Abstract
PURPOSE
There is a paucity of scalable advance care planning strategies that achieve the diverse goals of patients, families, and clinicians. We convened key stakeholders to gain their perspectives on developing a web-based advance care planning tool for lung disease.
MATERIALS AND METHODS
We conducted semi-structured interviews with 50 stakeholders: 21 patients with lung disease, 18 surrogates, and 11 clinicians. Interviews explored stakeholders’ desired content and design features of a web-based advance care planning tool. Participants also rated the tool’s acceptability and potential usefulness. We analyzed the interviews with modified grounded theory and validated themes though member checking.
RESULTS
Stakeholders highly rated the acceptability (median 5, IQR 5 to 5) and potential usefulness (median 5, IQR 4 to 5) of a web-based tool. Interviewees offered several suggestions: (1) use videos of medical scenarios and patient narratives rather than text; (2) include interactive content; and (3) allow the user control over how much they complete in one sitting. Participants identified challenges and potential solutions, such as how to manage the emotional difficulty of thinking about death and accommodate low computer literacy users.
CONCLUSIONS
There is strong stakeholder support for the development of a web-based advance care planning tool for lung disease.
Key words for indexing: Communication, Decision making, Public health, End of life care
Introduction
The Institute of Medicine recently stressed the need for advance care planning to promote patient centered care at the end of life. [1] They noted that this need is likely to increase as the population ages and acquires more serious, life limiting illnesses.
Although there are existing tools for advance care planning, [2] they are not sufficiently scalable to meet the growing public health demand nor do they accommodate the diverse needs of patients, families, and clinicians. For example, while traditional written advance directives are widely available, completion rates are low and the narrow approach to documenting treatment preferences may not help patients clarify their end-of-life goals or families prepare for the surrogate role. [3] In contrast, a recent randomized controlled trial found that facilitated advance care planning- where trained facilitators help patients reflect on their goals and values, document their preferences, and communicate with their families- is beneficial. [4] However, this approach requires the hiring, training, and maintenance of facilitators to perform multiple in-person counseling sessions. Given fiscal scarcity and the resource intense nature of this method, it would be hard to scale up to meet population demands.
A web-based approach to advance care planning is one promising strategy to develop a scalable tool that achieves diverse goals. Once developed, web-based tools are easily disseminated, and can be far more accessible to low literacy populations than written materials by incorporating video and narration in place of text. Precedence exists for using web-based tools to enhance aspects of medical practice that traditionally were managed through in-person encounters, such as web-based cognitive behavioral therapy for depression. [5]
A crucial and often overlooked aspect of web-based tool development is early stakeholder engagement. Doing so allows users, such as patients, clinicians and families, the opportunity to voice what they need from the tool so that developers can accommodate those needs. This approach has been shown to be a crucial aspect of developing new tools that impact outcomes important to patients and families. [6] Working closely with users beginning in early development has been shown to increase users’ participation compared with less user-friendly websites. [7]
We therefore conducted a study to explore the perspectives of patients with advanced lung disease, their surrogates and clinicians on the content and design development of a web-based advance care planning tool. We chose to focus on advanced lung disease as a model population in which to study advance care planning for the following reasons. Respiratory insufficiency frequently worsens to a point that decisions arise about the need for prolonged mechanical ventilation; [8–10] patients vary in their preferences about initiation and continuation of mechanical ventilation; [11,12] and deterioration is often sudden and patients are unable to participate in ongoing treatment decisions, necessitating surrogate decision makers involvement about whether to initiate or continue mechanical ventilation.
Methods
We conducted semi-structured interviews with 21 patients with advanced lung disease, 18 surrogate decision makers, and 11 clinicians from the pulmonary and primary care clinics and pulmonary rehabilitation at the University of Pittsburgh Medical Center between August and October 2014. We chose these stakeholders because any tool will need to meet their different advance care planning needs. We chose semi-structured interviews to produce reliable, comparable qualitative data and to allow the interviewer to follow relevant topics as they arose organically. [13] We continued participant enrollment and interviews until thematic saturation was reached.
