Abstract
Purpose
To investigate sociodemographic factors, health behaviors, and comorbidities associated with cataracts in a large, nationally representative Korean sample.
Materials and Methods
This cross-sectional study included 715554 adults aged 40 years or older who participated in the 2008-2012 Community Health Survey. Significant risk factors were identified using multivariate logistic regression analysis for self-reported cataract, and a nomogram for analysis of cataract risk was generated.
Results
Roughly 11% of participants (n=88464) reported being diagnosed with cataracts by a doctor. Age was the most important independent risk factor [adjusted odds ratio (aOR)=1.11, 99% confidence interval (CI), 1.11-1.11 for each increasing year]. Significant comorbidities with descending order of effect size (aOR, 99% CI), included diabetes mellitus (1.78, 1.71-1.85), osteoporosis (1.62, 1.56-1.69), arthritis (1.54, 1.48-1.59), hepatitis B infection (1.46, 1.31-1.63), atopic dermatitis (1.50, 1.33-1.69), angina (1.46, 1.35-1.57), allergic rhinitis (1.45, 1.36-1.55), dyslipidemia (1.38, 1.31-1.45), asthma (1.35, 1.26-1.44), and hypertension (1.23, 1.19-1.28). Subjects who sleep less than 6 hours/day were more likely to have cataract than subjects who sleep more than 9 hours/day as a reference group (aOR=1.22, 99% CI, 1.11-1.34).
Conclusion
While the most important cataract risk factor was age, the ten comorbidities mentioned above were also significant risk factors. Interestingly, longer duration of sleep was associated with a protective effect against cataract development.
Keywords: Cataract, a community health survey, risk factor, nomogram
INTRODUCTION
Age-related cataracts are the leading cause of blindness worldwide, including America and Asia.1,2,3,4,5,6,7 Identifying risk factors associated with cataract development will facilitate the identification of new prevention and treatment options. Previous studies have evaluated risk factors associated with cataract, including sociodemographic factors and comorbidities.3,6,8,9,10,11,12,13 These findings offer insight into the pathophysiology of this multifactorial disease.
In this study, we investigated the association between cataracts and sociodemographic factors, behavioral risk factors, and comorbidities in 715554 adults, aged 40 years and older, who participated in the Community Health Survey (CHS) 2008-2012. This is a nationally representative survey conducted by the Korea Centers for Disease Control and Prevention (KCDCP) that provides data on cataract diagnosis, health status, and sociodemographic factors.
MATERIALS AND METHODS
Statement of ethics
The study adhered to the tenets of the Declaration of Helsinki. The survey was reviewed and approved by the Institutional Review Board of the KCDCP, and all participants provided written informed consent. The study was approved by the Institutional Review Board of the Yonsei University College of Medicine, Seoul, Korea.
Design and study population
The CHS was administered to roughly 900 subjects from 253 community health centers throughout South Korea; participants were selected among adults, aged 19 years or older, who resided in the catchment area of each South Korean community health center. A stratified multistage probability sampling design was employed, and each participant was surveyed only once. This survey was performed for 3 months of every year, from 2008-2012. One-on-one, protocol-based interviews were conducted by trained interviewers. Questionnaires included 253 questions in 11 fields, covering sociodemographic factors, behavioral factors, comorbidities, and quality of life. In order to ensure high quality survey data, the Ministry of Health and Welfare selected another agency to re-administer the survey to 10% of subjects via telephone. If the results were not consistent, the interviewer involved was re-trained by KCDCP. The survey was administered to 220258 individuals in 2008; 230715 in 2009; 229229 in 2010; 229226 in 2011; and 228921 in 2012. The response rate was not available, because the subjects who did not participate were not included in this survey. Overall, the study included 715554 participants who completed the questionnaires about cataracts and potential risk factors.
Presence of self-reported cataract
Subjects were asked "Have you ever had a cataract before?" to ensure accurate self-reporting. They were also asked "Has a doctor ever diagnosed you with a cataract before (either eye)?"
Independent variables: potential risk factors
Sociodemographic variables included: current age, gender, residential area (rural/urban), monthly household income (lowest quintile/2nd-4th quintiles/highest quintile), highest educational level attained (elementary school graduate or lower/middle school graduate/high school graduate/university graduate or higher), Medicaid recipient, spouse, and occupation (administrator, management, professional occupations/business and financial operation occupations/sales and related occupations/farming, fishing and forestry occupations/installation, maintenance, and repair occupations or laborer/housewife/others, including unemployed).
Health status variables included hypertension, diabetes mellitus (DM; yes/no), dyslipidemia, cerebrovascular accident, myocardial infarction, angina, arthritis, osteoporosis, asthma, allergic rhinitis, atopic dermatitis, and hepatitis B infection. Health behavior variables included being a lifetime smoker, being a lifetime alcohol user, physical activity of moderate intensity (more than three times a week/no regular exercise), salt intake (low/normal/high), sleep duration (<6 hours/6-9 hours/>9 hours), and body mass index (BMI; quintile). Supplementary Table 1 (only online) lists detailed definitions of the independent variables. To assess co-morbidities, subjects were asked the question "Have you ever been diagnosed with [disease] by a doctor before?" with possible responses of "yes" or "no." The trained interviewer emphasized "by a doctor" to ensure more accurate results.
Statistical analysis
Basic characteristics of the study population were reported. We determined the age-standardized prevalence of cataracts in Korea using the weighting system recommended by the KCDCP. Statistical analyses were conducted using the Stata/SE version 13 (StataCorp, College Station, TX, USA) and survey procedures were used in all analyses to account for the stratified sampling design of CHS; this procedure is adjusted for oversampling, missing responses, and age structure of the Korean population.
