Abstract
While herpes zoster infection has been recognized since antiquity, chickenpox (varicella) was confused with smallpox until the 1800s, when both illnesses became better understood. In the 20th century, varicella zoster virus (VZV) was shown to cause varicella upon primary (first-time) infection and herpes zoster (shingles) after reactivation of latent VZV. Scientific progress over the past 50 years has rapidly advanced the understanding and prevention of disease produced by VZV. Combined imaging and virological studies continue to reveal the protean neurological, ocular and visceral disorders produced by VZV.
Keywords: Varicella-zoster virus, Infection, Vaccination, Neurologic disease
1. Introduction
In the past few hundred years, one of the most exciting adventures in medical virology has been the identification of varicella zoster virus (VZV) as the cause of both chickenpox (varicella) and herpes zoster (shingles). Clinical descriptions of zoster actually date back to antiquity. In the 1800s, chickenpox began to be distinguished from smallpox. Early in the 20th century, the causative agent of herpes zoster was shown to reside in ganglia. Later, the virus causing varicella and zoster was shown to be the same. Molecular virology proved that VZV is latent in ganglionic neurons along the entire neuraxis. Clinical-pathological-virological correlations revealed that VZV reactivation causes not only zoster and chronic pain (postherpetic neuralgia), but also meningoencephalitis, myelitis, VZV vasculopathy (stroke) and multiple serious ocular disorders. Most recently, the spectrum of VZV vasculopathies was expanded to include giant cell arteritis. Other developments have been the creation of live attenuated VZV vaccines to prevent varicella and zoster, including a non-replicating subunit vaccine containing the VZV glycoprotein E to prevent zoster. This review highlights important studies in the history of VZV biology and points to future directions for VZV research.
2. Background and origins in language
The word “herpes” (ëρπης) derives from the Greek word meaning “to creep”. Hippocrates first used the word to describe an ulcerative skin lesion that appeared to “crawl” along the skin, thus encompassing both herpes simplex and herpes zoster. However, zoster most commonly presents as a strip of painful blisters on an erythematous base in a dermatomal distribution on one side of the body (Fig. 1), while herpes simplex virus (HSV) infections are typically patchy. The Roman encyclopedistCelsus (c. 25 BC – c. 50 AD) was the first to use the term “herpes zoster” to describe the rounded lesions that eventually spread in a serpentine fashion like a belt. Indeed, the word “zoster” derives from Greek and Latin for the word “belt” and was used to describe a metal belt “ornamented with studs about half an inch in diameter” and a leather strap reaching halfway around the body [1]. Because the name herpes zoster is so descriptive, it is likely that ancient physicians recognized the dermatomal distribution of disease. The word “shingles” derives from the medieval Latin word “cingulus” meaning “girdle”, referring to the characteristic skin lesions often around the waist.
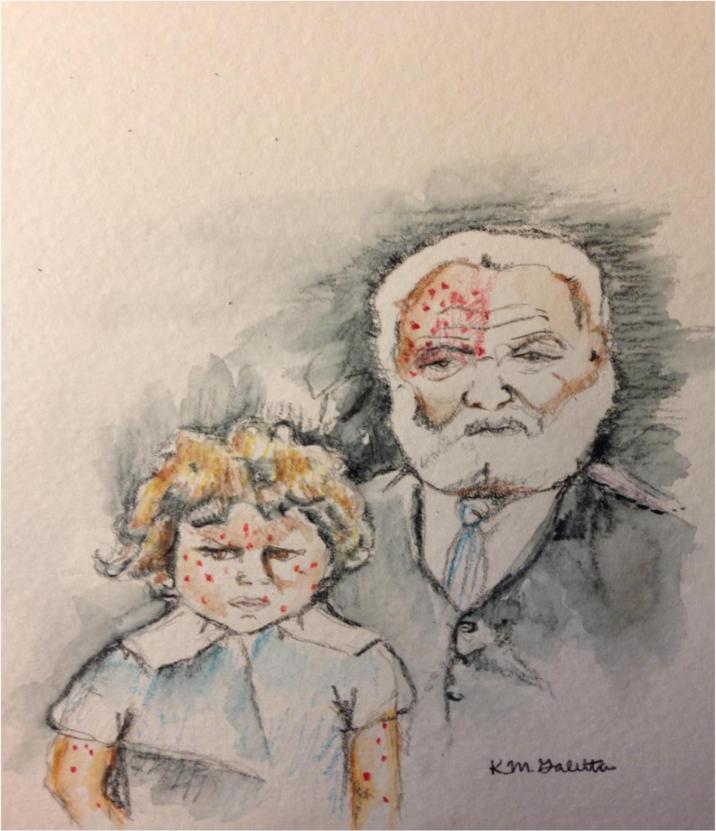
Fig. 1.
Girl with varicella and man with ophthalmologic-distribution herpes zoster. Drawing by Kristin Galetta, MD.
The lesions of varicella were first described by the Persian scientist Rhazes (865-925) and later by Giovanni Filipo (1510-1580) [2]. The name “chickenpox” was used by Richard Morton (1637-1698) who characterized it as a mild form of smallpox. The exact origin of the name “chickenpox” remains unclear. Samuel Johnson suggested that since the disease was “of no great danger,” it was a “chicken” form of smallpox. Other reasons given are that the scars remaining after chickenpox looked as though chickens had pecked at the skin. Furthermore, chickpea seeds are similar in size to the lesions, possibly contributing to the name. Finally, the term may have originated from corruption of the Old English word “giccin” which means “itching.” The term “pox” meant “curse” in medieval times, which is thought to have contributed to the name as well.
The exact origin of the term “varicella” is also uncertain. Vogel referred to chickenpox as varicella in 1765. Some authors suggested that “varicella” is the derivative of “varus”, the Latin word for “pimple” [3]. It is also possible that varicella comes from the diminutive form of the word variola, derived from the medieval Latin word for smallpox which means “speckled”.
3. Identification and initial work on virus localization
Both varicella and herpes zoster were investigated independently until their stories finally merged. Their histories are complicated by several factors, including the difficulty in interpreting medical literature describing skin conditions before the 16th century, inconsistent terminology, and use of data from earlier medical writers without proper citation. During the 18th and 19th centuries, there was an explosion of medical writings about both diseases, but with little overlap.
The fundamental challenge to understanding VZV was the ability to identify disease produced by it. William Heberden is credited with distinguishing the difference between smallpox and chickenpox. In his address to the College of Physicians in London in 1768, Heberden described the clinical distinction between the two disorders [4], underscoring the importance of recognizing that a history of chickenpox did not confer immunity to smallpox. While today it is understood that chickenpox, as compared to smallpox, has no or mild prodrome, and lesions at different stages of development and generally a more centripetal distribution, Heberden's insights regarding the distinction between smallpox and chickenpox were not accepted immediately.