Participants and Enrollment
Patients met inclusion criteria if they were at least 18 years old, able to give full informed consent, and able to understand English without the help of an interpreter, and if they had lung disease that requires supplemental oxygen. We chose supplemental oxygen requirement as a marker for advanced lung disease because it is associated with a poor prognosis, [14] has been shown to predict mortality [15] and is associated with adverse outcomes such as the need for mechanical ventilation in acute exacerbations. [16] Surrogate decision makers were identified by the patient as someone who would make medical decisions for them should they become incapacitated. Surrogates met inclusion criteria if they were 18 years or older, able to give informed consent, and able to understand English without the help of an interpreter. We performed purposeful sampling of participants to create a sample that is diverse in terms of race, gender and pulmonary pathophysiology. We recruited a convenience sample of pulmonary and critical care physicians, nurses, and primary care providers all from an academic hospital setting who self-identify as regularly caring for patients with advanced lung disease.
Study coordinators identified eligible patients by screening daily in the clinics and pulmonary rehabilitation. Prior to approaching potential participants, the study coordinator obtained permission from their clinic physician or respiratory therapist. All participants provided written informed consent prior to the initiation of any research procedures. Participants did not receive any compensation. The University of Pittsburgh institutional review board approved all study procedures.
Study Procedures
A researcher conducted the interviews in a private room. We took the following measures to minimize the interviewer from leading interviewees to specific responses: First, the interviewer received training in semi-structured interviewing techniques. Second, the multidisciplinary research team created and iteratively refined the interview script to be open-ended and minimize leading questions. Third, the interviewer completed several mock interviews with an experienced qualitative researcher who is not part of the study team. Finally, when the interview was coded by a member of the research team other than the interviewer instances of leading of interviewees were identified
Interviews were first conducted with patients and surrogates. Once thematic saturation was achieved with patients and surrogates, the themes from those interviews were taken to the clinicians for a more focused semi-structured interview. The clinician interviews focused on the main content and design themes brought up by patients and families in order to assess clinicians’ acceptability of these themes and to allow them an opportunity to elaborate. Clinician enrollment also continued until thematic saturation was reached.
To create the interview guide, we identified interview topics by reviewing existing literature on advance care planning for lung disease, [17,18] user-centered design, [19,20] and decision-support tools. [21,22] The interview guide began with open-ended questions about participants’ general advance care planning needs. Subsequent questions elicited specific feedback about how these needs could be accommodated in a web-based, interactive advance care planning tool. Specific topics that arose organically throughout the interviews were expanded upon through iterative revision of the interview guide in order to explore emerging themes. The main interview questions asked of patients, surrogates, and clinicians are contained in the Supplemental Table. Themes that arose in the interviews are outlined in detail in Table 2. The average interview length was 42 minutes.
Table 2.
Framework of needs expressed by stakeholders with exemplars
| Theme | Exemplars | Total N (%) | ||
|---|---|---|---|---|
| Patients (%) | Surrogates (%) | Clinicians (%) | ||
| General Advance Care Planning Needs | ||||
| Learning about future health states | Patient: “I think they’d have to see what it’s like to be in that situation, and this is what you’re going to have to deal with. And maybe you don’t want to do that, you know, this is your other option.” | 48 (96) | ||
| 19 (91) | 18 (100) | 11 (100) | ||
| Clarifying values | Clinician: “I’d like to know what things are most important to them and in particular, are there any things that they think the loss of them would be so great that the burdens or medical treatment wouldn’t be worth it.” | 47 (94) | ||
| 20 (95) | 18 (100) | 9 (82) | ||
| Communicating with family and clinician | Surrogate: “That would be good especially if the patient and a caregiver were watching together. Because as the patient was looking at what’s going to happen… then they can share those thoughts. The caregiver could say, ‘What do you want me to do? What’s your feeling about this?’” | 43 (86) | ||
| 19 (91) | 17 (94) | 7 (64) | ||
| Remembering past experiences | Surrogate: “Because it was hard watching my mom just for 11 years, just lay in the bed. So, I know he [my husband] doesn’t want that.” | 34 (68) | ||
| 18 (86) | 15 (83) | 1 (9) | ||
| Acknowledging uncertainty | Clinician: “This is a population of patients that have a real decline-unpredictable. Some of them it’s two years, some of them it’s ten years. But that’s been a very important part of how I prepare them for what is likely to be.” | 28 (56) | ||
