Abstract
BACKGROUND
Hepatitis C virus (HCV) is a major cause of chronic liver disease and cancer. Vietnamese Americans are at high risk of HCV infection, with men having the highest US incidence of liver cancer. This study examines an intervention to improve HCV knowledge among Vietnamese Americans.
STUDY
Seven Vietnamese community-based organizations in Pennsylvania and New Jersey recruited a total of 306 Vietnamese participants from 2010 to 2011.
RESULTS
Average knowledge scores for pretest and posttest were 3.32 and 5.88, respectively (maximum 10). After adjusting for confounding variables, age and higher education were positively associated with higher pretest scores and having a physician who spoke English or Vietnamese was negatively associated with higher pretest scores. Additionally, after adjusting for confounding variables, household income, education, and having an HCV-infected family member significantly increased knowledge scores.
CONCLUSIONS
Promotion and development of HCV educational programs can increase HCV knowledge among race and ethnic groups, such as Vietnamese Americans. Giving timely information to at-risk groups provides the opportunity to correct misconceptions, decrease HCV risk behaviors, and encourage testing that might improve timely HCV diagnosis and treatment.
Keywords: hepatitis C, liver cancer, Vietnamese
Introduction
Over 1.5 million Vietnamese Americans reside in the US, of whom 67.8% are foreign born.1 The Vietnamese American population has been growing rapidly with a 37.9% increase since 2000.1 In Vietnam, the prevalence of chronic hepatitis C virus (HCV) infection in the general population ranges from 1% to 9% (rural and urban) compared to the overall US HCV prevalence of 1.8%.2,3 Among high-risk groups in Vietnam, the prevalence of chronic HCV is 19.2–87% for intravenous drug users, 54% for hemodialysis patients, and 29% for hemophiliacs.2 The particularly high HCV prevalence among these groups is attributable to HCV exposure through contaminated medical devices, such as needles or blood products.4,5 In developing countries, the transmission of HCV through hospital-acquired infections is high because of the frequent reuse of contaminated syringes and needles for medical and dental procedures.6,7 In a study of 837 northern Vietnam residents, hospital admission and having a tattoo were found to be independent risk factors for HCV infection.8
In addition, previous studies suggest that the lack of safe blood transfusions contributes to the high HCV infection prevalence in Vietnam.9,10 Unlike in the US where HCV was eliminated from the blood supply in 1992, providing safe blood transfusions has been difficult in Vietnam, given the lack of government resources to ensure the safety of donated blood from blood banks.3,10–12 However, through funding from the International Development Association and efforts taken by the World Bank’s Regional Blood Transfusion Centers Project, 93% of Vietnam’s blood supply now comes from safe donation centers.13
HCV is a major cause of chronic liver disease, including cirrhosis and liver cancer.14–17 Asian patients with chronic HCV and cirrhosis have a fourfold increased risk of developing liver cancer compared to White patients with the same conditions.18,19 In the US, liver cancer incidence among Vietnamese ranks third highest for men and fifth highest for women.20 Compared to other racial and Asian–American ethnic groups, Vietnamese men have the highest incidence rate of 41.8/100,000 for liver cancer compared to only 3.8/100,000 for White men.21 Vietnamese Americans have higher incidence and mortality rates for liver cancer compared to most Asian ethnic groups and non-Hispanic Whites.22 Patients with chronic HCV typically do not show symptoms until the late disease stage, when they show signs of cirrhosis or liver cancer. Because they may be unaware of their HCV infection, they do not seek treatment that would reduce morbidity and mortality and may continue to spread the virus to others.2,15,23 Thus, screening individuals with antibody tests and HCV core antigen tests is essential for early and accurate diagnosis.2,24 When an individual is infected with HCV, antiviral therapy can delay the progression to cirrhosis and liver cancer, perhaps by as much as 48%.25,26 The Centers for Disease Control and Prevention recommend HCV screening for those who are at high risk, including those who have used intravenous drugs, been on chronic hemodialysis, received blood transfusions or organ transplants before July 1992, received clotting factor products before 1987, have had occupational exposure to HCV-positive blood, or were born to HCV-positive mothers, and adults born between 1945 and 1965.27–29 Adults born within these years are significantly more likely to be infected with HCV potentially because of experimentation with intravenous drug use, common in the 1960s and 1970s.30,31 Vietnam War veterans are also considered to be a high-risk group for HCV, with high HCV prevalence ranging from 10% to 20%.32 Drug use, combat exposure (eg, blood contact during fighting), having had surgery or a blood transfusion, and having engaged in sexual encounters with a prostitute are factors that are believed to contribute to their high prevalence within this group.33
Effects of HCV interventions on increases in HCV knowledge
Few intervention studies have focused on changes in HCV knowledge in the general population. Most of the existing studies target high-risk groups, such as intravenous drug users or blood transfusion recipients, and often were not conducted in the US.34,35 Two studies conducted in the Alpes-Maritimes area of France examined HCV awareness among adolescents.34 In the first study, a 30-minute slide-show about HCV transmission, followed by a question and answer session, increased overall HCV knowledge from 21% to 95% (P < 0.001). Having a good overall knowledge of HCV infection at baseline was linked to being female, being in high school (versus middle school), having one or two employed parents, and having an intention to have a piercing or tattoo. Improved knowledge was associated with having one or two employed parents and being in high school (versus middle school). Another randomized control study in California and Virginia evaluated a six-week HCV self-management workshop.35 Compared to those in the control group, participants attending the self-management workshop improved more on HCV knowledge, HCV self-efficacy, and health-related quality of life (specifically, SF-36 energy/vitality). Together, these two studies suggest that increasing knowledge among those at risk for HCV or who have HCV is feasible, yet linking the knowledge gains with preventive or treatment behaviors is crucial to the study.
