Abstract
Pulmonary dysfunction is a common complication of cardiac surgery. The mechanisms involved in the development of pulmonary dysfunction are multifactorial and can be related to the activation of inflammatory and oxidative stress pathways. Clinical manifestation varies from mild atelectasis to severe respiratory failure. Managing pulmonary dysfunction postcardiac surgery is a multistep process that starts before surgery and continues during both the operative and postoperative phases. Different pulmonary protection strategies have evolved over the years; however, the wide acceptance and clinical application of such techniques remain hindered by the poor level of evidence or the sample size of the studies. A better understanding of available modalities and/or combinations can result in the development of customised strategies for the different cohorts of patients with the potential to hence maximise patients and institutes benefits.
1. Introduction
Pulmonary dysfunction is a common complication of cardiac surgery that can impact patient's outcomes and health economics. It is recognised that many patients will have altered pulmonary mechanics after surgery which may appear in a wide range of clinical presentations, from mild atelectasis to life threatening acute lung injury (ALI) or adult respiratory distress syndrome (ARDS) [1–3].
Surgical incisions by abolishing the integrity of the chest wall affect respiratory mechanics leading to impaired respiratory effort. Postoperative pain has been shown to be associated with decreased lung function by precluding deep inspirations. Furthermore, patients undergoing surgical procedures associated with opening the pleura will have increased rates of atelectasis, pleural effusions, and postoperative pain especially in the early postoperative period [4–6].
Cardiopulmonary bypass (CPB) can lead to the activation of different inflammatory and coagulation pathways and alters redox balance due to the passage of blood through the circuit (contact activation) and ischaemia and reperfusion injury [7–10].
Vascular endothelial cells (EC) dysfunction during CPB due to changes in blood flow patterns, shear stress, ischaemia, and reperfusion and circulating cytokines will result in the activation of multiple proinflammatory and proapoptosis pathways [11–14] while suppressing its ability to produce vasoprotective mediators [14–17]. EC activation is known to initiate leukocytes adhesion cascade by the expression of members of the selectin family which are responsible for the initial attachment of leukocytes from circulation. Transmigration of leukocyte through EC (crucial step for leukocytes recruitment to tissue) follows leukocytes attachment and is mediated by the upregulation of different adhesion molecules such as platelet endothelial cell adhesion molecule- (PECAM-) 1, ICAM-1, and very late antigen-4 (VLA-4) [18–21].
CPB is traditionally associated with inadequate lung perfusion as there is no flow to the pulmonary artery during periods of cross clamping and when the heart is not ejecting blood, and thus blood supply is limited to the bronchial arteries [22]. Pulmonary physiology alteration during CPB can result in disturbing the balance in the blood gas barrier due to the alteration of the different force affecting the parenchyma thus abolishing gas exchange by passive diffusion at the blood-gas barrier level and leading to ventilation/perfusion mismatch and impaired pulmonary compliance [23, 24]. Moreover, ischaemia during CPB is associated with reduced alveolar blood supply resulting in alveolar ischaemia and hypoxic pulmonary vasoconstriction [25]. Pulmonary vascular endothelial cells dysfunction and activated neutrophils sequestration into lungs parenchyma during period of reperfusion can increase lung tissue permeability and elevate vascular resistance and pulmonary surfactant changes leading to alveolar protein accumulation and pulmonary oedema and driving more ROS and cytokines production [26–28]. This will be manifested as abnormal gas exchange, poor lung mechanics, increased pulmonary shunt fraction and reduced functional residual capacity, and carbon monoxide transfer factor [28–30] (Figure 1).
Figure 1.
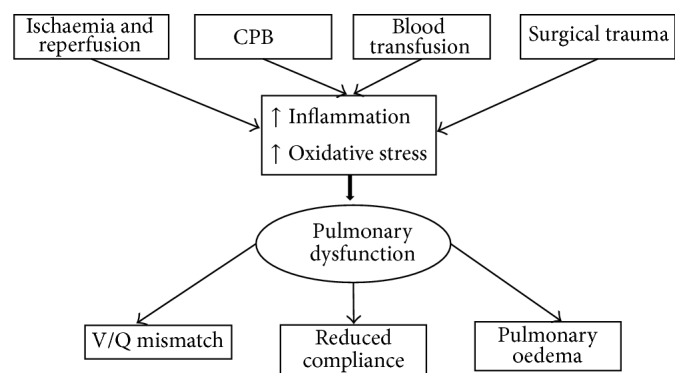
Mechanisms involved in pulmonary dysfunction during cardiac surgery and its consequences.
Blood and blood products usage after surgery can be associated with the production of excessive amount of ROS and systemic and pulmonary inflammation. It has been previously shown that the duration of blood storage before transfusion can influence adverse effect associated with transfusion as there are an increased risk of respiratory insufficiency and the need for prolonged ventilation in patients receiving blood stored for longer than two weeks [10, 31–34].
Here we review the most commonly used strategies to minimise pulmonary dysfunction after cardiac surgery.
2. Pulmonary Protection Strategies
2.1. Pharmacological Interventions
The fact that inflammation and oxidative stress play a pivotal role in the development of pulmonary dysfunction resulted in multiple studies aimed toward modulating such events by the administration of vasodilators and antioxidant and anti-inflammatory medications in experimental animal models or patients undergoing cardiac surgery.
Prostacyclins can induce vascular smooth muscle cells relaxation by the release of intracellular adenosine 3′,5′ cyclic monophosphate (cAMP) resulting in pulmonary and systemic vasodilation [35–38]. Moreover, they can have inhibitory effect on platelet aggregation and leukocytes and monocytes activity [39]. The use of inhaled prostacyclins (Epoprostenol or Flolan) has been shown to decrease pulmonary arterial endothelial dysfunction induced by CPB in experimental studies [40–42]. Furthermore, when administered prior to CPB, they can have beneficial effect in the presence of pulmonary hypertension and may result in lower rate of reintubation in high risk postoperative cardiac patients [43, 44].
Phosphodiesterase inhibitors such as pentoxifylline (PTX) which is a known nonselective phosphodiesterase (PDE) inhibitor can result in elevated levels of intracellular cAMP and vasodilatation. Although PTX has been used classically for claudication symptoms in peripheral vascular disease [45], it has been shown to exert anti-inflammatory and antioxidative properties resulting in modulation of ALI [46–48]. More selective PDE inhibitors such as milrinone can be an advantageous therapeutic strategy for cardiac surgical patients with increased pulmonary vascular resistance (PVR) and right ventricular failure when nebulized and inhaled. It can cause selective pulmonary vasodilation and potentiate the vasodilation effects of inhaled prostacyclin [49, 50].