| 10 (47) | 14 (78) | 4 (36) | ||
| Learning about principles of surrogate decision making | Surrogate: “I have to talk to him about it and we have to really know exactly what we want to do or what he wants to do. But I will honor his wishes even though it may be against my own.” | 23 (46) | ||
| 11 (52) | 9 (50) | 3 (27) | ||
| Desired Features in an Advance Care Planning Tool | ||||
| Watching videos about likely future health states | Patient: “it would give you a mindset of what could happen to you. If you actually see it, you have time to dwell on it and work it in your mind and be comfortable with it. I’d rather see a video, see what the possibilities are.” | 45 (90) | ||
| 19 (91) | 18 (100) | 8 (73) | ||
| Watching video testimonials | Clinician: “I think having testimonials of what the experience is like, and both good and bad, would be tremendously helpful, because fear of the unknown is probably one of the greatest fears.” | 41 (82) | ||
| 15 (71) | 16 (89) | 10 (91) | ||
| Interacting with the tool | Patient: “it would give me a chance to change scenarios and say, what would happen if I do this, the outcome might be this. It gives you an opportunity to play with the results and give you a different outcome. Yeah, I like that. In fact, I love it.” | 35 (70) | ||
| 16 (76) | 14 (76) | 5 (46) | ||
| Controlling the tool | Patient: “I would want to be able to control it. So that if I got tired [I’d] be able to turn it off and go back to it.” | 28 (56) | ||
| 17 (81) | 11 (61) | 0 | ||
| Completing the tool at home on their own time | Surrogate: “I think it’d be good to do it at home. In their own time, and own comfortable place.” | 23 (46) | ||
| 9 (43) | 8 (44) | 6 (54) | ||
| Completing documentation | Clinician: “I’d love to see the program give you a summary of your choices, [then] let’s schedule a meeting a month from now and we’ll go over it. That’s perfect, that’s perfect.” | 13 (26) | ||
| 3 (14) | 1 (6) | 9 (82) | ||
After each interview, the participant filled out a two-part questionnaire. This questionnaire was adapted by the research team from existing framework to assess the acceptability of decision support tools [23] and did not undergo psychometric testing. The first part assessed the potential usefulness and acceptability of such an advance care planning tool on a 1–5 Likert scale. All stakeholders completed this first questionnaire. The second part of the questionnaire asked the patients and surrogates to rate how potentially helpful specific design features could be on a 1–5 Likert scale. Clinicians did not rate specific design features. We asked participants to rate the design features that emerged organically during the interviews. For design features that came up in later interviews, a researcher called earlier interview participants to obtain their rating over the phone. We elicited participants’ ratings of potential design and content features of the tool to assess buy-in for the creation of the tool as a whole as well as the importance of specific elements. This initial needs assessment is crucial before expending resources on tool development. All questionnaires are included in the online supplementary material.
Analysis
Interviews were audio-recorded and transcribed verbatim. A multidisciplinary team that included researchers from pulmonary and critical care (JC), public health (NCE), and anthropology (KR) reviewed transcripts and used the modified grounded theory approach as described by Crabtree and Miller [24] to analyze the semi-structured interviews. This method is well suited for the practical application of qualitative data in a medical setting. We constructed a codebook through an iterative process using constant comparisons. [25] We began analysis shortly after the first interviews were completed. We iteratively refined the codebook during line-by-line coding of 5 transcripts to develop a final coding framework. We reached thematic saturation where all new data could be easily assigned to existing themes. We validated themes by performing member checking with 20% of participants.
Two coders (JC and NCE) applied the coding framework to all transcripts. All disagreements between coders were reviewed in multi-disciplinary team meetings and consensus was achieved. Coders had good inter-rater reliability with an overall Kappa statistic of 0.95. We used ATLAS.ti software (Berlin, Germany) for qualitative data management.
Because Likert scales are not normally distributed, we analyzed the survey data using medians and interquartile ranges.
Results
The overall enrollment rate was 93% (50/54). Among 25 eligible patients, 4 declined to participate. Three surrogates declined to participate after the patient had already completed the interview (18/21). All clinicians who were asked to participate did so.
Characteristics of Study Participants
Table 1 summarizes the demographic characteristics of the 21 patients, 18 surrogates, and 11 clinicians (n =50). The patients and surrogates were diverse in terms of gender, race, and education level. At the time of enrollment, patients had a median FEV1 of 1.14 liters, mean DLCO 37% predicted, and median supplemental oxygen requirement of 5 liters at rest. The clinicians included primary care physicians, pulmonary specialists, and nurses with a range of experience from 10–36 years in practice.
Table 1.
