Abstract
Background
Nonadherence to medications among Kuwaitis with type 2 diabetes mellitus (T2DM) is believed to be a major barrier to appropriate management of the disease. Published studies of barriers to medication adherence in T2DM suggest a Western bias, which may not adequately describe the Kuwaiti experience.
Aim
The purpose of this study was to explore barriers to medication adherence among Kuwaiti adults with T2DM.
Methods
Semi-structured interviews were conducted with 20 Kuwaiti patients with type 2 diabetes. The interviews were digitally recorded, transcribed, and analyzed using thematic analysis.
Results
Barriers to medication adherence were identified. Emerging themes were: 1) lack of education/awareness about diabetes/medications, 2) beliefs about medicines/diabetes, 3) spirituality and God-centered locus of control, 4) attitudes toward diabetes 5) perceptions of self-expertise with the disease and body awareness, 6) social stigma, 7) perceptions of social support, 8) impact of illness on patient’s life, 9) perceptions of health care providers’ attitudes toward patients, and 10) health system-related factors, such as access difficulties and inequalities of medication supply and services.
Conclusion
Personal, sociocultural, religious, health care provider, and health care system-related factors may impede medication adherence among Kuwaitis with type 2 diabetes. Interventions to improve care and therapeutic outcomes in this particular population must recognize and attempt to resolve these factors.
Keywords: medication adherence, type 2 diabetes mellitus, Kuwait, qualitative
Introduction
Diabetes is emerging as a major clinical and public health concern among the Kuwaiti population. The reported prevalence rate of known type 2 diabetes in 1990 was 7.6%, ranging from 5.6% to 10% in different governorates.1 In 1996, the overall prevalence rate of type 2 diabetes in Kuwaiti adults of age 20 years and over was as high as 14.8%.2 A remarkable increase in prevalence has been reported in more recent studies. In one study utilizing a cross-sectional household survey of 2,487 Kuwaiti nationals aged 50 years and over in 2005/2006 from two health governorates, the prevalence of physician-diagnosed diabetes was found to be 50.6%.3 Type 2 diabetes was detected even in adolescents, according to a population study of Kuwaiti school children,4 making the disease a public health problem. The burden of diabetes in Kuwait is high, and it has a serious impact on morbidity and mortality.2 Despite the availability and accessibility to evidence-based treatments for diabetes, patient outcomes are far from optimal, and the development of complications such as blindness, end-stage renal disease, stroke, coronary artery disease, and peripheral vascular disease continues to be a challenge in many patients.
There is evidence that patients’ adherence to medication in type 2 diabetes is suboptimal worldwide. Systematic reviews estimated that nonadherence to medications ranges from 7% to 64% for oral hypoglycemic medications, and 19%–46% for insulin only or insulin concomitant therapy.5,6
Many qualitative studies have been carried out to identify barriers to medication adherence, mostly in the Western world, particularly in USA, Canada, UK, Germany, Italy, France, Belgium, and Croatia. These studies have shown that many variables may play a role in causing patients’ nonadherence to medication, including poor knowledge about type 2 diabetes mellitus (T2DM),7–9 lack of diabetes education by health care providers,9,10 health care providers’ attitudes,7,9,11 patients’ beliefs about their illness or medicines,12 fear of medication adverse effects,13 use of alternative or herbal remedies,14 complexity of diabetic treatment,9,10 and lack of social support.7
Despite decades of research, nonadherence to medications remains an unresolved problem.15 It has been highlighted that one of the most striking reasons for the lack of progress is the absence of the patient’s perspective when designing interventions.16 Although there are some studies of the barriers and facilitators of medication adherence in type 2 diabetes in other parts of the world, there are no studies exploring these issues in Kuwaiti patients. In addition, traditional Western perspective models used to explain nonadherence to medications may not fully explain these behaviors in Kuwaiti patients. The lifestyle of Kuwaitis must be understood within a framework of Islamic religion, Arabic tradition, and other cultural customs that may influence adherence to medications among this population. Identifying barriers to medication adherence could aid the development of targeted interventions designed to improve medication adherence.
Aim
The aim of this study was to explore barriers to medication adherence among Kuwaiti patients with type 2 diabetes. Factors that may present barriers to medication adherence identified from the literature were explored to check their relevance to this particular population.
Study design and methods
Due to the exploratory nature of the research aim of this study, qualitative methods were chosen. With qualitative data, one can precisely explore which events lead to which consequences, and derive fruitful explanations. In addition, qualitative methods were more appropriate at this stage as findings of this exploratory study were meant to be incorporated into and inform the development of a quantitative survey, which would be used to test the relevance of these findings, and assess the prevalence of nonadherence to medications among a larger sample of Kuwaiti patients with T2DM. Qualitative in-depth face-to-face interviews were chosen as the method for data collection. This method allows respondents to freely express their individual opinions, and allows the researcher to have a better opportunity to deeply explore the processes and patterns that shape peoples’ behaviors and attitudes, clarify ambiguities, ask for more details, and check inconsistencies and misinterpretations.
Sampling and recruitment of subjects
A purposive maximum variation sampling technique was applied. This involves purposefully picking a wide range of variation on dimensions of interest. Although the sample obtained was not meant to be statistically representative of all Kuwaiti patients with T2DM, efforts were made to ensure that the sample recruited reflected the diversity of Kuwaiti patients with T2DM. Patients of various demographic and clinical characteristics were included (the sample varied in terms of age, sex, area of residence, education level, employment status, marital status, duration of diabetes, place of diabetes care, mode of treatment, dosage regimen, presence of complications, and presence of comorbidities). Therefore, the data collected allowed a range of perspectives to be identified. Table 1 shows the various demographic and clinical characteristics of study participants.
Table 1.
