Abstract
Epithelial ovarian cancer is the fifth leading cause of cancer-related deaths in women and the most lethal gynecological malignancy. Extracellular matrix (ECM) is an integral component of both the normal and tumor microenvironment. ECM composition varies between tissues and is crucial for maintaining normal function and homeostasis. Dysregulation and aberrant deposition or loss of ECM components is implicated in ovarian cancer progression. The mechanisms by which tumor cells induce ECM remodeling to promote a malignant phenotype are yet to be elucidated. A thorough understanding of the role of the ECM in ovarian cancer is needed for the development of effective biomarkers and new therapies.
Keywords: extracellular matrix, ovarian cancer, proteases, collagen, proteoglycan
Introduction
Epithelial ovarian cancer (EOC) is currently the most lethal gynecological malignancy affecting women and the fifth leading cause of cancer-related deaths in the United States (1). Early diagnosis of EOC grants a favorable prognosis and an average 5-year survival rate of 92%. However, due to the lack of available screening tests (2), diagnosis of patients is predominantly made at an advanced stage, reducing the average 5-year survival rate to only 27% (3). Standard treatment has not significantly improved for decades. The tumor microenvironment is gaining recognition in facilitating cancer progression, playing an essential role in mediating the growth, invasion, and metastasis of malignant tumors and therefore represents an attractive therapeutic target in solid tumors, including EOC. The tumor microenvironment consists of a variety of cell types including fibroblasts, immune cells, and endothelial cells, as well as non-cellular components such as the extracellular matrix (ECM), ECM remodeling enzymes [e.g., matrix metalloproteinases (MMPs), tissue inhibitors of metalloproteinases (TIMPs), and lysyl oxidases (LOXs)], and growth factors (e.g., VEGF, TGF-β, and PDGF). All these components work to create a microenvironment permissive for tumor cell growth, migration, and invasion. This review will focus on our current understanding of the roles that the ECM and ECM remodeling enzymes play in EOC progression, with specific emphasis placed on the individual key factors in the ECM known to date.
ECM Remodeling Promotes Ovarian Cancer Progression
The ECM is constructed from cellular secretions and is a critical regulator of normal tissue development and function (4). It is a dynamic, non-cellular structure existing within all tissues, which not only serves as a physical support for cells, but also has a unique role in tissue homeostasis (5). These diverse functions of the ECM are conferred through its complex organization, composition, and its continuous remodeling. The constituents of the ECM in different tissues vary, imparting a unique ability to accommodate the specific needs required by different tissues (6). This is facilitated by the chemical and physical interactions between the resident cells and the continuously changing microenvironment (7). The ECM is composed of two main types of macromolecules: fibrous proteins and proteoglycans (8).
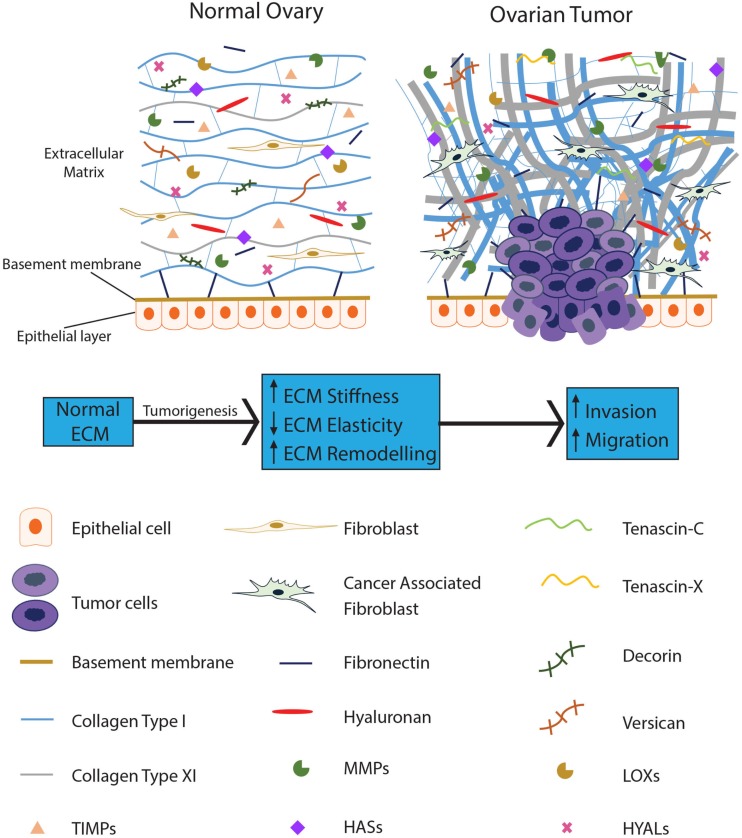
An increasing number of studies have proposed an essential role for the ECM in tumor progression, with dysregulation of the ECM implicated in cancer and characterized by extensive modification of its structure and composition. The secretion and/or inhibition of various ECM components and the subsequent remodeling by tumor cells creates a protumorigenic microenvironment which ultimately assists in tumor cell survival while disregarding the normal physiological function of the tissue (9). Stiffness and atypical ECM deposition are recognized in various cancers (10), with ECM alteration necessary for tumor initiation, progression, and intraperitoneal dissemination in EOC (11). Figure 1 provides a schematic representation of the ECM components involved in EOC.
Figure 1.
The ECM becomes dysregulated during ovarian tumorigenesis and contributes to tumor progression. The normal ovarian ECM consists of a highly ordered arrangement of collagen fibers, with hyaluronan interspersed throughout, regulating the distribution of the collagen in the ECM. Several proteoglycans, such as decorin and versican, are present to provide pressure and hydration to the tissue. In EOC, stromal fibroblasts are activated; collagen becomes progressively remodeled into short thick fibrils, randomly orientated into tracks at angles tending toward perpendicular rather than parallel to the epithelial boundary. In addition, versican, fibronectin, tenascin-C, and tenascin-X are upregulated with the loss of decorin. Reduced levels of HYALs lead to accumulation of hyaluronan; upregulation of LOXs leads to increased crosslinking of the ECM proteins resulting in increased stiffness of the ECM. MMPs are overexpressed in the EOC ECM, actively remodeling the ECM to promote tumor progression while TIMPs are unable to restrain these enzymes from dysregulating the ECM.
Fibrous Proteins
Fibrous proteins are major components of the ECM that provide tensile strength, elasticity, and structure to tissues. Many of these proteins become dysregulated in solid tumors and contribute to tumor growth and metastasis. Listed below are the fibrous proteins involved in EOC development and progression. Table 1 provides a summary of the ECM fibrous proteins reviewed here and their potential roles in EOC.
Table 1.
Summary of the ECM proteins and their roles in EOC.
| ECM protein | Role in EOC | Reference | |
|---|---|---|---|
| Fibrous proteins | Collagen I | Preferential and strong adhesion of primary ovarian cancer cells and spheroids to collagen I | (12, 13) |
| Promotes migration | (14, 15) | ||
| Provides a steering cue for cell migration | (16) | ||
| Collagen XI | Expression levels correlate with tumor grade | (17–19) | |
| Associated with poor clinical outcome and overall survival | (20, 21) | ||
| Predictor of recurrence | (17) | ||
| Contributes to paclitaxel resistance by upregulating tau | (22) | ||
| Fibronectin | Expressed in the ECM and ascites | (23, 24) | |
| Indicator of poor prognosis | (25) | ||
| Mediates migration, invasion, and metastasis | (15, 23, 26, 27) | ||
| Fibronectin fragments enhances adhesion of EOC cells to the peritoneal surface | (28) | ||
| Tenascin-C | Promoted increased adhesion and migration | (29) | |
| Tenascin-X | Levels associated with tumor grade | (30) | |
| Strong positive correlation with serum CA-125 levels | (31) | ||
| Laminin | Absent in microinvasive cells and low malignant tumors | (32) | |
| Significantly higher in EOC ascites than normal peritoneal fluid | |||
| No difference in serum levels between EOC and healthy control | |||
| Significantly higher serum levels in malignant EOC than in benign tumors and healthy controls | (33) | ||
| Ascites levels >serum levels in malignant EOC | |||
| Serum levels significantly reduced after surgery | (34) | ||
| Proteoglycans | Decorin | Cancer progression associated with reduced or loss of expression in EOC ECM | (35–38) |
| Lumican | Downregulation may have role in cancer aggression | (39) | |
| Versican | Elevated levels in EOC ECM correlated with poor disease outcome | (40–42) | |
| Perlecan | Expression lost in BM which facilitated invasion | (43) | |
| Hyaluronan | Elevated HA levels correlated with tumor grade and metastasis | (44) | |
| Strong, independent prognostic factor | (42) | ||
| Positive correlation with invasion and metastasis | (42, 45) | ||
| Facilitates adhesion of tumor cells to the peritoneum | (11, 46, 47) | ||
| Reduces efficacy of chemotherapy and induces chemoresistance in response to chemotherapy | (48) | ||
| Conjugates with chemotherapy increased the efficacy of chemotherapy | (49, 50) |
Collagens
Collagens are the most abundant fibrous proteins of the ECM. They associate with other collagens and interact with extracellular proteins, glycosaminoglycans and nucleic acids (7). Currently, there are 28 types of collagen identified which are divided into three major sub-groups: fibrillar, non-fibril forming, and fibril-associated collagens (51–53). Fibrillar collagens are the predominant sub-group present in the ECM, and their unique functions are governed by their conformation and structure, allowing them to form highly organized fibrils (6, 51). Particular focus will be placed on this specific sub-family of collagens. Fibrillar collagens are comprised of three α chains which assemble intracellularly into a triple helix that is secreted into the ECM as a procollagen molecule. Cleavage by metalloproteinases present in the ECM convert procollagen into collagen (6).
Insight into collagen morphology and organization and the resultant fibril composition and structure in the ECM are crucial for understanding how structural modifications are associated not only with the normal physiology of healthy tissue, but also with malignant processes linked to cancer progression (54). In normal tissue including normal ovary, collagen is organized as thin, long wavy fibrils, parallel to the epithelial boundary and providing elasticity to the ECM (Figure 1). In contrast, collagen remodeling in tumor stroma results in thicker and shorter fibrils, bunched into tracts at angles tending toward perpendicular to the epithelial boundary (Figure 1). Collagen tracts perpendicular to the epithelial boundary (also known as Tumor-Associated Collagen Signature (TACS)-3) are found in EOC (55). TACS-3 may facilitate entry into the stroma with invasive foci observed at these sites in mammary tumors (56). TACS-3 is also associated with a loss of elasticity and increase in stiffness of the ECM. These findings illustrate that ECM remodeling occurs in tumors and that fibrillar collagen contributes to this remodeling affecting the function of the resultant ECM.
Collagen-rich ECM was originally postulated to regulate normal tissue architecture and act as a physical barrier to tumor cell migration. However, it was shown that collagen-dense ECM induced by tumor cells essentially increased invasiveness and promoted tumor progression rather than inhibiting it (57). Increased risk of breast cancer has been associated with excessive collagen deposition and crosslinking (57, 58). Elevated collagen deposition and remodeling compromises drug delivery (59) and has been observed to be linked to cisplastin resistance in EOC (60–62). Collagen composition of the tumor ECM is crucial in mediating EOC progression and contributes to the poor response of ovarian cancer patients to chemotherapy, further emphasizing the importance of the ECM as an active participant in tumor progression.
Collagen I
Fibrillar type I collagen is the most abundant structural component of the ovarian ECM. Several in vitro studies have established the importance of type I collagen in EOC adhesion and migration, successfully demonstrating that collagen I enhanced migration of multiple EOC cell lines (14, 15), and primary EOC cells and spheroids preferentially and strongly adhered to type I collagen (12, 13). Collagen I has been demonstrated to have a novel role in inducing chemoresistance by upregulating tau (22), a microtubule-associated protein, which has been associated with paclitaxel resistance in EOC (63, 64). Flate and Stalvey (16) presented a study which implicates type I collagen as a steering mechanism for selected EOC cell lines in vitro and indicated that the migration of EOC cells induced by type I collagen was partially due to increased directionality. The promigratory cues which type I collagen confers on EOC cells highlight the multiple ways in which collagen can facilitate cancer cell migration. Thus, not only does collagen have a physical role in cancer progression, but it also has a potential role as a chemoattractant and may have an underlying role in chemoresistance. However, further studies are needed to consolidate these findings.
Collagen XI
Collagen XI is a minor fibrillary collagen predominantly found in cartilage with low or absent expression in most tissues (65–68). Hence stromal changes of collagen XI α-1 (COL11A1) expression are regarded as markers of cancer initiation and progression (20). High COL11A1 expression is associated with poor overall survival, poor clinical outcome and is a predictor of EOC recurrence correlating with the stage of disease (17, 20, 21). Increased gene expression of COL11A1 was observed in all EOC patients during tumor progression and was greatly increased in metastases (18). Varying mRNA and protein expression levels of COL11A1 at different stages and sites of the tumor suggests COL11A1 as a potential biomarker, with the highest COL11A1 levels detected in late stage disease (recurrent metastases) and lowest levels in earlier stage disease (primary ovarian tumors) (19). Though COL11A1 is clearly associated with cancer progression and metastasis, there are a limited number of studies detailing the role and mechanism of COL11A1 overexpression in metastasis. With limited biomarkers available for EOC, COL11A1 has potential as a clinical screening tool and prognostic marker.
Fibronectin
Fibronectin is implicated in cell growth, migration, and differentiation in processes including wound healing, embryonic development, and tumorigenesis (69, 70). Fibronectin plays a significant role in tumor progression, promoting metastasis, angiogenesis (71), and inhibiting apoptosis (72). Fibronectin expression is observed in the submesothelial basement membrane (BM) of metastatic omental tumors, ECM (23), and ascites (24). It is an indicator of poor prognosis in invasive EOC (25) and has been shown to mediate EOC cell migration and invasion (26) through the upregulation of the FAK/PI3K/Akt pathway (15). EOC cell motility and early metastatic competence is stimulated through the release of fibronectin from peritoneal mesothelial cells (23, 27). The protumorigenic role of fibronectin is further illustrated by Kenny et al. (23), who showed a significant reduction in the invasive and metastatic ability of EOC cells when fibronectin was knocked out from the peritoneal microenvironment. Another study by Kenny et al. (28) demonstrated that adhesion of EOC cells to the peritoneal surface was enhanced by MMP2 cleavage of fibronectin into small fragments. These studies have established fibronectin as a critical promoter of EOC migration and invasion. With its strong correlation with EOC progression, fibronectin presents a favorable target in cancer treatment.
Tenascin
There are four large extracellular glycoproteins which constitute the tenascin family: –C, –X, –R, and –W (73). Tenascins have roles in cell adhesion and proliferation. In certain cell types, they act as antiproliferative agents, while in other cell types, they act to promote adhesion and migration (74).
