Abstract
Epidermal growth factor receptor (EGFR) mutations in non-small cell lung cancer (NSCLC) patients are associated with sensitivity to small molecule tyrosine kinase inhibitors (TKIs) such as erlotinib, gefitinib, and afatinib. Although studies show an increased progression free survival (PFS) with use of EGFR TKIs in the first-line setting, most patients will develop resistance to therapy after the first 8-16 months. T790M is an acquired resistance mutation reported in 60-70% of patients who initially responded to a prior EGFR TKI. Recently, EGFR TKIs targeting T790M have been developed to overcome resistance with positive results in PFS and objective response rate in patients who have had disease progression on at least one TKI. Two EGFR TKIs targeting T790M, AZD9291 and rociletinib, are new active treatment options for NSCLC but differ in adverse effect profiles. Dose-limiting hyperglycemia has been reported with rociletinib and has required dose reduction, an oral antihyperglycemic, or both, without discontinuation of therapy. This suggests that patients may be effectively treated chronically for hyperglycemia associated with EGFR TKIs targeting T790M, however, guidelines for treatment of hyperglycemia in this setting have not been published. We discuss mechanisms of hyperglycemia associated with TKIs and initial management of hyperglycemia, including benefits and limitations of oral antihyperglycemic options, adjustment of therapy based on grade of hyperglycemia, and recommendations for follow-up glucose monitoring.
Keywords: Hyperglycemia, epidermal growth factor receptor (EGFR), T790M
Background
The treatment approach to non-small cell lung cancer (NSCLC) has become more individualized based on several biomarkers that have emerged as predictive and prognostic markers for NSCLC. Data show that progression free survival (PFS) is improved with the use of targeted epidermal growth factor receptor (EGFR) tyrosine kinase inhibitors (TKIs) in patients with sensitizing EGFR mutations when compared to standard therapy as first-line systemic therapy (1,2). Approximately 45% and 40% of NSCLC patients with a positive EGFR mutation have exon 19 deletion or exon 21 L858R mutations, respectively, which are predictive of treatment benefit to small molecule TKIs such as erlotinib, gefitinib, and afatinib. These sensitizing EGFR mutations are found in approximately 10% of Caucasian patients and up to 50% of Asian patients with NSCLC (3).
Although patients with sensitizing EGFR mutations have positive initial responses of 56-74% and a median PFS of 10-14 months, most will become resistant to first-generation TKI therapy (e.g., erlotinib and gefitinib) after about 8-16 months (4). Acquired resistance due to an EGFR T790M mutation occurs in 60-70% of patients with disease progression after an initial response to erlotinib (4). The mutation is due to a replacement of threonine with methionine that interferes with TKI binding by altering the conformation of the tyrosine kinase domain of EGFR, restoring the affinity of the receptor for adenosine triphosphate (ATP), and reducing the ability of TKIs to compete with ATP (4-9). Second generation irreversible EGFR inhibitors such as afatinib inhibit EGFR T790M in vitro but are associated with response rates of less than 10% and a PFS of 4 months in patients with NSCLC who have received previous treatment with a first-generation TKI. The clinical activity of afatinib monotherapy is impacted by the inability to achieve the dose required to inhibit T790M due to wild type activity. Vertical pathway suppression with afatinib and cetuximab appears more effective (10). Studies have also shown that the T790M mutation may also occur in patients who have not previously received a TKI (11).
Recently, two newer third-generation EGFR TKIs targeting T790M have been developed to attempt to overcome EGFR TKI resistance. AZD9291 and rociletinib (CO-1686) received breakthrough designation by the U.S. Food and Drug Administration (FDA) in 2014 for the treatment of patients with EGFR T790M mutation-positive NSCLC whose disease has progressed during treatment with a prior TKI. Both agents were active in preclinical models of EGFR-mutated NSCLC with or without T790M, but the clinical adverse effect profiles for the two agents were different. Diarrhea, rash and nausea were the most common for AZD9291, whereas hyperglycemia, nausea and fatigue were the most common for rociletinib. The only dose-limiting toxicity for either agent was hyperglycemia reported with rociletinib, however, a maximum tolerated dose was not identified for either agent (12-14).
