Abstract.
The objective of this study was to identify factors affecting on errors in carbohydrate (CHO) content estimation during CHO counting. Thirty-seven type 1 diabetes patients and 22 of their parents and 28 physicians/dieticians were enrolled in this study. CHO counting was counted in “Carb”, with 1 Carb defined as 10 g of CHO. To evaluate the accuracy of CHO counting, 80 real-size photographs of cooked meals were presented to the subjects for Carb estimation. Carbs tended to be overestimated for foods containing relatively small amounts of Carbs. On the other hands, Carbs tended to be underestimated for foods with higher than 6 Carbs. Accurate estimation of the Carbs in food containing a large amount of rice was particularly difficult even in the subjects having the CHO counting experience. The Carb contents of high-calorie foods such as meats, fried foods, and desserts tended to be overestimated. This error was smaller in subjects having the CHO counting experience. In conclusion, misunderstanding of high-calorie dishes containing high amounts of CHO was observed in inexperienced subjects, indicating the efficacy of the current methodology of CHO counting. On the other hand it was difficult even for experienced subjects to assess the amount of seasoned rice, suggesting the need for a new methodology for accurate estimation.
Keywords: carbohydrate counting, type 1 diabetes, education, estimation of carbohydrate content
Introduction
Carbohydrate (CHO) counting is a meal plan approach for diabetes mellitus that focuses on the fact that among the nutrients contained in food, CHO has the strongest activity in elevating the postprandial blood glucose level and its amount rather than its type is directly associated with postprandial blood glucose level (1, 2).
The practical use of CHO counting to adjust insulin doses was first reported in 1987 (3). In that report, the patients were taught to adjust their insulin dose according to the CHO content of foods, which resulted in improvements in blood glucose control. In the Diabetes Control and Complications Trial (DCCT) (4), a large-scale clinical study involving 1441 patients with type 1 diabetes mellitus in the United States and Canada, CHO counting was adopted as one of the diet therapies (5), and its usefulness was demonstrated. Since then, the usefulness of CHO counting for insulin therapy of diabetes mellitus has been gradually recognized across the world. In the Dose Adjustment For Normal Eating (DAFNE) Study, carried out in the United Kingdom in 1999 (6), insulin therapy matched to a diet making use of CHO counting resulted in an improvement in hemoglobin A1c (HbA1c), degree of freedom as to meal content, and quality of life. In the DAFNE study, a rapid-acting insulin analog (RA) was used. RA acts within a time frame similar to the effect of CHO on the blood glucose level and is much better than regular insulin for CHO counting (1). Many studies regarding CHO counting have been reported (7, 8), and advanced CHO counting is included in some official guidelines for the treatment of type 1 diabetes (9, 10).
In Japan, the Japan Diabetes Society recommends that diabetic individuals use the Food Exchange Lists, first published in 1965, for their nutritional management (11, 12). The lists define 80 kcal as a unit of energy and focuses on weight control for type 2 diabetes. In contrast, CHO counting focuses on the CHO content regardless of the number of calories in food.
At the Department of Pediatrics, Osaka City University Hospital, CHO counting was actively adopted into basal-bolus therapy during routine clinical management of type 1 diabetes mellitus more than 10 yr ago, which is when RA began to be available in Japan. In recent years, an increasing number of medical facilities have adopted CHO counting for type 1 diabetes (13,14,15). However, CHO counting has not come into widespread use in Japan, possibly because of the wide variety of Japanese foods currently available. Various Western and Chinese cuisines are already part of the Japanese diet. Therefore, it is not easy to evaluate the dietary CHO content of a typical Japanese meal.
Using CHO counting, CHO intake is calculated in either grams or CHO servings. In the United States, patients are advised to count 15 g of CHO as 1 CHO serving (2). At our facility, for convenience of calculation, we define 10 g of CHO as 1 Carb (13, 16) and we used this definition in the present study and expressed in which the amount of CHO is expressed in Carb units.
During implementation of CHO counting, the insulin to Carb ratio (I/C ratio), which represents the amount (units) of RA needed for 1 Carb, is used to calculate the amount of insulin needed for the CHO contained in meals. The magnitude of the reduction in blood glucose level approximately 4 h after a dose of 1 U of RA is the insulin sensitivity and is used for calculating the amount of insulin needed to correct a high blood glucose level.
The I/C ratio and insulin sensitivity vary depending on various factors such as age, body weight, time of day, physical activity, and general condition and so on. Even when the I/C ratio and the insulin sensitivity have been adjusted appropriately, the insulin dose cannot be adjusted satisfactorily if the Carb amount is unknown. An error by 1 Carb in estimation for a patient with an I/C ratio of 1.0 can lead to a 1-U error in calculating the amount of insulin needed. Therefore, an adequate understanding of CHO-rich foods and an accurate estimation of the Carbs in individual foods are very important in practicing and maintaining good blood glucose control.