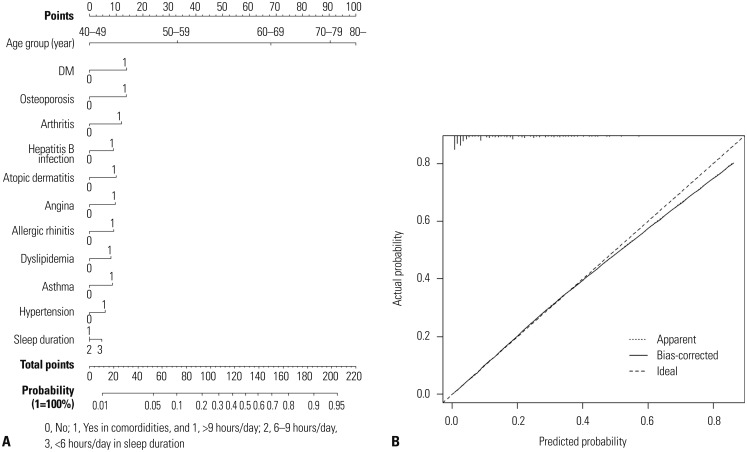
A two-step approach was used to identify cataract risk factors. First, we constructed multivariate logistic regression models to identify cataract risk factors using all variables, including sociodemographic factors, comorbidities, and health behavior. In order to compare the effect size [adjusted odds ratio (aOR)], we defined the group with the smallest values of effect size as a reference group. Second, a final model was constructed to include the ten most important variables in regards to comorbidities, based on aOR values (aOR, 1.24-1.87); the most important variable, sleep duration, in regards to health behavior (aOR=1.33); and age, according to 5-year intervals. Other variables related to health behavior had an aOR of less than1.10, and were not included in the final model due to small effect size, compared to comorbidities. A nomogram was constructed using the final model. We used receiver operating characteristics derived area under the curve to quantify the predictive accuracy of our model. We graphically investigated the performance characteristics of the nomogram using calibration plots. Models were internally validated via bootstrapping with 200 replicates. Nomograms were created using R software for Windows version 3.1.0 (R Foundation for Statistical Computing, Nashville, TN, USA). All statistical tests were performed in Stata/SE version 13. Because this study had such a large sample size, there was the potential to obtain results that were statistically significant according to their p-values but do not have practical significance. For this reason, a relatively strict cut-off of a two-sided p-value<0.01 was considered statistically significant.14
RESULTS
Characteristics of the study population and prevalence of cataract
Of the 715554 adults over age forty, 11.3% (88464) reported being diagnosed with cataract by a doctor. Within the sample, 45.7% of participants were male, 50.0% lived in an urban area, 5.7% were Medicaid recipients, and 22.0% lived without a spouse. Supplementary Table 1 (only online) lists detailed characteristics of the study population. Supplementary Table 2 (only online) provides the age-standardized prevalence of cataract for the years 2008-2012, based on questionnaire answers. The overall age-standardized prevalence in 2008-2011 was 9.1%. This prevalence increased from 2008 to 2011 and remained similar between 2011 and 2012; the prevalences of cataract in subjects aged 40 years and older were 6.9% in 2008, 8.1% in 2009, 8.7% in 2010, 10.2% in 2011, and 10.0% in 2012.
Factors associated with cataract
Table 1 presents the factors associated with cataract in multivariate logistic regression models using all variables, including sociodemographic factors, comorbidities, and health behavioral factors. All variables except gender, presence of a spouse, having experienced a cerebrovascular accident, and physical activity displayed statistically significant associations with cataract (p<0.01). Increasing monthly household income was associated with a lower prevalence of cataract. Subjects who had graduated from high school (as a reference group) were less likely to have cataracts than those who had graduated from a higher or lower level of education. Subjects living in urban areas were more likely to have cataracts than those living in rural areas. Subjects who received Medicaid were more likely to have cataracts than those who did not, with a relatively large aOR [=1.22, 99% confidence interval (CI) 1.13-1.32; 2nd order of effect size in sociodemographic factors]. Housewives were more likely to have cataracts than participants who worked in sales and related occupations as a reference group, with the largest aOR value among all sociodemographic factors (aOR=1.32, 99% CI 1.21-1.43).
Table 1. Factors Associated with Cataract-Univariate and Multivariate Logistic Regression Analysis (n=715554).
| Unadjusted OR | Adjusted OR (99% CI) | ||
|---|---|---|---|
| Age | |||
| One yr increase | 1.12 | 1.11 (1.11-1.12) | |
| Sex | |||
| Male | 1.0 (ref) | 1.0 (ref) | |
| Female | 1.63 | 1.04 (0.97-1.12) | |
| Monthly household income (≒USD) | |||
| Lowest quintile (<500) | 5.97 | 1.12 (1.05-1.20) | |
| 2nd-4th quintile (500-2000) | 1.99 | 1.09 (1.03-1.15) | |
| Highest quintile (>2000) | 1.0 (ref) | 1.0 (ref) | |
| Education | |||
| Elementary school | 4.93 | 1.16 (1.10-1.23) | |
| Middle school | 2.08 | 1.09 (1.02-1.15) | |
| High school | 1.0 (ref) | 1.0 (ref) | |
| University or higher | 0.92 | 1.14 (1.06-1.22) | |
| Residential area | |||
| Rural | 1.0 (ref) | 1.0 (ref) | |
| Urban | 0.70 | 1.11 (1.06-1.16) | |
| Medicaid recipient | |||
| No | 1.0 (ref) | 1.0 (ref) | |
| Yes | 2.56 | 1.22 (1.13-1.32) | |
| Spouse | |||
| Lives with spouse | 1.0 (ref) | 1.0 (ref) | |
| Lives without spouse | 3.01 | 1.03 (0.99-1.08) | |
| Occupation | |||
| Administrative, management, or professional occupations | 0.89 | 1.09 (0.96-1.22) | |