AZD9291 is an irreversible inhibitor of EGFR and T790M mutations with a reduced affinity for wild-type EGFR and more antitumor activity in EGFR L858R tumors with a concurrent T790M mutation than afatinib. In a dose-escalation and expansion study, 253 patients with NSCLC who progressed on at least one prior EGFR TKI received at least one dose of AZD9291. The overall objective tumor response rate was 51% (95% CI: 45 to 58) and among 127 patients with centrally confirmed EGFR T790M, the response rate was 61% (95% CI: 52 to 70). The median PFS was 9.6 months (95% CI: 8.3 to not reached) in EGFR T790M mutation-positive patients compared to 2.8 months (95% CI: 2.1 to 4.3) in patients who did not have an EGFR T790M mutation. The most common all-cause adverse events were diarrhea (47%), rash (40%), nausea (22%), and decreased appetite (21%). Six patients (2.4%) reported hyperglycemia, however, there were no dose-limiting adverse effects observed. AZD9291 was effective in the T790M mutation-positive setting with limited skin and gastrointestinal adverse effects (13).
Rociletinib is a covalent inhibitor of mutated forms of EGFR including exon 19 deletions, L858R, and T790M mutations, but not exon 20 insertions. In a dose-escalation and expansion study, 130 patients with NSCLC who progressed following treatment with a first- or second-generation EGFR TKI were enrolled to receive two formulations of rociletinib, the first 57 patients receiving a free-base and the remaining patients receiving a hydrogen bromide salt formulation. The objective response rate among the patients with T790M mutation-positive disease who could be evaluated was 59% (95% CI: 45 to 73) compared to 29% (95% CI: 98 to 51) in 17 patients with T790M mutation-negative disease. Patients received a range of 500 milligrams twice daily to 1,000 milligrams twice daily of the hydrogen bromide formulation being used in all ongoing and future development. Based on the dose relationship with toxicity, it appears that 500 milligrams twice daily has decreased rates of toxicity and preserved response rate. Grade 3 toxicities included QT prolongation and hyperglycemia. Hyperglycemia occurred in 20 of the 92 patients (22%) who received therapeutic doses and 25 of the 92 patients (38%) received glucose-lowering therapy. Hyperglycemia generally occurred within the first 3 weeks of therapy (14).
While the two TKIs targeting T790M are both new active treatment options for EGFR-mutated NSCLC, the adverse effect profile differences may distinguish place in therapy. Patients who had hyperglycemia with rociletinib were most often managed with dose reduction, an oral hypoglycemic agent, or both. No patients in the study discontinued therapy (14), suggesting that hyperglycemia can be managed while on long-term TKI therapy to maintain treatment response and tolerability. Because there have not been published recommendations regarding hyperglycemia induced by EGFR TKIs targeting T790M, this review aims to highlight hyperglycemia management based on previous study protocols, related hyperglycemia guidelines, and reviews in other patient populations and anticancer pathways.
Overview of hyperglycemia induced by targeted anticancer agents
Prior to the development of EGFR TKIs targeting T790M, other TKIs have been shown to influence glucose metabolism attributed to various proposed mechanisms and pathways. The molecular mechanism of TKI glucose homeostasis remains unknown and is complicated by the fact that TKIs in the same class can be associated with both hypo- and hyper-glycemia. For example, although imatinib, dasatinib and nilotinib all target the fusion of the breakpoint cluster region gene and Abelson murine leukemia (BCR-ABL) gene for the treatment of chronic myelogenous leukemia, nilotinib causes hyperglycemia in up to 40% of patients and imatinib and dasatinib has been reported to cause hypoglycemia (15). TKIs classified as anaplastic lymphoma kinase (ALK) inhibitors used to treat NSCLC have different effects on glucose within the same drug class. The ALK inhibitor ceritinib causes hyperglycemia in 49% of patients, whereas crizotinib does not cause hyperglycemia (16,17). To date, only hyperglycemia has been reported with EGFR TKIs targeting T790M; hypoglycemia has not been observed in clinical trials of patients receiving AZD9291 or rociletinib (13,14).
Hyperglycemia has been reported with agents inhibiting the phosphoinositide 3-kinase (PI3K)-Akt-mammalian target of rapamycin (PAM) pathway. This pathway affects key insulin signaling pathways downstream by increasing insulin resistance and reducing beta-cell function and mass with an insulin-induced tyrosine phosphorylation pattern mimicking that found in type 2 diabetes (18). A study investigating the mechanism of hyperglycemia for a pan-Akt kinase inhibitor in mice and rats showed increased glucose and insulin levels with hyperglycemia lasting for about 6 hours post dose. Analysis of animal livers showed potential inhibition of glycogen synthesis and/or activation of glycogenolysis, inhibition of peripheral glucose uptake, and lack of response to antihyperglycemic medications such as insulin infusions (19).
