Abstract
Purpose
Although bilateral lower-limb lengthening has been performed on patients with achondroplasia, the outcomes for the tibia and femur in terms of radiographic parameters, clinical results, and complications have not been compared with each other. We proposed 1) to compare the radiological outcomes of femoral and tibial lengthening and 2) to investigate the differences of complications related to lengthening.
Materials and Methods
We retrospectively reviewed 28 patients (average age, 14 years 4 months) with achondroplasia who underwent bilateral limb lengthening between 2004 and 2012. All patients first underwent bilateral tibial lengthening, and at 9-48 months (average, 17.8 months) after this procedure, bilateral femoral lengthening was performed. We analyzed the pixel value ratio (PVR) and characteristics of the callus of the lengthened area on serial radiographs. The external fixation index (EFI) and healing index (HI) were computed to compare tibial and femoral lengthening. The complications related to lengthening were assessed.
Results
The average gain in length was 8.4 cm for the femur and 9.8 cm for the tibia. The PVR, EFI, and HI of the tibia were significantly better than those of the femur. Fewer complications were found during the lengthening of the tibia than during the lengthening of the femur.
Conclusion
Tibial lengthening had a significantly lower complication rate and a higher callus formation rate than femoral lengthening. Our findings suggest that bilateral limb lengthening (tibia, followed by femur) remains a reasonable option; however, we should be more cautious when performing femoral lengthening in selected patients.
Keywords: Achondroplasia, bone lengthening
INTRODUCTION
Achondroplasia is the most common form of rhizomelic dwarfism, with an incidence of approximately 1 in 25000 people.1,2,3,4 Bilateral lower-limb lengthening has been commonly performed for patients with achondroplasia, as it improves the quality of life (QOL) in selected patients.2 However, only a small number of reports have described bilateral lengthening of both the femur and tibia in these patients.5,6,7 Moreover, these and other previous studies analyzed the femur and tibia as a whole, and these bones were not compared with each other in terms of the proportion of each limb segment and the rates of callus formation, consolidation, and complications.2,4,6,8,9,10
Therefore, we proposed 1) to compare the radiological outcomes of femoral and tibial lengthening and 2) to investigate the differences of complications related with bilateral lower-limb lengthening in patients with achondroplasia.
MATERIALS AND METHODS
After receiving approval from the Institutional Review Board of our hospital, we retrospectively reviewed 142 patients with achondroplasia who underwent lengthening procedures between January 2004 and December 2012. All patients were diagnosed with achondroplasia as proven by genetic evaluation. The clinical features and radiographic findings were examined by pediatric orthopedic surgeons and musculoskeletal radiologists. Any patient with achondroplasia who had joint pain related to abnormal limb alignment and functional deficit (including gait impairment) and who was willing to undergo surgery for limb lengthening for psychological or cosmetic reasons was eligible for the surgery. Patients who had previous injuries or bony surgery involving the lower extremities, medical comorbidities (e.g., heart disease, restrictive or obstructive lung diseases, neurologic issues such as cervicomedullary compression) that could render the patient at high risk for surgery, or other systemic diseases were excluded. Ultimately, 28 patients (112 segments; 56 femora and 56 tibias) who underwent bilateral tibial lengthening with an Ilizarov ring fixator and bilateral femoral lengthening with a monolateral external fixator were included in this study. Our goals of surgery were to realign the mechanical axis and to lengthen of bone segment by more than 30% of its initial length. The average ages of the patients at tibial and femoral lengthening surgeries were 9.2 years (range, 5.5-20.3 years) and 10.8 years (range, 6.8-21.5 years), respectively. The study population consisted of 10 males and 18 females. All patients first underwent bilateral tibial lengthening, and 9-48 months (average, 17.8 months) after this procedure, bilateral femoral lengthening was performed. The minimum follow-up period was 1 year after the femoral lengthening surgery (average, 3.8 years; range, 1.3-6.8 years). All data were obtained from medical records and radiographs.