Research on HCV behaviors among Vietnamese Americans is scarce and even scarcer is that on their HCV knowledge. Given the increased risk of liver cancer once infected with HCV and high incidence rates of liver cancer among Vietnamese Americans, a great need exists to assess the factors associated with HCV knowledge. The goal of this study is to use multivariate-adjusted models to examine the change in knowledge because of an HCV intervention looking for associations between demographics, HCV history, acculturation, and healthcare variables. The results of this study can be used to further develop culturally and linguistically appropriate interventions for increasing HCV knowledge. Assisting Vietnamese Americans become more cognizant of HCV risk factors and transmission helps to avoid infections and results in a better informed patient, monitoring his or her health and protecting others.
Materials and Methods
Study population
This study was reviewed and approved by Temple University Institutional Review Board (protocol number PT 11187). Participants were recruited from seven Vietnamese community-based organizations (CBOs) located in Pennsylvania and New Jersey from 2010 to 2011. These seven Vietnamese CBOs are members of Asian Community Health Coalition and partners of Center for Asian Health (CAH), Temple University. A total of 321 Vietnamese American participants were recruited. They attended the education program and completed pre- and postquestionnaires that contained items on demographics, acculturation, HCV history, awareness, and knowledge. Data from participants who did not answer the knowledge questions in the pre- or posttest were excluded from the final analysis, resulting in a total sample of 306 participants. This study involved research on humans, and complied with the principles of the Declaration of Helsinki. Subjects gave their written, informed consent to participate in the research.
HCV community intervention
The 2–2.5-hour intervention was delivered to Vietnamese by CAH-trained, bilingual community health educators. The intervention included lecture using PowerPoint® and discussion using visual aids and handouts and covered the following topics: (1) what is hepatitis C and HCV in Asian Americans, (2) what happens after exposure to HCV and HCV symptoms, (3) HCV transmission routes, (4) community misconceptions about HCV transmission of how it is both spread and not spread, and (5) how to find out if you have HCV and how to avoid getting HCV.
Outcome variable
The outcome variable was knowledge of HCV, measured before and after HCV education, using a 10-item questionnaire. Each knowledge question was assigned equal weight, which resulted in a score that ranged from 0 to 10 for pre- and posttests. To examine the change in knowledge score after the education program, a change-in-score variable was created based on the difference between knowledge pre- and post-HCV education scores.
Independent variables
Detailed sociodemographic information was self-reported in the baseline survey. Sociodemographic characteristics included age, gender, education, household income, language that the physician usually spoke with the participant, and acculturation. Age was a continuous variable, and gender was grouped as male (reference) and female. Education comprised four categories: university or above, high school graduate, less than high school (reference), and missing. Household income comprised five categories: <$10,000 (reference), between $10,000 and $19,999, between $20,000 and $29,999, >$30,000, and missing. Family history of HCV was determined by asking whether a family member had ever had liver disease or whether anyone in the family had been infected with HCV.
Language that the physician usually spoke with the participant was categorized as follows: Vietnamese (reference), English or both English and Vietnamese, and missing. Acculturation-related variables included years lived in Vietnam, participation in social–cultural gatherings, and language spoken at home. Using the information gathered from the open-ended question “How many years did you live in Vietnam?” we categorized the length of stay in Vietnam as 0–20 years (reference), 21–30 years, 31–40 years, or over 40 years. Participation in social–cultural gatherings was grouped into two categories: yes and no, not at all. Language spoken at home was categorized as Vietnamese, English or both English and Vietnamese, and missing.
Data analysis
Descriptive statistics were generated for all the variables in the dataset. A t-test was used to determine whether there was a significant difference between the pre- and posttest knowledge scores. The nature of associations between knowledge scores and the independent variables was analyzed using simple linear regression. To study the adjusted associations between risk factors and knowledge scores, we developed multivariate-adjusted linear regression models. To check the normality of outcomes used in multiple regression analysis, residuals were generated using Q–Q plot. All the residuals for the pretest and posttest scores and change in scores were distributed normally, and so no data transformations were performed (see Figs. 1–3). All the variables that were significantly associated with the outcome variables in the bivariate analysis were entered into the multivariate linear regression models. Variation inflation factor (VIF) values were used to assess multicollinearity. All the variables had VIF values that were in an acceptable range (1.13–3.47). Possible interaction effects were tested for various combinations of gender, income, education, age, years lived in Vietnam, and family history of HCV. Because no interaction terms were significant, they were not included in further analyses, and the results are not presented. Analyses were conducted using Stata 11.
Figure 1.
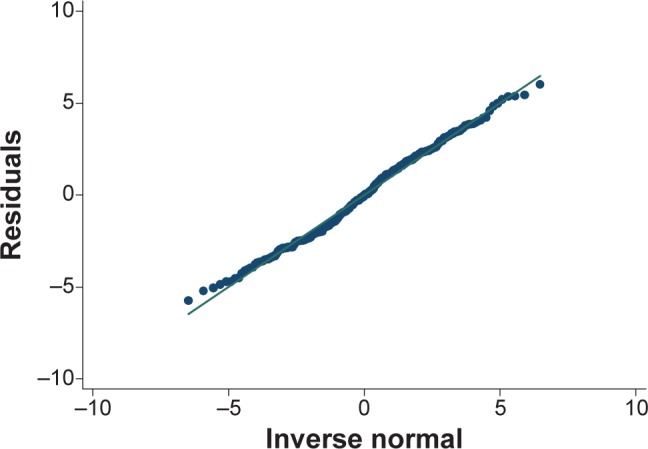
Residual plot of HCV pretest knowledge scores.
Figure 2.
