Abstract
Global Health 2035, the report of The Lancet Commission on Investing in Health, laid out a bold, highly ambitious framework for making rapid progress in improving global public health outcomes. It showed that with the right health investments, the international community could achieve a "grand convergence" in global health—a reduction in avertable infectious, maternal, and child deaths down to universally low levels—within a generation. Rwanda’s success in rapidly reducing such deaths over the last 20 years shows that convergence is feasible. Binagwaho and Scott have argued that 5 lessons from this success are the importance of equity, quality health services, evidence-informed policy, intersectoral collaboration, and effective collaboration between countries and multilateral agencies. This article re-examines these lessons through the lens of the Global Health 2035 report to analyze how the experience in Rwanda might be generalized for other countries to making progress towards achieving a grand convergence.
Keywords: Grand Convergence, Equity, Pro-poor Universal Health Coverage, Domestic Financing of Health, Population, Policy, and Implementation Research, Intersectoral Collaboration, Global Health, Aid Effectiveness
In December 2013, the Lancet Commission on Investing in Health (CIH), an international collaboration of economists and health experts co-chaired by Lawrence Summers and Dean Jamison, published Global Health 2035: A World Converging within a Generation.1 The report laid out a bold, highly ambitious framework for making rapid progress in improving global public health outcomes.
Global Health 2035 showed that through a combination of increased domestic health investments by low-income countries (LICs) and lower-middle-income countries (LMICs), together with a realignment of donor priorities, the international health community could achieve a “grand convergence” in global health by 2035. Grand convergence, as defined by the CIH, refers to a reduction in avertable infectious, maternal, and child deaths down to universally low levels. In addition, the report showed that progressive public policies, such as taxing tobacco, sugar, and alcohol and redirecting fossil fuel subsidies towards the health sector, could sharply curb mortality and morbidity from noncommunicable diseases and injuries. And it made the case that the most efficient way for LICs and LMICs to reach universal health coverage (UHC)—a pathway that offers the most health and financial risk protection per dollar—is “progressive universalism,” defined by Gwatkin and Ergo2 as “a determination to include people who are poor from the beginning.”
How feasible are these goals? LICs and LMICs certainly face an array of economic, social, and political challenges in pushing health higher up their domestic agendas. But there are historical examples of countries that were able to overcome such obstacles to make extraordinary progress in health. Chile, Costa Rica, and Cuba make up a trio of countries that Abraham Horwitz, former Director of the Pan American Sanitary Bureau, called the “countries that cope.”3 In 1990, they were all classified as LICs or LMICs, and yet by 2011 they had dramatically reduced their child and maternal death rates despite facing “political vicissitudes, severe economic crisis, epidemic outbreaks, and other social banes.”3 And now, as described by Binagwaho and Scott in their perspective article,4 we can add Rwanda as a contemporary example of a “country that copes.”
Rwanda has achieved the fastest decline in child mortality in recorded history (Figure 1).5 If other LICs and LMICs could emulate this rate of mortality reduction, nearly all countries could reach grand convergence by 2035.6 At international meetings, however, it is all too common to hear health experts argue that the so-called Rwandan miracle is unique and impossible for other nations to replicate. They characterize Rwanda’s success as “a ‘black box’ case with few lessons for others.”5 Binagwaho and Scott4 have done a valuable service in shattering this argument. Rwanda “was considered by many to be a “lost cause” 20 years ago with its devastated economy and health system following the genocide,” they say. It was one of the poorest countries in the world, struggling with an enormous burden of uncontrolled infectious diseases, including HIV/AIDS, tuberculosis, and water-borne diseases.5 The nation’s turnaround from such devastation was the product of strong health leadership, a commitment to accountability and evidence-based practice, and highly focused attention on scaling up essential health tools and services.
Figure 1.
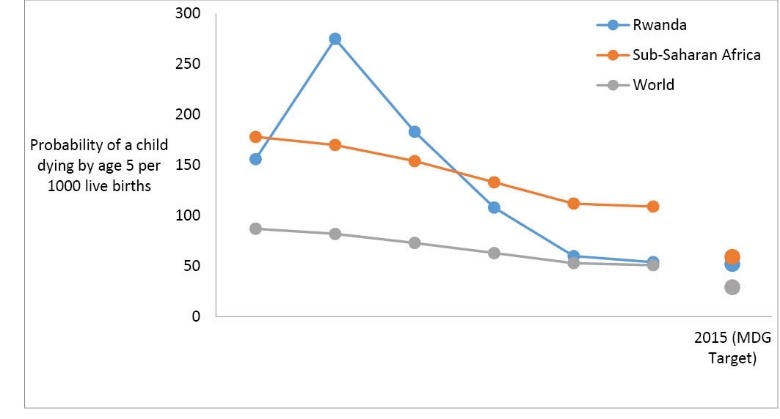
Decline in Child Mortality in Rwanda (Adapted from reference 5).
