Abstract
This study investigated gender differences in symptom profiles of major depressive disorder (MDD) in the Korean general population. Data were pooled from the series of nationwide Korean Epidemiologic Catchment Area surveys conducted in 2001, 2006 and 2011, respectively. Of the 18,807 participants, 507 (397 women and 110 men) were diagnosed with MDD within the prior 12 months. In agreement with previous studies, women with MDD appeared to be more vulnerable to experiencing atypical depressive episodes defined as depression with two or more symptoms of fatigue, increased appetite and hypersomnia (P < 0.001). In terms of individual symptoms, female gender was significantly related with higher prevalence of fatigue (P = 0.008), hypersomnia (P = 0.001), noticeable psychomotor retardation (P = 0.029) and suicidal attempts (P = 0.016) with adjustment for birth cohort effect, partner status, and employment status. In the same analysis, men with MDD appeared more vulnerable to decreased libido than women (P = 0.009). This is the first report to demonstrate gender differences in symptomatology of MDD in the general Korean population, and the results are comparable to previous investigations from western societies. Assumingly, the intercultural similarity in female preponderance to atypical depression might reflect the common biological construct underlying the gender difference in mechanism of MDD. In clinical settings, gender differences of MDD should be carefully considered, because these features could be related with treatment response and drug side effects.
Keywords: Depressive Disorder, Major; Symptoms; Sex; Women, Korea
Graphical Abstract
INTRODUCTION
It has been repeatedly shown that women are at greater risk of major depressive disorder (MDD) than men, as the female-to-male (F:M) prevalence ratio of the disorder has been widely accepted to be approximately 2:1 (1). However, this may artifactually reflect a greater tendency of women to seek help or over-report depressive symptoms than men (1). Furthermore, women may be more apt to dwell on their stress and turn transient negative emotions into severe depressive symptoms, whereas men tend to minimize their depressive mood engaging in more active behaviors (2). However, as argued by Kessler (1), the findings that female preponderance to MDD could be closely related with a higher risk of first episode, would be the evidence that gender difference in vulnerability to MDD is not artifactual. Further studies of the interactions among biological vulnerabilities and aggravating environmental factors are needed.
If the female predominance to MDD is genuine, it leads to the question whether the clinical manifestations are different between men and women. Previous studies produced inconsistent results. One study showed no or minimal differences in symptomatology and severity of MDD between men and women (3), whereas others documented higher prevalence of atypical symptoms in females than males with MDD (4,5). In the latest two editions of Diagnostic and Statistical Manual of Mental Disorders (DSMIV and -5) (6,7), the definition of atypical features in MDD requires mood reactivity, and two or more of the symptoms of significant weight gain or increased appetite, hypersomnia, leaden paralysis, and interpersonal rejection sensitivity. Angst et al. (4) simplified and validated the triadic concept of atypical depression, which requires two or more symptoms of fatigue, increased appetite and hypersomnia. The clinical concern is that higher levels of atypical depressive symptoms in women could be associated with younger age of MDD onset, longer duration of episode, increased comorbidity of other mental disorders, higher suicidal risks, and greater functional impairment (8).
Previous epidemiological studies have shown lower prevalence of MDD in East-Asian countries including Korea, Japan and China than in the West (9,10,11). A recent investigation showed that Koreans are less likely to report depressed mood and more apt to experience concentration difficulty and low energy. Such cross-cultural differences would make higher diagnostic threshold for MDD in East-Asian countries (12). Presumably, these cultural differences also might influence the gender effects on MDD. Therefore, it is essential to identify the gender differences in psychopathology of MDD in a sample representing the entire population, and compare them to previous reports. For this purpose, the present study was carried out to profile symptoms of MDD using a large, nationwide sample of Korean adults.
MATERIALS AND METHODS
Data were derived from the nationally representative surveys based on DSM-IV (6) in Korea: Korean Epidemiologic Catchment Area study (KECA) (11), Korean Epidemiologic Catchment Area study replication (KECA-R) (13) and 2011 Korean Epidemiologic Catchment Area study (KECA-2011) (14). Data from the three surveys were pooled and respondents diagnosed with MDD were analyzed.
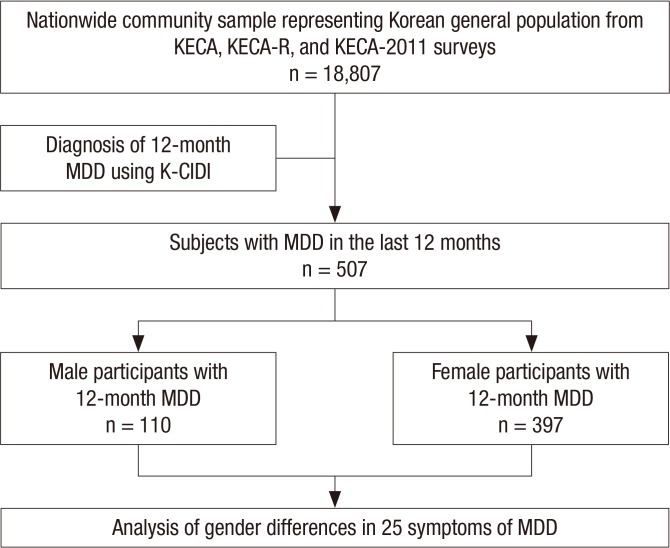
A total of 18,807 respondents (6,275 in KECA, 6,510 in KECA-R, and 6,022 in KECA-2011) completed the interviews which were conducted using the same methods for all 3 surveys. Sampling of the subjects was carried out across similar 12 catchment areas using a multistage, cluster-sampling design. The target population included all eligible community-dwelling residents ≥18 yr-of-age. Face-to-face interviews were conducted using the Korean version of Composite International Diagnostic Interview (K-CIDI), a fully structured diagnostic interview validated by Cho et al. (15) following the guidelines of the World Health Organization (WHO) (16) (Fig. 1).
