Abstract
Introduction:
Cervical cancer is one of the most common causes of death in women worldwide.[1] The introduction of cervical cytology in screening programs is an effective way for early detection and treatment of cervical precancerous lesions. Conventional screening of cervical cytology slides is still considered the current “gold standard” for the assessment of proficiency in becoming a cytotechnician, but diagnosis using digital whole slide images (WSI) may offer many advantages.
Materials and Methods:
In this study, we have used a selection of WSI from thin-layer specimens of the most common cervical infections and (pre) neoplastic lesions, and hypothesized that weekly WSI based case-meetings would help to obtain optimal acceptance of the new digital workflow in daily pathology practice. A questionnaire, before and after the test period was used to study the effect of our approach.
Results:
The participants clearly had to go through a learning curve to get accustomed to viewing WSI. In the beginning, there was a little self-confidence in recognizing classical cervical cytomorphological features in the WSI, and there were complaints about the speed of viewing and insufficient Z-resolution for cell groups. Adjusting the Z-stack settings resulted in better three-dimensional information due to better focusing options. Weekly meetings appeared to be instrumental in the implementation process, as participants had to select and present WSI from thematic cases themselves, and thereby, got used to viewing WSI. Some WSI were replaced by better ones until a final set of 45 representatives WSI remained. Eventually, the consensus was reached among all participants that cytomorphological features in WSI from thin-layers cervical specimens could comparably be appreciated in WSI as by conventional microscopy. The selection of 45 WSI was now used to create a digital WSI based reference atlas to support further studies.
Conclusion:
We have obtained consensus between professionals that WSI from cervical cytology can be used to identify cytomorphological features, necessary for diagnosis. In addition, we observed that active participation of professionals had a positive effect on the overall acceptance of WSI and was important in the change management.
Keywords: Cervical cytology, digital pathology reference atlas, education, implementation, whole slide images
INTRODUCTION
The development of fast and high-resolution slide scanners and viewing software has enabled viewing digital whole slide images (WSI) on a computer screen next to the traditional viewing under the microscope.[2,3,4] WSI has already been implemented in different fields of pathology,[3,5] mostly in histology, where WSI are used in tele-consultations for difficult cases, slide conferences and panels, tele-revision and quality assurance, frozen sections diagnosis, and image analysis.[3,6] In addition, several validation studies have recently investigated the possibility of introducing WSI in primary histological diagnostics.[6,7,8,9] However, for cytology, there is only a limited number of studies available that investigated, whether it is possible to use WSI in primary diagnostics of cytology specimens,[10,11,12,13] and even fewer comparing WSI based cervical cytodiagnostics with conventional thin-layer cytodiagnostics.[10,13] These studies suggested that WSI may potentially replace the conventional microscope.[11,12,13] However, there are also limitations such as long scanning time, focus problems due to the often used single focus plane (even in thin-layer specimens), huge storage requirements, and high initial costs.[13,14,15] Perhaps even more importantly are the human limitations such as the reluctance to rely on making a diagnosis, often requiring subtle high-resolution cytological features, on a digital image with its inherent limitations.[4]
Primary WSI based diagnostics would, however, provide opportunities for cytotechnicians (CT) and cytopathologists to do their work on remote sites, having the opportunity to easily tele-consult with other professionals around the globe. Particularly, in parts of the world where there is a shortage of professionals in (cyto)-pathology, WSI can provide a solution by remote diagnosis. In addition, WSI offers the possibility to duplicate, catalog, manage, or save representative images for training purposes, accessible by multiple users at the same time over the internet without deterioration of image quality.[10] Finally, quality assurance can easily be achieved using an independent external cytopathologist.[4] Before introducing digital cytology in primary diagnosis, two major issues have to be addressed. The most important is the establishment of consensus that the cytomorphological features in WSI can be recognized in a similar way as by conventional microscopy. The second might be the change management.[16,17] Changing existing work procedures usually evokes resistance, the question is how to cope with this. Conventional screening of cervical cytology slides is still considered the current “gold standard” for the assessment of proficiency in becoming a CT. Cervical cytology might, therefore, be an excellent source to investigate these aspects.
