Abstract
Objective
Attention bias modification treatment (ABMT) is a promising novel treatment for anxiety disorders, but clinical trials have focused largely on stand-alone formats among adults. This randomized controlled trial examined the augmenting effects of threat-based ABMT on cognitive behavioral therapy (CBT) in clinically anxious youth.
Method
Sixty-three treatment-seeking children with anxiety disorder were randomly assigned to 1 of the following 3 treatment groups: ABMT + CBT; ABMT placebo + CBT; and CBT-alone. Participants in the 2 ABMT conditions received repeated training on dot–probe tasks either designed to shift attention away from threats (active) or designed to induce no changes in attention patterns (placebo). Primary outcome measures were frequency and severity of anxiety symptoms as determined by a clinician using a semi-structured interview. Self- and parent-rated anxiety measures and threat-related attention bias scores were also measured before and after treatment.
Results
Both the active and placebo ABMT groups showed greater reductions in clinician-rated anxiety symptoms than the CBT-alone group. Furthermore, only the active ABMT group showed significant reduction in self- or parentrated anxiety symptoms. Finally, all groups showed a shift in attention patterns across the study, starting with a bias toward threat at baseline and shifting attention away from threat after treatment.
Conclusions
Active and placebo ABMT might augment the clinical response to CBT for anxiety. This effect could arise from benefits associated with performing computer-based paradigms such as the dot–probe task. Given the absence of group differences in attention-bias changes during treatment, possible mechanisms and methodological issues underlying the observed findings are discussed. Clinical trial registration information—Augmenting Effects of ABMT on CBT in Anxious Children: A Randomized Clinical Trial; http://clinicaltrials.gov/; NCT01730625.
Keywords: anxiety, attention bias, attention bias modification treatment (ABMT), cognitive behavioral therapy (CBT)
The development of easily disseminated, safe, and efficacious treatments is an important goal for translational neuroscience research. To that end, attention bias modification treatment (ABMT) shows promise based on its ability to target threat-related attention biases1,2 and associated heightened anxiety in adults.3–5 A small series of randomized controlled trials also suggests the potential efficacy of ABMT in pediatric anxiety.6–10 The current RCT examined the degree to which threat-focused ABMT augments the response to cognitive behavioral therapy (CBT), an established treatment for pediatric anxiety disorders.
ABMT emerged from work linking anxiety to threat-related biases in attention. Anxious individuals commonly show excessive vigilance toward minor threats.2 The dot–probe task is 1 common method for quantifying such threat-related attention biases.11 In this task, a pair of stimuli, 1 threat and another neutral, appears concurrently in 2 different spatial locations on a computer screen. Their offset is followed by a probe that appears in the location previously occupied by 1 of the 2 stimuli. Allocation of attention is measured by the reaction time (RT) difference for identifying probes across the 2 spatial conditions. A faster RT to probes appearing in the location previously occupied by threat-related stimuli, relative to probes appearing in the location of neutral stimuli, indicates an attention bias toward threat.
ABMT uses the dot–probe task not merely to measure attention biases but also to implicitly modify such biases in anxious individuals. During ABMT, the location of the probe is manipulated to implicitly train attention. For example, training intended to reduce bias toward threat repeatedly presents probes in the location of the neutral rather than the threat stimulus. Over time, an implicitly learned bias away from threat is induced because such contingency provides prediction about target location.1
Because CBT and ABMT may target different cognitive aspects of anxiety, they may provide complementary benefits for anxious children. CBT modifies explicit and voluntary attention through verbal intervention (top–down approach); ABMT alters implicit and involuntary attention biases through computer-based training (bottom–up approach). Thus, ABMT may augment the response to CBT. To date, only 1 study has examined this potential synergistic effect in adult patients with generalized anxiety disorder.12 However, this study tested only the application of these 2 interventions together in an open trial without a control group affording a test of the augmenting effects of ABMT on CBT.
Although recent studies suggest that anxious children, like anxious adults, may also manifest attention bias toward threat,13 more ABMT studies focus on anxious adults than on anxious children. Only 2 studies to date on threat-focused ABMT in clinically anxious children found preliminary evidence of efficacy.6,10 And yet, as in similar RCTs of other computer-based treatments,7,8 ABMT was offered as a stand-alone treatment6 or compared only with the 2 ABMT groups without including a CBT-alone group.10 Available data in pediatric anxiety suggest that medications augment response to CBT.14,15 ABMT might provide similar augmenting benefits without the potential adverse side effects associated with medication. The current study examined the clinical response to CBT in groups of anxious children randomized to 1 of 3 treatments as follows: CBT with active ABMT (ABMT + CBT); CBT with placebo ABMT (ABMT placebo + CBT); or CBT with no additional intervention. The study tested the hypothesis that children randomized to ABMT + CBT would show greater reduction in anxiety symptoms than children randomized to either of the other 2 treatments.
METHOD
Participants
Participants were children or adolescents seeking treatment in a large child anxiety clinic (mean age = 11.5 years, SD = 2.91, range = 6.5–18). Children were invited to enroll in the study if, based on a structured psychiatric interview, they met DSM-IV criteria for separation anxiety disorder (SAD), social phobia (SoPh), specific phobia (SpPh), or generalized anxiety disorder (GAD). Exclusion criteria were as follows: lifetime history of psychosis; a clinical judgment that the child could not comply with CBT; a primary diagnosis of post-traumatic stress disorder (PTSD), obsessive compulsive disorder (OCD), or selective mutism.
Of 119 assessed children, 63 who met inclusion criteria agreed to participate. All 63 children received CBT and were randomly assigned to 1 of 3 groups: ABMT condition (ABMT+CBT), trained to induce an attentional bias away from threat (n = 18); attention bias placebo training (ABMT Placebo + CBT) (n = 25); CBT-alone, with no ABMT add-ons (n = 20). Differences in sample sizes in the 3 groups were the result of using random assignment. Of the 63 children assigned to the study, 8 children were not able to complete it, resulting in a total of 55 participants who were included in the final analysis (ABMT + CBT, n = 15; ABMT placebo + CBT, n = 22; CBT-alone, n = 18). This sample size is consistent with our power calculation. Based on a previous study, in the same clinic,6 we used effect sizes of Cohen’s d = 2.10 for the Anxiety Disorders Interview Schedule (ADIS) symptom count and d = 2.25 for symptom severity to calculate the required sample size with 80% power, yielding an estimate of 15 participants per group.