The mechanism of action of multikinase ABL inhibitors such as imatinib and dasatinib on glucose metabolism has been demonstrated to occur via human beta cells from chemical-induced apoptosis in vitro through activation of nuclear factor-kappa B (NFκB). The inhibitory effect on platelet-derived growth factor receptor (PDGFR) and tumor necrosis factor alpha (TNF-α) may also affect induction of beta cell apoptosis and insulin resistance in peripheral tissues (15). Imatinib and dasatinib have also been shown to ameliorate hyperglycemia in patients with pre-existing type 2 diabetes. Other multikinase agents such as axitinib, sorafenib, pazopanib, sunitinib, vandetanib, and ponatinib may cause hypoglycemia (20-22). Remission of long-standing type 1 diabetes has also been reported with sunitinib (23). Furthermore, chemical structure analysis has suggested an additional mechanism through modulation of farnesoid X receptor (FXR) involved in glucose and lipid homeostasis (20).
Based on preclinical studies with EGFR TKIs targeting T790M, it is suggested that hyperglycemia or potentially hyperinsulinemia from rociletinib may be caused by a metabolite with targets other than those of the parent molecule. The metabolite inhibits the type I insulin-like growth factor receptor (IGF-IR) and insulin receptor kinases and induces hyperglycemia in rats following an oral glucose tolerance test. The half-life of the parent molecule and the metabolite may allow for reversibility of hyperglycemia in 48-72 hours by withholding EGFR TKI therapy (14). IGF-IR has been proposed as an additional resistance mechanism for EGFR inhibition (24,25).
Initial management of hyperglycemia
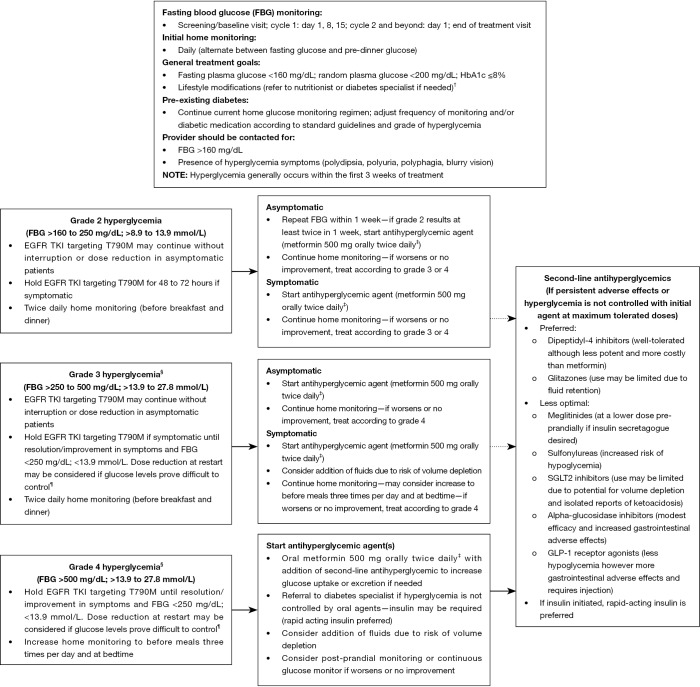
Similar to previous reviews for other anticancer agents, the goal of hyperglycemia management of EGFR TKIs targeting T790M should be to maintain quality of life, prevent acute signs and symptoms of hyperglycemia, and avoid complications of sustained hyperglycemia such as infection, diabetic ketoacidosis, and osmotic diuresis. General treatment goals should include: fasting plasma glucose <160 mg/dL, random plasma glucose <200 mg/dL, and HbA1c ≤8%. Modulation of intensity of glucose lowering is a consideration in advanced cancer patients and less aggressive blood glucose goals may be appropriate. Factors to be considered include the risk of hypoglycemia in patients with co-morbid conditions, such as nausea or stomatitis, as well as life expectancy (26). Some reviews suggest home blood glucose monitoring daily for the first week of the first cycle and 2-3 times per week in subsequent cycles for anticancer agents such as PAM pathway inhibitors (18). Based on clinical experience and onset of hyperglycemia with rociletinib, more intensive glucose monitoring during the first several weeks is warranted. In one study protocol, patients receiving rociletinib had fasting blood glucose monitored weekly for 3 weeks during cycle 1, on the first day of each subsequent cycle, and at the end of treatment visit (14). Patients with pre-diabetes or diabetes should continue their current monitoring regimens and frequency of home glucose monitoring. Monitoring should be increased if the grade of hyperglycemia advances (Figure 1) (18).