A selection of classical examples from the most common cervical infections and (pre) neoplastic lesions was used to create a collection of WSI that could serve as a support in our discussions toward a possible consensus. We hypothesized that weekly WSI based case-meetings with the active participation of all members of our diagnostic staff would help to obtain optimal acceptance of digital images as a support in daily pathology practice.
MATERIALS AND METHODS
Technical Information
The thin-layer slides of the cervix were selected from the archive of the Atrium Medical Center, Heerlen, The Netherlands. They were completely digitized using 3DHistech 250 flash II scanner (www.3dhistech.com, 3dhistech Kft. Hungary). The imaging system consists of a CIS VCC-FC60 FR 19 CL camera and a 20x objective (numerical aperture 0.8), using a camera/adapter magnification of 1.6 and quality factor of 70 (jpeg image compression). At the beginning of the case-meetings, three of the 45 cases were scanned with Z-stack application. Initially, the focus range was set with 1 μm Z-stacks made by scanning at seven levels (three levels up and down from the central plane). During the process, it became clear that the resolution of the Z-stack did not provide enough information. From that point onward, we changed the Z-stack levels into 2 μm scanning at seven levels. Twenty of the 45 cases were scanned with this approach. The storage of one thin-prep cervical slide scanned at one plane was between 400 Mb and 600 Mb. The average scan time for thin-prep cervical slides is 1 min. 30 s. When there was a Z-stack scan (scanning at different planes) needed for a thin-prep cervical slide, the storage was between the 2 GB and 4 GB and the average scan time was 24 min. WSI were displayed at the workspace of the participants on an HD computer screen (HP 23-inch 1920 × 1080 LCD color monitor) and viewed with the Pannoramic Viewer (3DHistech Kft, Budapest, Hungary). The high-resolution reference images from selected annotations (see below) were taken using the Pannoramic snapshot tool.
Participants
Of the 12 participants, four were pathologists, seven were CTs, and one pathology resident. Within the time frame of the study, the residents succeed each other and at some meetings even two residents participated. From the nonresidental participants, eight were females and three were males. The CTs were aged 25–63 years, all were certified in gynecological and nongynecological cytology and had more than 5 years experience in conventional screening of cervical cytology. The four pathologists were 40–60 years and the residents were 27–35 years.
Organizing the Textual and Image Information as a Reference Atlas
To structure our weekly consensus meetings, a category list with the most common cytomorphological features of cervical infections and lesions was composed based on www.cytologystuff.com [Table 1]. Each category contains subcategories with tables and with descriptions of the specific cytomorphological features and links to WSI of a specific subject. From our archive, from the period 2008–2014 cervical thin-layer specimens, representative cases were selected based on local searches in the PALGA system,[18] and representative snapshots from annotations were taken from WSI as described above. The images were ordered in a logical fashion again according to www.cytologystuff.com [Figure 1] and categorized in the tables with a related description of the specific cytological features. The snapshot images contained hyperlinks to their original WSI. The images and cervix reference atlas were available on a central shared partition of a hard disk.
Table 1.
