Objectives:
Our objective was to determine the impact that a patient's geographic status has on the efficacy of first-time methadone maintenance therapy (MMT) retention.
Methods:
We conducted an observational cohort study using administrative health care databases for patients who commenced methadone therapy between 2003 and 2012. Patients were stratified on the basis of their location of residence into 1 of 4 groups—Southern Urban, Southern Rural, Northern Urban, or Northern Rural. The primary outcome was continuous retention in treatment, defined as 1 year of uninterrupted therapy on the basis of prescription refill data. Mortality was measured as a secondary outcome.
Results:
We identified 17,211 patients initiating first-time MMT during this 10-year period. Nearly half of patients initiating therapy in northern regions completed 1 year of treatment (48.9%; N = 258 and 47.0%; N = 761 in Northern Rural and Urban regions, respectively), whereas lower rates of 40.6% (N = 410) and 39.3% (N = 5,518) occurred in Southern Rural and Urban regions, respectively. Patients residing in Northern Rural and Northern Urban regions were 31% (adjusted odds ratio = 1.31; 95% confidence interval [CI], 1.09%–1.58%] and 14% (adjusted odds ratio = 1.14; 95% CI, 1.02%–1.27%] more likely to be retained in treatment compared with those residing in Southern Urban regions. There was no significant difference in treatment retention between those residing in Southern Rural and Southern Urban regions. A mortality rate of 3% was observed within 1 year of patients initiating treatment, with patients in the Southern Rural region having the highest rate (4.85%).
Conclusions:
Our study identified regional differences in retention rates and mortality of first-time MMT. These findings may relate to geographic isolation and limited methadone program availability experienced in northern regions. We interpret the data to suggest that patients who have reduced access to treatment experience higher retention rates when they are able to access therapy.
Keywords: addiction, geography, harm reduction, opioid agonist therapy, rurality
Opioid addiction is recognized as a critical health care issue that has increased in recent years due to the advent and subsequent abuse of slow release opioids such as oxycodone (Dhalla et al., 2009; Dhalla et al., 2011; Juurlink et al., 2013). Across the province of Ontario (Canada), opioid use and subsequent addiction is seen as a major health crisis (Gomes et al., 2011; Kiepek et al., 2012; Lynas, 2013a, 2013b). For example, Gomes et al. (2014) recently reported that approximately 12% of deaths in patients between the ages of 25 and 34 years occur due to opioid-related overdoes.
Despite the severity of opioid dependence in Ontario and a rapid expansion in access to treatment over the past 20 years, access to addiction therapy is not uniformly distributed across all regions of the province (Brands, 2000). Clinical practice guidelines state that methadone maintenance therapy (MMT) is the standard of care for treating patients with opioid dependence (Health Canada, 2002; Centre for Addiction and Mental Health, 2011). Methadone maintenance therapy is a substitution/maintenance treatment model whereby the patient receives methadone in a structured treatment environment to reduce or eliminate the uncontrolled use of illicit opioids (Connock et al., 2007). With substance use disorders as a primary driver of opiate-related overdoses, expanding access to addiction treatment services is recognized to be an important goal of treatment programming and policy throughout North America and Europe (Volkow et al., 2014).
In Ontario, patients receiving MMT will frequently commence treatment at a specialized addiction clinic where a nurse or pharmacist will observe medication intake on a daily basis during initial treatment, with the future possibility of treatment in a family physician's office or community pharmacy following stabilization (Health Canada, 2002; Bell et al., 2006). It is a noteworthy difference from the American mode such that, in Ontario, observed dosing can be administered at several types of approved locations including a family physician's office, addiction clinic, or local pharmacy. By contrast, the American model of directly observed therapy is considerably more restrictive only allowing methadone dosing to occur at regulated opioid treatment programs.
Best results for MMT, including reduced mortality rate and improved psychosocial function, are linked to continuous treatment, often over the course of several years or even decades, with gradual reduction in the level of observed medication (Health Canada, 2002; Peles et al., 2008; Bell et al., 2006; Nosyk et al., 2009, 2010, 2012; Degenhardt et al., 2011; Tetrault and Fiellin, 2012). Maintenance treatment is fundamentally different from weaning strategies because patients may remain on methadone or buprenorphine for extended periods (Peles et al., 2010). A key element of treatment is that patients receive frequent and detailed care by an addiction-trained physician including urine drug screening, counseling, and general medical care (Health Canada, 2002).