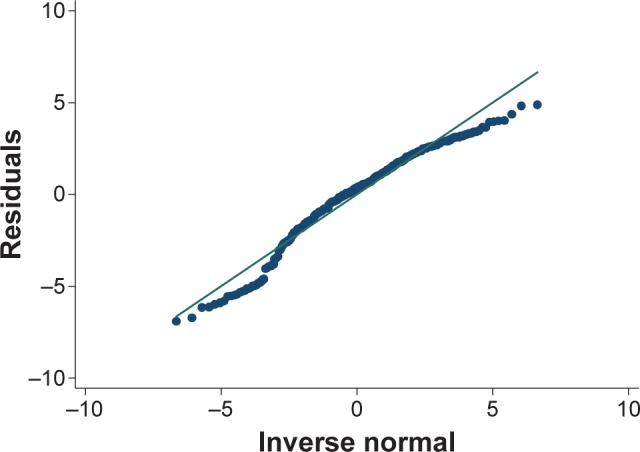
Residual plot of HCV posttest knowledge scores.
Figure 3.
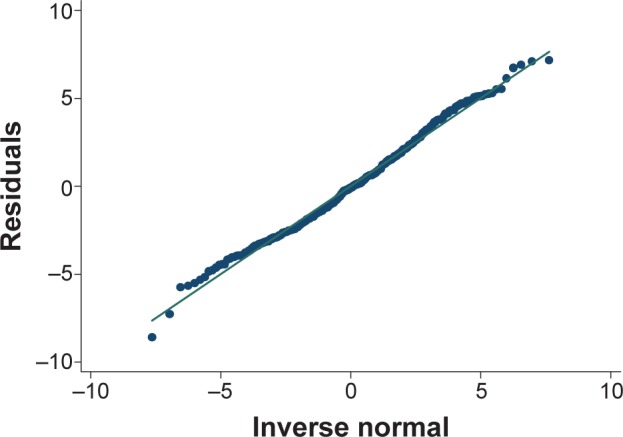
Residual plot of HCV knowledge about change in scores.
Results
Descriptive statistics
A total of 306 Vietnamese community members were chosen to participate in this study. The average knowledge scores for pretest and posttest were 3.32 and 5.88 (out of 10), respectively, and there was a significant difference between the scores before and after HCV education (t = −12.16, P < 0.001). The mean change in scores was 2.56. Table 1 presents the sociodemographic characteristics for the sample used to examine HCV knowledge. Overall, participants had a mean age of 50, more females (58.2%) participated, and approximately two-thirds were married (65.7%). The proportion of participants who lived in Vietnam for over 40 years was higher than that for the other categories (≤20 years, 21–30 years, 31–40 years, and missing). With regard to education, 25.5% of participants had a university or above education, 40.2% had a high school education, 20.9% had below a high school education, and 13.4% (n = 41) did not respond to this item. Additionally, 38.2% of participants reported that their annual household income was <$10,000, and 47.1% of participants had physicians who spoke Vietnamese and 37.2% had physicians who spoke English or both English and Vietnamese. Most participants (85.0%) spoke Vietnamese at home. Almost half (47.1%) reported that they participated in social–cultural gatherings. Among them, only 1.3% participated in English-speaking social–cultural gatherings more often, 72.6% participated in Vietnamese-speaking groups more often, 18.3% participated in both equally, and 7.8% did not provide an answer.
Table 1.
Characteristics of participants (n = 306).
| CHARACTERISTICS | N | % |
|---|---|---|
| Gender | ||
| Male | 128 | 41.8 |
| Female | 178 | 58.2 |
| Years lived in Vietnam | ||
| <=20 years | 55 | 18.0 |
| 21–30 years | 70 | 22.9 |
| 31–40 years | 39 | 12.7 |
| >40 years | 89 | 29.1 |
| Missing | 53 | 17.3 |
| Education grade | ||
| Less than high school | 78 | 25.5 |
| High school graduate | 123 | 40.2 |
| University or above | 64 | 20.9 |
| Missing | 41 | 13.4 |
| Household income | ||
| Less than $10,000 | 117 | 38.2 |
| $10,000–$20,000 | 44 | 14.4 |
| $20,000–$30,000 | 31 | 10.1 |
| Above $30,000 | 23 | 7.5 |
| Missing | 91 | 29.8 |
| Language spoken by physician | ||
| Vietnamese | 144 | 47.1 |
| English or both | 114 | 37.2 |
| Missing | 48 | 15.7 |
| Language spoken at home | ||
| Vietnamese | 260 | 85.0 |
| English or both | 46 | 15.0 |
| Social cultural gatherings | ||
| Yes | 231 | 75.5 |
| No, not at all | 75 | 24.5 |
| Family history of HCV | ||
| No | 39 | 12.7 |
| Yes | 151 | 49.4 |
| Don’t know | 116 | 37.9 |
| Age mean (SD) | 50 (14.6) | – |
| Knowledge pretest score mean (SD) | 3.3 (2.6) | – |
| Knowledge posttest score mean (SD) | 5.9 (2.6) | – |
| Change of knowledge score mean (SD) | 2.6 (3.0) | – |
The pretest knowledge mean scores were 3.3 at baseline and 5.9 at posttest, demonstrating a 2.6 change in the overall scores.
Knowledge pretest and posttest scores
Table 2 presents the pre- and post-HCV knowledge scores of demographic variables. Household income, language spoken by physician, social–cultural gatherings, family history of HCV, and age had significant differences in mean HCV knowledge scores at pretest. For posttest, only language spoken at home had significant mean score differences in HCV knowledge. Note that for every variable and category, there is an increase in knowledge scores between pre- and posttest.
Table 2.