Sample demographics are presented in Table 1. The final sample included 7 anxious children diagnosed with comorbid ADHD: 2 children in the ABMT group, 2 children in the ABMT placebo group, and 3 in the CBT-alone condition. All of these patients received pharmacological treatment (methylphenidate) as described in Table 1.
TABLE 1.
Demographics and Pretreatment DSM-IV Diagnoses Among Completers Across the 3 Treatment Groups
| Demographics, m (SD) | ABMT n = 15 | ABMT-Placebo n = 22 | CBT Alone n = 18 | Statistics |
|---|---|---|---|---|
| Age | 11.5 (2.87) | 11.6 (2.90) | 10.18 (3.09) | F2,52 = 0.844 |
| SES | 3.20 (0.56) | 3.36 (0.58) | 3.24 (0.90) | F2,51 = 0.300 |
| Boys, n | 8 | 15 | 8 | χ2(2) = 0.310 |
| Girls, n | 7 | 7 | 10 | |
| Anxiety Dx, n (%) | ||||
| GAD only | 3 (20) | 4 (18) | 4 (20) | |
| SAD only | – | 2 (9) | 2 (11) | |
| SoPh only | – | – | 1 (6) | |
| SpPh only | 5 (33) | 4 (18) | 3 (17) | |
| GAD and SAD | 2 (13) | 3 (14) | 2 (11) | |
| GAD and SoPh | – | 2 (9) | 1 (6) | |
| GAD and SpPh | 1 (7) | 2 (9) | 1 (6) | |
| SAD and SpPh | 2 (13) | 1 (5) | 2 (11) | |
| SoPh and SpPh | – | 2 (9) | – | |
| GAD and SAD and SpPh | 1 (7) | 1 (5) | 1 (6) | |
| GAD and SpPh and SoPh | 1 (7) | 1 (5) | 1 (6) | |
| Comorbid Dx, n (%) | ||||
| ADHD | 2 (13) | 2 (9) | 3 (17) | χ2(2) = 0.518 |
| Medication, n (%) | ||||
| SSRIs | 1 (7) | 4 (18) | 2 (11) | |
| Stimulants | 2 (13) | 2 (9) | 3 (17) | |
| Total meds, % | 13 | 27 | 33 | χ2(2) = 0.390 |
Note: Statistics report F and χ2 values. Because of the small number of observations in diagnosis (Dx) cells, only descriptive statistics are reported. Medication at pretreatment. All medication remained constant during trial. ABMT = attention bias modification training; ADHD = attention-deficit/hyperactivity disorder; CBT = cognitive behavioral therapy; GAD = generalized anxiety disorder; meds = medications; SAD = separation anxiety disorder; SES = socioeconomic status; SoPh = social phobia; SpPh = specific phobia; SSRIs = selective serotonin reuptake inhibitors.
Materials and Tasks
Anxiety Disorders Interview Schedule for DSM-IV: C/P (ADIS)
Diagnosis was established with a structured psychiatric interview, the ADIS for DSM-IV: C/P,16 which assesses the major anxiety, mood, and externalizing DSM-IV disorders experienced by children and adolescents 7 to 18 years old. Patients and parents are presented with the same detailed list of symptoms (e.g., “when you are not with your parents, do you worry a lot that something bad might happen to them, like they might get sick or hurt and die?”) to which they have the option to respond “yes/no/other”. In line with the DSM-IV criteria, if patients or parents report sufficient numbers of symptoms (e.g., 3 items for simple phobia, 5 items for social anxiety), they meet criteria for the disorder. Once symptom criteria are met, patients and parents are asked about the severity of interference by the symptoms on a scale ranging from 0 to 8, with scores less than 4 indicating subthreshold levels of a symptom. If clinical severity is reported to be 4 or greater, a DSM-IV disorder is diagnosed. The ADIS possesses excellent test–retest reliability for both symptom scales and diagnoses,17 and has been translated into Hebrew in collaboration with the original authors. Interviewers were psychology graduate students who were trained on ADIS administration and reached 85% reliability criterion with an experienced psychologist. Two clinical psychologists supervised all the interviews and helped resolve any clinical or diagnostic issues that emerged.
Screen for Child Anxiety Related Emotional Disorders (SCARED)
The SCARED is a 41-item parent and child reported questionnaire, measuring DSM-IV-defined anxiety disorder symptoms (e.g., “My child is a worrier”—parent version; “I am nervous”—child version) in children and adolescents 7–19 years old). The scale measures symptoms of separation anxiety, generalized anxiety disorder, panic disorder, social phobia, and school phobia, on a 3-point scale (0 = not true or hardly true; 1 = somewhat true or sometimes true; 2 = very true or often true). SCARED total and subscale scores can be obtained by summing across relevant items. The SCARED is a reliable and valid child anxiety instrument18 that has been extensively used in clinical and research contexts in Israel.6 In line with the SCARED recommendations, a clinician explained all items in the questionnaire for children younger than 10 years. In the current study we used the average of the total SCARED scores reported by the children and their parent as an outcome measure. Cronbach’s α coefficients in the current study were 0.88 for child-report and 0.91 for parent-report.
Demographic Questionnaire
This questionnaire contained a series of demographic questions for descriptive and comparative purposes. For socioeconomic status (SES), participants rated the total monthly income in relation to the average family income on a 5-point scale (1 = much below the average; 2 = below average; 3 = average; 4 = above average; 5 = much above average relative to the national average of 12,345 NIS published by Israel’s Central Bureau of Statistics.