Tenascin-C
Tenascin-C (TNC) is an important tissue remodeling glycoprotein which contributes to tumorigenesis and metastasis by promoting proliferation, invasion, and angiogenesis (29, 75). TNC is either absent or present in minute amounts in healthy, developed tissues and significantly increased in pathological conditions, such as cancer (75). High TNC expression has been demonstrated in solid tumors, including breast, pancreas, prostate, brain, and ovary. High TNC expression correlated with poor survival in lung, glioma, breast, and colon cancers (76). In EOC, TNC levels were significantly higher than in non-cancer controls (75) and increased with increasing grade and stage, with malignant tumors displaying the highest expression (30). A subsequent study by the same investigators demonstrated a 100-fold increase in ovarian fibroblast media compared to media derived from EOC cell lines, suggesting that TNC is predominately secreted by fibroblasts (29). This study also indicated a potential role of TNC in invasion, demonstrating increased adhesion and migration in vitro.
The consistent finding of increasing TNC levels with increasing tumor stage for several cancer types suggests a potential biomarker role for TNC. However, a study by Didem et al. (75) determined that serum TNC levels had no prognostic value in EOC, with no correlation between high serum TNC levels and any prognostic factors, including tumor stage and grade, response to chemotherapy or survival, although patients with high TNC levels were observed to have poorer overall survival (75). This study only investigated serum TNC levels as a prognostic marker. It did not examine TNC levels in the immediate ECM of the ovarian tumor. There are limited studies available which examine TNC in EOC tumor tissue specifically, and further studies are required to establish its potential role in EOC progression.
Tenascin-X
Tenascin-X (TNX) is the largest member of the tenascin family, and during development TNX is widely expressed (77). TNX levels are significantly elevated in EOC compared to healthy tissues, normal ovaries, and benign tumors (31). Levels in ascites from EOC patients correlated with serum CA-125, implying that TNX secretion may be coordinated with the release of CA-125 (31), and may prove useful as a potential biomarker to complement CA-125. However, like TNC, there are limited studies available implicating TNX in EOC development (30).
Elastin
Elastin is a strong and insoluble biopolymer which constitutes ~90% of elastic fibers and is responsible for the resilience and elastic recoil of elastic vertebrate tissues (78). It has an extremely low turnover rate (79) and is formed through the crosslinking of its soluble precursor, tropoelastin, by LOX (80). Elastin has to some degree been associated with tumor growth and progression in other tumor types (81–83). Only one study is available to our knowledge which associates elastin with EOC. This study by Stewart et al. (84) evaluated the value of elastin staining in grading peritoneal implants associated with borderline serous EOC and demonstrated potential value in confirming superficial distribution of non-invasive peritoneal implants. However, this study did not specifically look at elastin levels in primary EOC tumors, and no studies are available at present which detail the potential role of elastin in EOC development and progression.
Laminin
The laminin family of glycoproteins consists of 12 unique heterotrimers and is the major non-collagen structural component of the BM (85). In addition to its structural functions, laminin also regulates cell adhesion and migration, demonstrating a role in tissue homeostasis and morphogenesis (86–89). This is partially mediated by the interactions between laminin and other ECM molecules, such as collagen type IV, fibronectin, and heparin sulfate proteoglycans (90). The role of laminin in the BM of EOC has been well studied; however, its potential role in the ECM has not been thoroughly examined. Laminin was observed to be absent around microinvasive cells and also in tumors of low malignant potential in the early stages of invasion (32). Studies show elevated laminin levels in the ascites from EOC patients compared to normal peritoneal fluid; however, there are conflicting results as to whether this corresponds to an increase in serum laminin levels (33, 34). Though there are strong indications of the possible tumor-promoting roles of laminin in EOC, further studies are needed to establish this association and its potential value as a biomarker or therapeutic target.
Proteoglycans
Proteoglycans are dispersed throughout ECM and act to provide compressive resistance and hydration to the tissue (6, 8). The two major ECM proteoglycan families consist of those containing leucine-rich repeats and hyalectans. Table 1 provides a summary of proteoglycans reviewed in this section and their potential roles in EOC.
Small Leucine-Rich Repeat Proteoglycans
Leucine-rich repeat (LRR) proteoglycans are the most abundant and also the largest class of proteoglycans in the ECM. They have various functions, combining roles as signaling molecules and structural components during tissue remodeling in cancer and inflammation. LRR proteoglycans are regulated by the TGF-β and Wnt signaling pathways and interact with a range of Toll-like receptors, receptor tyrosine kinases, and growth factors to regulate homeostatic processes, such as apoptosis, migration, proliferation, angiogenesis, differentiation, and survival (91–96). They are also involved with regulating fibrillary collagen assembly, degradation, and organization (97–103). Of the LRR proteoglycan family members, only decorin and lumican have to date been shown to play roles in the ovarian tumor ECM.
Decorin
Decorin, a fundamental component of the ECM, binds to collagen and facilitates tissue scaffolding (104). However, its expression in cancer, including EOC, is generally reduced or undetectable (35–38, 105–107). Decorin-induced growth suppression was observed in a study by Merle et al. (108), highlighting the importance of decorin in possibly inhibiting tumor growth. It was proposed that decorin was able to interfere with the interactions between the resident cells and the ECM, by inhibiting fibronectin binding and integrin interaction. Nash et al. (109) and Teicher et al. (110) demonstrated the synergistic effects of decorin with cisplastin and carboplatin in inhibiting the growth of breast and EOC. Decorin can inhibit tumor growth by suppressing TGF-β (105, 111) and directly interacting with the epidermal growth factor receptor and ERBB2 (112–115). The direct interaction with these receptors diminishes receptor-mediated intracellular signaling and induces apoptosis (116, 117). These studies suggest that decorin plays a major role in controlling tumor growth and its subsequent downregulation is associated with EOC development, indicating that possible therapies involving the restoration of decorin expression in the tumor stroma, coupled with chemotherapy, could potentially retard the growth of EOC.
Lumican
Lumican, another LRR proteoglycan, is involved in the regulation of collagen fibrillogenesis, migration, invasion, angiogenesis, and apoptosis (104, 118–120). Varying levels have been reported in the stroma of different tumor types (121–126). In breast and pancreatic cancers, high stromal lumican was associated with advanced cancer stage, invasion, and poor survival (127, 128), whereas a negative correlation was found between tumor grade and expression in neuroendocrine tumors of the colon (129). In support of this, lumican has been shown to inhibit tumor growth and progression in lung cancer and melanoma (92). To date, a single study has examined lumican expression in EOC, demonstrating reduced stromal expression and suggesting a possible role in cancer aggression (39). Given the varying clinical associations with lumican in several cancer types, more research is needed to determine the precise role of lumican in EOC.
Versican
In the healthy ovary, versican (VCAN) is tightly regulated and acts as an important ECM proteoglycan present in the granulosa cells of growing follicles, to aid in the expansion of the cumulus oophorus in the preovulatory stage (130). Normal processes, such as wound healing (131), follicle growth (130), and inflammation (132), induce VCAN expression. Many malignant tumors have elevated levels of VCAN (133–140). Elevated VCAN levels were also observed in the ECM of EOC and correlated with increased hyaluronan (HA) levels, suggesting that they may form a supportive partnership to assist in EOC survival and spread (40, 41). In vitro studies have demonstrated the production of VCAN by malignant cells; however, the source of VCAN in tumors remains to be elucidated, with no clear answer on the in vivo source of VCAN, which may also include stromal cells (137, 141–143). Upregulation of VCAN in EOC correlates with a poor disease outcome; however, the significance of VCAN as a prognostic marker is debatable, with HA, its binding partner, presenting greater value as a prognostic marker (42). The same study showed that despite a strong association with the apparent initiation and development of EOC, VCAN was not an independent indicator for patient survival.
Perlecan
Perlecan is a core heparan sulfate proteoglycan of the ECM and BMs of normal tissues and blood vessels (8, 144, 145). Perlecan is stored in abundant quantities in the BM. Degradation of the BM by MMPs during tumor invasion causes the release of perlecan into the ECM, and increased expression is reported in various cancer cell lines and tumors (146–148). Perlecan has been suggested to have various roles in tumor progression, by regulating the cell’s response to mitogenic and angiogenic growth factors, and mediating adhesion and migration (149, 150). Its inhibition is reported to impede tumor growth and invasion (144, 151). A study by Davies et al. (43) observed heterogeneous perlecan expression in ovarian tumors compared to normal ovary. Perlecan expression was observed in the BM, the stroma, the internal elastic lamina of blood vessels, and the submesothelial layer of the normal ovary. Perlecan was also present in the BM of benign and borderline tumors but absent in the BM of malignant tumors, enhancing invasive potential. Loss of perlecan was not observed in the stroma and BMs of blood vessels. Further studies are needed to determine its potential role in EOC progression.
Hyaluronan
Hyaluronan is strongly implicated in cell proliferation, migration, wound healing, and inflammation (152). HA binds and interacts closely with fibronectin during matrix construction (152–154) and regulates the distribution of collagen fibrils (155). HA can interact directly with cells by binding to cell surface receptors and constructing a protective coat (156–158). It also has a role in the distribution of proteoglycans in the ECM through non-covalent interactions (159–161). Changes in HA content and size are associated with tissue remodeling and pathological processes, such as tumor progression (162–166). Studies from several cancer types have recognized the elevation of HA in serum (167–169), and recently a study by Wu et al. (170) demonstrated the novel use of serum HA in differentiating non-metastatic from metastatic breast cancer, which suggests HA as a potential biomarker. Elevated HA levels were observed in and associated with tumor aggression in breast, lung, prostate, colorectal, and bladder cancer (163).
Epithelial ovarian cancer grade and metastasis are correlated with increasing HA levels, with Hiltunen et al. (44) demonstrating a 100-fold increase in HA expression in grade three EOC. Many cancers, including ovarian, are enveloped in a HA rich ECM (11, 42, 44). HA upregulation has been implicated as a strong, independent prognostic factor for EOC (42) and is positively correlated with invasion and metastasis (42, 45). Adhesion of ovarian cancer cells to the peritoneum is facilitated by interactions between HA and its major surface receptor CD44 (45–47, 171). HA has been shown to reduce the ability of chemotherapeutic drugs to induce cell death in several cancers (172–175). Ricciardelli et al. (48) demonstrated chemotherapy-induced HA production facilitates chemoresistance and EOC cell survival through a HA-CD44-mediated pathway. HA-chemotherapy conjugates were successful in increasing the efficacy of standard chemotherapy in EOC patients by CD44-mediated uptake of the chemotherapy (49, 50). Hence, HA is a promising therapeutic target, with HA inhibition potentially suppressing adhesion of EOC cells to the peritoneum, which is the preferential place for EOC metastasis. Conversely, HA can be utilized to enhance the cytotoxic effects of chemotherapy.
Enzymes
Abnormal expression and deposition of ECM components and alteration to its structure are implicated in malignancies such as EOC. Remodeling of the ECM in healthy tissues through chemical modification, synthesis, degradation, and reassembly are tightly controlled processes induced by cells in homeostasis (176). Crosstalk between the ECM and cancer cells causes the alteration of ECM structure and composition, resulting in the dysregulation of this tightly controlled system (5). Cleavage of ECM components by proteases and the subsequent remodeling of the ECM is implicated in EOC progression, where the degradation of the BM and ECM is necessary for the invasion and metastasis of EOC cells (177, 178). Malignant cells produce a wide range of ECM-degrading proteases implicated in ECM dysregulation and cancer progression. Inhibiting their activity may be of potential therapeutic value. Table 2 provides a summary of the ECM remodeling enzymes reviewed here and their potential roles in EOC.
Table 2.
Summary of the ECM remodeling enzymes and their roles in EOC.
| Enzyme | Role in EOC | References |
|---|---|---|
| MMP2/MMP9 | Expression associated with EOC aggression | (179–181) |
| Identified to be secreted by cancer cells and expression correlated with invasiveness | (182–185) | |
| Higher total activity in the metastatic site | ||
| Promotes metastasis | (180) | |
| MMP9 – conflicting reports as a prognostic marker | ||
| High levels of epithelial MMP9 associated with a better DRS | (179, 188) | |
| High stromal levels of MMP associated with worse DRS | (189–192) | |
| High epithelial and stromal MMP9 associated with poor DRS and metastasis | ||
| MMP7 | Conflicting findings in promoting tumor progression | |
| Overexpression promoted invasion | (193) | |
| Suppression of MMP7 inhibited migration and invasion | (194) | |
| MMP7 expression lower in malignant tumors | (181, 195) | |
| Higher expression correlated with good clinical and survival parameters | (196) | |
| LOX | LOX G473A polymorphism correlated with advanced stages and increased susceptibility | (197, 198) |
| Overexpression correlated with metastasis and tumor stage | (199) | |
| Promoted migration and tumor growth by repressing E-cadherin | (200) | |
| LOXL2 | Upregulated specifically in EOC endothelial cells. Inhibition of LOXL2 reduced endothelial cell concentration | (201) |
| LOXL2 inhibition suppressed tumor angiogenesis and induced normalization of tumor-associated vasculature | (202) | |
| LOXL4 | Tumor suppressive effect, however, LOXL4 splice variants enhanced tumor progression and metastatic potential | (203) |
| Hyaluronan Synthases | Low HAS1 – independent predictor of ovarian cancer patient survival High HAS1 correlated with high microvessel density in ovarian cancer | (204) |
| HAS2 and HAS3 – no consistent increase | ||
| HAS1 – barely detectable in EOC | (205) | |
| HAS1, HAS2, and HAS3 – overexpressed in effusions, solid metastases, and primary EOC, respectively | (206) | |
| High HAS1 expression in EOC effusion correlated with shorter survival | ||
| Hyaluronidases | HYAL1–3 – chromosomal loss in tumor and stromal tissue | (207) |
| Reduced activity and expression in malignant EOC – also differentially expressed | (44, 206) | |
| HYAL1 – absent in serous EOC | (206, 208) | |
| HYAL2-var2 and HYAL3 variant – overexpressed in solid metastases and primary EOC tumors, respectively | (206) |
Matrix Metalloproteinases
Matrix metalloproteinases are a family of extracellular proteins comprising >20 zinc metalloproteases which play major roles in tissue repair and remodeling in response to injury (209). In normal conditions, the activity of MMPs is low. However, in response to cellular and matrix interactions, growth factors, hormones, and inflammatory cytokines released during remodeling or repair processes and in inflamed or diseased tissues, MMP activity increases (5, 210). MMPs remodel the ECM and contribute to the tumor microenvironment by promoting tumor growth, metastasis, and angiogenesis (211, 212). Through these activities, MMPs promote cancer progression and correlate with poor patient prognosis (213).
