Abstract
The healing potential for articular cartilage lesions is limited due to many physiological, local and mechanical factors. Spontaneous healing of partial- and full-thickness lesions is slow, and subsequent tissue response is usually not durable. In symptomatic, and high-demand, patients, a definitive treatment modality must be offered which allows for a sustained recovery with minimal debilitation. Injuries, which damage the subchondral bone, heal with the formation of fibrocartilage. This tissue fails long-term survival because of its inability to withstand the variable cyclic loads and compression forces that it is subjected to. While regeneration of the damaged cartilage by an entirely new articular surface is a goal beyond current available techniques, repair of the osteochondral defects with normal hyaline cartilage is possible by various options. Osteochondral defects that are larger then 2 cm are best treated by osteochondral autograft technique. The short-term outcomes of the present series show excellent results.
Keywords: Osteochondral autograft, Tidemark, Cartilage repair
Introduction
Full-thickness articular defects have little potential for self-repair. When such defects penetrate the subchondral bone, the healing capacity is further compromised. The quality of the spontaneously repaired articular cartilage leaves much to be desired because of its inability to sustain the cyclical loads and high compression forces [1]. The naturally “repaired” surface is formed of fibrocartilage, which can deteriorate over time leading to functional deterioration [2]. Curl et al. found that articular cartilage defects are seen in nearly 63 % of patients undergoing arthroscopy, but barely 5 % are of International Cartilage Repair Society (ICRS) grades III and IV [3]. The treatment of these focal chondral defects presents many challenges, especially in the younger and more active population.
One of the more successful procedures to repair the defect involved drilling multiple holes through the subchondral bone in an attempt to stimulate bone-marrow-derived stem cells to form cartilage. This “microfracture” process reintroduced by Steadman produces fibrocartilage and is indicated for small defects in a younger subject [4]. Brittberg pioneered autologous chondrocyte implantation where autologous cultured chondrocytes are injected under a sutured periosteal flap. The results of this procedure, though favourable, are not popular due to the technical difficulties of procuring the chondrocytes and suturing the flap in place. More recently, the autologous chondrocytes are either cultured or engineered from stem cells onto an osteochondral matrix or scaffold and delivered arthroscopically, as shown by Zheng [5].
The challenge of treating larger focal defects led to the development of using osteochondral grafts from autologous source (autografts) such as the patella or the posterior femoral condyle [6, 7]. However, due to an anatomical mismatch, and non-congruence with the surrounding tissue, these procedures were not successful. This was overcome by the use of multiple cylinder osteochondral grafts by Hangody and Bobic, a process they described as mosaicplasty. They harvest cylindrical osteocartilaginous plugs from the non-articular area of the femur and transferred it to the site of the defect. Though the osseous integration occurred at roughly 4 weeks, the gaps persisted between the donor cartilage and recipient. The intervening connective tissue was fibrocartilage when evaluated at 8 weeks [8, 9•].
Technique of osteochondral autologous transfer
The surgical procedure starts with careful arthroscopic inspection and evaluation of the chondral or osteochondral defect. The size of the defect is carefully measured, as this has an important bearing on further treatment planning and execution. The periphery of the chondral defects demonstrates increased peak pressure as the diameter of the defect increases. The donor area for graft harvest should ideally be subjected to low stress, with curve and cartilage thickness characteristics similar to that of the recipient site. The femoral trochlea is a preferred site because the medial trochlea experiences low contact pressures and has a convex surface, which matches closely with the weight-bearing region of the condyles. Depending on the tools available, one can either harvest the autograft donor plugs via open or arthroscopic surgery. The recipient site needs to be sized and prepared to receive the donor plugs. Care must be taken to limit the removal of normal healthy tissue while ensuring a uniform clean margin. Testing with a long needle such that it is perpendicular to the condylar defect can assess if open or arthroscopic surgery is required, depending on recipient site accessibility. The defect is then prepared to receive the donor autograft by press-fit. The donor graft usually has a slightly larger diameter, which helps with horizontal graft stability [10]. The autograft is delivered by either gentle tapping or a screw-home technique, depending on the instrumentation. As long as the insertion forces remain below a threshold of 400 N (<10 MPa) on an 8-mm diameter graft, the cell viability of the graft remains good. In general, several low-force impactions are less damaging than a few high-force blows on the graft [11] Care must be taken to deliver the graft either congruent with the surrounding or countersunk by 1 mm. If the graft remains proud, it undergoes necrosis due to stress concentration. If the graft is recessed beyond 2 mm, it may get resorbed due to the lack of surface stress [12].