Operative technique
All surgeries were performed by the senior author (HRS). At the time of the initial visit, all patients showed short stature (<3% of the average age-matched height) with genu varum deformity, ankle varus related to a long fibula, and severe medial deviation of the mechanical axis. Lengthening and angular correction of the tibia was performed first, as there should be no difference between the anatomical axis and the mechanical axis of tibia. We used the Ilizarov ring fixator for tibial lengthening after peroneal nerve release. Three or four rings were used depending on whether unifocal or bifocal osteotomies were performed around the center of rotation of angulation (CORA) for gradual correction of the deformity (if indicated) and lengthening. Paired hinges were aligned with the apex of the deformity, and a single lengthening rod was placed opposite to these hinges. We used two wires each at the proximal and distal rings. The proximal and distal tibiofibular joints were each transfixed with a wire to prevent distal or proximal migration of the fibula, respectively. We inserted two additional half pins at the proximal and middle rings. Osteotomy was performed using the multiple drill hole method around the level of the CORA. A monolateral external fixator (Dynaextor, BK Meditech, Seoul, Korea) was used for femoral lengthening. Two to four Schanz screws were inserted in the proximal and distal ends of the femur perpendicular to the anatomic axis. A transverse osteotomy was performed at the mid-diaphyseal region in all cases after longitudinally incising the periosteum. All procedures were conducted under image intensifier guidance. Postoperatively, full weight bearing was allowed from 3 days after the surgery, and lengthening was started after 7 days at a rate of 1 mm/day (0.25 mm every 6 hours). For tibial bone segments with bifocal osteotomies, lengthening was performed on the proximal metaphyseal area. The rate was adjusted during follow-up according to the morphologic features of the callus as described by Li, et al.11 Rotational deformities were gradually corrected at the end of the lengthening period. We removed the fixator when we observed three continuous cortices on the radiographs, and we also based our decision on the serial pixel value ratios (PVRs) as previously described.12 Patients underwent supervised daily physiotherapy, including active and passive range of motion (ROM) of the knee and ankle, beginning 2 days after surgery. Patients were followed on a weekly basis for the first month, bi-weekly during the lengthening period, and then monthly during the consolidation period.
Radiographic evaluation
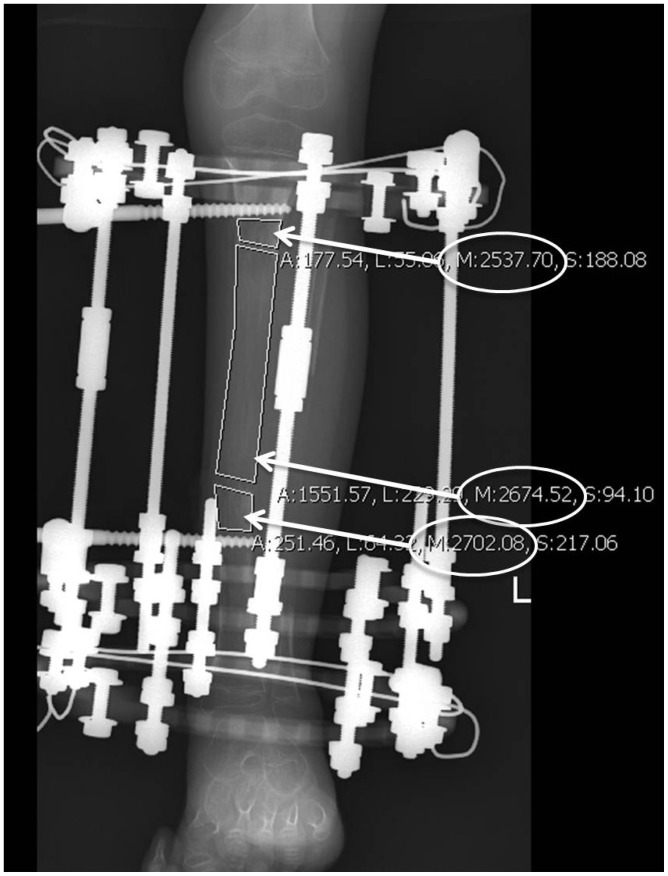
Standard radiographs of both lower limbs were taken at each follow-up visit and compared with the preoperative and immediate postoperative images. All radiographs were studied by three independent observers (KWP, RNG, CAR) using Star PACS PiView (Star 5.0.6.1 software, Infinitt Co. Ltd., Seoul, Korea). At the time of each visit, we measured the amount of lengthening and the PVR. The serial PVR was measured on the calluses of the regeneration areas using the free-line range of interest method (Fig. 1).12,13 A PVR of 1 indicated corticalization of the regenerate in the lengthening area. The radiological features of distraction osteogenesis were classified with regard to shape and type on the basis of the Li, et al.11 classification. The shape was based on the width of the callus compared to the original osteotomy site. The type was based on the callus shape (cylindrical, fusiform, or concave), three patterns of osteogenesis (homogeneous, heterogeneous, and lucent), and three densities (low, intermediate, and normal). The density was judged relative to the adjacent soft tissues and cortex. At the final follow up, we recorded the amount of lengthening, percentage of initial length gained, lengthening index (LI), external fixator index (EFI), and healing index (HI). The LI was calculated by dividing the duration of lengthening in days by the total length of the regenerate in cm. EFI was calculated by dividing the entire duration of external fixator application in days by the total length of the regenerate in cm. The HI was calculated by dividing the duration of consolidation in days (from the time of lengthening cessation to the time of removal of the external fixator) by the total length of the regenerate in cm. We estimated the intraclass correlation coefficient (ICC) values and corresponding 95% confidence intervals (CIs) for the interobserver reliability of all radiographic parameters. The estimated ICC values for interobserver reliabilities of the PVR and the amount of lengthening were 0.85 (95% CI, 0.68-0.94) and 0.94 (95% CI, 0.89-0.98), respectively.