In northern regions of Ontario, patients are subject to several barriers in accessing care. For example, northern patients may have difficulty enrolling in treatment due to the well-documented lack of primary care physicians, and they may also have to travel longer distances to reach a nurse or pharmacist prepared to provide observed dosing (Aird and Kerr, 2007; Canadian Mental Health Association, 2009; Kiepek et al., 2012).
Currently, there is a gap in knowledge with respect to MMT retention and mortality rates for patients residing in differing geographies, especially where access to addiction services are markedly reduced. Here, we evaluate the relationship between location of residence and both treatment retention and mortality among first time MMT patients across Ontario, Canada.
METHODS
Cohort Definition
We conducted a retrospective cohort study of patients initiating MMT for the first time between January 1, 2003, and March 31, 2012, in the province of Ontario. First-time MMT therapy was defined as no previous history of methadone or buprenorphine use in the year before the first treatment episode. Although all patients started on methadone, we did include patients who transitioned to buprenorphine over the course of treatment. New starts on buprenorphine were excluded because of the small number of such treatment episodes within the time frame studied. All patients were at least 10 years or older (to exclude data entry errors for newborns; patients <18 years accounted for <1% of cohort) and were eligible for public drug coverage through the Ontario Drug Benefit (ODB) plan. Patients with less than 180 days of eligibility for public drug coverage before initiating MMT (as evidenced by no prescriptions for any drug in the 180 to 365 days before cohort entry) were excluded to avoid incomplete drug records. In Ontario, methadone used for addiction treatment is dispensed exclusively in liquid formulation (with very few exceptions). Therefore, patients prescribed methadone in a tablet formulation, with a medication possession ratio greater than 20% over a 1-year period, were excluded due to the likelihood that methadone was being administered for chronic pain management despite being coded for addiction therapy in the billing records. We also excluded patients with missing information regarding place of residence, age, or sex. All patients were followed from their date of MMT initiation to the date of treatment discontinuation (patient did not receive a prescribed dose of methadone or buprenorphine within 30 days of their last methadone or buprenorphine prescribed dose), death, 1-year follow-up, or end of the study period (March 31, 2013).
Data Sources
The ODB database was used to identify all patients initiating MMT and to determine their past medication use. The ODB database contains detailed records of all prescriptions dispensed to Ontario residents eligible for public drug coverage. In Ontario, residents are eligible for public drug coverage if they are aged 65 years or older, reside in a long-term care facility, are disabled, are receiving social benefits for income support, or have high prescription drug costs relative to their net household income. Emergency department visits were identified using the Canadian Institute for Health Information National Ambulatory Care Reporting System, and hospital admissions were identified using the Canadian Institute for Health Information Discharge Abstract Database. All diagnosis information from physician visits was determined using billing data from the Ontario Health Insurance Plan database (Ontario Health Insurance Plan covers physician services for all permanent residents of Ontario). We obtained patient location of residence and demographic information from the Ontario Registered Persons Database, which contains a unique entry for each resident who has ever received insured health services. Patient information was linked anonymously across databases using encrypted 10-digit health card numbers. The linking protocol has been described extensively elsewhere (Levy et al., 2003; Hall et al., 2006), and it is used routinely for health system research in Ontario (Mamdani et al., 2003; Juurlink, 2009; Juurlink et al., 2009).
Geographic Definitions
We used each patient's postal code to determine their location of residence at the outset of MMT. Provincially defined health regions (Local Health Integration Networks) were used to stratify patient location of residence into northern and southern regions. Local Health Integration Networks are regional health authorities who govern the administration of health service funding across defined geographic areas of Ontario. We distinguished rural from urban locations using the Rurality Index of Ontario (RIO) (Aird and Kerr, 2007). The RIO metric is influenced by 3 weighted components—population density, travel time to nearest advanced referral center, and travel time to basic referral center. A region with a RIO of 40 or more was defined as rural on the basis of scoring system defined by the Ontario Medical Association (Kralj, 2009). All patients were stratified into 1 of the following 4 geographic regions: Southern Urban, Southern Rural, Northern Urban, or Northern Rural.
Definition of Treatment Retention
All patients were followed for at least 1 year, to a maximum follow-up date of March 31, 2013. Continuous MMT was assessed on the basis of a prescription refill within 30 days of the previous prescription (ie, no period of 30 consecutive days without a prescribed dose). We defined a patient as having been retained in treatment if they completed at least 1 year of continuous and uninterrupted MMT.
Definition of Mortality
All patients were followed for 1 year after MMT initiation to determine the all-cause mortality rate in each geographic region.