MMP2 and MMP9
Matrix metalloproteinase 2 and MMP9 have been implicated to contribute to the malignant potential of tumor cells, due to their ability to degrade a major component of the BM, collagen type IV (214). MMP2 and MMP9 activity varies between normal ovaries and malignant ovarian tumors. MMP2 was observed to be prevalent in normal ovaries, while MMP9 was predominant in malignant tissues (215). EOC aggressiveness has been linked to MMP2 and MMP9 expression (179–181). Several studies have demonstrated the secretion of MMP2 and MMP9 from EOC cell lines in vitro and in ascites from advanced EOC patients. In vitro expression of MMP2 and -9 also correlated with the invasiveness of the EOC cell lines (182–185, 216). Schmalfeldt et al. (180) confirmed these studies, by not only demonstrating elevated levels of MMP2 and -9, but also identified higher total MMP2 and MMP9 activity in the metastatic site, compared to the primary site, suggesting their likely role in the progression from a benign state to an advanced stage. MMP2 expression correlated with clinical stage (186) and promoted metastasis along with MMP9 (187).
Sillanpää et al. (188) evaluated the prognostic significance of MMP9 in EOC, where high levels of epithelial MMP9 were associated with a better 10-year disease-related survival (DRS), while high stromal levels of MMP9 were associated with worse survival. This was supported by a study by Ozalp et al. (179). This however, has been contradicted by several other studies (189–192) which associated high epithelial and stromal MMP9 with shorter disease-specific survival and metastasis.
MMP7
Matrix metalloproteinase 7 is involved in the proteolysis of several ECM substrates, growth factors, and cellular receptors including collagens, proteoglycans, insulin-like growth factor-binding protein, heparin-binding epidermal growth factor, E-cadherin, and tumor necrosis factor-alpha precursor (193, 217). Overexpression of MMP7 in EOC has been demonstrated in several studies (193, 195, 196). Wang et al. (193) showed that overexpression of MMP7 promoted the invasion of EOC cells in vitro and likewise, suppression of MMP7 inhibited migration and invasion (194). These findings are in contrast to the study by Brun et al. (181) who showed that epithelial MMP7 expression was lower in malignant serous tumors, compared to its benign or borderline counterparts, while there was no difference observed among the mucinous tumors. Shigemasa et al. also supported this finding in mucinous ovarian tumors (195). MMP7 was observed to be an independent prognostic factor, with higher MMP7 expression in ovarian tumor cells correlating with good clinical and survival parameters (196). These discrepancies highlight the need to elucidate the functional role of MMP7 in EOC, where the grade and subtype of the tumor may result in these contrasting findings.
While MMP2, -7, and -9 have been implicated to play a role in EOC, there are discrepancies correlating the expression of these MMPs with the prognosis and certain clinicopathological features of EOC. This suggests that the functions of MMPs in EOC may be dependent on their epithelial or stromal associations in conjunction with the grade of the tumor and possibly the surrounding stroma. This highlights the complexity of MMPs and their roles in EOC progression and emphasizes the need for additional studies to provide an explanation for these differences. Nonetheless, MMPs have potential as therapeutic targets due to their indisputable activity during EOC progression. MMP2, -7, and -9 expression are elevated in EOC regardless of the grade; therefore, inhibition of MMPs may decrease the aggressiveness of EOC and aid in preventing invasion and metastasis.
Tissue Inhibitors of Metalloproteinases
Tissue inhibitors of metalloproteinases are endogenous inhibitors of major ECM remodeling proteinases, such as MMPs, and subsequently they play a crucial role in regulating ECM composition and function. TIMPs also have multiple functions in regulating cell proliferation, migration, invasion, apoptosis, and angiogenesis (218). There are four TIMP paralogs: TIMP1–4 (219). TIMP1 is the most widely distributed TIMP and has the ability to inhibit all active forms of MMP (220). TIMP2 is most selective for MMP2 (221). Simultaneous increase of MMP2 and decrease of TIMP2 levels were observed in malignant tumors compared to benign tumors and the normal ovary, with this imbalance indicative of the importance of MMP2–TIMP2 levels in promoting invasion (222). In contrast, TIMP1 levels were increased in malignant tumors compared to the normal ovary (222–224). Okamoto et al. (222) observed that despite the synchronous increase of MMP9 and TIMP1 in malignant tumors, the degree of increase of MMP9 was much greater than TIMP1, suggesting that TIMP1 has limited ability in compensating for an increase in MMP9. A study by Kikkawa et al. (225) also reported elevated TIMP1 and MMP9 levels in EOC samples compared to normal ovary. Given their role as inhibitors of MMPs, the relative levels of each family of enzymes are important when considering their function in EOC. MMPs and TIMPs have a dynamic relationship not just in normal ovaries, but also in EOC, where the expression of TIMPs adjusts with the relative levels of MMPs present to ultimately promote tumor progression.
Lysyl Oxidase
The LOX family comprises five members: LOX and four LOX-like isoenzymes LOXL1–4. LOX is a copper-dependent amine oxidase secreted by fibroblasts and, together with the other family members, has an important role in remodeling the ECM by regulating collagen and elastin crosslinking and therefore contributes to the strength and structure of many tissues (226–228). LOX and LOXL2 are heavily implicated in cancer progression (229, 230).
Lysyl Oxidase
The importance of the LOX family in ECM remodeling during normal physiological processes has been established in a variety of tissues. In the ovary, LOX is activated during ovulation, following follicle rupture and is critical in collagen synthesis and reassembly in the ovarian follicle (231). Several studies have demonstrated the expression of LOX in granulosa cells (232–234), and its expression and activity is tightly controlled by follicle-stimulating hormone during follicle development (232, 234). Wang et al. (197) initially showed that a single nucleotide polymorphism of the LOX gene, G473A, correlated with advanced stages and increased susceptibility to EOC in a Chinese population. This finding was supported by Wu et al. (198). In hypoxic conditions, hypoxia inducible factor-1α (HIF-1α) induced LOX expression and facilitated tumor migration, invasion, and metastasis in a range of cancers (229). LOX and HIF-1α overexpression were observed in hypoxic EOC cells, with expression levels correlating significantly with metastasis and tumor stage in EOC (199). HIF-1α upregulation induced LOX transcription through the accumulation of reactive oxygen species, subsequently repressing E-cadherin. Loss of E-cadherin was observed to promote EOC cell migration in vitro and tumor growth in vivo, while also correlating with tumor stage, differentiation, metastasis, and a poorer 5-year survival rate (200).
LOXL2
LOXL2 plays a similar role to LOX in crosslinking collagen and elastin in the ECM, contributing to the stability and strength of the tissue (226). LOXL2 overexpression has been linked to the aggressiveness of breast (235), skin (236), and colon cancers (237). Specific upregulation of the LOXL2 protein is found in EOC endothelial cells, where inhibition of LOXL2 reduced endothelial cell concentration within the tumor (201). A study by Zaffryar-Eilot et al. (202) confirmed the direct role of LOXL2 in angiogenesis, with LOXL2 inhibition decreasing microvessel density for the normalization of tumor-associated vasculature resulting in reduced tumor hypoxia with better response to therapy (238).
LOXL4
LOXL4 is expressed in head and neck squamous cell carcinoma and gastric cancer cell lines, and upregulation of LOXL4 significantly correlates with tumor stage and lymph node metastases (239–241). LOXL4 promotes proliferation, migration, and invasion in gastric cancer cell lines in vitro (241). A study by Sebban et al. (203) demonstrated a tumor suppressive effect in EOC in vivo, while also indicating a contrasting role of LOXL4 splice variants in vitro, with the variants enhancing tumor progression and metastatic potential. This study demonstrates the paradoxical roles of LOXL4 and its alternatively spliced isoforms. Specific variants of LOXL4 could be promising as a prognostic marker and a potential therapeutic target.
To our knowledge, only LOX, LOXL2, and LOXL4 have been studied in EOC. Aberrant LOX, LOXL2, and LOXL4 expression are implicated in dysregulating the ECM and inducing a malignant phenotype and promoting tumor progression in EOC. However, additional studies are needed to elucidate further potential roles of these LOX family members in EOC, where a wide range of studies have demonstrated a strong association between these enzymes and several tumorigenic pathways in a variety of other cancers (230). Due to the protumorigenic role of LOX, LOXL2, and LOXL4, inhibition of these LOX family members in conjunction with chemotherapy could potentially enhance its antitumorigenic effect and result in a better prognosis.
Hyaluronan Synthases
Hyaluronan synthases (HASs) are integral plasma membrane proteins which synthesize HA (242, 243). Three isoenzymes of HAS with differing enzymatic activities have been identified in humans: HAS1, HAS2, and HAS3 (244). Overexpression of HAS is implicated to promote growth and metastasis in a variety of cancers through excessive production of HA (245–249). In one study of ovarian cancer by Yabushita et al., HAS1-negative tumors were associated with increased overall survival and lower microvessel density relative to HAS1-positive tumors. No relationships were found between the levels of HAS2–3 and tumor stage, survival, chemotherapy, or microvessel density (204). Weiss et al. (206) compared the expression of HAS1–3 mRNA in serous EOC between effusions, primary carcinomas, and solid metastases, with differential HAS overexpression observed in each region. HAS1, HAS2, and HAS3 were overexpressed in effusions, solid metastases, and primary carcinomas, respectively. High HAS1 expression in EOC effusions correlated with shorter survival in agreement with the results of Yabushita et al. (204). However, a study by Nykopp et al. (205) demonstrated barely detectable HAS1 in EOC and no consistent increase in the HAS2 and HAS3 expression. These result suggest unique roles for each HAS isoenzyme during different stages of EOC progression, although no clear associations have been identified to date.
Hyaluronidases
Hyaluronan synthesis by HASs is opposed by the enzymatic action of hyaluronidases (HYALs), which degrade HA. The family of HYALs consists of six members (250), of which HYAL1 and HYAL2 are particularly well characterized (205). HYAL1 and HYAL2 are the main members responsible for HA turnover, with these two enzymes bearing several physiological and pathological roles, such as wound healing and inflammation (250, 251). High molecular weight HA is antiangiogenic; HYALs cleave HA into low molecular weight HA fragments which may promote angiogenesis, subsequently enhancing tumor growth (252). While chromosomal loss at the locus encoding HYAL1–3 (3p21.3) is common in both tumor and stromal tissue from EOC patients, this allelic loss is not associated with increased tissue HA levels (207). HYAL activity and expression were reported to be reduced and differentially expressed in malignant EOC compared to its benign and normal counterparts (44, 206). HYAL1 was absent in all serous EOC samples (206); however, expression of HYAL1 in EOC is subtype specific, with clear cell and mucinous EOC showing elevated levels of HYAL1 compared to serous and endometrioid EOC (208). Comparing transcript levels in serous EOC between primary tumors, solid metastases, and effusions, HYAL2 splice variant, HYAL2-var2, was significantly overexpressed in solid metastases, and HYAL3 var1–3 was significantly underexpressed in solid metastases. A positive correlation was identified between HYAL3 levels in effusions and paclitaxel treatment (206).
Regulation of HA synthesis and degradation is mediated by HASs and HYALs, respectively. As described above, HA accumulation is associated with the aggressiveness of EOC and has been demonstrated to promote EOC progression. The displacement of this otherwise delicate equilibrium of controlled HA synthesis and degradation by HASs and HYALs in EOC has major implications on the subsequent structure and function of the ECM and therefore may represent promising targets for cancer treatment.
Discussion
The ECM is a dynamic structure. It is crucial in regulating specific function, development, and homeostasis, achieved by organizing and regulating the plethora of ECM components unique to each differentiated tissue (4, 7, 176, 253). Remodeling of the ECM in EOC is thought to promote tumor progression. The interactions between the ECM and the resident cells are tightly regulated, and disruption of the ECM has severe consequences as described in this review. It is evident that the ECM in EOC remains relatively unexplored, with the mechanisms involved in tumor progression yet to be fully elucidated. To fully understand how alterations to the ECM influence tumorigenesis, it is essential to investigate not only how the ECM interacts with tumor cells, but also how the ECM components interact with each other.
The constituents of the ECM offer potential biomarkers and therapeutic targets, where the manipulation of the ECM composition may complement current chemotherapeutic treatment. Enzymes involved in ECM remodeling and elevated in EOC, such as MMPs and LOXs, which have been shown in preclinical models to promote tumor progression in other cancers, could also be a potential therapeutic targets in EOC. Though CA-125 is clinically approved to be used as a serum tumor biomarker for ovarian cancer, Moss et al. (254) demonstrated its poor sensitivity and specificity, with a high false positive rate. Other than CA-125, there are currently no reliable biomarkers for the staging and prognosis of ovarian cancer. With low overall survival rates for patients diagnosed with advanced disease, a sensitive and specific diagnostic biomarker of early stage EOC is needed. Tenascins have a limited presence in healthy tissues, hence could potentially serve as biomarkers for early diagnosis of EOC.
Though the identification of individual ECM components allows us to understand their basic functions in EOC, the ECM must be considered not just as its individual elements, but as a collective entity. EOC progression is multifactorial and influenced by an altered ECM. The ECM constituents described in this review reflect the complexity of the EOC microenvironment which is an evolving area of research. Advances in understanding how the ECM contributes to EOC pathogenesis and progression will assist in the development of better treatments for EOC.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
This work was supported by a Cancer Institute NSW Fellowship (to EC), Cure Cancer Australia Foundation (EC), Cancer Australia (EC) and the Bill Walsh Cancer Research Fund (VH).
