subgroups. CRT-D: cardiac resynchronization therapy with defibrillator; CRT-P: cardiac resynchronization therapy without defibrillator.
However, when considering the specific cause-of-death analysis (Table 3), the increase in mortality among CRT-P patients was not related to that in SCD, though SCD incidence was higher in the CRT-P group: 11.8 per 1000 among CRT-P vs. 7.5 per 1000 among CRT-D recipients (P = 0.26). The main reasons for the almost twice-higher risk of death in the CRT-P group were an increase in non-SCD cardiovascular mortality, mainly comprising progressive HF (RR 2.27, 95% CI 1.62–3.18) as well as other cardiovascular mortality (RR 4.40, 95% CI 1.29–15.03). Overall, 95% of the excess mortality among CRT-P recipients was not related to SCD.
Table 3.
Incidence of specific causes of death among CRT-P and CRT-D recipients
| Incidences (per 1000 patient-years) | CRT-P (N = 535) | CRT-D (N = 1170) | Unadjusted risk ratio (95% CI) |
|---|---|---|---|
| Total mortality | 130.8 | 65.1 | 2.01 (1.56–2.58) |
| Cardiovascular | |||
| Heart failure | 75.4 | 33.3 | 2.27 (1.62–3.18) |
| Sudden death | 11.8 | 7.5 | 1.57 (0.71–3.46) |
| Others | 8.3 | 1.9 | 4.40 (1.29–15.03) |
| Device-related | 1.2 | 2.8 | 0.42 (0.05–3.48) |
| Non-cardiovascular | 31.8 | 19.7 | 1.62 (1.00–2.62) |
CRT-D: cardiac resynchronization therapy with defibrillator; CRT-P: cardiac resynchronization therapy without defibrillator.
Discussion
To the best of our knowledge, our study provides the first cause-of-death analysis comparing CRT-P with CRT-D patients in a real-world population. We demonstrate that CRT-P patients, as chosen in routine clinical practice, were older, more likely to be female, with less ischaemic heart disease, more advanced HF, and greater co-morbidity burden compared with CRT-D patients. These characteristics of the CRT-P patients are in agreement with previous reports.14,19 At 2 years, the overall mortality in the CRT-P group was greater than that in the CRT-D group. However, importantly, this difference in mortality was mostly accounted for by an increase in non-SCD. Since SCD did not significantly contribute to the excess mortality in the CRT-P group, it suggests that the presence of a back-up defibrillator would probably not have been beneficial in terms of improving survival for these patients. The rates of HF hospitalization were greater in the CRT-P group, which is in line with the greater HF mortality in this group. This is likely related to a sicker population with more co-morbidity, older age, and potentially more severe HF and serves to highlight that progressive HF rather than SCD may be the main driver of morbidity as well as mortality in the CRT-P population. These results from a large, prospective cohort with robust cause-of-death adjudication need careful consideration in the context of the current controversy in the selection of CRT-P vs. CRT-D. Our study is not intended as a direct comparison of outcomes between CRT-D and CRT-P, and subgroup analyses should be interpreted with caution. While direct comparisons in observational studies may reveal differences in death rates, knowledge of what makes up this difference takes our understanding an important step further. Cause-of-death analysis, while being technically challenging to perform in a large population, represents an innovative, alternate approach to this problem. It also helps bring to the forefront the issue of competing risks for mortality in any population of this nature.
With the exception of patients with AF, where the evidence-base is admittedly weaker,20 CRT represents an important therapeutic option for a growing segment of the HF population. Though the guidelines presently do not make definitive recommendations for CRT-D vs. CRT-P, in practice, many physicians may feel compelled to use CRT-D, as a defibrillator is considered ‘necessary’ in the presence of low LVEF. The effect of this choice may be even greater in light of the fact that many centres are exploring broader indications for CRT in patients with milder symptoms and narrow QRS.23 This has important economic implications in that the incremental cost of CRT-D over CRT-P is significantly greater when compared with the cost over optimal medical therapy and this difference is even steeper in the older age group.24 The addition of a defibrillator lead can also contribute to additional adverse events and need for repeat procedures.25 Thus, there is a fairly urgent need for more data such as from the present study to tease out the putative benefits of an added defibrillator over CRT-P,25 and to better define optimal criteria to select CRT-P or CRT-D. Since the CRT-P group had a greater proportion of non-ischaemic cardiomyopathy where the benefit from primary preventive ICD is lower, this could influence results as well.6 In the absence of proven superiority by trials and the small survival benefit, the 2013 European Society of Cardiology Task Force was of the opinion that no strict recommendations can be made, and has preferred to merely offer guidance regarding the selection of patients for CRT-D or CRT-P,13 based on overall clinical condition, device-related complications, and cost; factors favouring CRT-P being advanced HF, co-morbidities, including frailty and cachexia. In contrast, factors favouring CRT-D implantation are life expectancy >1 year, stable HF, moderate functional status, ischaemic heart disease, and lack of comorbidities being in favour of CRT-D implantation, and the French practice appears to be in agreement with this.