The accuracy of the estimations of Carbs in foods by individual seems to be affected by various factors such as the patient’s experience and knowledge, type of foods, and methods of cooking. The Japanese dietary style involves diverse foods and cooking methods, and it is not clear which dishes or foods are likely to cause errors in Carb estimation.
In the present study, we focused on the relationship between the accuracy of Carb estimation for Japanese meals and that dished and carried out a Carb estimation test using photographs of various cooked meals. The purpose of this study was to identify foods and dished likely to cause errors in Carb estimation from the external appearance of foods and to explore factors determining the accuracy of Carb estimation, with an ultimate goal of collecting information useful in establishing an effective method for advising patients.
Subjects and Methods
The subjects of this study were patients with type 1 diabetes mellitus managed as outpatients at the Department of Pediatrics, Osaka City University Hospital, and their parents and the health-care professionals (physicians, dieticians, and others) who were involved in their care of these patients. Thirty-seven patients (28 children aged 10–19 yr, and 9 young adult aged 20–32 yr), 22 parents of who patients were below 10 yr old, and 28 health-care professionals (12 physicians and 16 dieticians) were enrolled in this study. In addition, the patients and parents were combined into a group, the Pt group and were divided into two subgroups—those having experience with CHO counting (C+Pt group) and those not having experience with CHO counting (C-Pt group)—and the health-care professionals were combined into a group, the Tc group and similarly divided into those involved in advising patients regarding CHO counting (C+Tc group) and those not involved in advising patients regarding CHO counting (C-Tc group). Experience with CHO counting was defined as having if they have received the instruction of it even once. Consequently, 24 subjects were in the C+Pt group, 35 subjects were in the C-Pt group, 19 subjects were in the C+Tc group, and 9 subjects were in the C-Tc group.
To examine the accuracy of estimated Carbs from the external appearance of food, 80 full-sized photographs of cooked meals, “Sonomanma Syokuzai Syashin” (Real Foodstuff Pictures) (Yodosha Co., Ltd., Tokyo, Japan), were presented to each subject to estimate the Carbs from the photographs at the Outpatient Pediatric Office. During this test, each subject was given no information as to the weight or nutritional value of the samples. The differences between the Carbs estimated by subjects and the actual Carbs were analyzed as the estimation errors for each group. Estimation error = (estimated Carbs) – (actual Carbs). Actual Carbs were calculated from the information supplied by the manufacturers about the amounts of CHO contained in each food or meal represented in the photograph.
Photographs of cooked meals were divided into three groups: (1) a high-CHO group (main materials were grains and potatoes, e.g., rice, noodles, bread, and fried potatoes), (2) a low-CHO group (main materials were meat, fish/shellfish, and low-CHO vegetables), and (3) a dessert and fruit group (confectionery, fruits, etc.). To examine which dishes among each meal group resulted in larger estimation errors, the estimation errors of each dish were compared. To determine whether or not CHO counting experience affects the accuracy of Carb estimation or not, the estimation errors of each dishes were compared between subjects with and without CHO counting experience. Finally, the relationship between Carbs for all dishes and the estimation errors of the experiment subjects was analyzed.
The ethics committee of the Osaka City University Institutional Review Board, Osaka, Japan, approved this protocol.
The significance of intergroup differences in estimation errors was tested by Mann-Whitney U-test, and P < 0.05 was regarded as statistically significant. Linear regression analysis was used for the relationship between Carbs for foods and estimation error. Statistical analysis was carried out with SPSS version 11.0 (SPSS Inc., Chicago, IL, USA).
Results
High-CHO food group
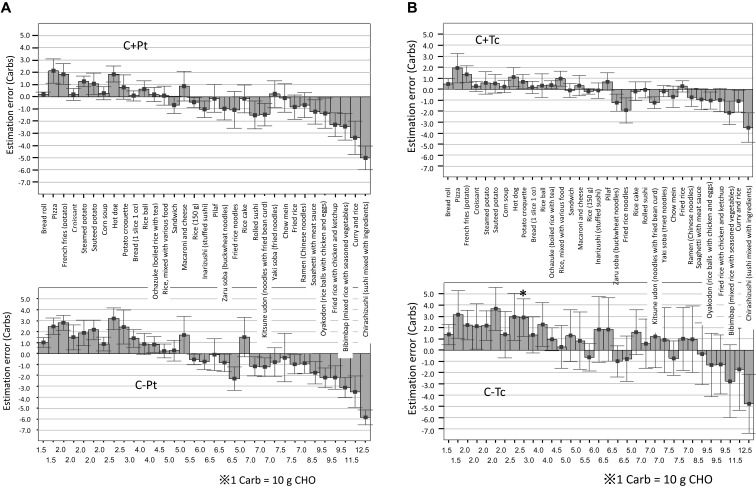
Estimation errors for the high-CHO food tests are shown in Fig. 1. The estimation errors for dishes such as bread, pizza, and the common potato, which contain relatively small amounts of CHO per dish, were small in both the Pt groups (Fig. 1A) and the Tc groups (Fig. 1B) of whether or not the subjects had experience with CHO counting. In contrast, Carbs tended to be markedly underestimated for dishes containing relatively large amounts of CHO per dish, such as fried rice with chicken and ketchup, rolled sushi, chirashizushi (a vinegared rice mixed and/or topped with other ingredients), bibimbap (Korean rice bowl mixed with seasoned vegetables), oyakodon (rice bawl with chicken and eggs), and curry and rice. Among others dishes, the estimation error was 1 Carb or more on average in each group for chirashizushi, bibimbap, oyakodon, and curry and rice.