Statistical Analysis
Descriptive statistics were summarized for baseline characteristics of patients, and standardized differences were used to compare characteristics between those residing in Southern Urban (locations to each of the other geographic regions). We chose the Southern Urban group as the reference group because it represents the majority of MMT delivered in the province of Ontario. Standardized differences less than 0.1 are generally not considered to be meaningful (Mamdani et al., 2005). For the primary analysis, we used logistic regression analysis to test the association between geographic location of residence and successful retention in MMT for at least 1 year, adjusting for patient covariates that were imbalanced between geographic regions. Covariates included age, sex, income quintile, Charlson score, prior prescription of benzodiazepine stimulant or antidepressant, the number of hospitalizations, the number of physician visits, the number of emergency department visits, and the number of prescribed drugs. We used the Kaplan-Meier method to characterize the time to discontinuation across the 4 groups. For the secondary analysis, we used logistic regression analysis to test the association between geographic location of residence and all-cause mortality within 1 year of treatment initiation, adjusting for the patient covariates that were imbalanced between geographic regions.
Ethics Review
This study was approved by the Research Ethics Board of Sunnybrook Health Sciences Centre, Toronto, Ontario, and the Research Ethics Board of Laurentian University, Sudbury, Ontario.
RESULTS
Over the study period, we identified 17,211 publicly funded eligible patients who commenced MMT. Of these, 14,052 (81.7%) resided in a Southern Urban region, 1,011 (5.9%) in a Southern Rural region, 1,620 (9.4%) in a Northern Urban region, and 528 (3.1%) in a Northern Rural region of the province.
Characteristics of patients initiating MMT did not differ substantially by age or sex based on location of residence (Table 1). However, individuals initiating MMT in northern regions were more likely to have previously received prescriptions for benzodiazepines, stimulants, and antidepressants compared with those residing in Southern Urban regions. There were no significant differences between Southern Rural and Southern Urban patients with respect to these classes of prescriptions. Patients in northern regions also had more emergency department and hospital visits but had fewer physician visits overall. Patients residing in Northern Rural locations resided much farther from their addiction care provider (median distance = 127 km; interquartile range = 52–287 km) compared with patients residing in Southern Urban regions (median distance = 16 km, interquartile range = 4–52 km).
TABLE 1.
Characteristics of Geographic Patient Groups
| Variable | Southern Urban | Southern Rural | Northern Urban | Northern Rural |
| N = 14,052 | N = 1,011 | N = 1,620 | N = 528 | |
| Age, yr | ||||
| Median (IQR) | 39 (29–52) | 37 (28–52) | 35 (27–45)* | 36 (27–47)* |
| Sex | ||||
| Male | 7,063 (50.3%) | 498 (49.3%) | 720 (44.4%)* | 244 (46.2%) |
| Charlson score | ||||
| No hospitalizations | 8,529 (60.7%) | 581 (57.5%) | 854 (52.7%)* | 261 (49.4%)* |
| 0 | 3,714 (26.4%) | 288 (28.5%) | 560 (34.6%)* | 201 (38.1%)* |
| 1 | 836 (5.9%) | 60 (5.9%) | 96 (5.9%) | 25 (4.7%) |
| 2+ | 973 (6.9%) | 82 (8.1%) | 110 (6.8%) | 41 (7.8%) |
| Prior prescribed medications (180 days before cohort entry) | ||||
| Opioids | 7,923 (56.4%) | 580 (57.4%) | 884 (54.6%) | 305 (57.8%) |
| Benzodiazepines | 5,440 (38.7%) | 366 (36.2%) | 694 (42.8%) | 237 (44.9%)* |
| Stimulants | 394 (2.8%) | 27 (2.7%) | 88 (5.4%)* | 26 (4.9%)* |
| Cannabinoids | 225 (1.6%) | 16 (1.6%) | 9 (0.6%) | ≤5 |
| Barbiturates | 17 (0.1%) | ≤5 | ≤5 | ≤5 |
| Antidepressants | 5,953 (42.4%) | 463 (45.8%) | 724 (44.7%) | 256 (48.5%)* |
| Antipsychotics | 2,497 (17.8%) | 158 (15.6%) | 282 (17.4%) | 109 (20.6%) |
| Health system use (1 year before cohort entry) | ||||
| No hospitalizations (mean ± SD) | 0.33 ± 0.86 | 0.38 ± 1.01 | 0.43 ± 1.03* | 0.47 ± 1.01* |
| No physician visits | ||||
| Median (IQR) | 21 (11–37) | 21 (11–35) | 19 (10–33)* | 17 (10–29)* |
| No ED visits | ||||
| Median (IQR) | 1 (0–4) | 2 (0–5)* | 2 (0–4) | 4 (1–8)* |
| No drugs | ||||
| Median (IQR) | 10 (5–16) | 9 (5–15)* | 9 (4–15)* | 9 (5–14)* |
| Distance to care provider (km) | ||||
| Median (IQR) | 16 (4–52) | 91 (34–159)* | 9 (3–320)* | 127 (52–287)* |
*Indicates standardized difference >0.10 when performing pair-wise comparison with Southern Urban group.