Sociodemographic and medical history of study participants (n=20)
| Variables | Summary statistics |
|---|---|
| Age, years | |
| Mean | 53.7 |
| 30–39 | 1 (5%) |
| 40–49 | 6 (30%) |
| 50–59 | 8 (40%) |
| 60–69 | 3 (15%) |
| ≥70 | 2 (10%) |
| Sex, n (%) | |
| Female | 10 (50) |
| Male | 10 (50) |
| Education, n (%) | |
| No formal education | 3 (15) |
| Primary/intermediate school | 1 (5) |
| High/secondary school | 7 (35) |
| Diploma/bachelor | 6 (30) |
| Marital status, n (%) | |
| Single | 2 (10) |
| Married | 18 (90) |
| Employment, n (%) | |
| Employed | 6 (30) |
| Retired | 10 (50) |
| Never employed | 4 (20) |
| Area of residence, n (%) | |
| Urban | 14 (70) |
| Rural | 6 (30) |
| Place of diabetes care, n (%) | |
| Primary care clinic | 13 (65) |
| Secondary care (outpatient hospital) clinic | 2 (10) |
| Combination of primary and secondary | 5 (25) |
| Duration of diabetes, n (%) | |
| <1 year | 2 (10) |
| 1 year | 2 (10) |
| 5–10 years | 5 (25) |
| >10 years | 11 (55) |
| Diabetes treatment, n (%) | |
| Oral hypoglycemic agent | 14 (70) |
| Insulin | 1 (5) |
| Oral plus insulin | 5 (25) |
| Dosage regimen, n (%) | |
| Once daily | 1 (5) |
| Twice daily | 9 (45) |
| Three times daily | 6 (30) |
| Four times daily | 4 (20) |
| Evidence of diabetes complications, n (%) | 10 (50) |
| Comorbidity, n (%) | 16 (80) |
A sample of Kuwaiti patients with type 2 diabetes were recruited from different general practices and hospitals of Kuwait. Patients were approached by the principal investigator as they presented for their outpatient appointments. The researcher introduced herself as a PhD student who was independent and separate from the hospital or polyclinic health care team. This was done to ensure that patients’ honest and accurate views were obtained. The researcher then explained to the participants that the aim of the study was to explore their views and experiences with their medications, as well as their disease and how they managed it. The agenda of the interview was hidden (ie, was not too obvious for participants) as participants were given only a vague idea of the central topic of the study so that spontaneous reactions could be obtained instead of thought out positions. Participation was voluntary, and participants were assured that the conduct of the study would have no impact on the health care they received by their health care professionals (eg, doctors, pharmacists, nurses, etc) as their responses would be anonymous and would not be communicated to their health care providers. Participants were also assured that there were no right or wrong answers, and that their honest views and opinions were the primary interest of the study. If respondents were willing to and could spare the time, they were given a patient information leaflet, which further explained the study’s aims and processes, along with contact details of the principal researcher for further details. Once, they had agreed to participate, participants were asked to sign a written consent to allow the interview to be digitally recorded, transcribed, analyzed, and published. Confidentiality and anonymity were reemphasized at this point. Sampling was guided by emerging data and continued until no new themes appeared (ie, when saturation of data was achieved). This was achieved with 20 participants. The first three participants were interviewed at home, while the remaining 17 participants were interviewed at the hospital or polyclinics were they were recruited from, as they preferred. Careful attention was given to make sure no one was around who could overhear or affect the flow of the interview.
The inclusion criteria for the study were: 1) Kuwaiti nationality, 2) age 18 years and older, 3) diagnosis of type 2 diabetes, 4) currently using oral hypoglycemic tablets, insulin, or both for the management of diabetes, and 5) no salient physical distress or cognitive dysfunction hindering the ability to participate in the study.
Interview topic guide
To meet the aim and objectives, a semi-structured topic guide was developed. Topics included were based on a review of the literature of factors that may influence medication adherence. The literature review included both qualitative and quantitative studies conducted in different countries around the world and revealed that many variables may act as barriers to patients’ medication adherence, such as poor knowledge about T2DM,7–9 lack of diabetes education by health care providers,9,10 health care providers’ attitudes,7,9,11 patients’ beliefs about their illness or medicines,12 fear of medication adverse effects,13 use of alternative or herbal remedies,14 complexity of diabetic treatment,9,10 and lack of social support.7 Therefore, topics included in the interview topic guide were designed to stimulate participants to talk about issues that might be related to adherence to their oral hypoglycemic medications or insulin (eg, their experiences with diagnosis, knowledge about diabetes/its medications, experiences with diabetes medications, experiences with alternative/herbal medicines, experiences with health care providers, experiences with current health care system, impact of diabetes on their lives, actual/perceived social support). The interview topic guide was flexible; more questions were added during the course of the interviews as participants raised issues of concern. Therefore, the researcher followed and expanded on arising issues to ensure obtaining participants’ individual experiences and concerns. In addition, respondents were allowed to talk freely, and in no particular order, which allowed exploration of topics according to the issues raised by participants. In this way, the researcher was able to tell which issues were most relevant and important to each participant.
The interview topic guide included both open-ended and closed questions. Closed questions were mostly used to gather factual data (eg, are you currently treated with tablets, insulin or both, for your diabetes?). Open-ended questions were used to capture and expand on the participant’s experience relevant to the topic of interest (eg, could you describe your experience of taking your diabetes tablets/insulin?). Furthermore, probes were also used to aid in deeper exploration of the participant’s perspectives. Leading questions were avoided to avoid introducing bias. The complete interview topic guide can be found in Table S1.
Data analysis, validity, and reliability of analysis
Framework analysis, which involves the use of a thematic framework to classify data according to key themes, concepts, and categories, was used to assess the interviews. This was carried out in a systematic process of sifting, charting, and sorting material according to key issues and themes. It is a matrix-based analytic method, which facilitates rigorous, transparent, and systematic data management, allowing researchers to move back and forth between different levels of abstraction without losing sight of the “raw” data.17 Sessions were digitally recorded and transcribed verbatim in Arabic by the principal investigator (FJA). Final themes were translated into English language by the principal investigator (FJA) and checked by another bilingual researcher. A qualitative data indexing software package (MAXQDA, 2007; VERBI GmbH, Berlin, Germany) was used to facilitate coding. The software allowed coding segments of text, storing the transcribed text in an organized form, searching and retrieval of particular segments of texts for inspection, linking relevant data to form categories, writing memos, counting frequencies of words or phrases, drawing of conclusions, and verification.
To ensure validity and reliability of the analyses, two interview transcripts (2/20, 10%) were separately and independently co-coded by the principal investigator (FJA) and another bilingual researcher (MW). The two then compared codes and resolved any differences by discussion. The number of agreements/disagreements between the two researchers in coding was counted, and intercoder reliability was estimated using the following formula:
Therefore, the percentage of agreement was 93% for the first transcript and 98% for the second interview transcript.