During the 19th century, Richard Bright in his Reports of Medical Cases in 1831 first suggested that the nervous system was the source of herpes. In 1863, Von Barensprung further postulated that zoster originated in sensory ganglia based on correlations of the lesions of zoster with spinal nerves [5]. In the late 1800s, cases of individuals who died shortly after developing herpes zoster eruptions were found to have hemorrhagic ganglia with purulent infiltration [6], findings consistent with earlier claims that disease was likely initiated by damage in ganglia.
The late 1800s also saw great strides toward understanding varicella. In 1875, Steiner inoculated healthy volunteers with vesicular fluid from individuals with active varicella infection [7], thus demonstrating that chickenpox is caused by an infectious agent. In 1892, a case presentation by Osler emphasized that smallpox and chickenpox were not the same disease, and that infection with one did not provide immunity to the other, solidifying Herbeden's initial assessment that chickenpox and smallpox were unrelated. A few years later, Ernest Tyzzer developed a bedside test to distinguish smallpox from chickenpox based on the presence of multinucleated cells in varicella lesions that were not found in smallpox [8].
At the turn of the 20th century, clinical-pathologic studies further advanced the understanding of zoster. In the seminal neuropathological study by Head and Campbell [9], analysis of 400 clinical cases and precise clinico-pathological correlations from 15 autopsies allowed mapping of the sensory dermatomes. The cardinal pathological features of zoster consisting of acute interstitial inflammation and necrosis of ganglion cells were shown to be in the posterior root ganglion, although the causative agent was unknown. As elegantly pointed out by Kennedy [10], an important lesson of that study rests in the value of careful and precise clinical observations in providing key clues to disease pathogenesis, even before a causative agent has been identified.
4. Varicella and herpes zoster: the virus connection
Von Bókay, in 1892, first suggested a relationship between varicella and herpes zoster when he noted the occurrence of both disorders at the same time in homes of his patients. He recognized the similar appearance of the skin findings and hypothesized that the same virus produced the two, thus setting the stage for experimental analysis. Histopathological studies of varicella revealed large multinucleated cells with intranuclear inclusion bodies similar to those of zoster described by Tyzzer [11]. In 1923, de Lange claimed to have demonstrated antibodies to varicella in the blood of a patient suffering from zoster. One year later, Netter and Urbain studied blood from 100 patients with zoster who had no apparent contact with varicella subjects; 93 of the zoster patients had antibodies that reacted with antigen prepared from crusts of vesicles derived from patients with either varicella or zoster, and sera from varicella patients were later shown to react with similarly prepared varicella or zoster antigen [12]. Shortly thereafter, scientists and physicians began to more formally test the hypothesis that the two diseases were related. Lipschutz and Kundratitz (1925) and Bruusgaard (1932) inoculated humans with vesicular fluid from patients with herpes zoster and found that some subjects developed diffuse vesicular skin lesions clinically and microscopically identical to those in varicella [13].
Morphological studies of varicella and zoster were also conducted during this time by light and electron microscopy. Paschen described elementary bodies in smears of vesicles obtained from patients with varicella [14] and in vesicular fluid from patients with herpes zoster [15]. Amies showed that elementary bodies were agglutinated by serum of patients with either varicella or zoster [16]. Ruska, who invented the electron microscope, reported that the morphology of virus particles from patients with varicella or zoster was indistinguishable at an ultrastructural level [17]. Garland hypothesized that zoster (shingles) was due to reactivation of a latent varicella zoster virus [18]. In 1953, Weller propagated VZV in tissue culture and found that cytopathic effects, virion morphology and antigenic profiles were indistinguishable when cells were inoculated with lesion fluid from patients with varicella or zoster, resulting in the name “varicella zoster virus” [11].
Yet the association between zoster and varicella still required clarification. In his landmark presentation in 1965, Hope-Simpson [19] postulated that zoster was due to reactivation of latent virus and that viral latency was maintained by repeated exposure to exogenous virus, based on all cases of herpes zoster he encountered during 16 years in general practice and on evidence that zoster was unrelated to epidemics. He hypothesized that virus reactivated when antibody levels fell below a critical level [20], although it has since been shown that the presence of anti-VZV antibodies in sera from individuals age 60-94 years is variable [21], and that a declining cell-mediated immune response to VZV is more important in allowing VZV to reactivate. Overall, while primary VZV infection in childhood usually produces varicella, seronegative adults can develop varicella (often severe) when exposed to children with varicella or adults with zoster.
Proof of VZV latency in ganglia came from Gilden et al. [22], who showed that radiolabeled VZV DNA probes hybridized to DNA extracted from trigeminal ganglia, and from Hyman et al. [23], who found that radiolabeled VZV RNA hybridized in situ to trigeminal ganglionic neurons. Although there were some years of controversy regarding the site of VZV latency in ganglia, combined polymerase chain reaction (PCR), ISH, and PCR in situ amplification technologies with several gene probes confirmed that VZV resides predominantly in the nuclei of ganglionic neurons [24]. In 1984, Straus et al. [25] used restriction endonuclease analysis of VZV DNA from viruses isolated from an immunocompromised patient who had varicella and subsequently developed zoster, to show that reactivation was caused by the original infecting virus. The extent of viral gene expression in ganglia appears to be restricted. In human ganglia analyzed within 9 hours after death, only VZV gene transcripts are found [26] while additional transcripts can be detected in the first 24 hours.
In 1986, Davison and Scott determined the complete nucleotide sequence of the VZV genome (the Dumas strain), the first herpesvirus to be fully sequenced. Since then, sequencing of more than 30 VZV isolates has revealed the remarkable stability of the genome. Mutagenesis of the VZV genome using cosmids or bacterial artificial chromosome methods has permitted functional analyses of many VZV genes in recombinant viruses.
Further understanding of the pathogenesis of VZV infection has been difficult, mainly due to lack of a satisfactory animal model. Based on our current understanding of VZV latency in human ganglia, an animal model used to study varicella latency should fulfill the following criteria: (1) virus must be present exclusively in ganglionic neurons, (2) latent virus must reactivate, and (3) virus transcription must be restricted. These criteria have not been fulfilled by any small animal models. To date, the best animal model is simian varicella virus (SVV) infection of non-human primates, which shares clinical, pathological, immunological and virological features with human VZV infection. Primary SVV infection results in varicella, followed by the development of virus latency in ganglionic neurons; spontaneous virus reactivation produces zoster [27,28]. The SVV model has shown that after primary infection, hematogenous spread of virus leads to ganglionic infection before the onset of varicella rash [29]. In seronegative African green monkeys inoculated intratracheally with SVV, analyses reveal infection of alveolar myeloid cells and T cells in lungs and initial infection of central memory T cells and subsequent infection of effector memory T cells during viremia. At 9 days after infection, SVV is present in perivascular skin infiltrates consisting of macrophages, dendritic cells, dendrocytes and memory T cells; in ganglia, SVV is present primarily in neurons and occasionally in memory T cells adjacent to neurons, suggesting the role of memory T cells in dissemination.