The bony part of the transplanted graft usually heals completely with the surrounding bone, while the cartilage surface though viable may not be fully healed to the surrounding bone. The autograft is a viable living structure, which provides excellent bony support to the overlying hyaline cartilage. The use of either a single or multiple grafts, to achieve congruent repair, can cover the recipient defect. The space between the osteochondral plugs gets filled by fibrocartilage. The donor sites may be left empty and show filling up by a fibrous tissue [13].
Author’s experience
We have performed the osteochondral autograft transfer surgery on a cohort of 20 patients.
Material and methods
Twenty patients (15 males, 5 females) aged between 19 and 46 years (mean 31.4; SD 7) were operated for chondral defects between 5- and 12-mm diameter. Clinical evaluation included detailed history, examination, assessment and severity of pain and association with other symptoms such as locking or effusion. Pre-operative imaging included long leg weight-bearing views, anteroposterior, lateral and skyline radiographs to rule out any impingement or alignment issues. Pre-operative MRI scans were utilized to assess the size, location and severity of the chondral defect. Donor site was also evaluated to match congruence as well as cartilage thickness. Specific cartilage sequences such as 3D gradient echo T1 sequences with fat saturation provide 3- to 4-mm-thick slices on three spatial planes, and fast spin echo T2 (FSE) sequences with fat saturation which improve these results were employed in the scanning. Cartilage maps were generated pre-operatively for assessment of the cartilage adjacent to the defect. Post-operative MRI was performed at 1 year for assessment by all points on the MOCART score and for viability of the graft.
Results
The mean follow-up was 42 months (24 to 64 months). The operating surgeon evaluated all patients clinically. At latest follow-ups, the patients were all evaluated according to the International Knee Documentation Committee (IKDC) evaluation protocol for cartilage injuries. One out of the 20 had a patellar chondral defect while the rest were all femoral. The commonest locations in order of frequency were medial condyle, lateral condyle and trochlea (10, 7 and 3, respectively). The mean Tegner activity scores were 4 and SD 2 currently, as compared to the pre-injury scores of 4.7 and SD 1. The mean IKDC subjective score was 81.6 (SD 15.3, range 34.5–100). The poorest scores (34.5) were seen in a patient who had suffered a road traffic accident resulting in multiple ligament ruptures on the affected knee. Both his cruciate ligaments and his partially torn menisci were repaired along with a 6-mm grade 3A chondral injury. One female patient with 10-mm-diameter chondral defects on both condyles secondary to osteonecrosis had a subjective score of 69. The younger, more active patients with less than 8-mm diameter had scores greater than 85. While MRI scans were not available at latest follow-up for all patients, bony consolidation had been achieved at 1-year follow-up for the subjects in the cohort.
Twelve of the 20 patients had an associated injury to the knee, which required additional surgical interventions. Nine of the 12 had an ACL repair done. Other procedures included meniscal suturing for a bucket handle tear and partial meniscectomy, as well as an open-wedge medial osteotomy for a varus knee deformity. The following figure (Fig. 1) shows an example of a successfully treated patient.
Fig. 1.
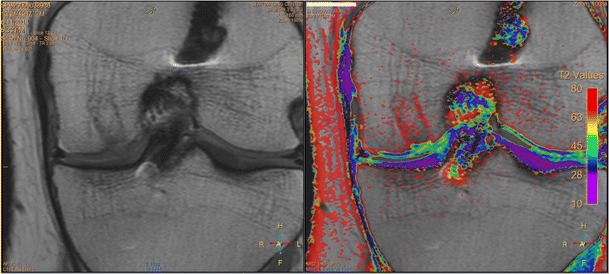
Two years post-mosaicplasty shows full bony integration as well cartilage healing as seen on the cartilage mapping. (T2 image scale between 40 and 50 indicating healing)
Discussion
The largest cohort of 789 defects with a maximum of 15 years follow-up, published by Hangody [14•] showed 92 % of good or very good results for the femoral condyle. Numerous reports have shown 84–88 % very good results at minimum 2 years follow-up [15, 16]. All the reports emphasize the simplicity of a single-stage procedure to deliver living tissue at lower cost and limited morbidity. The frequency of associated injuries in Gudas’ and Horas’ series ranged from 45 to 85 % [17•, 18].