Pre- and post-HCV knowledge scores of the demographic variables (n = 306).
| CHARACTERISTICS | PRE-TEST HCV KNOWLEDGE | T-TEST/F TEST STATISTICS | PRE-TEST HCV KNOWLEDGE | T-TEST/F TEST STATISTICS |
|---|---|---|---|---|
| Gender | −1.11 | −1.86 | ||
| Male | 3.13 (2.52) | 5.56 (2.58) | ||
| Female | 3.47 (2.74) | 6.11 (2.52) | ||
| Years lived in Vietnam | 2.11 | 1.13 | ||
| <=20 years | 2.87 (2.77) | 5.35 (3.10) | ||
| 21–30 years | 3.00 (2.40) | 5.89 (2.41) | ||
| 31–40 years | 3.51 (2.88) | 5.84 (2.36) | ||
| >40 years | 3.94 (2.60) | 6.27 (2.24) | ||
| Missing | 3.04 (2.62) | 5.81 (2.74) | ||
| Education grade | 0.56 | 2.00 | ||
| Less than high school | 3.11 (2.86) | 6.24 (2.47) | ||
| High school graduate | 3.44 (2.40) | 6.00 (2.45) | ||
| University or above | 3.55 (2.92) | 5.72 (2.86) | ||
| Missing | 3.02 (2.53) | 5.10 (2.45) | ||
| Household income | 3.31* | 0.26 | ||
| Less than $10,000 | 3.93 (2.73) | 5.81 (2.69) | ||
| $10,000–$20,000 | 3.48 (2.45) | 6.20 (2.24) | ||
| $20,000–$30,000 | 2.55 (2.55) | 5.68 (2.95) | ||
| Above $30,000 | 2.61 (2.39) | 5.78 (2.54) | ||
| Missing | 2.91 (2.58) | 5.91 (2.43) | ||
| Language spoken by physician | 8.96** | 2.21 | ||
| Vietnamese | 3.99 (2.61) | 6.19 (2.33) | ||
| English or both | 2.74 (2.60) | 5.52 (2.91) | ||
| Missing | 2.73 (2.44) | 5.83 (2.22) | ||
| Language spoken at home | 1.45 | 2.37* | ||
| Vietnamese | 3.42 (2.63) | 6.02 (2.46) | ||
| English or both | 2.80 (2.70) | 5.07 (2.96) | ||
| Social cultural gatherings | 1.98* | 1.52 | ||
| Yes | 3.49 (2.64) | 6.01 (2.49) | ||
| No, not at all | 2.80 (2.61) | 5.50 (2.74) | ||
| Family history of HCV | 10.82** | 2.63 | ||
| No | 3.26 (2.73) | 6.51 (1.77) | ||
| Yes | 3.97 (2.61) | 6.00 (2.45) | ||
| Don’t know | 2.50 (2.45) | 5.51 (2.86) | ||
| Age | −2.64* | −1.83 | ||
| Below 50 years old | 2.91 (2.56) | 5.61 (2.71) | ||
| 50 years old or above | 3.70 (2.68) | 6.14 (2.39) | ||
| Overall knowledge score | 3.23 (2.65) | – | 5.88 (2.56) | – |
| Overall change of knowledge score | 2.56 (3.01) | – | – |
Notes:
P < 0.05 and
P < 0.01.
Knowledge pretest, posttest, and change scores
Table 3 presents the results for the associations between the independent variables and pretest and posttest scores and change in scores. In the unadjusted model, pretest scores had significant associations with age, and some had categories of years lived in Vietnam, household income, language that the physician spoke, and social–cultural gatherings (data not shown). After adjusting for potential confounding variables in multivariate analyses, age was positively associated with pretest scores. As the age increased by 10 years, the pretest score increased by 0.04 (95% CI: 0.01, 0.06). Compared to participants who had less than a high school education, those with a high school education scored 0.81 points higher on the pretest (95% CI: 0.07, 1.55) and those with a university education or above scored 1.22 points higher (95% CI: 0.31, 2.12). Participants whose physicians spoke English or both English and Vietnamese scored 1 point less on the pretest (β = −1.00; 95% CI: −1.71, −0.28).
Table 3.
Adjusted multivariate linear regression between each predictors and knowledge score.
| VARIABLE | PRETEST SCORE | PRETEST SCORE | CHANGE OF SCORE | |||
|---|---|---|---|---|---|---|
| βa | 95% Clb | βa | 95% Clb | βa | 95% Clb | |
| Years lived in Vietnam | ||||||
| <=20 years | Reference | Reference | Reference | |||
| 21–30 years | −0.20 | (−1.14, 0.74) | −0.71 | (−0.71, 1.21) | 0.45 | (−0.65, 1.55) |
| 31–40 years | 0.15 | (−1.00, 1.30) | −0.86 | (−0.86, 1.50) | 0.17 | (−1.18, 1.52) |
| >40 years | −0.39 | (−1.50, 0.71) | −0.58 | (−0.58, 1.69) | 0.95 | (−0.35, 2.24) |
| Missing | −0.23 | (−1.29, 0.82) | −0.96 | (−0.96, 1.20) | 0.35 | (−0.89, 1.59) |
| Age | 0.04 | (0.01, 0.06)*** | 0.00 | (−0.02, 0.03) | −0.03 | (−0.06, −0.00) |
| Gender | ||||||
| Male | Reference | Reference | Reference | |||
| Female | 0.35 | (−0.23, 0.94) | 0.66 | (0.06, 1.27)** | 0.31 | (−0.39, 1.00) |
| Household income | ||||||
| Less than $10,000 | Reference | Reference | Reference | |||
| $10,000–$19,999 | −0.67 | (−1.54, 0.20) | 0.40 | (−0.50, 1.29) | 1.07 | (0.04, 2.09)** |
| $20,000–$29,999 | −1.00 | (−2.02, 0.03)* | 0.42 | (−0.63, 1.47) | 1.42 | (0.21, 2.62)** |
| Above $30,000 | −0.64 | (−1.85, 0.56) | 0.84 | (−0.39, 2.07) | 1.48 | (0.07, 2.89)** |
| Missing | −0.99 | (−1.70, 0.29)*** | 0.28 | (−0.45, 1.00) | 1.27 | (0.44, 2.10)*** |
| Education | ||||||
| Less than high school | Reference | Reference | Reference | |||
| High school graduate | 0.81 | (0.07, 1.55)** | −0.11 | (−0.88, 0.65) | −0.92 | (−1.80, −0.05)** |
| University or above | 1.22 | (0.31, 2.12)*** | −0.23 | (−1.16, 0.69) | −1.45 | (−2.51, −0.39)*** |
| Missing | 0.27 | (−0.71, 1.25) | −1.17 | (−2.17, −0.16)** | −1.44 | (−2.59, −0.28)** |
| Language spoken by physician | ||||||
| Vietnamese | Reference | Reference | Reference | |||
| English or both | −1.00 | (−1.71, −0.28)*** | −0.26 | (−0.99, −0.48) | 0.74 | (−0.10, 1.58)* |
| Missing | −0.66 | (−1.52, 0.21) | −0.30 | (−1.18, 0.59) | 0.36 | (−0.66, 1.37) |
| Language spoken at home | ||||||
| Vietnamese | Reference | Reference | Reference | |||
| English or both | 0.20 | (−0.71, 1.12) | −0.71 | (−1.64, 0.23) | −0.91 | (−1.98, 0.16)* |
| Family history of HCV | ||||||
| No | Reference | Reference | Reference | |||
| Yes | 0.68 | (−0.23, 1.59) | −0.72 | (−1.65, 1.59) | −1.40 | (−2.46, −0.33)** |
| Don’t know | −0.64 | (−1.57, 0.29) | −1.04 | (−1.57, 0.29)** | −0.40 | (−1.48, 0.69) |
Notes:
β-coefficient from linear regression.