The Dot–Probe Task
The dot–probe task used to measure threat-related attention bias in the current study comprised 160 trials. Each trial began with a gray fixation cross (20 × 20 mm) in the center of the screen for 500 milliseconds, followed by a face pair display for 500 milliseconds. The face stimuli were photographs of 12 actors (6 males), with closed-mouth expressions, taken from the NimStim set,19 each contributing 2 pictures of the same actor: 1 expressing disgust and the other a neutral expression. Faces were presented in Disgust–Neutral or Neutral–Neutral pairs, 1 face above and 1 face below a central fixation position. Following the faces display, a target probe appeared in 1 of the locations vacated by the faces, and remained on the screen until response. The target-probe consisted of 2 letters, either the letter “E” or the letter “F”. Participants were required to determine which letter appeared on the screen by pressing prespecified buttons on the computer mouse using their dominant hand. Participants were told that it was important that they perform the task as quickly as possible without compromising accuracy. Disgust faces were equally likely to appear on the top or bottom. The face stimuli were split into 2 sets, set A and set B, each consisting of 6 faces (3 male).
Pre- and Posttreatment Assessments
In the pre-treatment assessment, participants were randomly assigned to complete 160 dot–probe trials of either set A or B. A total of 128 trials (80% of trials) consisted of Disgust–Neutral face pairs, with equal proportions of the target probes appearing at the location of the disgust face (“congruent” trials) and the neutral face (“incongruent” trials). Thirty-two trials (20% of trials) consisted of Neutral–Neutral face pairs. In the post-treatment assessment, participants completed 320 trials with the same proportion of trial types as in the pretreatment assessment. For posttreatment assessment, the task used 160 trials of the same face stimulus set used in the pretest and an additional 160 trials with the alternate set. Presentation of the stimuli of the 2 sets (A and B) was intermixed. The use of trials with new faces allowed testing regardless of whether training generalized to new faces not used in pre-assessment and in training.
Attention Bias Modification and Placebo Training
Training with the dot-probe task was delivered to participants in the ABMT groups during the CBT sessions. Specifically, in the ABMT + CBT condition, participants were presented with the same 128 Disgust–Neutral face pairs and 32 Neutral–Neutral face pairs as in the pretreatment session. However, in the Disgust–Neutral trials, the target-letters always appeared at the location of the neutral face (“incongruent” trials), thereby inducing a contingency between target location and face valence. In the ABMT placebo + CBT condition, participants were presented with the exact same stimuli, but with the target probes appearing with equal probabilities at the locations of the disgust and the neutral face (50% “congruent” and 50% “incongruent” trials). The same set of images as in the pretreatment assessment was used for the ABMT and placebo training.
CBT Procedure
All treatments were delivered in the Child Anxiety Clinic at Schneider Children’s Medical Center, Israel from October 2010 to July 2012. CBT involved 16 50-minute sessions, based on the Coping Cat program.20,21 This protocol targets the physiological, cognitive, and behavioral aspects of anxiety, teaching children to recognize signs of anxiety and to implement strategies to better cope with its debilitating challenges. The Coping Cat protocol was developmentally adapted to better fit patients younger than 9 years based on suggestions provided by its authors.22 Early stages of treatment focus on improving affective awareness, psycho-education, somatic management, and cognitive restructuring of maladaptive thoughts. Exposure to feared situations was gradually conducted both within session and outside the clinical context. Experienced psychologists trained in the Coping Cat protocol delivered the treatment; psychologists were supervised in a group setting through 90-minute weekly meetings during which detailed case presentations were discussed and treatment progression was monitored.
Procedure
The study was approved by the Ethic committee of Schneider Children’s Medical Center and the Israeli Administration of Health. Participants and their parents were asked to participate in a study that examined the use of a computer task for treating anxiety. They were told that this computer task was part of the therapy session and was to be delivered by the therapist. Furthermore, they were told that this task had been examined in previous studies and that it had been found to be beneficial for some anxious adults and youth. Participants were told that some anxious individuals show a tendency to focus on minor threats in the environment and that this computer task was designed to help them change this tendency. Finally, participants were told that they would be randomly assigned to 1 of the 3 treatment groups and that they were free to stop participation in the study at any time, and, if they choose to do so, it would have no effect on completing the CBT treatment. Parents provided written consent and children provided their assent.
Baseline assessments involved the dot–probe task, ADIS interview, and questionnaires, completed in approximately 90 minutes, after which participants were randomly assigned to 1 of 3 treatment conditions: ABMT + CBT, ABMT placebo + CBT, or CBT-alone. In the active and placebo ABMT conditions, therapists used their clinical judgment to select the time for dot–probe training within the 50-minute CBT session, such that contact time with therapists was equal in all 3 conditions. Post-treatment assessment took place 2 weeks after the last CBT session. All study personnel and all research participants were blind to participants’ training condition. A Consolidated Standards Of Reporting Trials (CONSORT) diagram illustrating the flow of participants through each stage of the study is shown in Figure 1.
FIGURE 1.
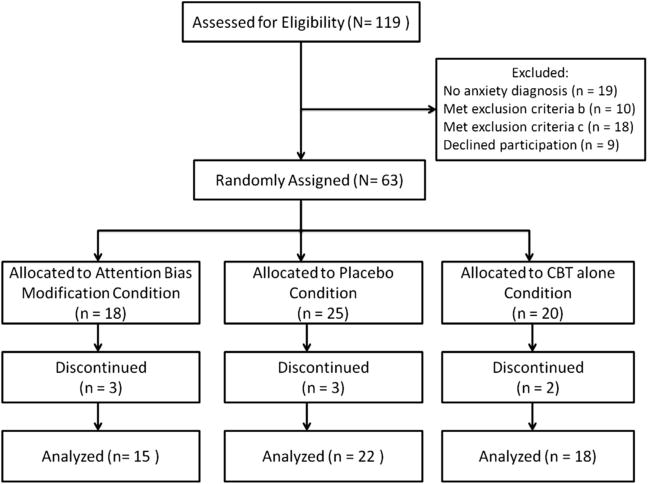
Consolidated Standards Of Reporting Trials (CONSORT) diagram of study design. Note: CBT = cognitive behavioral therapy.
Participants were not paid to participate in the study. Because the study was conducted in a public hospital’s anxiety clinic and because all children received CBT, a treatment known to be effective, patients had to pay a small amount to cover treatment expenses. However, this payment for treatment was significantly subsidized by mandatory public health insurance bills. In addition, the pre- and post-assessments were implemented as an integral part of the treatment plan in the clinic and were given to all participants free of charge.
