Abstract
Revision total knee arthroplasty (TKA) represents a technically challenging procedure. The use of an offset stem extension can help in addressing some of the difficulties that can be encountered during surgery and, in particular, anatomical mismatch, malalignment, and gap balancing. Different offset stem extensions are available and can be classified according to four parameters: modularity, location of the offset, direction, and size of the displacement. Offset stem extensions can assist with implant alignment on the metaphysis if there is an offset diaphysis, can avoid medial-lateral or anterior-posterior component overhang, can reduce the incidence of coronal or sagittal malalignment, and can help in balancing the flexion and extension spaces by effectively translating the components. The aim of this study is to give an overview of the currently available evidence regarding the use of offset stem extensions in revision TKA as well as some useful surgical tips.
Keywords: Knee arthroplasty, Revision, Offset stem, Stem extension
Introduction
Revision total knee arthroplasty (TKA), either for septic or aseptic causes, oftentimes poses additional challenges to restoring stable, well-balanced, and well-fixed implants. In particular, revision TKA aims to restore bone stock, long-term stability of implants, and, possibly, immediate weight-bearing and functional activity. However, the removal of a previously well-fixed prosthesis can produce a loss of bone mass between the distal femur and the proximal tibia. These large bone defects and compromised bone stock can thus make reconstruction and fixation highly challenging [1]. Achieving solid fixation of revision implants is essential to ensure early postoperative mobilization and rehabilitation and to improve the longevity of the construct [2, 3]. Hence, an accurate preoperative radiographic classification of the severity of the bone defect based on the location of the defect and the bone quality is paramount. Among the various classification systems, the Anderson Orthopaedic Research Institute (AORI) classification is the most commonly used system for treating revision TKA with bone loss [4]. However, this classification system helps surgeons only to establish whether they will have to manage an intact, a damaged, or a deficient tibial and femoral condyle. In cases involving bone loss, though, this classification is not enough to guarantee a successful revision TKA. Indeed, in revisions, the femoral and tibial bone quality (viable or sclerotic) and the location of the defect are crucial aspects to consider when having to choose the grade of fixation. Accordingly, both the distal femur and proximal tibia can be divided into three anatomical zones in which fixation can be achieved: the joint surface or epiphysis (zone 1), the metaphysis (zone 2), and the diaphysis (zone 3). Achieving a solid implant requires that fixation be applied in at least two of these three zones, thereby highlighting the importance of preoperative planning and implant selection [5•].
The concept of zonal fixation provides a working methodology applicable to both the tibia and the femur when planning revision total knee replacement. During the preoperative planning, three questions need to be addressed: which zones are available for fixation, which fixation method is appropriate, and, finally, which implants are best suited to the case. For example, when the bone is deficient or the metaphysis needs to be stabilized, it is desirable to transfer stress from the joint to the tibial and femoral diaphysis (zone 3) and to shield any residual metaphysis.
A valuable option in zonal fixation in revision TKA is the use of stemmed implants. Practically, stems confer stability to the construct also when we stabilize the metaphysis. Indeed, they distribute load away from the femoral condyles and tibial plateau [6], thereby not only protecting damaged bone in these areas from mechanical overload and failure but also reducing stress on critical implant interfaces in these locations [7]. Another practical advantage of stems is that they allow surgeons to bypass bone defects on the distal femur and proximal tibia, thereby reducing the risk of bone collapse or periprosthetic fracture. Biomechanically, stems reduce bone stress by 30 %, increase support to axial and bending loads, and reduce micromotion of wedges or augments at the interfaces [8]. Further, stems often help surgeons to optimize implant alignment and the mechanical axis of the limb [9, 10]. Lastly, they also provide an expanded interface for cemented or uncemented implant fixation to the bone. Although the use of stems has few drawbacks—including the difficulties encountered by surgeons in removing them as opposed to non-stemmed implants—the general consensus among surgeons is that in revision TKA, they can reduce the risk of mechanical implant failure [11]. These results, in addition to the theoretical advantages of stems outlined above, have made their use mandatory in revision TKA. However, in some patients, the distal femur and proximal tibia in revision TKA may be shaped in such a way that the relationship between the articular surface and the diaphysis imposes a stem pathway that does not allow the use of standard straight stems. Offset stems offer a sound solution to this problem. This paper highlighted the need for offset stems in revision TKA focusing on the classification of the offset stems, on their basic indications, on the surgical technique, and on the reported outcomes presented in the recent scientific literature.