Demographics of Stakeholders (n=50)
| Patients (n=21) | Surrogates (n=18) | Clinicians (n=11) | |
|---|---|---|---|
| Mean Age (range) | 62 (45–80) | 50 (25–69) | 50 (43–59) |
| Female (%) | 13 (62) | 12 (67) | 5 (45) |
| African American (%) | 4 (19) | 4 (22) | 1 (9) |
| High school education or less (%) | 8 (38) | 4 (22) | |
| Pulmonary disease | |||
| COPD (%) | 12 (57) | ||
| IPF (%) | 4 (19) | ||
| PAH (%) | 2 (10) | ||
| Scleroderma (%) | 2 (10) | ||
| Sarcoidosis (%) | 1 (4) | ||
| Median supplemental oxygen in liters (interquartile range) | 5 (4–8) | ||
| Median FEV1 in liters (interquartile range) | 1.14 (0.82–1.37) | ||
| Mean DLCO (% predicted) | 37 | ||
| Clinician Specialty | |||
| PACCM (%) | 6 (55) | ||
| Nursing (%) | 3 (27) | ||
| Primary Care (%) | 2 (18) | ||
| Average Years in Practice (range) | 23 (10–36) |
Ratings of Acceptability and Potential Usefulness of the Tool
Stakeholders highly rated the acceptability of a web-based advance care planning tool (median 5, IQR 5 to 5) and its potential usefulness (median 5, IQR 4 to 5). Figure 1 shows the ratings of the tool’s potential usefulness and acceptability stratified by stakeholder group. Patients and surrogates liked the ability to complete the tool at home or with their loved ones. When participants were asked why they gave the rating they did, one surrogate’s response was typical: “I think it’s a great idea, just to help the family, and the patient, get on the same page, so that if something happens they’re not running around completely clueless as what to do.”
Figure 1.
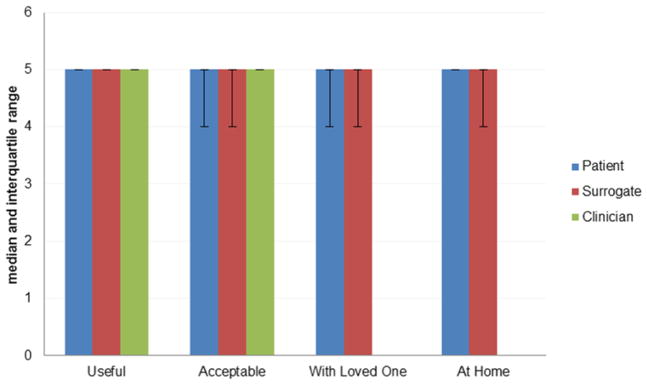
Patient, surrogate, and clinician ratings of potential usefulness and acceptability
Stakeholder Perspectives on Advance Care Planning Needs and the Design of a Tool
Table 2 contains the main themes that arose in the interviews. Patients and surrogates wanted to advance care planning to help them learn about future health states (91% and 100%, respectively), clarify values (95% and 100%), and communicate with their clinician (91% and 94%). They wanted the advance care planning tool to allow them to watch videos about likely future health states (91% and 100%) and watch testimonials of other patients and families (71% and 89%). Clinicians most frequently talked about creating useful and accessible documentation (82%); this was discussed less by patients and surrogates (14% and 6%, respectively).
Stakeholders Discuss Perceived Barriers and Potential Solutions
Table 3 contains the perceived barriers to using an online advance care planning tool and potential solutions. The most frequent barrier mentioned by patients, surrogates, and clinicians is that the content may be scary and emotionally difficult (67%, 72%, and 91%, respectively). One patient voiced concerns that were typical: “You would have to be prepared for it to depress people. And you have to deal with their depression.”
Table 3.
Barriers and Proposed Solutions
| Barriers | Total N (%) | Proposed Solutions | ||
|---|---|---|---|---|
| Patients (%) | Surrogates (%) | Clinicians (%) | ||
| The tool may be scary and emotionally difficult. | 37 (74) | Frame the content in a positive way and allow the user to do as much or as little as they choose in one sitting. | ||
| 14 (67) | 13 (72) | 10 (91) | ||
| The tool may eliminate crucial, in- person advance care planning. | 18 (36) | Conceptualize the tool as a supplement to patient-family- clinician communication rather than a replacement. | ||
| 5 (24) | 5 (28) | 8 (73) | ||
| The tool may be difficult for elderly users with low computer literacy. | 20 (40) | Employ principles of user-centered design throughout development. | ||
| 8 (38) | 9 (50) | 3 (27) | ||
Participants offered several suggestions to overcome the potential barriers to an online advance care planning tool. Regarding the most frequent concern that the content may be emotionally difficult, one surrogate’s solution of controlling how much of the tool to complete in one sitting was typical: “You could pace it yourself, like if it like freaked you out, you could stop and then go back to it later.” Clinicians addressed this barrier by emphasizing that the content should be framed positively with a focus on helping patients achieve their goals: “I think to err on the side of optimism- establishing goals and expectations for your life and then achieving them.”