Osteochondral autograft allows return to sports at about 6 months after surgery, particularly in athletes younger than 30 years of age [19]. At long-term follow-up, MRI and radiographs show incorporation of bone plugs with restoration of articular surface. The histology of this restored surface is more often hyaline or fibro-hyaline. Though there is clinical improvement, lack of peripheral integration of the cartilage is frequently observed [20].
Very meticulous attention to the harvesting and delivery of the graft is necessary to ensure that the articular surface is not damaged. The grafts may fracture during insertion and thus lead to instability within the recipient site. This instability may cause the graft to sink beyond 2 mm from the surface, thereby rendering it ineffective. Donor site defects can lead to haemarthrosis in early post-operative period requiring needle aspiration. It can also remain painful for up to 12 weeks and interfere with patellofemoral movement. Necrosis of the cartilage and non-union of the graft with surrounding tissue have also been seen [11].
Osteochondral autografts are an attractive method of treatment of medium- and small-sized chondral and osteochondral lesions of the knee. The beauty of the technique is in its capability to restore the articular geometry and the subchondral bone as a single-step procedure that is easily reproducible and relatively inexpensive.
The success of the procedure depends on the correct selection of the patient. There have been various studies to determine the best outcomes of this procedure. If one considers the patient demographics to be taken into consideration, then we would need to look into the following parameters:
Size of the defect
Site of the defect
Age of the patient
Return to sport
The size and site of the chondral or osteochondral defect is probably the most important determinant of success of the procedure. It is accepted that the smaller the defect size, the better the outcome. Gudas et al. reported that the lesions that were less than 2 cm2 reported better outcomes with osteochondral transfer than similar lesions treated with microfracture [21]. Krych looked at his patient cohort of 96 who had lesion sizes ranging from 1 to 6 cm2 with a mean size of 2.65 cm2 [22]. He did not find any differences within the lesion sizes but demonstrated the efficacy of osteochondral autografts over microfracture for all lesion sizes. Gudas et al. also documented that defect sizes that were less than 2.8 cm2 were associated with better outcomes than larger lesions [23, 24].
There are a few levels I and II studies published that compare the efficacy of osteochondral autografts with microfracture and/or autologous cartilage implantation. The technique of osteochondral autografts has been found to be consistently superior for lesions that are on an average less than 3 cm2. Horas et al. looked at lesions in 40 patients that were randomized to receive either osteoarticular autografts or an Autologous Chondrocyte Implantation (ACI). The mean size was 3.75 cm2. They conducted post-treatment 2-year biopsies on representative patients from each group that showed predominant fibrocartilage fill of the ACI patients and hyaline character in osteoarticular autograft patients. Both group patients had resolution and had a decrease in their symptoms, but the ACI group showed slower progress as compared to the osteoarticular autograft group [18] Bentley et al. looked at 100 patients with a mean defect size of 4.66 cm2 with a mean follow-up of 19 months. Functional and clinical assessments showed superiority of ACI over osteoarticular autografts (88 vs. 68 % excellent results, respectively) [25]. The efficacy of osteoarticular autografts has been proven to be superior to microfracture in terms of quality of cartilage formed and return to sport as well as the satisfaction rates.
The currently available commercial systems allow for single-donor plugs of 2.7-, 3.5-, 4.5-, 6.5-, 8- and 10-mm diameter. When tackling lesions that are greater than 4 cm2, one needs to use more than one plug. This presents with certain unique peculiarities. Thus, it is safe to conclude that in lesions up to 3 cm2, osteoarticular autograft is the preferred treatment option to microfracture as well ACI [26].
The lesions that are treated most commonly affect the medial femoral condyle. The lateral femoral condyle is probably the next most commonly treated site followed by the trochlea, patella and the tibia [27, 28]. The same findings were echoed in our clinical experience as well. Patellar osteochondral defects are particularly not favourable for osteoarticular autografts since there is difference in the morphology of the cartilage of the patella and the donor site. The differences of structural orientation, cartilage thickness and stress shear patterns make the osteoarticular autograft technique less suitable for the patella. The femoral condyle defects report the best outcomes of this procedure.
Chondral and osteochondral injuries most frequently occur with medium- to high-velocity injuries. There is injury and tearing of ligaments associated with these injuries. A significant proportion of these may be in high-level athletes. Gudas reported in his series of elite athletes that 82 % were able to return to the same level of sport. The type of cartilage treatment determined the time for returning to sport. The group with ACL reconstruction with osteochondral autograft recovered the fastest with a mean time of return to sport at 10.2 months, as against 11.1 and 11.5 months for the ACL reconstruction with microfracture and ACL reconstruction with debridement groups, respectively [19].
