Abstract
Objective
Little is known about the consequences of tobacco smoking stigma on smokers and how smokers may internalize smoking-related stigma. This review summarizes existing literature on tobacco smoking self-stigma, investigating to what extent smokers are aware of negative stereotypes, agree with them and apply them to themselves.
Methods
We carried out a systematic search of Pubmed/Web of Science/PsycInfo databases for articles related to smoking self-stigma through June 2013. Reference lists and citations of included studies were also checked and experts were contacted. After screening articles for inclusion/exclusion criteria we performed a quality assessment and summarized findings according to the stages of self-stigma as conceptualized in Corrigan’s progressive model of self-stigma (aware, agree, apply and harm). Initial searches yielded 570 articles.
Results
Thirty of these articles (18 qualitative and 12 quantitative studies) met criteria for our review. Awareness of smoking stigma was virtually universal across studies. Coping strategies for smoking stigma and the degree to which individuals who smoke internalized this stigma varied both within and across studies. There was considerable variation in positive, negative, and non-significant consequences associated with smoking self-stigma. Limited evidence was found for subgroup differences in smokingrelated stigma.
Conclusion
While there is some evidence that smoking self-stigma leads to reductions in smoking, this review also identified significant negative consequences of smoking self-stigma. Future research should assess the factors related to differences in how individuals respond to smoking stigma. Public health strategies which limit the stigmatization of smokers may be warranted.
Keywords: smoking, tobacco use, self-stigma, stigma
INTRODUCTION
Tobacco smoking is, in many countries, subject to restrictive public health efforts, aimed at discouraging smoking and making it an unacceptable behavior. Many public health institutions including the World Health Organization(2012) and the Centers for Disease Control (2014) advocate the denormalization of tobacco use and changing social norms around tobacco use to combat the negative health effects of tobacco. Approaches include smoke free air laws (Tynan, Babb, MacNeil, & Griffin, 2011), media campaigns (Wakefield, Loken, & Hornik, 2010), and pictorial health warnings on tobacco products (Cameron, Pepper, & Brewer, 2015; Hammond, 2011; Monarrez-Espino, Liu, Greiner, Bremberg, & Galanti, 2014). In addition, some organizations have instituted anti-smoking policies such as prohibiting the hiring of smokers (Asch, Muller, & Volpp, 2013) or requiring higher health insurance premiums for smokers (Madison, Schmidt, & Volpp, 2013). Alongside changes in social attitudes, these policies could contribute to the stigmatization of smokers (Bayer, 2008; Bell, McCullough, Salmon, & Bell, 2010a). However, social control strategies, which are employed in an effort to reduce the prevalence and incidence of smoking and reduce exposure of non-smokers to second-hand (Baxi et al., 2014) and thirdhand smoking (Ferrante et al., 2013), may actually further marginalize ‘residual smokers’ who may be more disadvantaged and have fewer resources to help them quit (Burns & Warner, 2000).
Comparative studies on the stigma of health conditions suggest a difference between uncontrollable conditions like schizophrenia, which the general public does not primarily associate with guilt (but with notions of unpredictability and dangerousness), and seemingly controllable conditions like alcohol use disorders (Schomerus et al., 2011). In the latter, stigma is hypothesized to carry a strong normative function: unacceptable behavior is stigmatized to clarify boundaries of acceptable, normal behavior (Phelan, Link, & Dovidio, 2008). Stigmatized persons are excluded and can only rejoin the group if they change their behavior. Goffman defines stigma as an attribute considered undesirable and unpleasant by society differentiating the person from other members of the community. He also refers to ‘spoiled identity’ but acknowledges there are different degrees to which stigma is experienced (1968). Presumably, the stigma of smoking, although certainly not as severe as the stigma of alcohol dependence, follows the same pattern. One main factor that distinguishes smoking stigma from other stigmatized conditions is its relative recency. While not always considered acceptable throughout history, a few decades ago, smokers were revered as “cool,” and “mysterious” invoking images such as the Marlboro Man (Corrigan, 2004; Hafez & Ling, 2005). However, in recent decades the social status associated with being a smoker has diminished (Stuber, Galea, & Link, 2009). Other mental and physical health conditions have not seen this dramatic shift in status through the 20th century making smoking stigma an important and distinct area of research.
There is broad consensus regarding the impact of smoking on individual and public health (e.g., Mokdad etal., 2004; Oberg, Jaakkola, Woodward, Peruga, & Pruss-Ustun, 2011) and considerable research on the degree to which anti-smoking campaigns are successful in encouraging individuals to quit and in reducing overall smoking rates (Levy, Chaloupaka, & Gitchell, 2004; Wakefield etal., 2010). Yet, little is known about how those who smoke cope with smoking-related stigma that may stem from these strategies and the negative consequences of smoking-related stigma on those who smoke. Of particular concern are the potential consequences of internalizing public stigma which is referred to as self-stigma or internalized stigma (Link & Phelan, 2001).
A prominent cognitive model of self-stigma, originally proposed by Corrigan et al. for mental illness (Corrigan & Watson, 2002), describes self-stigma as a process of four interrelated steps. According to this progressive model of self-stigma (Corrigan & Watson, 2002), a person is first aware of prevalent negative stereotypes and, second, personally agrees to some extent with the negative stereotypes. The person may then, thirdly, self-identify with the stigmatized group and apply negative stereotypes to himself/herself, which may finally result in negative consequences such as loss of self-esteem and reduced self-efficacy. This model has been validated for mental illness (e.g., Corrigan & Watson, 2002; Corrigan, Rafacz, & Rusch, 2011 and alcohol use disorder (Schomerus et al., 2011) but has not been examined in the context of tobacco use and dependence. A particular strength of this model is that it incorporates both perceived stigma (first stage) and internalized stigma (stages three and four) and thus provides a framework with which to explore the relationship between negative public attitudes and individual self-stigma. Because of the broad perspective of this model, describing different stages from stigma perception to self-stigma, it provides a useful framework to examine self-stigma-related findings.
We hypothesized that if the public stigma of tobacco smoking results in self-stigma and reduced self-efficacy among those who smoke, it could have detrimental effects. Intended to reduce smoking, it could instead undermine abilities of those affected to quit smoking. In this context, the aim of this review is to summarize existing literature on smoking self-stigma and the degree to which the current literature addresses the stages of self-stigma according to the progressive model of self-stigma. Moreover, we know that smoking rates differ greatly by gender, culture, SES, and age (e.g., Evans-Polce, Vasilenko, & Lanza, 2015) and there may also be differences in self-stigma according to these characteristics, with certain groups being particularly vulnerable. Thus, we examine the degree to which current literature has examined differences in smoking self-stigma by the following subgroups: gender, SES, culture, and age.