Patients and Surrogates Rate Potential Design Features for the Tool
Figure 2 shows the patients’ and surrogates’ median ratings with interquartile ranges of specific design features on a 1–5 Likert scale, with 1 being an unhelpful feature and 5 being a very helpful feature. Patients and surrogates both rated the same five features the highest: 1) videos illustrating possible future medical scenarios, 2) testimonials from other patients and families, 3) interacting with the tool, 4) providing a bulletin board of frequently asked questions, and 5) providing a question prompt list.
Figure 2.
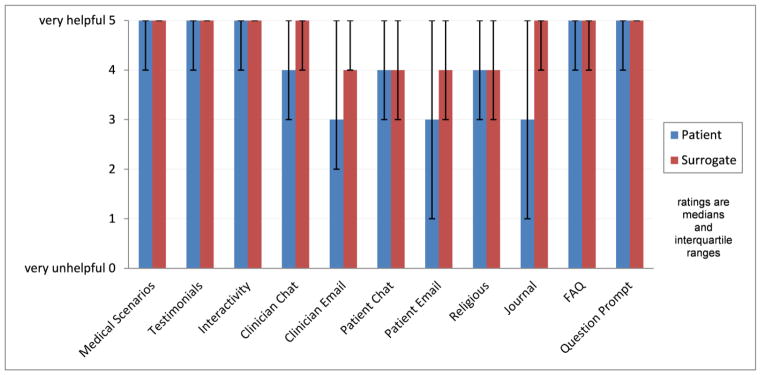
Patient and surrogate ratings of specific design and content features
When we asked why they rated viewing videos of future medical scenarios so highly, one patient’s response was typical: “I’d rather see something like this because then I get a mindset I can get comfortable with.” One surrogate summed up why she rated testimonials so highly: “Personally, had there been someone that looked like me, gone through the same, that I can actually relate [to], see the feelings, see their facial expressions, it would have changed a lot of things that I’ve done.”
Discussion
We found strong support among key stakeholders for a web-based advance care planning tool for lung disease. Participants offered important suggestions for tool development, including using videos of medical scenarios and patient narratives to minimize cognitive load. They also stressed the importance of allowing the user control over where and when they access the tool.
To our knowledge, this is the first attempt to prospectively engage patients, families, and clinicians in the process of creating a web-based advance care planning tool. Obtaining stakeholders’ perspectives revealed important insights about how to design a tool to meet all three users’ needs. For example, clinicians focused on accessible documentation of treatment preferences. Patients and families, on the other hand, said they are more concerned with documenting their loved one’s values and end of life goals. One potential way to accomplish these goals is to use the tool to link the patient’s values and goals with potential medical treatments. For example, if the patient indicates that living as long a life as possible is important to them, then treatment considerations may include tracheostomy and chronic mechanical ventilation. A successful tool will need to meet all users’ needs to ensure that values are elicited, shared and then influence clinical care. The importance of obtaining insights from end users is consistent with a large body of research in nonmedical web design that shows how user input is important for online tool design. [26–28] For example, a website about the state budget was created according to users’ wants and needs and the participants who used this site were significantly more likely to have positive attitudes toward civic engagement compared with those who saw a site not designed for usability. [7]
Our approach to advance care planning for lung disease has other advantages compared to prior approaches. First, participants’ suggestions offer clues on how to motivate and engage patients and families in advance care planning. For example, surrogates’ narratives can tell the story of how difficult it is to talk about their loved one getting sicker and how planning ahead made it easier to make the decisions their loved one would have wanted. Motivation has been shown to be a key factor in promoting health behavior change [29] and is an important part of any advance care planning intervention. [30] Second, existing decision aids for lung disease focus solely on patients’ decision about mechanical ventilation. [31,32] Our data indicate that users desire more from advance care planning. For example, families want education about the surrogate role and clinicians want the in-person encounter to be more efficient. Our approach is consistent with literature suggesting that focusing beyond treatment preferences may help better prepare patients and surrogates for the types of future decisions and conflicts they may encounter. [30] Third, we found that users desire an interactive experience to stay engaged. Compared with existing pen-and-paper tools, such as advance directives, a web-based approach can incorporate proven multimedia, interactive behavior change techniques. [33] For example, interactive values clarification exercises lead to better preparation and less regret compared with passive exercises. [34] Finally, we found that advanced lung disease patients and families desire some features tailored to the disease at hand, for example medical scenarios and narratives relevant to lung disease. Existing approaches aimed at all older adults have shown encouraging results [35] and leveraging disease specific content for those with serious illness may further help to match patient preferences with care received at the end-of-life. [36]
We are proposing a new decision support tool for advance care planning. The proposed tool is not a decision aid because it does not address a discrete decision and it does not include information about risk at the patient level. Rather, the goal is to support the process of advance care planning which includes preparing for future decision-making, clarifying values, and facilitating communication with health care providers. The proposed tool does meet several of the core quality criteria proposed by the International Patient Decision Aids Standards (IPDAS) Collaboration. [37] First, we used a systematic development process that involved several stakeholder groups. We will recruit members of these stakeholder groups to an expert advisory panel to help steer further development of the tool. Second, we used the stakeholders’ qualitative data to conceptualize components of the tool that fulfill many of the core dimensions of decision aids including providing information about options, clarifying values, using personal narratives, guiding communication between patients, families, and clinicians, and delivery of the tool online.