Stem types
The various different types of stems currently available reflect the varying perspectives among surgeons on their purposes and optimal uses. For instance, whereas some polished stems can be used with both cemented and uncemented stem fixations, others are designed exclusively for either one or the other usage. Cemented stems are versatile and can be used in a wide variety of femoral and tibial geometries because cement provides excellent fixation even when the bone and stem geometries are quite different [12]. One major advantage of cemented stems is that their placement is less constrained by bone geometry. In particular, when a diaphyseal engagement could cause implant malalignment due to a deformed diapyhsis. Indeed, they can be inserted inside the medullary canal without altering the position of the implant. Equally important is that cemented stems can be shorter than uncemented press-fit stems because they do not need to engage the diaphysis. Accordingly, they are suitable for patients with a poor diaphyseal bone structure and large canal diameter. Unsurprisingly, they have proven useful either in patients whose canal geometry renders press-fit uncemented stems unreliable or in patients with sclerotic or damaged metaphyseal bone, a bone condition that results in inadequate fixation requiring extension of cementing into the diaphyseal canal [13].
Unlike cemented stems, uncemented press-fit stems are indicated in patients either with good diaphyseal bone and favorable canal geometry or with periprosthetic fracture. In addition, press-fit stems by engaging the diaphysis are also effective in correcting limb alignment. Despite their effectiveness in diaphyseal stem fixation, press-fit stems may give rise to problems, including the need for offset capability when diaphyseal engagement causes implant malalignment, as well as iatrogenic fracture and end of stem pain. Finally, uncemented stems appear to have less of an effect on metaphyseal bone density, although radiolucent lines of uncertain significance can develop around stems over time [14, 15].
Although in the past most stems were an integral part of the femoral or tibial component, in most cases, they are now separate modular devices which are fixed to the condylar femoral or tibial portion of the implant with bolts, tapers, or both. Despite having many practical advantages, as for instance the need for a smaller inventory, modular stems do introduce new areas of weakness, and, hence, potential failure locations, into implants. Stems, which may be made of various metals, including cobalt-chromium or titanium, have different surface finishing ranging from smooth to rough to porous coated. Moreover, they also have varied geometrical features including slots (designed to reduce rigidity), flutes (designed to enhance fixation), kinks (designed to accommodate different bony geometries), and bows (designed to accommodate the bowed femoral diaphysis). Therefore, achieving a successful stem fixation in revision TKA requires a preoperative templating on both the anterior-posterior and lateral view so as to choose the proper stem length, diameter, alignment, and need for offset stems.
Offset stems
The offset is defined as the distance between the center of the tibial or femoral metaphysis and the center of the tibial or femoral diaphysis [16]. Different offset stem extensions are available from different manufacturers. Four parameters can be used in order to classify an offset stem: modularity, location of the offset, direction, and size of the displacement (Table 1). A first distinction can be made between non-modular and modular systems. In non-modular systems, the offset displacement is intrinsic to the structure of the stem extension. On the contrary, in modular systems, the offset is not an integral part of the stem extension structure but it derives from a coupler which allows to move the component anterior/posterior or medial/lateral relative to the stem. A second distinction can be made basing on the offset location. The offset can be positioned at the junction between the main body of the stem and its attachment point to the prosthesis base or between the main body of the stem and its extension. Finally, offset stems differ for the direction and size of tibial/femoral component displacement that can be obtained. With regard to the direction, in some prosthesis, only defined directions of displacement are allowed (i.e., medial, lateral, anterior, posterior) while in others, a 360° arc displacement is available. With regard to the size, in some prosthesis, a series of offset size is available while in others, only one offset size is available. In particular, the tibial offset options are 2, 4, 6, and 8 mm for Triathlon TS (Stryker, Mahwah, NJ); 2, 4, and 6 mm for Legion (Smith&Nephew, Memphis, TN); neutral and 2.5 and 5 mm for Vanguard (Biomet);, 4 mm for TC3 Sigma (DePuy, Warsaw, IN); and 4.5 mm for LCCK (Zimmer, Warsaw, IN). The femoral offset options are 2 and 4 mm for Triathlon TS (Stryker, Mahwah, NJ); 2, 4, and 6 mm for Legion (Smith&Nephew, Memphis, TN); 2 and 4 mm for TC3 Sigma (DePuy, Warsaw, IN); and 4.5 mm for LCCK (Zimmer, Warsaw, IN).