Nitric oxide (NO) is known to play a pivotal role in vascular endothelial cells homeostasis and regulation of oxidative stress and inflammatory responses [51]. Ischaemia and reperfusion injury during surgery is associated with significant loss in NO; thus NO preconditioning has been suggested to reduce perioperative pulmonary dysfunction and its sequels [52–54]. The protective effects may be due to reversal of postischemic lung hypoperfusion and reduction of lung neutrophil sequestration. The administration of NO in patients with severe left ventricular dysfunction can lead to pulmonary vasodilatation and may augment left ventricular filling [55–57]. The timing of administration and/or concentration of inhaled NO during ischaemia or reperfusion periods is a very important determinant of its effect as NO is toxic early in reperfusion, due to its interaction with superoxide which may lead to damage of alveolar type 2 cells [58, 59].
A large number of other drugs have been used with various degrees of success. Aprotinin (serine proteases) had been shown to reduce neutrophil elastase, malondialdehyde, and proinflammatory cytokines levels in bronchoalveolar lavage fluids of patients undergoing cardiac surgery [60]. The use of aprotinin can result in improving lung function and reducing reperfusion lung injury [61]. The administration of corticosteroids before CPB may reduce the activation of multiple proinflammatory mediators. The translation of proinflammatory mediator's changes into clinical outcomes remains controversial and most of the evidence in the literature originates from small RCTs or observational studies with biomarkers as primary end points [62, 63].
2.2. CPB Modification
Different strategies have been attempted over the years to minimise proinflammatory activation and oxidative stress when using CPB such as coating the circuit with biocompatible material (heparin, poly-2-methoxyethyl acrylate, synthetic protein, and phosphorylcholine), removal of leukocytes (by adding special filters to the CPB), ultrafiltration, and reduced haemodilution.
Heparin is thought to reduce the inflammatory responses linked to platelets and leukocytes by reducing the release of IL-6, IL-8, E-selectin, lactoferrin, myeloperoxidase, integrin, selectin, and platelet thromboglobulin and decreasing the production of oxygen free radicals [64–66]. It has been suggested that compared with conventional circuits (poly-2-methoxyethyl acrylate, synthetic protein, and phosphorylcholine), the heparin-coated circuit may improve lung compliance and pulmonary vascular resistance and thus reduce intrapulmonary shunt although intubation time and ICU stay were not affected [67, 68].
The use of leukocyte filtration mechanisms can modulate proinflammatory cytokines and oxidative stress [69–71]. A clinical study compared the effectiveness of leukocyte filter depletion with a common arterial filter in CABG patients who reported better oxygenation indices and less duration of postoperative mechanical ventilation in the leukocyte depletion filter group [71]. Another study suggested that leukocyte depletion filters preferentially remove activated leukocytes. Improvement in lung function was evident only in the early postoperative phase, but this did not lead to decreasing mortality or better clinical outcomes [72]. The use of ultrafiltration or modified ultrafiltration techniques at the end of surgery may reduce postoperative oedema specifically that of lungs resulting in better oxygenation and improved lung compliance postoperatively. Furthermore, ultrafiltration may remove proinflammatory mediators from the circulation such as IL-6 and IL-8 but it did not result in significant improvement of clinical outcomes [73]. Similarly, controlled haemodilution to regulate oncotic pressure can reduce priming volumes and result in better haemodynamic parameters such as vascular resistance and higher oxygen delivery and affect hospital stay significantly [74, 75].
Understanding problems associated with pulmonary ischaemia and reperfusion results in attempts to provide continuous pulmonary perfusion during CPB. Experimental animal models of pulmonary perfusion demonstrated reduced inflammatory and apoptosis pathways activation with such strategy [25, 76, 77]. Moreover, pulmonary perfusion was found to have favorable effect on lung compliance, oxygenation, and vascular resistance in patients undergoing CABG [78, 79]. Furthermore, pulmonary artery perfusion during CPB can be effective in reducing postoperative right ventricular dysfunction in high-risk patients undergoing LVAD placement [80]. The translation of such changes into better clinical outcomes remains unclear and may be restricted to selective group of patients as demonstrated by a recent trial in patients with COPD undergoing cardiac surgery using CPB where no significant protective effect on lungs was documented [81].
The deleterious effects of surface contact activation as discussed previously have led to the development of minimised cardiopulmonary bypass circuit (mini-CPB). This is characterised by reduced surface area and thus priming volume and prevention of air-blood contact. The utilisation of mini-CPB has been shown to be associated with attenuated production of proinflammatory cytokines and complement activation and blunted leukocytes activation compared to conventional circuit. Markers of oxidative stress tend to be reduced in patients undergoing surgery using mini-CPB compared to conventional circuit [82, 83]. Additionally, mini-CPB reduces organ damage and results in better postoperative gas exchange and lower lung injury scores [84, 85]. Unfortunately most of the clinical trials investigating the role of mini-CPB have evaluated diverse technologies of varying complexity and degree of miniaturisation, which would be expected to give rise to heterogeneity in findings.
2.3. Surgical Strategies
It has been suggested that eliminating the usual standard of no lung inflation during CPB by maintaining a degree of lung ventilation may be beneficial. The use of continuous positive airway pressure (CPAP) during CPB may result in less shunt and better gas exchange [86]; however, it seems that such effect is dependent on the airway pressure used. Using low frequency ventilation (LFV) along with CPAP during CPB to reduce post-CPB lung injury has been evaluated in an experimental pig model [87]. This study showed that the use of LFV is associated with significantly better pulmonary gas exchange, higher adenine nucleotide, lower LDH levels, and reduced histological damage in lung biopsies as well as lower DNA levels in bronchoalveolar lavage (BAL) compared to the collapsed lungs control group. However, a clinical study in patients undergoing cardiac surgery compared the effect of low volume ventilation to conventional strategy of no ventilation and demonstrated no significant changes in PVRI, PaO(2)/FiO(2) ratio, postoperative length of stay, and postoperative pulmonary complications [88]. Furthermore, a meta-analysis of 814 cases in 16 RCTs looking at three lung protective strategies in patients during CPB including CPAP, low-volume ventilation, and vital capacity manoeuvres during CPB showed that the effects of the designated techniques are probably short lived with a questionable impact on the long term clinical outcome of the treated patients [89].
Off pump coronary artery bypass (OPCAB) surgery seems to provide better lung protection by eliminating ischemia-reperfusion injury through maintaining lung ventilation and avoiding CPB. Many studies consistently reported better early and midterm outcomes in OPCAB when compared with conventional on-pump CABG: fewer respiratory complications, shorter intubation time and ITU stay, reduced incidence of pneumonia, and overall shorter hospital stay [90–92].
2.4. Physiotherapy
Preoperative prophylactic physiotherapy with inspiratory or expiratory muscle training can be used as a preventative measure for lung protection [93, 94]. Postoperative physiotherapy is used prophylactically in patients undergoing cardiac surgery. Different techniques can be utilised during this period to improve ventilation-perfusion inequalities, increase pulmonary compliance, and help reinflate collapsed alveoli.