References
- 1.Siegel RL, Miller KD, Jemal A. Cancer statistics, 2015. CA Cancer J Clin (2015) 65(1):5–29. 10.3322/caac.21254 [DOI] [PubMed] [Google Scholar]
- 2.Kurman RJ, Visvanathan K, Roden R, Wu TC, Shih IeM. Early detection and treatment of ovarian cancer: shifting from early stage to minimal volume of disease based on a new model of carcinogenesis. Am J Obstet Gynecol (2008) 198(4):351–6. 10.1016/j.ajog.2008.01.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Siegel R, Ma J, Zou Z, Jemal A. Cancer statistics, 2014. CA Cancer J Clin (2014) 64(1):9–29. 10.3322/caac.21208 [DOI] [PubMed] [Google Scholar]
- 4.Mecham RP. Overview of extracellular matrix. Curr Proto Cell Biol. (2014). 10.1002/0471143030.cb1001s57. [DOI] [PubMed] [Google Scholar]
- 5.Bonnans C, Chou J, Werb Z. Remodelling the extracellular matrix in development and disease. Nat Rev Mol Cell Biol (2014) 15(12):786–801. 10.1038/nrm3904 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mouw JK, Ou G, Weaver VM. Extracellular matrix assembly: a multiscale deconstruction. Nat Rev Mol Cell Biol (2014) 15(12):771–85. 10.1038/nrm3902 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Naba A, Clauser KR, Hoersch S, Liu H, Carr SA, Hynes RO. The matrisome: in silico definition and in vivo characterization by proteomics of normal and tumor extracellular matrices. Mol Cell Proteomics (2012) 11(4):M111.014647. 10.1074/mcp.M111.014647 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hynes RO, Naba A. Overview of the matrisome – an inventory of extracellular matrix constituents and functions. Cold Spring Harb Perspect Biol (2012) 4(1):a004903. 10.1101/cshperspect.a004903 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zigrino P, Löffek S, Mauch C. Tumor-stroma interactions: their role in the control of tumor cell invasion. Biochimie (2005) 87(3–4):321–8. 10.1016/j.biochi.2004.10.025 [DOI] [PubMed] [Google Scholar]
- 10.Frantz C, Stewart KM, Weaver VM. The extracellular matrix at a glance. J Cell Sci (2010) 123(Pt 24):4195–200. 10.1242/jcs.023820 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ween MP, Oehler MK, Ricciardelli C. Role of versican, hyaluronan and CD44 in ovarian cancer metastasis. Int J Mol Sci (2011) 12(2):1009–29. 10.3390/ijms12021009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Moser TL, Pizzo SV, Bafetti LM, Fishman DA, Stack MS. Evidence for preferential adhesion of ovarian epithelial carcinoma cells to type I collagen mediated by the alpha2beta1 integrin. Int J Cancer (1996) 67(5):695–701. [DOI] [PubMed] [Google Scholar]
- 13.Burleson KM, Casey RC, Skubitz KM, Pambuccian SE, Oegema TR, Jr, Skubitz AP. Ovarian carcinoma ascites spheroids adhere to extracellular matrix components and mesothelial cell monolayers. Gynecol Oncol (2004) 93(1):170–81. 10.1016/j.ygyno.2003.12.034 [DOI] [PubMed] [Google Scholar]
- 14.Shen Y, Shen R, Ge L, Zhu Q, Li F. Fibrillar type I collagen matrices enhance metastasis/invasion of ovarian epithelial cancer via beta1 integrin and PTEN signals. Int J Gynecol Cancer (2012) 22(8):1316–24. 10.1097/IGC.0b013e318263ef34 [DOI] [PubMed] [Google Scholar]
- 15.Ahmed N, Riley C, Rice G, Quinn M. Role of integrin receptors for fibronectin, collagen and laminin in the regulation of ovarian carcinoma functions in response to a matrix microenvironment. Clin Exp Metastasis (2005) 22(5):391–402. 10.1007/s10585-005-1262-y [DOI] [PubMed] [Google Scholar]
- 16.Flate E, Stalvey JR. Motility of select ovarian cancer cell lines: effect of extra-cellular matrix proteins and the involvement of PAK2. Int J Oncol (2014) 45(4):1401–11. 10.3892/ijo.2014.2553 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wu YH, Chang TH, Huang YF, Huang HD, Chou CY. COL11A1 promotes tumor progression and predicts poor clinical outcome in ovarian cancer. Oncogene (2014) 33(26):3432–40. 10.1038/onc.2013.307 [DOI] [PubMed] [Google Scholar]
- 18.Cheon DJ, Tong Y, Sim MS, Dering J, Berel D, Cui X, et al. A collagen-remodeling gene signature regulated by TGF-beta signaling is associated with metastasis and poor survival in serous ovarian cancer. Clin Cancer Res (2014) 20(3):711–23. 10.1158/1078-0432.CCR-13-1256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tothill RW, Tinker AV, George J, Brown R, Fox SB, Lade S, et al. Novel molecular subtypes of serous and endometrioid ovarian cancer linked to clinical outcome. Clin Cancer Res (2008) 14(16):5198–208. 10.1158/1078-0432.CCR-08-0196 [DOI] [PubMed] [Google Scholar]
- 20.Raglow Z, Thomas SM. Tumor matrix protein collagen XIα1 in cancer. Cancer Lett (2015) 357(2):448–53. 10.1016/j.canlet.2014.12.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Teng PN, Wang G, Hood BL, Conrads KA, Hamilton CA, Maxwell GL, et al. Identification of candidate circulating cisplatin-resistant biomarkers from epithelial ovarian carcinoma cell secretomes. Br J Cancer (2014) 110(1):123–32. 10.1038/bjc.2013.687 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gurler H, Yu Y, Choi J, Kajdacsy-Balla AA, Barbolina MV. Three-dimensional collagen type I matrix up-regulates nuclear isoforms of the microtubule associated protein tau implicated in resistance to paclitaxel therapy in ovarian carcinoma. Int J Mol Sci (2015) 16(2):3419. 10.3390/ijms16023419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kenny HA, Chiang CY, White EA, Schryver EM, Habis M, Romero IL, et al. Mesothelial cells promote early ovarian cancer metastasis through fibronectin secretion. J Clin Invest (2014) 124(10):4614–28. 10.1172/JCI74778 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wilhelm O, Hafter R, Coppenrath E, Pflanz MA, Schmitt M, Babic R, et al. Fibrin-fibronectin compounds in human ovarian tumor ascites and their possible relation to the tumor stroma. Cancer Res (1988) 48(12):3507–14. [PubMed] [Google Scholar]
- 25.Franke FE, Von Georgi R, Zygmunt M, Münstedt K. Association between fibronectin expression and prognosis in ovarian carcinoma. Anticancer Res (2003) 23(5b):4261–7. [PubMed] [Google Scholar]
- 26.Lou X, Han X, Jin C, Tian W, Yu W, Ding D, et al. SOX2 targets fibronectin 1 to promote cell migration and invasion in ovarian cancer: new molecular leads for therapeutic intervention. OMICS (2013) 17(10):510–8. 10.1089/omi.2013.0058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rieppi M, Vergani V, Gatto C, Zanetta G, Allavena P, Taraboletti G, et al. Mesothelial cells induce the motility of human ovarian carcinoma cells. Int J Cancer (1999) 80(2):303–7. [DOI] [PubMed] [Google Scholar]
- 28.Kenny HA, Kaur S, Coussens LM, Lengyel E. The initial steps of ovarian cancer cell metastasis are mediated by MMP-2 cleavage of vitronectin and fibronectin. J Clin Invest (2008) 118(4):1367–79. 10.1172/JCI33775 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wilson KE, Bartlett JM, Miller EP, Smyth JF, Mullen P, Miller WR, et al. Regulation and function of the extracellular matrix protein tenascin-C in ovarian cancer cell lines. Br J Cancer (1999) 80(5–6):685–92. 10.1038/sj.bjc.6690410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wilson KE, Langdon SP, Lessells AM, Miller WR. Expression of the extracellular matrix protein tenascin in malignant and benign ovarian tumours. Br J Cancer (1996) 74(7):999–1004. 10.1038/bjc.1996.480 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kramer M, Pierredon S, Ribaux P, Tille JC, Petignat P, Cohen M. Secretome identifies tenascin-X as a potent marker of ovarian cancer. Biomed Res Int (2015) 2015:9. 10.1155/2015/208017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Campo E, Merino MJ, Tavassoli FA, Charonis AS, Stetler-Stevenson WG, Liotta LA. Evaluation of basement membrane components and the 72 kDa type IV collagenase in serous tumors of the ovary. Am J Surg Pathol (1992) 16(5):500–7. 10.1097/00000478-199205000-00009 [DOI] [PubMed] [Google Scholar]
- 33.Byers LJ, Osborne JL, Carson LF, Carter JR, Haney AF, Weinberg JB, et al. Increased levels of laminin in ascitic fluid of patients with ovarian cancer. Cancer Lett (1995) 88(1):67–72. 10.1016/0304-3835(94)03625-S [DOI] [PubMed] [Google Scholar]
- 34.Chu Y, Yang Y, Lin M, Wang Z. Detection of laminin in serum and ascites from patients with epithelial ovarian tumor. J Huazhong Univ Sci Technolog Med Sci (2002) 22(1):58–9. 10.1007/BF02904790 [DOI] [PubMed] [Google Scholar]
- 35.Nash MA, Deavers MT, Freedman RS. The expression of decorin in human ovarian tumors. Clin Cancer Res (2002) 8(6):1754–60. [PubMed] [Google Scholar]
- 36.Shridhar V, Lee J, Pandita A, Iturria S, Avula R, Staub J, et al. Genetic analysis of early- versus late-stage ovarian tumors. Cancer Res (2001) 61(15):5895–904. [PubMed] [Google Scholar]
- 37.Grisaru D, Hauspy J, Prasad M, Albert M, Murphy KJ, Covens A, et al. Microarray expression identification of differentially expressed genes in serous epithelial ovarian cancer compared with bulk normal ovarian tissue and ovarian surface scrapings. Oncol Rep (2007) 18(6):1347–56. 10.3892/or.18.6.1347 [DOI] [PubMed] [Google Scholar]
- 38.Grazio D, Pichler I, Fuchsberger C, Zolezzi F, Guarnieri P, Heidegger H, et al. Differential gene expression analysis of ovarian cancer in a population isolate. Eur J Gynaecol Oncol (2008) 29(4):357–63. [PubMed] [Google Scholar]
- 39.Amankwah EK, Wang Q, Schildkraut JM, Tsai YY, Ramus SJ, Fridley BL, et al. Polymorphisms in stromal genes and susceptibility to serous epithelial ovarian cancer: a report from the ovarian cancer association consortium. PLoS One (2011) 6(5):e19642. 10.1371/journal.pone.0019642 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Voutilainen K, Anttila M, Sillanpää S, Tammi R, Tammi M, Saarikoski S, et al. Versican in epithelial ovarian cancer: relation to hyaluronan, clinicopathologic factors and prognosis. Int J Cancer (2003) 107(3):359–64. 10.1002/ijc.11423 [DOI] [PubMed] [Google Scholar]
- 41.Ghosh S, Albitar L, LeBaron R, Welch WR, Samimi G, Birrer MJ, et al. Up-regulation of stromal versican expression in advanced stage serous ovarian cancer. Gynecol Oncol (2010) 119(1):114–20. 10.1016/j.ygyno.2010.05.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Anttila MA, Tammi RH, Tammi MI, Syrjänen KJ, Saarikoski SV, Kosma VM. High levels of stromal hyaluronan predict poor disease outcome in epithelial ovarian cancer. Cancer Res (2000) 60(1):150–5. [PubMed] [Google Scholar]
- 43.Davies EJ, Blackhall FH, Shanks JH, David G, McGown AT, Swindell R, et al. Distribution and clinical significance of heparan sulfate proteoglycans in ovarian cancer. Clin Cancer Res (2004) 10(15):5178–86. 10.1158/1078-0432.CCR-03-0103 [DOI] [PubMed] [Google Scholar]
- 44.Hiltunen EL, Anttila M, Kultti A, Ropponen K, Penttinen J, Yliskoski M, et al. Elevated hyaluronan concentration without hyaluronidase activation in malignant epithelial ovarian tumors. Cancer Res (2002) 62(22):6410–3. [PubMed] [Google Scholar]
- 45.Yeo TK, Nagy JA, Yeo KT, Dvorak HF, Toole BP. Increased hyaluronan at sites of attachment to mesentery by CD44-positive mouse ovarian and breast tumor cells. Am J Pathol (1996) 148(6):1733–40. [PMC free article] [PubMed] [Google Scholar]
- 46.Catterall JB, Jones LM, Turner GA. Membrane protein glycosylation and CD44 content in the adhesion of human ovarian cancer cells to hyaluronan. Clin Exp Metastasis (1999) 17(7):583–91. 10.1023/A:1006756518500 [DOI] [PubMed] [Google Scholar]
- 47.Casey RC, Skubitz AP. CD44 and beta1 integrins mediate ovarian carcinoma cell migration toward extracellular matrix proteins. Clin Exp Metastasis (2000) 18(1):67–75. 10.1023/A:1026519016213 [DOI] [PubMed] [Google Scholar]
- 48.Ricciardelli C, Ween MP, Lokman NA, Tan IA, Pyragius CE, Oehler MK. Chemotherapy-induced hyaluronan production: a novel chemoresistance mechanism in ovarian cancer. BMC Cancer (2013) 13:476. 10.1186/1471-2407-13-476 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Auzenne E, Ghosh SC, Khodadadian M, Rivera B, Farquhar D, Price RE, et al. Hyaluronic acid-paclitaxel: antitumor efficacy against CD44(+) human ovarian carcinoma xenografts. Neoplasia (2007) 9(6):479–86. 10.1593/neo.07229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Banzato A, Bobisse S, Rondina M, Renier D, Bettella F, Esposito G, et al. A paclitaxel-hyaluronan bioconjugate targeting ovarian cancer affords a potent in vivo therapeutic activity. Clin Cancer Res (2008) 14(11):3598–606. 10.1158/1078-0432.CCR-07-2019 [DOI] [PubMed] [Google Scholar]
- 51.Carter EM, Raggio CL. Genetic and orthopedic aspects of collagen disorders. Curr Opin Pediatr (2009) 21(1):46–54. 10.1097/MOP.0b013e32832185c5 [DOI] [PubMed] [Google Scholar]