For adequate outcomes of chondral and osteochondral defects, it is necessary to obtain a stable joint and a well-aligned joint. The results of osteochondral autograft treatment in malaligned or unstable knees are poorer than in stable and aligned knees [29]. The importance of this observation is that many times, osteochondral defects are discovered incidentally at the time of arthroscopy and the surgeon should be prepared for treating the same adequately.
There is paucity of levels I and II studies as regards the long-term results of osteochondral autografts. Gudas reported on 10-year outcomes of cartilage procedure in athletes and showed that 75 % of athletes treated with osteochondral autografts could engage in sport as compared to about 37 % athletes treated with microfracture [19]. Ulstein also reported on 10-year outcomes in a non-athletic population [26]. He did not find any difference between microfracture and osteochondral autografts. He also reported that the microfracture group (54 %) had more incidences of re-operations as compared to osteochondral autografts (36 %).
Osteoarticular autografts have also been used to cover defects in the patella, tibia, capitellum, talus and the hip with varying degrees of success [30–32].
Conclusions
Osteochondral autologous transfer surgery delivers viable hyaline cartilage to a damaged articular surface in a weight-bearing region of the knee in a single-stage procedure. There are many treatment options for isolated symptomatic femoral condyle defects. Ideally, chondral repair should be considered in cases of deep local loss of cartilage (ICRS grades III and IV) with painful knee and associated injuries. Lesions smaller than 1 cm2 can be left alone and observed. Autografts work well when they cover less than 3 cm2 of defects and the graft provides maximum coverage and press-fit stability. Any misalignment of the limb beyond 5° and any associated intra-articular injury need to be addressed simultaneously to ensure a good result. Current evidence shows improved clinical outcomes with the osteochondral autograft technique when compared with preoperative conditions. Further high-quality prospective studies are necessary to develop an algorithm for management and intervention of articular cartilage defects.
Acknowledgments
Compliance with Ethics Guidelines
ᅟ
Conflict of Interest
Dr. Tapasvi reports grants and personal fees received from Smith & Nephew.
Dr. Patil has nothing to disclose.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Footnotes
This article is part of the Topical Collection on Cartilage Repair Techniques in the Knee
Contributor Information
Shantanu Patil, Phone: +91 70301 427 27, Email: shantanusp@gmail.com.
Sachin R. Tapasvi, Phone: +91 98220 18871, Email: stapasvi@gmail.com
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
- 1.Buckwalter JA, Mankin HJ. Articular cartilage degeneration and osteoarthritis, repair, regeneration and transplantation. Instr Course Lect. 1998;47:487–504. [PubMed] [Google Scholar]
- 2.Mithoefer K, McAdams T, Williams RJ, Kreuz PC, Mandelbaum BR. Clinical efficacy of the microfracture technique for articular cartilage repair in the knee: an evidence-based systematic analysis. Am J Sports Med. 2009;37(10):2053–2063. doi: 10.1177/0363546508328414. [DOI] [PubMed] [Google Scholar]
- 3.Curl W, Krome J, Gordon ES, Rusching J, Smith BP, Poehling GG. Cartilage injuries: a review of 31,516 knee arthroscopies. Arthroscopy. 1997;13:456–460. doi: 10.1016/S0749-8063(97)90124-9. [DOI] [PubMed] [Google Scholar]
- 4.Steadman JR, Rodkey WG, Singleton SB, Briggs KK. Microfracture technique for full thickness chondral defects: technique and clinical results. Oper Tech Orthop. 1997;7:300–304. doi: 10.1016/S1048-6666(97)80033-X. [DOI] [Google Scholar]
- 5.Zheng MH, Willers C, Kirilak L, Yates P, Xu J, Wood D, et al. Matrix-induced autologous chondrocyte implantation (MACI): biological and histological assessment. Tissue Eng. 2007;13(4):737–746. doi: 10.1089/ten.2006.0246. [DOI] [PubMed] [Google Scholar]
- 6.Outerbridge KK, Outerbridge AR, Outerbridge RE. The use of a lateral patellar autologous graft for the repair of a large osteochondral defect of the knee. J Bone Joint Surg. 1995;77:65–72. doi: 10.2106/00004623-199501000-00009. [DOI] [PubMed] [Google Scholar]
- 7.Müller W. Osteochondritis dissecans. In: Hastings DE, editor. Progress in orthopaedic surgery, vol. 3. Springer-Verlag; 1978. p. 135–6.