Data Analysis
Baseline characteristics among the 3 randomized treatment groups were compared using χ2 statistics and an-alysesofvariance (ANOVAs). Three dependent variables were used to examine differences in treatment efficacy across the 3 groups. Two primary outcome measures were examined, based on rating by clinicians blind to participants’ group assignment. The 2 measures comprised the average number of anxiety symptom counts reported by parents and children on the ADIS, and the averaged symptom severity scale scores on different ADIS items. A secondary outcome was total SCARED score, computed as the mean of child and parent SCARED total scores. Each of these 3 measures was submitted to a separate analysis of variance (ANOVA), with Time (pretreatment, posttreatment) as a within-subject factor and Condition (ABMT + CBT, ABMT Placebo + CBT, CBT-alone) as a between-subjects factor.
Attention bias scores were computed as the difference score between reaction time in congruent trials and reaction time in incongruent trials. Only correct trials with reaction time in the range of 150 to 1500 milliseconds were included in the analysis. Reaction time less than 150 milliseconds could reflect a mere random finger press not associated with the stimuli, whereas reaction times longer than 1500 milliseconds could either tap into higher cognitive processes involving more awareness or simply indicate processes irrelevant to the task.1,6,9 A z-score for each trial within each of 3 possible trial types (neutral–threat congruent, neutral–threat incongruent, neutral–neutral) were computed, and trials with z-scores greater than |2.5| were removed. To test the effect of attention training, attention bias scores before and after treatment were submitted to an ANOVA, with Time (pretreatment, posttreatment) as a within-subject factor and Condition (ABMT + CBT, ABMT Placebo + CBT, CBT-alone) as a between-subjects factor. Pearson correlations were used to test for possible associations among continuous measures.
Intent-to-Treat Analyses
Similar ANOVAs were performed using the last observation carried forward method, whereby participants’ pretreatment assessment data were entered as their posttreatment data had they failed to complete the study. These analyses included 3 participants in the ABMT group, 3 participants in the ABM placebo group, and 2 participants in the CBT-alone group who dropped out before completion. All statistical significance thresholds were set to α = 0.05.
RESULTS
Sample Characteristics
Sample characteristics at baseline by treatment group are provided in Tables 1 and 2. No group differences in demographic, clinical, or attention variables emerged (all p > 0.30). In addition, no group differences in number of training sessions was noted between the ABMT group (mean = 8.00, SD = 3.38, range = 4–13) and the ABMT placebo training group (mean = 8.14, SD = 3.15, range = 4–15; t[35] = −.13, p > 0.90). Finally, no correlation was found between participant age and accuracy levels in the dot–probe task.
TABLE 2.
Clinical Variables Pre- and Posttreatment Among Completers Across the 3 Treatment Groups
| ABMT n = 15 | ABMT-Placebo n = 22 | CBT Alone n = 18 | Statistics | |
|---|---|---|---|---|
| ADIS | ||||
| Anxiety Dx, % | ||||
| Pretreatment | 100 | 100 | 100 | |
| Posttreatment | 33 | 36 | 72 | χ2(2) = 6.72* |
| Symptom Frequency, m (SD) | ||||
| Pre-treatment | 8.31 (3.61) | 6.80 (3.31) | 7.19 (2.91) | F2,48 = 0.665 |
| Posttreatment | 3.13 (3.73) | 1.20 (1.33) | 5.14 (4.32) | F2,48 = 4.66* |
| Symptom Severity, m (SD) | ||||
| Pretreatment | 7.13 (0.71) | 6.24 (1.43) | 6.64 (1.25) | F2,47 = 0.963 |
| Posttreatment | 2.55 (2.80) | 1.13 (1.30) | 4.05 (2.40) | F2,47 = 5.61** |
| SCARED, m (SD) | ||||
| Pretreatment | 33.64 (15.17) | 29.73 (9.10) | 34.50 (14.18) | F2,52 = 0.728 |
| Posttreatment | 22.63 (11.47) | 25.84 (14.06) | 36.11 (17.93) | F2,52 = 3.88* |
| Attention Bias, m (SD) | ||||
| Accuracy Threat | ||||
| Pretreatment | 0.92 (0.05) | 0.90 (0.10) | 0.94 (0.04) | |
| Posttreatment | 0.94 (0.05) | 0.89 (0.12) | 0.95 (0.03) | |
| Accuracy Neutral | ||||
| Pretreatment | 0.93 (0.05) | 0.91 (0.09) | 0.94 (0.08) | |
| Posttreatment | 0.95 (0.05) | 0.91 (0.08) | 0.96 (0.04) | |
| RT-Threat | ||||
| Pretreatment | 811.80 (195.01) | 800.80 (201.48) | 863.09 (263.33) | |
| Posttreatment | 753.40 (200.63) | 707.09 (224.59) | 753.25 (237.99) | |
| RT-Neutral | ||||
| Pretreatment | 823.92 (211.23) | 822.41 (211.47) | 885.24 (244.41) | |
| Posttreatment | 738.25 (209.78) | 693.70 (245.83) | 749.95 (248.53) | |
| Bias Score | ||||
| Pretreatment | 12.11 (30.84) | 21.61 (65.35) | 22.15 (51.43) | F2,52 = 0.183 |
| Posttreatment | −15.15 (40.80) | −13.39 (48.13) | −3.30 (56.17) | F2,52 = 0.293 |
Note: ABMT = attention bias modification training; ACC = accuracy rates; ADIS = Anxiety Disorders Interview Schedule; CBT = cognitive behavioral therapy; RT = reaction time; SCARED = Screen for Child Anxiety Related Emotional Disorders, mean score of parent and child SCARED.
p < .05
p < .01.
Between-Group Differences After Treatment: Primary Outcomes
Symptom Frequency
The ANOVA on symptom frequency yielded a significant group-by-time interaction effect (F2,42 = 4.05, p = .025, partial η2 = 0.16) (Table 2 and Figure 2A). Follow-up contrasts revealed significant reductions in the average number of anxiety symptom counts after treatment in the ABMT + CBT group, t(13) = 5.22, p < .001 and the ABMT placebo + CBT conditions, t(16) = 6.27, p < .001, but only a trend in the CBT-alone group t(13) = 2.01, p = .06.