| Business and financial operations occupations | 0.56 | 1.00 (0.85-1.18) | |
| Sales and related occupations | 1.0 (ref) | 1.0 (ref) | |
| Farming, fishing, and forestry occupations | 4.19 | 1.13 (1.03-1.23) | |
| Installation, maintenance, and repair occupations/laborers | 1.39 | 1.06 (0.97-1.16) | |
| Housewives | 4.74 | 1.32 (1.21-1.43) | |
| Other, including unemployed | 8.52 | 1.19 (1.09-1.29) | |
| Comorbidities: "No" as a reference group (ordered by effect size) | |||
| Diabetes mellitus (1st) | Yes | 3.48 | 1.87 (1.78-1.96) |
| Osteoporosis (2nd) | Yes | 5.15 | 1.62 (1.54-1.71) |
| Arthritis (3rd) | Yes | 4.63 | 1.53 (1.46-1.60) |
| Hepatitis B infection (4th) | Yes | 1.06 | 1.49 (1.33-1.67) |
| Atopic dermatitis (5th) | Yes | 1.64 | 1.47 (1.29-1.68) |
| Angina (6th) | Yes | 4.03 | 1.42 (1.30-1.55) |
| Allergic rhinitis (7th) | Yes | 0.91 | 1.42 (1.32-1.52) |
| Dyslipidemia (8th) | Yes | 1.89 | 1.41 (1.33-1.49) |
| Asthma (9th) | Yes | 3.24 | 1.31 (1.20-1.42) |
| Hypertension (10th) | Yes | 3.26 | 1.24 (1.19-1.29) |
| Myocardial infarction | Yes | 3.58 | 1.20 (1.09-1.32) |
| Cerebrovascular accident | Yes | 3.47 | 1.06 (0.97-1.16) |
| Health behavior | |||
| Lifetime smoker | |||
| No | 1.0 (ref) | 1.0 (ref) | |
| Yes | 0.74 | 1.10 (1.04-1.16) | |
| Lifetime alcohol user | |||
| No | 1.0 (ref) | 1.0 (ref) | |
| Yes | 0.47 | 1.06 (1.02-1.11) | |
| Physical activity | |||
| No regular physical activity | 1.0 (ref) | 1.0 (ref) | |
| Regular physical activity | 0.74 | 1.04 (0.99-1.10) | |
| Salt consumption | |||
| High | 1.40 | 1.09 (1.05-1.14) | |
| Normal | 1.0 (ref) | 1.0 (ref) | |
| Low | 1.26 | 1.08 (1.03-1.13) | |
| Sleep duration | |||
| >9 hrs/day | 1.0 (ref) | 1.0 (ref) | |
| 6-9 hrs/day | 0.43 | 1.14 (1.01-1.28) | |
| <6 hrs/day | 0.79 | 1.33 (1.17-1.50) | |
| Obesity (BMI, kg2/m2) | |||
| 1st quintile (<20.20) | 1.73 | 1.00 (0.94-1.06) | |
| 2nd quintile (20.20-21.93) | 1.06 | 1.01 (0.95-1.07) | |
| 3rd quintile (21.93-23.39) | 1.0 (ref) | 1.0 (ref) | |
| 4th quintile (23.39-25.16) | 1.11 | 1.07 (1.01-1.14) | |
| 5th quintile (>25.16) | 1.12 | 0.99 (0.94-1.05) | |
OR, odds ratio; CI, confidence interval; BMI, body mass index.
In terms of comorbidities with descending order by effect size (aOR, 99% CI), adults with DM (1.87, 1.78-1.96), osteoporosis (1.62, 1.54-1.71), arthritis (1.53, 1.46-1.60), hepatitis B infection (1.49, 1.33-1.67), atopic dermatitis (1.47, 1.29-1.68), angina (1.42, 1.30-1.55), allergic rhinitis (1.42, 1.32-1.52), dyslipidemia (1.41, 1.33-1.49), asthma (1.31, 1.20-1.42), and hypertension (1.24, 1.19-1.29) were relatively more likely to have cataract than those who were unaffected. The aOR of myocardial infarction was relatively small (aOR=1.20), compared to the ten comorbidities above, and cerebrovascular accidents were not statistically significant, even though this was a large-scale study.
In terms of health behaviors, aOR were relatively small compared to the above comorbidities except sleep duration. Subjects who slept less than 6 hours/day (aOR=1.33, 99% CI 1.17-1.50) were more likely to have cataracts than those who slept more than 9 hours/day as a reference group.
Table 2 summarizes the final model including the ten most important comorbidities, sleep duration, which had the largest effect size, and age. If subjects were aged 80 years or older, the risk increased about 90-fold, compared to subjects aged between 40 and 44 years as a reference group. Other variables including ten comorbidities and sleep duration were still important with the range of aOR between 1.22 (sleep duration, minimum) and 1.78 (DM, maximum).
Table 2. Factors Associated with Cataract, Final Model-Multivariate Logistic Analysis (n=715554).
| Adjusted OR | 99% CI | |
|---|---|---|
| Age | ||
| 40-44 | 1.0 (ref) | |
| 45-49 | 2.21 | (1.86-2.64) |
| 50-54 | 4.06 | (3.45-4.78) |
| 55-59 | 7.78 | (6.65-9.10) |
| 60-64 | 16.70 | (14.35-19.43) |
| 65-69 | 31.64 | (27.23-36.76) |
| 70-74 | 50.62 | (43.56-58.82) |
| 75-79 | 71.04 | (61.06-82.67) |
| 80- | 87.70 | (75.26-102.21) |
| Diabetes mellitus | ||
| No | 1.0 (ref) | |
| Yes | 1.78 | (1.71-1.85) |
| Osteoporosis | ||
| No | 1.0 (ref) | |
| Yes | 1.62 | (1.56-1.69) |
| Arthritis | ||
| No | 1.0 (ref) | |
| Yes | 1.54 | (1.48-1.59) |
| B-viral hepatitis | ||
| No | 1.0 (ref) | |
| Yes | 1.46 | (1.31-1.63) |
| Atopic dermatitis | ||
| No | 1.0 (ref) | |
| Yes | 1.50 | (1.33-1.69) |
| Angina | ||
| No | 1.0 (ref) | |
| Yes | 1.46 | (1.35-1.57) |
| Allergic rhinitis | ||
| No | 1.0 (ref) | |
| Yes | 1.45 | (1.36-1.55) |
| Dyslipidemia | ||
| No | 1.0 (ref) | |
| Yes | 1.38 | (1.31-1.45) |
| Asthma | ||
| No | 1.0 (ref) | |
| Yes | 1.35 | (1.26-1.44) |
| Hypertension | ||
| No | 1.0 (ref) | |
| Yes | 1.23 | (1.19-1.28) |
| Sleep duration | ||
| >9 hrs/day | 1.0 (ref) | |
| 6-9 hrs/day | 1.03 | (0.94-1.13) |
| <6 hrs/day | 1.22 | (1.11-1.34) |
OR, odds ratio; CI, confidence interval.