ED, emergency department; IQR, interquartile range; SD, standard deviation.
Nearly half of patients initiating MMT in northern regions successfully completed 1 year of continuous treatment (48.9%; N = 258 and 47.0%; N = 761 in Northern Rural and Urban regions, respectively). In comparison, in Southern Rural and Urban regions, only 40.6% (N = 410) and 39.3% (N = 5,518) successfully completed 1 year of treatment. After multivariate adjustment, patients residing in Northern Rural regions were 31% more likely to successfully be retained in MMT for at least 1 year compared with those residing in Southern Urban regions (adjusted odds ratio [aOR] = 1.31; 95% confidence interval [CI], 1.09%–1.58%). Similarly, those residing in Northern Urban regions were 14% more likely to successfully be retained in treatment for at least 1 year (aOR = 1.14; 95% CI, 1.02%–1.27%) compared with those residing in Southern Urban regions. There was no statistically significant difference in the likelihood of successful retention in MMT between those initiating therapy in Southern Rural and Southern Urban locations (aOR = 1.06; 95% CI, 0.92%–1.22%). The time to discontinuation of MMT differed significantly by geographic region over follow-up (Fig. 1; P < 0.001). In particular, the median time to discontinuation was shortest in Southern Urban regions (188 days) and longest in Northern Rural regions (351 days).
FIGURE 1.
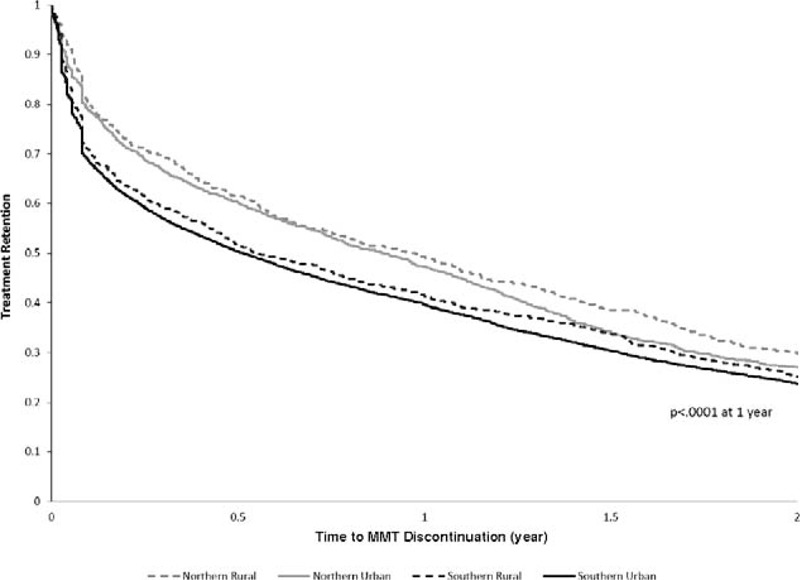
Time to discontinuation for patients from various geographic settings undergoing methadone maintenance therapy.
To identify if geographic status may also contribute to risk of mortality, we examined all-cause mortality rates within 1 year of a patient initiating MMT. Of the 17,211 patients initiating MMT, 585 deaths were observed within 1 year of date of initiation; of which, 140 deaths occurred while the patients were actively enrolled in treatment and 445 occurred in patients who had discontinued MMT (ie, >30 days following most recent methadone prescription). Methadone maintenance therapy patients in the Southern Rural region of the province demonstrated a mortality rate of 4.85% as compared to 3.38% for patients from the Southern Urban reference group. After adjusting for age, sex, income quintile, Charlson score, prior prescription of benzodiazepine, stimulant or antidepressant, the number of hospitalizations, the number of physician visits, the number of emergency department visits, and the number of prescribed drugs, patients in the Southern Rural region of the province had a 54% (aOR = 1.54; 95% CI, 1.09%–2.17%) increased likelihood of mortality within 1 year of initiating MMT as compared to the Southern Urban reference group. Comparatively, Northern Urban and Northern Rural patients were not as pronounced a difference as compared to the reference group (Table 2).