This study has limitations. First, though we recruited a broad sample of stakeholders, our participants are volunteers from a single region of the country, thus potentially limiting the generalizability of the results. Also, there may be other important needs that did not come out due to the population studied. For example, it is likely that the concern noted by our population about being able to access the tool anywhere would be even more prominent among a more rural population.
In conclusion, there is strong support among key stakeholders for the development of a web-based advance care planning tool for lung disease. Early collection of stakeholders’ perspectives revealed insights we would not have otherwise known and are crucial to developing a tool that will meet the diverse needs of patients, surrogates, and clinicians.
Supplementary Material
Highlights.
Current advance care planning strategies are either not scalable or do not meet the goals of patients, families, and clinicians.
We explored key stakeholders’ perspectives on developing a web-based advance care planning tool.
We conducted semi-structured interviews with patients with lung disease, their families and clinicians.
Stakeholders give high ratings of potential usefulness and acceptability of a web-based tool. We also uncovered key design features desired in such a tool and potential barriers to its use.
In conclusion, there is strong stakeholder support for the development of a web-based advance care planning tool.
Acknowledgments
Supported by: National Institutes of Health grants 2T32 HL007563-26, 5R01 AG045176-03, and KL2 TR000146; Dr. White was supported by a Greenwall Faculty Scholars Award in Bioethics
Footnotes
Sponsors had no role in the study design, in the collections, analysis and interpretations of data, in the writing of the manuscript, and in the decision to submit the manuscript for publication.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Dying in America: Improving Quality and Honoring Individual Preferences Near the End of Life. Institute of Medicine; 2014. [accessed November 21, 2014]. http://www.iom.edu/Reports/2014/Dying-In-America-Improving-Quality-and-Honoring-Individual-Preferences-Near-the-End-of-Life.aspx. [Google Scholar]
- 2.Butler M, Ratner E, McCreedy E, Shippee N, Kane RL. Decision Aids for Advance Care Planning: An Overview of the State of the Science. Ann Intern Med. 2014 doi: 10.7326/M14-0644. [DOI] [PubMed] [Google Scholar]
- 3.Fagerlin A, Schneider CE. Enough: The Failure of the Living Will. [accessed October 24, 2014];Hasings Cent Rep. 2004 34(2):30–42. http://www.thehastingscenter.org/pdf/publications/hcr_mar_apr_2004_enough.pdf. [PubMed] [Google Scholar]
- 4.Detering KM, Hancock AD, Reade MC, Silvester W. The impact of advance care planning on end of life care in elderly patients: randomised controlled trial. Br Med J. 2010;340:c1345. doi: 10.1136/bmj.c1345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kaltenthaler E, Papaioannou D, Boland A, Dickson R. The National Institute for Health and Clinical Excellence Single Technology Appraisal process: lessons from the first 4 years. Value Health. 2011;14:1158–65. doi: 10.1016/j.jval.2011.06.007. [DOI] [PubMed] [Google Scholar]
- 6.Carman KL, Dardess P, Maurer M, Sofaer S, Adams K, Bechtel C, et al. Patient and family engagement: A framework for understanding the elements and developing interventions and policies. Health Aff. 2013;32:223–31. doi: 10.1377/hlthaff.2012.1085. [DOI] [PubMed] [Google Scholar]
- 7.Coleman R, Lieber P, Mendelson AL, Kurpius DD. Public life and the internet: if you build a better website, will citizens become engaged? New Media Soc. 2008;10:179–201. doi: 10.1177/1461444807086474. [DOI] [Google Scholar]