Table 1.
Classification of offset stem extensions
| Modularity | Non-modular | Modular | |||||
| Location | Stem/platform | Stem/stem extension | |||||
| Direction | Defined direction (ant, post, med, lat) | 360° arc | |||||
| Size (mm) | 2 | 2.5 | 4 | 4.5 | 5 | 6 | 8 |
Indications
Revision TKA represents a technically challenging procedure. The use of an offset stem can help in addressing some of the difficulties that can be encountered during surgery. The indications for an offset stem are three: (1) anatomical mismatch, (2) malalignment, and (3) gap balancing.
Anatomical mismatch
If a stem extension is used, component position will be dictated by the position of the intramedullary rod. Offset stems can facilitate implant alignment on the metaphysis if there is an offset diaphysis and avoid medial-lateral or anterior-posterior component overhang [17] (Fig. 1). Different studies have showed that the center of the metaphysis is not always coincident with the center of the diaphysis in particular in the tibial side. Hicks et al. observed a variability in the location of the tibial canal of 1–15 mm from any direction to the center of the tibial component [16]. Because of the variations in anatomy, the use of a straight stem is not always possible and can lead to a poor coverage of the proximal part of the tibia and overhang of the tibial tray, coronal or sagittal malalignment of the mechanical axis of the knee, and non-filling of the tibial canal [18–20]. Therefore, in order to achieve maximal coverage of the tibial plateau without overhang and a well-centered stem, a tibial component with an offset stem is often needed. This is particularly important when a hybrid fixation technique is used. Cortical contact is paramount for press-fit cementless stems. With a canal-filling stem, there will be medial overhang of the tibial tray unless an offset stem is used [19]. In a cadaveric study of 20 tibiae which were instrumented with a revision canal-filling uncemented stem, Abraham et al. [19] measured an average offset of 4.1 mm posterolateral to the metaphyseal center. They concluded that a wide range of offsets are necessary for optimal placement of the prosthesis. Offset stems are especially valuable after a previous distal femoral or proximal tibial osteotomy, when the metaphyseal portion of the bone may not be directly centered over the diaphysis [17]. A previous fracture and growth deficiency represents other conditions that generate an anatomical metaphyseal/diaphyseal mismatch and that can be well addressed with an offset stem [21].
Fig. 1.

On the left, it is shown the typical mismatch between tibial metaphysis and diaphysis centers. On the right, an implanted tibial component with a lateral tibial offset stem extension to accomodate tibial natural anatomy
Malalignment
The ability to achieve a proper coronal alignment in revision TKA is critical to the success of the procedure and directly influences the clinical outcome and the survivorship of the implant [22, 23]. Several studies reported that failure in obtaining a correct alignment represents one of the major causes of aseptic loosening [24, 25]. However, although critical for the success of the procedure, a correct mechanical alignment is difficult to obtain in the revision setting due to significant metaphyseal bone defects and soft tissue alterations that are often present [26]. When uncemented press-fit stems are used, the alignment of the component is dictated by the axis of the diaphyseal bone. The use of an offset stem can facilitate the correction of varus/valgus malalignment as demonstrated by the work of Nakasone et al. [26].