METHODS
Search strategy and study selection
We searched the following databases for articles related to tobacco smoking self-stigma: Pubmed, Web of Science, and PsycINFO through June 2013. Further articles were identified through hand-searching reference lists of retrieved articles. We also contacted expert stigma researchers for additional studies, including those not published in peer-reviewed journals. These methods identified 661 articles. We used the following search terms: internalized stigma OR felt stigma OR imagined stigma OR self-stigma OR shame OR blame OR hopelessness OR guilt OR fear of discrimination OR anticipated discrimination) AND (smok* OR tobacco OR nicotine OR cigarette). The review protocol was registered at PROSPERO International Prospective Register of Systematic Reviews (PROSPERO 2013:CRD42013005093).
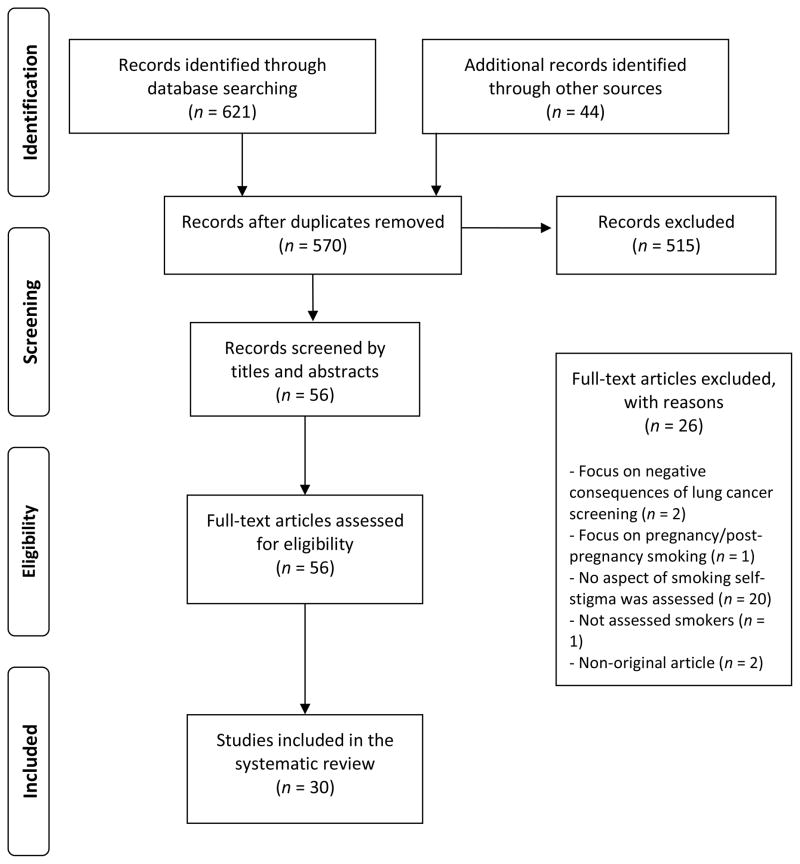
One reviewer (JMCM) screened all titles and abstracts and a second reviewer (SEL) independently screened a random sample of 10% of selected studies. Both reviewers evaluated articles using the inclusion and exclusion criteria detailed below. Disagreements were resolved through discussion and consultation. Agreement for article exclusion was greater than 80%. A diagram of the study selection process is presented in Figure 1.
Fig. 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram.
A priori inclusion and exclusion criteria were set by the authors. The criteria were: (1) original data based articles (quantitative and qualitative), (2) articles published in English, German, Portuguese, or Spanish, (3) articles that dealt, totally or partially, with tobacco smokers’ self-stigma, (3) articles which used the term stigma to refer to botanical elements, cellular biology, or stigmata) were excluded. Additional exclusion criteria were added after a pilot search of articles. These comprised articles which discussed stigma only in relation to: other types of substance use, general drug use (not just nicotine/tobacco use), other psychiatric disorders, other clinical diseases, socio-demographic characteristics, patients in treatment for diseases such as cancer, tuberculosis, or COPD due to past or current tobacco smoking.
Data extraction and quality assessment
One author (JMCM) tabulated data for all included studies using a pre-piloted form. Information was extracted on: (1) study characteristics, (2) participant characteristics, (3) results relevant to self-stigma (i.e., relationship between self-stigma and quit attempts, attitudes toward smoking/smokers, consequences of self-stigma), and other relevant information.
The quality assessment was performed separately for quantitative and qualitative studies. For quantitative studies, six criteria were used, adapted from the Evidence for Policy and Practice Information and Co-ordinating Centre (Oliver et al., 2005). These were: (1) aims clearly stated, (2) design appropriate to the stated objectives, (3) justification for sample size, (4) evidence provided of reliability or validity of measures used, (5) statistics accurately reported, (6) sample selection relatively unbiased. For the 18 qualitative studies, seven criteria were used, adapted from the Critical Appraisal Skills Programme Qualitative Research Checklist [25]. These were: (1) aims clearly stated, (2) design appropriate for stated objectives, (3) study context described in detail, (4) data collection and sampling appropriate, justified, and clearly reported, (5) analysis was rigorous and clearly described, (6) a reflexive account of the researchers’ influence was provided, and (7) a clear statement of the findings was provided. Because relatively little data exists on smoking self-stigma we used broad and not overly restrictive quality criteria in our assessments, including studies meeting at least four of the six criteria for quantitative studies and six of the seven criteria for qualitative studies, as reported in previous systematic reviews (Clement et al., 2014).
Results were synthesized using the Corrigan model as a framework. In our synthesis we examined three categories: (1) stereotype awareness (‘aware’), (2) personal stereotype agreement (‘agree’), and (3) applying stereotypes to oneself and experiencing consequences associated with self-stigmatization (‘apply’ and ‘harm’). While the Corrigan Model has traditionally divided this third step into two separate processes, empirical studies have consistently found very high correlations between measures of ‘apply’ and ‘harm’ [20]. For our synthesis, we found it most appropriate to combine these two stages of internalized stigma into one.
RESULTS
Our database searches identified 570 non-duplicate records. After reviewing titles and abstracts, 56 articles were identified as potentially relevant papers and these full papers were assessed against eligibility criteria during which approximately half (n = 26) were removed. The remaining 30 studies were included in the review. Eighteen of these studies were qualitative [26–41] and 13 were quantitative (one used mixed methods). This process, including reasons for article exclusion, is outlined in Figure 1.
Quality assessment
Among quantitative studies, 10 of the 13 studies met at least five and 12 of 13 studies met at least four of the six quality criteria. One study used a mixed methods approach; however, only qualitative findings were included as the study’s quantitative results only met three of the six criteria, and thus were excluded from subsequent analyses. The main methodological weakness identified by the quality assessment was lack of sample size justification (n = 13 studies).
In assessing qualitative studies, 15 of the 18 studies met at least six of the seven criteria. The remaining three studies met five of the seven criteria. The most frequently neglected criterion was having a reflexive account of the researchers’ influence on the study (n = 12). Table 1 summarizes characteristics of included studies and additional details can be found in a supplementary table.
Table 1.