Figure 1.
Initial management of hyperglycemia induced by EGFR TKIs targeting T790M. †, Some patients may be able to stop therapy with therapeutic lifestyle changes; ‡, U.S. labeling recommends that metformin should be held for computed tomography scans and should not be used if serum creatinine is >1.3 mg/dL in women; >1.4 mg/dL in men or if decreased tissue perfusion/hemodynamic instability. Recent studies suggest that use in mild to moderate renal insufficiency is safe with appropriate monitoring. Using the extended release form, initiating at lower doses, taking with food, and coaching through the first two weeks of therapy may alleviate nausea and abdominal cramping symptoms. May increase to a maximum total daily dose of metformin 2,000 mg orally daily as tolerated prior to starting or adding a second-line antihyperglycemic agent; §, may require hospitalization for more effective glucose control and intravenous fluids; ¶, initial dose reduction recommendation is to decrease rociletinib from 500 to 375 mg twice daily for persistent FBG >200 mg/dL despite anithyperglycemics. Reductions should occur by one dose level (equivalent of 125 mg twice daily). EGFR, epidermal growth factor receptor; TKI, tyrosine kinase inhibitor.
All patients should be counseled on signs and symptoms of hypo- and hyper-glycemia, although clinical experience with rociletinib has shown that symptoms more commonly associated with diabetes, such as polydipsia, polyuria, and polyphagia, were less frequent with rociletinib. The symptoms more commonly associated with rociletinib-induced hyperglycemia were nausea, vomiting, diarrhea, and fatigue. The lack of classic hyperglycemic symptoms may reflect the relatively modest elevation in blood glucose encountered in this setting. Conversely, the gastrointestinal effects described in clinical studies with rociletinib use may be in part due to treatment with metformin (14). Providers should be contacted when home glucose values are routinely above 160 mg/dL and any time new symptoms occur. Follow-up laboratory testing should be performed to confirm hyperglycemia (18). We also recommend routine HgA1c testing per American Diabetes Association guidelines (27).
Management of hyperglycemia induced by EGFR TKIs targeting T790M based on grade is shown in Figure 1. Because evidence suggests that rociletinib-induced hyperglycemia is due to a mechanism associated with the development of type 2 diabetes, insulin-sensitizing agents are rational first-line agents in this setting in addition to dietary counseling. Of these agents, metformin is the preferred drug for its efficacy, safety profile, and relatively low cost. An initial metformin dose of 500 mg orally twice daily with food is recommended. Recent evidence suggests that the current cut-off values for creatinine in the U.S. labeling should be relaxed. Several studies support the use of metformin in stable mild to moderate renal insufficiency (26,28,29). While several antihyperglycemic medications have been studied for potential antitumor effects, metformin may be particularly promising in this regard (30-32). Potential adverse effects, such as nausea and abdominal cramping, are alleviated in most patients by using the extended release form, initiating at lower doses, taking with food, and coaching through the first 2 weeks of therapy. Extended release metformin has been used in an ongoing study of rociletinib (NCT01526928) with improved tolerability.