TABLE 2.
Treatment Retention at 1 Year and Mortality Rates During Course of First MMT Episode
| Region | No Patients, N | No Outcomes, N(%) | Unadjusted OR | Unadjusted 95% CI | Adjusted OR* | Adjusted 95% CI |
| Primary outcome: MMT retention at 1 y | ||||||
| Southern Urban (reference group) | 14,052 | 5,518 (39.3) | 1 | 1 | ||
| Southern Rural | 1,011 | 410 (40.6) | 1.06 | (0.93, 1.20) | 1.06 | (0.92, 1.22) |
| Northern Urban | 1,620 | 761 (47.0) | 1.37 | (1.24, 1.52) | 1.14 | (1.02, 1.27) |
| Northern Rural | 528 | 258 (48.9) | 1.48 | (1.24, 1.76) | 1.31 | (1.09, 1.58) |
| Secondary outcome: risk of death for all patients within 1 y of initiating MMT by geographic area | ||||||
| Southern Urban (reference group) | 14,052 | 475 (3.38) | 1 | 1 | ||
| Southern Rural | 1,011 | 49 (4.85) | 1.46 | (1.08, 1.97) | 1.54 | (1.09, 2.17) |
| Northern Urban | 1,620 | 45 (2.78) | 0.82 | (0.60, 1.11) | 1.16 | (0.82, 1.64) |
| Northern Rural | 528 | 16 (3.03) | 0.89 | (0.54, 1.48) | 1.03 | (0.59, 1.81) |
*Adjusted for age, sex, income quintile, Charlson score, prior prescription of benzodiazepine stimulant or antidepressant, the number of hospitalizations, the number of physician visits, the number of emergency department visits, and the number of prescribed drugs.
CI, confidence interval; MMT, methadone maintenance therapy; OR, odds ratio.
DISCUSSION
Our primary finding highlights that northern geographic status is associated with improved treatment retention in first-time MMT patients in the province of Ontario, Canada. Both rural and urban regions of Northern Ontario have well-documented geographic characteristics, which contribute to reduced access to care and limited health human resources (Aird and Kerr, 2007; Canadian Mental Health Association, 2009; Kiepek et al., 2012). Methadone maintenance therapy is a treatment strategy that centers initially on the observed dosing of methadone or buprenorphine under the medical supervision of an addiction specialist. In Ontario, there is a requirement for patients to present to an addiction treatment center or pharmacy for observed dosing during the initial period of therapy. In Northern Ontario, the need to travel can pose a barrier to accessing treatment, due to the considerable distance a patient may be required to travel to reach the site of observed dosing or the longer lead-time required to access care (Canadian Mental Health Association, 2009; Kiepek et al., 2012). We demonstrate that patients in Northern Urban and Rural regions of Ontario have a higher likelihood of successful treatment retention despite having to overcome barriers to care, including geography. Interpreted more generally, our data suggest that increased barriers to therapy may contribute to higher treatment retention for first-time MMT patients. It is very common for MMT patients to reinitiate treatment multiple times before they are stabilized (Nosyk et al., 2009). Thus, we suggest that our finding should be interpreted in the context of the relationship which exists between the patient and program accessibility, treatment retention, and treatment re-entry.
The primary finding was counter to our initial hypothesis. In the case of MMT, residence in Northern regions improved the likelihood of positive treatment retention for first-time MMT patients. This is somewhat surprising because our findings suggest that Northern Rural patients were required to travel much further to access therapy as compared to urban counterparts. It should be noted that patients in Ontario are able to receive daily supervised dosing at local pharmacies, and they are only required to see their prescribing physician 1 to 4 times per month. Thus, it is not uncommon for Northern patients to be physically removed from their physician by several hundred kilometers, but the patient would only be required to travel to the clinic for physician visits or urine testing once or twice per week while receiving observed daily doses at the pharmacy. Conversely, Southern Urban patients have considerably shorter distances to travel, and thus have a lower barrier to access care.