As with latent VZV in human ganglia, transcription of SVV in latently infected monkey ganglia is limited. Experimental immunosuppression by X-irradiation and treatment with tacrolimus and prednisone of African green monkeys, rhesus monkeys and cynomolgus macaques latently infected with SVV produces both subclinical SVV reactivation as well as zoster [30]. T cell infiltration in ganglia with reactivated SVV in cynomolgus macaques correlates with expression of CXCL10 transcripts, but not with SVV proteins, suggesting that SVV-specific T cells do not control reactivation in ganglia.
5. History of prevention and vaccination for VZV disease
5.1. Varivax
Major clinical advances came from development of the live attenuated Oka varicella vaccine, making varicella and zoster the only vaccine-preventable human herpesvirus infection. In 1974, Takahashi and colleagues generated the first varicella vaccine, inspired by Takahashi's observations of a family member with severe chickenpox and fever, wherein he harvested the “Oka strain” of vaccine virus from a 3-year old boy and propagated it 11 times in human embryonic lung cells and in guinea pig embryo cells [31]. Initially, clinical trials with vaccine were conducted in healthy children found to have anti-VZV antibodies. Follow-up antibody studies of household contacts of immunized children showed that the vaccine was effective [32]. Numerous clinical trials throughout the United States and Japan demonstrated the long-term efficacy of VZV vaccine in healthy children and adults, including the elderly. In 1995, varicella vaccine became available in the United States. The CDC recommends immunization at 1 year of age, and a second dose at age 4-6. Contraindications to the vaccine include life-threatening allergy to previous administration, gelatin or neomycin, if an individual is pregnant, is severely ill and in some cases of immunosuppression. People with life-threatening allergic reactions to Among states that accurately reported the incidence of varicella, disease declined by 79% overall between 2000 and 2010, likely due to vaccine [33].
The creation of varicella immunoglobulin (VariZig) provided an alternative for individuals who were ineligible for vaccine to acquire immunity. In the early 1960s, Ross showed that although VariZig did not halt transmission, disease severity was reduced [34]. Later that decade, a small study showed that passive immunization with high-titer VariZig protected siblings exposed to varicella [35]. By 1976, the first commercial preparation of immune globulin from healthy volunteers with high VZV antibody titers became available in the US and was shown to improve outcomes in children if administered within 96 hours of exposure [36]. In 2013, the CDC issued updated recommendations for the use of VariZig.
5.2. Zostavax
Compared to varicella, zoster is far more serious and can be complicated by disabling disorders such as post-herpetic neuralgia (PHN) and crippling VZV myelitis, life-threatening VZV encephalitis and vasculopathy, as well as multiple serious ocular disorders. Thus in 1992, Zostavax, that boosted cell-mediated immunity to VZV, was developed [37]. Studies throughout the 1990s supported the effects of booster shots for the elderly. In 2005, the Shingles Prevention Study (SPS), a randomized placebo-controlled trial, provided evidence that the herpes zoster vaccine reduced the incidence of zoster and PHN in the elderly [38]. In that study, 38,546 healthy adults ≥60 years of age (median 69 years) were randomly assigned to receive a single dose of high-potency attenuated VZV with 14-fold higher potency than varicella vaccine or placebo. The higher-potency vaccine was required to increase VZV-specific cell-mediated immunity in latently infected older adults. The incidence of zoster as well as the burden of illness due to zoster (total pain and discomfort) and the incidence of PHN were determined. Average follow-up of 3.13 years in a total of 19,270 people who received zoster vaccine and 19,276 who received placebo revealed 957 confirmed cases of zoster (315 in vaccine recipients; 642 in placebo recipients). In both groups, >93% of the subjects with zoster were positive for wild-type VZV DNA by PCR; none had vOka DNA. Zoster vaccine reduced the incidence of zoster by 51.3% (63.9% in people aged 60-69 years, but only 37.6% in people aged ≥70 years). The burden of disease was reduced by 61.1% (65.5% in people aged 60-69 years and 55.4% in people age ≥70 years), and the duration of pain and discomfort among subjects with zoster was shorter in vaccinated candidates compared with placebo recipients. PHN was reduced by >65% for both age groups, with most benefit in the ≥70 years old age group. SPS also showed that vaccine reduced the adverse impact of zoster on patients’ capacity to perform activities of daily living and health-related quality-of-life.
Zoster vaccine is safe. Rates of serious adverse events, systemic adverse events, hospitalizations and deaths were low in vaccine recipients in the SPS and comparable to those in placebo recipients. During the first 42 days after vaccination, there were 24 cases of zoster in placebo recipients and 7 cases in the vaccination group, but none were caused by vOka. Unlike prophylactic vaccines such as those against varicella and measles, zoster vaccine is a therapeutic vaccine aimed at preventing reactivation of latent VZV in humans who have been infected before vaccination and already have substantial immunity.
The CDC recommends Zostavax for healthy adults age ≥60 years to prevent herpes zoster [39]. Post-licensure studies have confirmed the vaccine's safety and efficacy [40,41]. Unfortunately, participation in the zoster vaccine program has been low, likely due to cost and failure to recognize the importance of preventing infectious diseases in older adults. Zoster vaccine has now been shown to be safe and effective in healthy persons 50–59 years of age [42]. Thus, the FDA has approved its administration in healthy adults ≥50 years of age with contraindications in those with anaphylaxis to gelatin or neomycin, with immunosuppression, immunodeficiency or pregnancy. [43] The SPS demonstrated efficacy for 4 years after vaccination, while subsequent studies [44,45] indicated efficacy for the incidence of zoster for 8 years [46]. Currently, CDC does not recommend booster doses of zoster vaccine, but may in the future.
5.3. GSK vaccine (HZ/su)
A recent development in zoster prevention has been the creation of a liposome-based subunit vaccine (HZ/su) containing the VZV glycoprotein E and the adjuvant ASO1B. Studies revealed that 2 doses of HZ/su containing 50 μg of recombinant VZV glycoprotein E administered at 1- or 2- month intervals were well-tolerated and induced much more robust VZV-specific and VZV glycoprotein E-specific CD4+T cell and antibody responses than did vOka [47,48]. A randomized placebo-controlled study of 15.411 subjects ≥50 years of age revealed a remarkable 97.2% efficacy in preventing zoster for a 3.2-year period that did not diminish with increasing age [49]. Compared to the placebo group, systemic adverse reactions were 2.2-fold greater in the vaccine group. Because HZ/su does not replicate, it will be safe for immunosuppressed patients. The duration of its effect is unknown. HZ/su vaccine is not yet FDA approved.
6. Increased understanding of the complications of zoster
The pathogenesis of VZV infection has become better understood as our recognition and analysis of the multiple disease entities that complicate herpes zoster has increased. Epidemiological studies have enabled a better characterization of the relationship of VZV to cancer and cardiovascular disease. Results of studies on the association of zoster with cancer are mixed, with one study suggesting an insignificant risk [50], but two recent nationwide studies in Taiwan indicating an increased risk [51,52]; one of those studies found that patients with herpes zoster ophthalmicus were 9 times more likely to die of cancer within 1 year.