The only randomized trial to have CRT-P as well as CRT-D arms—the COMPANION trial did not show a significant benefit of CRT-D over CRT-P for the primary endpoint.6 However, the study was not powered to compare these two treatments. Non-randomized studies, which have compared outcomes for these two modalities, have yielded conflicting results. Using registry-based data, Morani et al.14 showed that among patients with an European Society of Cardiology Class IA indication for CRT, CRT-D was associated with better survival than CRT-P. Similar findings were reported from a US-based registry, which concluded that ‘CRT-D should be recommended to most congestive HF patients with indications for biventricular pacing’.27 However, recent experience with reasonable numbers of patients emphasized the higher risk of mortality among CRT-P patients compared with CRT-D, indicating that long-term benefit of an additional defibrillator may be restricted to a selected subgroup.15,19 Furthermore, logistic regression models which are relied on in comparative studies to draw conclusions, may not adequately overcome the limitations in comparing heterogeneous groups.28 A Bayesian network meta-analysis in 2007 concluded that evidence from randomized trials is insufficient to prove the superiority of CRT-D over CRT-P.29
Whether CRT-P by itself reduces risk of arrhythmia is still a matter of some debate. Long-term data from CARE-HF show reduction in SCD rates by CRT.30 A mechanistic link is supported by the fact that SCD is reduced in subjects with systolic HF and ventricular dyssynchrony.31 Recent analysis from the MADIT-CRT trial showed that risk of ventricular arrhythmias was significantly reduced in CRT patients with normalization of LVEF. Importantly, risk of inappropriate ICD therapy was unchanged, suggesting that these patients may be better served by a downgrade to CRT-P at device change.32 Similarly, another study showed that based on LVEF improvement, up to one-third of CRT-D patients no longer had an ongoing indication for ICD at the time of battery change and the rate of device therapy in this group was very low.33 By inducing favourable remodelling of the LV, CRT may reduce the substrate for ventricular arrhythmias. Some patients experience rapid reverse remodelling (‘super responders’), with major improvement in EF so that they are no longer ICD candidates. Data suggest that such patients have excellent long-term prognosis.34,35 In anticipation of rapid improvement of LVEF, it would seem logical to provide temporary protection against SCD such as using a life vest rather than implanting a defibrillator. However, although predictors of super response have been proposed,36,37 it is still difficult to identify such super responders with a high degree of confidence; thus, more work may be needed in this regard. The rationale for an anti-arrhythmic effect of CRT is also tempered to some extent by concerns over the pro-arrhythmic effects of LV pacing.38,39 Prospective follow-up of patients with CRT-P has shown that the incidence was overall relatively low, and that sudden cardiac death events were likely to be preceded by recorded sustained ventricular arrhythmias, emphasizing the importance of regular CRT-P device memory interrogation, as well as the potential benefit of remote monitoring in these patients, for possible urgent upgrading to CRT-D.40 The possibility of accurate and continuous surveillance to detect life-threatening arrhythmias, with upgrading of CRT-P patients to CRT-D only after such objective documentation during follow-up, might represent a safe and cost-effective alternative to the practice of universal CRT-D implantation in all CRT candidates.
Our results should not be interpreted as a general lack of benefit from CRT-D vs. CRT-P or vice versa. Rather, we demonstrate that given currently selected CRT-P patients in the French population, addition of a defibrillator may not significantly add to survival. At least in a subset of the ‘CRT eligible’ HF population, competing risks of non-sudden death may diminish the incremental value of adding a defibrillator to CRT; therefore, all patients eligible for CRT cannot be ‘automatically’ considered as requiring a CRT-D. Thus, in a broader context, the requirement for CRT-D in similar populations needs careful consideration of the putative risks and benefits.
Relative strengths of the present study include the fact that it is prospective, multicentric with dedicated cause-of-death adjudication. However, we acknowledge some limitations. First, the study was non-randomized and therefore, selection bias may have influenced results. The clinical decision concerning device type may affect subsequent management as well lead to variations in clinical care. On the other hand, randomized trials, while being a rigorous design, have rigid selection criteria, which often do not reflect real-world scenarios. Though the results need to be interpreted with caution in view of potential confounding, it reflects actual clinical practice. Secondly, follow-up was censured at 2 years, which can influence results as device utilization is a function of time; however, there were adequate events during follow-up to draw reasonable conclusions. Thirdly, information on QRS morphology was unavailable and the extent of LBBB in the two groups may have influenced CRT outcomes. Finally, although our study suggests that mortality in this real-world CRT-P population may not be improved by upgrade to CRT-D, it does not address the question of whether, in the population implanted with a CRT-D device, CRT-P would perform just as well. Thus, this study was not intended to answer the question of whether CRT-P is comparable with CRT-D overall, but rather provides a real-world assessment of cause of death in a contemporary CRT-P vs. CRT-D population, which we believe can more meaningfully inform clinical practice. It should be borne in mind that these outcomes mainly pertain to a HF population with broad QRS.