Furthermore, five coded interview transcripts (5/20, 25%) along with their coding indexes were translated to English by the principal investigator and then reviewed by the UK research team (NDB and TPB). In all cases, congruence was achieved.
Ethical approval
The study was approved by The Research Ethics Committee of the Ministry of Health, State of Kuwait. Informed consent was obtained from all patients prior to their participation in the study.
Results
A total of 20 Kuwaiti patients with T2DM participated in the study. This number of participants established the sample size for the study due to saturation of data. All those who were approached agreed to participate in the study, except for one participant who refused due to time constraints. Interviews were carried out between February and June, 2008. Interview duration ranged from 11 to 47 minutes, with a mean duration of 29 minutes. For most participants, interviews lasted between 35 and 45 minutes. The average time duration was brought down because of two exceptionally short interviews (~11 minutes). These two patients provided responses that were brief despite frequent probing attempts.
Themes
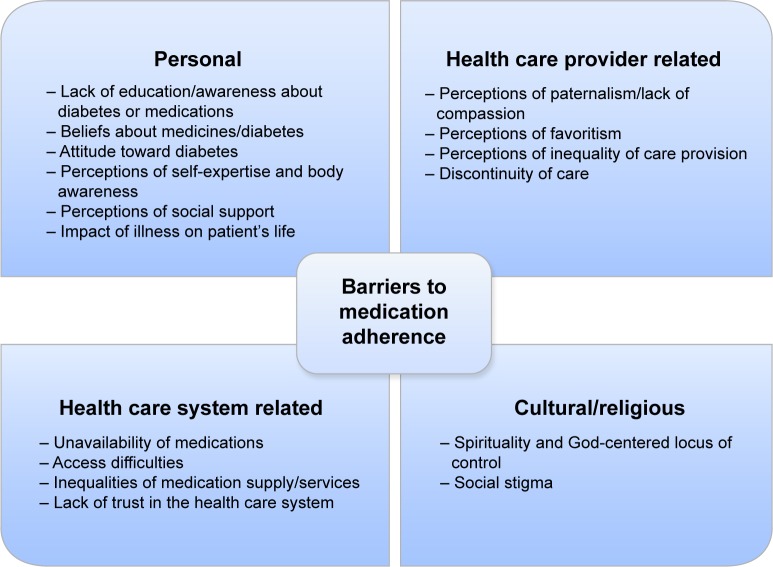
Analysis of the interviews revealed thematic saturation at 20 participants (ie, after 20 interviews, no new themes appeared). Themes related to barriers to medication adherence fell into four general types: 1) personal barriers, 2) health care provider-related barriers, 3) health care system-related barriers, and 4) cultural/religious barriers. Figure 1 illustrates these and lists the specific themes emerging under each type. The individual themes identified as barriers to medication adherence in the study sample are explained here, with representative quotations for further clarification.
Figure 1.
Types of identified barriers to medication adherence.
Main theme 1: personal barriers
Lack of education/awareness about diabetes/medications
Participants in this study showed insufficient knowledge about diabetes and its treatment. All but one participant (19/20, 95%) complained they had received little/no education from the physician.
I thought diabetes was like the flu, just a month or so at most and it would be gone. So I took my tablet for a while and then I stopped it for years until things got worse.
Some participants (6/20, 30%) doubted the effectiveness or lacked the understanding of how their medications worked to control their blood glucose levels.
These medications are useless! I’ve been taking them for years now and I still didn’t feel anything; my diabetes was never cured!
Although diabetic patients feared diabetic complications, they did not know how these occurred and how to manage or avoid them. In cases where diabetes education was provided by doctors, it was considered rather too little or too late, ie, after complications of diabetes had already developed.
As for pharmacists, participants reported a lack of education and counseling by pharmacists. Almost half the participants (11/20, 55%) perceived pharmacists to have a negligible or minimal role in providing care for patients with diabetes, seeing their role as limited to providing dosage instructions:
Pharmacists don’t provide any medication counseling, I just hand them my prescription and they just dispense me my medications. That’s how it is normally.
Pharmacists just tell you take this medication once, twice, or three times, that’s it!
Pharmacists often provided their dosage instructions by sketching a number of lines on the medication packaging, which corresponds to the number of times the patient is supposed to take the medication. Pharmacists likely assumed that the patient would find this easy and straightforward; however, many participants found it to be confusing:
To us the pharmacist is just the person who dispenses and writes instructions on the medications for us. To be more precise, it’s not even written, the pharmacist would just sketch a number of lines on the medication package corresponding to the number of times you should take that medicine, and it is up to you to figure the exact timings! (laughing).
Beliefs about medicines/diabetes
Having competing beliefs in effectiveness of herbal remedies was evident with a few participants (4/20, 20%), and might explain why some participants doubted the effectiveness of their traditional medications.
I sometimes use herbal remedies along with my diabetes medications, and believe it or not, I find herbal remedies better at lowering my blood glucose levels!
Almost half the participants (9/20, 45%) perceived traditional medications as harmful chemicals, too much of which, could have devastating effects on one’s health. Some participants believed that if you take too many medications, your body might somehow lose its immunity and grow weaker; therefore, they thought it might be wise to take less of these medications.
Potential or actual adverse effects of medications were a common concern shared by more than half of the participants (11/20, 55%), often resulting in patients deliberately stopping/taking less of their medications to avoid/alleviate these adverse effects (ie, intentional nonadherence).
For ten years now, I have been taking one tablet of Glucophage® instead of three because I don’t eat much, and I’m afraid I might get hypoglycaemia if I take three tablets.
In addition, some participants (4/20, 20%) perceived that physicians prescribe too many medications, without first checking whether patients really need them. Physicians’ overprescribing of insulin was of particular concern.
One conflicting belief emerged relating to the perceived quality of certain brands of medications. For example, some participants (3/20, 15%) believed that Western brands of diabetes medications were somehow more effective at lowering blood glucose levels than the local alternatives.
The German brand of Daonil® is the best. I have tried the Kuwaiti, Saudi and the UAE brands and they were all no good, they made my blood glucose levels go high.