Postherpetic neuralgia (PHN) is the most common complication of zoster. PHN is operationally defined as dermatomal-distribution pain persisting for more than 3 months after zoster. Age is the most important factor that predicts its development. Among persons older than 50 and 80 years, the incidence of PHN in zoster patients is 18% and 33%, respectively. Overall, 80% of PHN occurs among persons 50 years and older. In addition, more than 40% of zoster patients >60 years of age experience chronic pain. Analysis of ganglia from an early case of PHN of 2.5 months’ duration revealed diffuse and focal infiltration by chronic inflammatory cells [53], an observation confirmed by Watson et al. [54], who found prominent collections of lymphocytes in ganglia from a patient with PHN of 2 years’ duration. The inflammatory response in ganglia raised the possibility of prolonged viral infection. Further evidence that PHN may be produced by low-level ganglionitis has come from the detection of VZV DNA and proteins in blood MNCs of many patients with PHN and from the favorable response of some PHN patients to antiviral treatment.
Technology has also allowed better attribution of nervous system illness to VZV. For example, PCR and detection of anti-VZV antibody in CSF revealed that VZV reactivation produces not only zoster and PHN, but also VZV meningoencephalitis, VZV myelitis, VZV vasculopathy, all of which may develop in the absence of rash [55]. VZV reactivation can also cause acute retinal necrosis, progressive outer retinal necrosis, and retinal hemorrhage, often in association with zoster, meningitis, vasculitis and myelitis. In addition, complications of herpes zoster ophthalmicus include dendriform keratitis, stromal keratitis, endothelial keratitis, uveitis, and neurotrophic keratopathy [56]. Particularly interesting is the analysis of large and small vessel disease secondary to VZV infection [57]. In 1959, Cravioto and Feigin [58] described the first documented case of VZV vasculopathy, which was followed by case reports of VZV vasculopathy throughout the following decades. It is now known that VZV vasculopathy is caused by productive infection of cerebral arteries, most often leading to ischemic stroke as well as hemorrhagic stroke, aneurysm with and without subarachnoid and intracerebral hemorrhage, dolichoectasia, dissection and venous sinus thrombosis. A study of 30 subjects with virologically confirmed VZV vasculopathy [59] revealed rash in 63%, CSF pleocytosis in 67% and imaging abnormalities in 97% of patients; angiography indicated abnormalities in 70% of subjects, with large and small arteries involved in 50%, small arteries in 37% and large arteries in only 13% of 30 subjects. The average time from rash to neurologic symptoms and signs was 4.1 months, and from neurologic symptoms and signs to CSF virologic analysis, 4.2 months. The CSF of only 30% of subjects contained VZV DNA, whereas 93% had anti-VZV IgG antibody in CSF with a reduced serum/CSF ratio of anti-VZV IgG that confirmed intrathecal synthesis of anti-VZV IgG. Thus, detection of anti-VZV IgG antibody in CSF is the best test to diagnose VZV vasculopathy [60]. Importantly, diagnosis of this treatable cause of stroke using intravenous acyclovir is often missed because there is no history of zoster rash in 1/3 of subjects, the CSF is normal in 1/3 of subjects, there is an average 4.2-month delay from zoster to neurological symptoms and signs, and VZV DNA is often not present in CSF [61]
After reactivation from cranial nerve ganglia, VZV likely spreads transaxonally to the outermost adventitial layer of the artery wall; infected cerebral arteries contain a thickened intima composed of myofibroblasts, a disrupted internal elastic lamina, and a paucity of smooth muscle cells [62]. Inflammatory cells (primarily CD4 and CD8 T cells and CD68 macrophages) are present predominantly in the adventitia and to a lesser degree, in the luminal surface of the thickened intima [63]. Early VZV vasculopathy reveals a striking numbers of neutrophils in the adventitia. A remarkable finding in a VZV-infected artery is the association of inflammation with a thickened intima, supporting findings in the cardio- and pulmonary- vascular fields that inflammation is heavily involved in vascular remodeling.
7. VZV and stroke
While the exact incidence of VZV vasculopathy is unknown, recent epidemiological studies from Taiwan, Denmark and the UK have all revealed an increased risk of stroke after zoster, particularly when zoster is in the ophthalmic-distribution of the trigeminal nerve [63]. Multiple studies from the UK, Europe and Asia have revealed that stroke incidence after zoster is greater than in age-matched control subjects. Analysis of medical records from the Taiwan National Health Research Institute revealed a 30% increased risk of stroke in the year after zoster, a risk that was increased 4-fold when zoster was in the ophthalmic division of the trigeminal nerve [64]. Similar analysis of medical records from a Danish national registry revealed a 126% increased risk of stroke within 2 weeks after zoster, a 17% increased risk from 2 weeks to 1 year after zoster, and a 5% increased risk of stroke after the first year, compared to a control group of untreated zoster patients [65]. Analysis of the UK Health Improvement Network general practice database indicated a significant increase in transient ischemic attacks and myocardial infarctions in patients with zoster; importantly, the increased risk was greatest in zoster patients younger than 40 years of age [67]. Most recently, analysis of the UK General Practice Research Database showed that stroke risk decreased over time after zoster in any dermatome as compared to control time periods. Statistically significant age-adjusted incidence ratios of stroke were found 1-4 weeks after zoster (1.63), 5-12 weeks after zoster (1.42), and 13-26 weeks after zoster (1.23), with no increase at later times. In patients with ophthalmic-distribution zoster, the risk of stroke was increased 3-fold from 5-12 weeks after zoster. Finally, among the 55% of zoster patients who received oral antiviral therapy, the risk of stroke was reduced compared to untreated patients with zoster [68], indicating the value of antiviral treatment in reducing stroke incidence after zoster.
8. Association of VZV with giant cell arteritis
In the past few years, VZV infection was demonstrated in extracranial temporal arteries (TAs) in 3 patients. The first case was in an elderly man who developed ophthalmic-distribution zoster, followed one month later by multifocal VZV vasculopathy that manifested as ischemic optic neuropathy (ION) and with clinical features of giant cell arteritis (GCA) [69]. The second case was an elderly woman who also developed ION with no other features of GCA and in whom VZV was demonstrated in the ipsilateral TA; importantly the patient had no history of recent zoster [70]. The third case was a 54-year-old diabetic individual, also with no history of recent zoster, who developed ION followed by acute retinal necrosis and TA infection [71].
These remarkable reports were followed by studies addressing the prevalence of VZV infection in patients with biopsy-negative GCA TAs. Immunohistochemical examination of archived biopsy-negative TAs for the presence of VZV antigen from patients with clinically suspect GCA revealed VZV in 5 (21%) of 24 such TAs [72]. All 5 subjects whose TAs contained VZV antigen presented with clinical and laboratory abnormalities of GCA and early visual disturbances, indicating that multifocal VZV vasculopathy can present with the full spectrum of features seen in GCA.