Conclusion
In this prospective, multicentre cohort study, CRT-P patients were older, with more advanced HF, and co-morbidities when compared with CRT-D recipients. At 2-year follow-up, CRT-P patients had 2-fold higher mortality than CRT-D. By cause-of-death analysis, the excess mortality among CRT-P subjects was almost entirely related to non-SCD. Our results indicate that CRT-P patients, as currently selected in routine clinical practice, would potentially not benefit from addition of a defibrillator, emphasizing that there is still considerable room for CRT-P in the present day HF treatment.
Authors’ contributions
E.M., S.J., M.-C.P., J.-P.E., and X.J.: performed statistical analysis; J.-Y.L.H.: handled funding and supervision; E.M., J.L.-G., M.-C.P., and G.M.: acquired the data; E.M., C.L., M.C., G.M., J.-C.D., and J.-Y.L.H.: conceived and designed the research; C.L., K.N., S.B., D.K., P.D., and O.P.: drafted the manuscript; J.-C.D., J.-S.H., P.M., D.G., O.C., F.H.-L., F.A., P.C., and P.M.: made critical revision of the manuscript for key intellectual content.
Supplementary material
Supplementary material is available at European Heart Journal online.
Funding
CeRtiTuDe was funded by grants from the French Institute of Health and Medical Research (INSERM) and from the French Society of Cardiology. A specific research grant support was funded specifically for the CeRtiTuDe cohort study from Biotronik, Boston Scientific, Medtronic, Sorin and St. Jude Medical. Funding to pay the Open Access publication charges for this article was provided by the French Society of Cardiology.
Conflict of interest: S.B. is a consultant for Medtronic, Inc., Boston Scientific, and Sorin Group. P.D. is a consultant for Medtronic, Boston Scientific. and Sorin Group. D.G. is a consultant for Medtronic, Boston Scientific, Saint Jude Medical, and Biotronik. C.L. received lectures and honorarium from Medtronic, Inc., Boston Scientific, St. Jude Medical, Biotronik, and Sorin Group. P.M. received lectures and honorarium from Boston Scientific, Biotronik, and Sorin Group. O.P. received lectures and honorarium from Medtronic, Inc., St. Jude Medical, Biotronik, and Sorin Group. F.H.-L. is a consultant for Medtronic, Inc., and Biotronik. S.C. is a consultant for Medtronic and Sorin Group.
Acknowledgement
The authors thank Guillaume Galidie, MD, Frankie Beganton, MS, Florence Bourrely, MS, Nicolas Estrugo, MS, and Florian Prevost, MS, for collecting data.
Appendix
The following investigators and institutions participated in the conception of the registry, and in the organization, collection, storage, and analysis of the data.
Principal Investigator: Jean-Yves Le Heuzey, MD
Collaborating Investigators
Ambroise Pare Clinic: Bruno Cauchemez, Alain Khemache, and Olivier Thomas.
Amiens University Hospital: Jean-Sylvain Hermida, Mathieu Kubala, Armelle Mathiron, and Sarah Traullé.
Angers University Hospital: Jean-Marc Dupuis, Anthony Foucault, and Aude Tassin.
Antoine Beclere University Hospital: Vincent Algalarrondo, Sylvie Dinanian, Christophe Juin, and Claude Sebag.
Besançon University Hospital: Florent Briand, Alexandre Guignier, and Sébastien Janin.
Caen University Hospital: Laure Champ-Rigot, Sophie Gomes, Paul Milliez, Arnaud Pellissier, and Patrice Scanu.
Dijon University Hospital: Olivier Barthez, Géraldine Bertaux-Cattarossi, Régine Duvernay-Debin, Fabien Farnier, Gabriel Laurent, and Alexandra Martel-Bourcier.
Grenoble University Hospital: Pascal Defaye and Peggy Jacon.
Infirmerie Protestante de Lyon: Cyril Durand, Alexis Durand-Dubief, Nicolas Monsarrat, and Hervé Poty.
Lille University Hospital: Stéphane Boulé, François Brigadeau, Frédéric Fossati, Laurence Guédon-Moreau, Mustapha Jarwe, Salem Kacet, Didier Klug, Claude Kouakam, Dominique Lacroix, and Christelle Marquie.
Limoges University Hospital: Patrick Blanc, Najmeddine Echahidi, Eric Espaliat, Benoit Guy-Moyat, and Jérôme Lesage.
Marseille University Hospital: Jean-Claude Deharo, Frédéric Franceschi, and Sébastien Prévot.
Nancy University Hospital: Etienne Aliot, Marius Andronache, Béatrice Brembillat Perrot, Christian de Chillou, and Nicolas Sadoul.
Pitie Salpetriere: Nicolas Badenco, Thomas Chastre, Guillaume Duthoit, Robert Frank, Estelle Gandjbakhch, Olivier Gartenlaub, Françoise Hidden-Lucet, Caroline Himbert, Xavier Waintraub, and Thierry Zerah.