Gap balancing
In revision TKA, the elevation of the joint line is a common occurrence associated with poorer clinical and functional results [27, 28]. Different studies have demonstrated the detrimental effect of joint line elevation on range of motion, extensor strength, anterior knee pain, patellar stability, and mid-flexion stability [27–29, 30•]. During revision surgery, the flexion space is generally wider than extension space because the capsuloligamentous structures that control flexion instability (in particular the anterior longitudinal portion of the medial collateral ligament) are more damaged than those that control the knee in extension. In this scenario, in order to balance the flexion-extension space, the surgeon may choose to fill up the flexion space by using a thicker insert and perform a compensatory increase of the extension space by resecting additional distal femur, resulting in a proximalization of the femoral component and elevation of the joint line [31]. The use of a straight femoral stem may contribute to increase this tendency towards an excessive flexion space [32]. The position of a diaphyseal press-fit femoral stem determines both mediolateral and antero-posterior position of the condylar portion of the femoral component. The majority of stems are attached to the femoral component at a fixed valgus angle of 5°–7° in the coronal plane and perpendicular in the sagittal plane [30•]. Since the distal femur is bowed anteriorly, a straight diaphyseal press-fit stem would be expected to displace the femoral component anteriorly, thus increasing even more the flexion space [30•]. The use of an offset femoral stem allows to fill in the flexion space without elevating the joint line by restoring the posterior condylar offset (Fig. 2). Using an offset stem permits to displace the femoral component as posterior as possible, thus reducing the flexion gap with central stem positioning within the femoral canal [30•] (Fig. 3). Moreover, Brilhault et al. in a cadaveric study simulated the position of a press-fit stemmed revision femoral component [33]. They demonstrated that every diaphyseal-engaging stem required the use of a posterior offset coupler to achieve engagement in the femoral isthmus.
Fig. 2.
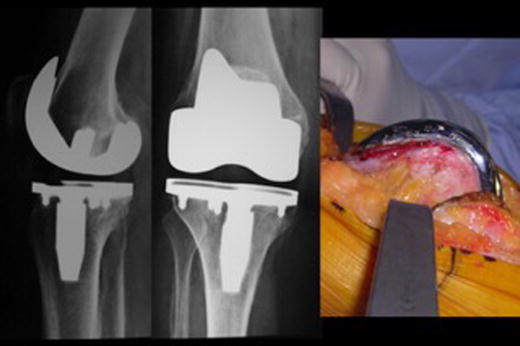
On the left, lateral and AP preoperative views of a painful stiff TKA. On the right, intraoperative sagittal femoral view showing the amount of anteriorization of the femoral component resulting in overstuffed extensor mechanism and flexion instability duo to reduced posterior femoral condylar offset
Fig. 3.

Postoperative AP and lateral view of the revision TKA which addressed the cause of TKA failure by posteriorizing the femoral component. This will simultaneously fill the flexion gap and relief the extensor mechanism
Surgical technique
Surgical technique begins with preoperative planning on radiograms. The evaluation of stem extension’s position on the radiogram should take into account various angles and axis. In particular, the relationship between the mechanical axis (MA) of the single bones (femur and tibia) and the angle formed with the distal femoral anatomical axis (dFA) generates the anatomical-to-mechanical axis (AMA) which is utilized by the surgeon for his intraoperative correction. Planning on the radiograms provides useful information on entry point levels relative both to the center of the metaphysis and to the parts of the previous implant (box, corners, stems). When planning the implant position on the femur relative to the AMA, surgeons should take into account the fixed angle between the metaphyseal part and the diaphyseal part of the implant, which is approximately 6°. If AMA is 6° ± 2°, no modifications from the planned standard entry point drawn in the planning should be made. If the AMA is significantly different, it is possible to move in the varus or valgus direction the final implant position. Moving towards the lateral side of the joint produces a valgus additional alignment, while moving medially produces additional varus. Reaming diaphyseal canals by hand does not permit to drive the proper direction of the reamer because the power of reaming is concentrated by the surgeon on torquing the reamer instead of displacing it. Power reaming is recommended to impose the reaming direction dictated by the planning.