These techniques include deep breathing exercises, slow maximal inspirations with an inspiratory hold, intermittent deep breathing exercises with and without the use of incentive spirometer, and deep breathing exercises with expiratory resistance [95–98].
2.5. Postoperative Noninvasive Ventilation (NIV)
NIV refers to the administration of ventilatory support without using an invasive artificial airway (endotracheal tube or tracheostomy tube). NIV exerts its main effects on the pulmonary and on the cardiovascular systems through the application of a positive end-expiratory pressure (PEEP); with or without a pressure support during inspiration, NIV restores lung volumes by opening atelectatic areas, increases alveolar ventilation, and reduces the work of breathing [99–101].
Continuous positive airway pressure (CPAP) aims to maintain a level of positive airway pressure in a spontaneously breathing patient. It is functionally similar to positive end-expiratory pressure (PEEP), except that PEEP is an applied pressure against exhalation and CPAP is a pressure applied by a constant flow. The ventilator does not cycle during CPAP, no additional pressure above the level of CPAP is provided, and patients must initiate all of their breaths. To avoid drying of the respiratory mucosa, there has been general agreement that the application of humidified CPAP helps to recruit the lungs by increasing functional residual capacity (FRC), increase the surface area of lung, decrease intrapulmonary shunt, and improve oxygenation [102–104].
Bilevel positive airway pressure (BLPAP) is a continuous positive airway pressure with pressure support breaths. It delivers a preset inspiratory positive airway pressure (IPAP) during inspiration and expiratory positive airway pressure (EPAP). BLPAP can be described as CPAP with a time-cycled or flow-cycled change of the applied pressure level [105]. BLPAP senses patients breathing efforts by monitoring air flow in the patient's circuit and adjusts its output by assisting inspiration. Therefore, its physiological effects can benefit the patient in both phases of respiration [106–108]. BLPAP application can only be commenced on conscious, cooperative, and hemodynamically stable patients who can breathe spontaneously, have an adequate gag and cough reflex, and are able to remove the mask when required. Several studies have demonstrated beneficial effects of BLPAP in reducing pulmonary complications and overall length of hospital stay after cardiac surgery [109–111]. Furthermore, the prophylactic use of BLPAP after early extubation has been shown to be safe and effective [111, 112]. A better tolerance was noted when BLPAP settings were commenced on low level and gradually adjusted to achieve the therapeutic target. Radiological improvement of atelectasis after cardiac surgery has been achieved on maintaining 8–10 mL/kg of tidal volume with BLPAP [113].
3. Conclusions
Pulmonary dysfunction is one of the most common and serious complications after cardiac surgery and can significantly impact on patient outcomes and health economics. The mechanisms involved in the development of pulmonary dysfunction are multifactorial and are related to the activation of different inflammatory and oxidative stress pathways. Clinical manifestation varies from mild atelectasis to severe respiratory failure. Managing pulmonary dysfunction postcardiac surgery is a multistep process that starts before surgery and continues during both the operative and postoperative phases. Pulmonary protection strategies have evolved over the years with various degrees of success. The main weakness of the majority of studies is often being observational in nature, small sample size, or being concentrated on a single intervention. Managing pulmonary dysfunction needs to be a multistep process involving more than one modality for each step of the surgical pathway. A better understanding of available modalities and/or combinations will result in the development of customised strategies for the different cohorts of patients. This in turn will help reduce pulmonary dysfunction and hence improve early outcome and costs after cardiac surgery.
Acknowledgment
This research was supported by the National Institute for Health Research Biomedical Research Unit in Cardiovascular Disease at the University Hospitals Bristol NHS Foundation Trust and the University of Bristol.
Conflict of Interests
No conflict of interests is declared by any of the authors.
References
- 1.Ascione R., Lloyd C. T., Underwood M. J., Lotto A. A., Pitsis A. A., Angelini G. D. Economic outcome of off-pump coronary artery bypass surgery: a prospective randomized study. The Annals of Thoracic Surgery. 1999;68(6):2237–2242. doi: 10.1016/s0003-4975(99)01123-6. [DOI] [PubMed] [Google Scholar]
- 2.Hill G. E. Cardiopulmonary bypass-induced inflammation: is it important? Journal of Cardiothoracic and Vascular Anesthesia. 1998;12(2):21–25. [PubMed] [Google Scholar]
- 3.Apostolakis E. E., Koletsis E. N., Baikoussis N. G., Siminelakis S. N., Papadopoulos G. S. Strategies to prevent intraoperative lung injury during cardiopulmonary bypass. Journal of Cardiothoracic Surgery. 2010;5(1, article 1) doi: 10.1186/1749-8090-5-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ali-Hassan-Sayegh S., Mirhosseini S. J., Vahabzadeh V., Ghaffari N. Should the integrity of the pleura during internal mammary artery harvesting be preserved? Interactive CardioVascular and Thoracic Surgery. 2014;19(5):838–847. doi: 10.1093/icvts/ivu254. [DOI] [PubMed] [Google Scholar]
- 5.Ragnarsdóttir M., Kristjánsdóttir Á., Ingvarsdóttir I., Hannesson P., Torfason B., Cahalin L. P. Short-term changes in pulmonary function and respiratory movements after cardiac surgery via median sternotomy. Scandinavian Cardiovascular Journal. 2004;38(1):46–52. doi: 10.1080/14017430310016658. [DOI] [PubMed] [Google Scholar]