Fig. 1. Free line range of interest drawn at each segment. The value M (encircled in white) indicates the mean pixel value for that segment, and it was used in the computation of the pixel value ratio.
Clinical results and complications
All patients were examined for any signs of pin tract infection, ROM of adjoining joints, angulation or translation of the osteotomy site, and other complications that could occur during lengthening. The complications were recorded according to the classification of Paley (problems, obstacles, sequelae).7 Subsequent treatment and any secondary operations were also documented.
Statistical analysis
Differences in the LI, EFI, HI, and PVR were assessed using a linear mixed-effect model analysis. Statistical differences in callus features were analyzed using a repeated-measures analysis of variance. The data were recorded using Microsoft® Exce® 2010 version (Microsoft Corp, Redmond, WA, USA) and analyzed using SPSS® software (SPSS Inc., Chicago, IL, USA). A p-value <0.05 was considered significant.
RESULTS
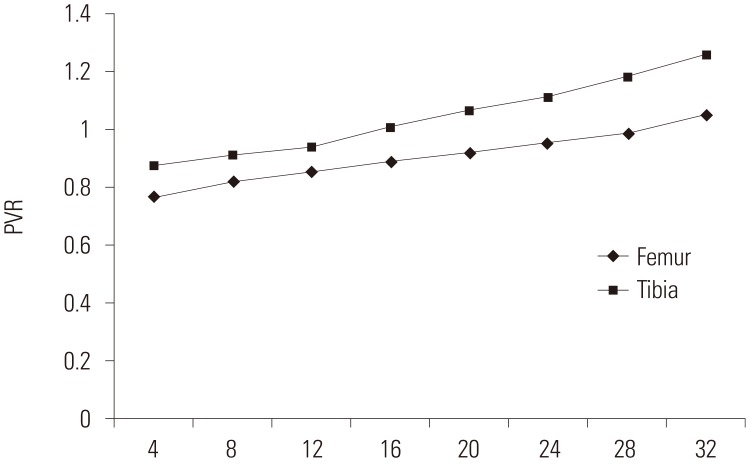
All procedures achieved the planned lengthening. The average gain in length was 9.8 cm (95% CI, 9.2-10.5) in the tibia and 8.4 cm (95% CI, 7.8-9.0) in the femur. The mean values of the LI, EFI, HI, and PVR of the tibia were significantly better than those of the femur (Table 1). The PVR at the regenerate of each bone increased during the distraction period, and a PVR of 1.0 at the regenerate was first achieved in the tibia. The mean PVR in the tibia was significantly higher than that in the femur during the entire distraction period (Fig. 2). In the 56 lengthened tibial segments, there were 54 homogeneous, two lucent, and no heterogenous pathways during the consolidation period, whereas in the 56 femoral segments, there were 37 homogenous, seven lucent, and 12 heterogenous pathways. In the tibia, there were 46 cylindrical, ten fusiform, and no concave shapes, whereas in the femur there were 36 cylindrical, 12 fusiform, five concave, one central, and two lateral shapes. Homogeneous and cylindrical shapes were more prominent in the tibia than in the femur (p<0.05).