If adverse effects persist or hyperglycemia is not controlled after titrating metformin to maximum tolerated doses, another oral agent may be initiated prior to consideration of insulin. Each antihyperglycemic class has strengths and limitations. Dipeptidyl-4 inhibitors may be considered as preferred next-line agents as they are well tolerated and do not result in hypoglycemia, however these agents are not as potent as metformin and have a higher cost. While glitazones and sodium-glucose cotransporter-2 (SGLT2) inhibitors are effective, fluid retention with thiazolidinediones such as pioglitazone and volume depletion with SGLT2 inhibitors, respectively, may limit the use of these classes in patients who may be undergoing toxic oncologic therapies affecting fluid balance. Recent reports have also raised the concern that SGLT2 inhibitors may increase the risk for ketoacidosis (33). If an insulin secretagogue is desired, meglitinides at a lower dose pre-prandially may be preferred because of their rapid onset and short duration of action. Sulfonylureas, particularly long-acting forms, are usually not optimal in patients with unpredictable nutrient intake because of increased risk of hypoglycemia, especially in patients with current or potential renal compromise. The relatively modest efficacy with potential for gastrointestinal adverse effects may render alpha-glucosidase inhibitors less preferred as first or second-line agents. GLP-1 receptor agonists are potent insulin-sensitizers that do not induce hypoglycemia, however, they require injection and may result in significant gastrointestinal effects and undesirable weight loss. For hyperglycemia uncontrolled by oral agents, insulin is the best option for efficacy and flexibility of dosing but requires injection (18). Because of their short half-lives, rapid-acting insulins can be safely used when renal compromise is present and withheld in situations of variable oral intake (26). There is concern that exogenous insulin or medications which increase endogenous insulin levels may promote tumorigenesis and is the subject of ongoing research (34).
In study protocols, TKI therapy was either restarted at the same dose per physician discretion or reduced if glucose levels were difficult to control after initiation of treatment for hyperglycemia. Because of the short half-life of rociletinib, symptomatic patients could hold rociletinib to reverse hyperglycemia and initiate an oral antihyperglycemic agent prior to reaching grade 4 toxicity (14).
Follow-up and monitoring of hyperglycemia
Fasting blood glucose levels of patients on antihyperglycemic medications should be closely monitored throughout therapy with EGFR TKIs targeting T790M. Antihyperglycemic agents should be discontinued in normo-glycemic patients who are no longer taking EGFR TKIs. Routine monitoring of blood glucose following discontinuation should be performed at subsequent visits to assess need for adjustments or re-initiation of treatment (18).
Discussion
Targeted therapy with TKIs has broadened the scope of treatment in various types of malignancy, including NSCLC. Although there are positive clinical outcomes and additional agents available based on known mechanisms of resistance, agent and target specific adverse effects may limit therapy. The effects of TKIs on glucose metabolism should be considered with close monitoring and initiation of antihyperglycemic therapy based on grade of hyperglycemia.
Current studies investigating EGFR TKIs targeting T790M have included patients with pre-existing diabetes who were treated uneventfully with antihyperglycemic agents (13,14). Metformin is the preferred initial therapy after lifestyle modification, with additional therapy choices dictated in part by individual patient considerations. Anticipated gastrointestinal adverse effects may be prevented or alleviated by simple measures in most patients. It is important that diabetic patients continue to be considered for inclusion in ongoing clinical trials since these patients are a large part of the cancer population. Standard practice recommendations for pre-existing diabetes and consultation with a diabetes specialist is recommended for hyperglycemia management since these patients were not separated into diabetic and non-diabetic cohorts at study initiation and hyperglycemia algorithms in this setting have not been published. Treatment recommendations beyond oral antihyperglycemic agents are unclear as most patients were managed in clinical trials without initiation of insulin. It should be noted that the safety of various antihyperglycemic regimens has not been specifically studied in cancer patients.
Patients who received EGFR TKIs targeting T790M and experienced hyperglycemia more frequently reported adverse events than those that did not (14). The setting of hyperglycemia may also theoretically induce tumor growth since it has been suggested that cells can undergo a signaling switch under hyperglycemic conditions that can lead to alternative mechanisms utilized to activate the mitogenic pathways of the IGF-IR independent from tyrosine phosphorylation of the IGF-IR (35). The effect of hyperglycemia on toxicity and tumor growth in vivo remains to be seen, and may not be well studied due to lack of sustained clinical sequelae with appropriate management of toxicity. The outcomes for patients treated with rociletinib who developed hyperglycemia and those without hyperglycemia appear to be similar (14,31). Further study is needed to discern the possible pro- and anti-tumor effects of various antihyperglycemic regimens.
Overall, results have been encouraging with efficacy of EGFR TKIs targeting T790M and the treatment of adverse effects such as hyperglycemia may promote chronic use and tolerability in appropriate patients. Our understanding of the mechanism of hyperglycemia and long-term outcomes following treatment will evolve with follow-up of patients currently receiving EGFR TKIs targeting T790M in ongoing studies.