- 6.Locke T. J., Griffiths T. L., Mould H., Gibson G. J. Rib cage mechanics after median sternotomy. Thorax. 1990;45(6):465–468. doi: 10.1136/thx.45.6.465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Baufreton C., Corbeau J.-J., Pinaud F. Inflammatory response and haematological disorders in cardiac surgery: toward a more physiological cardiopulmonary bypass. Annales Francaises d'Anesthesie et de Reanimation. 2006;25(5):510–520. doi: 10.1016/j.annfar.2005.12.002. [DOI] [PubMed] [Google Scholar]
- 8.Kirklin J. K., Westaby S., Blackstone E. H., Kirklin J. W., Chenoweth D. E., Pacifico A. D. Complement and the damaging effects of cardiopulmonary bypass. Journal of Thoracic and Cardiovascular Surgery. 1983;86(6):845–857. [PubMed] [Google Scholar]
- 9.Suleiman M.-S., Zacharowski K., Angelini G. D. Inflammatory response and cardioprotection during open-heart surgery: the importance of anaesthetics. British Journal of Pharmacology. 2008;153(1):21–33. doi: 10.1038/sj.bjp.0707526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zakkar M., Guida G., Suleiman M. S., Angelini G. D. Cardiopulmonary bypass and oxidative stress. Oxidative Medicine and Cellular Longevity. 2015;2015:8. doi: 10.1155/2015/189863.189863 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fiotti N., Giansante C., Ponte E., et al. Atherosclerosis and inflammation. Patterns of cytokine regulation in patients with peripheral arterial disease. Atherosclerosis. 1999;145(1):51–60. doi: 10.1016/S0021-9150(99)00013-1. [DOI] [PubMed] [Google Scholar]
- 12.Tesfamariam B., DeFelice A. F. Endothelial injury in the initiation and progression of vascular disorders. Vascular Pharmacology. 2007;46(4):229–237. doi: 10.1016/j.vph.2006.11.005. [DOI] [PubMed] [Google Scholar]
- 13.van der Heiden K., Cuhlmann S., Luong L. A., Zakkar M., Evans P. C. Role of nuclear factor κB in cardiovascular health and disease. Clinical Science. 2010;118(10):593–605. doi: 10.1042/cs20090557. [DOI] [PubMed] [Google Scholar]
- 14.Boyle E. M., Jr., Lille S. T., Allaire E., Clowes A. W., Verrier E. D. Endothelial cell injury in cardiovascular surgery: atherosclerosis. The Annals of Thoracic Surgery. 1997;63(3):885–894. doi: 10.1016/s0003-4975(97)00057-x. [DOI] [PubMed] [Google Scholar]
- 15.Gao M., Xie B., Gu C., Li H., Zhang F., Yu Y. Targeting the proinflammatory cytokine tumor necrosis factor-α to alleviate cardiopulmonary bypass-induced lung injury (review) Molecular Medicine Reports. 2014;11:2373–2378. doi: 10.3892/mmr.2014.3050. [DOI] [PubMed] [Google Scholar]
- 16.Khan S. R. Reactive oxygen species, inflammation and calcium oxalate nephrolithiasis. Translational Andrology and Urology. 2014;3:256–276. doi: 10.3978/j.issn.2223-4683.2014.06.04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rochette L., Lorin J., Zeller M., et al. Nitric oxide synthase inhibition and oxidative stress in cardiovascular diseases: possible therapeutic targets? Pharmacology and Therapeutics. 2013;140(3):239–257. doi: 10.1016/j.pharmthera.2013.07.004. [DOI] [PubMed] [Google Scholar]
- 18.Muller W. A. Leukocyte-endothelial-cell interactions in leukocyte transmigration and the inflammatory response. Trends in Immunology. 2003;24(6):327–334. doi: 10.1016/s1471-4906(03)00117-0. [DOI] [PubMed] [Google Scholar]
- 19.McEver R. P. Selectins. Current Opinion in Immunology. 1994;6(1):75–84. doi: 10.1016/0952-7915(94)90037-X. [DOI] [PubMed] [Google Scholar]
- 20.McEver R. P. Selectins: lectins that initiate cell adhesion under flow. Current Opinion in Cell Biology. 2002;14(5):581–586. doi: 10.1016/s0955-0674(02)00367-8. [DOI] [PubMed] [Google Scholar]
- 21.Dustin M. L., Rothlein R., Bhan A. K., Dinarello C. A., Springer T. A. Induction by IL 1 and interferon-gamma: tissue distribution, biochemistry, and function of a natural adherence molecule (ICAM-1) The Journal of Immunology. 1986;137:245–254. The Journal of Immunology (Baltimore, Md, 1950), vol. 186, pp. 5024–5033, 2011. [PubMed] [Google Scholar]
- 22.Ng C. S. H., Wan S., Yim A. P. C., Arifi A. A. Pulmonary dysfunction after cardiac surgery. Chest. 2002;121(4):1269–1277. doi: 10.1378/chest.121.4.1269. [DOI] [PubMed] [Google Scholar]
- 23.Magnusson L., Zemgulis V., Wicky S., Tydén H., Thelin S., Hedenstierna G. Atelectasis is a major cause of hypoxemia and shunt after cardiopulmonary bypass: An experimental study. Anesthesiology. 1997;87(5):1153–1163. doi: 10.1097/00000542-199711000-00020. [DOI] [PubMed] [Google Scholar]
- 24.Verheij J., van Lingen A., Raijmakers P. G. H. M., et al. Pulmonary abnormalities after cardiac surgery are better explained by atelectasis than by increased permeability oedema. Acta Anaesthesiologica Scandinavica. 2005;49(9):1302–1310. doi: 10.1111/j.1399-6576.2005.00831.x. [DOI] [PubMed] [Google Scholar]
- 25.Li W., Wu X., Yan F., et al. Effects of pulmonary artery perfusion with urinary trypsin inhibitor as a lung protective strategy under hypothermic low-flow cardiopulmonary bypass in an infant piglet model. Perfusion. 2014;29(5):434–442. doi: 10.1177/0267659113517286. [DOI] [PubMed] [Google Scholar]
- 26.Callister M. E., Burke-Gaffney A., Quinlan G. J., et al. Extracellular thioredoxin levels are increased in patients with acute lung injury. Thorax. 2006;61(6):521–527. doi: 10.1136/thx.2005.053041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lamb N. J., Gutteridge J. M. C., Baker C., Evans T. W., Quinlan G. J. Oxidative damage to proteins of bronchoalveolar lavage fluid in patients with acute respiratory distress syndrome: evidence for neutrophil-mediated hydroxylation, nitration, and chlorination. Critical Care Medicine. 1999;27(9):1738–1744. doi: 10.1097/00003246-199909000-00007. [DOI] [PubMed] [Google Scholar]
- 28.Weissman C. Pulmonary complications after cardiac surgery. Seminars in Cardiothoracic and Vascular Anesthesia. 2004;8(3):185–211. doi: 10.1177/108925320400800303. [DOI] [PubMed] [Google Scholar]
- 29.Goodyear-Bruch C., Pierce J. D. Oxidative stress in critically ill patients. The American Journal of Critical Care. 2002;11(6):543–551. [PubMed] [Google Scholar]