Fig. 1.
Carb estimation error in the tests using photographs of cooked meals (high-CHO foods). Estimation error = (estimated Carbs) – (actual Carbs). On the x-axis of the top panels, the foods are listed in ascending order of Carbs (lowest on the left to highest on the right). The numbers below the bottom panels show the actual Carbs of each food. A) Comparison of Carb estimation errors between the C+Pt and C-Pt groups. * Significant vs C+Pt group (P < 0.05). B) Comparison of Carb estimation errors between the C+Tc and C-Tc groups. * Significant vs C+Tc group (P < 0.05).
When analyzed by food category, a tendency for underestimation of Carbs was noted for each type of noodle. This tendency was seen to a similar degree in the C+Pt, C-Pt, and C+Tc groups, but the C-Tc group tended to overestimate Carbs for kitsune udon (noodles with fried bean curd), ramen (Chinese noodles in soup), and yakisoba (fried noodles). Estimation errors were small for bread and bread rolls. However, Carbs for high-calorie cooked foods made with bread, such as pizza and hot dogs, tended to be markedly overestimated (by at least 1 Carb). Estimation errors were slightly greater in subjects without CHO counting experience, but not significant. The tendency for estimation errors for the high-CHO foods differed little among the different groups of subjects, but the error was particularly small in the C+Tc group.
Low-CHO food group
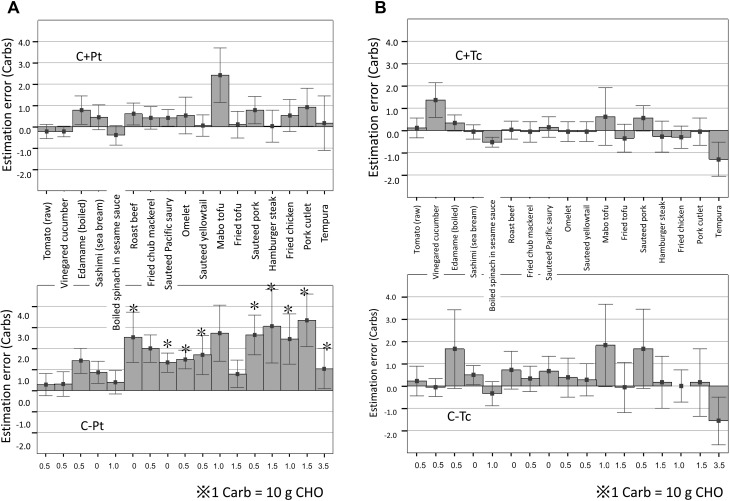
Estimation errors for the low-CHO food tests are shown in Fig. 2. For all dishes in the low-CHO group, Carbs tended to be overestimated.
Fig. 2.
Carb estimation error in the tests using photographs of cooked meals (low-CHO foods). Estimation error = (estimated Carbs) – (actual Carbs). On the x-axis of the top panels, the foods are listed in ascending order of Carbs (lowest on the left to highest on the right). The numbers below the bottom panels show the actual Carbs of each food. A) Comparison of Carb estimation errors between the C+Pt and C-Pt groups. * Significant vs C+Pt group (P < 0.05). B) Comparison of Carb estimation errors between the C+Tc and C-Tc groups.
For the low-CHO foods, the overall estimation error was small in the C+Pt and C+Tc groups, whereas the C-Pt and C-Tc groups tended to overestimate Carbs (this tendency was particularly marked in the C-Pt group for estimation of Carbs in high-calorie foods). When the estimation error was compared between Pt groups with or without CHO counting experience (Fig. 2A), the error was significantly greater in the C-Pt group than in the C+Pt group for estimation of Carbs in sauteed Pacific saury, omelets, sauteed yellowtail, sauteed pork, hamburger steak, fried chub mackerel, fried chicken, and pork cutlets (P < 0.05).