Conclusions
Understanding the management of potential toxicities of EGFR TKIs targeting T790M such as hyperglycemia may be helpful in clinical-decision making in selection of therapy in an era of new personalized drug development targeting established biomarkers and mechanisms of resistance. Hyperglycemia has been shown to be a dose-limiting toxicity in one agent targeting T790M, however, this can be managed with appropriate antihyperglycemic therapy without EGFR TKI discontinuation in most patients.
Acknowledgements
None.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- 1.Rosell R, Carcereny E, Gervais R, et al. Erlotinib versus standard chemotherapy as first-line treatment for European patients with advanced EGFR mutation-positive non-small-cell lung cancer (EURTAC): a multicentre, open-label, randomised phase 3 trial. Lancet Oncol 2012;13:239-46. [DOI] [PubMed] [Google Scholar]
- 2.Sequist LV, Yang JC, Yamamoto N, et al. Phase III study of afatinib or cisplatin plus pemetrexed in patients with metastatic lung adenocarcinoma with EGFR mutations. J Clin Oncol 2013;31:3327-34. [DOI] [PubMed] [Google Scholar]
- 3.Langer CJ. Epidermal growth factor receptor inhibition in mutation-positive non-small-cell lung cancer: is afatinib better or simply newer? J Clin Oncol 2013;31:3303-6. [DOI] [PubMed] [Google Scholar]
- 4.Yu HA, Arcila ME, Rekhtman N, et al. Analysis of tumor specimens at the time of acquired resistance to EGFR-TKI therapy in 155 patients with EGFR-mutant lung cancers. Clin Cancer Res 2013;19:2240-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pao W, Miller VA, Politi KA, et al. Acquired resistance of lung adenocarcinomas to gefitinib or erlotinib is associated with a second mutation in the EGFR kinase domain. PLoS Med 2005;2:e73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Onitsuka T, Uramoto H, Nose N, et al. Acquired resistance to gefitinib: the contribution of mechanisms other than the T790M, MET, and HGF status. Lung Cancer 2010;68:198-203. [DOI] [PubMed] [Google Scholar]
- 7.Kosaka T, Yatabe Y, Endoh H, et al. Analysis of epidermal growth factor receptor gene mutation in patients with non-small cell lung cancer and acquired resistance to gefitinib. Clin Cancer Res 2006;12:5764-9. [DOI] [PubMed] [Google Scholar]
- 8.Gainor JF, Shaw AT. Emerging paradigms in the development of resistance to tyrosine kinase inhibitors in lung cancer. J Clin Oncol 2013;31:3987-96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Finlay MR, Anderton M, Ashton S, et al. Discovery of a potent and selective EGFR inhibitor (AZD9291) of both sensitizing and T790M resistance mutations that spares the wild type form of the receptor. J Med Chem 2014;57:8249-67. [DOI] [PubMed] [Google Scholar]
- 10.Janjigian YY, Smit EF, Groen HJ, et al. Dual inhibition of EGFR with afatinib and cetuximab in kinase inhibitor-resistant EGFR-mutant lung cancer with and without T790M mutations. Cancer Discov 2014;4:1036-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rosell R, Molina MA, Costa C, et al. Pretreatment EGFR T790M mutation and BRCA1 mRNA expression in erlotinib-treated advanced non-small-cell lung cancer patients with EGFR mutations. Clin Cancer Res 2011;17:1160-8. [DOI] [PubMed] [Google Scholar]
- 12.Tartarone A, Lerose R. Clinical approaches to treat patients with non-small cell lung cancer and epidermal growth factor receptor tyrosine kinase inhibitor acquired resistance. Ther Adv Respir Dis 2015;9:242-50. [DOI] [PubMed] [Google Scholar]
- 13.Jänne PA, Yang JC, Kim DW, et al. AZD9291 in EGFR inhibitor-resistant non-small-cell lung cancer. N Engl J Med 2015;372:1689-99. [DOI] [PubMed] [Google Scholar]
- 14.Sequist LV, Soria JC, Goldman JW, et al. Rociletinib in EGFR-mutated non-small-cell lung cancer. N Engl J Med 2015;372:1700-9. [DOI] [PubMed] [Google Scholar]
- 15.Deangelo DJ. Managing chronic myeloid leukemia patients intolerant to tyrosine kinase inhibitor therapy. Blood Cancer J 2012;2:e95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zykadia™ (ceritinib) [prescribing information]. East Hanover, NJ: Novartis Pharmaceuticals Corporation; 2014. [Google Scholar]
- 17.Xalkori® (crizotinib) [prescribing information]. Pfizer, Inc: New York, NY; 2013.