Common mistakes in reaming directions are made on the sagittal plane. Typically, on the femoral side, flexion position of the stem extension is generated by the procurvatum of the femur with consequent tip of the stem impinging on the anterior femoral cortex and undersize of the final stem diameter. On the tibial side, again, flexion direction of the reaming is facilitated by difference in bone density between the anterior medullary bone of the tibia (usually harder) and the posterior medullary bone. This will generate a flexed position of the stem with additional degrees of implant slope. The need for an offset in the sagittal plane for the tibia is often related to incorrect reaming direction. On the femoral side, due to the sagittal procurvatum, a long cementless stem extension drives the metaphyseal portion of the implant anteriorly. In particular, if the stem is longer than 190–200 mm in females or 210–250 in men (combined length), the posterior offset may become a need in order to seat the trochlea of the femoral component properly on the anterior cortex. Alternatively, the femur is anteriorized and an anterior modular femoral augment is needed together with a bigger femoral size to balance an enlarged flexion gap.
Offset tibial preparation
On the tibial side, offset stems can be utilized with an instrumented technique which will assist the surgeon in positioning the tibial platform and the stem extension. Canal is prepared with power reaming, and the stem trial is left in place. The tibial finishing guide is positioned on the tibial surface after the tibial refining cut has been made. The tibial finishing guide and the stem are combined with an offset bushing which will rotate with the tibial guide until it will match the best position according to the plateau coverage and to proper rotational alignment. The tibial guide can then be fixed, and the tibial keel can be prepared. If there is a central cavitary defect in the tibia, the surgeon can use stem extensions after preparing the canal using a “manual technique” which implies the positioning of the trial tibial implant loosely connected to the offset stem extension which finds the final position by itself. After impacting the component onto the surface, the connecting screw can be locked and this will make the final implant-to-stem offset relationship which will be replicated on the final component before being cemented.
Offset femoral preparation
After femoral canal reaming, the stem extension trial is left in place and the femoral finishing guide will be positioned on the metaphysis according to the best medial-lateral coverage. A mismatch between the stem and the center of the guide will be managed by a specific guide which will be represented by a rotating bushing by most of the available systems. If this offset is within the offset system capabilities which on average are around 5 mm, finishing femoral cuts can be done. The trial and the final femoral components can then be inserted with the specific femoral offset. Preparation of the posterior femoral offset is usually done manually. After preparing the intercondylar box of the implant, additional bone can be removed with a reamer directed towards the posterior cortex and this space will be occupied by the stem offset. Similarly to the tibia, when a central cavitary defect is present on the femur, a non-instrumented preparation for the femoral offset can be done. After inserting the trial offset stem into the diaphysis, the surgeon will judge if the metaphyseal part of the implant is in an acceptable position or not. Possible modifications of the metaphyseal position can be done with reaming direction or offset redirectioning.
Reported outcomes