The continuing search for VZV antigen in GCA-negative TAs has revealed abundant VZV antigen as well as VZV DNA in multiple regions (skip areas) of a GCA-negative TA and in skeletal muscle adjacent to the infected TA; additional pathological analysis of sections adjacent to those containing viral antigen revealed inflammation involving the arterial media and abundant multinucleated giant cells characteristic of GCA [73], thus providing virological support for the causal role of VZV in GCA.
In 2015, a prospective analysis of archived formalin-fixed, paraffin-embedded GCA-positive TA biopsies (50 sections/TA), including adjacent skeletal muscle, and normal TA biopsies from subjects >50 years of age detected VZV antigen in 74% GCA-positive TAs compared with 1/13 normal TAs. Most GCA-positive TAs contained viral antigen in skip areas. VZV antigen was present mostly in adventitia, followed by media and intima. VZV antigen was found in 38% of skeletal muscles adjacent to VZV antigen-positive TAs. Despite formalin fixation, VZV DNA was detected in 40% of GCA-positive, VZV antigen-positive TAs, in 60% of VZV antigen-positive skeletal muscles and in one VZV antigen-positive normal TA. VZ virions were found in a GCA-positive TA. GCA pathology in sections adjacent to those containing VZV was seen in 89% of GCA-positive TAs, but in none of 18 adjacent sections from the normal TA. Most GCA-positive TAs contained VZV in skip areas that correlated with adjacent GCA pathology, supporting the hypothesis that VZV triggers GCA immunopathology [74]. Since skip areas of pathology are characteristic of GCA, the detection of VZV in 74% GCA-positive TAs likely reflects the value of staining a minimum of 50 sections from every artery.
Further examination of TAs from patients with clinically suspect GCA whose TAs were histopathologically negative as compared with normal TAs removed postmortem from age-matched subjects revealed VZV antigen in 64% of GCA-negative TAs compared with 22% normal TAs [74]. Overall, in patients with clinically suspect GCA, the prevalence of VZV in their TAs is similar independent of whether biopsy is negative or positive pathologically.
Finally, VZV vasculopathy causes symptoms and signs of anterior ischemic optic neuropathy (AION). Examination of TAs from 7 AION patients for VZV identified VZV antigen in 5 of 7 AION patients with GCA-negative TA biopsies [75]. Of those 5, 2 had symptoms of GCA, 3 had an elevated ESR or CRP, and 3 presented with features atypical of nonarteritic ischemic optic neuropathy, including progressive loss of vision, subretinal hemorrhage or perivascular gliosis of the optic disc. In one patient, GCA pathology was detected in a tissue section adjacent to VZV antigen, confirming the diagnosis of arteritic AION. Overall, the presence of VZV in TA biopsies of AION patients with or without clinical or laboratory abnormalities characteristic of GCA suggests a link between VZV and ION that may offer a novel avenue to the treatment of ischemic optic neuropathies.
9. Future directions
Both the AIDS epidemic and increased use of immunosuppresive therapies has led to a steady increase in the number of immunocompromised individuals [76]. VZV infection incidence among AIDS patients is several times higher than in healthy individuals of the same age, and 50 to 100 times higher among children with leukemia than their same age counterparts [39]. The prevalence of zoster among recipients of hematopoietic stem cell transplantation is 30 - 53% [27,77-79]. Antiviral therapy provides a variable duration of prophylaxis for VZV reactivation, but individuals receiving stem cell transplantation remain at increased risk when antiviral treatments are discontinued [28,76,81]. Not only is VZV reactivation more common in immunocompromised individuals, but disease is often protracted and severe, including disseminated zoster with pneumonia and encephalitis. While widespread vaccination in many, but not all, countries has reduced disease produced by VZV, multiple disorders produced by reactivation is a continuing problem.
Many challenges remain in vaccination and prevention of VZV reactivation. The long-term outcomes of both varicella and zoster vaccines are still unknown. VZV in varicella vaccine becomes latent and can reactivate to produce meningitis [81] and VZV vasculopathy [82]. While repeated exposure to VZV may decrease rates of reactivation, vaccination may increase the incidence of zoster that might be reduced by boosters early on [83]. Many aspects of virus transmission, such as the effect of living in different climates, require further study. Thus, even with the development of the vaccine, there continue to be individuals at risk for the disease, particularly in the immunocompromised population.
Future efforts will continue to focus on treatment and prevention of VZV infection and reactivation. As noted, varicella vaccine consists of a live attenuated virus that becomes latent, as does wild-type VZV. Efforts to generate a killed VZV vaccine that produces a strong immune response against a specific VZV protein [84] have shown promise. In that context, the use of the simian varicella virus model in primates may identify specific varicella virus proteins responsible for virulence and pathogenicity. A subunit zoster vaccine may be particularly useful, not only because it does not become latent, but also because of its stability, probable low cost and the possibility of using it in immunocompromised individuals. Whether a subunit vaccine can also be used to induce stable primary immunity to varicella remains unclear and awaits further research.
10. Conclusions
The history of VZV is one of the most fascinating in all of medicine. Today, we are challenged by the protean disorders VZV produces, including stroke as well as giant cell arteritis [73,74]. Optimal immunization against varicella in childhood and the prevention of zoster in the elderly are goals of the future.
HIGHLIGHTS.
Herpes zoster has been recognized since antiquity
Varicella (chickenpox) was not distinguished from smallpox until the 1800s
Varicella zoster virus (VZV) was first proven to be latent in ganglia in 1983
VZV reactivation produces meningoencephalitis, myelitis and vasculopathy without rash
VZV causes giant cell arteritis
Acknowledgements
This work was supported in part by Public Health Service grants AG032958 (D.G.) and NS093716 (D.G.) from the National Institutes of Health. The authors thank Marina Hoffman for editorial assistance and Cathy Allen for the word processing and formatting of the manuscript.
Abbreviations
- IE63
immediate early protein 63
- VariZig
varicella zoster immune globulin
- CDC
Center for Disease Control and Prevention
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of interest statement
Both authors report no conflicts of interest.