On the whole, estimation errors were relatively small for low-calorie foods. However, Carbs for roast beef (a low-calorie food) were overestimated by 2 or more Carbs in the C-Pt group, and the estimation error for this food differed significantly between the C+Pt group and the C-Pt group (P < 0.05).
When the estimation error was compared among health-care professionals (Fig. 2B), the estimations were more accurate in the C+Tc group than in the C-Tc group, but the difference was not statistically significant.
Dessert and fruit food group
Carbs tended to be overestimated for most foods in the dessert and fruit group (data not shown).
Among the fruits, the estimation error was largest for strawberries. Among the confectionery foods, cheesecake was overestimated by 1 Carb or more in both the patient and the professional groups. An exception was sweet red bean jelly for which Carbs tended to be underestimated. Among patients, the C-Pt group had a significantly larger error in estimation of Carbs for doughnuts compared with the C+Pt group. For the other foods, there were no significant intergroup differences in estimation errors.
The tendency of estimation error differed little among the foods in this group. In the C+Tc group, the estimation error was small (less than ± 1 Carb) for most foods.
Relationship between Carbs for foods and estimation error in the subjects with CHO counting experience
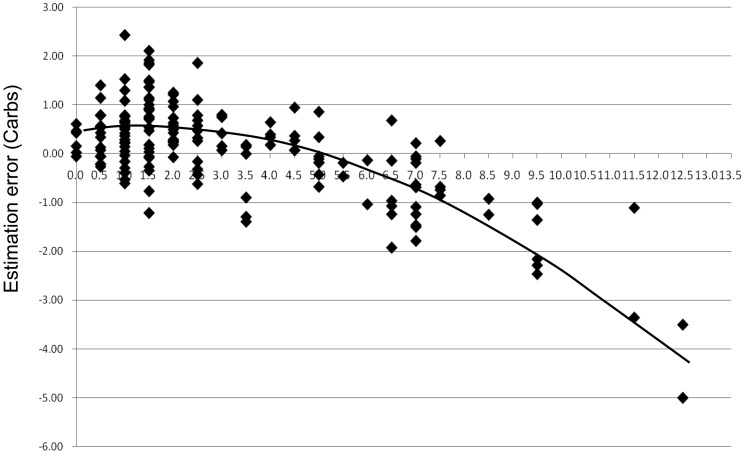
After the finding that Carbs tended to be overestimated for foods with low actual Carbs and underestimated for foods with high actual Carbs, we analyzed the relationship between Carbs and estimation errors in all subjects with CHO counting experience without dividing the foods into different groups. In this analysis, we found a relation between food Carbs and estimation errors (Fig. 3). The curve fitted by regression analysis to data plots was shown in the figure (y = –0.35x2 + 0.104x + 0.415, R2 = 0.603). Underestimation tended to occur for foods with actual Carbs over about 6 even in the subjects having the experience with CHO counting.
Fig. 3.
Relationship between Carbs and estimation errors in both the C+Pt and C+Tc groups. The graph depicts the relationship between Carbs (x-axis) and mean estimation error (y-axis) for each food in 63 patients who had previously practiced CHO counting and 19 health-care professionals who had been involved in giving advice regarding CHO counting. The curve fitted by regression analysis to data plots is shown (y = –0.35x2 + 0.104x + 0.415, R2 = 6.03).
Discussion
The present study was designed to analyze errors in estimation of Carbs depending on foodstuffs and dishes in patients with type 1 diabetes mellitus and health-care professionals.
During CHO counting, there is no necessity to estimate the Carbs in grams, but it seems realistic to set a goal of estimating the approximate Carbs based on the external appearance of foods. Smart et al. (17) reported that elevations in postprandial blood glucose arising from a 10-g difference in CHO intake can be adequately controlled by calculating the insulin dose level on the basis of the commonly used I/C ratio. For this reason, it seems valid to set a goal of keeping the estimation error within ± 1 Carb.
The estimation error for Carb may be evaluated by the proportion of error relative to the total actual Carbs. However, the estimation error is directly related to the dose of insulin in the clinical field as mentioned as above. Therefore, in this study the estimation error was used for the evaluation.
The percentage of CHO relative to the total energy sources is approximately 10% higher in Japanese people than in Americans, and Japanese people take approximately 50–60% of their daily total energy from CHO (18, 19). Staple foods (rice, bread, and noodles) are a major source of CHO according to the Japanese dietary style. Because CHO affects the postprandial blood glucose level most, it is of utmost importance to estimate Carbs in staple foods as accurately as possible.
The results of the Carb estimation tests during this study revealed a tendency for Carbs to be estimated inaccurately for foods in the high-CHO group, particularly rice, noodles, and buns (small bread rolls).