95% confidence interval.
P ≤ 0.10,
P ≤ 0.05, and
P ≤ 0.01.
Table 3 also presents the posttest results. After adjusting for covariates, female participants scored 0.66 points higher than did male participants (β = 0.66; 95% CI: 0.06, 1.27). Participants who had missing values in education or did not know their family history of HCV were more likely to have a lower score in the posttest, after adjusting for other covariates (β = −1.17; 95% CI: −2.17, −0.16 and β = −1.04; 95% CI: −1.57, 0.29, respectively).
Household income, education, and family infected with HCV were significantly associated with a change in score, adjusting for covariates. Overall, all income groups had significant changes in their knowledge scores, but they varied by level. Compared to those with an annual household income of <$10,000, participants with income between $10,000 and $19,999 had a mean change score that was 1.07 point higher (β = 1.07; 95% CI: 0.04, 2.09). A similar trend was found in other income categories (β = 1.42; 95% CI: 0.21, 2.62 for $20,000–$29,999 and β = 1.48; 95% CI: 0.07, 2.89 for ≥$30,000). The mean posttest scores increased in all educational levels; only the degree of increase differed. Therefore, negative coefficients shown later in scores changed by the level of education are explained because compared to the reference group (less than high school education), the change in knowledge was less for those with more education. For example, although the less than high school category had the lowest pretest score, those in this category had the highest posttest score, observing the highest change in score. Therefore, when we compare the degree of change in this group, all higher levels of education experienced smaller increase in posttest, leading to smaller change in score and a negative coefficient in multiple regression. Specifically, compared to participants with less than a high school education, participants who had a high school education scored 0.92 points lower at posttest than at pretest, after adjusting for other covariates (high school: β = −0.92; 95% CI: −1.80, −0.05). Those in university or above education experienced even small degree of change in score between pretest and posttest (β = −1.45; 95% CI: −2.51, −0.39). Compared to those who had no family member infected with HCV, participants who had a family member infected with HCV had less change in score (β = −1.40; 95% CI: −2.46, −0.33), after adjusting for covariates.
Discussion
The current study found that age, some categories of years lived in Vietnam, household income, language that the physician spoke, and social–cultural gatherings were significantly associated with knowledge score at baseline. The results also indicated that HCV education substantially improved knowledge of HCV among Vietnamese Americans (change in score: 2.56 points out of 10; t = −12.16, P < 0.001). Those with higher education had high scores at pretest and even higher scores at posttest, although the increase in HCV knowledge was smaller than that in other educational groups. The main factor that was significantly associated this change was household income; participants with a higher income performed better at posttest.
Pretest (baseline) scores
Our findings highlight the low levels of baseline knowledge of HCV among Vietnamese Americans, which is consistent with previous studies among the Vietnamese in Sydney.36 The Australian study found that the mean score of HCV knowledge was 4.9 out of 10 (95% CI: 4.6, 5.3) among Vietnamese men compared with 7.6 (95% CI: 7.4, 7.8) among men across all racial groups, which indicates that Vietnamese men were significantly less likely to have HCV knowledge.37 Another large population-based study of sexual and related risk behaviors by telephone interview in Australia36 showed that men who spoke a language other than English had a significantly lower blood-borne virus knowledge score compared to men who spoke English. Findings from these studies suggest that targeted HCV awareness-raising programs are urgently needed for the Vietnamese community.
We found that, at baseline, participants with a higher level of education tend to have higher HCV knowledge compared to those with a lower level of education. This finding is consistent with previous research conducted on intravenous drug users in California. Patients with a high school or at least some college education were more likely to have HCV-related knowledge than those with less than a high school education (P = 0.031).38 Similarly, in an intervention study among vulnerable populations, the HCV baseline knowledge scores were significantly higher in individuals with a high school and above education (P = 0.0006). We also found that, among Vietnamese Americans, the baseline knowledge score was higher as age increased. This is consistent with one study that examined HCV awareness among adolescents in the Alpes-Maritimes area of France.34 The results indicated that older age was associated with better overall knowledge of HCV infection. However, these results stood in contrast to the results of a study conducted among HCV-infected patients in California, which found that older age was associated with lower baseline HCV knowledge scores.39
No previous work has specifically addressed the relationship between the language that one’s physician spoke and HCV knowledge. Our findings show that participants whose physicians spoke English or both English and Vietnamese had a lower baseline knowledge score compared to those whose physicians spoke Vietnamese. It is likely that, when the physician does not speak Vietnamese, limited English proficiency is a barrier to medical communication between the physician and the patient,40,41 and non-Vietnamese-speaking physicians may not be aware of the Vietnamese population being at high risk for HCV, as would Vietnamese-speaking physicians.