FIGURE 2.
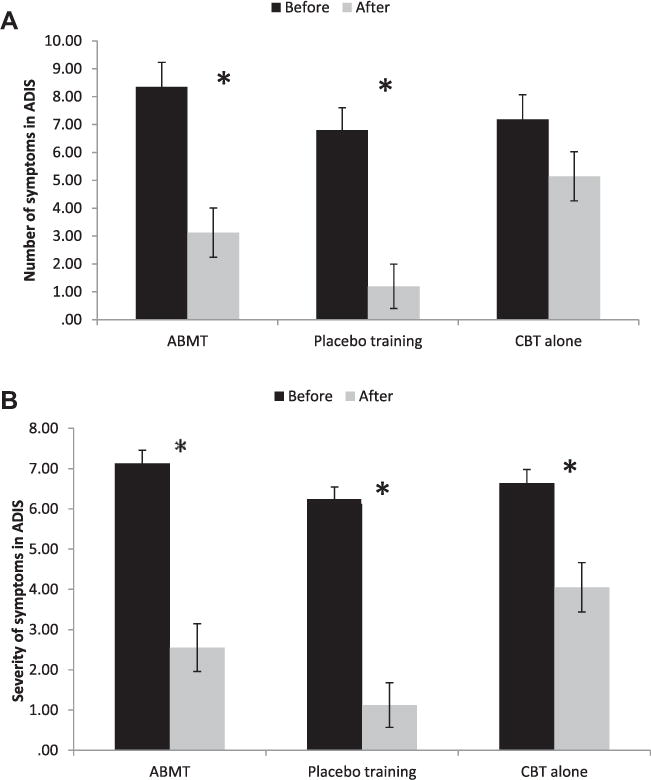
(A) Number of anxiety symptoms before and after treatment across the 3 treatment groups; (B) severity of anxiety symptoms before and after treatment across the 3 treatment groups. Note: CBT = cognitive behavioral therapy.
Symptom Severity
The ANOVA on symptom severity also revealed a significant group-by-time interaction (F2,40 = 3.66, p = .035, partial η2 = 0.155) (Table 2 and Figure 2B). However, unlike for symptom frequency, a significant reduction in symptom severity was noted across all 3 groups: ABMT + CBT, t(13) = 5.57, p < .001; ABMT placebo + CBT, t(15) = 9.91, p < .001; and the CBT-alone, t(12) = 3.60, p = .004, with a larger effect in the 2 ABMT groups than in the CBT-alone group, t(40) = 2.62, p = .012.
To control for possible age effect, the same analyses were conducted with age of participants as a covariate. The same results were observed for both the frequency and the severity of symptoms.
Between-Group Differences After Treatment: Secondary Outcomes
SCARED
The ANOVA on averaged SCARED total scores also yielded a significant time-by-group interaction (F2,52 = 5.52, p = .007, partial η2 = 0.175) (Table 2 and Figure 3). Follow-up contrasts indicated a significant reduction in symptoms only in the ABMT + CBT group (t[14] = 3.13, p = .007), with a trend in the ABMT placebo + CBT [t(21) = 1.99, p = .06], but no significant change in the CBT-alone group (t[17] = −0.75, p > .48).
FIGURE 3.
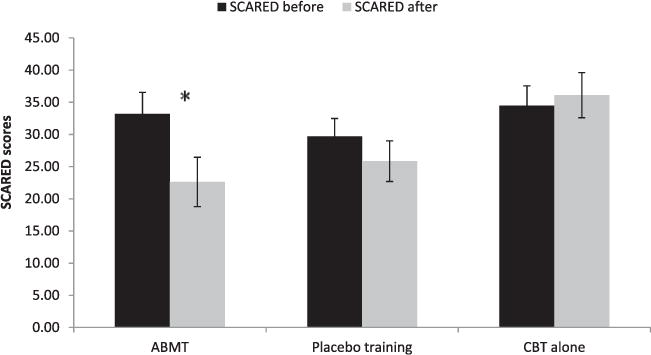
Screen for Child Anxiety Related Emotional Disorders (SCARED) scores before and after treatment across the 3 treatment groups. Note: CBT = cognitive behavioral therapy.
Finally, at the posttreatment assessment, the 3 groups differed in terms of their rates of an ongoing anxiety disorder (Table 2). No differences between the ABMT and the ABMT placebo groups were noted (χ2(1) = 0.03, p > .05). However, both the ABMT (χ2(1) = 4.99, p = .025) and the ABMT placebo groups (χ2(1) = 5.11, p = .024) differed from the CBT-alone group.
Intent-to-Treat Analysis
The intent-to-treat analysis results and the results obtained from the completers analyses reported thus far were similar. The ANOVA on symptom frequency yielded a significant group-by-time interaction effect (F2,44 = 3.24, p = .049, partial η2 = 0.13). Follow-up contrasts revealed significant reductions in the average number of anxiety symptom counts after treatment in the ABMT + CBT group (t[14] = 4.90, p < .001) and the ABMT placebo + CBT conditions (t[17] = 5.89, p < .001), but only a trend in the CBT-alone group (t[13] = 2.06, p = .06). The ANOVA for symptom severity revealed a trend for the group-by-time interaction effect (F2,42 = 2.57, p = .088, partial η2 = 0.11). A significant reduction in symptom severity was noted across all 3 groups (ABMT + CBT, t[14] = 5.18, p < .001; ABMT placebo + CBT, t[16] = 8.43, p < .001; and the CBT-alone, t[12] = 3.56, p = .004). The ANOVA on averaged SCARED total scores also yielded a significant time-by-group interaction (F2,59 = 5.16, p = .009, partial η2 = 0.15. Follow-up contrasts indicated a significant reduction in symptoms only in the ABMT + CBT group (t[16] = 3.02, p = .008), but no significant changes in the ABMT placebo + CBT, (t[24] = 1.67, p > .10) or in the CBT-alone groups (t[19] = −0.72, p > .48).