References
- 1.Sykes W. Origin of “zoster” in herpes zoster. Br Med J. 1902;1:930. [Google Scholar]
- 2.Saraya T, Inoue M, Takizawa H, Goto H. Varicella-zoster virus pneumonia in an immunocompetent patient. Intern Med. 2013;52:1003. doi: 10.2169/internalmedicine.52.0150. [DOI] [PubMed] [Google Scholar]
- 3.Joseph CA, Noah ND. Epidemiology of chickenpox in England and Wales, 1967-85. Br Med J (Clin Res Ed) 1988;296:673–6. doi: 10.1136/bmj.296.6623.673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lian TY, Lim KKT. The legacy of William Heberden the Elder (1710-1801). Rheumatology. 2004;43:664–5. doi: 10.1093/rheumatology/keg007. [DOI] [PubMed] [Google Scholar]
- 5.Gorden JE. Chickenpox: an epidemiological review. Am J Med Sci. 1962;244:362–89. [PubMed] [Google Scholar]
- 6.Rosenow C, Oftedal S. The etiology and experimental production of herpes zoster. J Infect Dis. 1916;18:477–500. [Google Scholar]
- 7.White CJ. Varicella-zoster virus vaccine. Clin Infect Dis. 1997;24:753–61. doi: 10.1093/clinids/24.5.753. quiz 762-3. [DOI] [PubMed] [Google Scholar]
- 8.Weller TH. Varicella and herpes zoster: a perspective and overview. J Infect Dis. 1992;166(Suppl 1):S1–6. [PubMed] [Google Scholar]
- 9.Head H, Campbell AW. The pathology of herpes zoster and its bearing on sensory localization. Brain. 1900;23:353–62. doi: 10.1002/(sici)1099-1654(199709)7:3<131::aid-rmv198>3.0.co;2-7. [DOI] [PubMed] [Google Scholar]
- 10.Head H, Campbell AW, Kennedy PG. The pathology of herpes zoster and its bearing on sensory localization. Rev Med Virol. 1997;7:131–43. doi: 10.1002/(sici)1099-1654(199709)7:3<131::aid-rmv198>3.0.co;2-7. [DOI] [PubMed] [Google Scholar]
- 11.Weller TH, Witton HM, Bell EJ. The etiologic agents of varicella and herpes zoster; isolation, propagation, and cultural characteristics in vitro. J Exp Med. 1958;108:843–68. doi: 10.1084/jem.108.6.843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Brain WR. A lecture on zoster, varicella, and encephalitis. Br Med J. 1931;1:81–4. doi: 10.1136/bmj.1.3654.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Seiler HE. A study of herpes zoster particularly in its relationship to chickenpox. J Hyg (Lond) 1949;47:253–62. doi: 10.1017/s002217240001456x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Paschen E. Ueber die pockendiagnose. Hyg. Rundschau. 1919;29:269–77. [Google Scholar]
- 15.Paschen E. Weitere mitteilungen über vakzineviruszüchtung in der gewebekultur. Elementarkörperchen im bläascheninhalt bei herpes zoster und varizellen. Zentr Bakt Parasitenk. 1933;130:190–3. [Google Scholar]
- 16.Nagler FP, Rake G. The use of the electron microscope in diagnosis of variola, vaccinia, and varicella. J Bacteriol. 1948;55:45–51. doi: 10.1128/jb.55.1.45-51.1948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ruska H. Über das virus der varizellen und des zoster. Klin Wochenschr. 1943;22:703–4. [Google Scholar]
- 18.Garland J. Varicella following herpes zoster. N Engl J Med. 1943;228:336–7. [Google Scholar]
- 19.Hope-Simpson RE. The nature of herpes zoster: A long-term study and a new hypothesis. Proc R Soc Med. 1965;58:9–20. doi: 10.1177/003591576505800106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bennett GJ, Watson CPN. Herpes zoster and postherpetic neuralgia: past, present and future. Pain Res Manag. 2009;14:275–82. doi: 10.1155/2009/380384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Vafai A, Mahalingam R, Zerbe G, Wellish M, Gilden DH. Detection of antibodies to varicella-zoster virus proteins in sera from the elderly. Gerontology. 1988;34:242–9. doi: 10.1159/000212962. [DOI] [PubMed] [Google Scholar]
- 22.Gilden DH, Vafai A, Shtram Y, Becker Y, Devlin M, Wellish M. Varicella-zoster virus DNA in human sensory ganglia. Nature. 1983;306:478–80. doi: 10.1038/306478a0. [DOI] [PubMed] [Google Scholar]
- 23.Hyman RW, Ecker JR, Tenser RB. Varicella-zoster virus RNA in human trigeminal ganglia. Lancet. 1983;2:814–6. doi: 10.1016/s0140-6736(83)90736-5. [DOI] [PubMed] [Google Scholar]
- 24.Kennedy PG, Grinfeld E. Latent varicela-zoster virus is located predominiantly in neurons in human trigeminal ganglia. Proc Natl Acad Sci U S A. 1998;95:4658–62. doi: 10.1073/pnas.95.8.4658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Straus SE, Reinhold W, Smith HA, et al. Endonuclease analysis of viral DNA from varicella and subsequent zoster infections in the same patient. N Engl J Med. 1984;311:1362–4. doi: 10.1056/NEJM198411223112107. [DOI] [PubMed] [Google Scholar]
- 26.Ouwendijk WJD, Choe A, Nagel MA, et al. Restricted varicela zoster virus transcription in human trigeminal ganglia obtained son after death. J Virol. 2012;86:10203–6. doi: 10.1128/JVI.01331-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Locksley RM, Flournoy N, Sullivan KM, Meyers JD. Infection with varicella-zoster virus after marrow transplantation. J Infect Dis. 1985;152:1172–81. doi: 10.1093/infdis/152.6.1172. [DOI] [PubMed] [Google Scholar]
- 28.Asano-Mori Y, Kanda Y, Oshima K, et al. Long-term ultra-low-dose acyclovir against varicella-zoster virus reactivation after allogeneic hematopoietic stem cell transplantation. Am J Hematol. 2008;83:472–6. doi: 10.1002/ajh.21152. [DOI] [PubMed] [Google Scholar]
- 29.Mahalingam R, Wellish M, Soike K, White T, Kleinschmidt-DeMasters BK, Gilden DH. Simian varicella virus infects ganglia before rash in experimentally infected monkeys. Virology. 2001;279:339–42. doi: 10.1006/viro.2000.0700. [DOI] [PubMed] [Google Scholar]
- 30.Mahalingam R, Traina-Dorge V, Wellish M, et al. Simian varicella virus reactivation in cynomolgus monkeys. Virology. 2007;368:50–9. doi: 10.1016/j.virol.2007.06.025. [DOI] [PubMed] [Google Scholar]
- 31.Takahashi M, Otsuka T, Okuno Y, Asano Y, Yazaki T. Live vaccine used to prevent the spread of varicella in children in hospital. Lancet. 1974;2:1288–90. doi: 10.1016/s0140-6736(74)90144-5. [DOI] [PubMed] [Google Scholar]
- 32.Takahashi M, Asano Y, Kamiya H, et al. Development of varicella vaccine. J Infect Dis. 2008;197(Suppl 2):S41–4. doi: 10.1086/522132. [DOI] [PubMed] [Google Scholar]
- 33.Centers for Disease Control and Prevention (CDC) Evolution of varicella surveillance--selected states, 2000-2010. MMWR Morb Mortal Wkly Rep. 2012;61:609–12. [PubMed] [Google Scholar]
- 34.Ross AH. Modification of chicken pox in family contacts by administration of gamma globulin. N Engl J Med. 1962;267:369–76. doi: 10.1056/NEJM196208232670801. [DOI] [PubMed] [Google Scholar]
- 35.Brunell PA, Ross A, Miller LH, Kuo B. Prevention of varicella by zoster immune globulin. N Engl J Med. 1969;280:1191–4. doi: 10.1056/NEJM196905292802201. [DOI] [PubMed] [Google Scholar]
- 36.Marin M, Güris D, Chaves SS, Schmid S, Seward JF, Advisory Committee on Immunization Practices. Centers for Disease Control and Prevention (CDC) Prevention of varicella: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep. 2007;56(RR-4):1–40. [PubMed] [Google Scholar]
- 37.Levin MJ, Murray M, Rotbart HA, Zerbe GO, White CJ, Hayward AR. Immune response of elderly individuals to a live attenuated varicella vaccine. J Infect Dis. 1992;166:253–9. doi: 10.1093/infdis/166.2.253. [DOI] [PubMed] [Google Scholar]
- 38.Oxman MN, Levin MJ, Johnson GR, et al. A vaccine to prevent herpes zoster and postherpetic neuralgia in older adults. N Engl J Med. 2005;352:2271–84. doi: 10.1056/NEJMoa051016. [DOI] [PubMed] [Google Scholar]
- 39.Centers for Disease Control and Prevention Nutrition. 2015 Retrieved from http://www.cdc.gov/vaccines/vpd-vac/shingles/vacc-need-know.htm.