Study Characteristics for included studies (n=27)
| Author and year | Country | Participants | Type of study | Design |
|---|---|---|---|---|
| Allan et al., 2012 | Scotland | Smokers who dropped out of a smoking cessation program that had a final incentive (n=14) | Qualitative | Unstructured interviews |
| Baer et al., 1989 | USA | Smokers who had not resumed regular smoking 4 weeks post-treatment (n=102) | Quantitative | Prospective, in context cessation intervention, followed up to 1 year post-treatment. |
| Bell et al., 2010 | Canada | Smokers and ex-smokers recruited from newspaper advertisements (n=25) | Qualitative | Open-ended interviews |
| Bennasar Veny et al., 2011 | Spain | Female nurses who had been habitual smokers for at least two years prior to the study (n=15) | Qualitative | Semi-structured interviews |
| Berlin & Covey, 2006 | USA | Smokers recruited for a smoking cessation trial (n=600) | Quantitative | Prospective, in context of cessation intervention, followed through 3 months of treatment and 6 months post-treatment. |
| Betzner et al., 2012 | USA | Smokers and recent quitters who responded to a tobacco cessation program (n=166) | Qualitative | Focus groups and in-depth interviews |
| Bottorff et al., 2013 | Canada | Mother and father dyads who were current and former smokers with a 1 year old child at baseline (n=28) | Qualitative | In-depth interviews when child was 1 year, 20–35 months, and 36–48 months |
| Bush et al., 2003 | England | Purposive sample of Bangladeshi and Pakistani smokers and nonsmokers in Newcastle (n=141) | Qualitative | Semi-structured, in-depth interviews and focus groups |
| Copeland, 2003 | Scotland | Female smokers, General Practitioners, and nursing staff recruited from a general practice (n=41) | Qualitative/Quantitative | Observational cross-sectional quantitative survey and open-ended qualitative questionnaire |
| Farrimond & Joffe, 2006 | UK | Smokers and non-smokers with diverse socioeconomic statuses (n=40) | Qualitative | Conceptual mapping, ‘episodic’ interviews, semi-structured interview |
| Fong et al., 2004 | Australia, Canada, USA and UK | Participants from the International Tobacco Control Policy Evaluation Survey (Canada n=2,193; United States n=2,115; United Kingdom n=2,344; Australia n=2,271) | Quantitative | Observational cross-sectional survey |
| Frohlich et al., 2010 | Canada | Current adult smokers recruited with purposive sampling (n=17) | Qualitative | Semi-structured interviews |
| Gibbons et al., 1991 | USA | Adult smokers responding to a smoking cessation program advertisement (n=120) | Quantitative | Prospective, 16 weekly surveys in context of intervention and 6 month post-quit date follow up survey |
| Goldstein, 1991 | Canada | Adult smokers and nonsmokers household level 1989 Winnipeg Area Study (n=521) | Quantitative | Observational cross-sectional survey |
| Greaves et al., 2010 | Canada | New fathers who continued to smoke during partner’s pregnancy and/or post-partum (n=29) | Qualitative | In-depth, semi-structured interviews |
| Grove, 1993 | Australia | Smokers who had ever made a quit attempt (n=155) | Quantitative | Observational cross-sectional survey |
| Holdsworth & Robinson, 2008 | UK | Mothers with at least one smoking parent and a child under 5 (n=17) | Qualitative | Interviews using the Bibliographic Narrative Interpretative Method |
| Kirchner et al., 2012 | USA | Smokers enrolled in a research smoking cessation clinic who had experienced a lapse (n=203) | Quantitative | Prospective, in the context of a cessation intervention, ecological momentary assessments collected during the first 6 weeks of a quit attempt |
| Lee & Paek, 2012 | Korea | Male smokers (n=255) | Quantitative | Quasi-experimental, survey pre and post one of 3 types of anti-smoking message conditions |
| Lee & Paek, 2013 | Korea and USA | University student smokers (n=310) | Quantitative | Quasi-experimental survey pre and post one of 3 types of anti-smoking message conditions |
| Louka et al., 2006 | UK and Greece | Adult smokers (n=21) | Qualitative | Semi-structured interviews and focus groups |
| McCarthy et al., 2010 | USA | Adult daily smokers (n=463) | Quantitative | Prospective, in the context of a cessation intervention, ecological momentary assessments pre- and post-quitting smoking |
| Oliffe et al., 2012 | Canada | New fathers who smoked (n=24) | Qualitative | Four audio-recorded group sessions |
| Ritchie et al., 2010 | Scotland | Adult current smokers and recent ex-smokers (n=40) | Qualitative | Three-wave longitudinal in-depth interviews |
| Scheffels, 2009 | Norway | Established daily smokers sampled for diversity on gender and social class (n=21) | Qualitative | Semi-structured interviews |
| Stuber et al., 2008 | USA | Current and former smokers in New York City (n=816) | Quantitative | Observational cross-sectional survey |
| Stuber & Galea, 2009 | USA | Current New York City smokers (n=835) | Quantitative | Observational cross-sectional survey |
| Supnick & Colletti, 1984 | USA | Individuals who completed a smoking cessation program (n=33) | Quantitative | Prospective, followed up after a cessation intervention monthly through 6 months post-treatment |
| Thompson, et al., 2007 | New Zealand | Smokers (n=17) and ex-smokers (n=9) living in a diverse, socioeconomically disadvantaged neighborhood | Qualitative | Semi-structured interviews |
| Van der Heiden et al., 2013 | Netherlands | Lower-educated daily smokers (n=18) | Qualitative | Structured in-depth interviews |
Evidence of smoking self-stigma in the literature using the progressive model of self-stigma
We categorized findings of smoking-related self-stigma into three groups according to the stages represented in the progressive model of self-stigma (Corrigan & Watson, 2002): (1) Stereotype awareness, (2) stereotype agreement, and (3) applying stereotypes to oneself. Of the 30 studies assessed in the review, eight studies addressed all three stages within the Corrigan model. Table 2 shows the stages addressed in each of the studies.
Table 2.
Summary of the stages of the progressive model of self-stigma addressed in the studies.