There is a paucity of information available in literature about clinical and radiological outcomes of revision TKA with the use of offset stem extensions. PubMed and EMBASE databases were searched for relevant studies up to 1 July 2015, using the combined terms “revision total knee arthroplasty” and “offset.” At the first electronic search, we identified 26 relevant publications. Two authors (G.B. and V.F.) independently reviewed the content of each abstract. Once an article was identified as likely to be included, full-text versions were obtained to evaluate the exact content of the study. Studies focusing on clinical or radiological outcome of offset stem extensions were included in this review. Eventually, only four publications relevant to the topic were included. Nakasone et al. performed a retrospective radiographic study of the component alignment in a series of 52 revision TKAs using a diaphyseal-engaging, modular offset, press-fit stem [26]. The canal-fill ratio (CFR) was calculated by dividing the stem diameter by the endosteal diameter at the stem tip and correlated with anatomic alignment. A near ideal femoral and tibial component alignment was observed in all patients with a narrow range of variation. Specifically, the mean pre-revision AP femoral component angle was 8.6° of valgus (range 10° varus–35° valgus), while the mean post-revision value was 6.5° of valgus (range 1.3° valgus–10° valgus). The mean pre-revision AP tibial component angle was 1.4° of varus (range 14° varus–4.3° valgus), while the mean post-revision value was 0.5° of valgus (range 1.9° varus–3.9° valgus). In the coronal plane, the mean post-revision canal-fill ratio (CFR; calculated by dividing the stem diameter by the endosteal diameter at the stem tip) was 93 % for the femur and 91 % for the tibia. In the sagittal plane, the CFR was 82 % and 87 % for the femur and tibia, respectively. The authors concluded that the use of this type of stem facilitate accurate alignment for both femoral and tibial components. Brilhault et al. recently compared 91 revision TKAs with femoral straight stems with 35 revision TKAs with femoral offset stems. After a mean follow-up of 4.5 years, they concluded that the use of offset stems is associated with a better restoration of the posterior condylar offset and a better coronal alignment of the stem within the intramedullary femoral canal [30•]. Innocenti et al. retrospectively reviewed a series of 40 revision TKAs, 25 with posterior offset femoral stem and 15 with a straight stem, after a mean follow-up of 3.5 years [31]. The posterior offset stem provided increased posterior condylar offset, balancing a wider flexion space, allowing better position of the stem into the femoral canal and restoring accurately the joint line. In particular, in the offset stem knees, the mean intended joint line position was 0.9 mm as compared with 3.2 mm for the straight stem knees. Clinically, the knee score improved from an average of 33 points preoperatively to 83 at the final follow-up. The functional score improved from 31 point to 82, while the mean total flexion arc improved from 54° to 108°. However, despite improvements in radiographic parameters, the use of posterior femoral offset did not provide better clinical results. Mahoney et al. retrospectively analyzed 22 femur revision cases using modular offsets and reported a mean postoperative joint line height 1.6 mm distal to baseline [29]. One year after surgery, the mean range of motion was 105.1° ± 16.9, and KSS pain score was 46.5 ± 6.1. Twelve of 20 patients were pain free, and 18 of 20 had KSS pain scores >45, indicating no more than occasional pain.
Conclusions
In the surgeon’s armamentarium for revision TKA, offset stems have a crucial role. The development of a growing number of modular options allows the surgeon to personalize fixation and position to nearly every revision scenario. Offsetting the position of the metaphysis relatively to the dyaphisis can be mandatory and related to anatomical features, or it can represent a surgeon’s strategy to accommodate the implant position to his reconstructive strategies. Results of revision TKA with offset stem extensions have now withstand the mid-term demonstrating good results and no complications specific to their use. Design refinements and the search for a proximal fixation at the metaphyseal level will drive the evolution of diaphyseal expansions in the future.
Compliance with Ethics Guidelines
Conflict of Interest
Giovanni Balato and Vincenzo Franceschini declare that they have no conflict of interest. Andrea Baldini is a consultant with ZimmerBiomet with speaker agreement.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Footnotes
This article is part of the Topical Collection on Revision Knee Arthroplasty