- 52.Grassel S, Bauer RJ. Collagen XVI in health and disease. Matrix Biol (2013) 32(2):64–73. 10.1016/j.matbio.2012.11.001 [DOI] [PubMed] [Google Scholar]
- 53.Ricard-Blum S. The collagen family. Cold Spring Harb Perspect Biol (2011) 3(1):a004978. 10.1101/cshperspect.a004978 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Zoumi A, Yeh A, Tromberg BJ. Imaging cells and extracellular matrix in vivo by using second-harmonic generation and two-photon excited fluorescence. Proc Natl Acad Sci USA (2002) 99(17):11014–9. 10.1073/pnas.172368799 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Adur J, Pelegati VB, de Thomaz AA, Baratti MO, Andrade LA, Carvalho HF, et al. Second harmonic generation microscopy as a powerful diagnostic imaging modality for human ovarian cancer. J Biophotonics (2014) 7(1–2):37–48. 10.1002/jbio.201200108 [DOI] [PubMed] [Google Scholar]
- 56.Provenzano PP, Eliceiri KW, Campbell JM, Inman DR, White JG, Keely PJ. Collagen reorganization at the tumor-stromal interface facilitates local invasion. BMC Med (2006) 4(1):38. 10.1186/1741-7015-4-38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Provenzano PP, Inman DR, Eliceiri KW, Knittel JG, Yan L, Rueden CT, et al. Collagen density promotes mammary tumor initiation and progression. BMC Med (2008) 6:11. 10.1186/1741-7015-6-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ursin G, Hovanessian-Larsen L, Parisky YR, Pike MC, Wu AH. Greatly increased occurrence of breast cancers in areas of mammographically dense tissue. Breast Cancer Res (2005) 7(5):R605–8. 10.1186/bcr1260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Egeblad M, Nakasone ES, Werb Z. Tumors as organs: complex tissues that interface with the entire organism. Dev Cell (2010) 18(6):884–901. 10.1016/j.devcel.2010.05.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Helleman J, Jansen MP, Span PN, van Staveren IL, Massuger LF, Meijer-van Gelder ME, et al. Molecular profiling of platinum resistant ovarian cancer. Int J Cancer (2006) 118(8):1963–71. 10.1002/ijc.21599 [DOI] [PubMed] [Google Scholar]
- 61.Jazaeri AA, Awtrey CS, Chandramouli GV, Chuang YE, Khan J, Sotiriou C, et al. Gene expression profiles associated with response to chemotherapy in epithelial ovarian cancers. Clin Cancer Res (2005) 11(17):6300–10. 10.1158/1078-0432.CCR-04-2682 [DOI] [PubMed] [Google Scholar]
- 62.Sherman-Baust CA, Weeraratna AT, Rangel LB, Pizer ES, Cho KR, Schwartz DR, et al. Remodeling of the extracellular matrix through overexpression of collagen VI contributes to cisplatin resistance in ovarian cancer cells. Cancer Cell (2003) 3(4):377–86. 10.1016/S1535-6108(03)00058-8 [DOI] [PubMed] [Google Scholar]
- 63.Smoter M, Bodnar L, Grala B, Stec R, Zieniuk K, Kozlowski W, et al. Tau protein as a potential predictive marker in epithelial ovarian cancer patients treated with paclitaxel/platinum first-line chemotherapy. J Exp Clin Cancer Res (2013) 32:25. 10.1186/1756-9966-32-25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Kavallaris M, Kuo DY, Burkhart CA, Regl DL, Norris MD, Haber M, et al. Taxol-resistant epithelial ovarian tumors are associated with altered expression of specific beta-tubulin isotypes. J Clin Invest (1997) 100(5):1282–93. 10.1172/JCI119642 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Yoshioka H, Iyama K, Inoguchi K, Khaleduzzaman M, Ninomiya Y, Ramirez F. Developmental pattern of expression of the mouse alpha 1 (XI) collagen gene (Col11a1). Dev Dyn (1995) 204(1):41–7. 10.1002/aja.1002040106 [DOI] [PubMed] [Google Scholar]
- 66.Fischer H, Stenling R, Rubio C, Lindblom A. Colorectal carcinogenesis is associated with stromal expression of COL11A1 and COL5A2. Carcinogenesis (2001) 22(6):875–8. 10.1093/carcin/22.6.875 [DOI] [PubMed] [Google Scholar]
- 67.Fischer H, Salahshor S, Stenling R, Björk J, Lindmark G, Iselius L, et al. COL11A1 in FAP polyps and in sporadic colorectal tumors. BMC Cancer (2001) 1:17. 10.1186/1471-2407-1-17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Imamura Y, Scott IC, Greenspan DS. The pro-alpha3(V) collagen chain. Complete primary structure, expression domains in adult and developing tissues, and comparison to the structures and expression domains of the other types V and XI procollagen chains. J Biol Chem (2000) 275(12):8749–59. 10.1074/jbc.275.12.8749 [DOI] [PubMed] [Google Scholar]
- 69.Ritzenthaler JD, Han S, Roman J. Stimulation of lung carcinoma cell growth by fibronectin-integrin signalling. Mol Biosyst (2008) 4(12):1160–9. 10.1039/b800533h [DOI] [PubMed] [Google Scholar]
- 70.Williams CM, Engler AJ, Slone RD, Galante LL, Schwarzbauer JE. Fibronectin expression modulates mammary epithelial cell proliferation during acinar differentiation. Cancer Res (2008) 68(9):3185–92. 10.1158/0008-5472.CAN-07-2673 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Desgrosellier JS, Cheresh DA. Integrins in cancer: biological implications and therapeutic opportunities. Nat Rev Cancer (2010) 10(1):9–22. 10.1038/nrc2748 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Sakai T, Johnson KJ, Murozono M, Sakai K, Magnuson MA, Wieloch T, et al. Plasma fibronectin supports neuronal survival and reduces brain injury following transient focal cerebral ischemia but is not essential for skin-wound healing and hemostasis. Nat Med (2001) 7(3):324–30. 10.1038/85471 [DOI] [PubMed] [Google Scholar]
- 73.Tucker RP, Chiquet-Ehrismann R. The regulation of tenascin expression by tissue microenvironments. Biochim Biophys Acta (2009) 1793(5):888–92. 10.1016/j.bbamcr.2008.12.012 [DOI] [PubMed] [Google Scholar]
- 74.Jones FS, Jones PL. The tenascin family of ECM glycoproteins: structure, function, and regulation during embryonic development and tissue remodeling. Dev Dyn (2000) 218(2):235–59. [DOI] [PubMed] [Google Scholar]
- 75.Didem T, Faruk T, Senem K, Derya D, Murat S, Murat G, et al. Clinical significance of serum tenascin-c levels in epithelial ovarian cancer. Tumour Biol (2014) 35(7):6777–82. 10.1007/s13277-014-1923-z [DOI] [PubMed] [Google Scholar]
- 76.Orend G, Chiquet-Ehrismann R. Tenascin-C induced signaling in cancer. Cancer Lett (2006) 244(2):143–63. 10.1016/j.canlet.2006.02.017 [DOI] [PubMed] [Google Scholar]
- 77.Hsia HC, Schwarzbauer JE. Meet the tenascins: multifunctional and mysterious. J Biol Chem (2005) 280(29):26641–4. 10.1074/jbc.R500005200 [DOI] [PubMed] [Google Scholar]
- 78.Mithieux SM, Weiss AS. Elastin. Adv Protein Chem (2005) 70:437–61. 10.1016/S0065-3233(05)70013-9 [DOI] [PubMed] [Google Scholar]
- 79.Petersen E, Wågberg F, Ängquist KA. Serum concentrations of elastin-derived peptides in patients with specific manifestations of atherosclerotic disease. Eur J Vasc Endovasc Surg (2002) 24(5):440–4. 10.1053/ejvs.2002.1750 [DOI] [PubMed] [Google Scholar]
- 80.Kagan HM, Sullivan KA. Lysyl oxidase: preparation and role in elastin biosynthesis. Methods Enzymol. (1982) 82(Pt A):637–50. 10.1016/0076-6879(82)82092-2 [DOI] [PubMed] [Google Scholar]
- 81.Lapis K, Tímár J. Role of elastin-matrix interactions in tumor progression. Semin Cancer Biol (2002) 12(3):209–17. 10.1016/S1044-579X(02)00024-X [DOI] [PubMed] [Google Scholar]
- 82.Toupance S, Brassart B, Rabenoelina F, Ghoneim C, Vallar L, Polette M, et al. Elastin-derived peptides increase invasive capacities of lung cancer cells by post-transcriptional regulation of MMP-2 and uPA. Clin Exp Metastasis (2012) 29(5):511–22. 10.1007/s10585-012-9467-3 [DOI] [PubMed] [Google Scholar]
- 83.Devy J, Duca L, Cantarelli B, Joseph-Pietras D, Scandolera A, Rusciani A, et al. Elastin-derived peptides enhance melanoma growth in vivo by upregulating the activation of Mcol-A (MMP-1) collagenase. Br J Cancer (2010) 103(10):1562–70. 10.1038/sj.bjc.6605926 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Stewart CJ, Brennan BA, Crook ML, Russell P. Value of elastin staining in the assessment of peritoneal implants associated with ovarian serous borderline tumours. Histopathology (2007) 51(3):313–21. 10.1111/j.1365-2559.2007.02789.x [DOI] [PubMed] [Google Scholar]
- 85.Colognato H, Yurchenco PD. Form and function: the laminin family of heterotrimers. Dev Dyn (2000) 218(2):213–34. [DOI] [PubMed] [Google Scholar]
- 86.Hamill KJ, Kligys K, Hopkinson SB, Jones JC. Laminin deposition in the extracellular matrix: a complex picture emerges. J Cell Sci (2009) 122(Pt 24):4409–17. 10.1242/jcs.041095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Aumailley M, Bruckner-Tuderman L, Carter WG, Deutzmann R, Edgar D, Ekblom P, et al. A simplified laminin nomenclature. Matrix Biol (2005) 24(5):326–32. 10.1016/j.matbio.2005.05.006 [DOI] [PubMed] [Google Scholar]
- 88.Tzu J, Marinkovich MP. Bridging structure with function: structural, regulatory, and developmental role of laminins. Int J Biochem Cell Biol (2008) 40(2):199–214. 10.1016/j.biocel.2007.07.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Yurchenco PD, Quan Y, Colognato H, Mathus T, Harrison D, Yamada Y, et al. The α chain of laminin-1 is independently secreted and drives secretion of its β- and γ-chain partners. Proc Natl Acad Sci U S A (1997) 94(19):10189–94. 10.1073/pnas.94.19.10189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Lee VH, Britt JH, Dunbar BS. Localization of laminin proteins during early follicular development in pig and rabbit ovaries. J Reprod Fertil (1996) 108(1):115–22. 10.1530/jrf.0.1080115 [DOI] [PubMed] [Google Scholar]
- 91.Iozzo RV, Schaefer L. Proteoglycan form and function: a comprehensive nomenclature of proteoglycans. Matrix Biol (2015) 42(0):11–55. 10.1016/j.matbio.2015.02.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Brezillon S, Zeltz C, Schneider L, Terryn C, Vuillermoz B, Ramont L, et al. Lumican inhibits B16F1 melanoma cell lung metastasis. J Physiol Pharmacol (2009) 60(Suppl 4):15–22. [PubMed] [Google Scholar]
- 93.Dellett M, Hu W, Papadaki V, Ohnuma S. Small leucine rich proteoglycan family regulates multiple signalling pathways in neural development and maintenance. Dev Growth Differ (2012) 54(3):327–40. 10.1111/j.1440-169X.2012.01339.x [DOI] [PubMed] [Google Scholar]
- 94.Melchior-Becker A, Dai G, Ding Z, Schäfer L, Schrader J, Young MF, et al. Deficiency of biglycan causes cardiac fibroblasts to differentiate into a myofibroblast phenotype. J Biol Chem (2011) 286(19):17365–75. 10.1074/jbc.M110.192682 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Nikitovic D, Berdiaki K, Chalkiadaki G, Karamanos N, Tzanakakis G. The role of SLRP-proteoglycans in osteosarcoma pathogenesis. Connect Tissue Res (2008) 49(3):235–8. 10.1080/03008200802147589 [DOI] [PubMed] [Google Scholar]
- 96.Shimizu-Hirota R, Sasamura H, Kuroda M, Kobayashi E, Hayashi M, Saruta T. Extracellular matrix glycoprotein biglycan enhances vascular smooth muscle cell proliferation and migration. Circ Res (2004) 94(8):1067–74. 10.1161/01.RES.0000126049.79800.CA [DOI] [PubMed] [Google Scholar]
- 97.Iozzo RV. The biology of the small leucine-rich proteoglycans. Functional network of interactive proteins. J Biol Chem (1999) 274(27):18843–6. [DOI] [PubMed] [Google Scholar]
- 98.Kalamajski S, Oldberg A. Homologous sequence in lumican and fibromodulin leucine-rich repeat 5-7 competes for collagen binding. J Biol Chem (2009) 284(1):534–9. 10.1074/jbc.M805721200 [DOI] [PubMed] [Google Scholar]
- 99.Kalamajski S, Oldberg A. The role of small leucine-rich proteoglycans in collagen fibrillogenesis. Matrix Biol (2010) 29(4):248–53. 10.1016/j.matbio.2010.01.001 [DOI] [PubMed] [Google Scholar]
- 100.Kresse H, Liszio C, Schönherr E, Fisher LW. Critical role of glutamate in a central leucine-rich repeat of decorin for interaction with type I collagen. J Biol Chem (1997) 272(29):18404–10. 10.1074/jbc.272.29.18404 [DOI] [PubMed] [Google Scholar]
- 101.Neame PJ, Kay CJ, McQuillan DJ, Beales MP, Hassell JR. Independent modulation of collagen fibrillogenesis by decorin and lumican. Cell Mol Life Sci (2000) 57(5):859–63. 10.1007/s000180050048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Reinboth B, Thomas J, Hanssen E, Gibson MA. Beta ig-h3 interacts directly with biglycan and decorin, promotes collagen VI aggregation, and participates in ternary complexing with these macromolecules. J Biol Chem (2006) 281(12):7816–24. 10.1074/jbc.M511316200 [DOI] [PubMed] [Google Scholar]
- 103.Keene DR, San Antonio JD, Mayne R, McQuillan DJ, Sarris G, Santoro SA, et al. Decorin binds near the C terminus of type I collagen. J Biol Chem (2000) 275(29):21801–4. 10.1074/jbc.C000278200 [DOI] [PubMed] [Google Scholar]
- 104.Iozzo RV. The family of the small leucine-rich proteoglycans: key regulators of matrix assembly and cellular growth. Crit Rev Biochem Mol Biol (1997) 32(2):141–74. 10.3109/10409239709108551 [DOI] [PubMed] [Google Scholar]