Reims University Hospital: Karine Bauley, Jean-Pierre Chabert, Alain Deschildre, François Lesaffre, Angéline Martin, and Colette Rio.
Rennes University Hospital: Jean-Claude Daubert, Christophe Leclercq, Philippe Mabo, and Dominique Pavin.
Rouen University Hospital: Fréderic Anselme, Bénédicte Godin, and Arnaud Savouré.
Saint-Etienne University Hospital: Laurence Bisch, Antoine Da Costa, and Cécile Romeyer.
Strasbourg University Hospital: Babe Bakou Boula, François Bronner, Michel Chauvin, Marie-Pierre Douchet, Laurence Jesel, Halim Marzak, and Alexandre Schatz.
Toulouse University Hospital: Christelle Cardin, Talia Chilon, Marc Delay, Alexandre Duparc, Anne Garderes-Rollin, Philippe Maury, Pierre Mondoly, Elisabeth Somody, and Emile Thomson.
Lyon University Hospital: Philippe Chevalier, Arnaud Dulac, Marcin Mlotek, and Emilie Nonin-Babary.
European Georges Pompidou Hospital: Xavier Jouven, Thomas Lavergne, Jean-Yves Le Heuzey, Eloi Marijon, and Akli Otmani.
Nouvelles Cliniques Nantaises: Marc Burban, Jean-Pierre Cebron, and Daniel Gras.
Pole Sante Republique: Pascal Barraud, Stéphane Langlade, Janusz Lipiecki, François Philippot, Alain Richard, Isabelle Robin, Christian Schandrin, and Dominique Vacher.
Albi General Hospital: Christelle Cardin, Mohammed Reza Rezaei, and Philippe Rumeau.
Belfort-Monbeliard General Hospital: Renaud Fouché and Stéphane Fromentin.
Bretagne Sud General Hospital: Pierre Khattar, Jacques Le Potier, Jamal Mouhid, and Laurent Palud.
Centre hospitalier Marechal Joffre – Hôpital Saint-Jean: Henri Andres, Christian Boureux, Patrick Chopat, Georges Nadji, Pierre Sultan, and Frédéric Targosz.
Montauban General Hospital: Jean-Philippe Doazan, Nourédine El Hajjaji, Sofiene Hannachi, Romain Noblemaire, and Elisabeth Somody.
Centre Cardiologique du Nord: Xavier Copie, Gilles Lascault, Olivier Paziaud, and Olivier Piot.
La Roche sur Yon General Hospital: Olivier Billon, Claude Gully, Georges Haddad, Damien Lipp, and Driss Mouhoub.
La Rochelle General Hospital: Paul Bru, Cécile Duplantier-Duchêne, and Antoine Milhem.
Metz General Hospital: Julien Bertrand, Michel Boursier, Khalifé Khalife, Noura Zannad, and Aude Zanutto.
Saint Philibert General Hospital: Estelle Cuvelier, Cécile Donfafk, Pierre Graux, Aurélie Guiot, Yves Guyomar, Sébastien Heuls, John Kallumannil, and Marc Semichon.
Saint-Joseph et Saint-Luc General Hospital: Benjamin Gal, Michel Lopez, and Julien Pineau.
Clinique Belledonne: Xavier Dreyfus, Laure Hammer, and Luc Petit.
Clinique Lafourcade: Xavier Harle and Julien Laborderie.
Clinique Pasteur: Jean-Paul Albenque, Serge Boveda, Nicolas Combes, Stéphane Combes, and Christophe Goutner.
Clinique Saint Gatien: Olivier Césari, Patrick Chenevez, Christophe Loose, and Patrick Peycher.
Clinique du Tonkin: Cyril Durand, Alexis Durand-Dubief, and Hervé Poty.
Clinique Bizet: Christine Alonso, Serge Cazeau, Caroline Grimard, Gael Jauvert, and Arnaud Lazarus.