| Author and year | Type of study | Stage 1 | Stage 2 | Stage 3 | Consequences |
|---|---|---|---|---|---|
| Awareness | Agreement | Application | |||
| Allan et al., 2012 | Qualitative | X | X | −; guilt, smoking behavior | |
| Baer et al., 1989 | Quantitative | −; guilt, smoking behavior | |||
| Bell et al., 2010 | Qualitative | X | X | X | +/−; smoking behavior, concealment |
| Bennasar-Veny et al., 2011 | Qualitative | X | X | +/−; smoking behavior, guilt | |
| Berlin & Covey, 2006 | Quantitative | n.s.; self-blame | |||
| Betzner et al., 2012 | Qualitative | X | X | +/−; smoking behavior, self-efficacy | |
| Bottorff et al., 2013 | Qualitative | X | X | +/−; guilt | |
| Bush et al., 2003 | Qualitative | X | |||
| Copeland, 2003 | Qualitative/Quantitative | X | X | ||
| Farrimond & Joffe, 2006 | Qualitative | X | X | X | |
| Fong et al., 2004 | Quantitative | X | |||
| Frohlich et al., 2010 | Qualitative | X | X | ||
| Gibbons et al., 1991 | Quantitative | X | X | n.s.; smoking behavior | |
| Goldstein, 1991 | Quantitative | X | X | ||
| Greaves et al., 2010 | Qualitative | X | X | X | −; stress, guilt |
| Grove, 1993 | Quantitative | n.s.; self-efficacy | |||
| Holdsworth & Robinson, 2008 | Qualitative | X | X | X | |
| Kirchner et al., 2012 | Qualitative | +; guilt, self-blame | |||
| Lee & Paek, 2012 | Quantitative | +; guilt | |||
| Lee & Paek, 2013 | Quantitative | X | +; guilt | ||
| Louka et al., 2006 | Qualitative | X | X | X | −; guilt, self-efficacy |
| McCarthy et al., 2010 | Quantitative | n.s.; guilt | |||
| Oliffe et al., 2012 | Qualitative | X | X | ||
| Ritchie et al., 2010 | Qualitative | X | X | X | −; concealment |
| Scheffels, 2009 | Qualitative | X | −; smoking behavior | ||
| Stuber et al., 2008 | Quantitative | X | |||
| Stuber & Galea, 2009 | Quantitative | X | −; concealment | ||
| Supnick & Colletti, 1984 | Quantitative | +; smoking behavior, guilt | |||
| Thompson, et al., 2007 | Qualitative | X | |||
| Van der Heiden et al., 2013 | Qualitative | X | X | +/−; smoking behavior |
Note: − = negative consequences, + = positive consequences, +/− = mix of positive and negative consequences, n.s. = non-significant
Stage 1: Stereotype awareness
The majority of studies addressed smoker’s awareness of smoking-related stigma. The stereotypes that smokers reported to be associated with smoking were almost universally negative. Most of the studies that addressed this stage were qualitative studies (n = 17); however three quantitative studies addressed this stage as well. The first found that 30–40% of current smokers felt high levels of family disapproval and general social unacceptability of smoking and 27% perceived differential treatment due to their smoking status (Stuber, Galea, & Link, 2008). The remaining two studies which comprised both current and former smokers who recently quit found similarly high levels of awareness of social stigma with 39% reporting that people think less of a person who smokes (Stuber & Galea, 2009) and smokers to be rated less favorably than nonsmokers (Goldstein, 1991).
Within the qualitative studies, participants reported almost exclusively negative perceptions of smokers and smokers felt acutely aware of these negative stereotypes. Many smokers reported feeling stigmatized for their smoking status, including feeling ostracized or through perceptions of negative judgments, stares, or nonverbal communication. However, some studies also reported more explicit experiences in the form of overtly negative comments or actions displayed by others (e.g., Bell et al., 2010a; Greaves et al., 2010). In the four studies in which parents were interviewed, participants reported feeling that stigma was particularly strong for parents. Stigmatizing perceptions were felt from many different social domains including: family members, coworkers, individuals encountered in public spaces, and even health care providers. In multiple studies participants reported avoiding smoking in public spaces due to fear of stigmatization. Thus, this increased awareness of stereotypes may lead to increased social distance between smokers and non-smokers (Thompson et al., 2007). One exception to these negative perceptions was a study of Pakistani and Bangladeshi immigrants in the UK in which some reported that for men cigarette smoking was seen as “macho” and fashionable (Bush, White, Kai, Rankin, & Bhopal, 2003).
Stage 2: Personal stereotype agreement
While there was wide discussion and acknowledgement of the existence of social stigma around smoking, personal agreement with these perceptions and stereotypes was less frequently addressed. Only nine studies addressed this stage in some way-- seven qualitative and two quantitative studies. All studies found that at least some participants agreed with the stereotypes. One study reported that while participants were aware of negative stereotypes, some disagreed and contested stereotypes and even medical advice, for example, denying that smoking around children was dangerous (Holdsworth & Robinson, 2008). However this was not the norm and all other studies that addressed this stage found exclusive agreement with negative stereotypes. Interestingly, a few studies found that smokers only applied negative stereotypes, or applied them more strongly, to a subset of smokers such as older and heavier smokers or those that smoked around children (Frohlich et al., 2010; Greaves et al., 2010; Ritchie, Amos, & Martin, 2010; Louka et al., 2006). This “downward comparison” by smokers allowed them to agree with negative stereotypes but resist applying these stereotypes to themselves.
Stage 3: Applying stereotypes to oneself and experiencing consequences associated with self-stigmatization
Almost all studies addressed the third stage of applying the stereotypes to one’s self and the consequences associated with doing so. Sixteen were qualitative and 10 were quantitative.
Interestingly, the consequences reported were not always negative, nor were smoking stereotypes always personally applied to themselves even if it appeared that there was personal agreement with stereotypes generally. As discussed above in Stage 2, while some participants agreed with stigmatizing stereotypes, they only applied these stereotypes to a subset of smokers who they saw as worse off than them. Similarly, one study reported that participants in a smoking cessation program perceived themselves to have little in common with the “typical smoker.” Moreover, their image of a “typical smoker” became more negative over the course of the program, regardless of whether they were successful in quitting smoking (Gibbons, Gerrard, Lando, & McGovern, 1991). However, the vast majority of studies which addressed application of stereotypes to one’s self overwhelmingly reported that participants felt shame, guilt, and embarrassment for their own smoking behavior. In multiple studies, participants applied words such as “leper,” “outcast,” “bad person,” “low-life,” and “pathetic” in reference to their own smoking behaviors. Some reported an increase in these feelings following a failed quit attempt (Bennasar-Veny et al., 2011; Copeland, 2003).
Table 2 shows whether consequences were positive, negative, mixed, or non-significant (e.g., stigma was not associated with relapse) for each study. In four studies, negative consequences of smoking self-stigma were exclusively reported. Negative consequences included relapse, increased resistance to smoking cessation or reduction, self-induced social isolation, increases in stress due to non-disclosure of smoking status to one’s healthcare provider. Four studies exclusively reported positive consequences. Positive consequences included smoking cessation, decreased risk of lapse or relapse, and increased intentions to quit. Multiple studies (n = 5) reported a mix of positive and negative consequences from smoking stigma. The mix of positive and negative consequences related to smoking self-stigma may be partially due to subgroup differences. Five studies also reported non-significant findings in relation to consequences.
Group differences in self-stigma
Very few studies addressed population subgroup differences in smoking self-stigma. We summarize the findings from the small number examining these differences.
Two studies examined gender differences in smoking self-stigma (Bush et al., 2003; Fong et al., 2004). One study examined differences in awareness or perceptions of stigma towards smokers by both smokers and nonsmokers. This study was among Pakistani and Bangladeshi adults and found greater awareness of stigma for women compared to men. A woman who smoked was seen as shameful and “tainted” whereas smoking among men was seen as acceptable and “macho.” The second study examined differences in personal agreement and consequences and found women experienced more regret with regard to smoking compared to men (Fong et al., 2004).