Table 1. Summary of Patient Parameters after Lengthening (Mean Value and 95% CI).
| Parameter | Tibia | Femur | p value |
|---|---|---|---|
| Mean lengthening (cm)* | 9.8 (95% CI, 9.2-10.5) | 8.4 (95% CI, 7.8-9.0) | 0.02 |
| Mean lengthening percentage (%)* | 54.7 (95% CI, 50.5-58.8) | 37 (95% CI, 34.0-39.9) | < 0.001 |
| Mean lengthening index (days/cm)* | 12.1 (95% CI, 11.1-13.2) | 15.3 (95% CI, 13.8-16.7) | 0.01 |
| Mean external fixator index (days/cm)* | 23.0 (95% CI, 21.0-24.9) | 42.5 (95% CI, 38.9-46.0) | < 0.001 |
| Mean healing index (days/cm)* | 10.7 (95% CI, 8.8-12.6) | 28.1 (95% CI, 24.1-32.1) | < 0.001 |
| Mean pixel value ratio at 28 wks* | 1.19 (95% CI, 1.14-1.24) | 0.99 (95% CI, 0.97-1.01) | 0.001 |
CI, confidence interval.
*p<0.05.
Fig. 2. Serial graph of the pixel value ratio measurements for the tibia and femur during the lengthening period. PVR, pixel value ratio.
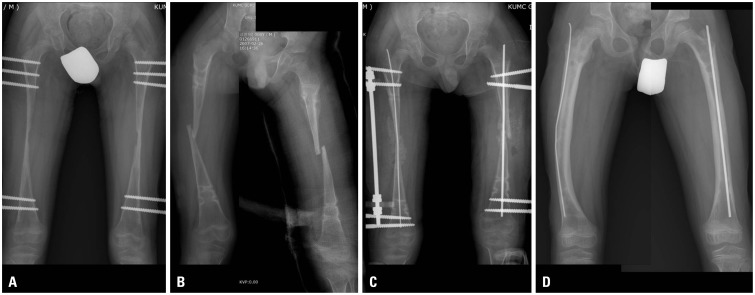
A total of 61 complications were encountered in the 64 segments (23 during tibial lengthening and 38 during femoral lengthening) (Table 2 and 3). In tibial lengthening, there were 17 segments (30.4%) with joint complications and four segments (7.1%) with bony complications. Most problems in the tibial segments were due to the development of equinus deformities during lengthening (17 segments, 30.4%); however, these were all successfully managed by intramuscular gastrocnemius-soleus recession and the application of an Ilizarov foot frame for gradual correction. Relatively more complications occurred during femoral lengthening. Joint complications occurred in 18 segments (32.1%), and bony complications occurred in 18 segments (32.1%). A flexion contracture >30° with or without adductor tightness, which occurred in 16 (28.5%) patients, was the most frequent joint complication. Refracture was the most common bony complication during femoral lengthening (15 instances, 26.8%), followed by varus angular deformity (three instances, 5.4%). All of these complications were managed operatively (Fig. 3).
Table 2. Treatment for Complications after Tibial Lengthening.
| No. of cases | Complications | Treatment |
|---|---|---|
| 17 | Equinus deformity | Intramuscular gastrocnemius-soleus recession and application of the Ilizarov foot frame for gradual correction |
| 2 | Genu valgum | Acute correction and insertion of additional half pins |
| 2 | Superficial pin-track infection | Oral antibiotics and local wound care |
| 1 | Distal migration of proximal fibular segment | Repeat distal fibular osteotomy and half-pin insertion |
| 1 | Refracture after external fixator removal | Medial closing wedge osteotomy, flexible IM rod insertion and supplemental K-wire fixation |
IM, intramedullary.
Table 3. Treatment for Complications after Femoral Lengthening.
| No. of cases | Complications | Treatment |
|---|---|---|
| 16 | Hip flexion contracture | Intramuscular recession of the rectus femoris, sartorius, and iliopsoas muscles with or without adductor longus release |
| 15 | Refracture after external fixator removal | External fixator reapplication with flexible intramedullary nailing with or without bone grafting (n=12) Plate fixation with or without bone grafting (n=3) |
| 3 | Varus angular deformity | Repeat osteotomy for acute correction |
| 2 | Knee stiffness | Quadricepsplasty |
| 1 | Deep surgical-site infection | Formal debridement in the operating room |
| 1 | Superficial pin-track infection | Oral antibiotics and local wound care |
Fig. 3. Radiographs of a 7-year-old male who underwent bilateral femoral lengthening. (A) Prior to external fixator removal (note the lateral shape of the callus), (B) bilateral femoral re-fracture after fixator removal, (C) treated with bilateral Ilizarov external fixator application with Nancy nail supplementation and autologous iliac bone grafting, and (D) at the last follow-up (17 months after surgery), showing complete union and consolidation.