Change in scores
Consistent with other studies,34,35,39 HCV education significantly improved knowledge of HCV among Vietnamese Americans. This suggests that HCV education can play an important role in increasing knowledge related to HCV and ultimately reducing the HCV knowledge disparity in the Vietnamese American population. The gain in HCV knowledge after education was strongly associated with household income, an association that rarely has been examined in the literature. One study that examined HCV awareness among teenagers indicated that factors associated with improvement in overall knowledge included one employed parent (OR: 2.3, 95% CI: 1.4, 3.7) or two employed parents (OR: 3.6, 95% CI: 2.2, 5.9), compared to both parents being unemployed.35 This result may be similar to our finding that participants with a higher income had more improvement in HCV knowledge compared to those with a lower income. Those with higher education experienced lesser degree of increase in HCV knowledge at posttest. Because those with higher education had high scores at pretest, these participants had less room to improve their scores at posttest. Although HCV knowledge has improved, the scores showed lesser increase at posttest, hence resulting in the negative coefficients.
Limitations
There are several limitations associated with this study. First, we used a convenient sample drawn from seven Vietnamese communities in Pennsylvania and New Jersey, which limits the generalizability of our findings to other regions and populations. Second, family history was self-reported and may be prone to recall bias. Third, the study lacked an assessment of the long-term effect of the intervention, as the second questionnaire was completed immediately after the intervention.
In other studies, a local, primary preventive intervention improved the long-term knowledge, which suggests that the same effect could be true for our intervention.42,43 Because Vietnamese Americans are at great risk of HCV transmission, this study may have a large impact on their behaviors linked to increase in knowledge, which would be an important follow-up study. This study also has unique strengths that will contribute to the existing literature. First, few studies have examined the factors related to knowledge of HCV before and after an educational intervention. These findings allow us to tailor the intervention further to take into consideration information that may or may not be available from primary physicians. Participants from lower education groups who had low initial scores had the greatest increase in knowledge, which is an important program success. Second, to the best of our knowledge, this is one of the first studies that examined the factors that influence knowledge of HCV in the Vietnamese population in the United States.
Conclusion
Education plays an important role in the improvement of HCV knowledge among Vietnamese Americans. Considering that individuals of a younger age and a lower education level tend to have low baseline HCV knowledge, promoting effective HCV educational programs among this population is an important factor in reducing knowledge and health HCV disparities. The results also argue for the necessity of raising awareness of the importance of HCV screening and education among the Vietnamese population by physicians. Findings from this study indicate a strong need for education and training programs that are linguistically and culturally appropriate for the Vietnamese population. Further studies could be conducted to determine the feasibility of such interventions and to ascertain their long-term impact on both knowledge and behavior. In this day of abundant information about HCV, little of this is available to Vietnamese Americans. This intervention is vital for disseminating HCV health education in a timely manner to isolated race and ethnic enclaves in the US who are at high risk of HCV infection. Only with correct HCV knowledge, at-risk race and ethnic groups can protect themselves against infection. For those infected with HCV, HCV knowledge provides information necessary for timely testing and treatment to reduce mortality and morbidity.
Acknowledgments
The authors wish to thank Asian Community Health Coalition partners, volunteers, community coordinators of Vietnamese CBOs (Thoa Tran), and the research team of the CAH, Temple University, including Mei Zhao, who facilitated the completion of the study.
Footnotes
ACADEMIC EDITOR: Melpakkam Srinivas, Editor in Chief
PEER REVIEW: Two peer reviewers contributed to the peer review report. Reviewers’ reports totaled 673 words, excluding any confidential comments to the academic editor.
FUNDING: This research was supported by National Institutes of Health, U54 CA153513 Asian Community Cancer Health Disparities Center (PI: Dr. Grace Ma). The authors confirm that the funder had no influence over the study design, content of the article, or selection of this journal.
COMPETING INTERESTS: Authors disclose no potential conflicts of interest.
Paper subject to independent expert blind peer review. All editorial decisions madeby independent academic editor. Upon submission manuscript was subject to anti-plagiarism scanning. Prior to publication all authors have given signed confirmation of agreement to article publication and compliance with all applicable ethical and legal requirements, including the accuracy of author and contributor information, disclosure of competing interests and funding sources, compliance with ethical requirements relating to human and animal study participants, and compliance with any copyright requirements of third parties. This journal is a member of the Committee on Publication Ethics (COPE).
Author Contributions
Drafted the manuscript and conducted the data analysis: SL. Supervised data collection and project implement: YT. Project draft manuscript: XL. Manuscript draft and revision: XSM. Expanded and updated the literature review and conclusions, and edited other sections in response to reviewer comments: BS. Developed the project: GZ and SZ. Provided advice for study intervention message design and questionnaire development: PS. Developed the study protocol and oversaw the overall scientific integrity of the study, drafted and final edited the manuscript: GXM. All authors read and approved the final manuscript.