- 8.Bobic V. Arthroscopic osteochondral autograft transplantation in ACL reconstruction: a preliminary clinical study. Knee Surg Sports Traumatol Arthrosc. 1996;3:262–264. doi: 10.1007/BF01466630. [DOI] [PubMed] [Google Scholar]
- 9.•.Hangody L, Kish G, Karpati Z. Arthroscopic autogenous osteochondral mosaicplasty for the treatment of femoral condylar articular defect. Knee Surg Sports Traumatol Arthrosc. 1997;5:262–267. doi: 10.1007/s001670050061. [DOI] [PubMed] [Google Scholar]
- 10.Pearce SG, Hurtig MB, Clarnette R, Kalra M, Cowan B, Miniaci A. An investigation of 2 techniques for optimizing joint surface congruency using multiple osteochondral autografts. Arthroscopy. 2001;17:50–55. doi: 10.1053/jars.2001.19966. [DOI] [PubMed] [Google Scholar]
- 11.Patil S, Butcher W, D’Lima DD, Steklov N, Bugbee WD, Hoenecke HR. Effect of osteochondral graft insertion forces on chondrocyte viability. Am J Sports Med. 2008;36:1726–1732. doi: 10.1177/0363546508316765. [DOI] [PubMed] [Google Scholar]
- 12.Huang FS, Simonean PT, Norman AG, Clark JM. Effects of small incongruities in a sheep model of osteochondral grafting. Am J Sports Med. 2004;32:1842–1848. doi: 10.1177/0363546504264895. [DOI] [PubMed] [Google Scholar]
- 13.Ahmad C, Guiney WB, Drinkwater CJ. Evaluation of site intrinsic healing response in autologous osteochondral grafting of the knee. Arthroscopy. 2002;18:95–98. doi: 10.1053/jars.2002.25967. [DOI] [PubMed] [Google Scholar]
- 14.•.Hangody L, Vasarhelyi G, Hangody LR, Sukosd Z, Tibay G, Bartha L, et al. Autologous osteochondral grafting, technique and long-term results. Injury. 2008;39S1:S32–S39. doi: 10.1016/j.injury.2008.01.041. [DOI] [PubMed] [Google Scholar]
- 15.Jacob R, Franz T, Gautier E, Mainil Varlet P. Autologous osteochondral grafting in the knee: indications results and reflections. Clin Orthop. 2002;401:170–184. doi: 10.1097/00003086-200208000-00020. [DOI] [PubMed] [Google Scholar]
- 16.Chow JCY, Hantes ME, Houle JB, Zalavras CG. Arthroscopic autogenous osteochondral transplantation for treating knee cartilage defect: a 2-to-5-year follow-up study. Arthroscopy. 2004;7:681–690. doi: 10.1016/S0749-8063(04)00590-0. [DOI] [PubMed] [Google Scholar]
- 17.•.Gudas R, Gudaite A, Pocius A, et al. Ten-year follow-up of a prospective, randomized clinical study of mosaic osteochondral autologous transplantation versus microfracture for the treatment of osteochondral defects in the knee joint of athletes. Am J Sports Med. 2012;40(11):2499–2508. doi: 10.1177/0363546512458763. [DOI] [PubMed] [Google Scholar]
- 18.Horas U, Pelinkovic D, Herr G, Aigner T, Schnettler R. Autologous chondrocyte implantation and osteochondral cylinder transplantation in cartilage repair of the knee joint. A prospective, comparative trial. J Bone Joint Surg Am. 2003;85-A(2):185–192. doi: 10.2106/00004623-200302000-00001. [DOI] [PubMed] [Google Scholar]
- 19.Gudas R, Stankevicius E, Monastyreckiene E, Pranys D, Kalesinskas RJ. Osteochondral autologous transplantation versus microfracture for the treatment of articular cartilage defects in the knee joint in athletes. Knee Surg Sports Traumatol Arthrosc. 2006;14(9):834–842. doi: 10.1007/s00167-006-0067-0. [DOI] [PubMed] [Google Scholar]
- 20.Lane JG, Massie JB, Ball ST, Amiel ME, Chen AC, Bae WC, et al. Follow-up of osteochondral plug transfers in a goat model: a 6-month study. Am J Sports Med. 2004;32(6):1440–1450. doi: 10.1177/0363546504263945. [DOI] [PubMed] [Google Scholar]