Four studies examined differences in self-stigma by socioeconomic status (SES), with conflicting results. Two studies found that those with a higher SES (measured by income or education) experience more stigma, guilt, and embarrassment compared to those of lower SES (Frolich et al., 2010; Stuber et al., 2008). However, the remaining studies found the opposite with one showing more regret among those with less than a university education. The other found that those of low SES were more aware of the “outcast” label of a smoker, more accepting of negative stereotypes, and more likely to internalize these stereotypes, while those of higher SES were better able to distance themselves from smoking stereotypes (Farrimond & Joffe, 2006).
Three studies addressed cultural differences. The first found that compared to those in the U.S., Korean smokers experienced more guilt following an anti-smoking message (Lee & Paek, 2014). Another study also examined racial/ethnic differences in the U.S. and found Whites to have more awareness of stereotypes (Stuber et al., 2008) compared to Blacks or Hispanics/Latinos. The third study examined differences between Greek and U.K. smokers finding heightened stereotype awareness and guilt among U.K. versus Greek smokers (Louka et al., 2006).
Two studies addressed age differences, both in terms of awareness of stereotypes. One study identified older smokers as being more aware of smoking stereotypes and how they have evolved and intensified over time (Betzner et al., 2012). The second study found that gender difference in stereotypes – specifically the stronger negative stereotypes for women- was stronger in older generations than younger ones.
Variations in Coping with Smoking Stigma
We found considerable heterogeneity in whether individuals internalized stigma and the coping strategy they employed in reaction to smoking stigma. Strategies ranged from guilt and internalization of stigma to defensiveness and rejection of stereotypes. Defensive strategies comprised reports of a strengthening of resolve to continue smoking because of experienced stigma and a general anger and frustration with the restrictive policies around smoking and frank stigma they experienced.
DISCUSSION
Overall, these findings provide tentative support for intended consequences of stigmatizing smoking/smokers (i.e., reducing smoking); but, also for unintended consequences (e.g., guilt, loss of selfesteem, defensiveness and resolve to continue smoking). There are several mechanisms upon which tobacco control programs could influence smoking including directly through an individual’s decision to smoke or indirectly by facilitating discussion around smoking (and its potential harms) or through changing social norms which may lead to pressure to quit and influence policymakers (Wakefield et al., 2010). In relation to the process of self-stigma and smoking, while our review found no studies that specifically used the Corrigan Model of Self Stigma, many studies addressed multiple components of the model within their findings. The vast majority of studies addressed both awareness of smoking stereotypes and the application and consequences of self-stigma. While findings regarding awareness were for the most part consistent across and within studies, the evidence regarding applying stereotypes and the consequences of self-stigma was much more heterogeneous. Personal agreement with stereotypes was assessed much less often. This stage appears to often be overlooked in the literature and it may be that this stage is often assumed or it is not considered an important intermediary step from stereotype awareness to consequences. While previous self-stigma research indicates that not all individuals who are aware of public stigma internalize it (Corrigan & Watson, 2002; Rusch et al., 2005), in the case of smoking, negative stereotypes are so dominant throughout many communities that it may be inevitable that all smokers would agree with these stigmatizing views as well.
Variation in Coping with Smoking Stigma
While we were not able to decipher the types of coping strategies from the studies we reviewed, it was evident that different strategies were used by smokers to deal with the stigma they experienced. W Given the pervasiveness of smoking stigma awareness and the abundance of public health strategies and campaigns that aim to denormalize smoking (CDC, 2014; WHO, 2012; Bell et al. 2010a], a better understanding of the coping strategies used by individuals who smoke in the face of this stigma is warranted. In particular, there is little research on individuals who use a defensive coping strategy in response to smoking stigma or other strategies outside of the dominant strategy to internalize. This defensive strategy is also employed by other marginalized groups such as individuals with mental illness (Rusch et al., 2005) and individuals with weight difficulties (Puhl & Brownell, 2003). For smoking, defending one’s self-esteem against the internalization of public stigma can result in maintaining smoking behavior and it thus poses a serious health risk to themselves, their families, and the broader community. However, why certain individuals are defensive or more resistant to public stigma compared to others and if health outcomes differ for these individuals is not well understood. More research is needed to understand the different smoking stigma coping strategies and if they are similar to those of other mental and physical health conditions (Link, Mirotznik, & Cullen, 1991) as well as how different coping strategies may lead to different outcomes.
Self-stigma consequences
Consequences varied widely both across and within studies. Only four studies exclusively reported positive consequences as a result of smoking self-stigma. While this corroborates that there can in fact be positive consequences from self-stigma such as smoking cessation and reduction, these are far from universal. Many smokers also report negative consequences as a result of stigma and selfstigma. Additionally, negative consequences were even found in healthcare settings (Allan, Radley, & Williams, 2012; Stuber & Galea, 2009). Other research has also suggested that fear of stigma can lead individuals to avoid treatment for a health condition (Rusch et al., 2005; Clement et al., 2014). It appears public stigma of smoking could result in four different individual outcomes. The desired outcome and the one often assumed by public health practitioners is that smokers will internalize the stigma and quit smoking in order to feel better. However, there are at least three other potential outcomes: (1) the smoker internalizes the smoking stigma, loses self-esteem and self-efficacy, and fails to quit smoking, (2) the smoker resists internalizing the smoking stigma remaining indifferent and fails to quit smoking, or (3) the smoker resists smoking stigma internalization, may become angry and defensive at the public for stigmatizing smoking, fails to quit smoking and may even increase their self-esteem and self-efficacy regarding smoking. In severe mental illness, severity of stigma-related outcomes such as low self-esteem and hopelessness may be determined by personal stress appraisal, coping resources and individual emotional and cognitive stress reactions (Rusch et al., 2009a; Rusch et al., 2009b). The role of individual coping resources for outcomes of smoking stigma has not yet been investigated; but, understanding these mechanisms could help tailor anti-smoking programs to be more effective, particularly for vulnerable groups with few coping resources.
To date, much of the public health and psychology literature emphasizes the positive consequences of smoking stigma. This study sheds light on potential negative consequences when this stigma is internalized into smoking self-stigma. There is not enough understanding of potential unintended negative consequences that can result from anti-smoking policies. Research in other areas of mental health and public health tend to agree that stigmatization strategies are not effective and lead to more negative consequences than positive ones (Bayer, 2008). Other research has also shown that stigmatizing attitudes are complex and that different types of stigma are associated with varied consequences (Castaldelli-Maia et al., 2011; Evans-Lacko et al., 2012). More attention should be given to negative consequences given the large portion of public health interventions to reduce smoking that make use of socially stigmatizing strategies.