Among rice-based dishes, the estimation error was small for dishes with approximately 5 Carbs, such as rice, ochazuke (boiled rice with tea), and gomoku rice (rice mixed with various foods), suggesting that accurate estimation of Carbs from external appearance is relatively easy for these dishes. In contrast, the estimation error was high for dishes containing large amounts of rice with high actual Carbs, such as chirashizushi (vinegared rice mixed and/or topped with other ingredients) and curry and rice, regardless of the presence or absence of CHO counting experience. The likelihood for erroneous estimation of Carbs for these dished is possibly attributable to difficulty in assessing the amount of rice at a glance because of other foodstuff either placed atop the rice or mixed with the rice. The reason for a marked tendency for underestimation of Carbs for chirashizushi is probably associated with sugar (contained in this dish), which increases the actual Carbs compared with the Carbs estimated from external appearance.
Carbs for noodles tended to be underestimated in the tests using photographs of meals, suggesting that dished with noodles are likely to be underestimated regardless of the type of noodle used. Noodles are often 6–7 Carbs/dish, and it needs to be borne in mind that Carbs for the same weight of noodles can vary depending on the thickness of the noodles. For example, for 200 g of noodles, there are 4.5 Carbs for udon and 5 Carbs for soba or somen; thus, the amount of Carbs per serving decreases as the noodle becomes thicker and vice versa.
It has been pointed out that knowing the Carbs of staple foods is a basic requirement for individuals to accurately estimate the Carbs for these foods. Essential points in advising patients regarding CHO counting vary from report to report. For individuals not familiar with CHO counting, it has been recommended to weigh foods with a balance or to refer to a food composition table or guidebook when calculating the Carbs. In the case of rice, for example, it is advisable that the individual puts rice into a bowl, weighs the rice and bowl together, and remembers the external appearance and the Carbs recorded at that time or that the individual remembers the external appearance and Carbs of 150 g of rice (a standard volume of rice placed in a bowl), which is equivalent to 5.5 Carbs, so that this memory can be referred to when estimating Carbs in the future (16). Recently, rice bowls with graduations, enabling quick assessment of the rice weight, have become commercially available, and this type of bowl should be used if needed. In the present study, the estimation error was large for rice served in the form of sushi. The CHO content of sushi is higher than that of ordinary rice due to the sugar added, which amounts to 3–5% of the rice weight. For dishes such as rice bowls and curry and rice, the amount of rice per dish is often 250–300 g, and this amount of rice contains approximately 10 Carbs (16, 20). Patients often complain of the difficulty in estimating the Carbs when they are eating out at restaurants and without a scale. In such cases, estimation of Carbs from external appearance would be easier if these data are borne in mind. However, the results from the present study revealed no significant difference in estimation error for high-CHO foods between the experienced subjects (patients practicing CHO counting during daily life and health-care professionals and others involved in advising patients) and the inexperienced subjects. This result suggests that accurate estimation of the weight of rice is difficult even for individuals having experience with CHO counting. It is therefore desirable to establish a new method of advising patients how to accurately estimate the amount of rice.
Buns and cooked foods made with bread are diverse in type and content, and their Carbs per piece vary greatly. In the present study, the estimation error was larger for pizza and hot dogs compared with bread rolls and loaf bread. This result suggests that estimating Carb from the external appearance of buns and cooked foods made with bread is difficult. The food labels on the commercially available buns and cooked foods made with bread often specify the amount of CHO. This information deserves attention if present. Among buns of the same weight, those containing jam or bean jam have higher Carbs (5–6 Carbs) than those containing cream. Among cooked foods made with bread, curry bread, pizza, and hot dogs are rich in fat and calories but low in Carbs (approximately 3 Carbs). This information needs to be provided to patients so that patients can refer to such data when the product carries no information about nutrient composition.
For the low-CHO foods, there was a tendency to overestimate Carbs in fried dishes (such as fried chicken, tempura, fried shrimp, and pork cutlets) and high-calories foods. However, the estimation error was small for patients with CHO counting experience and health-care professionals involved in advising patients. These results suggest that as far as dishes of the low-CHO group are concerned, the accuracy of Carb estimation can be improved by receiving advice at outpatient clinics or diabetes summer camps or through practicing CHO counting in daily life.
When guiding patients in CHO counting for dishes with low-CHO foods, it is important to make the patient understand that meat, fish, eggs, etc. have 0 Carbs if no seasoning is used. If the fundamental food has 0 Carbs, adding seasoning will add approximately 0.5–1 Carbs, and using wheat flour or breadcrumbs for frying will add 1.5–2 Carbs. Therefore, dishes composed of meat, fish, or eggs will have only 2–3 Carbs per dish unless foods rich in CHO (e.g., potato, pumpkin, or macaroni) are used (20).