Contributor Information
Collaborators: for the CeRtiTuDe Investigators, Jean-Yves Le Heuzey, Bruno Cauchemez, Alain Khemache, Olivier Thomas, Jean-Sylvain Hermida, Mathieu Kubala, Armelle Mathiron, Sarah Traullé, Jean-Marc Dupuis, Anthony Foucault, Aude Tassin, Vincent Algalarrondo, Sylvie Dinanian, Christophe Juin, Claude Sebag, Florent Briand, Alexandre Guignier, Sébastien Janin, Laure Champ-Rigot, Sophie Gomes, Paul Milliez, Arnaud Pellissier, Patrice Scanu, Olivier Barthez, Géraldine Bertaux-Cattarossi, Régine Duvernay-Debin, Fabien Farnier, Gabriel Laurent, Alexandra Martel-Bourcier, Pascal Defaye, Peggy Jacon, Cyril Durand, Alexis Durand-Dubief, Nicolas Monsarrat, Hervé Poty, Stéphane Boulé, François Brigadeau, Frédéric Fossati, Laurence Guédon-Moreau, Mustapha Jarwe, Salem Kacet, Didier Klug, Claude Kouakam, Dominique Lacroix, Christelle Marquie, Patrick Blanc, Najmeddine Echahidi, Eric Espaliat, Benoit Guy-Moyat, Jérôme Lesage, Jean-Claude Deharo, Frédéric Franceschi, Sébastien Prévot, Etienne Aliot, Marius Andronache, Béatrice Brembillat Perrot, Christian de Chillou, Nicolas Sadoul, Nicolas Badenco, Thomas Chastre, Guillaume Duthoit, Robert Frank, Estelle Gandjbakhch, Olivier Gartenlaub, Françoise Hidden-Lucet, Caroline Himbert, Xavier Waintraub, Thierry Zerah, Karine Bauley, Jean-Pierre Chabert, Alain Deschildre, François Lesaffre, Angéline Martin, Colette Rio, Jean-Claude Daubert, Christophe Leclercq, Philippe Mabo, Dominique Pavin, Fréderic Anselme, Bénédicte Godin, Arnaud Savouré, Laurence Bisch, Antoine Da Costa, Cécile Romeyer, Babe Bakou Boula, François Bronner, Michel Chauvin, Marie-Pierre Douchet, Laurence Jesel, Halim Marzak, Alexandre Schatz, Christelle Cardin, Talia Chilon, Marc Delay, Alexandre Duparc, Anne Garderes-Rollin, Philippe Maury, Pierre Mondoly, Elisabeth Somody, Emile Thomson, Philippe Chevalier, Arnaud Dulac, Marcin Mlotek, Emilie Nonin-Babary, Xavier Jouven, Thomas Lavergne, Jean-Yves Le Heuzey, Eloi Marijon, Akli Otmani, Marc Burban, Jean-Pierre Cebron, Daniel Gras, Pascal Barraud, Stéphane Langlade, Janusz Lipiecki, François Philippot, Alain Richard, Isabelle Robin, Christian Schandrin, Dominique Vacher, Christelle Cardin, Mohammed Reza Rezaei, Philippe Rumeau, Renaud Fouché, Stéphane Fromentin, Pierre Khattar, Jacques Le Potier, Jamal Mouhid, Laurent Palud, Henri Andres, Christian Boureux, Patrick Chopat, Georges Nadji, Pierre Sultan, Frédéric Targosz, Jean-Philippe Doazan, Nourédine El Hajjaji, Sofiene Hannachi, Romain Noblemaire, Elisabeth Somody, Xavier Copie, Gilles Lascault, Olivier Paziaud, Olivier Piot, Olivier Billon, Claude Gully, Georges Haddad, Damien Lipp, Driss Mouhoub, Paul Bru, Cécile Duplantier-Duchêne, Antoine Milhem, Julien Bertrand, Michel Boursier, Khalifé Khalife, Noura Zannad, Aude Zanutto, Estelle Cuvelier, Cécile Donfafk, Pierre Graux, Aurélie Guiot, Yves Guyomar, Sébastien Heuls, John Kallumannil, Marc Semichon, Benjamin Gal, Michel Lopez, Julien Pineau, Xavier Dreyfus, Laure Hammer, Luc Petit, Xavier Harle, Julien Laborderie, Jean-Paul Albenque, Serge Boveda, Nicolas Combes, Stéphane Combes, Christophe Goutner, Olivier Césari, Patrick Chenevez, Christophe Loose, Patrick Peycher, Cyril Durand, Alexis Durand-Dubief, Hervé Poty, Christine Alonso, Serge Cazeau, Caroline Grimard, Gael Jauvert, and Arnaud Lazarus
References
- 1.Effect of metoprolol CR/XL in chronic heart failure: Metoprolol CR/XL Randomised Intervention Trial in Congestive Heart Failure (MERIT-HF). Lancet 1999;353:2001–2007. [PubMed] [Google Scholar]
- 2.Bardy GH, Lee KL, Mark DB, Poole JE, Packer DL, Boineau R, Domanski M, Troutman C, Anderson J, Johnson G, McNulty SE, Clapp-Channing N, Davidson-Ray LD, Fraulo ES, Fishbein DP, Luceri RM, Ip JH, Sudden Cardiac Death in Heart Failure Trial I. Amiodarone or an implantable cardioverter-defibrillator for congestive heart failure. N Engl J Med 2005;352:225–237. [DOI] [PubMed] [Google Scholar]
- 3.Cleland JG, Daubert JC, Erdmann E, Freemantle N, Gras D, Kappenberger L, Tavazzi L, Cardiac Resynchronization-Heart Failure Study Investigators. The effect of cardiac resynchronization on morbidity and mortality in heart failure. N Engl J Med 2005;352:1539–1549. [DOI] [PubMed] [Google Scholar]