- 30.Vidal Melo M. F., Musch G., Kaczka D. W. Pulmonary pathophysiology and lung mechanics in anesthesiology: a case-based overview. Anesthesiology Clinics. 2012;30(4):759–784. doi: 10.1016/j.anclin.2012.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Relevy H., Koshkaryev A., Manny N., Yedgar S., Barshtein G. Blood banking-induced alteration of red blood cell flow properties. Transfusion. 2008;48(1):136–146. doi: 10.1111/j.1537-2995.2007.01491.x. [DOI] [PubMed] [Google Scholar]
- 32.Karkouti K. Transfusion and risk of acute kidney injury in cardiac surgery. British Journal of Anaesthesia. 2012;109(supplement 1):i29–i38. doi: 10.1093/bja/aes422. [DOI] [PubMed] [Google Scholar]
- 33.Bitargil M., Arslan C., Başbuğ H., Göçer H., Günerhan Y., Bekov Y. Transfusion-related acute lung injury following coronary artery bypass graft surgery. Perfusion. 2015 doi: 10.1177/0267659114568367. [DOI] [PubMed] [Google Scholar]
- 34.Dasararaju R., Marques M. B. Adverse effects of transfusion. Cancer Control. 2015;22:16–25. doi: 10.1177/107327481502200104. [DOI] [PubMed] [Google Scholar]
- 35.Raud J. Vasodilatation and inhibition of mediator release represent two distinct mechanisms for prostaglandin modulation of acute mast cell-dependent inflammation. The British Journal of Pharmacology. 1990;99(3):449–454. doi: 10.1111/j.1476-5381.1990.tb12948.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Raslan Z., Naseem K. M. Compartmentalisation of cAMP-dependent signalling in blood platelets: the role of lipid rafts and actin polymerisation. Platelets. 2014:1–9. doi: 10.3109/09537104.2014.916792. [DOI] [PubMed] [Google Scholar]
- 37.Sprague A. H., Khalil R. A. Inflammatory cytokines in vascular dysfunction and vascular disease. Biochemical Pharmacology. 2009;78(6):539–552. doi: 10.1016/j.bcp.2009.04.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kawabe J.-I., Ushikubi F., Hasebe N. Prostacyclin in vascular diseases—recent insights and future perspectives. Circulation Journal. 2010;74(5):836–843. doi: 10.1253/circj.cj-10-0195. [DOI] [PubMed] [Google Scholar]
- 39.Kemming G., Habler O., Kleen M., Kisch-Wedel H., Welte M., Zwissler B. Searching the ideal inhaled vasodilator: from nitric oxide to prostacyclin. European Surgical Research. 2002;34(1-2):196–202. doi: 10.1159/000048909. [DOI] [PubMed] [Google Scholar]
- 40.Haché M., Denault A., Bélisle S., et al. Inhaled epoprostenol (prostacyclin) and pulmonary hypertension before cardiac surgery. Journal of Thoracic and Cardiovascular Surgery. 2003;125(3):642–649. doi: 10.1067/mtc.2003.107. [DOI] [PubMed] [Google Scholar]
- 41.de Wet C. J., Affleck D. G., Jacobsohn E., et al. Inhaled prostacyclin is safe, effective, and affordable in patients with pulmonary hypertension, right heart dysfunction, and refractory hypoxemia after cardiothoracic surgery. The Journal of Thoracic and Cardiovascular Surgery. 2004;127(4):1058–1067. doi: 10.1016/j.jtcvs.2003.11.035. [DOI] [PubMed] [Google Scholar]
- 42.Rex S., Schaelte G., Metzelder S., et al. Inhaled iloprost to control pulmonary artery hypertension in patients undergoing mitral valve surgery: a prospective, randomized-controlled trial. Acta Anaesthesiologica Scandinavica. 2008;52(1):65–72. doi: 10.1111/j.1399-6576.2007.01476.x. [DOI] [PubMed] [Google Scholar]
- 43.Fortier S., DeMaria R. G., Lamarche Y., et al. Inhaled prostacyclin reduces cardiopulmonary bypass-induced pulmonary endothelial dysfunction via increased cyclic adenosine monophosphate levels. Journal of Thoracic and Cardiovascular Surgery. 2004;128(1):109–116. doi: 10.1016/j.jtcvs.2003.09.056. [DOI] [PubMed] [Google Scholar]
- 44.Lowson S. M., Doctor A., Walsh B. K., Doorley P. A. Inhaled prostacyclin for the treatment of pulmonary hypertension after cardiac surgery. Critical Care Medicine. 2002;30(12):2762–2764. doi: 10.1097/00003246-200212000-00023. [DOI] [PubMed] [Google Scholar]
- 45.Porter J. M., Cutler B. S., Lee B. Y., et al. Pentoxifylline efficacy in the treatment of intermittent claudication: multicenter controlled double-blind trial with objective assessment of chronic occlusive arterial disease patients. American Heart Journal. 1982;104(1):66–72. doi: 10.1016/0002-8703(82)90642-1. [DOI] [PubMed] [Google Scholar]
- 46.Michetti C., Coimbra R., Hoyt D. B., Loomis W., Junger W., Wolf P. Pentoxifylline reduces acute lung injury in chronic endotoxemia. Journal of Surgical Research. 2003;115(1):92–99. doi: 10.1016/S0022-4804(03)00219-1. [DOI] [PubMed] [Google Scholar]
- 47.Kreth S., Ledderose C., Luchting B., Weis F., Thiel M. Immunomodulatory properties of pentoxifylline are mediated via adenosine-dependent pathways. Shock. 2010;34(1):10–16. doi: 10.1097/shk.0b013e3181cdc3e2. [DOI] [PubMed] [Google Scholar]
- 48.Konrad F. M., Neudeck G., Vollmer I., Ngamsri K. C., Thiel M., Reutershan J. Protective effects of pentoxifylline in pulmonary inflammation are adenosine receptor A2A dependent. The FASEB Journal. 2013;27(9):3524–3535. doi: 10.1096/fj.13-228122. [DOI] [PubMed] [Google Scholar]
- 49.Kumar V. H., Swartz D. D., Rashid N., et al. Prostacyclin and milrinone by aerosolization improve pulmonary hemodynamics in newborn lambs with experimental pulmonary hypertension. Journal of Applied Physiology. 2010;109(3):677–684. doi: 10.1152/japplphysiol.01082.2009. [DOI] [PubMed] [Google Scholar]
- 50.Haraldsson Å., Kieler-Jensen N., Ricksten S.-E. The additive pulmonary vasodilatory effects of inhaled prostacyclin and inhaled milrinone in postcardiac surgical patients with pulmonary hypertension. Anesthesia & Analgesia. 2001;93(6):1439–1445. doi: 10.1097/00000539-200112000-00018. [DOI] [PubMed] [Google Scholar]
- 51.Song P., Zou M.-H. Redox regulation of endothelial cell fate. Cellular and Molecular Life Sciences. 2014;71(17):3219–3239. doi: 10.1007/s00018-014-1598-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Guery B., Neviere R., Viget N., et al. Inhaled NO preadministration modulates local and remote ischemia- reperfusion organ injury in a rat model. Journal of Applied Physiology. 1999;87(1):47–53. doi: 10.1152/jappl.1999.87.1.47. [DOI] [PubMed] [Google Scholar]