Based on our final model that included the 10 most significant comorbidities, sleep duration, and age group (Table 2), we created a nomogram to predict cataract development (Fig. 1A). The combined predictive accuracy of the full nomogram, which contained information on all variables, was 83.8%, which exceeded the accuracy of any individual predictor. Fig. 1B shows the results of model calibration; the calibration plot shows the performance of the nomogram. A calibration curve can be approximated by a regression line with intercept α and slope β. Well-calibrated models have α=0 and β=1 as representing ideal line in Fig. 1A. X-axis represents nomogram predicted probability of having cataract. Y-axis shows observed probability of having cataract. Ideal line represents the perfect prediction, and bias-corrected line (solid) indicates bootstrap corrected nomogram performance. The rate of predicted cataract closely paralleled the observed rate of cataract and nearly corresponded to the ideal predictions. Finally, they demonstrate that the model is well calibrated.
Fig. 1. (A) A nomogram illustrating the effect of various risk factors on the probability of patient having cataracts. (B) A graph illustrating model calibration.
DISCUSSION
Sociodemographic factors and cataract
Age was the most important independent sociodemographic risk factor for cataract that we identified, with an adjusted OR of 1.11 (99% CI 1.11-1.11) for each additional year of age and an aOR of 1.71 (99% CI 1.70-1.73) for each additional 5-year increase (data not shown). One earlier study, examined the prevalence of cataracts based on diagnosis by slit lamp examination, and found that low monthly household income and low education were independent risk factors.8 We also found similar results, suggesting that these are indeed risk factors. We found that utilization of health centers was lower in the highest household income quintile (25.7%) than in the lowest (64.4%; data not shown); however, because of universal healthcare, economic barriers to medical services in Korea are relatively low. Health center usage rates were 58.6% among Medicaid recipients and 40.9% among non-Medicaid recipients. Also, Medicaid recipients might have more free time to visit their doctor, as they are more likely to be unemployed (42.7% of Medicaid recipients reported a job status of "Other, including unemployed;" data not shown). Thus, accessibility of medical service in Korea may be associated more with "free time" than with "economic status." With regard to occupation, 43.4% of housewives had utilized health centers over the past one year, while only 18.2% of the administrator/management/professional group did (data not shown). Again, more time to visit the doctor may account for the higher odds of housewives' being diagnosed with cataracts. Thus, there is a possibility of higher levels of ascertainment of cataract in both the housewife and Medicaid recipient groups, both of which had relatively high aORs. It is interesting to note that the unadjusted cataract OR for residents of urban areas was 0.70, while the adjusted OR was 1.11. A study on the Beaver Dam Cohort (n=3253) found that the incidence of all types of cataract waslower in rural areas.9 We suggest that a rural setting may provide a healthier environment and a way of living that is closer to nature, which could be protective factors against cataract, however, we cannot establish causality using these cross-sectional data.
We conclude that sociodemographic risk factors for cataract other than age are evident but are minimal, and likely have no meaningful effect. The development of cataracts is part of the aging process, and aging may contribute to the accumulation of damage from environmental sources, and deterioration of defense and repair mechanisms.
Comorbidities and cataract
Based on elevated CIs, independent comorbidity risk factors were identified, they included DM, osteoporosis, arthritis, hepatitis B infection, atopic dermatitis, angina, allergic rhinitis, dyslipidemia, asthma, and hypertension (by descending order of aOR). Previous studies found associations between the presence of cataracts and DM,10,15,16,17 osteoporosis,18 arthritis,11,19 hepatitis B infection,20 atopic dermatitis,21 angina,22 allergic rhinitis (due to nasal spray),23 asthma (due to inhaled steroids),24 dyslipidemia,25 and hypertension.8 Ophthalmic screening of patients with DM appears to be especially important (aOR=1.78, 99% CI 1.72-1.82). We generated a cataract nomogram containing age and comorbidities to increase the practical utility of our findings. Fig. 1 shows that the most important predictive factor is age. The presence of DM, osteoporosis, arthritis, or atopic dermatitis results in an increase of more than 10 points, and the probability of developing cataracts increases by about 10%. If a subject has more than 100 points, their probability of developing cataracts is approximately 25%. In order to obtain nomogram predicted probability, patient values at each axis are located, and a vertical line in drawn to the "Point" axis to determine how many points are attributed for each risk factor value. Sum up the points for all variables and locate the sum on the "Total point" line. Then, the "Total point" represents the individual probability of having cataract. For example, if subjects with 70 years old (point≒90) and have DM (point≒14) and hepatitis B infection (point≒9), total points (90+14+9≒113) indicate about 35% of probability of cataract. Because our results were obtained from questionnaires rather than clinical exams, the utility of our nomogram in clinical practice is limited; nevertheless, our results indicate that a subject with 100 points or more (e.g., someone over 70 years of age with DM) should be screened for cataracts, especially when one considers that only 25.1% of subject aged 40 or older in Korea are aware that they have cataract.26 While our nomogram is not a final model, we introduced this concept to highlight its potential for practical applications. Further refinement, based on ophthalmic and health exams, is needed.
Health behaviors and cataract
All health behavior variables, except physical activity, were independent risk factors for cataract (p<0.01). Relative to age or comorbidities, being a lifetime smoker (aOR=1.10) or a lifetime alcohol user (aOR=1.06) appeared to have a minimal effect on cataract status. Interestingly, both low and high salt intake was associated with cataract development. This finding must be interpreted cautiously, however, as salt intake was not measured by laboratory tests and was recorded based on the participants' subjective judgment using questionnaire. Two possible explanations are 1) both low and high salt intake influences cataract risk, despite low salt intake generally being considered a healthy behavior and 2) subjects with comorbidities switched from high to low salt intake for health reasons. Because of the cross-sectional design of the study, we were unable to determine whether low salt intake truly contributed to cataract development. In terms of sleep duration, subjects who slept <6 hours/day were more likely to have cataracts than those who slept >9 hrs/day. The 4th quintile of BMI was positively associated with cataract, but appeared to have a minimal effect on cataract status (aOR=1.07). As for the health behaviors, the most important risk factor is short duration of sleeping, and the effect size of sleep duration (aOR=1.22 of <6 hrs/day) was comparable to having hypertension (aOR=1.23) in the final model (Table 2). Again, we cannot establish causality using such cross-sectional data, but it is possible that longer sleep duration is associated with greater resilience toward oxidative stress27 and/or less exposure to ultraviolet light, which are both risk factors for cataracts.