Group differences
Only a few studies examined group differences, most often qualitatively. However, there were notable differences in terms of gender, culture, SES, and age. Additionally, two studies, highlighted potential cultural differences in the awareness of stigma. A study of a Pakistani and Bangladeshi sample in the U.K. was unique in that it was the only study to identify positive stereotypes associated with smoking (Bush et al., 2003). Additionally, smokers in Greece rarely reported experiencing stigma and disapproval with regard to their smoking (Louka et al., 2006). This suggests these stereotypes are dependent on cultural context. While there seems to be broad consensus in most mainstream Western culture that smoking is “bad,” there are other cultures which have managed to evade negative stereotypes that appear dominant in much of the Western world. Further research should explore cultural differences in awareness and whether this leads to differential smoking outcomes. Additionally, it may be beneficial to track changes in stereotypes among different cultures across historical time. Two of the studies that examined cultural differences occurred almost a decade or more ago. Given the pace at which smoking stigma has emerged in Western culture, there may be significant changes in awareness of smoking stigma even in the span of 10 years.
Group differences in self-stigma are not well understood. More research is needed that examines group differences at each of the three self-stigma stages and the extent to which negative and positive consequences and differences in coping strategies are distributed throughout the population. An uneven distribution of consequences may help explain health disparities related to smoking. Additionally, other potential group differences should be explored such as differences in family structure and family support or regional differences based on smoking policies.
Limitations
The limitations of our study need to be acknowledged. Using the Corrigan model of self-stigma, we tried to distinguish findings on perceived stigma, personal attitudes of the smokers and internalized stigma. Because none of the studies tested a theoretical model of self-stigma, we can only assume that the Corrigan model captures the most relevant aspects of smoking self-stigma. Due to the vague conceptualizations of stigma and self-stigma in many studies, it remains unclear whether the consequences discussed in these studies were a result of self-stigma or of overall smoking stigma. The heterogeneity of studies and the high number of qualitative studies prevented conducting any meta-analysis of findings. Additionally, although we defined cigarette smokers broadly and did not exclude studies based on where individuals fell on the smoking continuum, smoking levels varied across participants and studies and there may be differences in self-stigmatization depending on an individual’s smoking behavior which we are not able to determine. Another limitation is that the search terms emphasized negative factors such as stigma and discrimination and have the potential to bias our findings; however, more neutral terms such as attitudes, beliefs and perceptions are overly general and thus difficult to include while maintaining a reasonable scope to the study. It is also possible that some articles were missed that do not explicitly use the terms we have selected but have relevant information relating to smoking self-stigma. We attempted to mitigate this by contacting experts in the field to suggest any crucial articles we may have missed. The individual studies varied in methodological quality; however, we assessed this and to some degree excluded those that were of poor quality. In addition, as only one author performed data extraction and quality assessment for all of the articles, we were not able to determine inter-rater reliability. However, there were extensive discussions among authors throughout the review process and all authors discussed any articles that appeared unclear.
Implications
While there is evidence that internalizing smoking stigma may prompt some individuals to quit smoking, this review also suggests that smoking self-stigma can have profoundly negative consequences for some smokers and may make quitting more difficult. We do not suggest that internalization of smoking stigma has universally negative consequences; however, it is important to highlight the potential for negative consequences in response to the substantial research and public health effort focused on the positive consequences of smoking stigma. Public health policies aimed at smoking reduction, thus, might also, alongside current strategies, consider increasing the self-efficacy of smokers and avoiding messages that trigger potentially harmful defensive coping strategies and consequences. Instead of reiterating negative stereotypes about smokers or smoking, health policies could rely more on positive strategies. Currently, there may be an overreliance on strategies which focus on negative reinforcement including both strategies to change smoking norms and increase smoke-free public spaces as well as more structurally stigmatizing policies such as basing hiring decisions and health insurance costs on smoking status. Public health smoking prevention and cessation strategies might instead benefit from a greater inclusion of interventions and policies that focus on positive reinforcement and treatment in order to reduce smoking prevalence while avoiding the stigmatization of smokers.
Supplementary Material
Table 3 (online appendix only). Stages and findings of the progressive model of self-stigma addressed in the studies.
Highlights.
We used Corrigan’s model to summarize tobacco smoking self-stigma literature
Thirty qualitative and quantitative articles met criteria for review
Awareness of smoking stigma was virtually universal among smokers across studies
Coping strategies and stigma internalization varied across studies
Positive and negative consequences were found as a result of smoking self-stigma
Acknowledgments
Financial support
This research was funded by grants from the National Institute on Drug Abuse (NIDA) - P50DA010075 and T32DA017629. SEL has a Starting Grant from the European Research Council.
We would like to thank Kirsten Bell, Miquel Benassar-Veny John Brodersen, Kate Flemming, Winifried Gebhardt, Catriona Hooke, Hye-Jin Paek, Deborah Ritchie, and Jude Robinson for their expert advice on additional references.
Footnotes
Conflict of interest
SEL and GS have received consulting fees from Lundbeck unrelated to the current study.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Allan C, Radley A, Williams B. Paying the price for an incentive: an exploratory study of smokers’ reasons for failing to complete an incentive based smoking cessation scheme. Journal of Health Services Research & Policy. 2012;17(4):212–218. doi: 10.1258/jhsrp.2012.011084. [DOI] [PubMed] [Google Scholar]
- Asch DA, Muller RW, Volpp KG. Conflicts and compromises in not hiring smokers. New England Journal of Medicine. 2013;368(15):1371–1373. doi: 10.1056/NEJMp1303632. [DOI] [PubMed] [Google Scholar]
- Baer JS, Karmack T, Lichtenstein E, Ransom CC. Prediction of smoking relapse: Analyses of temptations and transgressions after initial cessation. Journal of Consulting and Clinical Psychology. 1989;57(5):623. doi: 10.1037//0022-006x.57.5.623. [DOI] [PubMed] [Google Scholar]
- Baxi R, Sharma M, Roseby R, Polnay A, Priest N, Waters E, Webster P. The Cochrane Library. 2014. Family and carer smoking control programmes for reducing children’s exposure to environmental tobacco smoke. [DOI] [PubMed] [Google Scholar]
- Bayer R. Stigma and the ethics of public health: not can we but should we. Social Science & Medicine. 2008;67(3):463–472. doi: 10.1016/j.socscimed.2008.03.017. [DOI] [PubMed] [Google Scholar]
- Bell K, Salmon A, Bowers M, Bell J, McCullough L. Smoking, stigma and tobacco ‘denormalization’: Further reflections on the use of stigma as a public health tool. A commentary on Social Science & Medicine’s Stigma, Prejudice, Discrimination and Health Special Issue (67: 3) Social Science & Medicine. 2010a;70(6):795–799. doi: 10.1016/j.socscimed.2009.09.060. [DOI] [PubMed] [Google Scholar]
- Bell K, McCullough L, Salmon A, Bell J. ‘Every space is claimed’: smokers’ experiences of tobacco denormalisation. Sociology of Health & Illness. 2010b;32(6):914–929. doi: 10.1111/j.1467-9566.2010.01251.x. [DOI] [PubMed] [Google Scholar]
- Bennasar Veny M, Pericas Beltrán J, González Torrente S, Segui González P, Aguiló Pons A, Tauler Riera P. Self-perceived factors associated with smoking cessation among primary health care nurses: a qualitative study. Revista Latino-Americana de Enfermagem. 2011;19(6):1437–1444. doi: 10.1590/s0104-11692011000600022. [DOI] [PubMed] [Google Scholar]
- Berlin I, Covey LS. Pre-cessation depressive mood predicts failure to quit smoking: the role of coping and personality traits*. Addiction. 2006;101(12):1814–1821. doi: 10.1111/j.1360-0443.2006.01616.x. [DOI] [PubMed] [Google Scholar]
- Betzner AE, Boyle RG, Luxenberg MG, Schillo BA, Keller PA, Rainey J, Saul JE. Experience of smokers and recent quitters with smokefree regulations and quitting. American Journal of Preventive Medicine. 2012;43(5):S163–S170. doi: 10.1016/j.amepre.2012.08.005. [DOI] [PubMed] [Google Scholar]
- Bottorff JL, Oliffe JL, Kelly MT, Johnson JL, Chan A. Reconciling parenting and smoking in the context of child development. Qualitative Health Research. 2013 doi: 10.1177/1049732313494118. 1049732313494118. [DOI] [PubMed] [Google Scholar]
- Briggs J. Cochrane Qualitative Research Methods Group. The Cochrane Collaboration. 2006 URL: http://www.joannabriggs.eduau/cqrmg/role.html.