- 18.Busaidy NL, Farooki A, Dowlati A, et al. Management of metabolic effects associated with anticancer agents targeting the PI3K-Akt-mTOR pathway. J Clin Oncol 2012;30:2919-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Crouthamel MC, Kahana JA, Korenchuk S, et al. Mechanism and management of AKT inhibitor-induced hyperglycemia. Clin Cancer Res 2009;15:217-25. [DOI] [PubMed] [Google Scholar]
- 20.Dy GK, Adjei AA. Understanding, recognizing, and managing toxicities of targeted anticancer therapies. CA Cancer J Clin 2013;63:249-79. [DOI] [PubMed] [Google Scholar]
- 21.Ono K, Suzushima H, Watanabe Y, et al. Rapid amelioration of hyperglycemia facilitated by dasatinib in a chronic myeloid leukemia patient with type 2 diabetes mellitus. Intern Med 2012;51:2763-6. [DOI] [PubMed] [Google Scholar]
- 22.Veneri D, Franchini M, Bonora E. Imatinib and regression of type 2 diabetes. N Engl J Med 2005;352:1049-50. [DOI] [PubMed] [Google Scholar]
- 23.Huda MS, Amiel SA, Ross P, et al. Tyrosine kinase inhibitor sunitinib allows insulin independence in long-standing type 1 diabetes. Diabetes Care 2014;37:e87-8. [DOI] [PubMed] [Google Scholar]
- 24.Vazquez-Martin A, Cufí S, Oliveras-Ferraros C, et al. IGF-1R/epithelial-to-mesenchymal transition (EMT) crosstalk suppresses the erlotinib-sensitizing effect of EGFR exon 19 deletion mutations. Sci Rep 2013;3:2560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cortot AB, Repellin CE, Shimamura T, et al. Resistance to irreversible EGF receptor tyrosine kinase inhibitors through a multistep mechanism involving the IGF1R pathway. Cancer Res 2013;73:834-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Inzucchi SE, Bergenstal RM, Buse JB, et al. Management of hyperglycemia in type 2 diabetes, 2015: a patient-centered approach: update to a position statement of the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care 2015;38:140-9. [DOI] [PubMed] [Google Scholar]
- 27.Standards of medical care in diabetes--2015: summary of revisions. Diabetes Care 2015;38 Suppl:S4. [DOI] [PubMed] [Google Scholar]
- 28.Lipska KJ, Bailey CJ, Inzucchi SE. Use of metformin in the setting of mild-to-moderate renal insufficiency. Diabetes Care 2011;34:1431-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Flory JH, Hennessy S. Metformin use reduction in mild to moderate renal impairment: possible inappropriate curbing of use based on food and drug administration contraindications. JAMA Intern Med 2015;175:458-9. [DOI] [PubMed] [Google Scholar]
- 30.Dowling RJ, Niraula S, Stambolic V, et al. Metformin in cancer: translational challenges. J Mol Endocrinol 2012;48:R31-43. [DOI] [PubMed] [Google Scholar]
- 31.He Y. Rociletinib in EGFR-Mutated Non-Small-Cell Lung Cancer. N Engl J Med 2015;373:578. [DOI] [PubMed] [Google Scholar]
- 32.Eikawa S, Nishida M, Mizukami S, et al. Immune-mediated antitumor effect by type 2 diabetes drug, metformin. Proc Natl Acad Sci U S A 2015;112:1809-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Taylor SI, Blau JE, Rother KI. SGLT2 Inhibitors May Predispose to Ketoacidosis. J Clin Endocrinol Metab 2015;100:2849-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Onitilo AA, Engel JM, Glurich I, et al. Diabetes and cancer II: role of diabetes medications and influence of shared risk factors. Cancer Causes Control 2012;23:991-1008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Janssen JA, Varewijck AJ. Insulin analogs and cancer: a note of caution. Front Endocrinol (Lausanne) 2014;5:79. [DOI] [PMC free article] [PubMed] [Google Scholar]