- 53.Bacha E. A., Sellak H., Murakami S., et al. Inhaled nitric oxide attenuates reperfusion injury in non-heartbeating-donor lung transplantation. Transplantation. 1997;63(10):1380–1386. doi: 10.1097/00007890-199705270-00002. [DOI] [PubMed] [Google Scholar]
- 54.Brovkovych V., Gao X.-P., Ong E., et al. Augmented inducible nitric oxide synthase expression and increased NO production reduce sepsis-induced lung injury and mortality in myeloperoxidase-null mice. American Journal of Physiology—Lung Cellular and Molecular Physiology. 2008;295(1):L96–L103. doi: 10.1152/ajplung.00450.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Bloch K. D., Ichinose F., Roberts J. D., Jr., Zapol W. M. Inhaled NO as a therapeutic agent. Cardiovascular Research. 2007;75(2):339–348. doi: 10.1016/j.cardiores.2007.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Price L. C., Wort S. J., Finney S. J., Marino P. S., Brett S. J. Pulmonary vascular and right ventricular dysfunction in adult critical care: current and emerging options for management: a systematic literature review. Critical Care. 2010;14(5, article R169) doi: 10.1186/cc9264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ichinose F., Roberts J. D., Jr., Zapol W. M. Inhaled nitric oxide: a selective pulmonary vasodilator: current uses and therapeutic potential. Circulation. 2004;109(25):3106–3111. doi: 10.1161/01.cir.0000134595.80170.62. [DOI] [PubMed] [Google Scholar]
- 58.Naka Y., Roy D. K., Smerling A. J., et al. Inhaled nitric oxide fails to confer the pulmonary protection provided by distal stimulation of the nitric oxide pathway at the level of cyclic guanosine monophosphate. The Journal of Thoracic and Cardiovascular Surgery. 1995;110(5):1434–1441. doi: 10.1016/s0022-5223(95)70066-8. [DOI] [PubMed] [Google Scholar]
- 59.Eppinger M. J., Ward P. A., Jones M. L., Bolling S. F., Deeb G. M. Disparate effects of nitric oxide on lung ischemia-reperfusion injury. The Annals of Thoracic Surgery. 1995;60(5):1169–1176. doi: 10.1016/0003-4975(95)00697-J. [DOI] [PubMed] [Google Scholar]
- 60.Hill G. E., Pohorecki R., Alonso A., Rennard S. I., Robbins R. A. Aprotinin reduces interleukin-8 production and lung neutrophil accumulation after cardiopulmonary bypass. Anesthesia and Analgesia. 1996;83(4):696–700. doi: 10.1097/00000539-199610000-00006. [DOI] [PubMed] [Google Scholar]
- 61.Erdogan M., Kalaycioglu S., Iriz E. Protective effect of aprotinin against lung damage in patients undergoing CABG surgery. Acta Cardiologica. 2005;60(4):367–372. doi: 10.2143/ac.60.4.2004984. [DOI] [PubMed] [Google Scholar]
- 62.Viviano A., Kanagasabay R., Zakkar M. Is perioperative corticosteroid administration associated with a reduced incidence of postoperative atrial fibrillation in adult cardiac surgery? Interactive Cardiovascular and Thoracic Surgery. 2014;18(2):225–229. doi: 10.1093/icvts/ivt486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Zakkar M., Kanagasabay R. Glucocorticoids in adult cardiac surgery; old drugs revisited. Perfusion. 2013;28(5):395–402. doi: 10.1177/0267659113488433. [DOI] [PubMed] [Google Scholar]
- 64.Weerwind P. W., Maessen J. G., van Tits L. J. H., et al. Influence of Duraflo II heparin-treated extracorporeal circuits on the systemic inflammatory response in patients having coronary bypass. The Journal of Thoracic and Cardiovascular Surgery. 1995;110(6):1633–1641. doi: 10.1016/s0022-5223(95)70024-2. [DOI] [PubMed] [Google Scholar]
- 65.Bozdayi M., Borowiec J., Nilsson L., Venge P., Thelin S., Hansson H. E. Effects of heparin coating of cardiopulmonary bypass circuits on in vitro oxygen free radical production during coronary bypass surgery. Artificial Organs. 1996;20(9):1008–1016. doi: 10.1111/j.1525-1594.1996.tb04588.x. [DOI] [PubMed] [Google Scholar]
- 66.Fukutomi M., Kobayashi S., Niwaya K., Hamada Y., Kitamura S. Changes in platelet, granulocyte, and complement activation during cardiopulmonary bypass using heparin-coated equipment. Artificial Organs. 1996;20(7):767–776. doi: 10.1111/j.1525-1594.1996.tb04538.x. [DOI] [PubMed] [Google Scholar]
- 67.Wan S., Leclerc J.-L., Antoine M., Desmet J.-M., Yim A. P. C., Vincent J.-L. Heparin-coated circuits reduce myocardial injury in heart or heart-lung transplantation: a prospective, randomized study. The Annals of Thoracic Surgery. 1999;68(4):1230–1235. doi: 10.1016/s0003-4975(99)00701-8. [DOI] [PubMed] [Google Scholar]
- 68.Ranucci M., Cirri S., Conti D., et al. Beneficial effects of Duraflo II heparin-coated circuits on postperfusion lung dysfunction. The Annals of Thoracic Surgery. 1996;61(1):76–81. doi: 10.1016/0003-4975(95)00820-9. [DOI] [PubMed] [Google Scholar]
- 69.Bando K., Pillai R., Cameron D. E., et al. Leukocyte depletion ameliorates free radical-mediated lung injury after cardiopulmonary bypass. The Journal of Thoracic and Cardiovascular Surgery. 1990;99(5):873–877. [PubMed] [Google Scholar]
- 70.Lemmer J. H., Jr., Dilling E. W., Morton J. R., et al. Aprotinin for primary coronary artery bypass grafting: a multicenter trial of three dose regimens. Annals of Thoracic Surgery. 1996;62(6):1659–1668. doi: 10.1016/s0003-4975(96)00451-1. [DOI] [PubMed] [Google Scholar]
- 71.Sheppard S. V., Gibbs R. V., Smith D. C. Does leucocyte depletion during cardiopulmonary bypass improve oxygenation indices in patients with mild lung dysfunction? British Journal of Anaesthesia. 2004;93(6):789–792. doi: 10.1093/bja/aeh267. [DOI] [PubMed] [Google Scholar]
- 72.Alexiou C., Sheppard S., Tang A., et al. Leukocytes-depleting filters preferentially remove activated leukocytes and reduce the expression of surface adhesion molecules during the simulated extracorporeal circulation of human blood. ASAIO Journal. 2006;52(4):438–444. doi: 10.1097/01.mat.0000225894.61493.2f. [DOI] [PubMed] [Google Scholar]
- 73.Zakkar M., Guida G., Angelini G. D. Modified ultrafiltration in adult patients undergoing cardiac surgery. Interactive CardioVascular and Thoracic Surgery. 2015;20(3):415–421. doi: 10.1093/icvts/ivu388. [DOI] [PubMed] [Google Scholar]