REFERENCES
- 1.U.S. Census Bureau . The Vietnamese Population in the United States: 2010. Atlanta, Georgia: 2011. Available at http://www.bpsos.org/mainsite/images/DelawareValley/community_profile/us.census.2010.the%20vietnamese%20population_july%202.2011.pdf. [Google Scholar]
- 2.Gish RG, Bui TD, Nguyen CT, et al. Liver disease in Vietnam: screening, surveillance, management and education: a 5-year plan and call to action. J Gastroenterol Hepatol. 2012;27(2):238–247. doi: 10.1111/j.1440-1746.2011.06974.x. [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization Hepatitis C: Global prevalence (update) Wkly Epidemiol Rec. 1999;74(49):425–427. [PubMed] [Google Scholar]
- 4.Nakata S, Song P, Duc DD, et al. Hepatitis C and B virus infections in populations at low or high risk in Ho Chi Minh and Hanoi, Vietnam. J Gastroenterol Hepatol. 1994;9(4):416–419. doi: 10.1111/j.1440-1746.1994.tb01265.x. [DOI] [PubMed] [Google Scholar]
- 5.Cheng JT, Hsien C, Josh Sun H-E, Tong MJ. The emerging importance of chronic hepatitis C infection in Asian Americans. Am J Gastroenterol. 2006;101(12):2737–2743. doi: 10.1111/j.1572-0241.2006.00831.x. [DOI] [PubMed] [Google Scholar]
- 6.Hutin YJ, Hauri AM, Armstrong GL. Use of injections in healthcare settings worldwide, 2000: literature review and regional estimates. BMJ. 2003;327(7423):1075. doi: 10.1136/bmj.327.7423.1075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Simonsen L, Kane A, Lloyd J, Zaffran M, Kane M. Unsafe injections in the developing world and transmission of bloodborne pathogens: a review. Bull World Health Organ. 1999;77(10):789–800. [PMC free article] [PubMed] [Google Scholar]
- 8.Nguyen VT, McLaws ML, Dore GJ. Prevalence and risk factors for hepatitis C infection in rural north Vietnam. Hepatol Int. 2007;1(3):387–393. doi: 10.1007/s12072-007-9008-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dunford L, Carr MJ, Dean J, et al. Hepatitis C virus in Vietnam: high prevalence of infection in dialysis and multi-transfused patients involving diverse and novel virus variants. PLoS One. 2012;7(8):e41266. doi: 10.1371/journal.pone.0041266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Viet L, Lan NTG, Ty PX, et al. Prevalence of hepatitis B & hepatitis C virus infections in potential blood donors in rural Vietnam. Indian J Med Res. 2012;136(1):74–81. [PMC free article] [PubMed] [Google Scholar]
- 11.Sievert W, Altraif I, Razavi HA, et al. A systematic review of hepatitis C virus epidemiology in Asia, Australia and Egypt. Liver Int. 2011;31:61–80. doi: 10.1111/j.1478-3231.2011.02540.x. [DOI] [PubMed] [Google Scholar]
- 12.Hepatitis C Support Project . HCV education & support: a brief history of hepatitis C. In: Franciscus A, editor. Hepatitis C Support Project FACT Sheet. 2010. [Google Scholar]
- 13.The World Bank. Vietnam: Regional Blood Transfusion Centers Project; 2011. [Google Scholar]
- 14.Chen SL, Morgan TR. The natural history of hepatitis C virus (HCV) infection. Int J Med Sci. 2006;3(2):47–52. doi: 10.7150/ijms.3.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Centers for Disease Control and Prevention Recommendations for prevention and control of hepatitis C virus (HCV) infection and HCV-related chronic disease. Centers for Disease Control and Prevention. MMWR Recomm Rep. 1998;47(RR-19):1–39. [PubMed] [Google Scholar]
- 16.Sharara AI. Chronic hepatitis C. South Med J. 1997;90(9):872. doi: 10.1097/00007611-199709000-00002. [DOI] [PubMed] [Google Scholar]
- 17.Hoofnagle JH. Hepatitis C: the clinical spectrum of disease. Hepatology. 1997;26(3 suppl 1):15S–20S. doi: 10.1002/hep.510260703. [DOI] [PubMed] [Google Scholar]
- 18.Nguyen MH, Whittemore AS, Garcia RT, et al. Role of ethnicity in risk for hepatocellular carcinoma in patients with chronic hepatitis C and cirrhosis. Clin Gastroenterol Hepatol. 2004;2(9):820–824. doi: 10.1016/s1542-3565(04)00353-2. [DOI] [PubMed] [Google Scholar]
- 19.Khan MH, Farrell GC, Byth K, et al. Which patients with hepatitis C develop liver complications? Hepatology. 2000;31(2):513–520. doi: 10.1002/hep.510310236. [DOI] [PubMed] [Google Scholar]
- 20.Miller BA, Chu KC, Hankey BF, Ries LA. Cancer incidence and mortality patterns among specific Asian and Pacific Islander populations in the U.S. Cancer Causes Control. 2008;19(3):227–256. doi: 10.1007/s10552-007-9088-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Miller BA, Kolonel LN, Bernstein L, et al. Racial/Ethnic Patterns of Cancer in the United States 1988–1992. Bethesda, MD: National Cancer Institute; 1996. [Google Scholar]
- 22.McCracken M, Olsen M, Chen MS, Jr, et al. Cancer incidence, mortality, and associated risk factors among Asian Americans of Chinese, Filipino, Vietnamese, Korean, and Japanese ethnicities. CA Cancer J Clin. 2007;57(4):190–205. doi: 10.3322/canjclin.57.4.190. [DOI] [PubMed] [Google Scholar]
- 23.Alter MJ, Kruszon-Moran D, Nainan OV, et al. The prevalence of hepatitis C virus infection in the United States, 1988 through 1994. N Engl J Med. 1999;341(8):556–562. doi: 10.1056/NEJM199908193410802. [DOI] [PubMed] [Google Scholar]