Fig. 1. Flow diagram of this study. MDD, major depressive disorder.
Assessment of MDD in the last 12 months
KECA, KECA-R and KECA-2011 determined MDD according to the mood section of K-CIDI based on DSM-IV criteria. All participants were initially screened by questioning whether they had experienced either depressive mood and/or loss of interest in the last 12 months. Those answered in the affirmative to any one of these items were queried further to assess whether they met criteria for MDD. Participants who were enrolled were asked a series of questions related to 25 depressive symptoms. These included questions about mood, sleep, appetite, concentration, psychomotor change, and others.
Statistical methods
IBM SPSS Statistics for Windows 20.0 (IBM Corp., Armonk, NY, USA) was used to complete all analyses. Survey weights were calculated for the participants and used to adjust the data to approximate the national age and sex distributions according to the Statistics Korea census. Demographic and clinical characteristics were compared between groups using chi-squared test for categorical variables and Mann-Whitney test for dimensional variables including age of onset, number and longest duration of major depressive episode (MDE), and number of depressive symptoms, because the normality assumption was not satisfied for those variables within the participants with MDD. Individual symptom profiles by gender were compared using chi-squared test, then two-step logistic regression analysis was created. After the step 1 logistic regression analysis was performed adjusted for possible birth cohort effect, step 2 logistic regression analysis was executed with adjustment for the demographic variables that were found to be different in frequency between groups. A P value ≤0.05 was considered to be significant.
Ethics statement
The institutional review board of Seoul National University College of Medicine reviewed the protocol and approved this study (IRB No. for KECA, C-0602-041-168; KECA-R, C-0607-009-177; KECA-2011, C-1104-092-359). All subjects were fully informed about the aims and methods of the study and submitted written informed consent prior to participation.
RESULTS
Demographic and clinical characteristics of subjects with MDD
Sociodemographic and clinical characteristics of subjects with MDD are summarized in Tables 1 and 2. Of the 18,807 respondents, 507 were diagnosed to have had at least one episode of MDD in the last 12 months before the study enrollment. The 12-month prevalence of MDD was 1.5% and 3.3% for men and women, respectively (P<0.001), whereas there were no significant differences between the genders in age, year of birth, and education level. However, partner and employment status showed significant differences (P=0.010 and <0.001, respectively). Medians of age of onset, number and longest duration of MDE, and number of depressive symptoms were not significantly different between men and women.
Table 1. Sociodemographic differences between male and female subjects with major depressive episode in the last 12 months.
| Parameters | Male | Female | χ2 | P | ||
|---|---|---|---|---|---|---|
| Unweighted n | Weighted % | Unweighted n | Weighted % | |||
| Prevalence of MDE* | 110 | 1.5 | 397 | 3.3 | 69.2 | <0.001 |
| Year of birth | 0.62 | 0.961 | ||||
| Before 1950 | 20 | 15.0 | 103 | 17.2 | ||
| 1950-1959 | 30 | 23.7 | 95 | 22.1 | ||
| 1960-1969 | 22 | 19.6 | 82 | 19.4 | ||
| 1970-1979 | 22 | 21.3 | 66 | 19.6 | ||
| Since 1980 | 16 | 20.3 | 51 | 21.7 | ||
| Partner status* | 6.01 | 0.010 | ||||
| Partnered | 50 | 43.3 | 240 | 55.9 | ||
| Unpartnered | 60 | 56.7 | 156 | 44.1 | ||
| Education (yr) | 3.89 | 0.270 | ||||
| 0-6 | 17 | 12.5 | 123 | 17.7 | ||
| 7-9 | 19 | 13.4 | 58 | 13.7 | ||
| 10-12 | 38 | 34.9 | 114 | 35.8 | ||
| ≥ 13 | 36 | 39.0 | 102 | 35.8 | ||
| Employment* | 22.96 | < 0.001 | ||||
| Employed | 45 | 42.9 | 113 | 29.7 | ||
| Student or housekeeper | 35 | 31.5 | 229 | 55.8 | ||
| Unemployed | 30 | 25.6 | 55 | 14.5 | ||
*P<0.05 by chi-squared test. MDE, major depressive episode.
Table 2. Clinical characteristics of male and female subjects with major depressive episode in the last 12 months.
| Parameters | Gender (median) | Statistics | ||
|---|---|---|---|---|
| Male | Female | Z | P | |
| Age of onset (yr) | 35.7 | 32.0 | -1.74 | 0.082 |
| No. of MDE | 4 | 4 | -0.98 | 0.328 |
| Longest duration of MDE (weeks) | 24 | 15.3 | -0.51 | 0.609 |
| No. of depressive symptoms | 14 | 14 | -1.56 | 0.118 |
MDE, major depressive episode.