- Burns DM, Warner KE. Those who continue to smoke, Smoking and Tobacco Control Monograph No, 15. US Department of Health and Human Services; Bethesda, MD: 2003. Smokers who have not quit: is cessation more difficult and should we change our strategies. [Google Scholar]
- Bush J, White M, Kai J, Rankin J, Bhopal R. Understanding influences on smoking in Bangladeshi and Pakistani adults: community based, qualitative study. BMJ. 2003;326(7396):962. doi: 10.1136/bmj.326.7396.962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cameron LD, Pepper JK, Brewer NT. Responses of young adults to graphic warning labels for cigarette packages. Tobacco Control. 2015;24(e1):e14–e22. doi: 10.1136/tobaccocontrol-2012-050645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castaldelli-Maia JM, Scomparini LB, Andrade AG, Bhugra D, de Toledo FAT, D’Elia G. Perceptions of and attitudes toward antidepressants: stigma attached to their use--a review. The Journal of Nervous and Mental Disease. 2011;199(11):866–871. doi: 10.1097/NMD.0b013e3182388950. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Best Practices for Comprehensive Tobacco Control Programs—2014. Atlanta: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2014. [Google Scholar]
- Clement S, Schauman O, Graham T, Maggioni F, Evans-Lacko S, Bezborodovs N, Thornicroft G. What is the impact of mental health-related stigma on help-seeking? A systematic review of quantitative and qualitative studies. 2014. [DOI] [PubMed] [Google Scholar]
- Copeland L. An exploration of the problems faced by young women living in disadvantaged circumstances if they want to give up smoking: can more be done at general practice level? Family Practice. 2003;20(4):393–400. doi: 10.1093/fampra/cmg410. [DOI] [PubMed] [Google Scholar]
- Corrigan PW, Watson AC. The paradox of self-stigma and mental illness. Clinical Psychology: Science and Practice. 2002;9(1):35–53. [Google Scholar]
- Corrigan PW. Marlboro man and the stigma of smoking. In: Gilman Sl, Xun Z., editors. Smoke: A global history of smoking. London, England: Reaktion books; 2004. [Google Scholar]
- Evans-Lacko S, Brohan E, Mojtabai R, Thornicroft G. Association between public views of mental illness and self-stigma among individuals with mental illness in 14 European countries. Psychological Medicine. 2012;42(08):1741–1752. doi: 10.1017/S0033291711002558. [DOI] [PubMed] [Google Scholar]
- Evans-Polce RJ, Vasilenko SA, Lanza ST. Changes in gender and racial/ethnic disparities in rates of cigarette use, regular heavy episodic drinking, and marijuana use: ages 14 to 32. Addictive Behaviors. 2015;41:218–222. doi: 10.1016/j.addbeh.2014.10.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farrimond HR, Joffe H. Pollution, peril and poverty: a British study of the stigmatization of smokers. Journal of Community & Applied Social Psychology. 2006;16(6):481–491. [Google Scholar]
- Ferrante G, Simoni M, Cibella F, Ferrara F, Liotta G, Malizia V, La Grutta S. Thirdhand smoke exposure and health hazards in children. Monaldi Arch Chest Dis. 2013;79(1):38–43. doi: 10.4081/monaldi.2013.108. [DOI] [PubMed] [Google Scholar]
- Fong GT, Hammond D, Laux FL, Zanna MP, Cummings KM, Borland R, Ross H. The near-universal experience of regret among smokers in four countries: findings from the International Tobacco Control Policy Evaluation Survey. Nicotine & Tobacco Research. 2004;6(Suppl 3):S341–S351. doi: 10.1080/14622200412331320743. [DOI] [PubMed] [Google Scholar]
- Frohlich KL, Poland B, Mykhalovskiy E, Alexander S, Maule C. Tobacco control and the inequitable socio-economic distribution of smoking: smokers’ discourses and implications for tobacco control. Critical Public Health. 2010;20(1):35–46. [Google Scholar]
- Gibbons FX, Gerrard M, Lando HA, McGovern PG. Social comparison and smoking cessation: The role of the “typical smoker”. Journal of Experimental Social Psychology. 1991;27(3):239–258. [Google Scholar]
- Goffman E. Asylums: Essays on the social situation of mental patients and other inmates. Aldine Transaction; 1968. [Google Scholar]
- Greaves L, Oliffe JL, Ponic P, Kelly MT, Bottorff JL. Unclean fathers, responsible men: Smoking, stigma and fatherhood. Health Sociology Review. 2010;19(4):522–533. [Google Scholar]
- Grove JR. Attributional correlates of cessation self-efficacy among smokers. Addictive Behaviors. 1993;18(3):311–320. doi: 10.1016/0306-4603(93)90032-5. [DOI] [PubMed] [Google Scholar]
- Hafez N, Ling PM. How Philip Morris built Marlboro into a global brand for young adults: implications for international tobacco control. Tobacco Control. 2005;14(4):262–271. doi: 10.1136/tc.2005.011189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammond D. Health warning messages on tobacco products: a review. Tobacco Control. 2011;20(5):327–337. doi: 10.1136/tc.2010.037630. [DOI] [PubMed] [Google Scholar]
- Holdsworth C, Robinson JE. ‘I’ve never ever let anyone hold the kids while they’ve got ciggies’: moral tales of maternal smoking practices. Sociology of health & illness. 2008;30(7):1086–1100. doi: 10.1111/j.1467-9566.2008.01102.x. [DOI] [PubMed] [Google Scholar]
- Kirchner TR, Shiffman S, Wileyto EP. Relapse dynamics during smoking cessation: recurrent abstinence violation effects and lapse-relapse progression. Journal of Abnormal Psychology. 2012;121(1):187. doi: 10.1037/a0024451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee H, Paek HJ. Impact of norm perceptions and guilt on audience response to anti-smoking norm PSAs: A case of Korean male smokers. Health Education Journal. 2012:1–9. [Google Scholar]
- Lee H, Paek HJ. Roles of guilt and culture in normative influence: testing moderated mediation in the anti-secondhand smoking context. Psychology, Health & Medicine. 2014;19(1):14–23. doi: 10.1080/13548506.2013.772303. [DOI] [PubMed] [Google Scholar]
- Levy DT, Chaloupka F, Gitchell J. The effects of tobacco control policies on smoking rates: a tobacco control scorecard. Journal of Public Health Management and Practice. 2004;10(4):338–353. doi: 10.1097/00124784-200407000-00011. [DOI] [PubMed] [Google Scholar]