Strengths, limitations, and conclusions
Most importantly, we relied on questionnaire data to ascertain cataracts. Diagnosis by an ophthalmologist is more desirable, since relying on self-reporting may introduce bias; however, to increase the accuracy of participant replies, we first asked an interviewee if he/she had cataracts, and then asked if he/she had been diagnosed by a doctor. Information on the sensitivity (91.0%) and specificity (58.0%) of cataract self-report has been collected from the Korea National Health and Nutrition Examination Survey (KNHANES), which is similar to our survey in terms of both design and interview format.8 We chose not to focus on age-standardized prevalence and comparison of prevalence with other country, which may be underestimated because of low awareness (25.1%) of cataract in Korea.26 Instead, we investigated independent risk factors for cataract development because of high sensitivity of self-report data. This study was performed in an Asian population, and circumstances may be different in Western countries, leading to different results. In addition, because this was a cross-sectional study, temporal cause and effect relationships could not be established.
Despite these limitations, this study also had a number of important strengths. First, this study involved a large sample size of 715554 participants. Second, previous reports indicated that self-report data is likely to have high sensitivity for cataracts. Thus, the CHS dataset allowed us to analyze a rich set of possible cataract risk factors. Finally, we introduced nomogram and its potential for practical applications as a cataract screening tool. We conclude that age is the most important risk factor for cataracts, although DM, osteoporosis, arthritis, atopic dermatitis and short sleep duration (<6 hours/day) may also increase the risk. Nomograms, such as the one presented here, might be helpful for non-ophthalmologists, including primary physicians or optometrists, to identify high-risk patients in need of cataract screening.
ACKNOWLEDGEMENTS
This study was supported by a grant of the Korean Health Technology R&D Project, Ministry for Health, Welfare & Family Affairs, Republic of Korea (HI13C1485).
Footnotes
The authors have no financial conflicts of interest.
Supplementary Material
Supplementary Table 1. Characteristics of Study Population (n=715554).
| n | % | |
|---|---|---|
| Cataract | ||
| No | 695152 | 88.7 |
| Yes | 88464 | 11.3 |
| Sociodemographic factors | ||
| Age (yrs) | ||
| 40-49 | 207293 | 29.0 |
| 50-59 | 192903 | 27.0 |
| 60-69 | 160605 | 22.4 |
| 70-79 | 120905 | 16.9 |
| 80+ | 33848 | 4.7 |
| Sex | ||
| Male | 327000 | 45.7 |
| Female | 388554 | 54.3 |
| Monthly household income (≒USD)* | ||
| Lowest quintile (<500) | 137527 | 19.2 |
| 2nd-4th quintile (500-2000) | 426393 | 59.6 |
| Highest quintile (>2000) | 151634 | 21.2 |
| Education | ||
| Elementary school | 186931 | 29.5 |
| Middle school | 116857 | 18.4 |
| High school | 208528 | 32.9 |
| University or higher | 122352 | 19.3 |
| Residential area† | ||
| Urban | 357519 | 50.0 |
| Rural | 358035 | 50.0 |
| Medicaid | ||
| No | 674762 | 94.3 |
| Yes | 40615 | 5.7 |
| Spouse | ||
| With spouse | 544931 | 78.0 |
| Without spouse | 153538 | 22.0 |
| Occupation | ||
| Administrative, management, or professional occupations | 55342 | 7.9 |
| Business and financial operation occupations | 33315 | 4.7 |
| Sales and related occupations | 87272 | 12.4 |
| Farming, fishing, and forestry occupations | 124456 | 17.6 |
| Installation, maintenance, and repair occupations/laborers | 131379 | 18.6 |
| Housewives | 148504 | 21.1 |
| Others, including unemployed | 125145 | 17.7 |
| Obesity (BMI)‡ | ||
| 1st quintile (<20.20) | 143159 | 20.0 |
| 2nd quintile (20.20-21.93) | 143417 | 20.0 |
| 3rd quintile (21.93-23.39) | 142873 | 20.0 |
| 4th quintile (23.39-25.16) | 144464 | 20.2 |
| 5th quintile (>25.16) | 141641 | 19.8 |
| Comorbidities | ||
| Hypertension | ||
| No | 508183 | 71.0 |
| Yes | 207128 | 29.0 |
| Diabetes mellitus | ||
| No | 637903 | 89.2 |
| Yes | 77397 | 10.8 |
| Dyslipidemia | ||
| No | 655021 | 91.5 |
| Yes | 60533 | 8.5 |
| Cerebrovascular accident | ||
| No | 695742 | 97.3 |
| Yes | 19626 | 2.7 |
| Myocardial infarction | ||
| No | 702444 | 98.2 |
| Yes | 12536 | 1.8 |
| Angina | ||
| No | 698441 | 97.7 |
| Yes | 16515 | 2.3 |
| Arthritis | ||
| No | 591879 | 82.7 |
| Yes | 123675 | 17.3 |
| Osteoporosis | ||
| No | 642225 | 89.8 |
| Yes | 72679 | 10.2 |
| Asthma | ||
| No | 693321 | 96.9 |
| Yes | 22059 | 3.1 |
| Allergic rhinitis | ||
| No | 668363 | 93.4 |
| Yes | 46921 | 6.6 |
| Atopic dermatitis | ||
| No | 705151 | 98.6 |
| Yes | 10217 | 1.4 |
| Hepatitis B infection | ||
| No | 699696 | 97.8 |
| Yes | 15355 | 2.2 |
| Health behaviors | ||
| Lifetime smoker§ | ||
| No | 440234 | 61.5 |
| Yes | 275320 | 38.5 |
| Lifetime alcohol user∥ | ||
| No | 203893 | 28.5 |
| Yes | 511577 | 71.5 |
| Physical activity¶ | ||
| Regular physical activity | 152525 | 21.3 |
| No regular physical activity | 563029 | 78.7 |
| Salt intake | ||
| High | 185665 | 26.0 |
| Normal | 365126 | 51.0 |
| Low | 164637 | 23.0 |
| Sleep duration | ||
| <6 hrs/day | 121100 | 16.9 |
| 6-9 hrs/day | 579158 | 81.0 |
| >9 hrs/day | 14994 | 2.1 |
BMI, body mass index.