Symptomatological differences between men and women with MDD
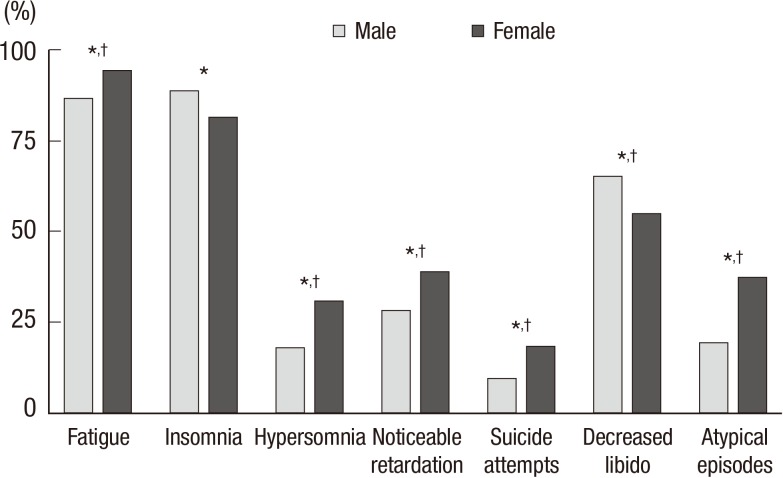
To reveal gender differences in symptomatology of MDD, chi-squared tests were done for the individual symptoms of MDD. The results are shown in Table 3. Women with MDD in the last 12 months appeared to experience more fatigue (94.5% vs. 86.9%, P=0.006), hypersomnia (30.9% vs. 18.1%, P=0.005), and suicidal attempts (18.3% vs. 9.8%, P=0.023) than men. Insomnia (81.5% vs. 88.9%, P=0.049) and decreased libido (54.9% vs. 65.6%, P=0.038) were more frequently reported by men than women (Fig. 2). Female preponderance to psychomotor retardation and slow thought showed borderline significance (P=0.091 and 0.078, respectively), but noticeable psychomotor retardation appeared to be significantly more frequent in women (28.4% vs. 39.0%, P=0.032). Additionally, two-step multivariable logistic regression analysis was carried out. In step 1, year of birth was included as a confounding factor to adjust for birth cohort effect. In step 2, partner and employment status, those appeared to be significantly different between men and women, were additionally adjusted as potential confounders. As demonstrated in Tables 3 and 4, results from step 1 analysis were virtually identical to those from chi-squared tests. Step 2 multivariable logistic regression analysis adjusting for year of birth, partner and employment status revealed slightly different patterns. The higher susceptibility of men to experience insomnia got just outside the conventional level of significance (P=0.111). Gender differences in frequency of fatigue (P=0.008), hypersomnia (P=0.001), noticeable psychomotor retardation (P=0.029), suicide attempt (P=0.016), and decreased libido (P=0.009) remained significant. Subjective psychomotor retardation (P=0.074), low self-confidence (P=0.084) and slow thought (P=0.072) approached nearer to the level of significance (Fig. 2 and Table 4).
Table 3. Symptomatological differences between male and female subjects with major depressive episode in the last 12 months.
| Symptoms | Gender (%) | Statistics | ||||
|---|---|---|---|---|---|---|
| Male | Female | χ2 | P | OR (SE) | 95% CI | |
| Depressed mood | 88.2 | 86.2 | 0.34 | 0.559 | 0.83 (0.31) | 0.45-1.54 |
| Loss of interest | 84.3 | 85.7 | 0.14 | 0.713 | 1.11 (0.29) | 0.63-1.95 |
| Fatigue* | 86.9 | 94.5 | 7.64 | 0.006 | 2.60 (0.96) | 1.29-5.23 |
| Decreased appetite | 78.7 | 80.9 | 0.29 | 0.589 | 1.15 (0.25) | 0.70-1.89 |
| Weight loss | 43.1 | 43.1 | < 0.001 | 0.995 | 1.00 (0.00) | 0.67-1.50 |
| Increased appetite | 12.8 | 13.4 | 0.03 | 0.858 | 1.06 (0.31) | 0.58-1.92 |
| Weight gain | 12.1 | 15.6 | 0.94 | 0.332 | 1.35 (0.31) | 0.74-2.45 |
| Insomnia* | 88.9 | 81.5 | 3.86 | 0.049 | 0.55 (0.31) | 0.30-1.01 |
| Hypersomnia* | 18.1 | 30.9 | 7.94 | 0.005 | 2.03 (0.25) | 1.23-3.34 |
| Psychomotor retardation | 59.9 | 68.2 | 2.87 | 0.091 | 1.43 (0.21) | 0.94-2.18 |
| Noticeable retardation* | 28.4 | 39.0 | 4.62 | 0.032 | 1.61 (0.22) | 1.04-2.49 |
| Psychomotor agitation | 51.8 | 51.6 | 0.001 | 0.977 | 0.99 (0.21) | 0.66-1.49 |
| Noticeable agitation | 24.2 | 28.5 | 0.90 | 0.343 | 1.25 (0.24) | 0.79-1.99 |
| Feeling worthless | 63.2 | 61.2 | 0.16 | 0.691 | 0.92 (0.21) | 0.61-1.39 |
| Feeling guilty | 39.8 | 45.3 | 1.18 | 0.278 | 1.25 (0.21) | 0.83-1.89 |
| Low self-esteem | 70.0 | 74.2 | 0.86 | 0.353 | 1.24 (0.23) | 0.79-1.93 |
| Low self-confidence | 56.2 | 63.4 | 2.03 | 0.154 | 1.35 (0.21) | 0.89-2.03 |
| Concentration difficulty | 77.6 | 83.3 | 2.06 | 0.152 | 1.44 (0.26) | 0.87-2.38 |
| Slow thought | 60.3 | 68.9 | 3.11 | 0.078 | 1.46 (0.21) | 0.96-2.21 |
