Abstract
Context:
The main objectives of triage are securing patient safety during the process of emergency diagnosis and treatment, and reduction of waiting time for medical services and transport. To date, there is no triage system for nerve agent victims.
Evidence Acquisition:
This systematic review proposes a new triage system for patients exposed to nerve agents. Information regarding clinical signs and symptoms of intoxication with nerve agents, primary treatments, and classification of patients were extracted from the literature. All related articles were reviewed. Subsequently, specialists from different disciplines were invited to discuss and draft protocols.
Results:
Finalized triage tables summarizing the classification methods and required protocols in the field were designed after several meetings.
Conclusions:
The proposed triage protocol encompasses aspects from most of the existing triage systems to create a single overarching guide for unifying the triage process. The proposed protocol can serve as a base for the designing future guidelines.
Keywords: Triage, Chemical Warfare, Nerve Agents, Protocol
1. Context
The triage system for classification of patients was first used by Baron Dominique Jean Larry, a chief surgeon in Napoleon’s army (1). Since in most mass casualty situations the number of patients exceeds the capacity of the medical facilities, there is an urgent need to prioritize equipment and medical supplies. The main objectives of triage are securing patient safety during the process of emergency diagnosis and treatment, and reduction of waiting time to receive medical services and transport. Despite this knowledge, evidence to support the use of one triage algorithm over another is limited, and development of effective triage protocols is an important research priority (2-5). Disastrous experiences of use of mass destruction chemical weapons during the First World War coerced countries to sign the Geneva protocol on 17 June, 1925 to prohibit use of any chemical and biological warfare. In spite of the international treaty forbidding use of chemical weapons, cyanide, nerve agents and blistering agents have been used during several wars, such as the Syria nerve agent attack, the Tokyo subway sarin attack and the Iraq-Iran war (6-9).
Nerve agents are colorless, odorless, and volatile liquids but their impure forms smell fruity, chocolaty, and camphoric. These agents are unstable and heavier than air. Molecular structure of nerve agents resembles organophosphate pesticides. Tabun (GA), Sarin (GB), Cyclosarin (GF), Soman (GD), GV, EA-3148, VE, VG, VM, VR, VX, and Novichok agents are members of the nerve agent family. Dermal and pulmonary absorption of nerve agents cause perturbations in the nervous system and leads to systemic paralysis, suffocation, and death. Symptoms of poisoning with nerve agents include miosis, blurry vision, gleamy eyes, severe eye irritation, salivation, watery mouth, sweating, rhinorrhea, muscle contractions, peripheral muscle fatigue, nausea, vomiting, abnormal and uncontrolled urination, headache, dizziness, difficulty in estimating the size of an object or distance , paroxysm, asthenia, and coma (7, 10).
2. Evidence Acquisition
Rapid care, therapy and transport of victims are among the primary tasks following exposure to nerve agents. Definition of a unique triage system for victims of nerve agents was the main objective of this study because experts do not always recommend the same guideline. Several protocols for triage of chemical victims exist without any international consensus. These protocols vary significantly in terms of proposed methods of care, treatments, equipment and different strategies that have been put forward by organizations in different countries (11). This study aimed to prepare a uniform triage protocol through systematic review of literature, laws, and regulations, analysis of personal experiences, and consultations with specialists. The ultimate goals of such a triage protocol are to prevent confusion and facilitate clinical decision making in difficult and complex situations.
2.1. Data Sources
Data were collected from published papers and books retrieved from MEDLINE, Cochrane, SID, Springer, Web of Knowledge, Science Citation Index, Web of Science, Academic Science, and PubMed, as well as local published papers in the Ministry of Health and Medical Education, Red Crescent, and army of the Islamic Republic of Iran.
2.2. Study Selection
Articles were assessed and classified according to their number of citations. Extracted protocols were introduced to a group of invited experts in various fields of medicine including emergency medicine, pulmonology, forensic medicine, ophthalmology, dermatology, pharmacology, toxicology and nursing. All experts were well-experienced in the treatment of nerve agent-related injuries. Invitees were asked for their own experiences and comments in confronting the nerve agent-related injuries. During several meetings, all comments, ideas, experience, and protocols were carefully discussed and revised. Final instructions were sent as a new triage protocol to the senior policy making authorities.
3. Results
3.1. Existing Triage Systems
Triage systems were divided into two categories: primary and secondary (12). Primary triage systems prioritize patients in the field for urgent assignment to medical care. Simple treatment and rapid transport (START) (13), the triage sieve (14), flight care triage (15), and the Sacco triage method (STM) (16) were primary triage systems identified.
Secondary triage is aimed at management of patients in hospital and on the scene. Secondary assessment of victim endpoint (SAVE) triage (17) and triage sort (14) were identified as secondary triage systems.