- Link BG, Phelan JC. Conceptualizing stigma. Annual review of Sociology. 2001:363–385. [Google Scholar]
- Livingston JD, Boyd JE. Correlates and consequences of internalized stigma for people living with mental illness: A systematic review and meta-analysis. Social Science & Medicine. 2010;71(12):2150–2161. doi: 10.1016/j.socscimed.2010.09.030. [DOI] [PubMed] [Google Scholar]
- Madison K, Schmidt H, Volpp KG. Smoking, obesity, health insurance, and health incentives in the Affordable Care Act. JAMA. 2013;310(2):143–144. doi: 10.1001/jama.2013.7617. [DOI] [PubMed] [Google Scholar]
- McCarthy DE, Piasecki TM, Jorenby DE, Lawrence DL, Shiffman S, Baker TB. A multi-level analysis of non-significant counseling effects in a randomized smoking cessation trial. Addiction. 2010;105(12):2195–2208. doi: 10.1111/j.1360-0443.2010.03089.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Annals of Internal Medicine. 2009;151(4):264–269. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- Mokdad AH, Marks JS, Stroup DF, Gerberding JL. Actual causes of death in the United States, 2000. JAMA. 2004;291(10):1238–1245. doi: 10.1001/jama.291.10.1238. [DOI] [PubMed] [Google Scholar]
- Monárrez-Espino J, Liu B, Greiner F, Bremberg S, Galanti R. Systematic review of the effect of pictorial warnings on cigarette packages in smoking behavior. American Journal of Public Health. 2014;104(10):e11–e30. doi: 10.2105/AJPH.2014.302129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Öberg M, Jaakkola MS, Woodward A, Peruga A, Prüss-Ustün A. Worldwide burden of disease from exposure to second-hand smoke: a retrospective analysis of data from 192 countries. The Lancet. 2011;377(9760):139–146. doi: 10.1016/S0140-6736(10)61388-8. [DOI] [PubMed] [Google Scholar]
- Oliffe JL, Bottorff JL, Sarbit G. Supporting fathers’ efforts to be smoke-free: program principles. Canadian Journal of Nursing Research. 2012;44(3):64–82. [PubMed] [Google Scholar]
- Oliver S, Harden A, Rees R, Shepherd J, Brunton G, Garcia J, Oakley A. An emerging framework for including different types of evidence in systematic reviews for public policy. Evaluation. 2005;11(4):428–446. [Google Scholar]
- Phelan JC, Link BG, Dovidio JF. Stigma and prejudice: one animal or two? Social Science & Medicine. 2008;67(3):358–367. doi: 10.1016/j.socscimed.2008.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Puhl R, Brownell KD. Ways of coping with obesity stigma: review and conceptual analysis. Eating Behaviors. 2003;4(1):53–78. doi: 10.1016/s1471-0153(02)00096-x. [DOI] [PubMed] [Google Scholar]
- Ritchie D, Amos A, Martin C. “But it just has that sort of feel about it, a leper”—Stigma, smoke-free legislation and public health. Nicotine & Tobacco Research. 2010:ntq058. doi: 10.1093/ntr/ntq058. [DOI] [PubMed] [Google Scholar]
- Rüsch N, Angermeyer MC, Corrigan PW. Mental illness stigma: concepts, consequences, and initiatives to reduce stigma. European Psychiatry. 2005;20(8):529–539. doi: 10.1016/j.eurpsy.2005.04.004. [DOI] [PubMed] [Google Scholar]
- Rüsch N, Corrigan PW, Wassel A, Michaels P, Olschewski M, Wilkniss S, Batia K. A stress-coping model of mental illness stigma: I. Predictors of cognitive stress appraisal. Schizophrenia Research. 2009;110(1):59–64. doi: 10.1016/j.schres.2009.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rüsch N, Corrigan PW, Powell K, Rajah A, Olschewski M, Wilkniss S, Batia K. A stress-coping model of mental illness stigma: II. Emotional stress responses, coping behavior and outcome. Schizophrenia Research. 2009;110(1):65–71. doi: 10.1016/j.schres.2009.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scheffels J. Stigma, or sort of cool Young adults’ accounts of smoking and identity. European Journal of Cultural Studies. 2009;12(4):469–486. [Google Scholar]
- Schomerus G, Corrigan PW, Klauer T, Kuwert P, Freyberger HJ, Lucht M. Self-stigma in alcohol dependence: consequences for drinking-refusal self-efficacy. Drug and Alcohol Dependence. 2011;114(1):12–17. doi: 10.1016/j.drugalcdep.2010.08.013. [DOI] [PubMed] [Google Scholar]
- Stuber J, Galea S. Who conceals their smoking status from their health care provider? Nicotine & Tobacco Research. 2009;11(3):303–307. doi: 10.1093/ntr/ntn024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stuber J, Galea S, Link BG. Smoking and the emergence of a stigmatized social status. Social Science & Medicine. 2008;67(3):420–430. doi: 10.1016/j.socscimed.2008.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Supnick JA, Colletti G. Relapse coping and problem solving training following treatment for smoking. Addictive Behaviors. 1984;9(4):401–404. doi: 10.1016/0306-4603(84)90041-8. [DOI] [PubMed] [Google Scholar]
- Thompson L, Pearce J, Barnett JR. Moralising geographies: stigma, smoking islands and responsible subjects. Area. 2007;39(4):508–517. [Google Scholar]
- Tynan M, Babb S, MacNeil A, Griffin M. State Smoke-Free Laws for Worksites, Restaurants, and Bars—United States, 2000–2010. Journal of the American Medical Association. 2011;305(21):2167–2169. [Google Scholar]
- Van der-Heiden S, Gebhardt WA, Willemsen MC, Nagelhout GE, Dijkstra A. Behavioural and psychological responses of lower educated smokers to the smoke-free legislation in Dutch hospitality venues: A qualitative study. Psychology & Health. 2013;28(1):49–66. doi: 10.1080/08870446.2012.712695. [DOI] [PubMed] [Google Scholar]
- Wakefield MA, Loken B, Hornik RC. Use of mass media campaigns to change health behaviour. The Lancet. 2010;376(9748):1261–1271. doi: 10.1016/S0140-6736(10)60809-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. 2012 global progress report on implementation of the WHO Framework Convention on Tobacco Control. World Health Organization; 2012. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table 3 (online appendix only). Stages and findings of the progressive model of self-stigma addressed in the studies.