| Indecisiveness | 69.7 | 70.1 | 0.006 | 0.937 | 1.02 (0.22) | 0.66-1.58 |
| Thought of death | 60.8 | 65.2 | 0.80 | 0.373 | 1.21 (0.21) | 0.80-1.83 |
| Thought of suicide | 51.3 | 49.7 | 0.09 | 0.769 | 0.94 (0.21) | 0.63-1.41 |
| Suicide plan | 23.7 | 21.2 | 0.33 | 0.564 | 0.87 (0.25) | 0.54-1.40 |
| Suicide attempts* | 9.8 | 18.3 | 5.15 | 0.023 | 2.06 (0.32) | 1.09-3.89 |
| Morning worsening | 42.6 | 46.7 | 0.64 | 0.424 | 1.18 (0.21) | 0.79-1.77 |
| Decreased libido* | 65.5 | 54.9 | 4.32 | 0.038 | 0.64 (0.21) | 0.42-0.98 |
| Loss of pleasure | 69.7 | 71.1 | 0.09 | 0.762 | 1.07 (0.23) | 0.69-1.66 |
*P<0.05 for chi-squared test. CI, confidence interval; OR, odds ratio; SE, standard error.
Fig. 2. Summary of gender differences in symptomatology and experience of atypical episodes of major depressive disorder in the last 12 months. *P < 0.05 for chi-squared test; †P < 0.05 for multivariable logistic regression adjusted for birth cohort effect, partner status, and employment status.
Table 4. Adjusted odds ratios of individual depressive symptoms for women compared to men.
| Symptoms | Step 1: adjusted for year of birth | Step 2: adjusted for year of birth, partner and employment status | ||||
|---|---|---|---|---|---|---|
| AOR (SE) | 95% CI | P | AOR (SE) | 95% CI | P | |
| Depressed mood | 0.83 (0.27) | 0.44-1.56 | 0.567 | 0.89 (0.29) | 0.47-1.71 | 0.738 |
| Loss of interest | 1.14 (0.33) | 0.64-2.01 | 0.660 | 1.08 (0.32) | 0.60-1.95 | 0.787 |
| Fatigue*,† | 2.62 (0.94) | 1.30-5.29 | 0.007 | 2.77 (1.06) | 1.31-5.85 | 0.008 |
| Decreased appetite | 1.15 (0.29) | 0.70-1.89 | 0.591 | 1.22 (0.32) | 0.73-2.05 | 0.451 |
| Weight loss | 1.01 (021) | 0.67-1.52 | 0.956 | 1.09 (0.24) | 0.71-1.66 | 0.700 |
| Increased appetite | 1.06 (0.33) | 0.58-1.94 | 0.856 | 1.10 (0.35) | 0.59-2.07 | 0.755 |
| Weight gain | 1.36 (0.42) | 0.74-2.49 | 0.324 | 1.29 (0.42) | 0.68-2.43 | 0.431 |
| Insomnia* | 0.53 (0.17) | 0.29-0.99 | 0.048 | 0.59 (0.19) | 0.31-1.13 | 0.111 |
| Hypersomnia*,† | 2.20 (0.60) | 1.29-3.76 | 0.004 | 2.52 (0.72) | 1.44-4.41 | 0.001 |
| Psychomotor retardation | 1.43 (0.31) | 0.94-2.18 | 0.093 | 1.49 (0.33) | 0.96-2.31 | 0.074 |
| Noticeable retardation*,† | 1.62 (0.36) | 1.04-2.51 | 0.032 | 1.65 (0.38) | 1.05-2.60 | 0.029 |
| Psychomotor agitation | 1.00 (0.21) | 0.66-1.51 | 0.997 | 1.08 (0.24) | 0.70-1.66 | 0.723 |
| Noticeable agitation | 1.28 (0.31) | 0.80-2.05 | 0.305 | 1.39 (0.35) | 0.85-2.27 | 0.183 |
| Feeling worthless | 0.92 (0.20) | 0.60-1.39 | 0.685 | 0.92 (0.20) | 0.59-1.41 | 0.688 |
| Feeling guilty | 1.28 (0.28) | 0.84-1.95 | 0.258 | 1.36 (0.31) | 0.88-2.12 | 0.168 |
| Low self-esteem | 1.25 (0.28) | 0.80-1.95 | 0.335 | 1.18 (0.28) | 0.75-1.87 | 0.490 |
| Low self-confidence | 1.36 (0.28) | 0.90-2.05 | 0.147 | 1.46 (0.32) | 0.95-2.24 | 0.084 |
| Concentration difficulty | 1.46 (0.37) | 0.88-2.41 | 0.143 | 1.39 (0.37) | 0.83-2.34 | 0.212 |
| Slow thought | 1.47 (0.32) | 0.96-2.24 | 0.074 | 1.50 (0.34) | 0.96-2.32 | 0.072 |
| Indecisiveness | 1.02 (0.23) | 0.66-1.59 | 0.913 | 1.04 (0.24) | 0.66-1.64 | 0.858 |
| Thought of death | 1.23 (0.26) | 0.80-1.87 | 0.342 | 1.23 (0.27) | 0.80-1.91 | 0.349 |
| Thought of suicide | 0.95 (0.20) | 0.63-1.44 | 0.824 | 0.96 (0.21) | 0.63-1.46 | 0.841 |
| Suicide plan | 0.87 (0.22) | 0.53-1.41 | 0.568 | 0.85 (0.22) | 0.52-1.41 | 0.538 |
| Suicide attempts*,† | 2.14 (0.70) | 1.13-4.05 | 0.020 | 2.27 (0.77) | 1.16-4.43 | 0.016 |
| Morning worsening | 1.18 (0.25) | 0.79-1.78 | 0.419 | 1.27 (0.28) | 0.83-1.94 | 0.272 |
| Decreased libido*,† | 0.64 (0.14) | 0.42-0.98 | 0.040 | 0.54 (0.13) | 0.35-0.86 | 0.009 |
| Loss of pleasure | 1.08 (0.24) | 0.69-1.68 | 0.750 | 0.96 (0.23) | 0.60-1.53 | 0.869 |