- 8.Olson AL, Swigris JJ, Lezotte DC, Norris JM, Wilson CG, Brown KK. Mortality from pulmonary fibrosis increased in the United States from 1992 to 2003. Am J Respir Crit Care Med. 2007;176:277–84. doi: 10.1164/rccm.200701-044OC. [DOI] [PubMed] [Google Scholar]
- 9.Groenewegen KH, Schols AMWJ, Wouters EFM. Mortality and mortality-related factors after hospitalization for acute exacerbation of COPD. Chest. 2003;124:459–67. doi: 10.1378/chest.124.2.459. [DOI] [PubMed] [Google Scholar]
- 10.Claessens MT, Lynn J, Zhong Z, Desbiens NA, Phillips RS, Wu AW, et al. Dying with lung cancer or chronic obstructive pulmonary disease: insights from SUPPORT. Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatments. J Am Geriatr Soc. 1998;48:1242–50. doi: 10.1111/j.1532-5415.2000.tb03124.x. [DOI] [PubMed] [Google Scholar]
- 11.Fried TR, Bradley EH, Towle VR, Allore H. Understanding the treatment preferences of seriously ill patients. N Engl J Med. 2002;346:1061–6. doi: 10.1056/NEJMsa012528. [DOI] [PubMed] [Google Scholar]
- 12.Connors AF, Dawson NV, Thomas C, Harrell FE, Desbiens N, Fulkerson WJ, et al. Outcomes following acute exacerbation of severe chronic obstructive lung disease. The SUPPORT investigators (Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatments) Am J Respir Crit Care Med. 1996;154:959–67. doi: 10.1164/ajrccm.154.4.8887592. [DOI] [PubMed] [Google Scholar]
- 13.Sankar P, Jones NL. Semi-Structured Interviews in Bioethics Research. Adv Bioeth. 2007;11:117–36. doi: 10.1016/S1479-3709(07)11006-2. [DOI] [Google Scholar]
- 14.Kawakami Y, Terai T, Yamamoto H, Murao M. Exercise and oxygen inhalation in relation to prognosis of chronic obstructive pulmonary disease. Chest. 1982;81:182–8. doi: 10.1378/chest.81.2.182. [DOI] [PubMed] [Google Scholar]
- 15.Casanova C, Cote C, Marin JM, Pinto-Plata V, de Torres JP, Aguirre-Jaíme A, et al. Distance and oxygen desaturation during the 6-min walk test as predictors of long-term mortality in patients with COPD. Chest. 2008;134:746–52. doi: 10.1378/chest.08-0520. [DOI] [PubMed] [Google Scholar]
- 16.Matkovic Z, Huerta A, Soler N, Domingo R, Gabarrús A, Torres A, et al. Predictors of adverse outcome in patients hospitalised for exacerbation of chronic obstructive pulmonary disease. Respiration. 2012;84:17–26. doi: 10.1159/000335467. [DOI] [PubMed] [Google Scholar]
- 17.Patel K, Janssen DJ, Curtis JR. Advance care planning in COPD. [Review] Respirology. 2012;17:72–8. doi: 10.1111/j.1440-1843.2011.02087.x. [DOI] [PubMed] [Google Scholar]
- 18.Curtis JR, Engelberg RA, Nielsen EL, Au DH, Patrick DL. Patient-physician communication about end-of-life care for patients with severe COPD. Eur Respir J Off J Eur Soc Clin Respir Physiol. 2004;24:200–5. doi: 10.1183/09031936.04.00010104. [DOI] [PubMed] [Google Scholar]
- 19.De Vito Dabbs A, Myers Ba, Mc Curry KR, Dunbar-Jacob J, Hawkins RP, Begey A, et al. User-centered design and interactive health technologies for patients. Comput Inform Nurs. 2009;27:175–83. doi: 10.1097/NCN.0b013e31819f7c7c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Abras C, Maloney-Krichmar D, Preece J. User-centered design. Design. 2004;37:1–14. doi: 10.3233/WOR-2010-1109. [DOI] [Google Scholar]
- 21.Murray MA, Miller T, Fiset V, O’Connor A, Jacobsen MJ. Decision support: helping patients and families to find a balance at the end of life. Int J Palliat Nurs. 2004;10:270–7. doi: 10.12968/ijpn.2004.10.6.13268. [DOI] [PubMed] [Google Scholar]
- 22.Légaré F, O’Connor AC, Graham I, Saucier D, Côté L, Cauchon M, et al. Supporting patients facing difficult health care decisions: Use of the Ottawa Decision Support Framework. Can Fam Physician. 2006;52:476–7. [PMC free article] [PubMed] [Google Scholar]
- 23.O’Connor A CA. User Manual-Accpetpability. [accessed October 8, 2014];Doc Online. 2012 http://decisionaid.ohri.ca/docs/develop/User_Manuals/UM_Acceptability.pdf.