Considering the importance that a patient's self-motivation is recognized to play in addiction therapy (Li et al., 2008), our findings can be reconciled under the presumption that the effort required to access care by northern patients selects for patients who do access therapy having a higher motivation for treatment. This may account for the improved retention rates reported here. A supporting phenomenon was reported in a longitudinal study performed during the expansion of MMT in Australia by Bell et al. (2006). These authors followed MMT retention as addiction therapy programming was developed and expanded in the state of New South Wales from 1990 to 2005. Importantly, Bell et al. (2006) reported that as the access to the methadone program increased, treatment retention declined and patient cycling between therapy discontinuation and subsequent reinitiation became more frequent. Thus, it may follow that the greater ease of entry into addiction services in Southern regions of Ontario may contribute to lower retention rates observed for these patient groups. Interestingly, Strike et al. (2005) conducted a similar analysis of MMT treatment retention earlier in the expansion of MMT across the province of Ontario, although using a different data source. In a cohort of approximately 10,000 patients from 1996 to 2001, these authors reported a retention of approximately 50% after 760 days of treatment (Strike et al., 2005). Our data indicate that retention rates have fallen to approximately 25% at this time point in the following decade (2003–2012). This observed difference in treatment retention, following Ontario MMT program expansion in the 2000 s, further supports the finding that lower first-time retention rates can be rationalized as access to addiction therapy become more widely available and barriers to access treatment decrease.
With respect to the Southern group of patients, several factors have been reported which may help to improve patient retention in the Southern regions of the province. For example, higher methadone dose (Booth et al., 2004; D’Aunno et al., 2014), patient treatment satisfaction, access to stable housing, access to social programming, employment opportunities, and reduced access to nonprescribed (illicit) drugs all contribute to improved retention (Lundgren et al., 2007). Furthermore, patients in Northern and rural regions may also benefit from social constructs such as community support and increased access to affordable housing. Because of the nature of the data set utilized for this study, we are unable to specifically test the contributions of each of these factors, but it is important to recognize that there are many clinical, social, and systemic factors which influence the efficacy of MMT.
In addition to Bell et al. (2006), congruent findings of MMT retention rates have been reported in the Ukraine. Importantly, the Ukraine is a jurisdiction with relatively limited opioid agonist therapy programming. Bachireddy et al. (2014) report that in a study group of 296 patients who were HIV-positive and opioid dependent, the median treatment retention in opioid substitution therapy was 31 months. Although not directly comparable with our study, the authors also reported that patients enrolled in opioid agonist therapy also experienced improved health-related quality of life (Bachireddy et al., 2014). Findings demonstrating improved quality of care and health in areas where treatment options are limited underscore the importance of broadening access to opioid agonist therapy in jurisdictions that have limited treatment options such as Northern Ontario.
Secondary analysis of mortality for patients initiating MMT is an important metric in light of a recent study by Gomes et al. (2014), which demonstrated that in 2010, 12.1% of deaths in adults between the ages of 25 and 34 years can be attributed to an opioid-related overdose in the province of Ontario. We find that the number of deaths within 1 year for the patient population initiating MMT to be relatively low (3%) in the context of opioid-related deaths reported in the general population (Dhalla et al., 2009; Gomes et al., 2014). Moreover, it should be highlighted that the majority of deaths (76%) in the study group occurred in patients who were not retained in the first treatment episode. Increased mortality rate in the Southern Rural group indicates that contributing factors such as increased distance to tertiary care center could account for this increased probability of death.
Our study has many strengths and limitations that warrant discussion. Using a health systems data approach over a 10-year study period, we were able to use robust statistical methods to characterize the effect of geography on MMT treatment retention in a cohort of patients with opioid addiction. Our analysis strategy enabled us to evaluate a critical aspect of addiction care that cannot be easily addressed by studying localized rates in large urban center programs or in a homogeneous clinical setting. However, we were unable to assess other societal factors that may influence treatment retention, such as access to and use of illicit drugs, employment opportunities, the stability of housing, or familial and community support. Further limitations to the health systems data approach include the potential for patients to lose eligibility for public drug coverage over follow-up (eg, as a result of becoming employed). In such cases, patients could seem to have discontinued therapy when they had instead changed coverage from public to private health-insurer. However, we do not believe that such cases would have a substantial impact on the data because they are likely to be rare in the first year of treatment and are unlikely to differ significantly by geography in a way that favors Northern or rural areas. As patients with incomplete health system profiles were excluded from analysis, patients accessing services outside the provincial health care funding would have fallen outside the scope of analysis (eg, undocumented immigrants). Because of the nature of the data and the time frame studied, we were also unable to assess the impact of telehealth-delivered MMT, which is recognized to be a treatment modality that has become more commonplace in rural and remote regions of Ontario (unpublished observation).