*P<0.05 for multivariable logistic regression adjusted for birth cohort effect; †P<0.05 for multivariable logistic regression adjusted for birth cohort effect, partner status, and employment status. AOR, adjusted odds ratio; CI, confidence interval; SE, standard error.
Atypical depression
Applying the criteria validated by Angst et al. (4), prevalence of atypical depression was compared between men and women. As can be seen from Fig. 2 and Table 5, women (37.3%) were at greater risk of atypical depression than men (19.6%) in chi-squared test (odds ratio: OR=2.45, P<0.001). Furthermore, this gender effect was maintained after adjustment for year of birth, partner and employment status (adjusted odds ratio: AOR=2.88, P<0.001).
Table 5. Gender difference in prevalence of atypical depression in the last 12 months.
| Gender (%) | Statistics | ||||
|---|---|---|---|---|---|
| Male | Female | ||||
| Experience of atypical depressive episode*,† | 19.6 | 37.3 | χ2 | OR (SE) | 95% CI |
| 13.71 | 2.45 (0.25) | 1.51-3.96 | |||
| Z | AOR (SE) | 95% CI | |||
| 3.94 | 2.88 (0.77) | 1.70-4.87 | |||
*P<0.001 for chi-squared test; †PP<0.001 for multivariable logistic regression adjusted for birth cohort effect, partner status, and employment status. AOR, adjusted odds ratio; CI, confidence interval; OR, odds ratio; SE, standard error.
DISCUSSION
The aim of the present study was to investigate the gender differences in the symptom profiles of MDD in the Korean population. Previous studies on clinical and epidemiological samples reported inconsistent results. One study demonstrated negligible differences in symptomatology and severity of MDD between men and women (3), whereas others showed female preponderance to atypical or somatic symptoms such as fatigue, and disturbance in appetite and sleep (4,5). Consistent with these reports, this study indicated that women with MDD are more likely to experience atypical depression than men. In terms of separate symptoms, women showed preponderance to fatigue, hypersomnia, and suicide attempts but not to changes in appetite or weight. Similar trends were observed in subjective psychomotor retardation and slow thought, but they were barely below the level of significance. Additionally, female respondents with MDD reported that their psychomotor retardation had been more easily observable compared with their male counterparts. Men with MDD appeared to be at significantly greater risk of decreased libido and marginally significant trend to experience more frequent insomnia than women.
Atypical depressive symptoms have not only appeared to be more prevalent in women, but have also been associated with earlier age of onset, larger number of depressive symptoms, longer duration of episode, increased comorbidity rate of other mental disorders, higher suicidal risk, and greater functional impairment (4,5,8). In addition, greater risk of MDD have been inferred to be relevant to higher rate of childhood sexual abuse and psychosocial gender role issues in women (17). In this study, the higher rate of suicidal attempts in women was consistent with the previous studies, whereas age of onset, number and duration of MDE, and number of depressive symptoms were not different between both genders in this study. These results are similar to the recent report from Marcus et al. (18) which demonstrated no gender differences in age of onset and length of illness, as well as more atypical and somatic symptoms in women than men. It appears that the relationships among gender, clinical course and atypical symptoms of MDD are not yet firmly established. Further investigations are needed to reveal the associations.