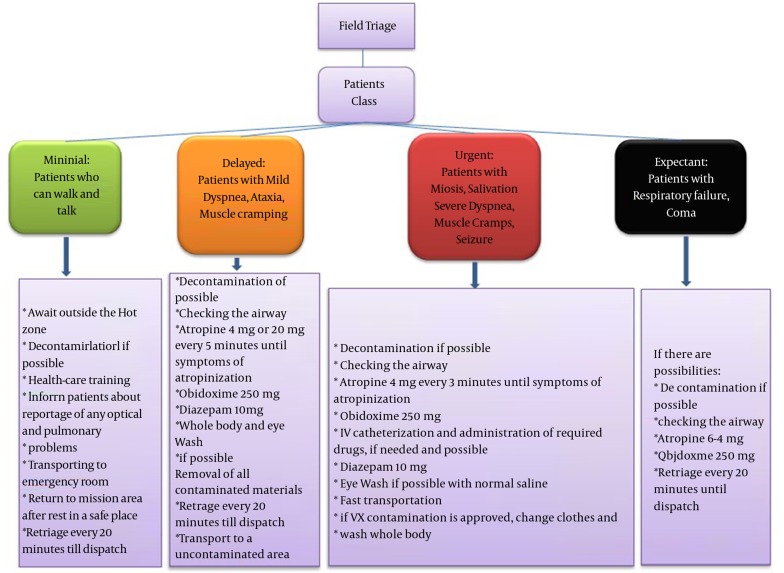
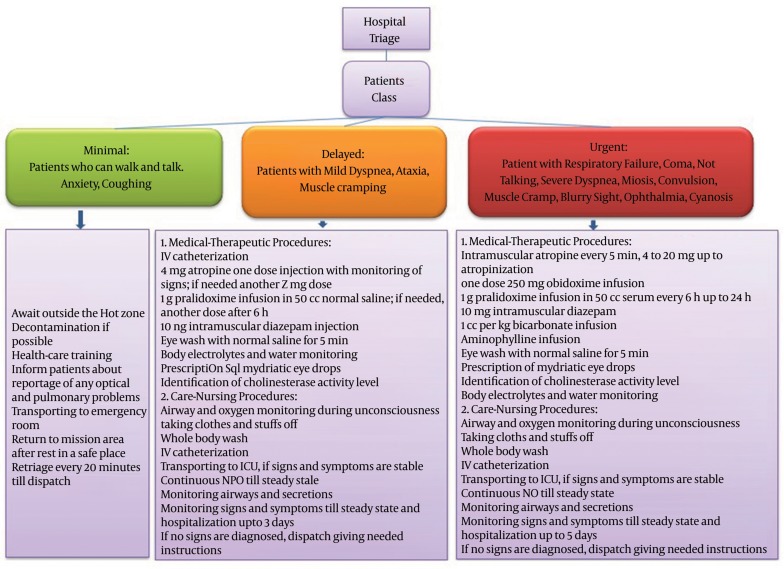
It was possible to use the strengths of existing triage systems for proposing a new protocol for the triage of nerve agents. Agreed protocols were: 1- classification and selection of the colors to designate seriousness of exposure at the scene (Table 1), 2- care-therapy-transport (Triage).
Table 1. Classification and Selection of the Colors to Designate Seriousness of Exposure at the Scene.
| Class | Color |
|---|---|
| Expectant | Black |
| Minimal | Green |
| Delayed | Yellow |
| Urgent | Red |
Figure 1. Extracted Protocol for Field Triage Algorithm.
Figure 2. Extracted Protocol for Hospital Triage Algorithm.
4. Conclusions
Systematic review is a useful tool to combine research findings and facilitate clinical decision making. The triage protocol proposed in the present review can be used in disastrous war conditions in field, while other traditional triage system may be used in hospital. In most triage systems, the first step is identification of individuals who have the ability to walk. In most cases, these individuals are considered as minimally injured. It is necessary to note that many of these patients leave the scene and will refer to health centers, and cause crowding in hospitals. On the other hand, these patients may require immediate or delayed treatment (1). In order to solve these problems and avoid self-triage of patients, the present proposed system recommends that patients are informed about possible early symptoms such as eye and respiratory symptoms, and a retriage is performed on site. Hence, if patients need immediate or delayed treatment, necessary actions will be performed, and these patients are not excluded from the triage system because of having the ability to walk. In all systems studied, life-saving interventions are considered during the initial stages of triage. In particular, all systems emphasize on opening the airway of patients before assigning them to the dead group. In the present triage system, airway control and administering specific antidotes of nerve agents such as atropine and obidoxime are initial components before assigning patients to the dead group.