Between-Group Differences in Attention Bias Scores After Treatment
The ANOVA on attention bias scores yielded a significant main effect of time (F1 52 = 7.06, p = .010, partial η2 = 0.12), but no interaction effect with treatment condition (Table 2). Participants in all 3 groups started with mean attention bias toward threat (mean = 19.20, SD = 52.53), and this bias decreased in a similar fashion among all 3 groups after treatment (mean = −10.56, SD = 48.50). No correlation was found between participants’ age and accuracy levels on the dot– probe task. No correlations were found between attention bias scores and baseline anxiety symptoms. Furthermore, no significant correlations were found between pre- and posttreatment attention bias change scores and anxiety symptoms.
The ANOVA on attention bias scores that were computed using the novel set of stimuli at post-treatment yielded similar results. A significant main effect of time (F1,52 = 9.09, p = .004, partial η2 = 0.15), but no interaction effect with treatment condition. Participants in all 3 groups started with mean attention bias toward threat (mean = 19.20, SD = 52.53), and this bias decreased in a similar fashion among all 3 groups after treatment (mean = −15.58, SD = 58.52).
DISCUSSION
This study is the first RCT to examine the augmenting effects of threat-based ABMT on the widely used CBT protocol (Coping Cat) for pediatric anxiety. Three main findings emerged. First, both the active and placebo ABMT groups showed greater reductions in clinician-rated anxiety symptoms than the CBT-alone group. Second, group differences also emerged in self/parent-rated anxiety symptoms. However, unlike for clinician-rated anxiety, only the active ABMT group and neither of the other 2 groups showed a significant reduction on this self-/parent-rated measure. Finally, all 3 groups showed a shift in attention from a bias toward threat before treatment to a bias away from threat at posttreatment with no between-group differences.
Findings in the current study are both similar and different from findings in 4 other threat-related ABMT RCT studies in pediatric anxiety. As in 2 prior studies that used ABMT as a stand-alone therapy for pediatric anxiety, between-group difference emerged here for clinician-rated symptoms.6,7 However, unlike these prior studies, in the current study both groups receiving a dot–probe task showed greater treatment benefits compared to the CBT-alone group. Thus, the current findings differ from 2 prior studies of ABMT delivered as a stand-alone treatment, which found differences between active and placebo ABMT. Interestingly, a recent study trained severely anxious adolescents in addition to a standard care at a residential anxiety treatment facility.10 Similar to our results, both the active and the placebo ABMT conditions showed improvement as indicated by reductions on SCARED scores. Yet, unlike our results, the active ABMT group experienced a significantly greater decrease in anxiety symptoms than the ABMT placebo group. However, the study by Riemann et al. did not compare ABMT to a CBT-alone group. Moreover, although the standard care treatment was CBT oriented, it did not follow a structured CBT protocol. Of note, a fourth ABMT study trained clinically anxious children to attend to happy faces; this study, much like the current one, found similar beneficial effects on self-report (SCARED) in the active and placebo forms of happy-face–based ABMT, added to CBT.9 Taken together, when combined with the current findings, all 5 studies of ABMT in pediatric anxiety report some evidence of clinical benefit. Nevertheless, this benefit appears to vary as a function of outcome measure, study design, and sample size.
ABMT is thought to reduce anxiety through specific effects on threat bias patterns. However, aspects of the current study raise questions about the mechanism through which ABMT achieves these anxiety-reduction effects. In the current study, no group differences in attention bias manifested after treatment, and mean attention bias scores showed reductions from pre- to posttreatment in all 3 treatment groups. These changes in bias score after treatment were apparent not only when posttreatment bias score was measured using the same set of stimuli as in pretreatment but also when a new set of stimuli was used, indicating the generalization of this effect beyond the specific stimuli used in training. Changes in threat-related attention biases after stand-alone CBT were previously reported by others,23,24 and were also associated with better CBT outcomes.25,26 Thus, CBT may reduce threat biases to a considerable degree on its own. In addition, some studies in anxious adults demonstrate that training away from threat reduced threat-related attentional bias only temporarily.27 Similar to the method used in the current study, no differences in attention bias were noted between the training and the control group 1 week after training completion, and both groups reported reduction in anxiety symptoms. This CBT-induced change could create a floor effect that might obscure the capacity to detect any additional effect on attention bias between the group that received active ABMT training and the 2 other groups, all of which received the same CBT treatment. Lack of group differences in the current study could also reflect other limitations. For example, because of participant burden, the timing of posttreatment assessments varied, occurring anywhere from 0 to 2 weeks after the last CBT session. This variability could further reduce the sensitivity of the dot–probe task, which exhibits only modest reliability even under the best circumstances.9 In addition, although no differences in number of ABMT sessions were found between the ABMT-active and the ABMT-placebo groups, the large range and the variability in number of ABMT sessions across participants could have influenced the current results. In particular, because overall exposure to ABMT differed in the current study, relative to other studies, this could influence attempts to compare findings across studies. Finally, unlike previous studies (e.g., that of Eldar et al.6), we did not use pretreatment threat bias score as an inclusion criterion. Regardless, the current pattern of results could arise from various mechanisms, each producing reductions in anxiety symptoms, beyond a direct effect from ABMT on attention bias. It is important to consider such possibilities.
One possibility would be for clinical benefits from dot–probe training to emerge through effects on attention that are not measurable with sufficient sensitivity based on RT data. Available data suggest that neural or eye-movement indices may be more sensitive than RT measures.9,28 Another possibility is that enhanced clinical effects in the 2 ABMT groups reflect general placebo-type expectancy effects in these groups, over the CBT-alone group. Given that no between-groups differences in attention patterns were detected, the reduction in anxiety captured by the clinician-rated measures support such a possibility. Although plausible, this possibility is less consistent with the findings for the self/parent-report SCARED. Specifically, if patients’ expectancy of benefit is the major contributor to the observed clinical effects, one would predict that such effects would manifest more strongly in children’s and parents’ ratings, than in clinicians’ ratings. The opposite pattern manifested here. A third possibility is for clinical benefit of ABMT to accrue from mechanisms independent of changes in attention bias. Nevertheless, such a conclusion is inconsistent with findings in other ABMT studies reporting an association between dot–probe performance and clinical outcome.3 Fourth, ABMT, much like other forms of computer training, could produce increased proficiency in diverse forms of attention control and flexibility. These nonspecific effects could reduce anxiety, accounting for the observed differences between the CBT-alone and the 2 ABMT groups. Finally, the mere exposure to aversive faces included in both the ABMT tasks may contribute to anxiety reduction. As with conclusions on the overall robustness of the ABM’s clinical effect, definitive conclusions on potential mechanism of change will have to await results from future studies designed to evaluate the plausibility of each mechanism.