Two participants (10%) held the opposite view about Western brands, with one believing that they were “poisons” imported from the West, while the other simply preferred local brands for their “freshness”. In terms of adverse effects, two out of 20 participants (10%) perceived Western brands of medications to have fewer adverse effects than local brands.
Attitude toward diabetes (eg, denial, downplaying severity of diabetes, fear of diabetes)
There was evidence that participants exhibited attitudes toward their diagnosis, which may have an impact on their adherence. For example, some participants (2/20, 10%) described feelings of denial toward their diagnosis with diabetes.
Deep inside, I just can’t accept that I have diabetes. I still haven’t come to terms with my diabetes, I’m in denial!
Other participants did not deny their diabetes, but yet did not pay careful attention to it, moving on with their lives as they would before their diagnosis (7/20, 35%). These participants showed evidence of downplaying the severity of their diabetes.
Diabetes is just an increase or decrease of blood glucose levels, that’s it! [...] you have to simplify things; diabetes is not a disease at all. You see, even kids can have it once the pancreas fails.
Interestingly, these comments did not appear to be out of ignorance, but rather a psychological defense strategy to avoid having to deal with the associated emotional and psychological pain.
Fear of diabetes or its complications was reported by the study participants and may have affected adherence to medications. For example, fear of hypoglycemia led some participants to decrease their medication intake, whereas for other participants, a fear of diabetes complications such as kidney damage and foot amputations led them to strictly adhere to their medications as directed by their doctors. Participants who had already developed complications (eg, kidney damage, retinal damage) or diabetes-related limitations in their daily lives appeared to be keener to adhere to their medication.
Perceptions of self-expertise with the disease and body awareness
Some participants (8/20, 40%) reported that they were able to skip and alter doses of their medications because they became experts at their diabetes. They reported being able to feel when they needed to reduce or increase the doses of their medications as their own bodies would provide cues for action.
When I have frequent urinations that would disrupt my sleep at night I know that I need to take an extra 20–30 units of insulin. I just know […] you kind of become an expert with time.
Perceptions of social support
This study identified the considerable role of participants’ families in their disease management in general and in medication taking in particular. Families were frequently quoted as an important source of support, providing moral as well as practical assistance to participants. More than half of participants (11/20, 55%) reported that their family members often made suitable meals for them to eat and reminded them to take their medications or to perform the self-monitoring activities.
My kids at home even the little ones now know my medications, they would get my tablets for me to take at lunch or dinner and they remind me when I forget.
Impact of illness on patient’s life
Whether or not diabetes had a great impact on participants’ lives seemed to influence their adherence to their medications/other diabetes treatment regimens. For example, some participants (5/20, 25%) reported that they had suffered eye or kidney damage as a result of diabetes. Additional participants (4/20, 20%) reported limitations in performing their daily activities because of diabetes.
I can’t even drive anymore, I can’t see properly so people have to drive me everywhere [...] I got my own driver now who takes me everywhere.
In general, participants who had developed diabetes complications or diabetes-related limitations seemed to be more careful about their medications than those who had not.
Main theme 2: health care provider-related barriers
Perceptions of paternalism/lack of compassion
Physicians, the perceived key players in delivering diabetes patient care in Kuwait, were frequently criticized for their paternalism and for ignoring the patient’s perspective during medical consultations.
The doctor doesn’t say much, he would only prescribe the medications and that’s it! Even when I try to discuss something about my medications, he just doesn’t care or pay attention.
An extreme case of paternalism was described by one participant, who illustrated how some physicians were not open for discussion or having their decisions challenged by patients:
My blood sugar level was high so the doctor wanted to put me on injections and I didn’t want that. She just told me (in a threatening tone), “That’s it! No more tablets for you; you are going straight on injections!” I said “Doctor, please, I would like to continue taking my tablets” [...] but then she said (angrily) “You are not the doctor here, I am, so that’s the end of discussion”!
It is worth highlighting here that while some participants disapproved of paternalism; others advocated for this approach and found it natural for physicians to be fully responsible for making treatment decisions. Five out of 20 participants (25%) had no wish to be involved in influencing their own treatment plans and thought that physicians were better suited to perform this task. These participants reported never questioning treatment options, considering it inappropriate to question or challenge the physician’s decisions.
Perceptions of favoritism/inequality of care provision
Health care providers’ inequality of care and favoritism was also raised by some participants (3/20, 15%) as an issue of concern. There was a notion that “better” medications and treatment were provided for certain people, such as friends or acquaintances of health care providers, or those of higher societal status.
The doctor would just look at the patient, if the patient appeared simple and modest the doctor would just talk down to him and not treat him right, or might even kick him out!
Let me tell you something, they (doctors) would never prescribe the good medications for me or for you. They would give them to other people, the “special” people. They have the good medications, it’s all available but they would never give it to me for example, they save the good stuff for some other people.
They (pharmacists) would never treat you right unless they personally know you. They have never been helpful to me my entire life, not even once have they said anything about the medications to me!
When I asked for an extra month’s supply they (pharmacists) declined to provide me with it, I’m sure they wouldn’t have if they personally knew me.
Discontinuity of care
Discontinuity of care was seen as a concern by some participants. Seven participants (7/20, 35%) had experienced a change in the physician who usually treated them. For the majority of these participants (6/7, 85%), the previous physician was usually the preferred one, and therefore, their transfer to another physician was seen as neither helpful nor appreciated.
My previous doctor was really nice and good, ever since he left I never came here for my diabetes.
Other issues related to health care providers identified in this study, which might have implications for patients’ adherence to medication, include inflexibility of physicians about their appointments (ie, being inconsiderate to patients if they missed their appointments) and having extended time gaps between appointments.
Main theme 3: health care system-related barriers
Unavailability of medications
Unavailability of specific medications and/or dosages in government pharmacies at the time of prescription refills was reported by a quarter of participants (5/20, 25%) and may present barriers to medication adherence.
The doctor told me to take two tablets of Glucophage® but I only take one because it’s 850 mg. You know, I am supposed to take two of the 500 mg tablets, but sometimes it’s not available and they give me the 850 mg instead.