*The income per adult equivalent was calculated using the following formula: household income/√number of people in household, †Residence was classified as either belonging to a metropolitan area or not depending on whether the administrative district had a population of 20000 or greater, ‡BMI was calculated using the equation: body weight (kg)/height (m2), §All respondents were asked if they had smoked a total of 100 cigarettes in their life.2 Those who answered 'yes' and still smoked were classified as 'lifetime smokers,' ∥Lifetime alcohol users were defined as those who have ever drunk alcohol in their life, ¶We defined moderate-intensity activities as those that lasted at least 30 minutes and increased the individual's heart rate slightly compared to sedentary activities; examples included volleyball, table tennis, swimming, yoga, and badminton, but not walking.
Supplementary Table 2. The Age-Specific Prevalence of Cataract According to Self-Report, Stratified by Survey Year.
| Age | 2008 | 2009 | 2010 | 2011 | 2012 | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | |
| 40-49 | 0.7 | (0.6-0.8) | 1.0 | (0.9-1.1) | 0.6 | (0.5-0.7) | 0.8 | (0.7-0.9) | 0.9 | (0.8-1.0) |
| 50-59 | 2.7 | (2.5-2.9) | 3.2 | (2.9-3.4) | 3.1 | (2.9-3.3) | 3.7 | (3.5-3.9) | 3.5 | (3.3-3.7) |
| 60-69 | 11.6 | (11.2-12.1) | 13.9 | (13.4-14.4) | 15.0 | (14.5-15.5) | 17.4 | (16.8-17.9) | 15.9 | (15.4-16.4) |
| 70-79 | 24.6 | (23.8-25.4) | 28.4 | (27.6-29.2) | 30.8 | (30.1-31.6) | 35.9 | (35.1-36.7) | 35.0 | (34.3-35.8) |
| 80- | 30.5 | (28.9-32.0) | 35.3 | (33.8-36.8) | 39.0 | (37.6-40.5) | 43.1 | (41.7-44.6) | 42.4 | (41.0-43.8) |
| ≥40* | 6.9 | (6.7-7.1) | 8.1 | (8.0-8.3) | 8.7 | (8.5-8.9) | 10.2 | (10.0-10.4) | 10.0 | (9.8-10.2) |
| ≥50 | 11.0 | (10.7-11.2) | 12.7 | (12.5-13.0) | 13.6 | (13.4-13.9) | 15.6 | (15.3-15.9) | 15.0 | (14.8-15.3) |
| ≥60 | 18.1 | (17.7-18.5) | 21.0 | (20.6-21.5) | 23.0 | (22.6-23.4) | 26.7 | (26.3-27.1) | 25.7 | (25.3-26.1) |
| ≥70 | 25.9 | (25.3-26.5) | 30.0 | (29.3-30.6) | 32.7 | (32.1-33.3) | 37.6 | (36.9-38.2) | 36.7 | (36.1-37.3) |
CI, confidence interval.
*≥X: subjects aged X years and older.
References
- 1.Klein BE, Klein R, Lee KE, Gangnon RE. Incidence of age-related cataract over a 15-year interval the Beaver Dam Eye Study. Ophthalmology. 2008;115:477–482. doi: 10.1016/j.ophtha.2007.11.024. [DOI] [PubMed] [Google Scholar]
- 2.Vashist P, Talwar B, Gogoi M, Maraini G, Camparini M, Ravindran RD, et al. Prevalence of cataract in an older population in India: the India study of age-related eye disease. Ophthalmology. 2011;118:272–278. doi: 10.1016/j.ophtha.2010.05.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Xu L, Cui T, Zhang S, Sun B, Zheng Y, Hu A, et al. Prevalence and risk factors of lens opacities in urban and rural Chinese in Beijing. Ophthalmology. 2006;113:747–755. doi: 10.1016/j.ophtha.2006.01.026. [DOI] [PubMed] [Google Scholar]
- 4.Seah SK, Wong TY, Foster PJ, Ng TP, Johnson GJ. Prevalence of lens opacity in Chinese residents of Singapore: the tanjong pagar survey. Ophthalmology. 2002;109:2058–2064. doi: 10.1016/s0161-6420(02)01221-6. [DOI] [PubMed] [Google Scholar]
- 5.Congdon N, Vingerling JR, Klein BE, West S, Friedman DS, Kempen J, et al. Prevalence of cataract and pseudophakia/aphakia among adults in the United States. Arch Ophthalmol. 2004;122:487–494. doi: 10.1001/archopht.122.4.487. [DOI] [PubMed] [Google Scholar]
- 6.Hiller R, Sperduto RD, Ederer F. Epidemiologic associations with nuclear, cortical, and posterior subcapsular cataracts. Am J Epidemiol. 1986;124:916–925. doi: 10.1093/oxfordjournals.aje.a114481. [DOI] [PubMed] [Google Scholar]
- 7.Kanthan GL, Wang JJ, Rochtchina E, Tan AG, Lee A, Chia EM, et al. Ten-year incidence of age-related cataract and cataract surgery in an older Australian population. The Blue Mountains Eye Study. Ophthalmology. 2008;115:808–814. doi: 10.1016/j.ophtha.2007.07.008. [DOI] [PubMed] [Google Scholar]
- 8.Rim TH, Kim MH, Kim WC, Kim TI, Kim EK. Cataract subtype risk factors identified from the Korea National Health and Nutrition Examination survey 2008-2010. BMC Ophthalmol. 2014;14:4. doi: 10.1186/1471-2415-14-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.McElroy JA, Klein BE, Lee KE, Howard KP, Klein R. Place-based exposure and cataract risk in the Beaver Dam cohort. J Environ Health. 2014;76:34–40. [PMC free article] [PubMed] [Google Scholar]