As mentioned in the results, red, yellow, green, and black colors were set for urgent, delayed, minimal, and expectant classes. However, there is a fifth class within some protocols named emergency class, in which patients who need a plan to survive several minutes after injury are categorized. However, sophisticated plans have limited resources in accelerating the rescue performance and increasing the output of medical team. Therefore, the experts involved in designing the current protocol agreed to exclude the fifth class (18).
Signs and symptoms of the expectant class from studied protocols match our study. Impaired breathing was mentioned as a constant feature of expectant class in all of the analyzed triage systems. US department of health and human services accepted walking and talking victims for the minimal class. Seemingly, published minimal symptoms under supervision of this department are applicable while secretions are decreased and breathing conditions are improved according to retriage of the urgent class. Spontaneous ventilation has also been mentioned as a sign of this class by Jagminas and Erdman (19). Convulsion, vomiting, severe breathing problems, choking, nausea, muscular spasms, shock, dyspnea, and asthenia along with nervous tics and coma are also considered as symptoms of the urgent class (20).
Sidell (21) have reported that some patients might survive if intensive care is performed. They administered 2 mg atropine and if possible obidoxime along with several doses of MARK 1 KIT (21). In emergency class, some protocols suggest prescription of MARK 1 kit containing 2 mg of atropine and 600 mg of pralidoxime chloride which can be self-injected along with additional 2 mg doses until atropinization (22).
Wiener and Hoffman mentioned the use of MARK 1 kit until atropinization signs after decontamination, according to the US military service recommendations. It has also been reported that after Tokyo chemical attack, only 21 out of 107 cases were injected with atropine doses above 2 mg (up to a maximum of 9 mg) (23). Also, oral prescription of benzodiazepines (in case of Somanagent) can be used in combination with atropine and diazepam (24). Pralidoxime can be prescribed for VX and Sarin agents while oral benzodiazepines along with 600 mg of oxime are combined with 100 mL of normal saline for 20 - 30 minutes for other nerve agents. Diazepam in combination with atropine and oxime can be administered for Soman (23). Sidell agreed to use MARK 1 kit with diazepam (21). For other agents of VX family, pralidoxime should be used. Eye drops at war field are prohibited. Also, injection of diazepam 10 mg is necessary (6).
Acknowledgments
Authors would like to thank the chemical injuries research center and nursing school of the Baqiyatallah University of Medical Sciences for their support. We sincerely acknowledge officials and staff of the institutions who were involved, and experts who helped us in preparing the present triage instructions.
Footnotes
Authors’ Contributions:Mohammad Ali Khoshnevis: acquisition of data, analysis and interpretation of data. Jafar Aslani: study supervision, study concept and design. Yunes Panahi: drafting of the manuscript, critical revision of the manuscript for important intellectual content. Mostafa Ghanei: drafting of the manuscript, critical revision of the manuscript for important intellectual content. Hojat Borna: drafting of the manuscript, analysis and interpretation of data. Amirhossein Sahebkar: contribution to the writing of the manuscript and revision.
Funding/Support:This study was conducted with financial support and supervisions of chemical injuries research center of Baqiyatallah University of Medical Sciences.
References
- 1.Burris DG, Welling DR, Rich NM. Dominique Jean Larrey and the principles of humanity in warfare. J Am Coll Surg. 2004;198(5):831–5. doi: 10.1016/j.jamcollsurg.2003.12.025. [DOI] [PubMed] [Google Scholar]
- 2.Niska RW, Burt CW. Bioterrorism and mass casualty preparedness in hospitals: United States, 2003. Adv Data. 2005;(364):1–14. [PubMed] [Google Scholar]
- 3.Jasper E, Miller M, Sweeney B, Berg D, Feuer E, Reganato D. Preparedness of hospitals to respond to a radiological terrorism event as assessed by a full-scale exercise. J Public Health Manag Pract. 2005;Suppl:S11–6. doi: 10.1097/00124784-200511001-00003. [DOI] [PubMed] [Google Scholar]