- 74.Habib R. H., Zacharias A., Schwann T. A., et al. Role of hemodilutional anemia and transfusion during cardiopulmonary bypass in renal injury after coronary revascularization: implications on operative outcome. Critical Care Medicine. 2005;33(8):1749–1756. doi: 10.1097/01.ccm.0000171531.06133.b0. [DOI] [PubMed] [Google Scholar]
- 75.Theusinger O. M., Felix C., Spahn D. R. Strategies to reduce the use of blood products: a European perspective. Current Opinion in Anaesthesiology. 2012;25(1):59–65. doi: 10.1097/aco.0b013e32834dec98. [DOI] [PubMed] [Google Scholar]
- 76.Yewei X., Liya D., Jinghao Z., Rufang Z., Li S. Study of the mechanism of pulmonary protection strategy on pulmonary injury with deep hypothermia low flow. European Review for Medical and Pharmacological Sciences. 2013;17(7):879–885. [PubMed] [Google Scholar]
- 77.Siepe M., Goebel U., Mecklenburg A., et al. Pulsatile pulmonary perfusion during cardiopulmonary bypass reduces the pulmonary inflammatory response. Annals of Thoracic Surgery. 2008;86(1):115–122. doi: 10.1016/j.athoracsur.2008.03.062. [DOI] [PubMed] [Google Scholar]
- 78.Santini F., Onorati F., Telesca M., et al. Selective pulmonary pulsatile perfusion with oxygenated blood during cardiopulmonary bypass attenuates lung tissue inflammation but does not affect circulating cytokine levels. European Journal of Cardio-Thoracic Surgery. 2012;42(6):942–950. doi: 10.1093/ejcts/ezs199.ezs199 [DOI] [PubMed] [Google Scholar]
- 79.Santini F., Onorati F., Telesca M., et al. Pulsatile pulmonary perfusion with oxygenated blood ameliorates pulmonary hemodynamic and respiratory indices in low-risk coronary artery bypass patients. European Journal of Cardio-Thoracic Surgery. 2011;40(4):794–803. doi: 10.1016/j.ejcts.2011.01.065. [DOI] [PubMed] [Google Scholar]
- 80.Macedo F. I. B., Panos A. L., Andreopoulos F. M., Salerno T. A., Pham S. M. Lung perfusion and ventilation during implantation of left ventricular assist device as a strategy to avoid postoperative pulmonary complications and right ventricular failure. Interactive CardioVascular and Thoracic Surgery. 2013;17(5):764–766. doi: 10.1093/icvts/ivt349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Kiessling A.-H., Guo F. W., Gökdemir Y., et al. The influence of selective pulmonary perfusion on the inflammatory response and clinical outcome of patients with chronic obstructive pulmonary disease undergoing cardiopulmonary bypass. Interactive Cardiovascular and Thoracic Surgery. 2014;18(6):732–739. doi: 10.1093/icvts/ivu062. [DOI] [PubMed] [Google Scholar]
- 82.Gerritsen W. B., van Boven W.-J. P., Boss D. S., Haas F. J., van Dongen E. P., Aarts L. P. Malondialdehyde in plasma, a biomarker of global oxidative stress during mini-CABG compared to on- and off-pump CABG surgery: a pilot study. Interactive Cardiovascular and Thoracic Surgery. 2006;5(1):27–31. doi: 10.1510/icvts.2005.116061. [DOI] [PubMed] [Google Scholar]
- 83.van Boven W.-J., Gerritsen W. B., Waanders F. G., Haas F. J., Aarts L. P. Mini extracorporeal circuit for coronary artery bypass grafting: initial clinical and biochemical results: a comparison with conventional and off-pump coronary artery bypass grafts concerning global oxidative stress and alveolar function. Perfusion. 2004;19(4):239–246. doi: 10.1191/0267659104pf746oa. [DOI] [PubMed] [Google Scholar]
- 84.Vohra H. A., Whistance R., Modi A., Ohri S. K. The inflammatory response to miniaturised extracorporeal circulation: a review of the literature. Mediators of Inflammation. 2009;2009:7. doi: 10.1155/2009/707042.707042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Zeitani J., Buccisano F., Nardella S., et al. Mini-extracorporeal circulation minimizes coagulation abnormalities and ameliorates pulmonary outcome in coronary artery bypass grafting surgery. Perfusion. 2013;28(4):298–305. doi: 10.1177/0267659113478322. [DOI] [PubMed] [Google Scholar]
- 86.Loeckinger A., Kleinsasser A., Lindner K. H., Margreiter J., Keller C., Hoermann C. Continuous positive airway pressure at 10 cm H2O during cardiopulmonary bypass improves postoperative gas exchange. Anesthesia and Analgesia. 2000;91(3):522–527. doi: 10.1213/00000539-200009000-00004. [DOI] [PubMed] [Google Scholar]
- 87.Imura H., Caputo M., Lim K., et al. Pulmonary injury after cardiopulmonary bypass: beneficial effects of low-frequency mechanical ventilation. The Journal of Thoracic and Cardiovascular Surgery. 2009;137(6):1530–1537. doi: 10.1016/j.jtcvs.2008.11.014. [DOI] [PubMed] [Google Scholar]
- 88.Gagnon J., Laporta D., Béïque F., Langlois Y., Morin J.-F. Clinical relevance of ventilation during cardiopulmonary bypass in the prevention of postoperative lung dysfunction. Perfusion. 2010;25(4):205–210. doi: 10.1177/0267659110373839. [DOI] [PubMed] [Google Scholar]
- 89.Schreiber J.-U., Lancé M. D., de Korte M., Artmann T., Aleksic I., Kranke P. The effect of different lung-protective strategies in patients during cardiopulmonary bypass: a meta-analysis and semiquantitative review of randomized trials. Journal of Cardiothoracic and Vascular Anesthesia. 2012;26(3):448–454. doi: 10.1053/j.jvca.2012.01.034. [DOI] [PubMed] [Google Scholar]
- 90.Berson A. J., Smith J. M., Woods S. E., Hasselfeld K. A., Hiratzka L. F. Off-pump versus on-pump coronary artery bypass surgery: does the pump influence outcome? Journal of the American College of Surgeons. 2004;199(1):102–108. doi: 10.1016/j.jamcollsurg.2004.03.014. [DOI] [PubMed] [Google Scholar]
- 91.Angelini G. D., Taylor F. C., Reeves B. C., Ascione R. Early and midterm outcome after off-pump and on-pump surgery in Beating Heart Against Cardioplegic Arrest Studies (BHACAS 1 and 2): a pooled analysis of two randomised controlled trials. The Lancet. 2002;359(9313):1194–1199. doi: 10.1016/s0140-6736(02)08216-8. [DOI] [PubMed] [Google Scholar]
- 92.Syed A., Fawzy H., Farag A., Nemlander A. Comparison of pulmonary gas exchange in OPCAB versus conventional CABG. Heart Lung and Circulation. 2004;13(2):168–172. doi: 10.1016/j.hlc.2004.03.015. [DOI] [PubMed] [Google Scholar]