Other aspects of the current study are important to consider in light of other ABMT work. For example, CBT effects in the current study were rather weak (~70% of the children still met anxiety criteria after treatment), relative to those reported in prior studies using similar CBT procedures (~40% of children).14,20,29 This effect is surprising, given that the CBT delivered in the current study followed a standardized 16-session protocol (“Coping Cat”) and may reflect the state of affairs in public hospital–based child anxiety clinics. Furthermore, participants were randomly assigned to 1 of the 3 groups, using the same set of clinicians for all groups and providing identical treatments in the 3 conditions. The fact that therapists were not completely blinded to the CBT-alone group, in which no computer task was delivered, could have had some degree of unintentional effect on the way in which they delivered CBT to the ABMT-training and placebo groups compared to the CBT-alone group. The presence of such bias, for example, could account for some findings where the 2 ABMT groups both exhibited greater improvements than the CBT-alone group, although it cannot account for the other differences that were observed for the 2 ABMT groups. Nevertheless, the current study was primarily designed to examine the effects of ABMT, and monitoring the consistency of CBT implementation across the 3 groups was not applied with the same level of care as in prior research with the primary goal of examining CBT efficacy. Thus, undetected differences in CBT procedures used in the current study, compared to other studies, also could explain the relatively low response rate in the current study. In addition, because of technical difficulties in running the computerized dot–probe task and other demands of treatment, only about half of the therapeutic sessions actually included ABMT training or placebo. Similarly, the dot–probe task was delivered by therapists at any given time during the session, according to their clinical judgment. Variability in delivery time of the dot–probe across sessions and across therapists could have some effect on treatment outcomes. Finally, findings from the current study should be considered in light of the relatively small groups that may contribute to low statistical power as well as the heterogeneous groups of diagnoses that were included here. Of note, although the nature of a child’s diagnosis did not moderate outcome in the current study, small sample size also would have limited the power on such tests of treatment moderation.
Despite the above-described limitations, results from this RCT suggest that active and placebo ABMT augments response to standard CBT. This study adds to the growing ABMT literature, laying the grounds for future work that should focus further on examining the most effective ABMT protocol and the most efficient way to implement these as augmenting treatments to CBT, and clarifying the cognitive mechanisms underlying the anxiolytic effect of ABMT.
Clinical Guidance.
Threat-related attention biases are implicated in the etiology and the maintenance of anxiety disorders. In recent years, a novel computer-based task designed to implicitly train anxious patients to shift attention from minor threats was found to be beneficial in reducing anxiety.
This randomized controlled trial (RCT) examined the augmenting effects of attention bias modification treatment on cognitive behavioral therapy (CBT) in clinically anxious youth.
Findings from this study indicate that patients who performed a visual attention task as part of a CBT session showed greater reductions in clinician-rated anxiety symptoms than the CBT-alone group. In addition, a certain training protocol of this task intended to train patients’ attention away from minor threat was found to be particularly beneficial in reducing self-reported anxiety symptoms.
The results of this study corroborate findings from other recent studies demonstrating the potential clinical gains associated with implicit attention training in augmenting CBT for anxiety disorders.
Acknowledgments
This study was partially supported by a grant from the Adler Center for Research in Child Development and Psychopathology to Dr. Bar-Haim and by the National Institutes of Health intramural research program.
Footnotes
Disclosure: Drs. Shechner, Britton, Apter, Bliese, Pine, and Bar-Haim, and Ms. Rimon-Chakir and Mr. Lotan report no biomedical financial interests or potential conflicts of interest.
References
- 1.Bar-Haim Y. Attention bias modification (ABM): a novel treatment for anxiety disorders [research review] J Child Psychol Psychiatry. 2010;51:859–870. doi: 10.1111/j.1469-7610.2010.02251.x. [DOI] [PubMed] [Google Scholar]
- 2.Bar-Haim Y, Lamy D, Pergamin L, Bakermans-Kranenburg MJ, van IMH. Threat-related attentional bias in anxious and nonanxious individuals: a meta-analytic study. Psychol Bull. 2007;133:1–24. doi: 10.1037/0033-2909.133.1.1. [DOI] [PubMed] [Google Scholar]
- 3.Amir N, Beard C, Taylor CT, et al. Attention training in individuals with generalized social phobia: a randomized controlled trial. J Consult Clin Psychol. 2009;77:961–973. doi: 10.1037/a0016685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hakamata Y, Lissek S, Bar-Haim Y, et al. Attention bias modification treatment: a meta-analysis toward the establishment of novel treatment for anxiety. Biol Psychiatry. 2010;68:982–990. doi: 10.1016/j.biopsych.2010.07.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schmidt NB, Richey JA, Buckner JD, Timpano KR. Attention training for generalized social anxiety disorder. J Abnorm Psychol. 2009;118:5–14. doi: 10.1037/a0013643. [DOI] [PubMed] [Google Scholar]