- 105.Iozzo RV, Cohen I. Altered proteoglycan gene expression and the tumor stroma. EXS (1994) 70:199–214. [DOI] [PubMed] [Google Scholar]
- 106.McDoniels-Silvers AL, Nimri CF, Stoner GD, Lubet RA, You M. Differential gene expression in human lung adenocarcinomas and squamous cell carcinomas. Clin Cancer Res (2002) 8(4):1127–38. [PubMed] [Google Scholar]
- 107.Troup S, Njue C, Kliewer EV, Parisien M, Roskelley C, Chakravarti S, et al. Reduced expression of the small leucine-rich proteoglycans, lumican, and decorin is associated with poor outcome in node-negative invasive breast cancer. Clin Cancer Res (2003) 9(1):207–14. [PubMed] [Google Scholar]
- 108.Merle B, Durussel L, Delmas PD, Clézardin P. Decorin inhibits cell migration through a process requiring its glycosaminoglycan side chain. J Cell Biochem (1999) 75(3):538–46. [DOI] [PubMed] [Google Scholar]
- 109.Nash MA, Loercher AE, Freedman RS. In vitro growth inhibition of ovarian cancer cells by decorin: synergism of action between decorin and carboplatin. Cancer Res (1999) 59(24):6192–6. [PubMed] [Google Scholar]
- 110.Teicher BA, Maehara Y, Kakeji Y, Ara G, Keyes SR, Wong J, et al. Reversal of in vivo drug resistance by the transforming growth factor-beta inhibitor decorin. Int J Cancer (1997) 71(1):49–58. [DOI] [PubMed] [Google Scholar]
- 111.Hirsch CS, Ellner JJ, Blinkhorn R, Toossi Z. In vitro restoration of T cell responses in tuberculosis and augmentation of monocyte effector function against Mycobacterium tuberculosis by natural inhibitors of transforming growth factor beta. Proc Natl Acad Sci U S A (1997) 94(8):3926–31. 10.1073/pnas.94.8.3926 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Iozzo RV, Moscatello DK, McQuillan DJ, Eichstetter I. Decorin is a biological ligand for the epidermal growth factor receptor. J Biol Chem (1999) 274(8):4489–92. 10.1074/jbc.274.8.4489 [DOI] [PubMed] [Google Scholar]
- 113.Moscatello DK, Santra M, Mann DM, McQuillan DJ, Wong AJ, Iozzo RV. Decorin suppresses tumor cell growth by activating the epidermal growth factor receptor. J Clin Invest (1998) 101(2):406–12. 10.1172/JCI846 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Santra M, Reed CC, Iozzo RV. Decorin binds to a narrow region of the epidermal growth factor (EGF) receptor, partially overlapping but distinct from the EGF-binding epitope. J Biol Chem (2002) 277(38):35671–81. 10.1074/jbc.M205317200 [DOI] [PubMed] [Google Scholar]
- 115.Santra M, Eichstetter I, Iozzo RV. An anti-oncogenic role for decorin. Down-regulation of ErbB2 leads to growth suppression and cytodifferentiation of mammary carcinoma cells. J Biol Chem (2000) 275(45):35153–61. 10.1074/jbc.M006821200 [DOI] [PubMed] [Google Scholar]
- 116.Csordás G, Santra M, Reed CC, Eichstetter I, McQuillan DJ, Gross D, et al. Sustained down-regulation of the epidermal growth factor receptor by decorin. A mechanism for controlling tumor growth in vivo. J Biol Chem (2000) 275(42):32879–87. 10.1074/jbc.M005609200 [DOI] [PubMed] [Google Scholar]
- 117.Seidler DG, Goldoni S, Agnew C, Cardi C, Thakur ML, Owens RT, et al. Decorin protein core inhibits in vivo cancer growth and metabolism by hindering epidermal growth factor receptor function and triggering apoptosis via caspase-3 activation. J Biol Chem (2006) 281(36):26408–18. 10.1074/jbc.M602853200 [DOI] [PubMed] [Google Scholar]
- 118.Vij N, Roberts L, Joyce S, Chakravarti S. Lumican regulates corneal inflammatory responses by modulating Fas-Fas ligand signaling. Invest Ophthalmol Vis Sci (2005) 46(1):88–95. 10.1167/iovs.04-0833 [DOI] [PubMed] [Google Scholar]
- 119.Vuillermoz B, Khoruzhenko A, D’Onofrio MF, Ramont L, Venteo L, Perreau C, et al. The small leucine-rich proteoglycan lumican inhibits melanoma progression. Exp Cell Res (2004) 296(2):294–306. 10.1016/j.yexcr.2004.02.005 [DOI] [PubMed] [Google Scholar]
- 120.Albig AR, Roy TG, Becenti DJ, Schiemann WP. Transcriptome analysis of endothelial cell gene expression induced by growth on matrigel matrices: identification and characterization of MAGP-2 and lumican as novel regulators of angiogenesis. Angiogenesis (2007) 10(3):197–216. 10.1007/s10456-007-9075-z [DOI] [PubMed] [Google Scholar]
- 121.Naito Z. Role of the small leucine-rich proteoglycan (SLRP) family in pathological lesions and cancer cell growth. J Nippon Med Sch (2005) 72(3):137–45. 10.1272/jnms.72.137 [DOI] [PubMed] [Google Scholar]
- 122.Leygue E, Snell L, Dotzlaw H, Troup S, Hiller-Hitchcock T, Murphy LC, et al. Lumican and decorin are differentially expressed in human breast carcinoma. J Pathol (2000) 192(3):313–20. [DOI] [PubMed] [Google Scholar]
- 123.Matsuda Y, Yamamoto T, Kudo M, Kawahara K, Kawamoto M, Nakajima Y, et al. Expression and roles of lumican in lung adenocarcinoma and squamous cell carcinoma. Int J Oncol (2008) 33(6):1177–85. 10.3892/ijo_00000107 [DOI] [PubMed] [Google Scholar]
- 124.Lu YP, Ishiwata T, Kawahara K, Watanabe M, Naito Z, Moriyama Y, et al. Expression of lumican in human colorectal cancer cells. Pathol Int (2002) 52(8):519–26. 10.1046/j.1440-1827.2002.01384.x [DOI] [PubMed] [Google Scholar]
- 125.Seya T, Tanaka N, Shinji S, Yokoi K, Koizumi M, Teranishi N, et al. Lumican expression in advanced colorectal cancer with nodal metastasis correlates with poor prognosis. Oncol Rep (2006) 16(6):1225–30. 10.3892/or.16.6.1225 [DOI] [PubMed] [Google Scholar]
- 126.Köninger J, Giese T, di Mola FF, Wente MN, Esposito I, Bachem MG, et al. Pancreatic tumor cells influence the composition of the extracellular matrix. Biochem Biophys Res Commun (2004) 322(3):943–9. 10.1016/j.bbrc.2004.08.008 [DOI] [PubMed] [Google Scholar]
- 127.Leygue E, Snell L, Dotzlaw H, Hole K, Hiller-Hitchcock T, Roughley PJ, et al. Expression of lumican in human breast carcinoma. Cancer Res (1998) 58(7):1348–52. [PubMed] [Google Scholar]
- 128.Ishiwata T, Cho K, Kawahara K, Yamamoto T, Fujiwara Y, Uchida E, et al. Role of lumican in cancer cells and adjacent stromal tissues in human pancreatic cancer. Oncol Rep (2007) 18(3):537–43. 10.3892/or.18.3.537 [DOI] [PubMed] [Google Scholar]
- 129.Shinji S, Naito Z, Ishiwata T, Tanaka N, Furukawa K, Suzuki H, et al. Neuroendocrine cell differentiation of poorly differentiated colorectal adenocarcinoma correlates with liver metastasis. Int J Oncol (2006) 29(2):357–64. 10.3892/ijo.29.2.357 [DOI] [PubMed] [Google Scholar]
- 130.Russell DL, Ochsner SA, Hsieh M, Mulders S, Richards JS. Hormone-regulated expression and localization of versican in the rodent ovary. Endocrinology (2003) 144(3):1020–31. 10.1210/en.2002-220434 [DOI] [PubMed] [Google Scholar]
- 131.Cattaruzza S, Schiappacassi M, Ljungberg-Rose A, Spessotto P, Perissinotto D, Mörgelin M, et al. Distribution of PG-M/versican variants in human tissues and de novo expression of isoform V3 upon endothelial cell activation, migration, and neoangiogenesis in vitro. J Biol Chem (2002) 277(49):47626–35. 10.1074/jbc.M206521200 [DOI] [PubMed] [Google Scholar]
- 132.Häkkinen L, Westermarck J, Kähäri VM, Larjava H. Human granulation-tissue fibroblasts show enhanced proteoglycan gene expression and altered response to TGF-beta 1. J Dent Res (1996) 75(10):1767–78. 10.1177/00220345960750101001 [DOI] [PubMed] [Google Scholar]
- 133.Isogai Z, Shinomura T, Yamakawa N, Takeuchi J, Tsuji T, Heinegård D, et al. 2B1 antigen characteristically expressed on extracellular matrices of human malignant tumors is a large chondroitin sulfate proteoglycan, PG-M/versican. Cancer Res (1996) 56(17):3902–8. [PubMed] [Google Scholar]
- 134.Theocharis AD. Human colon adenocarcinoma is associated with specific post-translational modifications of versican and decorin. Biochim Biophys Acta (2002) 1588(2):165–72. 10.1016/S0925-4439(02)00161-8 [DOI] [PubMed] [Google Scholar]
- 135.Theocharis AD, Vynios DH, Papageorgakopoulou N, Skandalis SS, Theocharis DA. Altered content composition and structure of glycosaminoglycans and proteoglycans in gastric carcinoma. Int J Biochem Cell Biol (2003) 35(3):376–90. 10.1016/S1357-2725(02)00264-9 [DOI] [PubMed] [Google Scholar]
- 136.Tsara ME, Theocharis AD, Theocharis DA. Compositional and structural alterations of proteoglycans in human rectum carcinoma with special reference to versican and decorin. Anticancer Res (2002) 22(5):2893–8. [PubMed] [Google Scholar]
- 137.Touab M, Villena J, Barranco C, Arumí-Uría M, Bassols A. Versican is differentially expressed in human melanoma and may play a role in tumor development. Am J Pathol (2002) 160(2):549–57. 10.1016/S0002-9440(10)64874-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Ito Y, Abiko Y, Tanaka Y, Rahemtulla F, Kaku T. Immunohistochemical localization of large chondroitin sulfate proteoglycan in odontogenic tumor. Med Electron Microsc (2002) 35(3):173–7. 10.1007/s007950200022 [DOI] [PubMed] [Google Scholar]
- 139.Nara Y, Kato Y, Torii Y, Tsuji Y, Nakagaki S, Goto S, et al. Immunohistochemical localization of extracellular matrix components in human breast tumours with special reference to PG-M/versican. Histochem J (1997) 29(1):21–30. 10.1023/A:1026460700592 [DOI] [PubMed] [Google Scholar]
- 140.Brown LF, Guidi AJ, Schnitt SJ, Van De Water L, Iruela-Arispe ML, Yeo TK, et al. Vascular stroma formation in carcinoma in situ, invasive carcinoma, and metastatic carcinoma of the breast. Clin Cancer Res (1999) 5(5):1041–56. [PubMed] [Google Scholar]
- 141.Dobra K, Andäng M, Syrokou A, Karamanos NK, Hjerpe A. Differentiation of mesothelioma cells is influenced by the expression of proteoglycans. Exp Cell Res (2000) 258(1):12–22. 10.1006/excr.2000.4915 [DOI] [PubMed] [Google Scholar]
- 142.Dours-Zimmermann MT, Zimmermann DR. A novel glycosaminoglycan attachment domain identified in two alternative splice variants of human versican. J Biol Chem (1994) 269(52):32992–8. [PubMed] [Google Scholar]
- 143.Bouterfa H, Darlapp AR, Klein E, Pietsch T, Roosen K, Tonn JC. Expression of different extracellular matrix components in human brain tumor and melanoma cells in respect to variant culture conditions. J Neurooncol (1999) 44(1):23–33. 10.1023/A:1006331416283 [DOI] [PubMed] [Google Scholar]
- 144.Sharma B, Handler M, Eichstetter I, Whitelock JM, Nugent MA, Iozzo RV. Antisense targeting of perlecan blocks tumor growth and angiogenesis in vivo. J Clin Invest (1998) 102(8):1599–608. 10.1172/JCI3793 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Iozzo RV, San Antonio JD. Heparan sulfate proteoglycans: heavy hitters in the angiogenesis arena. J Clin Invest (2001) 108(3):349–55. 10.1172/JCI200113738 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Cohen IR, Murdoch AD, Naso MF, Marchetti D, Berd D, Iozzo RV. Abnormal expression of perlecan proteoglycan in metastatic melanomas. Cancer Res (1994) 54(22):5771–4. [PubMed] [Google Scholar]
- 147.Datta MW, Hernandez AM, Schlicht MJ, Kahler AJ, DeGueme AM, Dhir R, et al. Perlecan, a candidate gene for the CAPB locus, regulates prostate cancer cell growth via the sonic hedgehog pathway. Mol Cancer (2006) 5:9. 10.1186/1476-4598-5-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Iozzo RV, Cohen IR, Grässel S, Murdoch AD. The biology of perlecan: the multifaceted heparan sulphate proteoglycan of basement membranes and pericellular matrices. Biochem J (1994) 302(Pt 3):625–39. 10.1042/bj3020625 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Blackhall FH, Merry CL, Davies EJ, Jayson GC. Heparan sulfate proteoglycans and cancer. Br J Cancer (2001) 85(8):1094–8. 10.1054/bjoc.2001.2054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Sanderson RD. Heparan sulfate proteoglycans in invasion and metastasis. Semin Cell Dev Biol (2001) 12(2):89–98. 10.1006/scdb.2000.0241 [DOI] [PubMed] [Google Scholar]
- 151.Aviezer D, Iozzo RV, Noonan DM, Yayon A. Suppression of autocrine and paracrine functions of basic fibroblast growth factor by stable expression of perlecan antisense cDNA. Mol Cell Biol (1997) 17(4):1938–46. 10.1128/MCB.17.4.1938 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Evanko SP, Potter-Perigo S, Petty LJ, Workman GA, Wight TN. Hyaluronan controls the deposition of fibronectin and collagen and modulates TGF-β1 induction of lung myofibroblasts. Matrix Biol (2015) 42:74–92. 10.1016/j.matbio.2014.12.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Laterra J, Culp LA. Differences in hyaluronate binding to plasma and cell surface fibronectins. Requirement for aggregation. J Biol Chem (1982) 257(2):719–26. [PubMed] [Google Scholar]
- 154.Yamada KM, Kennedy DW, Kimata K, Pratt RM. Characterization of fibronectin interactions with glycosaminoglycans and identification of active proteolytic fragments. J Biol Chem (1980) 255(13):6055–63. [PubMed] [Google Scholar]