Previous reports indicated overeating and/or weight gain to be the strong distinguishing features of women from men in MDD (4,8,18,19). Romans et al. (19) suggested increased appetite among women with MDD might paradoxically reflect their constant concern with body weight. In accord to this theory, women appeared to be more likely to restrain their diet as early as from adolescence (20) and restrained eaters (dieters) were more vulnerable to stress-induced overeating (21). Contrary to the previous literature, changes in appetite and weight did not account for female predominance in atypical depressive episodes in present study. Rather, fatigue and hypersomnia appeared to be major determinants of atypical depression. Possible explanations include that the social pressure on and/or desire of women to look thinner might be strong enough to defeat the urge of stress-induced overeating, or different genetic or biological factors in energy metabolism in the Korean population. To clarify those possibilities, future studies will need to be done.
Previous results on gender difference in psychomotor symptoms of MDD have been inconsistent. One reported more psychomotor retardation in men than in women (22), but others demonstrated the opposite direction (23), higher frequency of psychomotor agitation in men (8), or no significant gender difference (3). As Sobin and Sackheim (22) pointed out, psychomotor disturbance has been generally evaluated with single-item rating of global agitation or retardation. Nevertheless, psychomotor symptoms can manifest in various aspects, such as "gross motor activity, duration and frequency of body movement, speech pause time, reaction time," and others (22). To be precise in examining psychomotor symptoms of MDD, more detailed and objective methods should be adopted. In this regard, it requires care in interpreting the present results in which marginal trend towards higher vulnerability to psychomotor retardation and its significantly greater noticeability were found in women than men with MDD.
More frequent report of decreased libido by depressed men than women in this study is consistent with the previous result of Winkler et al. (24). They postulated that greater prevalence of decreased libido in men would originate in higher sexual desire in non-depressed state compared to women. They also suggested that men tend to recognize even minor deterioration of sexual function as injuring self-esteem (24). The literature shows that stronger sexual drive in men might be the consequence of interactions among biological inheritance and social influences (25). Nevertheless, it is not yet clear how sexual interest is differently affected by pathophysiologic process of depression between both genders. In any case, it is recommended to consider sexual dysfunction, especially in treatment of male patients with MDD.
Higher prevalence of atypical symptoms in women could reflect differences in neurobiological mechanism of MDD between male and female depression. Notable in this regard are the higher levels of inflammatory and metabolic dysregulation, reduced serotonin synthesis, and hypoactivity of hypothalamic-pituitary-adrenal (HPA) axis in atypical depression, in contrast to reduced 5-HT1A autoreceptor function and hyperactivity of HPA axis in melancholic depression (26). Given that female sex hormones have been suggested to play some roles in modulation of immune, endocrine and neurotransmitter systems, it could be speculated that female preponderance of atypical depression would be related with the action of those hormones (26). Recently, creatine monohydrate augmentation has been reported to enhance the efficacy of escitalopram, a selective serotonin reuptake inhibitor, in women with MDD (27), and the antidepressant-like response was limited to females in an animal study (28). It can be inferred that sexually dimorphic characteristics in brain bioenergetics might at least partially account for different symptom profiles between men and women. Further studies will be necessary to elucidate gender differences in neurobiological pathophysiology of MDD.
This study has several limitations to be considered when interpreting the results. First, it is based on cross-sectional surveys. Diagnosis of MDD and existence of its individual symptoms were based on retrospective reports, in which recall bias could have affected the results. Additionally, any causal inference cannot be made, but only associations be assumed. Second, non-respondents might have also influenced the prevalence data, as it has been known that non-respondents have higher rate of mental disorders than respondents (29,30). Third, false negative results cannot be ruled out, because participants with current MDD could have found it more difficult to complete the questionnaires due to their symptoms or related cognitive deficit. Fourth, severity of individual symptoms might have not been sufficiently assessed with K-CIDI, because it was developed not to evaluate minute severity, but to make diagnosis of mental disorders. Therefore, the severity dimension of MDD could only have been speculated with indirect features including age of onset, number and longest duration of MDE, number of depressive symptoms, and frequency of suicidal attempt. Fifth, we couldn't execute analyses on gender differences in depression-related somatic symptoms, because K-CIDI diagnosis of major depressive disorder was based on DSM-IV and ICD-10 definitions in which common somatic symptoms (e.g. headache, gastrointestinal trouble, and frequent palpitation) were not included. Sixth, sampling required that all respondents belonged to their households. Therefore, institutionalized patients and homeless individuals were not included in this study. Finally, we performed analyses on pooled data of 3 surveys over a decade, and there might have been generational changes in depressive symptomatology and/or recognition of depression itself during that time, especially in a rapidly westernizing society like Korea. To overcome this possible confounding factor, we included birth cohort effect as a covariate in logistic regression analyses.