The category list with the most common cytomorphological features
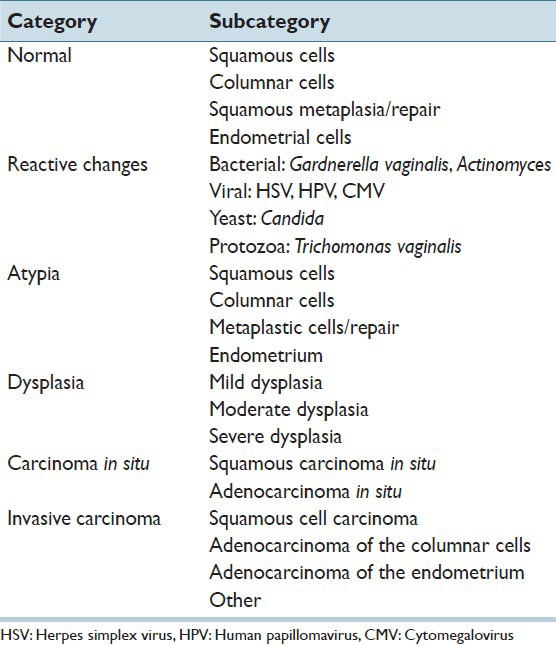
Figure 1.
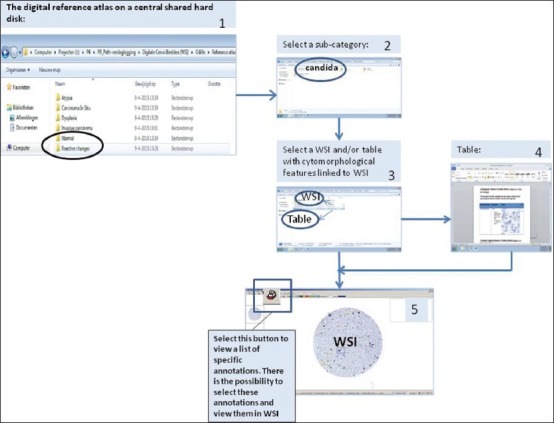
The work instructions to get access to whole slide images in the digital reference atlas on a central shared hard disk: (1) Select a subject from the topic list. (2) Choose a subcategory. (3) The possibility to view whole slide images directly or to open the table with the description of the specific cytological features. (4) After choosing the table, hyperlinks in the table can be activated. (5) The viewer opens the whole slide images. In the viewer, it is possible to open a box with annotations. Specific features can be viewed in the whole slide image
In the digital WSI reference atlas that was created in this way, for each subject of interest there are three possibilities. The first is displaying textual information about cervical cytology subjects in plain text or structured tables, the second is viewing cytomorphological features in the snapshots taken from annotated diagnostic items, included in the Word Document (Microsoft Corporation, Redmond, United States of America) and the third possibility is using hyperlinks in the texts or snapshot images to enter the original WSI. The difference between this approach and other digital reference material is that one can directly approach the cells of interest within the context of the whole slide [Figure 2].
Figure 2.
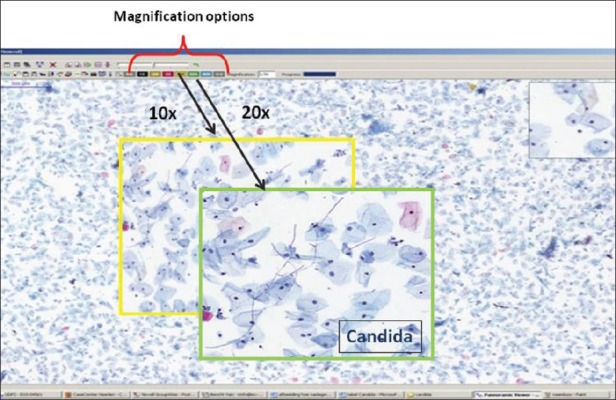
Whole slide images: After selecting a whole slide images or link in the specific table, it is possible to view the morphological features with the viewer in the whole slide image with different magnification
Change Management and User Satisfaction Analysis
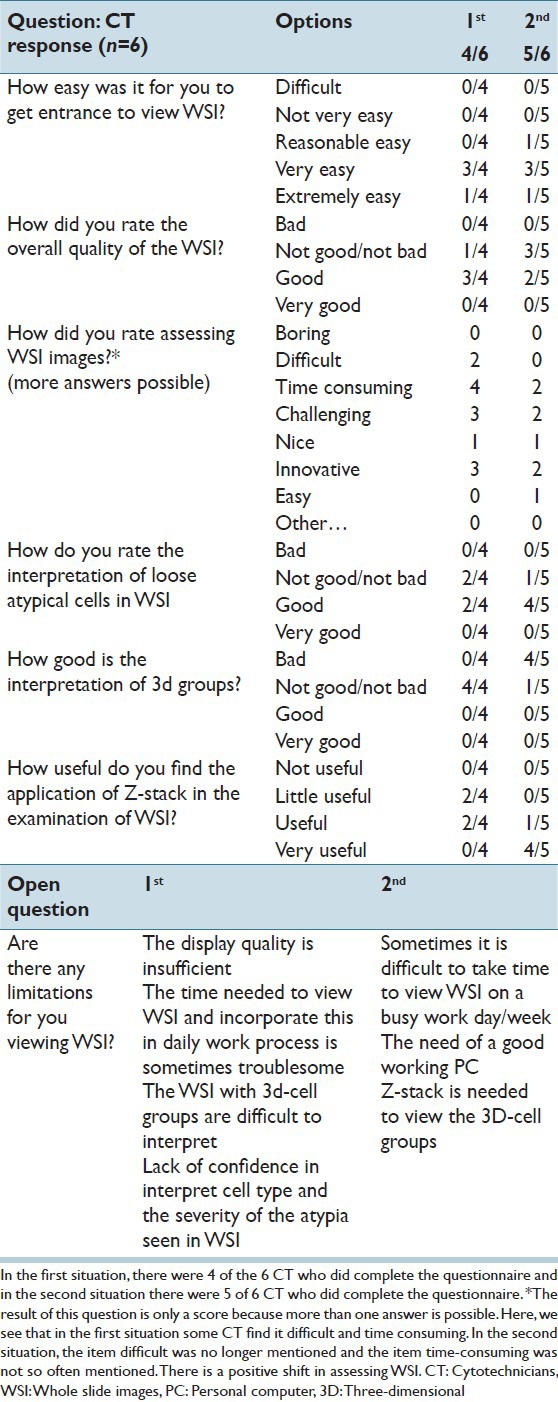
After constructing the WSI reference material, we initiated weekly meetings in which seven CTs, four Pathologists, and a Pathology Resident of the Atrium Medical Center participated. Representative cytomorphological features in the WSI that had been annotated before were presented on a 70-inch full HD screen and discussed. The CT took turns in preparing