DISCUSSION
Limb lengthening surgeries have widely been used for patients with achondroplasia, which is known as the most common form of disproportionate dwarfism. However, limb lengthening is a complex procedure that has a high complication rate; hence, the limb must be lengthened safely without causing deterioration in function.14 In this study, we proposed 1) to compare the radiological outcomes of femoral and tibial lengthening in patients with achondroplasia and 2) to investigate the differences of complications related with lengthening.
Our study had several limitations. First, the number of patients studied was relatively small and only represented the patients who underwent the lengthening procedures. However, achondroplasia is uncommon, as previously mentioned;1,2,3,4 hence, the number of patients was relatively large enough to investigate the effects of bilateral tibial and subsequent femoral lengthening. Second, the rate of distraction varied according to the morphology of the callus, and this may have had an effect on the PVR. However, we feel that this may not be significant, as it was validated in the senior author's previous study.15,16 Third, the order of lengthening might have influenced the radiographic and clinical results. Most of our patients showed severe genu varum deformities and ankle varus deformities at the time of the initial visit. Therefore, we always corrected those deformities first, and lengthened the tibia simultaneously. Moreover, the anatomical axis of the tibia segment should be aligned along the mechanical axis of the lower extremity; therefore, correction and lengthening of the tibial segment first and then lengthening of femoral segment could be a practically reasonable option for this particular patient group. Fourth, the different types of external devices that were used in the two groups might have influenced the radiographic and clinical results. Ilizarov believed that the biomechanical environment provided by a fine-wire circular frame combined with a corticotomy produced the most favorable conditions for distraction osteogenesis,17 providing significantly better results for tibial lengthening. Moreover, the distance between bone and external fixators is shorter in the tibia, thus increasing stability and decreasing the risk of axial deviations.
The ability of the Ilizarov technique to lengthen both lower limbs in patients with achondroplasia and other causes of short stature has been confirmed in several studies;8,9,10 however, our reason for using the monolateral fixator for the femur instead of the Ilizarov ring fixator was that the former provides greater comfort for patients without compromising stability.2 Lastly, we did not consider the preoperative and postoperative QOL assessment or correlate the findings with the complications that developed during lengthening. Hence, such an evaluation is recommended, as Kim, et al.18 mentioned that even with numerous complications, serial lower-limb lengthening is a good option for patients with achondroplasia, resulting in good QOL scores.
We found that the regenerate zone of the tibia had a significantly higher mean PVR than that of the femur, and all other parameters including the LI, EFI, and HI showed significantly higher values for tibial lengthening (Table 1), as callus formation in the tibia during distraction proceeds at a higher rate than that in the femur. Considering that the PVR method has been validated as an objective evaluation of mineralization in the lengthening zone,12,15,19 we were able to determine the rate of callus formation by measuring the serial PVR until 32 weeks instead of a single estimate of bone-mineral apparent density (Fig. 2). The difference in the rate of callus formation is likely associated with the complications of femoral lengthening, such as refracture, callus subsidence, and angulation of the osteotomy site during weight-bearing.