Access difficulties
Access to physicians for diabetes follow-up was perceived as unsatisfactory. Seven participants (7/20, 35%) reported that they were unable to see their physician as frequently as they liked. A few participants (3/20, 15%) complained that there was no specialized diabetes center where all diabetes-related services were provided. Participants reported having to go to a number of different places to carry out routine diabetes-related investigations, which was cumbersome and inconvenient. In addition, one of the concerns reported by a couple of participants (2/20, 10%) was that in case of diabetes emergencies, there was no choice but to go to hospitals which were far away.
Access to medications was also problematic. One common complaint was that some diabetes medications were unavailable for dispensing at polyclinics (4/20, 20%); patients had to go to hospitals to collect some of their diabetes medications. Having to wait for a long time for prescriptions to be filled or dispensed at the pharmacy was also a troublesome issue for a few participants (4/20, 20%) who complained of long queues, which made them avoid collecting their medications.
Inequalities of medication supply and services
A quarter of participants (5/20, 25%) perceived that there were inequalities in care provision and supply of medication at different clinics or hospitals. One participant complained of inequality in dispensing medication supplies in different health districts, with patients receiving more quantities of their medications at some districts. In addition, another participant perceived that there was a disparity in the quality of medical services provided for patients at different health districts, and considered people living in rural areas as disadvantaged compared to people living in inner cities of Kuwait.
People in Al-Jahra district have no access to good quality medical services like people in the city, so they often travel to get treated at city hospitals, where there are better services and where people treat them better.
Lack of trust in the government health care system
Participants (4/20, 20%) reported a lack of trust in the government health care system as a whole, with some (3/20, 15%) reporting turning to the private sector to provide them with better care.
If you catch the flu for example here at government sector they would typically give you a medication that won’t work, even if you finish the whole bottle. If you go to the private doctor however, he (the doctor) would prescribe you the best medication out there, you just have to take a tablet or two and you’d be all better already. Medications at the Ministry of Health are not that effective.
Main theme 4: cultural and religious barriers
Spirituality and God-centered locus of control
Participants in this study reflected an attitude of fatalism and God-centered locus of control, which might influence adherence to medications or other diabetes self-care behaviors. According to many participants (6/20, 30%), although medicines may control diabetes, only God can cure it.
Healing comes from God, not the doctor. If God wants to cure you, you will be cured, and if he wants to harm you, you will be harmed [...] If God wants you to live you will live, and if he wants you to die, you will die. It’s all up to God, not the doctor [...] what is meant to be will be.
Social stigma
Social stigma associated with the diagnosis of diabetes appeared to influence participants’ adherence to their medications. Some participants (2/20, 10%) reported that they would never take their medications in front of others, for fear of being stigmatized for having the disease. These participants were among the youngest participants of the sample (35 and 43 years old) and perceived diabetes to be associated with older people.
Discussion
This study is the first to explore nonadherence to medications among Kuwaiti patients with T2DM. Only three other studies have addressed the problem of nonadherence to medications in Kuwait;18–20 however, all focused on psychiatric patients. Till date, there have been no studies which included the patients’ perspective. It is argued that diabetes improvement initiatives that neglect the patient perspective may be destined for limited success.21–23 Furthermore, the methods employed in this study allowed access to participants’ views without using translators during interviews, thereby enhancing the quality of the data.
Results from this study suggest that barriers to medication adherence among Kuwaitis with T2DM can be categorized into four different groups: 1) personal barriers, 2) health care provider-related barriers, 3) health care system-related barriers, and 4) cultural or religious barriers. The themes falling under each category of barriers showed some similarities as well as notable differences when compared with studies carried out on Western populations.
In terms of the differences, one of the most interesting findings of our study was related to the set of beliefs about medicines held by some Kuwaiti T2DM patients. In our study, Western brands of medications were perceived by some participants as superior to local alternatives; they were specifically perceived to have better effectiveness, better quality, and fewer adverse effects. This finding is not adequately described in the literature, although similar perceptions were cited by British Pakistani and British Indian T2DM patients about their oral hypoglycemic compared to those which could be obtained from the Indian subcontinent.12 Interestingly, although some preferred Western brands, others preferred local brands of medicines for their perceived freshness or a general lack of trust in the Western world. Health care providers, particularly doctors and pharmacists, are in great position to identify patients’ preferences regarding specific brands of medications. Taking into account patients’ preferences by prescribing and dispensing the preferred brands of medications, where possible, may avoid the waste of expensive medications and ensure that patients would adhere to their prescribed medications. However, in real practice, this may not always be possible. In this case, health care providers need to address patients’ concerns and assure them about the bioequivalence of alternative brands.
In addition, results from our study revealed that some health care providers were perceived to have unethical attitudes, such as favoritism and inequality of care provision. Participants reported that doctors, or pharmacists, treated people they knew better and provided them with better medications and better treatment. Methods for detecting discriminatory practices and changing the behaviors of health care providers who demonstrate these are recommended.
Despite the culturally specific barriers to medication adherence identified in our study, our findings also showed that Kuwaiti patients with T2DM faced many similar barriers to medication adherence as those identified in the Western literature. Conversely, many variables which facilitate adherence to medications in our population were similar to those reported in the Western literature.
In accordance with the literature,24–27 our study highlighted that Kuwaiti T2DM patients’ families were an important source of support for patients in terms of managing diabetes and taking medications. This may be linked to the strong familial and social relations held within the Kuwaiti society and can therefore be utilized by health care providers through involving family members in the management of T2DM patients. Including patients’ families in discussions and decisions about diabetes treatment has the potential to promote medication adherence in T2DM.
Furthermore, and consistent with findings of other studies,8,10,11,14,25,28 this research highlighted that God-centered locus of control and religion played an important role in the way some Kuwaiti T2DM patients managed their diabetes. This may be related to the patients’ strong religious Muslim views, which shape and influence all aspects of life of the Kuwaiti people. The Islamic faith constitutes a major support system for Muslims, providing the strength and hope that allows people to cope with illness. To Muslims, everything is explained in terms of God’s will. This has implications for health care providers in terms of supporting patients who turn to their faith to help them cope with their disease, as patients’ with a God-centered locus of control may be underestimating the role of medications and demonstrate nonadherence. Nonetheless, Islamic religion supports the notion of integrity and wellbeing of the human soul and body, and therefore educational programs to raise religious and health awareness can be implemented to prevent non-adherence to medications as result of fatalism and a God-centered locus of control.