Estimation errors were large for high-calorie foods such as fried dishes. This is probably attributable to (1) confusion between a food’s calorie and CHO contents, resulting in erroneous estimation of Carbs, and (2) having no knowledge about or having forgotten the necessity of excluding protein and lipids from CHO counting.
The food exchange lists often used in Japan focus on calorie control (12). It seems likely that patients who began CHO counting after having used food exchange lists were excessively aware of calories and lipid levels from their experience with food exchange lists, possibly leading to erroneous estimation of Carbs. In a questionnaire survey of patients with type 2 diabetes mellitus scheduled to begin CHO counting, the patients were asked to list nutrients that affect blood glucose levels (21). In that survey, a high percentage of patients answered that calories affect blood glucose levels. Thus, it is not surprising that patients are confused when estimating Carbs because of the advice they received during conventional guidance at medical facilities (focusing on calorie restriction), the information on nutrient composition carried on food products, and information collected from journals and the media.
Regarding the influence of protein and lipids on the accuracy of Carb estimation, it has been shown that 50% of the protein is converted over time into glucose and that a meal rich in protein elevates blood glucose levels 3–5 hours after ingestion (22, 23). The percentage of lipids converted into glucose is small, but lipids can delay gastric emptying and thus delay the elevation of blood glucose levels (23). Thus, proteins and lipids can also affect postprandial blood glucose levels and the accuracy of Carb estimation if they are present in large amounts. Regarding low-CHO foods, it seems necessary to give concrete advice to patients, e.g., by presenting examples of high-calorie low-CHO foods using pictures or food models at places likely to catch the attention of patients, so that patients are well aware of the necessity of excluding proteins and lipids from CHO counting.
Confectioneries, classified in the dessert and fruit group, are diverse in type and content, as is the case with buns (small bread rolls), and CHO content is also diverse for foods in this category. In the present study, there was a strong tendency for overestimation of Carbs for cake (a Western-style confectionery). Western-style confectioneries are often higher in calories but lower in Carbs per piece (approximately 2–3 Carbs) compared with Japanese-style confectioneries. Japanese-style confectioneries use large amounts of beans rich in sugar and CHO and thus have higher Carbs per unit weight than Western-style confectioneries. Japanese-style confectioneries are smaller and lower in calories compared with Western-style confectioneries, which explains why the Carbs of Japanese-style confectioneries tend to be underestimated. The results of the present study suggest that awareness of the calories and lipids tends to result in overestimation of Carbs for Western-style confectioneries, as is the case for foods in the low-CHO group.
The study reported by Bishop et al. (24) concerned to the relationship between the accuracy of Carb estimation and blood glucose control. Their study incorporated a test for patients with type 1 diabetes mellitus aged between 12 and 18 years to estimate the amount of CHO contained in 32 foods. Among the 32 foods tested, the amount of CHO was significantly overestimated for syrup, hash browns (hashed potatoes), rice, spaghetti, and chips and underestimated for cereals, French fries, and soda. Their results differ from our findings that Carbs tended to be underestimated for main dishes such as rice and noodles. This discrepancy may be associated with differences in dietary style or sense about food weight between the subjects of their study and the subjects of our study. When the amount of food is estimated on the basis of photographs presented, the amount tends to be overestimated as the portion size becomes smaller and tends to be underestimated as the portion size becomes larger (25). Therefore, the discrepancy between these two studies may be attributable to smaller amounts of rice and noodles ingested by Western people compared with Japanese people. Furthermore, in the present study, there was a strong tendency for foods with lower actual Carbs to be overestimated regarding Carbs and foods with higher actual Carbs to be underestimated regarding Carbs. The foods with relatively low actual Carbs used in the present study were often typical of Western-style dishes, such as bread, potato dishes, and cake, whereas foods with relatively high actual Carbs were often typical of Japanese-style dishes, such as sushi, rice bowls, and curry and rice. Most of the high-CHO foods (over 7 Carbs) were made of rice. The discrepancy in results between the study of Bishop et al. (24) and the present study is thus attributable to the fact that the study conducted by Bishop et al. involved Western people and used foods with relatively low actual Carbs.
When Bishop et al. (24) analyzed the relationship between the accuracy of Carb estimation and HbA1c, they found that HbA1c was more favorable in patients who estimated the Carbs more accurately. However, to the best of our knowledge, there are no reports dealing with the influence of the accuracy of Carb estimation on blood glucose control. In this study, we did not analyze that relationship; we but suggest that further studies are needed concerning on this finding. We also did not evaluate whether the age and the duration of CHO counting experience might affect on the accuracy of Carb estimation too in this study.