In conclusion, the present study examined gender differences in symptom profiles of MDD in the last 12 months from the nationwide general population of Korea. In keeping with the reports from previous studies, women were more likely to experience atypical depression with fatigue and hypersomnia than men, whereas no gender differences were evident in disturbance of appetite or body weight. Additionally, women with MDD displayed higher vulnerability to apparent psychomotor retardation and suicide attempts, and less frequent reporting of decreased libido. Overall, the present study showed gender differences in symptoms of MDD in the Korean population were comparable to previous reports from the western society. These findings implicate the possibility that those differences may be manifested more biologically rather than socio-culturally, but the bio-psycho-social mechanism behind this phenomenon is not yet established. In clinical settings, gender differences in MDD should be thoroughly considered because they might be related with treatment response and prognosis. Clinicians should be more careful to recognize atypical symptoms and higher risk of suicide when treating female patients, because these features are difficult to be managed with conventional pharmacological interventions. Additionally, it should be reminded that men can be more prone to sexual dysfunction simultaneously as a depressive symptom and as a side effect of antidepressant medication than women.
ACKNOWLEDGMENTS
The authors wish to express their gratitude to investigators and interviewers of KECA team, and the Korean Ministry of Health and Welfare for their support and cooperation.
Footnotes
DISCLOSURE: The authors have no conflicts of interest to disclose.
AUTHOR CONTRIBUTION: Study concept and coordination: Cho MJ, Chang SM. Study design: Cho MJ, Chang SM, Hong JP. Data collection: Hong JP, Bae JN, Cho SJ, Hahm BJ, Lee DW, Park JI, Lee JY, Jeon HJ, Chang SM. Data review: Cho MJ, Hong JP, Chang SM. Data analysis: Kim JH, Chang SM. Manuscript preparation: Kim JH. Manuscript review and approval: all authors.
References
- 1.Kessler RC. Epidemiology of women and depression. J Affect Disord. 2003;74:5–13. doi: 10.1016/s0165-0327(02)00426-3. [DOI] [PubMed] [Google Scholar]
- 2.Nolen-Hoeksema S, Parker LE, Larson J. Ruminative coping with depressed mood following loss. J Pers Soc Psychol. 1994;67:92–104. doi: 10.1037//0022-3514.67.1.92. [DOI] [PubMed] [Google Scholar]
- 3.Hildebrandt MG, Stage KB, Kragh-Soerensen P. Gender and depression: a study of severity and symptomatology of depressive disorders (ICD-10) in general practice. Acta Psychiatr Scand. 2003;107:197–202. doi: 10.1034/j.1600-0447.2003.02108.x. [DOI] [PubMed] [Google Scholar]
- 4.Angst J, Gamma A, Benazzi F, Silverstein B, Ajdacic-Gross V, Eich D, Rössler W. Atypical depressive syndromes in varying definitions. Eur Arch Psychiatry Clin Neurosci. 2006;256:44–54. doi: 10.1007/s00406-005-0600-z. [DOI] [PubMed] [Google Scholar]
- 5.Smith DJ, Kyle S, Forty L, Cooper C, Walters J, Russell E, Caesar S, Farmer A, McGuffin P, Jones I, et al. Differences in depressive symptom profile between males and females. J Affect Disord. 2008;108:279–284. doi: 10.1016/j.jad.2007.10.001. [DOI] [PubMed] [Google Scholar]
- 6.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- 7.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Washington, DC: American Psychiatric Association; 2013. [Google Scholar]
- 8.Marcus SM, Young EA, Kerber KB, Kornstein S, Farabaugh AH, Mitchell J, Wisniewski SR, Balasubramani GK, Trivedi MH, Rush AJ. Gender differences in depression: findings from the STAR*D study. J Affect Disord. 2005;87:141–150. doi: 10.1016/j.jad.2004.09.008. [DOI] [PubMed] [Google Scholar]
- 9.Chen CN, Wong J, Lee N, Chan-Ho MW, Lau JT, Fung M. The Shatin community mental health survey in Hong Kong. II. Major findings. Arch Gen Psychiatry. 1993;50:125–133. doi: 10.1001/archpsyc.1993.01820140051005. [DOI] [PubMed] [Google Scholar]
- 10.Chiu E. Epidemiology of depression in the Asia Pacific region. Australas Psychiatry. 2004;12:S4–S10. doi: 10.1080/j.1039-8562.2004.02099.x-1. [DOI] [PubMed] [Google Scholar]
- 11.Cho MJ, Kim JK, Jeon HJ, Suh T, Chung IW, Hong JP, Bae JN, Lee DW, Park JI, Cho SJ, et al. Lifetime and 12-month prevalence of DSM-IV psychiatric disorders among Korean adults. J Nerv Ment Dis. 2007;195:203–210. doi: 10.1097/01.nmd.0000243826.40732.45. [DOI] [PubMed] [Google Scholar]
- 12.Chang SM, Hahm BJ, Lee JY, Shin MS, Jeon HJ, Hong JP, Lee HB, Lee DW, Cho MJ. Cross-national difference in the prevalence of depression caused by the diagnostic threshold. J Affect Disord. 2008;106:159–167. doi: 10.1016/j.jad.2007.07.023. [DOI] [PubMed] [Google Scholar]