- 4.Linde C, Leclercq C, Rex S, Garrigue S, Lavergne T, Cazeau S, McKenna W, Fitzgerald M, Deharo JC, Alonso C, Walker S, Braunschweig F, Bailleul C, Daubert JC. Long-term benefits of biventricular pacing in congestive heart failure: results from the MUltisite STimulation in cardiomyopathy (MUSTIC) study. J Am Coll Cardiol 2002;40:111–118. [DOI] [PubMed] [Google Scholar]
- 5.Gold MR, Linde C, Abraham WT, Gardiwal A, Daubert JC. The impact of cardiac resynchronization therapy on the incidence of ventricular arrhythmias in mild heart failure. Heart Rhythm 2011;8:679–684. [DOI] [PubMed] [Google Scholar]
- 6.Bristow MR, Saxon LA, Boehmer J, Krueger S, Kass DA, De Marco T, Carson P, DiCarlo L, DeMets D, White BG, DeVries DW, Feldman AM, Comparison of Medical Therapy Pacing and Defibrillation in Heart Failure Investigators. Cardiac-resynchronization therapy with or without an implantable defibrillator in advanced chronic heart failure. N Engl J Med 2004;350:2140–2150. [DOI] [PubMed] [Google Scholar]
- 7.Moss AJ, Hall WJ, Cannom DS, Klein H, Brown MW, Daubert JP, Estes NA, III, Foster E, Greenberg H, Higgins SL, Pfeffer MA, Solomon SD, Wilber D, Zareba W, MADIT-CRT Trial Investigators. Cardiac-resynchronization therapy for the prevention of heart-failure events. N Engl J Med 2009;361:1329–1338. [DOI] [PubMed] [Google Scholar]
- 8.Daubert JC, Donal E, Linde C. A plea for the wider use of CRT-P in candidates for cardiac resynchronisation therapy. Heart Fail Rev 2012;17:767–775. [DOI] [PubMed] [Google Scholar]
- 9.Linde C, Gold MR, Abraham WT, St John Sutton M, Ghio S, Cerkvenik J, Daubert C, REsynchronization reVErses Remodeling in Systolic left vEntricular dysfunction Study Group. Long-term impact of cardiac resynchronization therapy in mild heart failure: 5-year results from the REsynchronization reVErses Remodeling in Systolic left vEntricular dysfunction (REVERSE) study. Eur Heart J 2013;34:2592–2599. [DOI] [PubMed] [Google Scholar]
- 10.Aktas MK, Huang DT, Daubert JP, Schuger CD, McNitt S, Goldenberg I, Moss AJ, Zareba W. Effect of defibrillation threshold testing on heart failure hospitalization or death in the Multicenter Automatic Defibrillator Implantation Trial-Cardiac Resynchronization Therapy (MADIT-CRT). Heart Rhythm 2013;10:193–199. [DOI] [PubMed] [Google Scholar]
- 11.Singh JP, Klein HU, Huang DT, Reek S, Kuniss M, Quesada A, Barsheshet A, Cannom D, Goldenberg I, McNitt S, Daubert JP, Zareba W, Moss AJ. Left ventricular lead position and clinical outcome in the multicenter automatic defibrillator implantation trial-cardiac resynchronization therapy (MADIT-CRT) trial. Circulation 2011;123:1159–1166. [DOI] [PubMed] [Google Scholar]
- 12.Tracy CM, Epstein AE, Darbar D, Dimarco JP, Dunbar SB, Estes NA, III, Ferguson TB, Jr, Hammill SC, Karasik PE, Link MS, Marine JE, Schoenfeld MH, Shanker AJ, Silka MJ, Stevenson LW, Stevenson WG, Varosy PD. 2012 ACCF/AHA/HRS focused update of the 2008 guidelines for device-based therapy of cardiac rhythm abnormalities: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2012;60:1297–1313. [DOI] [PubMed] [Google Scholar]
- 13.Brignole M, Auricchio A, Baron-Esquivias G, Bordachar P, Boriani G, Breithardt OA, Cleland J, Deharo JC, Delgado V, Elliott PM, Gorenek B, Israel CW, Leclercq C, Linde C, Mont L, Padeletti L, Sutton R, Vardas PE, Guidelines ESCCfP, Zamorano JL, Achenbach S, Baumgartner H, Bax JJ, Bueno H, Dean V, Deaton C, Erol C, Fagard R, Ferrari R, Hasdai D, Hoes AW, Kirchhof P, Knuuti J, Kolh P, Lancellotti P, Linhart A, Nihoyannopoulos P, Piepoli MF, Ponikowski P, Sirnes PA, Tamargo JL, Tendera M, Torbicki A, Wijns W, Windecker S, Document R, Kirchhof P, Blomstrom-Lundqvist C, Badano LP, Aliyev F, Bansch D, Baumgartner H, Bsata W, Buser P, Charron P, Daubert JC, Dobreanu D, Faerestrand S, Hasdai D, Hoes AW, Le Heuzey JY, Mavrakis H, McDonagh T, Merino JL, Nawar MM, Nielsen JC, Pieske B, Poposka L, Ruschitzka F, Tendera M, Van Gelder IC, Wilson CM. 2013 ESC Guidelines on cardiac pacing and cardiac resynchronization therapy: the Task Force on cardiac pacing and resynchronization therapy of the European Society of Cardiology (ESC). Developed in collaboration with the European Heart Rhythm Association (EHRA). Eur Heart J 2013;34:2281–2329. [DOI] [PubMed] [Google Scholar]