Various techniques have been proposed to improve Carb estimation for foods based on external appearance, including (1) comparing the size of food with familiar objects such as the patient’s own palm, fist, or finger or a deck of playing cards; (2) checking the Carbs of foods the patient often eats in daily life; and (3) preparing a personal Carb table by referring to nutrient composition labels of commercial food products (16, 26). In any event, some training and experience are needed for individual patients to learn how to accurately estimate the Carbs of foods (26, 27). In this respect, it seems indispensable for patients to practice CHO counting under the guidance of physicians or dieticians and educational materials (leaflets, labels carrying information on nutrient composition, etc.) to increase the accuracy of Carb estimation.
As shown in Fig. 3, even the subjects having CHO counting experience seemed to underestimate the Carbs of food containing more than 6 Carbs. With the food containing more than 6 Carbs, the absolute value of estimation error become bigger. Physicians and dieticians should realize this tendency.
Furthermore, patients need to be guided not only regarding accurate estimation of Carbs but also regarding appropriately setting the I/C ratio and insulin sensitivity so that they can use CHO counting effectively tailored to their specific situation. Training is also needed for physicians and dieticians who are expected to guide patients. To date, however, education and training about CHO counting are seldomly provided within the framework of education programs at schools for dieticians. Cultivation of leaders and establishment of an education system for them are open issues related to CHO counting.
Conclusion
The accuracy of Carb estimation by CHO counting was analyzed in patients with type 1 diabetes mellitus.
In the analysis of trends in estimation error among different food groups, the tendency to underestimate Carbs was more marked for rice bowls and curry and rice (CHO-rich dishes with high Carbs) among the foods of the high-CHO group. Even the patients with CHO counting experience showed a 1 Carb or higher estimation error for these foods. This result suggests that accurate estimation of Carbs for dishes made of rice is difficult even for patients with CHO counting experience and that developing new tools and establishing new methods for guiding patients are desirable. Among the foods of the low-CHO group, high-calorie foods such as fried foods tended to be overestimated regarding Carb level in the subjects without CHO counting experience. This result showed that our current guidance method for CHO counting was helpful and also indicated the importance of guiding patients in appropriately making use of food models and leaflets to ensure that proteins and lipids were excluded from CHO counting.
References
- 1.Warshaw HS, Kulkarni K. Complete Guide to Carb Counting. How to Take the Mystery Out of Carb Counting and Improve Your Blood Glucose Control, Third Edition: Alexandria, American Diabetes Association, 2011. [Google Scholar]
- 2.Kawamura T. The importance of carbohydrate counting in the treatment of children with diabetes. Pediatr Diabetes 2007;8(Suppl 6): 57–62. doi: 10.1111/j.1399-5448.2007.00287.x [DOI] [PubMed] [Google Scholar]
- 3.Mühlhauser I, Bruckner I, Berger M, Cheţa D, Jörgens V, Ionescu-Tîrgovişte C, et al. Evaluation of an intensified insulin treatment and teaching programme as routine management of type 1 (insulin-dependent) diabetes. The Bucharest-Düsseldorf Study. Diabetologia 1987;30: 681–90. doi: 10.1007/BF00296989 [DOI] [PubMed] [Google Scholar]
- 4.The Diabetes Control and Complications Trial Research GroupThe effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med 1993;329: 977–86. doi: 10.1056/NEJM199309303291401 [DOI] [PubMed] [Google Scholar]
- 5.Anderson EJ, Richardson M, Castle G, Cercone S, Delahanty L, Lyon R, et al. The DCCT Research GroupNutrition interventions for intensive therapy in the Diabetes Control and Complications Trial. J Am Diet Assoc 1993;93: 768–72. doi: 10.1016/0002-8223(93)91750-K [DOI] [PubMed] [Google Scholar]
- 6.DAFNE Study GroupTraining in flexible, intensive insulin management to enable dietary freedom in people with type 1 diabetes: dose adjustment for normal eating (DAFNE) randomised controlled trial. BMJ 2002;325: 746. doi: 10.1136/bmj.325.7367.746 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schmidt S, Schelde B, Nørgaard K. Effects of advanced carbohydrate counting in patients with type 1 diabetes: a systematic review. Diabet Med 2014;31: 886–96. doi: 10.1111/dme.12446 [DOI] [PubMed] [Google Scholar]