Far from being a “black box” case, Binagwaho and Scott4 believe that the 5 guiding principles that Rwanda adopted in reducing its premature mortality rates “may be useful for countries to consider as the world sets and moves forward with the post-2015 development agenda.” Below we respond to each of these principles through the lens of the Global Health 2035 report, and examine how they might be generalized for the global community to achieve a grand convergence in global health. We do so as 3 members of the CIH Secretariat, based in the Global Health Group at the University of California, San Francisco; one of us (GY) also led the writing of the Global Health 2035 report.
First, the authors argue that equity agendas should drive the post-2015 goals. Achieving global health equity by ending the massive disparities in deaths from infectious, maternal, and child conditions between rich and poor countries is at the heart of the grand convergence agenda. But achieving convergence is impossible unless we also pay attention to inequities within countries. Many middle-income countries, such as India and China, have large rural populations of people living in poverty who face a high burden of disease. As the CIH notes, achieving grand convergence will require focused attention not only on LICs but also on “lower income groups in rural subregions of middle-income countries.”1
Second, many countries have sought technical assistance from the World Health Organization (WHO) in working towards UHC,and Binagwaho and Scott remind these countries that as they increase service coverage, they must also pay attention to quality. Indeed, Kruk7 has argued that “improvements in quality must go hand in hand with the expansion of access and financial protection.” Global Health 2035 makes the case that as countries set out on a path to building these 3 pillars of UHC—quality, access, and financial risk protection—they should begin by first offering universal, publicly financed services for the conditions that disproportionately affect the poor. Experience has shown that services that are only for the poor tend to become poor quality, ghettoized services that have patchy and incomplete coverage and that fail to narrow the health equity gap between rich and poor.8 A preferred approach is for countries to achieve full population coverage with an initial high quality package of highly cost-effective interventions (the package would then become broader over time, as a country’s resources grow).9 Countries will clearly need to increase their domestic commitments to health spending, not just to achieve UHC but also to reach the other targets contained in the post-2015 sustainable development goals (SDGs).
Third, Binagwaho and Scott4 call for nations to build their own research capacity so that health policies can be informed by locally generated, locally relevant evidence. This is a very timely call, given that the SDGs will be impossible to achieve without scaled up national, regional, and international research. Global Health 2035 argued that research aimed at improving the delivery of interventions and at informing public health policies, which the report called “PPIR—population, policy, and implementation research,” has been sorely neglected.1 Building national capacity to conduct PPIR will require governments to foster an environment that supports research, dedicate financing to the enterprise, build research infrastructure, and provide training opportunities for junior researchers.10 The CIH called on the international community to support such national PPIR.
Fifth, Binagwaho and Scott highlight the importance of intersectoral collaboration, which was also emphasized by Global Health 2035. There is strong evidence that health improvements can be achieved through “joined up” investments in health, agriculture, education, water, sanitation, and poverty alleviation.1
The authors also argue that monitoring progress towards the post-2015 goals will require a new era of improved collaborations between multilateral agencies and “the countries that are working to achieve improvements in health within their nation and across the world.”4 They vividly describe the burdensome reporting requirements that development partners have imposed on Rwanda. The past 15 years have been characterized by an explosion in the number of new global health initiatives—such as Gavi, the Vaccine Alliance, the Global Fund, UNITAID, the US President’s Emergency Plan for AIDS Relief, and the US President’s Malaria Initiative. While these have clearly mobilized new financing, brought welcome innovation to the health aid enterprise, and made a measurable public health impact,1 the explosion has had unintended consequences. These consequences include lack of coordination between initiatives, as well as duplication and fragmentation of activities.11 There have been several efforts to redress these problems, such as the adoption by donors of the 2005 Paris Declaration on Aid Effectiveness, but these have had mixed results.11
One new initiative that could potentially improve streamlining is the Global Financing Facility for Every Woman, Every Child, a new partnership that “aligns and unites resources”12 from multiple sources (donors, LICs and LMICs, and the private sector) to accelerate progress towards convergence. And perhaps the adoption of the SDGs will usher in a new period of more streamlined and effective collaboration, though the vast number of goals and targets leave us pessimistic.