- 4.Treat KN, Williams JM, Furbee PM, Manley WG, Russell FK, Stamper CJ. Hospital preparedness for weapons of mass destruction incidents: an initial assessment. Ann Emerg Med. 2001;38(5):562–5. doi: 10.1067/mem.2001.118009. [DOI] [PubMed] [Google Scholar]
- 5.Young CF, Persell DJ. Biological, chemical, and nuclear terrorism readiness: major concerns and preparedness of future nurses. Disaster Manag Response. 2004;2(4):109–14. doi: 10.1016/j.dmr.2004.08.010. [DOI] [PubMed] [Google Scholar]
- 6.Ali J. Chemical weapons and the Iran‐Iraq war: A case study in noncompliance. The Nonproliferation Review. 2001;8(1):43–58. doi: 10.1080/10736700108436837. [DOI] [Google Scholar]
- 7.Cone DC, Koenig KL. Mass casualty triage in the chemical, biological, radiological, or nuclear environment. Eur J Emerg Med. 2005;12(6):287–302. doi: 10.1097/00063110-200512000-00009. [DOI] [PubMed] [Google Scholar]
- 8.Ganesan K, Raza SK, Vijayaraghavan R. Chemical warfare agents. J Pharm Bioallied Sci. 2010;2(3):166–78. doi: 10.4103/0975-7406.68498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Okumura T, Suzuki K, Fukuda A, Kohama A, Takasu N, Ishimatsu S, et al. The Tokyo subway sarin attack: disaster management, Part 1: Community emergency response. Acad Emerg Med. 1998;5(6):613–7. doi: 10.1111/j.1553-2712.1998.tb02470.x. [DOI] [PubMed] [Google Scholar]
- 10.Aas P. Future considerations for the medical management of nerve-agent intoxication. Prehosp Disaster Med. 2003;18(3):208–16. doi: 10.1017/s1049023x00001072. [DOI] [PubMed] [Google Scholar]
- 11.Macintyre AG, Christopher GW, Eitzen EJ, Gum R, Weir S, DeAtley C, et al. Weapons of mass destruction events with contaminated casualties: effective planning for health care facilities. JAMA. 2000;283(2):242–9. doi: 10.1001/jama.283.2.242. [DOI] [PubMed] [Google Scholar]
- 12.Lerner EB, Schwartz RB, Coule PL, Weinstein ES, Cone DC, Hunt RC, et al. Mass casualty triage: an evaluation of the data and development of a proposed national guideline. Disaster Med Public Health Prep. 2008;2 Suppl 1:S25–34. doi: 10.1097/DMP.0b013e318182194e. [DOI] [PubMed] [Google Scholar]
- 13.Start Triage. 2007. Available from: http://www.start-triage.com.
- 14.Hodgetts TJ, Mackway-Jones K. Major Incident Medical Management and Support: The Practical Approach. London: BMJ Publishing; 1995. [Google Scholar]
- 15.Garner A, Lee A, Harrison K, Schultz CH. Comparative analysis of multiple-casualty incident triage algorithms. Ann Emerg Med. 2001;38(5):541–8. doi: 10.1067/mem.2001.119053. [DOI] [PubMed] [Google Scholar]
- 16.Sacco WJ, Navin DM, Fiedler KE, Waddell R2, Long WB, Buckman RJ. Precise formulation and evidence-based application of resource-constrained triage. Acad Emerg Med. 2005;12(8):759–70. doi: 10.1197/j.aem.2005.04.003. [DOI] [PubMed] [Google Scholar]
- 17.Benson M, Koenig KL, Schultz CH. Disaster triage: START, then SAVE--a new method of dynamic triage for victims of a catastrophic earthquake. Prehosp Disaster Med. 1996;11(2):117–24. doi: 10.1017/s1049023x0004276x. [DOI] [PubMed] [Google Scholar]
- 18.US Departments of the Army Navy and Air Force. In: NATO Handbook on the Medical Aspects of NBC Defensive Operations. US Departments of the Army NAAF, editor. Washington, DC: 1996. pp. 44–151. [Google Scholar]
- 19.Jagminas L, Erdman DP. CBRNE - Evaluation of a Chemical Warfare Victim, Emedicine. Medscape; 2006. Available from: http://www.emedicine.com/emerg/topic892.htm. [Google Scholar]
- 20.Leikin JB, Thomas RG, Walter FG, Klein R, Meislin HW. A review of nerve agent exposure for the critical care physician. Crit Care Med. 2002;30(10):2346–54. doi: 10.1097/01.CCM.0000029196.42315.83. [DOI] [PubMed] [Google Scholar]
- 21.Sidell F. Management of Chemical Warfare Agent Casualties: A Handbook for Emergency Medical Services. Maryland: Bel Air, MD: HB Publishing; 1995. [Google Scholar]
- 22.Berkman ND, Sheridan SL, Donahue KE, Halpern DJ, Viera A, Crotty K, et al. Articles by Database Search. Bulletin board AHRQ launches health literacy measurement tools. J AHIMA. 2009;80(3):12. [Google Scholar]
- 23.Wiener SW, Hoffman RS. Nerve agents: a comprehensive review. J Intensive Care Med. 2004;19(1):22–37. doi: 10.1177/0885066603258659. [DOI] [PubMed] [Google Scholar]
- 24.Wattana M, Bey T. Mustard gas or sulfur mustard: an old chemical agent as a new terrorist threat. Prehosp Disaster Med. 2009;24(1):19–29. doi: 10.1017/s1049023x0000649x. [DOI] [PubMed] [Google Scholar]