- 14.Morani G, Gasparini M, Zanon F, Casali E, Spotti A, Reggiani A, Bertaglia E, Solimene F, Molon G, Accogli M, Tommasi C, Paoletti Perini A, Ciardiello C, Padeletti L. Cardiac resynchronization therapy-defibrillator improves long-term survival compared with cardiac resynchronization therapy-pacemaker in patients with a class IA indication for cardiac resynchronization therapy: data from the Contak Italian Registry. Europace 2013;15:1273–1279. [DOI] [PubMed] [Google Scholar]
- 15.Looi KL, Gajendragadkar PR, Khan FZ, Elsik M, Begley DA, Fynn SP, Grace AA, Heck PM, Virdee M, Agarwal S. Cardiac resynchronisation therapy: pacemaker versus internal cardioverter-defibrillator in patients with impaired left ventricular function. Heart 2014;100:794–799. [DOI] [PubMed] [Google Scholar]
- 16.Curtis AB, Yancy CW, Albert NM, Stough WG, Gheorghiade M, Heywood JT, McBride ML, Mehra MR, Oconnor CM, Reynolds D, Walsh MN, Fonarow GC. Cardiac resynchronization therapy utilization for heart failure: findings from IMPROVE HF. Am Heart J 2009;158:956–964. [DOI] [PubMed] [Google Scholar]
- 17.Swedberg K, Cleland J, Cowie MR, Nieminen M, Priori SG, Tavazzi L, van Veldhuisen DJ, Alonso-Pulpon L, Camm J, Dickstein K, Drexler H, Filippatos G, Linde C, Lopez-Sendon J, Santini M, Zannad F. Successful treatment of heart failure with devices requires collaboration. Eur J Heart Fail 2008;10:1229–1235. [DOI] [PubMed] [Google Scholar]
- 18.Boriani G, Mantovani LG, Biffi M, Schalij MJ, Martignani C, Leclercq C, Bax JJ, Auricchio A. Cardiac resynchronization therapy: a cost or an investment? Europace 2011;13(Suppl 2):ii32–ii38. [DOI] [PubMed] [Google Scholar]
- 19.Kutyifa V, Geller L, Bogyi P, Zima E, Aktas MK, Ozcan EE, Becker D, Nagy VK, Kosztin A, Szilagyi S, Merkely B. Effect of cardiac resynchronization therapy with implantable cardioverter defibrillator versus cardiac resynchronization therapy with pacemaker on mortality in heart failure patients: results of a high-volume, single-centre experience. Eur J Heart Fail 2014;16:1323–1330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cleland JG, Keshavarzi F, Pellicori P, Dicken B. Case selection for cardiac resynchronization in atrial fibrillation. Heart Fail Clinics 2013;9:461–474. [DOI] [PubMed] [Google Scholar]
- 21.von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ 2007;335:806–808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fine JP, Gray RJ. A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc 1999;94:496–509. [Google Scholar]
- 23.Bogale N, Priori S, Gitt A, Alings M, Linde C, Dickstein K, Scientific Committee, National Coordinators, and Investigators. The European cardiac resynchronization therapy survey: patient selection and implantation practice vary according to centre volume. Europace 2011;13:1445–1453. [DOI] [PubMed] [Google Scholar]
- 24.Yao G, Freemantle N, Calvert MJ, Bryan S, Daubert JC, Cleland JG. The long-term cost-effectiveness of cardiac resynchronization therapy with or without an implantable cardioverter-defibrillator. Eur Heart J 2007;28:42–51. [DOI] [PubMed] [Google Scholar]
- 25.Schuchert A, Muto C, Maounis T, Frank R, Boulogne E, Polauck A, Padeletti L, MASCOT study group. Lead complications, device infections, and clinical outcomes in the first year after implantation of cardiac resynchronization therapy-defibrillator and cardiac resynchronization therapy-pacemaker. Europace 2013;15:71–76. [DOI] [PubMed] [Google Scholar]
- 26.Dickstein K, Normand C, Anker SD, Auricchio A, Lundqvist CB, Bogale N, Cleland J, Filippatos G, Gasparini M, Gitt A, Hindricks G, Kuck KH, Ponikowski P, Stellbrink C, Ruschitzka F, Linde C. European Cardiac Resynchronization Therapy Survey II: rationale and design. Europace 2015;17:137–141. [DOI] [PubMed] [Google Scholar]
- 27.Bai R, Di Biase L, Elayi C, Ching CK, Barrett C, Philipps K, Lim P, Patel D, Callahan T, Martin DO, Arruda M, Schweikert RA, Saliba WI, Wilkoff B, Natale A. Mortality of heart failure patients after cardiac resynchronization therapy: identification of predictors. J Cardiovasc Electrophysiol 2008;19:1259–1265. [DOI] [PubMed] [Google Scholar]