- 6.Eldar S, Apter A, Lotan D, et al. Attention bias modification treatment for pediatric anxiety disorders: a randomized controlled trial. Am J Psychiatry. 2012;169:213–220. doi: 10.1176/appi.ajp.2011.11060886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Waters AM, Pittaway M, Mogg K, Bradley BP, Pine DS. Attention training towards positive stimuli in clinically anxious children. Dev Cogn Neurosci. 2013;4:77–84. doi: 10.1016/j.dcn.2012.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bar-Haim Y, Morag I, Glickman S. Training anxious children to disengage attention from threat: a randomized controlled trial. J Child Psychol Psychiatry. 2011;52:861–869. doi: 10.1111/j.1469-7610.2011.02368.x. [DOI] [PubMed] [Google Scholar]
- 9.Britton JC, Bar-Haim Y, Clementi MA, et al. Training-associated changes and stability of attention bias in youth: implications for attention bias modification treatment for pediatric anxiety. Dev Cogn Neurosci. 2013;4:52–64. doi: 10.1016/j.dcn.2012.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Riemann BC, Kuckertz JM, Rozenman M, Weersing VR, Amir N. Augmentation of youth cognitive behavioral and pharmacological interventions with attention modification: a preliminary investigation. Depress Anxiety. 2013;30:822–828. doi: 10.1002/da.22127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Macleod C, Mathews A, Tata P. Attentional bias in emotional disorders. J Abnorm Psychol. 1986;95:15–20. doi: 10.1037//0021-843x.95.1.15. [DOI] [PubMed] [Google Scholar]
- 12.Amir N, Taylor CT. Combining computerized home-based treatments for generalized anxiety disorder: an attention modification program and cognitive behavioral therapy. Behav Ther. 2012;43:546–559. doi: 10.1016/j.beth.2010.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shechner T, Britton JC, Perez-Edgar K, et al. Attention biases, anxiety, and development: toward or away from threats or rewards? Depress Anxiety. 2012;29:282–294. doi: 10.1002/da.20914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Walkup JT, Albano AM, Piacentini J, et al. Cognitive behavioral therapy, sertraline, or a combination in childhood anxiety. N Engl J Med. 2008;359:2753–2766. doi: 10.1056/NEJMoa0804633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Storch EA, Murphy TK, Goodman WK, et al. A preliminary study of D-cycloserine augmentation of cognitive-behavioral therapy in pediatric obsessive-compulsive disorder. Biol Psychiatry. 2010;68:1073–1076. doi: 10.1016/j.biopsych.2010.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Albano AM, Silverman WK. The Anxiety Disorders Interview Schedule for Children for DSM-IV: Clinician Manual (Child and Parent Versions) San Antonio, TX: Psychological Corporation; 1996. [Google Scholar]
- 17.Silverman WK, Saavedra LM, Pina AA. Test-retest reliability of anxiety symptoms and diagnoses with the Anxiety Disorders Interview Schedule for DSM-IV: child and parent versions. J Am Acad Child Adolesc Psychiatry. 2001;40:937–944. doi: 10.1097/00004583-200108000-00016. [DOI] [PubMed] [Google Scholar]
- 18.Birmaher B, Brent DA, Chiappetta L, Bridge J, Monga S, Baugher M. Psychometric properties of the Screen for Child Anxiety Related Emotional Disorders (SCARED): a replication study. J Am Acad Child Adolesc Psychiatry. 1999;38:1230–1236. doi: 10.1097/00004583-199910000-00011. [DOI] [PubMed] [Google Scholar]
- 19.Tottenham N, Borscheid A, Ellertsen K, Marcus DJ, Nelson CA. Categorization of facial expressions in children and adults: establishing a larger stimulus set. J Cogn Neurosci Apr. 2002:74–74. [Google Scholar]
- 20.Kendall PC. Treating anxiety disorders in children: results of a randomized clinical trial. J Consult Clin Psychol. 1994;62:100–110. doi: 10.1037//0022-006x.62.1.100. [DOI] [PubMed] [Google Scholar]
- 21.Kendall PC, Southam-Gerow MA. Long-term follow-up of a cognitive-behavioral therapy for anxiety-disordered youth. J Consult Clin Psychol. 1996;64:724–730. doi: 10.1037//0022-006x.64.4.724. [DOI] [PubMed] [Google Scholar]
- 22.Kendall PC, Gosch E, Furr JM, Sood E. Flexibility within fidelity. J Am Acad Child Adolesc Psychiatry. 2008;47:987–993. doi: 10.1097/CHI.0b013e31817eed2f. [DOI] [PubMed] [Google Scholar]
- 23.Mathews A, Mogg K, Kentish J, Eysenck M. Effect of psychological treatment on cognitive bias in generalized anxiety disorder. Behav Res Ther. 1995;33:293–303. doi: 10.1016/0005-7967(94)e0022-b. [DOI] [PubMed] [Google Scholar]
- 24.Mogg K, Bradley BP, Millar N, White J. A follow-up study of cognitive bias in generalized anxiety disorder. Behav Res Ther. 1995;33:927–935. doi: 10.1016/0005-7967(95)00031-r. [DOI] [PubMed] [Google Scholar]
- 25.Legerstee JS, Tulen JH, Dierckx B, Treffers PD, Verhulst FC, Utens EM. CBT for childhood anxiety disorders: differential changes in selective attention between treatment responders and non-responders. J Child Psychol Psychiatry. 2010;51:162–172. doi: 10.1111/j.1469-7610.2009.02143.x. [DOI] [PubMed] [Google Scholar]
- 26.Waters AM, Mogg K, Bradley BP. Direction of threat attention bias predicts treatment outcome in anxious children receiving cognitive-behavioural therapy. Behav Res Ther. 2012;50:428–434. doi: 10.1016/j.brat.2012.03.006. [DOI] [PubMed] [Google Scholar]
- 27.Reese HE, McNally RJ, Najmi S, Amir N. Attention training for reducing spider fear in spider-fearful individuals. J Anxiety Disord. 2010;24:657–662. doi: 10.1016/j.janxdis.2010.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Shechner T, Jarcho JM, Britton JC, Leibenluft E, Pine DS, Nelson EE. Attention bias of anxious youth during extended exposure of emotional face pairs: an eye-tracking study. Depress Anxiety. 2013;30:14–21. doi: 10.1002/da.21986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kendall PC, Flannery-Schroeder E, Panichelli-Mindel SM, Southam-Gerow M, Henin A, Warman M. Therapy for youths with anxiety disorders: a second randomized clinical trial. J Consult Clin Psychol. 1997;65:366–380. doi: 10.1037//0022-006x.65.3.366. [DOI] [PubMed] [Google Scholar]