- 10.Leske MC, Wu SY, Hennis A, Connell AM, Hyman L, Schachat A. Diabetes, hypertension, and central obesity as cataract risk factors in a black population. The Barbados Eye Study. Ophthalmology. 1999;106:35–41. doi: 10.1016/s0161-6420(99)90003-9. [DOI] [PubMed] [Google Scholar]
- 11.Mukesh BN, Le A, Dimitrov PN, Ahmed S, Taylor HR, McCarty CA. Development of cataract and associated risk factors: the Visual Impairment Project. Arch Ophthalmol. 2006;124:79–85. doi: 10.1001/archopht.124.1.79. [DOI] [PubMed] [Google Scholar]
- 12.Berendschot TT, Broekmans WM, Klöpping-Ketelaars IA, Kardinaal AF, Van Poppel G, Van Norren D. Lens aging in relation to nutritional determinants and possible risk factors for age-related cataract. Arch Ophthalmol. 2002;120:1732–1737. doi: 10.1001/archopht.120.12.1732. [DOI] [PubMed] [Google Scholar]
- 13.Leske MC, Chylack LT, Jr, Wu SY. The Lens Opacities Case-Control Study. Risk factors for cataract. Arch Ophthalmol. 1991;109:244–251. doi: 10.1001/archopht.1991.01080020090051. [DOI] [PubMed] [Google Scholar]
- 14.Feder J. Too big to fail: the enactment of health care reform. J Health Polit Policy Law. 2011;36:413–416. doi: 10.1215/03616878-1271027. [DOI] [PubMed] [Google Scholar]
- 15.Nagatomo F, Roy RR, Takahashi H, Edgerton VR, Ishihara A. Effect of exposure to hyperbaric oxygen on diabetes-induced cataracts in mice. J Diabetes. 2011;3:301–308. doi: 10.1111/j.1753-0407.2011.00150.x. [DOI] [PubMed] [Google Scholar]
- 16.Chen KJ, Pan WH, Huang CJ, Lin BF. Association between folate status, diabetes, antihypertensive medication and age-related cataracts in elderly Taiwanese. J Nutr Health Aging. 2011;15:304–310. doi: 10.1007/s12603-010-0282-8. [DOI] [PubMed] [Google Scholar]
- 17.Kim SI, Kim SJ. Prevalence and risk factors for cataracts in persons with type 2 diabetes mellitus. Korean J Ophthalmol. 2006;20:201–204. doi: 10.3341/kjo.2006.20.4.201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nemet AY, Hanhart J, Kaiserman I, Vinker S. Are cataracts associated with osteoporosis? Clin Ophthalmol. 2013;7:2079–2084. doi: 10.2147/OPTH.S49927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Klein BE, Klein R, Lee KE. Diabetes, cardiovascular disease, selected cardiovascular disease risk factors, and the 5-year incidence of age-related cataract and progression of lens opacities: the Beaver Dam Eye Study. Am J Ophthalmol. 1998;126:782–790. doi: 10.1016/s0002-9394(98)00280-3. [DOI] [PubMed] [Google Scholar]
- 20.Naeem SS, Siddiqui EU, Kazi AN, Khan S, Abdullah FE, Adhi I. Prevalence of hepatitis 'B' and hepatitis 'C' among preoperative cataract patients in Karachi. BMC Res Notes. 2012;5:492. doi: 10.1186/1756-0500-5-492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Christensen JD. Frequency of cataract in atopic dermatitis. Acta Derm Venereol. 1981;61:76–77. [PubMed] [Google Scholar]
- 22.Pham TQ, Wang JJ, Rochtchina E, Maloof A, Mitchell P. Systemic and ocular comorbidity of cataract surgical patients in a western Sydney public hospital. Clin Experiment Ophthalmol. 2004;32:383–387. doi: 10.1111/j.1442-9071.2004.00842.x. [DOI] [PubMed] [Google Scholar]
- 23.LaForce C, Journeay GE, Miller SD, Silvey MJ, Wu W, Lee LA, et al. Ocular safety of fluticasone furoate nasal spray in patients with perennial allergic rhinitis: a 2-year study. Ann Allergy Asthma Immunol. 2013;111:45–50. doi: 10.1016/j.anai.2013.04.013. [DOI] [PubMed] [Google Scholar]
- 24.Emin O, Fatih M, Mustafa O, Nedim S, Osman C. Evaluation impact of long-term usage of inhaled fluticasone propionate on ocular functions in children with asthma. Steroids. 2011;76:548–552. doi: 10.1016/j.steroids.2011.02.003. [DOI] [PubMed] [Google Scholar]
- 25.Wang S, Xu L, Jonas JB, You QS, Wang YX, Yang H. Dyslipidemia and eye diseases in the adult Chinese population: the Beijing eye study. PLoS One. 2012;7:e26871. doi: 10.1371/journal.pone.0026871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rim TH, Park SY, Kim TI. Epidemiological Survey Regarding Cataract Awareness in Korea: KNHANES IV. J Korean Ophthalmol Soc. 2013;54:72–77. [Google Scholar]
- 27.McEwen BS. Sleep deprivation as a neurobiologic and physiologic stressor: allostasis and allostatic load. Metabolism. 2006;55(10 Suppl 2):S20–S23. doi: 10.1016/j.metabol.2006.07.008. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Table 1. Characteristics of Study Population (n=715554).