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
- 1.Engh GA, Ammeen DJ. Bone loss with revision total knee arthroplasty: defect classification and alternatives for reconstruction. Instr Course Lect. 1999;48:167–75. [PubMed] [Google Scholar]
- 2.Vince KG, Long W. Revision knee arthroplasty. The limits of press fit medullary fixation. Clin Orthop Relat Res. 1995;317:172–7. [PubMed] [Google Scholar]
- 3.Dalury DF, Pomeroy DL, Gorab RS, Adams MJ. Why are total knee arthroplasties being revised? J Arthroplasty. 2013;28(8 Supp):120–1. doi: 10.1016/j.arth.2013.04.051. [DOI] [PubMed] [Google Scholar]
- 4.Engh GA, Parks NL. The management of bone defects in revision total knee arthroplasty. Instr Course Lect. 1997;46:227–36. [PubMed] [Google Scholar]
- 5.•.Morgan-Jones R, Oussedik SI, Graichen H, Haddad FS. Zonal fixation in revision total knee arthroplasty. Bone Joint J. 2015;97-B(2):147–9. doi: 10.1302/0301-620X.97B2.34144. [DOI] [PubMed] [Google Scholar]
- 6.Bourne RB, Finlay JB. The influence of tibial component intramedullary stems and implant-cortex contact on the strain distribution of the proximal tibia following total knee arthroplasty. An in vitro study. Clin Orthop Relat Res. 1986;208:95–9. [PubMed] [Google Scholar]
- 7.Mabry TM, Hanssen AD. The role of stems and augments for bone loss in revision knee arthroplasty. J Arthroplasty. 2007;22(4 Suppl 1):56–60. doi: 10.1016/j.arth.2007.02.008. [DOI] [PubMed] [Google Scholar]
- 8.Rawlinson JJ, Closkey RF, Jr, Davis N, Wright TM, Windsor R. Stemmed implants improve stability in augmented constrained condylar knees. Clin Orthop Relat Res. 2008;466(11):2639–43. doi: 10.1007/s11999-008-0424-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Whittaker JP, Dharmarajan R, Toms AD. The management of bone loss in revision total knee replacement. J Bone Joint Surg (Br) 2008;90(8):981–7. doi: 10.1302/0301-620X.90B8.19948. [DOI] [PubMed] [Google Scholar]
- 10.van Loon CJ, Kyriazopoulos A, Verdonschot N, et al. The role of femoral stem extension in total knee arthroplasty. Clin Orthop Relat Res. 2000;378:282–9. doi: 10.1097/00003086-200009000-00039. [DOI] [PubMed] [Google Scholar]
- 11.Bugbee WD, Ammeen DJ, Engh GA. Does implant selection affect outcome of revision knee arthroplasty? J Arthroplasty. 2001;16(5):581–5. doi: 10.1054/arth.2001.23722. [DOI] [PubMed] [Google Scholar]
- 12.Hanssen AD. Cemented stems are requisite in revision knee replacement. Orthopedics. 2004;27(9):990–1003. doi: 10.3928/0147-7447-20040901-41. [DOI] [PubMed] [Google Scholar]
- 13.Nelson CL, Lonner JH, Rand JA, Lotke PA. Strategies of stem fixation and the role of supplemental bone graft in revision total knee arthroplasty. J Bone Joint Surg Am. 2003;85A:S52–7. doi: 10.2106/00004623-200300001-00010. [DOI] [PubMed] [Google Scholar]
- 14.Completo A, Simões JA, Fonseca F, Oliveira M. The influence of different tibial stem designs in load sharing and stability at the cement-bone interface in revision TKA. Knee. 2008;15(3):227–32. doi: 10.1016/j.knee.2008.01.008. [DOI] [PubMed] [Google Scholar]
- 15.Completo A, Fonseca F, Simões JA. Strain shielding in proximal tibia of stemmed knee prosthesis: experimental study. J Biomech. 2008;41(3):560–6. doi: 10.1016/j.jbiomech.2007.10.006. [DOI] [PubMed] [Google Scholar]
- 16.Hicks CA, Noble P, Tullos H. The anatomy of the tibial intramedullary canal. Clin Orthop Relat Res. 1995;321:111–6. [PubMed] [Google Scholar]
- 17.Radnay CS, Scuderi GR. Management of bone loss: augments, cones, offset stems. Clin Orthop Relat Res. 2006;446:83–92. doi: 10.1097/01.blo.0000214437.57151.41. [DOI] [PubMed] [Google Scholar]
- 18.Tang Q, Zhou Y, Yang D, Xu H, Liu Q. The offset of the tibial shaft from the tibial plateau in Chinese people. J Bone Joint Surg Am. 2010;92(10):1981–7. doi: 10.2106/JBJS.I.00969. [DOI] [PubMed] [Google Scholar]
- 19.Abraham R, Malkani AL, Lewis J, Beck D. An anatomical study of tibial metaphyseal/diaphyseal mismatch during revision total knee arthroplasty. J Arthroplasty. 2007;22(2):241–4. doi: 10.1016/j.arth.2006.06.001. [DOI] [PubMed] [Google Scholar]
- 20.Goosen JHM, Van Hellemondt GG. Tibial component offset in revision total knee arthroplasty. In: Rossi R, Bonasia DE, editors. Total Knee Revision Surgical Techniques. Edizioni Minerva Medica 2013.