- 8.Bell KJ, Barclay AW, Petocz P, Colagiuri S, Brand-Miller JC. Efficacy of carbohydrate counting in type 1 diabetes: a systematic review and meta-analysis. Lancet Diabetes Endocrinol 2014;2: 133–40. doi: 10.1016/S2213-8587(13)70144-X [DOI] [PubMed] [Google Scholar]
- 9.Dyson PA, Kelly T, Deakin T, Duncan A, Frost G, Harrison Z, et al. Diabetes UK Nutrition Working GroupDiabetes UK evidence-based nutrition guidelines for the prevention and management of diabetes. Diabet Med 2011;28: 1282–8. doi: 10.1111/j.1464-5491.2011.03371.x [DOI] [PubMed] [Google Scholar]
- 10.American Diabetes AssociationStandards of medical care in diabetes—2013. Diabetes Care 2013;36(Suppl 1): S11–66. 23264422 [Google Scholar]
- 11.Kitamura S. Diet therapy and food exchange lists for diabetic patients. Diabetes Res Clin Pract 1994;24(Suppl): S233–40. doi: 10.1016/0168-8227(94)90255-0 [DOI] [PubMed] [Google Scholar]
- 12.The Japanese Diabetes Society Tonyobyo Syokujiryoho no tameno Syokuhin Kokanhyo (Food exchange lists—Dietary guidance for persons with diabetes. 7th. edition). Tokyo: Bunkodo, 2014. (in Japanese). [Google Scholar]
- 13.Hirose H. Usefulness of carbohydrate counting in Japanese children with type 1 diabetes mellitus. J Jpn Diabetes Soc 2007;50: 731–8(in Japanese). [Google Scholar]
- 14.Ishida H, Kitahara A. Carbohydrate counting – its merits and demerits. J Jpn Diabetes Soc 2011;54: 257–9(in Japanese). [Google Scholar]
- 15.Shiraishi S, Kikuchi N, Ochi K, Sato E, Ohashi J, Kawamura R, et al. Effects of carbohydrate counting on glycemic control and quality of life in patients with type 1 diabetes: a pilot study. Diabetology International 2014;5:181–6. doi: 10.1007/s13340-013-0153-8 [DOI] [Google Scholar]
- 16.Kawamura T, editor. Tonyobyo no anata he Kantan kabo kaunto (Easy carbohydrate counting: for healthy life. 2nd. edition). Osaka: Iyaku (Medical & Drug) Journal Co. Ltd, 2009. (in Japanese). [Google Scholar]
- 17.Smart CE, Ross K, Edge JA, Collins CE, Colyvas K, King BR. Children and adolescents on intensive insulin therapy maintain postprandial glycaemic control without precise carbohydrate counting. Diabet Med 2009;26: 279–85. doi: 10.1111/j.1464-5491.2009.02669.x [DOI] [PubMed] [Google Scholar]
- 18.United State Department of Agriculture What We Eat in America, NHANES 2011-2012. http://www.ars.usda.gov/SP2UserFiles/Place/80400530/pdf/1112/Table_5_EIN_GEN_11.pdf. [PubMed]
- 19.The Ministry of Health, Labour and Welfare. Current health and nutritional status of the nation – From the Ministry of Health, Labour and Welfare Report on National Health and Nutritional Survey in 2012. Tokyo: Daiichi syuppan, 2013. (in Japanese).
- 20.Kawamura T, editor. Tonyobyo kanja no tameno Kabo furasyu kado (Carb flush card for diabetic patients). Osaka: Iyaku Journal Sha, 2007. (in Japanese). [Google Scholar]
- 21.Sato M, Ono Y, Kondo E. Carb-count for patients with type 2 diabetes mellitus. J Jpn Diabetes Soc 2008;51: S160.(in Japanese). [Google Scholar]
- 22.Franz MJ. Protein: metabolism and effect on blood glucose levels. Diabetes Educ 1997;23: 643–6, 648, 650–1. doi: 10.1177/014572179702300603 [DOI] [PubMed] [Google Scholar]
- 23.Peters AL, Davidson MB. Protein and fat effects on glucose responses and insulin requirements in subjects with insulin-dependent diabetes mellitus. Am J Clin Nutr 1993;58: 555–60. [DOI] [PubMed] [Google Scholar]
- 24.Bishop F, Maahs D, Spiegel G, Owen D, Klingensmith G, Bortsov A, et al. The carbohydrate counting in adolescents with type 1 diabetes (CCAT) study. Diabetes Spectrum 2009;22: 56–62. doi: 10.2337/diaspect.22.1.56 [DOI] [Google Scholar]
- 25.Nelson M, Atkinson M, Darbyshire S. Food photography II: use of food photographs for estimating portion size and the nutrient content of meals. Br J Nutr 1996;76: 31–49. doi: 10.1079/BJN19960007 [DOI] [PubMed] [Google Scholar]
- 26.Scheiner G. Counting carbohydrates like a pro. Practical tips for accurate counts. Diabetes Self Manag 2009;26: 8–, 10–2, 14.. [PubMed] [Google Scholar]
- 27.Spiegel G, Bortsov A, Bishop FK, Owen D, Klingensmith GJ, Mayer-Davis EJ, et al. Randomized nutrition education intervention to improve carbohydrate counting in adolescents with type 1 diabetes study: is more intensive education needed? J Acad Nutr Diet 2012;112: 1736–46. doi: 10.1016/j.jand.2012.06.001 [DOI] [PMC free article] [PubMed] [Google Scholar]