In our series, there were more instances of cylindrical shapes and homogeneous pathways in the tibia than in the femur during lengthening. These findings might be related to the significantly lower mean LI, EFI, and HI during tibial lengthening than during femoral lengthening. In our study, both the tibial and femoral EFIs appeared to be comparable to the values reported in the literature for lengthening in healthy bone.7,20,21 Previously, Singh, et al.13 reported that homogeneous pathways exhibited the most favorable outcomes during lengthening. Additionally, the callus pattern is known to be associated with a larger HI.22 We removed the external fixators only when a PVR of at least 1.0 was achieved, as we could safely rely on this variable to define the timing of fixator removal, given that it correlates well in patients with a cylindrical callus pattern regardless of whether the pathway is homogeneous or heterogeneous.16,23,24
The risk of complications from lengthening increases with length.25 Moreover, the regenerate bone is 40-60% weaker than normal bone from 6 weeks to 6 months, and normal strength is not regained until 2 years later.26 In the lower limbs, the number of complications appears to increase when the extent of lengthening exceeds 20%.25 In our study, we were able to lengthen the tibia and femur by 9.8 cm (54.7%) and 8.4 cm (37.0%), respectively. Paley7 mentioned that lengthening is limited by the soft tissues; hence, lengthening to 5-8 cm carries medium risk, and exceeding 8 cm carries high risk. However, we were able to perform extensive lengthening, as bone healing is known to be good in achondroplastic and hypochondroplastic patients.27 These patients tolerate lengthening well due to ligament and soft-tissue laxity, and their muscle length exceeds their bone length before lengthening.28
We encountered many complications related to lengthening, and those difficulties were subclassified into categories defined by Paley7 as problems, obstacles, and complications. In this series, superficial pin-tract infection was the only problem identified in both tibial (two cases) and femoral (one case) lengthening. It required no operative intervention to resolve. Three obstacles in the series were encountered that required operative intervention to resolve. These included equinus deformity (n=17), genu valgum deformity (n=2), and premature fibular consolidation (n=1) in the tibia. Hip flexion contracture (n=16), knee flexion contracture (n=2), and deep surgical-site infection (n=1) were the obstacles encountered in femoral lengthening. A total of 21 (18.8%) true complications were recognized, 16 of which were refractures at the osteotomy sites (one tibial and 15 femoral refractures), and the three remaining complications were varus angular deformities in the femur. Fewer complications were found during the lengthening of the tibia than during the lengthening of the femur.
Muscle contractures are common in limb lengthening;7 particularly equinus deformity is known to develop at a high rate during tibial lengthening,29 and hip-and-knee flexion contracture is common in femoral lengthening.2,14 Although the exact etiology of equinus deformity remains unknown,29 it has been hypothesized that the shortened soleus-gastrocnemius-Achilles tendon complex is the cause of this deformity.30 Hip-and-knee joint contracture is common particularly during the lengthening of a congenitally short femur and has been associated with the tremendous forces exerted across the joints, which can result in hip or knee instability.5
In our study, there was one incidence of distal fibular migration due to premature fibular consolidation, which may be an indication of a high rate of bone formation during the lengthening process.31 Refracture, callus subsidence, and angulation of the osteotomy site during weight-bearing are known complications of femoral lengthening7,14 as manifested by bony complications in this series. Despite these problems, obstacles, and complications, the original goals of surgery were achieved in all treated segments, and our true complication rate was lower than the rates of previous studies, which ranged from 46% to 72%.7,32,33
In addition, we believe that refractures and angulation deformities are more frequent in femoral lengthening than in tibial lengthening, as patella tendon bearing casts were applied after tibial fixator removal. Hence, tibial protection was added for 6 more weeks prior to full weight-bearing, whereas initially, weight-bearing with crutches was immediately started after femoral fixator removal. We suggest that the risk of refracture can be minimized by careful analysis of the regenerate during the consolidation period. It has been previously recommended to temporary cease distraction and apply gradual compression when concave, lateral, or central callus shapes appear in the regenerate bone until satisfactory regenerate with fusiform or cylindrical callus develops.14
In conclusion, tibial lengthening may be a more reliable procedure with a relatively lower complication rate compared with the findings for the femur. Callus formation in the tibia during the distraction period proceeds at a significantly higher rate than that in the femur. Our study suggests that bilateral limb lengthening of the tibia followed by femoral lengthening might be a reasonable option for patients with achondroplasia, provided that the patients are carefully monitored for complications and that these complications are promptly addressed whenever they occur.
ACKNOWLEDGEMENTS
We thank our clinical and research interns, Ms. Huo Da (Singapore), Ms. Jiashu Li (China), and Mr. Jun-ho Song (Korea) for their assistance with data collection and technical support.
The institution of one of the authors (HRS) received funding from the Korea Healthcare Technology R & D Project, Ministry of Health & Welfare, Republic of Korea (HI11C0388).
This study was also supported by a grant from the Korean Health Technology R&D Project, Ministry of Health & Welfare, Republic of Korea (HI13C1501).
Footnotes
The authors have no financial conflicts of interest.