| n | % | |
|---|---|---|
| Cataract | ||
| No | 695152 | 88.7 |
| Yes | 88464 | 11.3 |
| Sociodemographic factors | ||
| Age (yrs) | ||
| 40-49 | 207293 | 29.0 |
| 50-59 | 192903 | 27.0 |
| 60-69 | 160605 | 22.4 |
| 70-79 | 120905 | 16.9 |
| 80+ | 33848 | 4.7 |
| Sex | ||
| Male | 327000 | 45.7 |
| Female | 388554 | 54.3 |
| Monthly household income (≒USD)* | ||
| Lowest quintile (<500) | 137527 | 19.2 |
| 2nd-4th quintile (500-2000) | 426393 | 59.6 |
| Highest quintile (>2000) | 151634 | 21.2 |
| Education | ||
| Elementary school | 186931 | 29.5 |
| Middle school | 116857 | 18.4 |
| High school | 208528 | 32.9 |
| University or higher | 122352 | 19.3 |
| Residential area† | ||
| Urban | 357519 | 50.0 |
| Rural | 358035 | 50.0 |
| Medicaid | ||
| No | 674762 | 94.3 |
| Yes | 40615 | 5.7 |
| Spouse | ||
| With spouse | 544931 | 78.0 |
| Without spouse | 153538 | 22.0 |
| Occupation | ||
| Administrative, management, or professional occupations | 55342 | 7.9 |
| Business and financial operation occupations | 33315 | 4.7 |
| Sales and related occupations | 87272 | 12.4 |
| Farming, fishing, and forestry occupations | 124456 | 17.6 |
| Installation, maintenance, and repair occupations/laborers | 131379 | 18.6 |
| Housewives | 148504 | 21.1 |
| Others, including unemployed | 125145 | 17.7 |
| Obesity (BMI)‡ | ||
| 1st quintile (<20.20) | 143159 | 20.0 |
| 2nd quintile (20.20-21.93) | 143417 | 20.0 |
| 3rd quintile (21.93-23.39) | 142873 | 20.0 |
| 4th quintile (23.39-25.16) | 144464 | 20.2 |
| 5th quintile (>25.16) | 141641 | 19.8 |
| Comorbidities | ||
| Hypertension | ||
| No | 508183 | 71.0 |
| Yes | 207128 | 29.0 |
| Diabetes mellitus | ||
| No | 637903 | 89.2 |
| Yes | 77397 | 10.8 |
| Dyslipidemia | ||
| No | 655021 | 91.5 |
| Yes | 60533 | 8.5 |
| Cerebrovascular accident | ||
| No | 695742 | 97.3 |
| Yes | 19626 | 2.7 |
| Myocardial infarction | ||
| No | 702444 | 98.2 |
| Yes | 12536 | 1.8 |
| Angina | ||
| No | 698441 | 97.7 |
| Yes | 16515 | 2.3 |
| Arthritis | ||
| No | 591879 | 82.7 |
| Yes | 123675 | 17.3 |
| Osteoporosis | ||
| No | 642225 | 89.8 |
| Yes | 72679 | 10.2 |
| Asthma | ||
| No | 693321 | 96.9 |
| Yes | 22059 | 3.1 |
| Allergic rhinitis | ||
| No | 668363 | 93.4 |
| Yes | 46921 | 6.6 |
| Atopic dermatitis | ||
| No | 705151 | 98.6 |
| Yes | 10217 | 1.4 |
| Hepatitis B infection | ||
| No | 699696 | 97.8 |
| Yes | 15355 | 2.2 |
| Health behaviors | ||
| Lifetime smoker§ | ||
| No | 440234 | 61.5 |
| Yes | 275320 | 38.5 |
| Lifetime alcohol user∥ | ||
| No | 203893 | 28.5 |
| Yes | 511577 | 71.5 |
| Physical activity¶ | ||
| Regular physical activity | 152525 | 21.3 |
| No regular physical activity | 563029 | 78.7 |
| Salt intake | ||
| High | 185665 | 26.0 |
| Normal | 365126 | 51.0 |
| Low | 164637 | 23.0 |
| Sleep duration | ||
| <6 hrs/day | 121100 | 16.9 |
| 6-9 hrs/day | 579158 | 81.0 |
| >9 hrs/day | 14994 | 2.1 |
BMI, body mass index.
*The income per adult equivalent was calculated using the following formula: household income/√number of people in household, †Residence was classified as either belonging to a metropolitan area or not depending on whether the administrative district had a population of 20000 or greater, ‡BMI was calculated using the equation: body weight (kg)/height (m2), §All respondents were asked if they had smoked a total of 100 cigarettes in their life.2 Those who answered 'yes' and still smoked were classified as 'lifetime smokers,' ∥Lifetime alcohol users were defined as those who have ever drunk alcohol in their life, ¶We defined moderate-intensity activities as those that lasted at least 30 minutes and increased the individual's heart rate slightly compared to sedentary activities; examples included volleyball, table tennis, swimming, yoga, and badminton, but not walking.
Supplementary Table 2. The Age-Specific Prevalence of Cataract According to Self-Report, Stratified by Survey Year.
| Age | 2008 | 2009 | 2010 | 2011 | 2012 | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | |
| 40-49 | 0.7 | (0.6-0.8) | 1.0 | (0.9-1.1) | 0.6 | (0.5-0.7) | 0.8 | (0.7-0.9) | 0.9 | (0.8-1.0) |
| 50-59 | 2.7 | (2.5-2.9) | 3.2 | (2.9-3.4) | 3.1 | (2.9-3.3) | 3.7 | (3.5-3.9) | 3.5 | (3.3-3.7) |
| 60-69 | 11.6 | (11.2-12.1) | 13.9 | (13.4-14.4) | 15.0 | (14.5-15.5) | 17.4 | (16.8-17.9) | 15.9 | (15.4-16.4) |
| 70-79 | 24.6 | (23.8-25.4) | 28.4 | (27.6-29.2) | 30.8 | (30.1-31.6) | 35.9 | (35.1-36.7) | 35.0 | (34.3-35.8) |
| 80- | 30.5 | (28.9-32.0) | 35.3 | (33.8-36.8) | 39.0 | (37.6-40.5) | 43.1 | (41.7-44.6) | 42.4 | (41.0-43.8) |
| ≥40* | 6.9 | (6.7-7.1) | 8.1 | (8.0-8.3) | 8.7 | (8.5-8.9) | 10.2 | (10.0-10.4) | 10.0 | (9.8-10.2) |
| ≥50 | 11.0 | (10.7-11.2) | 12.7 | (12.5-13.0) | 13.6 | (13.4-13.9) | 15.6 | (15.3-15.9) | 15.0 | (14.8-15.3) |
| ≥60 | 18.1 | (17.7-18.5) | 21.0 | (20.6-21.5) | 23.0 | (22.6-23.4) | 26.7 | (26.3-27.1) | 25.7 | (25.3-26.1) |
| ≥70 | 25.9 | (25.3-26.5) | 30.0 | (29.3-30.6) | 32.7 | (32.1-33.3) | 37.6 | (36.9-38.2) | 36.7 | (36.1-37.3) |
CI, confidence interval.
*≥X: subjects aged X years and older.