Our findings suggest that patients initiating MMT in northern regions have a greater likelihood of a successful treatment outcome as compared to those in Southern regions of Ontario when enrolling in MMT for the first time. The specific differences in patient factors (eg, availability of heroin vs prescription opioids, frequency of other illicit drug use, mental health issues, homelessness, and familial and community support) and program factors (reliance on telehealth, prescribing practices, ease of accessibility, etc), which may explain this difference, and the underlying explanation for excess mortality in the Southern Rural group, require further study.
Ultimately, understanding the barriers and facilitators to successful MMT offers the potential for improved treatment systems in all locations. Finding the proper balance between the patient, program accessibility, and program retention should be considered by those responsible for delivering and evaluating addiction therapy.
Acknowledgment
We thank Brogan Inc, Ottawa, for use of their Drug Product and Therapeutic Class Database.
Footnotes
Supported by the Ontario Drug Policy Research Network, which is funded by grants from the Ontario Ministry of Health and Long-Term Care (MOHLTC) and the Northern Ontario Academic Medicine Association (NOAMA). It was also supported by the Institute for Clinical Evaluative Sciences (ICES), a nonprofit research institute sponsored by the Ontario MOHLTC. The design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation and review of the manuscript were conducted by the authors independently from the funding sources. No endorsement by ICES or the Ontario MOHLTC is intended or should be inferred. Dr Muhammad Mamdani has received honoraria from Boehringer Ingelheim, Pfizer, Bristol-Myers Squibb, and Bayer.
All other authors report no conflicts of interest.
REFERENCES
- Aird P, Kerr J. Factors affecting rural medicine: an improvement on the Rurality Index of Ontario. Can J Rural Med 2007; 12:245–246. [PubMed] [Google Scholar]
- Bachireddy C, Soule MC, Izenberg JM, et al. Integration of health services improves multiple healthcare outcomes among HIV-infected people who inject drugs in Ukraine. Drug Alcohol Depend 2014; 134:106–114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bell J, Burrell T, Indig D, et al. Cycling in and out of treatment; participation in methadone treatment in NSW, 1990–2002. Drug Alcohol Depend 2006; 81:55–61. [DOI] [PubMed] [Google Scholar]
- Booth RE, Corsi KF, Mikulich-Gilbertson SK. Factors associated with methadone maintenance treatment retention among street-recruited injection drug users. Drug Alcohol Depend 2004; 74:177–185. [DOI] [PubMed] [Google Scholar]
- Brands J, Brands B, Marsh DCT The expansion of methadone prescribing in Ontario, 1996–1998. Addict Res 2000; 8:485–496. [Google Scholar]
- Canadian Mental Health Association. BACKGROUNDER: Rural and Northern Community Issues. Ontario, Canada: Canadian Mental Health Association, 2009; 11. [Google Scholar]
- Centre for Addiction and Mental Health. Do You Know…Methadone. Toronto, Canada: Centre for Addiction and Mental Health; 2011. [Google Scholar]
- Connock M, Juarez-Garcia A, Jowett S, et al. Methadone and buprenorphine for the management of opioid dependence: a systematic review and economic evaluation. Health Technol Assess 2007; 11:1–171.iii-iv. [DOI] [PubMed] [Google Scholar]
- D’Aunno T, Pollack HA, Frimpong JA, et al. Evidence-based treatment for opioid disorders: a 23-year national study of methadone dose levels. J Subst Abuse Treat 2014; 47:245–250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Degenhardt L, Bucello C, Mathers B, et al. Mortality among regular or dependent users of heroin and other opioids: a systematic review and meta-analysis of cohort studies. Addiction 2011; 106:32–51. [DOI] [PubMed] [Google Scholar]
- Dhalla IA, Mamdani MM, Sivilotti ML, et al. Prescribing of opioid analgesics and related mortality before and after the introduction of long-acting oxycodone. CMAJ 2009; 181:891–896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dhalla IA, Persaud N, Juurlink DN. Facing up to the prescription opioid crisis. BMJ 2011; 343:d5142. [DOI] [PubMed] [Google Scholar]
- Gomes T, Juurlink D, Moineddin R, et al. Geographical variation in opioid prescribing and opioid-related mortality in Ontario. Healthc Q 2011; 14:22–24. [DOI] [PubMed] [Google Scholar]