References
- 1.Takken T, van Bergen MW, Sakkers RJ, Helders PJ, Engelbert RH. Cardiopulmonary exercise capacity, muscle strength, and physical activity in children and adolescents with achondroplasia. J Pediatr. 2007;150:26–30. doi: 10.1016/j.jpeds.2006.10.058. [DOI] [PubMed] [Google Scholar]
- 2.Paley D, Chaudray M, Pirone AM, Lentz P, Kautz D. Treatment of malunions and mal-nonunions of the femur and tibia by detailed preoperative planning and the Ilizarov techniques. Orthop Clin North Am. 1990;21:667–691. [PubMed] [Google Scholar]
- 3.Tandon A, Bhargava SK, Goel S, Bhatt S. Pseudoachondroplasia: a rare cause of rhizomelic dwarfism. Indian J Orthop. 2008;42:477–479. doi: 10.4103/0019-5413.43400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cattaneo R, Villa A, Catagni M, Tentori L. Limb lengthening in achondroplasia by Ilizarov's method. Int Orthop. 1988;12:173–179. doi: 10.1007/BF00547160. [DOI] [PubMed] [Google Scholar]
- 5.Coleman SS. Simultaneous femoral and tibial lengthening for limb length discrepancies. Arch Orthop Trauma Surg. 1985;103:359–366. doi: 10.1007/BF00435441. [DOI] [PubMed] [Google Scholar]
- 6.Tesiorowski M, Zarzycka M, Kacki W, Jasiewicz B. [Bilateral simultaneous limb lengthening of patients with short stature using the Ilizarov method] Chir Narzadow Ruchu Ortop Pol. 2002;67:421–426. [PubMed] [Google Scholar]
- 7.Paley D. Problems, obstacles, and complications of limb lengthening by the Ilizarov technique. Clin Orthop Relat Res. 1990:81–104. [PubMed] [Google Scholar]
- 8.Trivella G, Aldegheri R. Surgical correction of short stature. Acta Paediatr Scand Suppl. 1988;347:141–146. [PubMed] [Google Scholar]
- 9.De Bastiani G, Aldegheri R, Trivella G, Renzi-Brivio L, Agostini S, Lavini F. Lengthening of the lower limbs in achondroplastics. Basic Life Sci. 1988;48:353–355. doi: 10.1007/978-1-4684-8712-1_46. [DOI] [PubMed] [Google Scholar]
- 10.Peretti G, Memeo A, Paronzini A, Marzorati S. Staged lengthening in the prevention of dwarfism in achondroplastic children: a preliminary report. J Pediatr Orthop B. 1995;4:58–64. doi: 10.1097/01202412-199504010-00009. [DOI] [PubMed] [Google Scholar]
- 11.Li R, Saleh M, Yang L, Coulton L. Radiographic classification of osteogenesis during bone distraction. J Orthop Res. 2006;24:339–347. doi: 10.1002/jor.20026. [DOI] [PubMed] [Google Scholar]
- 12.Zhao L, Fan Q, Venkatesh KP, Park MS, Song HR. Objective guidelines for removing an external fixator after tibial lengthening using pixel value ratio: a pilot study. Clin Orthop Relat Res. 2009;467:3321–3326. doi: 10.1007/s11999-009-1011-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Singh S, Song HR, Venkatesh KP, Modi HN, Park MS, Jang KM, et al. Analysis of callus pattern of tibia lengthening in achondroplasia and a novel method of regeneration assessment using pixel values. Skeletal Radiol. 2010;39:261–266. doi: 10.1007/s00256-009-0703-0. [DOI] [PubMed] [Google Scholar]
- 14.Young JW, Kovelman H, Resnik CS, Paley D. Radiologic assessment of bones after Ilizarov procedures. Radiology. 1990;177:89–93. doi: 10.1148/radiology.177.1.2399344. [DOI] [PubMed] [Google Scholar]
- 15.Babatunde OM, Fragomen AT, Rozbruch SR. Noninvasive quantitative assessment of bone healing after distraction osteogenesis. HSS J. 2010;6:71–78. doi: 10.1007/s11420-009-9130-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hazra S, Song HR, Biswal S, Lee SH, Lee SH, Jang KM, et al. Quantitative assessment of mineralization in distraction osteogenesis. Skeletal Radiol. 2008;37:843–847. doi: 10.1007/s00256-008-0495-7. [DOI] [PubMed] [Google Scholar]