- 13.Cho MJ, Chang SM, Lee YM, Bae A, Ahn JH, Son J, Hong JP, Bae JN, Lee DW, Cho SJ, et al. Prevalence of DSM-IV major mental disorders among Korean adults: A 2006 National Epidemiologic Survey (KECA-R) Asian J Psychiatr. 2010;3:26–30. doi: 10.1016/j.ajp.2010.01.009. [DOI] [PubMed] [Google Scholar]
- 14.Cho MJ, Seong SJ, Park JE, Chung IW, Lee YM, Bae A, Ahn JH, Lee DW, Bae JN, Cho SJ, et al. Prevalence and correlates of DSM-IV mental disorders in South Korean adults: the Korean epidemiologic catchment area study 2011. Psychiatry Investig. 2015;12:164–170. doi: 10.4306/pi.2015.12.2.164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cho MJ, Hahm BJ, Suh DW, Hong JP, Bae JN, Kim JK, Lee DW, Cho SJ. Development of a Korean version of the composite international diagnostic interview (K-CIDI) J Korean Neuropsychiatr Assoc. 2002;41:123–137. [Google Scholar]
- 16.World Health Organization. Procedures for the Development of New Language Versions of the WHO Composite International Diagnostic Interview (WHO-CIDI) Geneva, Switzerland: World Health Organization; 1997. [Google Scholar]
- 17.Kuehner C. Gender differences in unipolar depression: an update of epidemiological findings and possible explanations. Acta Psychiatr Scand. 2003;108:163–174. doi: 10.1034/j.1600-0447.2003.00204.x. [DOI] [PubMed] [Google Scholar]
- 18.Marcus SM, Kerber KB, Rush AJ, Wisniewski SR, Nierenberg A, Balasubramani GK, Ritz L, Kornstein S, Young EA, Trivedi MH. Sex differences in depression symptoms in treatment-seeking adults: confirmatory analyses from the Sequenced Treatment Alternatives to Relieve Depression study. Compr Psychiatry. 2008;49:238–246. doi: 10.1016/j.comppsych.2007.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Romans SE, Tyas J, Cohen MM, Silverstone T. Gender differences in the symptoms of major depressive disorder. J Nerv Ment Dis. 2007;195:905–911. doi: 10.1097/NMD.0b013e3181594cb7. [DOI] [PubMed] [Google Scholar]
- 20.Rolls BJ, Fedoroff IC, Guthrie JF. Gender differences in eating behavior and body weight regulation. Health Psychol. 1991;10:133–142. doi: 10.1037//0278-6133.10.2.133. [DOI] [PubMed] [Google Scholar]
- 21.Zellner DA, Loaiza S, Gonzalez Z, Pita J, Morales J, Pecora D, Wolf A. Food selection changes under stress. Physiol Behav. 2006;87:789–793. doi: 10.1016/j.physbeh.2006.01.014. [DOI] [PubMed] [Google Scholar]
- 22.Sobin C, Sackeim HA. Psychomotor symptoms of depression. Am J Psychiatry. 1997;154:4–17. doi: 10.1176/ajp.154.1.4. [DOI] [PubMed] [Google Scholar]
- 23.Khan AA, Gardner CO, Prescott CA, Kendler KS. Gender differences in the symptoms of major depression in opposite-sex dizygotic twin pairs. Am J Psychiatry. 2002;159:1427–1429. doi: 10.1176/appi.ajp.159.8.1427. [DOI] [PubMed] [Google Scholar]
- 24.Winkler D, Pjrek E, Heiden A, Wiesegger G, Klein N, Konstantinidis A, Kasper S. Gender differences in the psychopathology of depressed inpatients. Eur Arch Psychiatry Clin Neurosci. 2004;254:209–214. doi: 10.1007/s00406-004-0471-8. [DOI] [PubMed] [Google Scholar]
- 25.Baldwin JD, Baldwin JI. Gender differences in sexual interest. Arch Sex Behav. 1997;26:181–210. doi: 10.1023/a:1024510528405. [DOI] [PubMed] [Google Scholar]
- 26.Antonijevic IA. Depressive disorders -- is it time to endorse different pathophysiologies? Psychoneuroendocrinology. 2006;31:1–15. doi: 10.1016/j.psyneuen.2005.04.004. [DOI] [PubMed] [Google Scholar]
- 27.Lyoo IK, Yoon S, Kim TS, Hwang J, Kim JE, Won W, Bae S, Renshaw PF. A randomized, double-blind placebo-controlled trial of oral creatine monohydrate augmentation for enhanced response to a selective serotonin reuptake inhibitor in women with major depressive disorder. Am J Psychiatry. 2012;169:937–945. doi: 10.1176/appi.ajp.2012.12010009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Allen PJ, D'Anci KE, Kanarek RB, Renshaw PF. Chronic creatine supplementation alters depression-like behavior in rodents in a sex-dependent manner. Neuropsychopharmacology. 2010;35:534–546. doi: 10.1038/npp.2009.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Eaton WW, Anthony JC, Tepper S, Dryman A. Psychopathology and attrition in the epidemiologic catchment area surveys. Am J Epidemiol. 1992;135:1051–1059. doi: 10.1093/oxfordjournals.aje.a116399. [DOI] [PubMed] [Google Scholar]
- 30.de Graaf R, Bijl RV, Smit F, Ravelli A, Vollebergh WA. Psychiatric and sociodemographic predictors of attrition in a longitudinal study: The Netherlands Mental Health Survey and Incidence Study (NEMESIS) Am J Epidemiol. 2000;152:1039–1047. doi: 10.1093/aje/152.11.1039. [DOI] [PubMed] [Google Scholar]