and presenting cases. For each case, it was discussed whether the cytomorphological features as previously seen in the thin-layer slides could also be recognized in the WSI. At the beginning of viewing WSI, the participants were asked to report their perceptions of viewing WSI of the cervix by completing a questionnaire [Table 2]. We collected information about how easy it was for them to get access to viewing WSI, the quality of the WSI, how they liked viewing WSI, how specific cytological features could be appreciated in WSI and whether the Z-stacks were useful.
Table 2.
The results of the questionnaire for CT: WSI users satisfaction analysis
After the implementation period, the participants were asked to report their perceptions again using the same questionnaire.
RESULTS
Organizing the Textual and Image Information as a Reference Atlas
The organization of text data with direct hyperlinks to WSI appeared successful and was accepted by all participants as a useful support in the consensus meeting. Snapshots from relevant annotations in the WSI were incorporated as additional teasers in the text to prompt the users to open the hyperlink to the WSI as well. The tools available in the different software components allowed easy processing. The final document and WSI files were stored as a “read only file” in a shared partition on a central hard disk that allowed access from participants.
The realization of the weekly cytology consensus WSI meetings was appreciated and resulted in an active participation in both presentation and discussion. Although at first the presentations by the CTs were done with some hesitation, the atmosphere was one of the open discussions and both pathologists and technicians, as well as residents, were actively invited by the chairperson to describe the features shown on screen and give their arguments and opinions for discussion. Based on these discussions, during the weekly meetings, some cases were replaced by more illustrative cases. After consensus was reached on the identification of diagnostic characteristics, marked with annotations in the WSI, finally, 45 cases remained.