- 93.Hulzebos E. H. J., Helders P. J. M., Favié N. J., de Bie R. A., de La Riviere A. B., van Meeteren N. L. U. Preoperative intensive inspiratory muscle training to prevent postoperative pulmonary complications in high-risk patients undergoing CABG surgery: a randomized clinical trial. Journal of the American Medical Association. 2006;296(15):1851–1857. doi: 10.1001/jama.296.15.1851. [DOI] [PubMed] [Google Scholar]
- 94.Herdy A. H., Marcchi P. L. B., Vila A., et al. Pre- and postoperative cardiopulmonary rehabilitation in hospitalized patients undergoing coronary artery bypass surgery a randomized controlled trial. American Journal of Physical Medicine & Rehabilitation. 2008;87(9):714–719. doi: 10.1097/phm.0b013e3181839152. [DOI] [PubMed] [Google Scholar]
- 95.Agostini P., Singh S. Incentive spirometry following thoracic surgery: what should we be doing? Physiotherapy. 2009;95(2):76–82. doi: 10.1016/j.physio.2008.11.003. [DOI] [PubMed] [Google Scholar]
- 96.Urell C., Emtner M., Hedenström H., Tenling A., Breidenskog M., Westerdahl E. Deep breathing exercises with positive expiratory pressure at a higher rate improve oxygenation in the early period after cardiac surgery—a randomised controlled trial. European Journal of Cardio-Thoracic Surgery. 2011;40(1):162–167. doi: 10.1016/j.ejcts.2010.10.018. [DOI] [PubMed] [Google Scholar]
- 97.Westerdahl E., Lindmark B., Eriksson T., Friberg Ö., Hedenstierna G., Tenling A. Deep-breathing exercises reduce atelectasis and improve pulmonary function after coronary artery bypass surgery. Chest. 2005;128(5):3482–3488. doi: 10.1378/chest.128.5.3482. [DOI] [PubMed] [Google Scholar]
- 98.Carvalho C. R. F., Paisani D. M., Lunardi A. C. Incentive spirometry in major surgeries: a systematic review. Revista Brasileira de Fisioterapia. 2011;15(5):343–350. doi: 10.1590/s1413-35552011005000025. [DOI] [PubMed] [Google Scholar]
- 99.Guarracino F., Cabrini L., Baldassarri R., et al. Non-invasive ventilation-aided transoesophageal echocardiography in high-risk patients: a pilot study. European Journal of Echocardiography. 2010;11(6):554–556. doi: 10.1093/ejechocard/jeq019. [DOI] [PubMed] [Google Scholar]
- 100.Guarracino F., Cabrini L., Baldassarri R., et al. Noninvasive ventilation for awake percutaneous aortic valve implantation in high-risk respiratory patients: a case series. Journal of Cardiothoracic and Vascular Anesthesia. 2011;25(6):1109–1112. doi: 10.1053/j.jvca.2010.06.032. [DOI] [PubMed] [Google Scholar]
- 101.Cabrini L., Plumari V. P., Nobile L., et al. Non-invasive ventilation in cardiac surgery: a concise review. Heart, Lung and Vessels. 2013;5:137–141. [PMC free article] [PubMed] [Google Scholar]
- 102.Denehy L., Berney S. The use of positive pressure devices by physiotherapists. The European Respiratory Journal. 2001;17(4):821–829. doi: 10.1183/09031936.01.17408210. [DOI] [PubMed] [Google Scholar]
- 103.Squadrone V., Coha M., Cerutti E., et al. Continuous positive airway pressure for treatment of postoperative hypoxemia: a randomized controlled trial. Journal of the American Medical Association. 2005;293(5):589–595. doi: 10.1001/jama.293.5.589. [DOI] [PubMed] [Google Scholar]
- 104.Pilkington F. Humidification for oxygen therapy in non-ventilated patients. British Journal of Nursing. 2004;13(2):111–115. doi: 10.12968/bjon.2004.13.2.12415. [DOI] [PubMed] [Google Scholar]
- 105.Hormann C., Baum M., Putensen C., Mutz N. J., Benzer H. Biphasic positive airway pressure (BIPAP)—a new mode of ventilatory support. European Journal of Anaesthesiology. 1994;11(1):37–42. [PubMed] [Google Scholar]
- 106.Baudouin S., Blumenthal S., Cooper B., et al. Non-invasive ventilation in acute respiratory failure: British thoracic society standards of care committee. Thorax. 2002;57(3):192–211. doi: 10.1136/thorax.57.3.192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Stoltzfus S. The role of noninvasive ventilation: CPAP and BiPAP in the treatment of congestive heart failure. Dimensions of Critical Care Nursing. 2006;25(2):66–70. doi: 10.1097/00003465-200603000-00006. [DOI] [PubMed] [Google Scholar]
- 108.Roberts C. M., Brown J. L., Reinhardt A. K., et al. Non-invasive ventilation in chronic obstructive pulmonary disease: management of acute type 2 respiratory failure. Clinical Medicine. 2008;8(5):517–521. doi: 10.7861/clinmedicine.8-5-517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Lopes C. R., Brandão C. M., Nozawa E., Auler J. O., Jr. Benefits of non-invasive ventilation after extubation in the postoperative period of heart surgery. Revista Brasileira de Cirurgia Cardiovascular. 2008;23(3):344–350. doi: 10.1590/s0102-76382008000300010. [DOI] [PubMed] [Google Scholar]
- 110.García-Delgado M., Navarrete I., García-Palma M. J., Colmenero M. Postoperative respiratory failure after cardiac surgery: use of noninvasive ventilation. Journal of Cardiothoracic and Vascular Anesthesia. 2012;26(3):443–447. doi: 10.1053/j.jvca.2011.11.007. [DOI] [PubMed] [Google Scholar]
- 111.Kilic A., Yapıci N., Bıcer Y., Corub T., Aykac Z. Early extubation and weaning with bilevel positive airway pressure ventilation after cardiac surgery (weaning with BiPAP ventilation after cardiac surgery) Southern African Journal of Anaesthesia and Analgesia. 2008;14(5):25–31. [Google Scholar]
- 112.Al Jaaly E., Fiorentino F., Reeves B. C., et al. Effect of adding postoperative noninvasive ventilation to usual care to prevent pulmonary complications in patients undergoing coronary artery bypass grafting: a randomized controlled trial. The Journal of Thoracic and Cardiovascular Surgery. 2013;146(4):912–918. doi: 10.1016/j.jtcvs.2013.03.014. [DOI] [PubMed] [Google Scholar]
- 113.Pasquina P., Merlani P., Granier J. M., Ricou B. Continuous positive airway pressure versus noninvasive pressure support ventilation to treat atelectasis after cardiac surgery. Anesthesia and Analgesia. 2004;99(4):1001–1008. doi: 10.1213/01.ANE.0000130621.11024.97. [DOI] [PubMed] [Google Scholar]