- 40.Oxman MN, Levin MJ. Vaccination against herpes zoster and postherpetic neuralgia. J Infect Dis. 2008;197(Suppl):S228–36. doi: 10.1086/522159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Levin MJ. In: Vaccines. Plotkin S, Orenstein W, Offit P, editors. Elsevier; 2013. pp. 969–80. [Google Scholar]
- 42.Schmader KE, Johnson GR, Saddier P, et al. Effect of a zoster vaccine on herpes zoster-related interference with functional status and health-related quality-of-life measures in older adults. J Am Geriatr Soc. 2010;58:1634–41. doi: 10.1111/j.1532-5415.2010.03021.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zostavax [package insert], Whitehouse Station. Merck & Co Inc; New Jersey: 2006. [Google Scholar]
- 44.Harpaz R, Ortega-Sanchez IR, Seward JF. Prevention of herpes zoster: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep. 2008;57:1–30. quiz CE2-4. [PubMed] [Google Scholar]
- 45.Simberkoff MS, Arbeit RD, Johnson GR, et al. Safety of herpes zoster vaccine in the shingles prevention study: a randomized trial. Ann Intern Med. 2010;152:545–54. doi: 10.7326/0003-4819-152-9-201005040-00004. [DOI] [PubMed] [Google Scholar]
- 46.Morrison VA, Johnson GR, Schmader KE, et al. Long-term persistence of zoster vaccine efficacy. Clin Infect Dis. 2015;60:900–9. doi: 10.1093/cid/ciu918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Tseng HF, Smith N, Harpaz R, Bialek SR, Sy LS, Jacobsen SJ. Herpes zoster vaccine in older adults and the risk of subsequent herpes zoster disease. JAMA. 2011;305:160–6. doi: 10.1001/jama.2010.1983. [DOI] [PubMed] [Google Scholar]
- 48.Langan SM, Smeeth L, Margolis DJ, Thomas SL. Herpes zoster vaccine effectiveness against incident herpes zoster and post-herpetic neuralgia in an older US population: a cohort study. PLoS Med. 2013;10:e1001420. doi: 10.1371/journal.pmed.1001420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lal H, Cunningham AL, Godeaux O, et al. Efficacy of an adjuvanted herpes zoster subunit vaccine in older adults. N Engl J Med. 2015;372:2087–96. doi: 10.1056/NEJMoa1501184. [DOI] [PubMed] [Google Scholar]
- 50.Ragozzino MW, Melton LJ, Kurland LT, Chu CP, Perry HO. Population-based study of herpes zoster and its sequelae. Medicine (Baltimore) 1982;61:310–6. doi: 10.1097/00005792-198209000-00003. [DOI] [PubMed] [Google Scholar]
- 51.Ho J-D, Xirasagar S, Lin H-C. Increased risk of a cancer diagnosis after herpes zoster ophthalmicus: a nationwide population-based study. Ophthalmology. 2011;118:1076–81. doi: 10.1016/j.ophtha.2010.10.008. [DOI] [PubMed] [Google Scholar]
- 52.Liu B, Heywood AE, Reekie J, et al. Risk factors for herpes zoster in a large cohort of unvaccinated older adults: a prospective cohort study. Epidemiol Infect. 2015 doi: 10.1017/S0950268814003653. doi: http://dx.doi.org/10.1017/S0950268814003653 [Epub ahead of print] [DOI] [PMC free article] [PubMed]
- 53.Smith FP. Pathological studies of spinal nerve ganglia in relation to intractable intercostal pain. Surg Neurol. 1978;10:50–3. [PubMed] [Google Scholar]
- 54.Watson CP, Deck JH, Morshead C, et al. Postherpetic neuralgia: further postmortem studies of cases with and without pain. Pain. 1991;44:105–17. doi: 10.1016/0304-3959(91)90124-G. [DOI] [PubMed] [Google Scholar]
- 55.Gilden D, Cohrs RJ, Mahalingam R, Nagel MA. Neurological disease produced by varicella zoster virus reactivation without rash. Curr Top Microbiol Immunol. 2010;342:243–53. doi: 10.1007/82_2009_3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Barry Lee W, Liesegang TJ. Herpes zoster keratitis. In: Krachmer JH, Mannis MJ, Holland EJ, editors. Cornea. 2nd ed. Mosby; St. Louis: 2004. pp. 1075–90. [Google Scholar]
- 57.Kleinschmidt-DeMasters BK, Amlie-Lefond C, Gilden DH. The patterns of varicella zoster virus encephalitis. Hum Pathol. 1996;27:927–38. doi: 10.1016/s0046-8177(96)90220-8. [DOI] [PubMed] [Google Scholar]
- 58.Cravioto H, Feigin I. Noninfectious granulomatous angiitis with a predilection for the nervous system. Neurology. 1959;9:599–609. doi: 10.1212/wnl.9.9.599. [DOI] [PubMed] [Google Scholar]
- 59.Nagel MA, Cohrs RJ, Mahalingam R, et al. The varicella zoster virus vasculopathies: clinical, CSF, imaging and virological features. Neurology. 2008;70:853–60. doi: 10.1212/01.wnl.0000304747.38502.e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Nagel MA, Forghani B, Mahalingam R, et al. The value of detecting anti-VZV IgG antibody in CSF to diagnose VZV vasculopathy. Neurology. 2007;68:1069–73. doi: 10.1212/01.wnl.0000258549.13334.16. [DOI] [PubMed] [Google Scholar]
- 61.Gilden D, Nagel MA, Cohrs RJ, Mahalingam R. The variegate neurological manifestations of varicella zoster virus infection. Curr Neurol Neurosci Rep. 2013;13:374. doi: 10.1007/s11910-013-0374-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Nagel MA, Traktinskiy I, Azarkh Y, et al. Varicella zoster virus vasculopathy: analysis of virus-infected arteries. Neurology. 2011;77:364–70. doi: 10.1212/WNL.0b013e3182267bfa. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Nagel MA, Traktinskiy I, Stenmark KR, Frid MG, Choe A, Gilden D. Varicella zoster virus vasculopathy: Immune characteristics of virus-infected arteries. Neurology. 2013;80:62–8. doi: 10.1212/WNL.0b013e31827b1ab9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Lin HC, Chien Cw, Ho JD. Herpes zoster ophthalmicus and the risk of stroke: a population-based follow-up study. Neurology. 2010;74:792–7. doi: 10.1212/WNL.0b013e3181d31e5c. [DOI] [PubMed] [Google Scholar]