User Satisfaction Analysis
During the kick-off WSI discussion meetings, the following objections were put forward [Table 2]: The time needed for viewing WSI was too long, misinterpretations of cells, or features in WSI resulted in lack of self-confidence, some WSI were produced from too thick thin-layer slides resulting in cells at different focus levels that were difficult to interpret, since focusing was not easy. At the end of the 45 cases discussion meetings, the questionnaire revealed that the time needed for viewing WSI still was too long, but the interpretation of loose atypical cells was now good, and the application of Z-stack appeared to be very useful in some cases for the interpretation of three-dimensional (3D) cell groups and cells at different focus levels.
Viewing time could not be further optimized at the time, but the Z-stack settings got changed from 1 μm to 2 μm, which resulted in better 3D information due to better focusing options in scans where cells lay at different levels.
We interpreted the changes between the first and second questionnaire among the CT's as a positive development particularly, because the item on the assessment showed a shift toward a higher level of acceptance. Eventually, there was a consensus among the participants that the cytomorphological features in WSI from thin-layers cervical slides could comparably be appreciated in WSI as by conventional microscopy. At this point, we could see that part of the resistance to change had been resolved, and participants were willing to further investigate if viewing time could be influenced by training.
DISCUSSION
While validation of digital diagnostics on WSI from tissue sections is rapidly advancing,[6,9] little work had been done on WSI from cytological specimens. In the present study, we reached consensus between the professionals about the conventional and digital cervical cytomorphological features during weekly discussion meetings with a fixed pool of participating CTs, pathologists, and residents. In these consensus case-meetings based on 45 selected cervical thin-layer slides with specific subjects feedback was obtained, which helped to make a digital WSI based reference atlas.
The specific advantage of a WSI based reference atlas, which originated as a result of the consensus meeting, is that the specific cytomorphological features first presented as high-resolution images are linked to WSI, where the specific cells or features can be viewed within the context of the full thin-layer specimen. This brings the learning environment much closer to daily clinical practice.
The participants clearly had to go through a learning curve to get accustomed to viewing WSI. In the beginning, there was little self-confidence in recognizing classical cervical cytomorphological features in the WSI, and there were complaints about the speed of viewing and insufficient Z-resolution for groups in some cases. There was not much that could be done with regard to viewing time, but adjusting the Z-stack settings resulted in better 3D information due to better focusing options. The space between surface glass and the glass (slide) of a cervical thin-layer slide is 29.5 μm as earlier demonstrated[14] and there is still no information about optimal number of scan layers or of an optimal spacing between them.[14] The settings of the Z-stack at the beginning of the case-meetings revealed just a scanning range of 7 μm and spacing of 1 μm. This range was too small to give enough focus of the cells at different levels. The adjustment of the Z-stack settings into seven levels of 2 μm resulted in a scanning range of 14 μm, which was acceptable in practically all situations. If we assume that the most likely plane of focus for most cells is at or slightly above the upper surface of the object glass and that focusing 3D groups will need a shift downward of the microscope stage, the Z-stack could be limited to one side of the average plane of focus. This will reduce the time and storage by almost 50%, which is an important issue in a routine diagnostic setting.
Fine tuning of the Z-stack settings for the optimal amount of scan layers and scan space for cervical thin-layer slides and comparing the Z-stack settings with different scanners will be subject of discussion with the software development team from the supplier 3DHistech.