- Gomes T, Mamdani MM, Dhalla IA, et al. The burden of premature opioid-related mortality. Addiction 2014; 109:1482–1488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall S, Schulze K, Groome P, et al. Using cancer registry data for survival studies: the example of the Ontario Cancer Registry. J Clin Epidemiol 2006; 59:67–76. [DOI] [PubMed] [Google Scholar]
- Health Canada. Best Practices: Methadone Maintenance Treatment. Publications, ed. Ottawa, Ontario, Canada: Health Canada, 2002. [Google Scholar]
- Juurlink DN. Proton pump inhibitors and clopidogrel: putting the interaction in perspective. Circulation 2009; 120:2310–2312. [DOI] [PubMed] [Google Scholar]
- Juurlink DN, Dhalla IA, Nelson LS. Improving opioid prescribing: the New York City recommendations. JAMA 2013; 309:879–880. [DOI] [PubMed] [Google Scholar]
- Juurlink DN, Gomes T, Lipscombe LL, et al. Adverse cardiovascular events during treatment with pioglitazone and rosiglitazone: population based cohort study. BMJ 2009; 339:b2942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiepek N, Hancock L, Toppozini D, et al. Facilitating medical withdrawal from opiates in rural Ontario. Rural Remote Health 2012; 12:2193. [PubMed] [Google Scholar]
- Kralj B, et al. Measuring Rurality—RIO2008_BASIC: Methodology and Results E. Department, ed. Ontario, Canada: Ontario Medical Association, 2009. [Google Scholar]
- Levy AR, O’Brien BJ, Sellors C, et al. Coding accuracy of administrative drug claims in the Ontario Drug Benefit database. Can J Clin Pharmacol 2003; 10:67–71. [PubMed] [Google Scholar]
- Li X, Sun H, Marsh DC, et al. Factors associated with seeking readmission among clients admitted to medical withdrawal management. Subst Abus 2008; 29:65–72. [DOI] [PubMed] [Google Scholar]
- Lundgren LM, Sullivan LM, Maina AW, et al. Client factors associated with length of stay in methadone treatment among heroin users who inject drugs: quantitative analysis of state-level substance abuse treatment utilization data. J Addict Med 2007; 1:26–32. [DOI] [PubMed] [Google Scholar]
- Lynas K. Ontario pharmacists concerned about the risks arising from approval of generic OxyContin. Can Pharm J (Ott) 2013; 146:12–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lynas K. Ontario police chiefs call on the federal government to keep generic OxyContin out of Canada. Can Pharm J (Ott) 2013; 145:204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mamdani M, Rochon P, Juurlink DN, et al. Effect of selective cyclooxygenase 2 inhibitors and naproxen on short-term risk of acute myocardial infarction in the elderly. Arch Intern Med 2003; 163:481–486. [DOI] [PubMed] [Google Scholar]
- Mamdani M, Sykora K, Li P, et al. Reader's guide to critical appraisal of cohort studies: 2. Assessing potential for confounding. BMJ 2005; 330:960–962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nosyk B, MacNab YC, Sun H, et al. Proportional hazards frailty models for recurrent methadone maintenance treatment. Am J Epidemiol 2009; 170:783–792. [DOI] [PubMed] [Google Scholar]
- Nosyk B, Marsh DC, Sun H, et al. Trends in methadone maintenance treatment participation, retention, and compliance to dosing guidelines in British Columbia, Canada: 1996–2006. J Subst Abuse Treat 2010; 39:22–31. [DOI] [PubMed] [Google Scholar]
- Nosyk B, Sun H, Evans E, et al. Defining dosing pattern characteristics of successful tapers following methadone maintenance treatment: results from a population-based retrospective cohort study. Addiction 2012; 107:1621–1629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peles E, Linzy S, Kreek M, et al. One-year and cumulative retention as predictors of success in methadone maintenance treatment: a comparison of two clinics in the United States and Israel. J Addict Dis 2008; 27:11–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peles E, Schreiber S, Adelson M. 15-Year survival and retention of patients in a general hospital-affiliated methadone maintenance treatment (MMT) center in Israel. Drug Alcohol Depend 2010; 107:141–148. [DOI] [PubMed] [Google Scholar]
- Strike CJ, Gnam W, Urbanoski K, et al. Factors predicting 2-year retention in methadone maintenance treatment for opioid dependence. Addict Behav 2005; 30:1025–1028. [DOI] [PubMed] [Google Scholar]
- Tetrault JM, Fiellin DA. Current and potential pharmacological treatment options for maintenance therapy in opioid-dependent individuals. Drugs 2012; 72:217–228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volkow ND, Frieden TR, Hyde PS, et al. Medication-assisted therapies—tackling the opioid-overdose epidemic. N Engl J Med 2014; 370:2063–2066. [DOI] [PubMed] [Google Scholar]