- 24.Crabtree B, Miller W. Review: Benjamin Crabtree & William Miller (Eds.) (1999). Doing Qualitative Research (2nd edition) Rev Lit Arts Am. 2002;3:406. [Google Scholar]
- 25.Ellis C, Strauss A, Corbin J. Basics of Qualitative Research: Grounded Theory Procedures and Techniques. Contemp Sociol. 1992;21:138. doi: 10.2307/2074814. [DOI] [Google Scholar]
- 26.Hinchliffe A, Mummery WK. Applying usability testing techniques to improve a health promotion website. Heal Promot J Aust. 2008;19:29–35. doi: 10.1071/he08029. [DOI] [PubMed] [Google Scholar]
- 27.Sørum H, Andersen KN, Vatrapu R. Public websites and human–computer interaction: an empirical study of measurement of website quality and user satisfaction. Behav Inf Technol. 2012;31:697–706. doi: 10.1080/0144929X.2011.577191. [DOI] [Google Scholar]
- 28.Norman DA, Draper SW. User Centered System Design; New Perspectives on Human-Computer Interaction. 1986. [Google Scholar]
- 29.Fisher WA, Fisher JD, Harman J. The Information-Motivation-Behavioral Skills Model: A General Social Psychological Approach to Understanding and Promoting Health Behavior. Soc Psychol Found Heal Illn. 2009:82–106. doi: 10.1002/9780470753552.ch4. [DOI] [Google Scholar]
- 30.Sudore RL, Fried TR. Redefining the “planning” in advance care planning: preparing for end-of-life decision making. Ann Intern Med. 2010;153:256–61. doi: 10.1059/0003-4819-153-4-201008170-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wilson KG, Aaron SD, Vandemheen KL, Hebert PC, McKim DA, Fiset V, et al. Evaluation of a decision aid for making choices about intubation and mechanical ventilation in chronic obstructive pulmonary disease. Patient Educ Couns. 2005;57:88–95. doi: 10.1016/j.pec.2004.04.004. [DOI] [PubMed] [Google Scholar]
- 32.Dales RE, O’Connor A, Hebert P, Sullivan K, McKim D, Llewellyn-Thomas H. Intubation and mechanical ventilation for COPD: Development of an instrument to elicit patient preferences. Chest. 1999;116:792–800. doi: 10.1378/chest.116.3.792. [DOI] [PubMed] [Google Scholar]
- 33.Webb TL, Joseph J, Yardley L, Michie S. Using the internet to promote health behavior change: a systematic review and meta-analysis of the impact of theoretical basis, use of behavior change techniques, and mode of delivery on efficacy. J Med Internet Res. 2010;12:e4. doi: 10.2196/jmir.1376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Feldman-Stewart D, Tong C, Siemens R, Alibhai S, Pickles T, Robinson J, et al. The Impact of Explicit Values Clarification Exercises in a Patient Decision Aid Emerges After the Decision Is Actually Made: Evidence From a Randomized Controlled Trial. Med Decis Mak. 2012;32:616–26. doi: 10.1177/0272989X11434601. [DOI] [PubMed] [Google Scholar]
- 35.Sudore RL, Knight SJ, McMahan RD, Feuz M, Farrell D, Miao Y, et al. A novel website to prepare diverse older adults for decision making and advance care planning: A pilot study. J Pain Symptom Manage. 2014;47:674–86. doi: 10.1016/j.jpainsymman.2013.05.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kirchhoff KT, Hammes BJ, Kehl KA, Briggs LA, Brown RL. Effect of a disease-specific advance care planning intervention on end-of-life care. J Am Geriatr Soc. 2012;60:946–50. doi: 10.1111/j.1532-5415.2012.03917.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hoffman AS, Volk RJ, Saarimaki A, Stirling C, Li LC, Härter M, et al. Delivering patient decision aids on the Internet: definitions, theories, current evidence, and emerging research areas. BMC Med Inform Decis Mak. 2013;13 (Suppl 2):S13. doi: 10.1186/1472-6947-13-S2-S13. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