Participants perceived physicians to be the key players in delivering care for patients with type 2 diabetes in Kuwait. Nevertheless, descriptions of paternalism during medical consultations were common throughout the interviews, consistent with qualitative studies from other parts of the world.7,9,11 Health care providers should make an effort to include patients more in their own health care plan and allow them to assume more responsibility for their disease outcomes.
Despite the key role played by doctors in providing T2DM patient care in Kuwait, data from this qualitative study suggest that health care providers such as doctors and pharmacists failed to provide sufficient education and support to the Kuwaiti T2DM patients, which is in line with findings of other studies of diabetic patients.8,9,28 This was attributed to a general lack of communication between doctors as well as pharmacists and their T2DM patients. Participants cited that the doctors’ role was limited to prescribing medications, whereas the pharmacists’ role was limited to dispensing medications, often with unclear labeling instructions. Consequently, if patients are unsure how to take the medications, they might use them the wrong way or not take them altogether resulting in unintentional nonadherence to their medications. This research suggests that more pharmacist involvement may have a great potential for improving adherence to T2DM medications in Kuwait.
Certain attitudes toward illness were salient among participants and appeared to have an impact on their adherence to medications. These attitudes influenced adherence either in positive or in a negative direction. Particularly, denial, downplaying severity of diabetes, social stigma, and perceptions of expertise with diabetes and body awareness appeared to hinder participants’ adherence to their medications. Conversely, fear of diabetes, and perceptions of social support appeared to improve medication adherence. Health care providers need to spot these attitudes and consider them when designing interventions to improve medication adherence.
Negative perceptions of systematic factors appear to be affecting access to and views of care and these may be contributing to system-related barriers to medication adherence. For example, results from our study showed that there was a lack of organization and coordination in diabetes services provided by different health care providers within the Ministry of Health. Furthermore, diabetes care was provided in places that were perceived to be inconveniently distanced from each other, and this was cited to present access difficulties, especially in rural areas of the country. In addition, the availability of diabetes medications varied between different districts, with rural areas of the country being perceived as disadvantaged in this regard. The evidence from the literature suggests that improving care and outcomes for patients with chronic disease depends on reshaping and organizing health care systems so that patients would receive planned, regular interactions with health care providers, with prevention of disease exacerbation and complications being the focus of the interaction. Further, systematic assessments of patients, adhering to treatment guidelines, supporting the patient’s role as a self-manager, and continuous follow-up are all necessary components of an organized health care system that would improve the care for patients with chronic disease.29,30
Findings of this research can augment what is known about medication adherence from the Western literature, can aid in the design of culturally sensitive adherence interventions, and can provide the foundation of governmental program development. The results will also inform a larger, quantitative assessment of medication adherence in Kuwait. This study identified a number of personal, health care provider-related and health care system-related barriers to medication adherence. However, findings of the current study must be interpreted with caution due to several limitations. First, the sample only included Kuwaitis with type 2 diabetes. Results may not be transferrable to non-Kuwaitis or patients taking medications for other diseases. In addition, participants were recruited from clinics, polyclinics, and hospitals, which may have introduced bias toward those who access medical care and who are likely to be more concerned about their health.
Supplementary material
Table S1.
Interview topic guide
| 1. Diagnosis |
| •Could you tell me when and how were you diagnosed? |
| •How did you experience the diagnosis of diabetes? |
| 2. Knowledge about diabetes and medications |
| •In your opinion what causes diabetes? |
| •In your opinion, how should diabetes best be treated? |
| •How do you describe your health at the present, and what do you think it is going to be like in 10–20 years’ time? |
| •Could you describe the consequences of diabetes in the future? (Probe: complications) |
| •How do you know when you are sick with your diabetes? (Probe: describe symptoms of hypoglycemia, hyperglycemia) |
| •Could you describe what do you do when you are sick with diabetes? (Probe: hyperglycemia, hypoglycemia, foot problems) |
| •What is/are the source(s) of your information/knowledge about diabetes/its medications? |
| 3. Views and experiences with diabetes medications |
| •Are you currently treated with tablets, insulin, or both for your diabetes? |
| •What medications are you currently taking for your diabetes? |
| •How do you take your medications? |
| •What do you think of your medications? (Probe: effectiveness in the short-term and in the long-term) |
| •Could you describe your experience of taking your diabetes tablets/insulin? (Probe: effectiveness, practical difficulties, adverse effects) |
| •Have you ever experienced difficulties taking your mediations for diabetes? If yes, please describe |
| •Can you remember a time where you could not take your medications as prescribed by your doctor? If yes, can you tell me what happened? |
| •Some people alter the use of their medications and find their own way of using their medications for many reasons. Can you think of a time when you have done so? |
| •If yes, how do you feel about this? Do you tell anyone about these decisions? |
| 4. Views and experiences with alternative/herbal medicines |
| •Do you use herbal/complimentary medicines for your diabetes? |
| •If yes, could you describe your experience with such therapy? |
| •If yes, how do you feel about these compared to your regular medications? (Probe: adverse effects, effectiveness) |
| 5. Views and experiences with health care providers (doctors, pharmacists, nurses, dietitians) |
| •Could you describe your views and experiences with your doctor? (Probe: type of relationship, communication style) |
| •How do you feel about the education and counseling provided by your doctor about diabetes/medications? (Probe: sufficiency of informationreceived about your diabetes/medications/other treatment behaviors) |
| •Has your doctor involved you in decisions relating to your own treatment plan? (Probe: to what degree?) |
| •If your doctor has decided on your therapeutic regimen, how do you feel about that? (Probe: degree of control and responsibility for own treatment desired) |
| •Do you always get the chance to be followed up with the same doctor? If not, how do you feel about that? |
| •Could you describe your experience with pharmacists? |
| •How do you feel about the education and counseling provided by your pharmacists? |
| •Could you describe your experience with other health care providers who were involved in your diabetes, eg, nurses, dietitians, etc? (Probe: who? What do you think of them in terms of diabetes care provided?) |
| 6. Views and experiences with current health care system at the Ministry of Health |
| •What is your view of the current health care system? (Probe: health services provided) |
| •How do you feel about access to health care providers or medications? (Probe: describe ease/difficulty?) |
| •What should the Ministry of Health do to help patients with type 2 diabetes? (Probe: sufficiency of what it currently provided) |
| 7. Impact of diabetes on participant’s life |
| •In what way have diabetes changed your life? (Probe: describe living with diabetes on a daily basis, how does your life differ from someone who does not have diabetes?) |
| •How do you feel about these changes? |
| 8. Actual/perceived social support |
| •Do you receive any kind of support from your family in terms of managing your diabetes? (Probe: help with medications, SBGM, preparation ofdiabetic meals, etc) |
| •If yes, could you describe the role of your family in management of your disease? (Probe: practical or moral support) |
| Is there anything else you think that you wanted to say? |
| Thank and close |
Abbreviation: SBGM, self-blood glucose monitoring.