- 21.Gudas R, Gudaitė A, Mickevičius T, et al. Comparison of osteochondral autologous transplantation, microfracture, or debridement techniques in articular cartilage lesions associated with anterior cruciate ligament injury: a prospective study with a 3-year follow-up. Arthroscopy. 2012. [DOI] [PubMed]
- 22.Krych AJ, Harnly HW, Rodeo SA, Williams RJ. Activity levels are higher after osteochondral autograft transfer mosaicplasty than after microfracture for articular cartilage defects of the knee: a retrospective comparative study. J Bone Joint Surg Am. 2012;94(11):971–978. doi: 10.2106/JBJS.K.00815. [DOI] [PubMed] [Google Scholar]
- 23.Gudas R, Kalesinskas RJ, Kimtys V, et al. A prospective randomized clinical study of mosaic osteochondral autologous transplantation versus microfracture for the treatment of osteochondral defects in the knee joint in young athletes. Arthroscopy. 2005;21(9):1066–1075. doi: 10.1016/j.arthro.2005.06.018. [DOI] [PubMed] [Google Scholar]
- 24.Gudas R, Simonaityte R, Cekanauskas E, Tamosiūnas R. A prospective, randomized clinical study of osteochondral autologous transplantation versus microfracture for the treatment of osteochondritis dissecans in the knee joint in children. J Pediatr Orthop. 2009;29(7):741–748. doi: 10.1097/BPO.0b013e3181b8f6c7. [DOI] [PubMed] [Google Scholar]
- 25.Bentley G, Biant LC, Carrington RWJ, et al. A prospective, randomized comparison of autologous chondrocyte implantation versus mosaicplasty for osteochondral defects in the knee. J Bone Joint Surg (Br) 2003;85(2):223–230. doi: 10.1302/0301-620X.85B2.13543. [DOI] [PubMed] [Google Scholar]
- 26.Ulstein S, Årøen A, Røtterud JH, Løken S, Engebretsen L, Heir S. Microfracture technique versus osteochondral autologous transplantation mosaicplasty in patients with articular chondral lesions of the knee: a prospective randomized trial with long-term follow-up. Knee Surg Sports Traumatol Arthrosc. 2014;22(6):1207–1215. doi: 10.1007/s00167-014-2843-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dozin B, Malpeli M, Cancedda R, et al. Comparative evaluation of autologous chondrocyte implantation and mosaicplasty: a multicenter randomized clinical trial. Clin J Sport Med. 2005;15(4):220–226. doi: 10.1097/01.jsm.0000171882.66432.80. [DOI] [PubMed] [Google Scholar]
- 28.Lim H-C, Bae J-H, Song S-H, Park Y-E, Kim S-J. Current treatments of isolated articular cartilage lesions of the knee achieve similar outcomes. Clin Orthop Relat Res. 2012;470(8):2261–2267. doi: 10.1007/s11999-012-2304-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Worthen J, Waterman BR, Davidson PA, Lubowitz JH. Limitations and sources of bias in clinical knee cartilage research. Arthroscopy. 2012;28(9):1315–1325. doi: 10.1016/j.arthro.2012.02.022. [DOI] [PubMed] [Google Scholar]
- 30.Ovesen J, Olsen BS, Johannsen HV. The clinical outcomes of mosaicplasty in the treatment of osteochondritis dissecans of the distal humeral capitellum of young athletes. J Shoulder Elb Surg. 2011;20(5):813–818. doi: 10.1016/j.jse.2010.09.001. [DOI] [PubMed] [Google Scholar]
- 31.Vannini F, Cavallo M, Baldassarri M, Castagnini F, Olivieri A, Ferranti E, et al. Treatment of juvenile osteochondritis dissecans of the talus: current concepts review. Joints. 2015;2(4):188–191. [PMC free article] [PubMed] [Google Scholar]
- 32.Gagala J, Tarczyńska M, Gawęda K. Clinical and radiological outcomes of treatment of avascular necrosis of the femoral head using autologous osteochondral transfer (mosaicplasty): preliminary report. Int Orthop. 2013;37(7):1239–1244. doi: 10.1007/s00264-013-1893-6. [DOI] [PMC free article] [PubMed] [Google Scholar]