- 24.Seme K, Poljak M, Babic DZ, Mocilnik T, Vince A. The role of core antigen detection in management of hepatitis C: a critical review. J Clin Virol. 2005;32(2):92–101. doi: 10.1016/j.jcv.2004.10.005. [DOI] [PubMed] [Google Scholar]
- 25.Lin OS, Keeffe EB. Current treatment strategies for chronic hepatitis B and C. Annu Rev Med. 2001;52:29–49. doi: 10.1146/annurev.med.52.1.29. [DOI] [PubMed] [Google Scholar]
- 26.Yoshida H, Shiratori Y, Moriyama M, et al. Interferon therapy reduces the risk for hepatocellular carcinoma: national surveillance program of cirrhotic and non-cirrhotic patients with chronic hepatitis C in Japan. Ann Intern Med. 1999;131(3):174–181. doi: 10.7326/0003-4819-131-3-199908030-00003. [DOI] [PubMed] [Google Scholar]
- 27.Smith BD, Morgan RL, Beckett GA, Falck-Ytter Y, Holtzman D, Teo C, et al. Recommendations for the Identification of Chronic Hepatitis C Virus Infection Among Persons Born During 1945–1965. Morbidity and Mortality Weekly Report (MMWR) Atlanta, GA: Centers for Disease Control and Prevention; 2012. [Accessed September 25, 2012]. Available at: http://www.cdc.gov/mmwr/preview/mmwrhtml/rr6104a1.htm#Box. [PubMed] [Google Scholar]
- 28.Smith BD, Morgan RL, Beckett GA, Falck-Ytter Y, Holtzman D, Ward JW. Hepatitis C virus testing of persons born during 1945 to 1965: recommendations from the Centers for Disease Control and Prevention. Ann Intern Med. 2012;157(11):817–822. doi: 10.7326/0003-4819-157-9-201211060-00529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Harvard Medical School CDC urges universal hepatitis C screening for baby boomers. Harv Womens Health Watch. 2012;19(12):1–8. [PubMed] [Google Scholar]
- 30.Spradling PR, Rupp L, Moorman AC, et al. Hepatitis B and C virus infection among 1.2 million persons with access to care: factors associated with testing and infection prevalence. Clin Infect Dis. 2012;55(8):1047–1055. doi: 10.1093/cid/cis616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.McHutchison JG, Bacon BR. Chronic hepatitis C: an age wave of disease burden. Am J Manag Care. 2005;11(10 suppl):S286–S295. quiz S307-211. [PubMed] [Google Scholar]
- 32.Ma GX, Tan Y, Ma X, Toubbeh JI. A Feasibility Intervention Study to Increase Hepatitis C Virus (HCV) Screening among Vietnamese Americans. Washington, DC: American Public Health Association; 2012. [Google Scholar]
- 33.Waters B. Hepatitis C in Vietnam era veterans. In: Advocate H, editor. Medical Writer’s Circle: Hepatitis C Support Project. 2003. [Google Scholar]
- 34.Gardella F, Marine-Barjoan E, Truchi R, et al. Hepatitis C awareness among adolescents in the Alpes-Maritimes area of France. Gastroenterol Clin Biol. 2007;31(5):485–492. doi: 10.1016/s0399-8320(07)89416-4. [DOI] [PubMed] [Google Scholar]
- 35.Groessl EJ, Weingart KR, Stepnowsky CJ, Gifford AL, Asch SM, Ho SB. The hepatitis C self-management programme: a randomized controlled trial. J Viral Hepat. 2011;18(5):358–368. doi: 10.1111/j.1365-2893.2010.01328.x. [DOI] [PubMed] [Google Scholar]
- 36.Grulich AE, de Visser RO, Smith AM, Rissel CE, Richters J. Sex in Australia: knowledge about sexually transmissible infections and blood-borne viruses in a representative sample of adults. Aust N Z J Public Health. 2003;27(2):230–233. doi: 10.1111/j.1467-842x.2003.tb00813.x. [DOI] [PubMed] [Google Scholar]
- 37.O’Connor CC, Shaw M, Wen LM, Quine S. Low knowledge and high infection rates of hepatitis in Vietnamese men in Sydney. Sex Health. 2008;5(3):299–302. doi: 10.1071/sh07084. [DOI] [PubMed] [Google Scholar]
- 38.Walley AY, White MC, Kushel MB, Song YS, Tulsky JP. Knowledge of and interest in hepatitis C treatment at a methadone clinic. J Subst Abuse Treat. 2005;28(2):181–187. doi: 10.1016/j.jsat.2004.12.004. [DOI] [PubMed] [Google Scholar]
- 39.Surjadi M, Torruellas C, Ayala C, Yee HF, Jr, Khalili M. Formal patient education improves patient knowledge of hepatitis C in vulnerable populations. Dig Dis Sci. 2011;56(1):213–219. doi: 10.1007/s10620-010-1455-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wilson E, Chen AH, Grumbach K, Wang F, Fernandez A. Effects of limited English proficiency and physician language on health care comprehension. J Gen Intern Med. 2005;20(9):800–806. doi: 10.1111/j.1525-1497.2005.0174.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Fernandez A, Schillinger D, Grumbach K, et al. Physician language ability and cultural competence. An exploratory study of communication with Spanish-speaking patients. J Gen Intern Med. 2004;19(2):167–174. doi: 10.1111/j.1525-1497.2004.30266.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ingrand I, Verneau A, Silvain C, Beauchant M. Prevention of viral hepatitis C: assessment of a comic strip-based information campaign targeting adolescents. Eur J Public Health. 2004;14(2):147–150. doi: 10.1093/eurpub/14.2.147. [DOI] [PubMed] [Google Scholar]
- 43.Giles ML, Garland SM, Grover SR, Lewin SM, Hellard ME. Impact of an education campaign on management in pregnancy of women infected with a blood-borne virus. Med J Aust. 2006;184(8):389–392. doi: 10.5694/j.1326-5377.2006.tb00288.x. [DOI] [PubMed] [Google Scholar]
- 44.Barnett AG, van der Pols JC, Dobson AJ. Regression to the mean: what it is and how to deal with it. Intl J Epidemiol. 2005;34:215–220. doi: 10.1093/ije/dyh299. [DOI] [PubMed] [Google Scholar]