Acknowledgments
Data were collected as part of a PhD program, funded by Faculty of Pharmacy, Kuwait University. The authors thank the patients who shared their experiences and perceptions. Special thanks to Miss Bothaina Alhaddad, Department of Practice and Policy, University College London School of Pharmacy for her help in the validation of translation of the interview transcripts.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Abdella N, Khogali M, Al-Ali S, Gumaa K, Bajaj J. Known type 2 diabetes mellitus among the Kuwaiti population. Acta Diabetol. 1996;33:145–149. doi: 10.1007/BF00569425. [DOI] [PubMed] [Google Scholar]
- 2.Abdella N, Alarouj M, Alnakhi A, Alassoussi A, Moussa M. Non-insulin-dependent diabetes in Kuwait: prevalence rates and associated risk factors. Diabetes Res Clin Pract. 1998;42:187–196. doi: 10.1016/s0168-8227(98)00104-1. [DOI] [PubMed] [Google Scholar]
- 3.Shah NM, Behbehani J, Shah MA. Prevalence and correlates of major chronic illnesses among older Kuwaiti nationals in two governorates. Med Princ Pract. 2010;19(2):105–12. doi: 10.1159/000273069. [DOI] [PubMed] [Google Scholar]
- 4.Moussa MA, Alsaeid M, Abdella N, Refai TM, Al-Sheikh N, Gomez JE. Prevalence of type 2 diabetes mellitus among Kuwaiti children and adolescents. Med Princ Pract. 2008;17(4):270–275. doi: 10.1159/000129604. [DOI] [PubMed] [Google Scholar]
- 5.Cramer JA. A systematic review of adherence with medications for diabetes. Diabetes Care. 2004;27:1218–1224. doi: 10.2337/diacare.27.5.1218. [DOI] [PubMed] [Google Scholar]
- 6.Lee WC, Balu S, Cobden D, Joshi AV, Pashos CL. Prevalence and economic consequences of medication adherence in diabetes: a systematic literature review. Manag Care Interface. 2006;19:31–41. [PubMed] [Google Scholar]
- 7.Vinter-Repalust N, Petricek G, Kati M. Obstacles which patients with type 2 diabetes meet while adhering to the therapeutic regimen in everyday life: qualitative study. Croat Med J. 2004;45:630–636. [PubMed] [Google Scholar]
- 8.Adams CR. Lessons learned from urban Latinas with type 2 diabetes mellitus. J Transcult Nurs. 2003;14:255–265. doi: 10.1177/1043659603014003012. [DOI] [PubMed] [Google Scholar]
- 9.Vermeire E, Van Royen P, Coenen S, Wens J, Denekens J. The adherence of type 2 diabetes patients to their therapeutic regimens: a qualitative study from the patient’s perspective. Pract Diabetes Int. 2003;20:209–214. [Google Scholar]
- 10.Utz SW, Steeves RH, Wenzel J, et al. “Working hard with it”: self-management of type 2 diabetes by rural African Americans. Fam Community Health. 2006;29:195–205. doi: 10.1097/00003727-200607000-00006. [DOI] [PubMed] [Google Scholar]
- 11.Greenhalgh T, Helman C, Chowdhury AM. Health beliefs and folk models of diabetes in British Bangladeshis: a qualitative study. BMJ. 1998;316:978–983. doi: 10.1136/bmj.316.7136.978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lawton J, Ahmad N, Hallowell N, Hanna L, Douglas M. Perceptions and experiences of taking oral hypoglycaemic agents among people of Pakistani and Indian origin: qualitative study. BMJ. 2005;330:1247. doi: 10.1136/bmj.38460.642789.E0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hayes RP, Bowman L, Monahan PO, Marrero DG, McHorney CA. Understanding diabetes medications from the perspective of patients with type 2 diabetes: prerequisite to medication concordance. Diabetes Educ. 2006;32:404–414. doi: 10.1177/0145721706288182. [DOI] [PubMed] [Google Scholar]
- 14.Devlin H, Roberts M, Okaya A, Xiong YM. Our lives were healthier before: focus groups with African American, American Indian, Hispanic/Latino, and Hmong people with diabetes. Health Promot Pract. 2006;7:47–55. doi: 10.1177/1524839905275395. [DOI] [PubMed] [Google Scholar]
- 15.Vermeire E, Hearnshaw H, Van RP, Denekens J. Patient adherence to treatment: three decades of research. A comprehensive review. J Clin Pharm Ther. 2001;26:331–342. doi: 10.1046/j.1365-2710.2001.00363.x. [DOI] [PubMed] [Google Scholar]
- 16.Donovan JL. Patient decision making. The missing ingredient in compliance research. Int J Technol Assess Health Care. 1995;11:443–455. doi: 10.1017/s0266462300008667. [DOI] [PubMed] [Google Scholar]
- 17.Ritchie J, Spencer L. Analyzing Qualitative Data. London, UK: Routledge; 1994. [Google Scholar]
- 18.Al-Saffar N, Deshmukh A, Eid S, Carter P. Health beliefs and drug compliance of depressed patients in Kuwait. J Soc Adm Pharm. 2003;20:142–150. [Google Scholar]
- 19.Al-Saffar N, Deshmukh AA, Carter P, Adib SM. Effect of information leaflets and counselling on antidepressant adherence: open randomised controlled trial in a psychiatric hospital in Kuwait. Int J Pharm Pract. 2005;13(2):123–131. [Google Scholar]
- 20.Fido A, Husseini A. Noncompliance with treatment among psychiatric patients in Kuwait. Med Princ Pract. 1998;7:28–32. [Google Scholar]
- 21.Padgett D, Mumford E, Hynes M, Carter R. Meta-analysis of the effects of educational and psychosocial interventions on management of diabetes mellitus. J Clin Epidemiol. 1988;41:1007–1030. doi: 10.1016/0895-4356(88)90040-6. [DOI] [PubMed] [Google Scholar]
- 22.Ball TD. Search for wholeness: the adventures of a doctor-patient. Pharos Alpha Omega Alpha Honor Med Soc. 1991;54:28–31. [PubMed] [Google Scholar]
- 23.Lorenz RA, Bubb J, Davis D, et al. Changing behavior. Practical lessons from the diabetes control and complications trial. Diabetes Care. 1996;19:648–652. doi: 10.2337/diacare.19.6.648. [DOI] [PubMed] [Google Scholar]
- 24.Lohri-Posey B. Middle-aged Appalachians living with diabetes mellitus: a family affair. Fam Community Health. 2006;29:214s–220s. doi: 10.1097/00003727-200607000-00008. [DOI] [PubMed] [Google Scholar]