- 155.Coleman PJ. Evidence for a role of hyaluronan in the spacing of fibrils within collagen bundles in rabbit synovium. Biochim Biophys Acta (2002) 1571(3):173–82. 10.1016/S0304-4165(02)00213-1 [DOI] [PubMed] [Google Scholar]
- 156.Toole BP. Hyaluronan: from extracellular glue to pericellular cue. Nat Rev Cancer (2004) 4(7):528–39. 10.1038/nrc1391 [DOI] [PubMed] [Google Scholar]
- 157.Evanko SP, Tammi MI, Tammi RH, Wight TN. Hyaluronan-dependent pericellular matrix. Adv Drug Deliv Rev (2007) 59(13):1351–65. 10.1016/j.addr.2007.08.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Itano N. Simple primary structure, complex turnover regulation and multiple roles of hyaluronan. J Biochem (2008) 144(2):131–7. 10.1093/jb/mvn046 [DOI] [PubMed] [Google Scholar]
- 159.Hascall VC, Heinegard D. Aggregation of cartilage proteoglycans. I. The role of hyaluronic acid. J Biol Chem (1974) 249(13):4232–41. [PubMed] [Google Scholar]
- 160.Bonnet F, Dunham DG, Hardingham TE. Structure and interactions of cartilage proteoglycan binding region and link protein. Biochem J (1985) 228(1):77–85. 10.1042/bj2280077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Mörgelin M, Paulsson M, Hardingham TE, Heinegård D, Engel J. Cartilage proteoglycans. Assembly with hyaluronate and link protein as studied by electron microscopy. Biochem J (1988) 253(1):175–85. 10.1042/bj2530175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Toole BP, Wight TN, Tammi MI. Hyaluronan-cell interactions in cancer and vascular disease. J Biol Chem (2002) 277(7):4593–6. 10.1074/jbc.R100039200 [DOI] [PubMed] [Google Scholar]
- 163.Tammi RH, Kultti A, Kosma VM, Pirinen R, Auvinen P, Tammi MI. Hyaluronan in human tumors: pathobiological and prognostic messages from cell-associated and stromal hyaluronan. Semin Cancer Biol (2008) 18(4):288–95. 10.1016/j.semcancer.2008.03.005 [DOI] [PubMed] [Google Scholar]
- 164.Itano N, Zhuo L, Kimata K. Impact of the hyaluronan-rich tumor microenvironment on cancer initiation and progression. Cancer Sci (2008) 99(9):1720–5. 10.1111/j.1349-7006.2008.00885.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Tolg C, Hamilton SR, Zalinska E, McCulloch L, Amin R, Akentieva N, et al. A RHAMM mimetic peptide blocks hyaluronan signaling and reduces inflammation and fibrogenesis in excisional skin wounds. Am J Pathol (2012) 181(4):1250–70. 10.1016/j.ajpath.2012.06.036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Tolg C, McCarthy JB, Yazdani A, Turley EA. Hyaluronan and RHAMM in wound repair and the “cancerization” of stromal tissues. Biomed Res Int (2014) 2014:103923. 10.1155/2014/103923 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Dahl IM, Laurent TC. Concentration of hyaluronan in the serum of untreated cancer patients with special reference to patients with mesothelioma. Cancer (1988) 62(2):326–30. [DOI] [PubMed] [Google Scholar]
- 168.Delpech B, Bertrand P, Maingonnat C. Immunoenzymoassay of the hyaluronic acid-hyaluronectin interaction: application to the detection of hyaluronic acid in serum of normal subjects and cancer patients. Anal Biochem (1985) 149(2):555–65. 10.1016/0003-2697(85)90613-X [DOI] [PubMed] [Google Scholar]
- 169.Yahya RS, El-Bindary AA, El-Mezayen HA, Abdelmasseh HM, Eissa MA. Biochemical evaluation of hyaluronic acid in breast cancer. Clin Lab (2014) 60(7):1115–21. 10.7754/Clin.Lab.2013.130413 [DOI] [PubMed] [Google Scholar]
- 170.Wu M, Cao M, He Y, Liu Y, Yang C, Du Y, et al. A novel role of low molecular weight hyaluronan in breast cancer metastasis. FASEB J (2015) 29(4):1290–8. 10.1096/fj.14-259978 [DOI] [PubMed] [Google Scholar]
- 171.Ween MP, Hummitzsch K, Rodgers RJ, Oehler MK, Ricciardelli C. Versican induces a pro-metastatic ovarian cancer cell behavior which can be inhibited by small hyaluronan oligosaccharides. Clin Exp Metastasis (2011) 28(2):113–25. 10.1007/s10585-010-9363-7 [DOI] [PubMed] [Google Scholar]
- 172.Vincent T, Molina L, Espert L, Mechti N. Hyaluronan, a major non-protein glycosaminoglycan component of the extracellular matrix in human bone marrow, mediates dexamethasone resistance in multiple myeloma. Br J Haematol (2003) 121(2):259–69. 10.1046/j.1365-2141.2003.04282.x [DOI] [PubMed] [Google Scholar]
- 173.Wang SJ, Bourguignon LY. Hyaluronan and the interaction between CD44 and epidermal growth factor receptor in oncogenic signaling and chemotherapy resistance in head and neck cancer. Arch Otolaryngol Head Neck Surg (2006) 132(7):771–8. 10.1001/archotol.132.7.771 [DOI] [PubMed] [Google Scholar]
- 174.Bourguignon LY, Peyrollier K, Xia W, Gilad E. Hyaluronan-CD44 interaction activates stem cell marker Nanog, Stat-3-mediated MDR1 gene expression, and ankyrin-regulated multidrug efflux in breast and ovarian tumor cells. J Biol Chem (2008) 283(25):17635–51. 10.1074/jbc.M800109200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Torre C, Wang SJ, Xia W, Bourguignon LY. Reduction of hyaluronan-CD44-mediated growth, migration, and cisplatin resistance in head and neck cancer due to inhibition of Rho kinase and PI-3 kinase signaling. Arch Otolaryngol Head Neck Surg (2010) 136(5):493–501. 10.1001/archoto.2010.25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Lu P, Takai K, Weaver VM, Werb Z. Extracellular matrix degradation and remodeling in development and disease. Cold Spring Harb Perspect Biol (2011) 3(12):a005058. 10.1101/cshperspect.a005058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Stack MS, Ellerbroek SM, Fishman DA. The role of proteolytic enzymes in the pathology of epithelial ovarian carcinoma. Int J Oncol (1998) 12(3):569–76. [DOI] [PubMed] [Google Scholar]
- 178.Kuhn W, Schmalfeldt B, Reuning U, Pache L, Berger U, Ulm K, et al. Prognostic significance of urokinase (uPA) and its inhibitor PAI-1 for survival in advanced ovarian carcinoma stage FIGO IIIc. Br J Cancer (1999) 79(11–12):1746–51. 10.1038/sj.bjc.6690278 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Ozalp S, Tanir HM, Yalcin OT, Kabukcuoglu S, Oner U, Uray M. Prognostic value of matrix metalloproteinase-9 (gelatinase-B) expression in epithelial ovarian tumors. Eur J Gynaecol Oncol (2003) 24(5):417–20. [PubMed] [Google Scholar]
- 180.Schmalfeldt B, Prechtel D, Härting K, Späthe K, Rutke S, Konik E, et al. Increased expression of matrix metalloproteinases (MMP)-2, MMP-9, and the urokinase-type plasminogen activator is associated with progression from benign to advanced ovarian cancer. Clin Cancer Res (2001) 7(8):2396–404. [PubMed] [Google Scholar]
- 181.Brun JL, Cortez A, Commo F, Uzan S, Rouzier R, Daraï E. Serous and mucinous ovarian tumors express different profiles of MMP-2, -7, -9, MT1-MMP, and TIMP-1 and -2. Int J Oncol (2008) 33(6):1239–46. 10.3892/ijo_00000114 [DOI] [PubMed] [Google Scholar]
- 182.Moser TL, Young TN, Rodriguez GC, Pizzo SV, Bast RC, Jr, Stack MS. Secretion of extracellular matrix-degrading proteinases is increased in epithelial ovarian carcinoma. Int J Cancer (1994) 56(4):552–9. 10.1002/ijc.2910560415 [DOI] [PubMed] [Google Scholar]
- 183.Young TN, Rodriguez GC, Rinehart AR, Bast RC, Jr, Pizzo SV, Stack MS. Characterization of gelatinases linked to extracellular matrix invasion in ovarian adenocarcinoma: purification of matrix metalloproteinase 2. Gynecol Oncol (1996) 62(1):89–99. 10.1006/gyno.1996.0195 [DOI] [PubMed] [Google Scholar]
- 184.Fishman DA, Bafetti LM, Banionis S, Kearns AS, Chilukuri K, Stack MS. Production of extracellular matrix-degrading proteinases by primary cultures of human epithelial ovarian carcinoma cells. Cancer (1997) 80:1457–63. [DOI] [PubMed] [Google Scholar]
- 185.Afzal S, Lalani el-N, Foulkes WD, Boyce B, Tickle S, Cardillo MR, et al. Matrix metalloproteinase-2 and tissue inhibitor of metalloproteinase-2 expression and synthetic matrix metalloproteinase-2 inhibitor binding in ovarian carcinomas and tumor cell lines. Lab Invest (1996) 74(2):406–21. [PubMed] [Google Scholar]
- 186.Wang L, Jin X, Lin D, Liu Z, Zhang X, Lu Y, et al. Clinicopathologic significance of claudin-6, occludin, and matrix metalloproteinases-2 expression in ovarian carcinoma. Diagn Pathol (2013) 8:190. 10.1186/1746-1596-8-190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Che YL, Luo SJ, Li G, Cheng M, Gao YM, Li XM, et al. The C3G/Rap1 pathway promotes secretion of MMP-2 and MMP-9 and is involved in serous ovarian cancer metastasis. Cancer Lett (2015) 359(2):241–9. 10.1016/j.canlet.2015.01.019 [DOI] [PubMed] [Google Scholar]
- 188.Sillanpää S, Anttila M, Voutilainen K, Ropponen K, Turpeenniemi-Hujanen T, Puistola U, et al. Prognostic significance of matrix metalloproteinase-9 (MMP-9) in epithelial ovarian cancer. Gynecol Oncol (2007) 104(2):296–303. 10.1016/j.ygyno.2006.09.004 [DOI] [PubMed] [Google Scholar]
- 189.Kamat AA, Fletcher M, Gruman LM, Mueller P, Lopez A, Landen CN, Jr, et al. The clinical relevance of stromal matrix metalloproteinase expression in ovarian cancer. Clin Cancer Res (2006) 12(6):1707–14. 10.1158/1078-0432.CCR-05-2338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Lengyel E, Schmalfeldt B, Konik E, Späthe K, Härting K, Fenn A, et al. Expression of latent matrix metalloproteinase 9 (MMP-9) predicts survival in advanced ovarian cancer. Gynecol Oncol (2001) 82(2):291–8. 10.1006/gyno.2001.6243 [DOI] [PubMed] [Google Scholar]
- 191.Sakata K, Shigemasa K, Nagai N, Ohama K. Expression of matrix metalloproteinases (MMP-2, MMP-9, MT1-MMP) and their inhibitors (TIMP-1, TIMP-2) in common epithelial tumors of the ovary. Int J Oncol (2000) 17(4):673–81. 10.3892/ijo.17.4.673 [DOI] [PubMed] [Google Scholar]
- 192.Hu X, Li D, Zhang W, Zhou J, Tang B, Li L. Matrix metalloproteinase-9 expression correlates with prognosis and involved in ovarian cancer cell invasion. Arch Gynecol Obstet (2012) 286(6):1537–43. 10.1007/s00404-012-2456-6 [DOI] [PubMed] [Google Scholar]
- 193.Wang FQ, So J, Reierstad S, Fishman DA. Matrilysin (MMP-7) promotes invasion of ovarian cancer cells by activation of progelatinase. Int J Cancer (2005) 114(1):19–31. 10.1002/ijc.20697 [DOI] [PubMed] [Google Scholar]
- 194.Zhao H, Yang Z, Wang X, Zhang X, Wang M, Wang Y, et al. Triptolide inhibits ovarian cancer cell invasion by repression of matrix metalloproteinase 7 and 19 and upregulation of E-cadherin. Exp Mol Med (2012) 44(11):633–41. 10.3858/emm.2012.44.11.072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Shigemasa K, Tanimoto H, Sakata K, Nagai N, Parmley TH, Ohama K, et al. Induction of matrix metalloprotease-7 is common in mucinous ovarian tumors including early stage disease. Med Oncol (2000) 17(1):52–8. 10.1007/BF02826217 [DOI] [PubMed] [Google Scholar]
- 196.Sillanpää SM, Anttila MA, Voutilainen KA, Ropponen KM, Sironen RK, Saarikoski SV, et al. Prognostic significance of matrix metalloproteinase-7 in epithelial ovarian cancer and its relation to beta-catenin expression. Int J Cancer (2006) 119(8):1792–9. 10.1002/ijc.22067 [DOI] [PubMed] [Google Scholar]
- 197.Wang X, Cong JL, Qu LY, Jiang L, Wang Y. Association between lysyl oxidase G473A polymorphism and ovarian cancer in the Han Chinese population. J Int Med Res (2012) 40(3):917–23. 10.1177/147323001204000310 [DOI] [PubMed] [Google Scholar]
- 198.Wu J, Cai C, Tong D, Hou H. Lysyl oxidase G473A polymorphism is associated with increased risk of ovarian cancer. Genet Test Mol Biomarkers (2012) 16(8):915–9. 10.1089/gtmb.2011.0374 [DOI] [PubMed] [Google Scholar]
- 199.Ji F, Wang Y, Qiu L, Li S, Zhu J, Liang Z, et al. Hypoxia inducible factor 1α-mediated LOX expression correlates with migration and invasion in epithelial ovarian cancer. Int J Oncol (2013) 42(5):1578–88. 10.3892/ijo.2013.1878 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Wang Y, Ma J, Shen H, Wang C, Sun Y, Howell SB, et al. Reactive oxygen species promote ovarian cancer progression via the HIF-1alpha/LOX/E-cadherin pathway. Oncol Rep (2014) 32(5):2150–8. 10.3892/or.2014.3448 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Barry-Hamilton V, Spangler R, Marshall D, McCauley S, Rodriguez HM, Oyasu M, et al. Allosteric inhibition of lysyl oxidase-like-2 impedes the development of a pathologic microenvironment. Nat Med (2010) 16(9):1009–17. 10.1038/nm.2208 [DOI] [PubMed] [Google Scholar]
- 202.Zaffryar-Eilot S, Marshall D, Voloshin T, Bar-Zion A, Spangler R, Kessler O, et al. Lysyl oxidase-like-2 promotes tumour angiogenesis and is a potential therapeutic target in angiogenic tumours. Carcinogenesis (2013) 34(10):2370–9. 10.1093/carcin/bgt241 [DOI] [PubMed] [Google Scholar]