- 17.Ilizarov GA. The tension-stress effect on the genesis and growth of tissues: Part II. The influence of the rate and frequency of distraction. Clin Orthop Relat Res. 1989:263–285. [PubMed] [Google Scholar]
- 18.Kim SJ, Balce GC, Agashe MV, Song SH, Song HR. Is bilateral lower limb lengthening appropriate for achondroplasia?: midterm analysis of the complications and quality of life. Clin Orthop Relat Res. 2012;470:616–621. doi: 10.1007/s11999-011-1983-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shim JS, Chung KH, Ahn JM. Value of measuring bone density serial changes on a picture archiving and communication systems (PACS) monitor in distraction osteogenesis. Orthopedics. 2002;25:1269–1272. doi: 10.3928/0147-7447-20021101-19. [DOI] [PubMed] [Google Scholar]
- 20.Monticelli G, Spinelli R. Leg lengthening by closed metaphyseal corticotomy. Ital J Orthop Traumatol. 1983;9:139–150. [PubMed] [Google Scholar]
- 21.Donnan LT, Saleh M, Rigby AS. Acute correction of lower limb deformity and simultaneous lengthening with a monolateral fixator. J Bone Joint Surg Br. 2003;85:254–260. doi: 10.1302/0301-620x.85b2.12645. [DOI] [PubMed] [Google Scholar]
- 22.Catagni M. Imaging techniques: the radiographic classification of bone regenerate during distraction. London: Williams and Wilkins; 1991. [Google Scholar]
- 23.Shyam AK, Singh SU, Modi HN, Song HR, Lee SH, An H. Leg lengthening by distraction osteogenesis using the Ilizarov apparatus: a novel concept of tibia callus subsidence and its influencing factors. Int Orthop. 2009;33:1753–1759. doi: 10.1007/s00264-008-0660-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Song SH, Sinha S, Kim TY, Park YE, Kim SJ, Song HR. Analysis of corticalization using the pixel value ratio for fixator removal in tibial lengthening. J Orthop Sci. 2011;16:177–183. doi: 10.1007/s00776-011-0036-4. [DOI] [PubMed] [Google Scholar]
- 25.Yun AG, Severino R, Reinker K. Attempted limb lengthenings beyond twenty percent of the initial bone length: results and complications. J Pediatr Orthop. 2000;20:151–159. [PubMed] [Google Scholar]
- 26.Al Turk M HF, Dwiri M. Limb Salvage Procedure in Malignant Bone Tumors using Resection-Shortening-Distraction Technique. A Report of Two Cases. Jordan Royal Med Serve J. 2004;11:52–55. [Google Scholar]
- 27.Yasui N, Kawabata H, Kojimoto H, Ohno H, Matsuda S, Araki N, et al. Lengthening of the lower limbs in patients with achondroplasia and hypochondroplasia. Clin Orthop Relat Res. 1997:298–306. [PubMed] [Google Scholar]
- 28.Paley D. Current techniques of limb lengthening. J Pediatr Orthop. 1988;8:73–92. doi: 10.1097/01241398-198801000-00018. [DOI] [PubMed] [Google Scholar]
- 29.Yoshino A, Takao M, Innami K, Matsushita T. Equinus deformity during tibial lengthening with ankle orthoses for equalization of leg-length discrepancies. J Orthop Sci. 2011;16:756–759. doi: 10.1007/s00776-011-0139-y. [DOI] [PubMed] [Google Scholar]
- 30.Lehman WB, Grant AD, Atar D. Preventing and overcoming equinus contractures during lengthening of the tibia. Orthop Clin North Am. 1991;22:633–641. [PubMed] [Google Scholar]
- 31.Cattaneo R, Catagni MA, Guerreschi F. Applications of the Ilizarov method in the humerus. Lengthenings and nonunions. Hand Clin. 1993;9:729–739. [PubMed] [Google Scholar]
- 32.Guidera KJ, Hess WF, Highhouse KP, Ogden JA. Extremity lengthening: results and complications with the Orthofix system. J Pediatr Orthop. 1991;11:90–94. [PubMed] [Google Scholar]
- 33.Dahl MT, Gulli B, Berg T. Complications of limb lengthening. A learning curve. Clin Orthop Relat Res. 1994:10–18. [PubMed] [Google Scholar]