The weekly meeting appeared to be instrumental in the implementation process. Every participant in turn presented a case with a specific subject from the reference atlas. This urged the participants to scrutinize the WSI for the most important cytomorphological features and present those to the other participants. Thereby, the participants got used to viewing WSI and self-confidence increased, as often it turned out that most of the WSI did provide relevant cytomorphological features. An important finding was the need to search for loose atypical cells beside 3D cell groups in case of suspected dysplasia or worse, since the finding of loose severe dysplastic cells is sufficient to diagnose severe dysplasia and the need to interpret the 3D groups by intensive focusing becomes less. Based on the feedback, some WSI were discarded for better ones until a final set of 45 representatives WSI remained. Eventually, as evident from the case meetings, participants agreed that cytomorphological features in WSI from thin-layer cervical slides could comparably be appreciated in WSI and by conventional microscopy. These meetings thereby were an important change management tool. It is indeed known that if change does not contribute to the interests of the participants than the preparedness of the participants to change is low.[17] Yet, several improvements to the digital WSI based reference atlas are needed. Viewing speed should be optimized, perhaps by faster network connections, and faster graphics speed of the computers, and more user-friendly viewer interaction devices.
Further investigations are needed to test whether an adjusted Z-stack setting will improve viewing of WSI from the thin-layer cytological material.
CONCLUSION
We reached consensus among professionals about the possibility of the identification of classical cervical cytomorphological characteristics in WSI. As a side effect of the consensus case meetings, we have created a structured digital reference atlas that we transferred in www.ex-pathcytology.com a digital WSI web-based reference atlas for the most common lesions and abnormalities in thin-layer specimens of the cervix, which can be useful for training purposes, during diagnosis or supportive for further studies [Figure 3]. Further studies will focus on validation of our reference approach before we eventually can incorporate it in our daily routine.
Figure 3.
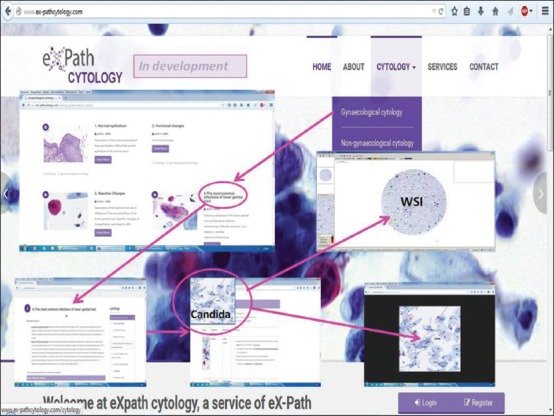
www.ex-pathcytology.com in development: In this website based reference atlas it is possible to find the cytomorphological features of the most common lesions and abnormalities in thin-layer specimens of the cervix and to view them in whole slide images
Financial Support and Sponsorship
Nil.
Conflicts of Interest
There are no conflicts of interest.
Acknowledgments
We would like to thank the next persons who did participate in the WSI case-meetings: Dr. Ruud Clarijs, Dr. Paul Theunissen, Drs. Nathalie Vandevijver, Carla Clevers CT, Marij Debets CT, Daniëlle Paffen CT, Lisanne Senden CT, Linda Ruiten CT, Kim Rijks CT. The residents: Marjolein Beer-Lentjes, Lisa Hillen, Jan Koster, Michiel van der Horst.
Footnotes
Available FREE in open access from: http://www.jpathinformatics.org/text.asp?2015/6/1/52/166013
REFERENCES
- 1.World Health Organisation. [Last updated on 2015 Mar 15]. Available from: http://www.who.int .