- 25.Puavilai A, Stuifbergen AK. Quality of life for Thai women with diabetes. Health Care Women Int. 2000;21:471–483. doi: 10.1080/07399330050130278. [DOI] [PubMed] [Google Scholar]
- 26.Xu Y, Toobert D, Savage C, Pan W, Whitmer K. Factors influencing diabetes self-management in Chinese people with type 2 diabetes. Res Nurs Health. 2008;31:613–625. doi: 10.1002/nur.20293. [DOI] [PubMed] [Google Scholar]
- 27.Stone M, Pound E, Pancholi A, Farooqi A, Khunti K. Empowering patients with diabetes: a qualitative primary care study focusing on South Asians in Leicester, UK. Fam Pract. 2005;22:647–652. doi: 10.1093/fampra/cmi069. [DOI] [PubMed] [Google Scholar]
- 28.Hernandez CA, Antone I, Corneliusn IA. Grounded theory study of the experience of type 2 diabetes mellitus in first nations adults in Canada. J Transcult Nurs. 1999;10:220–228. doi: 10.1177/104365969901000313. [DOI] [PubMed] [Google Scholar]
- 29.Wagner EH, Austin BT, Von KM. Organizing care for patients with chronic illness. Milbank Q. 1996;74:511–544. [PubMed] [Google Scholar]
- 30.Wagner EH. Chronic disease management: what will it take to improve care for chronic illness? Eff Clin Pract. 1998;1:2–4. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1.
Interview topic guide
| 1. Diagnosis |
| •Could you tell me when and how were you diagnosed? |
| •How did you experience the diagnosis of diabetes? |
| 2. Knowledge about diabetes and medications |
| •In your opinion what causes diabetes? |
| •In your opinion, how should diabetes best be treated? |
| •How do you describe your health at the present, and what do you think it is going to be like in 10–20 years’ time? |
| •Could you describe the consequences of diabetes in the future? (Probe: complications) |
| •How do you know when you are sick with your diabetes? (Probe: describe symptoms of hypoglycemia, hyperglycemia) |
| •Could you describe what do you do when you are sick with diabetes? (Probe: hyperglycemia, hypoglycemia, foot problems) |
| •What is/are the source(s) of your information/knowledge about diabetes/its medications? |
| 3. Views and experiences with diabetes medications |
| •Are you currently treated with tablets, insulin, or both for your diabetes? |
| •What medications are you currently taking for your diabetes? |
| •How do you take your medications? |
| •What do you think of your medications? (Probe: effectiveness in the short-term and in the long-term) |
| •Could you describe your experience of taking your diabetes tablets/insulin? (Probe: effectiveness, practical difficulties, adverse effects) |
| •Have you ever experienced difficulties taking your mediations for diabetes? If yes, please describe |
| •Can you remember a time where you could not take your medications as prescribed by your doctor? If yes, can you tell me what happened? |
| •Some people alter the use of their medications and find their own way of using their medications for many reasons. Can you think of a time when you have done so? |
| •If yes, how do you feel about this? Do you tell anyone about these decisions? |
| 4. Views and experiences with alternative/herbal medicines |
| •Do you use herbal/complimentary medicines for your diabetes? |
| •If yes, could you describe your experience with such therapy? |
| •If yes, how do you feel about these compared to your regular medications? (Probe: adverse effects, effectiveness) |
| 5. Views and experiences with health care providers (doctors, pharmacists, nurses, dietitians) |
| •Could you describe your views and experiences with your doctor? (Probe: type of relationship, communication style) |
| •How do you feel about the education and counseling provided by your doctor about diabetes/medications? (Probe: sufficiency of informationreceived about your diabetes/medications/other treatment behaviors) |
| •Has your doctor involved you in decisions relating to your own treatment plan? (Probe: to what degree?) |
| •If your doctor has decided on your therapeutic regimen, how do you feel about that? (Probe: degree of control and responsibility for own treatment desired) |
| •Do you always get the chance to be followed up with the same doctor? If not, how do you feel about that? |
| •Could you describe your experience with pharmacists? |
| •How do you feel about the education and counseling provided by your pharmacists? |
| •Could you describe your experience with other health care providers who were involved in your diabetes, eg, nurses, dietitians, etc? (Probe: who? What do you think of them in terms of diabetes care provided?) |
| 6. Views and experiences with current health care system at the Ministry of Health |
| •What is your view of the current health care system? (Probe: health services provided) |
| •How do you feel about access to health care providers or medications? (Probe: describe ease/difficulty?) |
| •What should the Ministry of Health do to help patients with type 2 diabetes? (Probe: sufficiency of what it currently provided) |
| 7. Impact of diabetes on participant’s life |
| •In what way have diabetes changed your life? (Probe: describe living with diabetes on a daily basis, how does your life differ from someone who does not have diabetes?) |
| •How do you feel about these changes? |
| 8. Actual/perceived social support |
| •Do you receive any kind of support from your family in terms of managing your diabetes? (Probe: help with medications, SBGM, preparation ofdiabetic meals, etc) |
| •If yes, could you describe the role of your family in management of your disease? (Probe: practical or moral support) |
| Is there anything else you think that you wanted to say? |
| Thank and close |
Abbreviation: SBGM, self-blood glucose monitoring.