- 203.Sebban S, Golan-Gerstl R, Karni R, Vaksman O, Davidson B, Reich R. Alternatively spliced lysyl oxidase-like 4 isoforms have a pro-metastatic role in cancer. Clin Exp Metastasis (2013) 30(1):103–17. 10.1007/s10585-012-9514-0 [DOI] [PubMed] [Google Scholar]
- 204.Yabushita H, Noguchi M, Kishida T, Fusano K, Noguchi Y, Itano N, et al. Hyaluronan synthase expression in ovarian cancer. Oncol Rep (2004) 12(4):739–43. 10.3892/or.12.4.739 [DOI] [PubMed] [Google Scholar]
- 205.Nykopp TK, Rilla K, Sironen R, Tammi MI, Tammi RH, Hämäläinen K, et al. Expression of hyaluronan synthases (HAS1-3) and hyaluronidases (HYAL1-2) in serous ovarian carcinomas: inverse correlation between HYAL1 and hyaluronan content. BMC Cancer (2009) 9:143. 10.1186/1471-2407-9-143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Weiss I, Trope CG, Reich R, Davidson B. Hyaluronan synthase and hyaluronidase expression in serous ovarian carcinoma is related to anatomic site and chemotherapy exposure. Int J Mol Sci (2012) 13(10):12925–38. 10.3390/ijms131012925 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Tuhkanen H, Anttila M, Kosma VM, Ylä-Herttuala S, Heinonen S, Kuronen A, et al. Genetic alterations in the peritumoral stromal cells of malignant and borderline epithelial ovarian tumors as indicated by allelic imbalance on chromosome 3p. Int J Cancer (2004) 109(2):247–52. 10.1002/ijc.11733 [DOI] [PubMed] [Google Scholar]
- 208.Yoffou PH, Edjekouane L, Meunier L, Tremblay A, Provencher DM, Mes-Masson AM, et al. Subtype specific elevated expression of hyaluronidase-1 (HYAL-1) in epithelial ovarian cancer. PLoS One (2011) 6(6):e20705. 10.1371/journal.pone.0020705 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Nagase H, Visse R, Murphy G. Structure and function of matrix metalloproteinases and TIMPs. Cardiovasc Res (2006) 69:562–73. 10.1016/j.cardiores.2005.12.002 [DOI] [PubMed] [Google Scholar]
- 210.Nagase H, Woessner JF., Jr Matrix metalloproteinases. J Biol Chem (1999) 274(31):21491–4. 10.1074/jbc.274.31.21491 [DOI] [PubMed] [Google Scholar]
- 211.Bhowmick NA, Neilson EG, Moses HL. Stromal fibroblasts in cancer initiation and progression. Nature (2004) 432(7015):332–7. 10.1038/nature03096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Kalluri R, Zeisberg M. Fibroblasts in cancer. Nat Rev Cancer (2006) 6(5):392–401. 10.1038/nrc1877 [DOI] [PubMed] [Google Scholar]
- 213.Cathcart J, Pulkoski-Gross A, Cao J. Targeting matrix metalloproteinases in cancer: bringing new life to old ideas. Genes Dis (2015) 2(1):26–34. 10.1016/j.gendis.2014.12.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Nelson AR, Fingleton B, Rothenberg ML, Matrisian LM. Matrix metalloproteinases: biologic activity and clinical implications. J Clin Oncol (2000) 18(5):1135. [DOI] [PubMed] [Google Scholar]
- 215.Tamakoshi K, Kikkawa F, Nawa A, Maeda O, Kawai M, Sugamuma N, et al. Different pattern of zymography between human gynecologic normal and malignant tissues. Am J Obstet Gynecol (1994) 171(2):478–84. 10.1016/0002-9378(94)90286-0 [DOI] [PubMed] [Google Scholar]
- 216.Yu Y, Li H, Xue B, Jiang X, Huang K, Ge J, et al. SDF-1/CXCR7 axis enhances ovarian cancer cell invasion by MMP-9 expression through p38 MAPK pathway. DNA Cell Biol (2014) 33(8):543–9. 10.1089/dna.2013.2289 [DOI] [PubMed] [Google Scholar]
- 217.Ii M, Yamamoto H, Adachi Y, Maruyama Y, Shinomura Y. Role of matrix metalloproteinase-7 (matrilysin) in human cancer invasion, apoptosis, growth, and angiogenesis. Exp Biol Med (Maywood) (2006) 231(1):20–7. [DOI] [PubMed] [Google Scholar]
- 218.Brew K, Nagase H. The tissue inhibitors of metalloproteinases (TIMPs): an ancient family with structural and functional diversity. Biochim Biophys Acta (2010) 1803(1):55–71. 10.1016/j.bbamcr.2010.01.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Nagase H, Murphy G. Tailoring TIMPs for selective metalloproteinase inhibition. In: Edwards D, et al., editors. The Cancer Degradome. New York, NY: Springer; (2008). p. 787–810. [Google Scholar]
- 220.Goldberg GI, Strongin A, Collier IE, Genrich LT, Marmer BL. Interaction of 92-kDa type IV collagenase with the tissue inhibitor of metalloproteinases prevents dimerization, complex formation with interstitial collagenase, and activation of the proenzyme with stromelysin. J Biol Chem (1992) 267(7):4583–91. [PubMed] [Google Scholar]
- 221.Stetler-Stevenson WG, Krutzsch HC, Liotta LA. Tissue inhibitor of metalloproteinase (TIMP-2). A new member of the metalloproteinase inhibitor family. J Biol Chem (1989) 264(29):17374–8. [PubMed] [Google Scholar]
- 222.Okamoto T, Niu R, Yamada S. Increased expression of tissue inhibitor of metalloproteinase-2 in clear cell carcinoma of the ovary. Mol Hum Reprod (2003) 9(10):569–75. 10.1093/molehr/gag074 [DOI] [PubMed] [Google Scholar]
- 223.Huang LW, Garrett AP, Bell DA, Welch WR, Berkowitz RS, Mok SC. Differential expression of matrix metalloproteinase-9 and tissue inhibitor of metalloproteinase-1 protein and mRNA in epithelial ovarian tumors. Gynecol Oncol (2000) 77(3):369–76. 10.1006/gyno.2000.5806 [DOI] [PubMed] [Google Scholar]
- 224.Obayashi Y, Yabushita H, Kanyama K, Noguchi M, Zhuo L, Kimata K, et al. Role of serum-derived hyaluronan-associated protein-hyaluronan complex in ovarian cancer. Oncol Rep (2008) 19(5):1245–51. 10.3892/or.19.5.1245 [DOI] [PubMed] [Google Scholar]
- 225.Kikkawa F, Tamakoshi K, Nawa A, Shibata K, Yamagata S, Yamagata T, et al. Positive correlation between inhibitors of matrix metalloproteinase 1 and matrix metalloproteinases in malignant ovarian tumor tissues. Cancer Lett (1997) 120(1):109–15. 10.1016/S0304-3835(97)00295-4 [DOI] [PubMed] [Google Scholar]
- 226.Kagan HM, Li W. Lysyl oxidase: properties, specificity, and biological roles inside and outside of the cell. J Cell Biochem (2003) 88(4):660–72. 10.1002/jcb.10413 [DOI] [PubMed] [Google Scholar]
- 227.Mäki JM. Lysyl oxidases in mammalian development and certain pathological conditions. Histol Histopathol (2009) 24:651–60. [DOI] [PubMed] [Google Scholar]
- 228.Li W, Nellaiappan K, Strassmaier T, Graham L, Thomas KM, Kagan HM. Localization and activity of lysyl oxidase within nuclei of fibrogeniccells. Proc Natl Acad Sci U S A (1997) 94(24):12817–22. 10.1073/pnas.94.24.12817 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Erler JT, Bennewith KL, Nicolau M, Dornhöfer N, Kong C, Le QT, et al. Lysyl oxidase is essential for hypoxia-induced metastasis. Nature (2006) 440(7088):1222–6. 10.1038/nature04695 [DOI] [PubMed] [Google Scholar]
- 230.Barker HE, Cox TR, Erler JT. The rationale for targeting the LOX family in cancer. Nat Rev Cancer (2012) 12(8):540–52. 10.1038/nrc3319 [DOI] [PubMed] [Google Scholar]
- 231.Himeno N. [Effect of prostaglandins on collagen synthesis in rabbit ovarian follicles during the ovulatory process]. Nihon Naibunpi Gakkai Zasshi (1986) 62(10):1181–93. [DOI] [PubMed] [Google Scholar]
- 232.Slee RB, Hillier SG, Largue P, Harlow CR, Miele G, Clinton M. Differentiation-dependent expression of connective tissue growth factor and lysyl oxidase messenger ribonucleic acids in rat granulosa cells. Endocrinology (2001) 142(3):1082–9. 10.1210/en.142.3.1082 [DOI] [PubMed] [Google Scholar]
- 233.Kendall NR, Marsters P, Scaramuzzi RJ, Campbell BK. Expression of lysyl oxidase and effect of copper chloride and ammonium tetrathiomolybdate on bovine ovarian follicle granulosa cells cultured in serum-free media. Reproduction (2003) 125(5):657–65. 10.1530/rep.0.1250657 [DOI] [PubMed] [Google Scholar]
- 234.Harlow CR, Rae M, Davidson L, Trackman PC, Hillier SG. Lysyl oxidase gene expression and enzyme activity in the rat ovary: regulation by follicle-stimulating hormone, androgen, and transforming growth factor-beta superfamily members in vitro. Endocrinology (2003) 144(1):154–62. 10.1210/en.2002-220652 [DOI] [PubMed] [Google Scholar]
- 235.Akiri G, Sabo E, Dafni H, Vadasz Z, Kartvelishvily Y, Gan N, et al. Lysyl oxidase-related protein-1 promotes tumor fibrosis and tumor progression in vivo. Cancer Res (2003) 63(7):1657–66. [PubMed] [Google Scholar]
- 236.Peinado H, Moreno-Bueno G, Hardisson D, Pérez-Gómez E, Santos V, Mendiola M, et al. Lysyl oxidase-like 2 as a new poor prognosis marker of squamous cell carcinomas. Cancer Res (2008) 68(12):4541–50. 10.1158/0008-5472.CAN-07-6345 [DOI] [PubMed] [Google Scholar]
- 237.Fong SF, Dietzsch E, Fong KS, Hollosi P, Asuncion L, He Q, et al. Lysyl oxidase-like 2 expression is increased in colon and esophageal tumors and associated with less differentiated colon tumors. Genes Chromosomes Cancer (2007) 46(7):644–55. 10.1002/gcc.20444 [DOI] [PubMed] [Google Scholar]
- 238.Goel S, Duda DG, Xu L, Munn LL, Boucher Y, Fukumura D, et al. Normalization of the vasculature for treatment of cancer and other diseases. Physiol Rev (2011) 91(3):1071–121. 10.1152/physrev.00038.2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Görögh T, Weise JB, Holtmeier C, Rudolph P, Hedderich J, Gottschlich S, et al. Selective upregulation and amplification of the lysyl oxidase like-4 (LOXL4) gene in head and neck squamous cell carcinoma. J Pathol (2007) 212(1):74–82. 10.1002/path.2137 [DOI] [PubMed] [Google Scholar]
- 240.Weise JB, Rudolph P, Heiser A, Kruse ML, Hedderich J, Cordes C, et al. LOXL4 is a selectively expressed candidate diagnostic antigen in head and neck cancer. Eur J Cancer (2008) 44(9):1323–31. 10.1016/j.ejca.2008.03.026 [DOI] [PubMed] [Google Scholar]
- 241.Li RK, Zhao WY, Fang F, Zhuang C, Zhang XX, Yang XM, et al. Lysyl oxidase-like 4 (LOXL4) promotes proliferation and metastasis of gastric cancer via FAK/Src pathway. J Cancer Res Clin Oncol (2015) 141(2):269–81. 10.1007/s00432-014-1823-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.DeAngelis PL. Hyaluronan synthases: fascinating glycosyltransferases from vertebrates, bacterial pathogens, and algal viruses. Cell Mol Life Sci (1999) 56(7–8):670–82. 10.1007/s000180050461 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Weigel PH, Hascall VC, Tammi M. Hyaluronan synthases. J Biol Chem (1997) 272(22):13997–4000. 10.1074/jbc.272.22.13997 [DOI] [PubMed] [Google Scholar]
- 244.Itano N, Sawai T, Yoshida M, Lenas P, Yamada Y, Imagawa M, et al. Three isoforms of mammalian hyaluronan synthases have distinct enzymatic properties. J Biol Chem (1999) 274(35):25085–92. 10.1074/jbc.274.35.25085 [DOI] [PubMed] [Google Scholar]
- 245.Itano N, Yamada Y, Yoshida M, Kimata K. [Cancer metastasis and extracellular matrix]. Gan To Kagaku Ryoho (1999) 26(11):1663–8. [PubMed] [Google Scholar]
- 246.Kimata K, Honma Y, Okayama M, Oguri K, Hozumi M, Suzuki S. Increased synthesis of hyaluronic acid by mouse mammary carcinoma cell variants with high metastatic potential. Cancer Res (1983) 43(3):1347–54. [PubMed] [Google Scholar]
- 247.Itano N, Sawai T, Miyaishi O, Kimata K. Relationship between hyaluronan production and metastatic potential of mouse mammary carcinoma cells. Cancer Res (1999) 59(10):2499–504. [PubMed] [Google Scholar]
- 248.Simpson MA, Reiland J, Burger SR, Furcht LT, Spicer AP, Oegema TR, Jr, et al. Hyaluronan synthase elevation in metastatic prostate carcinoma cells correlates with hyaluronan surface retention, a prerequisite for rapid adhesion to bone marrow endothelial cells. J Biol Chem (2001) 276(21):17949–57. 10.1074/jbc.M010064200 [DOI] [PubMed] [Google Scholar]
- 249.Simpson MA, Wilson CM, Furcht LT, Spicer AP, Oegema TR, Jr, McCarthy JB. Manipulation of hyaluronan synthase expression in prostate adenocarcinoma cells alters pericellular matrix retention and adhesion to bone marrow endothelial cells. J Biol Chem (2002) 277(12):10050–7. 10.1074/jbc.M110069200 [DOI] [PubMed] [Google Scholar]
- 250.Csoka AB, Frost GI, Stern R. The six hyaluronidase-like genes in the human and mouse genomes. Matrix Biol (2001) 20(8):499–508. 10.1016/S0945-053X(01)00172-X [DOI] [PubMed] [Google Scholar]
- 251.Stern R, Asari AA, Sugahara KN. Hyaluronan fragments: an information-rich system. Eur J Cell Biol (2006) 85(8):699–715. 10.1016/j.ejcb.2006.05.009 [DOI] [PubMed] [Google Scholar]
- 252.Montesano R, Kumar S, Orci L, Pepper MS. Synergistic effect of hyaluronan oligosaccharides and vascular endothelial growth factor on angiogenesis in vitro. Lab Invest (1996) 75(2):249–62. [PubMed] [Google Scholar]
- 253.Rozario T, DeSimone DW. The extracellular matrix in development and morphogenesis: a dynamic view. Dev Biol (2010) 341(1):126–40. 10.1016/j.ydbio.2009.10.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254.Moss EL, Hollingworth J, Reynolds TM. The role of CA125 in clinical practice. J Clin Pathol (2005) 58(3):308–12. 10.1136/jcp.2004.018077 [DOI] [PMC free article] [PubMed] [Google Scholar]