- 64.Kang JH, Ho JD, Chen YH, et al. Increased risk of stroke after a herpes zoster attack: a population-based follow-up study. Stroke. 2009;40:3443–8. doi: 10.1161/STROKEAHA.109.562017. [DOI] [PubMed] [Google Scholar]
- 65.Sreenivasan N, Basit S, Wohlfahrt J, et al. The short- and long-term risk of stroke after herpes zoster – a nationwide population-based cohort study. PLoS One. 2013;8:e69156. doi: 10.1371/journal.pone.0069156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Breuer J, Pacou M, Gauthier A, Brown MM. Herpes zoster as a risk factor for stroke and TIA: a retrospective cohort study in the UK. Neurology. 2014;82:206–12. doi: 10.1212/WNL.0000000000000038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Langan SM, Minassian C, Smeeth L, Thomas SL. Risk of stroke following herpes zoster: a self-controlled case-series study. Clin Infect Dis. 2014;58:1497–503. doi: 10.1093/cid/ciu098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Salazar R, Russman A, Nagel MA, et al. Varicella zoster virus ischemic optic neuropathy and subclinical temporal artery involvement. Arch Neurol. 2011;68:517–20. doi: 10.1001/archneurol.2011.64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Nagel MA, Russman AN, Feit H, et al. VZV ischemic optic neuropathy and subclinical temporal artery infection without rash. Neurology. 2013;80:220–2. doi: 10.1212/WNL.0b013e31827b92d1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Mathias M, Nagel MA, Khmeleva N, et al. VZV multifocal vasculopathy with ischemic optic neuropathy, acute retinal necrosis and temporal artery infection in the absence of zoster rash. J Neurol Sci. 2013;325:180–2. doi: 10.1016/j.jns.2012.12.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Nagel MA, Bennett JL, Khmeleva N, et al. Multifocal VZV vasculopathy with temporal artery infection mimics giant cell arteritis. Neurology. 2013;80:2017–21. doi: 10.1212/WNL.0b013e318294b477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Nagel MA, Khmeleva N, Boyer PJ, Choe A, Bert R, Gilden D. Varicella zoster virus in the temporal artery of a patient with giant cell arteritis. J Neurol Sci. 2013;335:228–30. doi: 10.1016/j.jns.2013.09.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Gilden D, White T, Khmeleva N, et al. Prevalence and distribution of VZV in temporal arteries of patients with giant cell arteritis. Neurology. 2015;84:1948–55. doi: 10.1212/WNL.0000000000001409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Nagel MA, White T, Khmeleva N, et al. Analysis of VZV in giant cell arteritis positive and negative temporal artery biopsies. JAMA Neurol. 2015 doi: 10.1212/NXI.0000000000000216. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Golas L, Bennett JL, White TM, Skarf B, et al. Varicella zoster virus in ischemic optic neuropathy. Ophthalmology. 2015 doi: 10.1016/j.ophtha.2015.04.026. pii: S0161-6420(15)00408-X. doi: 10.1016/j.ophtha.2015.04.026. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Löbermann M, Boršo D, Hilgendorf I, Fritzsche C, Zettl UK, Reisinger EC. Immunization in the adult immunocompromised host. Autoimmun Rev. 2012;11:212–8. doi: 10.1016/j.autrev.2011.05.015. [DOI] [PubMed] [Google Scholar]
- 77.Boeckh M, Kim HW, Flowers MED, Meyers JD, Bowden RA. Long-term acyclovir for prevention of varicella zoster virus disease after allogeneic hematopoietic cell transplantation--a randomized double-blind placebo-controlled study. Blood. 2006;107:1800–5. doi: 10.1182/blood-2005-09-3624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Su SH, Martel-Laferrière V, Labbé A-C, et al. High incidence of herpes zoster in nonmyeloablative hematopoietic stem cell transplantation. Biol Blood Marrow Transplant. 2011;17:1012–7. doi: 10.1016/j.bbmt.2010.10.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Issa NC, Marty FM, Leblebjian H, et al. Live attenuated varicella-zoster vaccine in hematopoietic stem cell transplantation recipients. Biol Blood Marrow Transplant. 2014;20:285–7. doi: 10.1016/j.bbmt.2013.11.013. [DOI] [PubMed] [Google Scholar]
- 80.Erard V, Guthrie KA, Varley C, et al. One-year acyclovir prophylaxis for preventing varicella-zoster virus disease after hematopoietic cell transplantation: no evidence of rebound varicella-zoster virus disease after drug discontinuation. Blood. 2007;110:3071. doi: 10.1182/blood-2007-03-077644. [DOI] [PubMed] [Google Scholar]
- 81.Esposito S, Bosis S, Pinzani R, Morlacchi L, Senatore L, Principi N. A case of meningitis due to varicella zoster virus reactivation in an immunocompetent child. Ital J Pediatr. 2013;39:72. doi: 10.1186/1824-7288-39-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Sabry A, Hauk PJ, Jing H, et al. Vaccine strain varicella-zoster virus-induced central nervous system vasculopathy as the presenting feature of DOCKS deficiency. J Allergy Clin Immunol. 2014;133:1225–7. doi: 10.1016/j.jaci.2013.11.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Brisson M, Gay NJ, Edmunds WJ, Andrews NJ. Exposure to varicella boosts immunity to herpes-zoster: implications for mass vaccination against chickenpox. Vaccine. 2002;20:2500–7. doi: 10.1016/s0264-410x(02)00180-9. [DOI] [PubMed] [Google Scholar]
- 84.Jacquet A, Haumont M, Massaer M, et al. Immunogenicity of a recombinant varicella-zoster virus gE-IE63 fusion protein, a putative vaccine candidate against primary infection and zoster reactivation. Vaccine. 2002;20:1593–1602. doi: 10.1016/s0264-410x(01)00486-8. [DOI] [PubMed] [Google Scholar]