In other ways, however, we are very optimistic. We are at a unique moment in history, in which, for the first time, we have the financial and ever improving scientific capacity to bring about radical, dramatic transformations in global health. Rwanda has shown the way, and other countries could follow suit.
Ethical issues
Not applicable.
Competing interests
GY led the writing of Global Health 2035, which is discussed in this commentary. GY, SF, and NB are in the CIH Secretariat.
Authors’ contributions
All 3 authors developed this commentary. GY wrote the first draft, and SF and NB contributed to subsequent drafts.
Citation: Yamey G, Fewer S, Beyeler N. Achieving a "grand convergence" in global health by 2035: Rwanda shows the way: Comment on "Improving the world’s health through the post-2015 development agenda: perspectives from Rwanda." Int J Health Policy Manag. 2015;4(11):789–791. doi:10.15171/ijhpm.2015.143
References
- 1.Jamison DT, Summers LH, Alleyne G. et al. Global health 2035: a world converging within a generation. Lancet. 2013;382:1898–1955. doi: 10.1016/S0140-6736(13)62105-4. [DOI] [PubMed] [Google Scholar]
- 2.Gwatkin DR, Ergo A. Universal health coverage: friend or foe of equity? Lancet. 2011;377(9784):2160–2161. doi: 10.1016/S0140-6736(10)62058-2. [DOI] [PubMed] [Google Scholar]
- 3. Horwitz A. Comparative public health: Costa Rica, Cuba, and Chile. http://archive.unu.edu/unupress/food/8F093e/8F093E04.htm. Accessed May 10, 2015. Published September 1987.
- 4.Binagwaho A, Scott KW. Improving the world’s health through the post-2015 development agenda: Perspectives from Rwanda. Int J Health Policy Manag. 2015;4(4):203–205. doi: 10.15171/ijhpm.2015.46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Farmer PE, Nutt CT, Wagner CM. et al. Reduced premature mortality in Rwanda: lessons from success. BMJ. 2013;346:f65. doi: 10.1136/bmj.f65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Verguet S, Norheim OF, Olson ZD, Yamey G, Jamison DT. Annual rates of decline in child, maternal, HIV, and tuberculosis mortality across 109 countries of low and middle income from 1990 to 2013: an assessment of the feasibility of post-2015 goals. Lancet Glob Health. 2014;2(12):e698–e709. doi: 10.1016/S2214-109X(14)70316-X. [DOI] [PubMed] [Google Scholar]
- 7.Kruk ME. Universal health coverage—a policy whose time has come. BMJ. 2013;347:f6360. doi: 10.1136/bmj.f6360. [DOI] [PubMed] [Google Scholar]
- 8. Reddy KS. Building a better India: health beyond healthcare. Hindustan Times. November 28, 2013. http://www.hindustantimes.com/hindustantimesleadershipsummit2013/building-a-better-india-health-beyond-healthcare/article1-1156866.aspx.
- 9. Nicholson D, Yates R, Warburton W, Fontana G. Delivering universal health coverage: A guide for policymakers. Report of the WISH Universal Health Coverage Forum 2015. http://wish-qatar.org/summit/2015-summit/forumsandpanels/universal-healthcare-coverage/universal-healthcare-coverage. Published 2015.
- 10.Whitworth J, Sewankambo NS, Snewin VA. Improving implementation: building research capacity in maternal, neonatal, and child health in Africa. PLoS Med. 2010;7(7):e1000299. doi: 10.1371/journal.pmed.1000299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Organisation for Economic Co-operation and Development (OECD). Better Aid. Aid Effectiveness 2011. Progress in Implementing the Paris Declaration. http://www.oecd.org/dac/effectiveness/2011surveyonmonitoringtheparisdeclaration.htm.
- 12.Desalegn H, Solberg E, Kim JY. The Global Financing Facility: country investments for every woman, adolescent, and child. Lancet. 2015;386:105–106. doi: 10.1016/S0140-6736(15)61224-7. [DOI] [PubMed] [Google Scholar]