- 28.Lam SK, Tse HF, Lau CP. CRT begets CRT-D: is one better than the other? J Cardiovasc Electrophysiol 2008;19:1266–1269. [DOI] [PubMed] [Google Scholar]
- 29.Lam SK, Owen A. Combined resynchronisation and implantable defibrillator therapy in left ventricular dysfunction: Bayesian network meta-analysis of randomised controlled trials. BMJ 2007;335:925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cleland JG, Daubert JC, Erdmann E, Freemantle N, Gras D, Kappenberger L, Tavazzi L. Longer-term effects of cardiac resynchronization therapy on mortality in heart failure [the CArdiac REsynchronization-Heart Failure (CARE-HF) trial extension phase]. Eur Heart J 2006;27:1928–1932. [DOI] [PubMed] [Google Scholar]
- 31.Uretsky BF, Thygesen K, Daubert JC, Erdmann E, Freemantle N, Gras D, Kappenberger L, Tavazzi L, Cleland JG. Predictors of mortality from pump failure and sudden cardiac death in patients with systolic heart failure and left ventricular dyssynchrony: results of the CARE-HF trial. J Cardiac Fail 2008;14:670–675. [DOI] [PubMed] [Google Scholar]
- 32.Ruwald MH, Solomon SD, Foster E, Kutyifa V, Ruwald AC, Sherazi S, McNitt S, Jons C, Moss AJ, Zareba W. Left ventricular ejection fraction normalization in cardiac resynchronization therapy and risk of ventricular arrhythmias and clinical outcomes: results from the Multicenter Automatic Defibrillator Implantation Trial with Cardiac Resynchronization Therapy (MADIT-CRT) trial. Circulation 2014;130:2278–2286. [DOI] [PubMed] [Google Scholar]
- 33.Sebag FA, Lellouche N, Chen Z, Tritar A, O'Neill MD, Gill J, Wright M, Leclercq C, Rinaldi CA. Positive response to cardiac resynchronization therapy reduces arrhythmic events after elective generator change in patients with primary prevention CRT-D. J Cardiovasc Electrophysiol 2014;25:1368–1375. [DOI] [PubMed] [Google Scholar]
- 34.Zecchin M, Proclemer A, Magnani S, Vitali-Serdoz L, Facchin D, Muser D, Nordio A, Barbati G, Puggia I, Sinagra G, Proclemer A. Long-term outcome of ‘super-responder’ patients to cardiac resynchronization therapy. Europace 2014;16:363–371. [DOI] [PubMed] [Google Scholar]
- 35.Castellant P, Fatemi M, Orhan E, Etienne Y, Blanc JJ. Patients with non-ischaemic dilated cardiomyopathy and hyper-responders to cardiac resynchronization therapy: characteristics and long-term evolution. Europace 2009;11:350–355. [DOI] [PubMed] [Google Scholar]
- 36.Gasparini M, Muto C, Iacopino S, Zanon F, Dicandia C, Distefano G, Favale S, Peraldo Neja C, Bragato R, Davinelli M, Mangoni L, Denaro A. Low-dose dobutamine test associated with interventricular dyssynchrony: a useful tool to identify cardiac resynchronization therapy responders: data from the LOw dose DObutamine stress-echo test in Cardiac Resynchronization Therapy (LODO-CRT) phase 2 study. Am Heart J 2012;163:422–429. [DOI] [PubMed] [Google Scholar]
- 37.Yanagisawa S, Inden Y, Shimano M, Yoshida N, Fujita M, Ohguchi S, Ishikawa S, Kato H, Okumura S, Miyoshi A, Nagao T, Yamamoto T, Hirai M, Murohara T. Clinical characteristics and predictors of super-response to cardiac resynchronization therapy: a combination of predictive factors. PACE 2014;37:1553–1564. [DOI] [PubMed] [Google Scholar]
- 38.Guerra JM, Wu J, Miller JM, Groh WJ. Increase in ventricular tachycardia frequency after biventricular implantable cardioverter defibrillator upgrade. J Cardiovasc Electrophysiol 2003;14:1245–1247. [DOI] [PubMed] [Google Scholar]
- 39.Di Cori A, Bongiorni MG, Arena G, Soldati E, Giannola G, Zucchelli G, Balbarini A. New-onset ventricular tachycardia after cardiac resynchronization therapy. J Interv Card Electrophysiol 2005;12:231–235. [DOI] [PubMed] [Google Scholar]
- 40.Boveda S, Marijon E, Jacob S, Defaye P, Winter JB, Bulava A, Gras D, Albenque JP, Combes N, Pavin D, Delarche N, Teubl A, Lambiez M, Chevalier P, Mona Lisa Study Group. Incidence and prognostic significance of sustained ventricular tachycardias in heart failure patients implanted with biventricular pacemakers without a back-up defibrillator: results from the prospective, multicentre, Mona Lisa cohort study. Eur Heart J 2009;30:1237–1244. [DOI] [PubMed] [Google Scholar]