- 2.Weinstein RS, Graham AR, Lian F, Braunhut BL, Barker GR, Krupinski EA, et al. Reconciliation of diverse telepathology system designs. Historic issues and implications for emerging markets and new applications. APMIS. 2012;120:256–75. doi: 10.1111/j.1600-0463.2011.02866.x. [DOI] [PubMed] [Google Scholar]
- 3.Pantanowitz L, Sinard JH, Henricks WH, Fatheree LA, Carter AB, Contis L, et al. Validating whole slide imaging for diagnostic purposes in pathology: Guideline from the College of American Pathologists Pathology and Laboratory Quality Center. Arch Pathol Lab Med. 2013;137:1710–22. doi: 10.5858/arpa.2013-0093-CP. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Thrall M, Pantanowitz L, Khalbuss W. Telecytology: Clinical applications, current challenges, and future benefits. J Pathol Inform. 2011;2:51. doi: 10.4103/2153-3539.91129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brachtel E, Yagi Y. Digital imaging in pathology – Current applications and challenges. J Biophotonics. 2012;5:327–35. doi: 10.1002/jbio.201100103. [DOI] [PubMed] [Google Scholar]
- 6.Al-Janabi S, Huisman A, Van Diest PJ. Digital pathology: Current status and future perspectives. Histopathology. 2012;61:1–9. doi: 10.1111/j.1365-2559.2011.03814.x. [DOI] [PubMed] [Google Scholar]
- 7.Ordi J, Castillo P, Saco A, Del Pino M, Ordi O, Rodríguez-Carunchio L, et al. Validation of whole slide imaging in the primary diagnosis of gynaecological pathology in a University Hospital. J Clin Pathol. 2015;68:33–9. doi: 10.1136/jclinpath-2014-202524. [DOI] [PubMed] [Google Scholar]
- 8.Bauer TW, Schoenfield L, Slaw RJ, Yerian L, Sun Z, Henricks WH. Validation of whole slide imaging for primary diagnosis in surgical pathology. Arch Pathol Lab Med. 2013;137:518–24. doi: 10.5858/arpa.2011-0678-OA. [DOI] [PubMed] [Google Scholar]
- 9.van der Post RS, van der Laak JA, Sturm B, Clarijs R, Schaafsma HE, van Krieken JH, et al. The evaluation of colon biopsies using virtual microscopy is reliable. Histopathology. 2013;63:114–21. doi: 10.1111/his.12131. [DOI] [PubMed] [Google Scholar]
- 10.Evered A, Dudding N. Accuracy and perceptions of virtual microscopy compared with glass slide microscopy in cervical cytology. Cytopathology. 2011;22:82–7. doi: 10.1111/j.1365-2303.2010.00758.x. [DOI] [PubMed] [Google Scholar]
- 11.Gerhard R, Teixeira S, Gaspar da Rocha A, Schmitt F. Thyroid fine-needle aspiration cytology: Is there a place to virtual cytology? Diagn Cytopathol. 2013;41:793–8. doi: 10.1002/dc.22958. [DOI] [PubMed] [Google Scholar]
- 12.Wright AM, Smith D, Dhurandhar B, Fairley T, Scheiber-Pacht M, Chakraborty S, et al. Digital slide imaging in cervicovaginal cytology: A pilot study. Arch Pathol Lab Med. 2013;137:618–24. doi: 10.5858/arpa.2012-0430-OA. [DOI] [PubMed] [Google Scholar]
- 13.Steinberg DM, Ali SZ. Application of virtual microscopy in clinical cytopathology. Diagn Cytopathol. 2001;25:389–96. doi: 10.1002/dc.10021. [DOI] [PubMed] [Google Scholar]
- 14.Lahrmann B, Valous NA, Eisenmann U, Wentzensen N, Grabe N. Semantic focusing allows fully automated single-layer slide scanning of cervical cytology slides. PLoS One. 2013;8:e61441. doi: 10.1371/journal.pone.0061441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Khurana KK. Telecytology and its evolving role in cytopathology. Diagn Cytopathol. 2012;40:498–502. doi: 10.1002/dc.22822. [DOI] [PubMed] [Google Scholar]
- 16.Homan TP. Veranderen als chaotic process. In: Change management Box. Main Press BV. 2009:39. [Google Scholar]
- 17.van den Akker T. First release. Zaltbommel NL: Van Haren; 2012. Verandermanagement. [Google Scholar]
- 18.The Nationwide Network and Registry of Histo en Cytopathology in the Netherlands. PALGA. [Last updated on 2015 Aug 24]. Available from: http://www.palga.nl .