- 21.Chan Â, Gamelas J, Folgado J, Fernandes PR. Biomechanical analysis of the tibial tray design in TKA: comparison between modular and offset tibial trays. Knee Surg Sports Traumatol Arthrosc. 2014;22(3):590–8. doi: 10.1007/s00167-013-2628-3. [DOI] [PubMed] [Google Scholar]
- 22.Bertin KC, Freeman MA, Samuelson KM, Ratcliffe SS, Todd RC. Stemmed revision arthroplasty for aseptic loosening of total knee replacement. J Bone Joint Surg (Br) 1985;67(2):242–8. doi: 10.1302/0301-620X.67B2.3980534. [DOI] [PubMed] [Google Scholar]
- 23.Parsley BS, Sugano N, Bertolusso R, Conditt MA. Mechanical alignment of tibial stems in revision total knee arthroplasty. J Arthroplasty. 2003;18(7 Suppl 1):33–6. doi: 10.1016/S0883-5403(03)00302-4. [DOI] [PubMed] [Google Scholar]
- 24.Friedman RJ, Hirst P, Poss R, Kelley K, Sledge CB. Results of revision total knee arthroplasty performed for aseptic loosening. Clin Orthop Relat Res. 1990;255:235–41. [PubMed] [Google Scholar]
- 25.Gustilo T, Comadoll JL, Gustilo RB. Long-term results of 56 revision total knee replacements. Orthopedics. 1996;19(2):99–103. doi: 10.3928/0147-7447-19960201-04. [DOI] [PubMed] [Google Scholar]
- 26.Nakasone CK, Abdeen A, Khachatourians AG, Sugimori T, Vince KG. Component alignment in revision total knee arthroplasty using diaphyseal engaging modular offset press-fit stems. J Arthroplasty. 2008;23(8):1178–81. doi: 10.1016/j.arth.2007.10.002. [DOI] [PubMed] [Google Scholar]
- 27.Partington PF, Sawhney J, Rorabeck CH, Barrack RL, Moore J. Joint line restoration after revision total knee arthroplasty. Clin Orthop Relat Res. 1999;367:165–71. [PubMed] [Google Scholar]
- 28.Laskin RS. Joint line position restoration during revision total knee replacement. Clin Orthop Relat Res. 2002;404:169–71. doi: 10.1097/00003086-200211000-00029. [DOI] [PubMed] [Google Scholar]
- 29.Mahoney OM, Kinsey TL. Modular femoral offset stems facilitate joint line restoration in revision knee arthroplasty. Clin Orthop Relat Res. 2006;446:93–8. doi: 10.1097/01.blo.0000214425.44582.6b. [DOI] [PubMed] [Google Scholar]
- 30.•.Brilhault JM, Ries MD. Influence of offset stem couplers in femoral revision knee arthroplasty: a radiographic study. Knee. 2012;19(2):112–5. doi: 10.1016/j.knee.2011.02.005. [DOI] [PubMed] [Google Scholar]
- 31.Innocenti M, Matassi F, Carulli C, Soderi S, Villano M, Civinini R. Joint line position in revision total knee arthroplasty: the role of posterior femoral off-set stems. Knee. 2013;20(6):447–50. doi: 10.1016/j.knee.2013.05.012. [DOI] [PubMed] [Google Scholar]
- 32.Bellemans J. Restoring the joint line in revision TKA: does it matter? Knee. 2004;11(1):3–5. doi: 10.1016/S0968-0160(03)00099-1. [DOI] [PubMed] [Google Scholar]
- 33.Brilhault JM, Ries MD. Posteriorly offset femoral component to restore anteroposterior position of the distal femur in revision total knee arthroplasty. J Arthroplasty. 2011;26(2):214–7. doi: 10.1016/j.arth.2010.02.016. [DOI] [PubMed] [Google Scholar]


