Abstract
Background:
The optimal technique for operative fixation of humeral shaft fractures remains controversial and warrants research.
Objectives:
The purpose of the current study was to compare the functional and clinical outcomes of conventional open reduction and internal fixation (ORIF) with minimally invasive plate osteosynthesis (MIPO) in patients with fractures in two-third distal humeral shaft.
Patients and Methods:
In the current prospective case-control study, 65 patients with humeral shaft fractures were treated using ORIF (33 patients) or MIPO (32 patients). Time of surgery, time of union, incidence of varus deformity and complications were compared between the two groups. Also, the university of California-Los Angeles (UCLA) shoulder rating scale and Mayo Elbow performance score (MEPS) were used to compare the functional outcomes between the two groups.
Results:
The median of union time was shorter in the MIPO group (4 months versus 5 months). The time of surgery and functional outcomes based on the UCLA and MEPS scores were the same. The incidence of varus deformity was more than 5° and was higher and the incidence of nonunion, infection and iatrogenic radial nerve injury were lower in the MIPO group; however, the differences were not significant.
Conclusions:
Due to the shorter union time, to some extent less complication rate and comparable functional and clinical results, the authors recommend to use the MIPO technique in treating the mid-distal humeral shaft fracture.
Keywords: Humeral Shaft; Minimally Invasive Surgical Procedures; Humerus, Internal Fracture Fixation
1. Background
Humeral shaft fracture is one of the common injuries encountered in orthopedic surgery (1) accounting for 1% - 5% of all fractures (2-4). Although nonoperative treatment of humeral shaft fracture is associated with satisfying clinical and functional outcomes in most cases (5-8), usually results in varus deformity and limitation of shoulder and elbow motion in some patients (5, 9, 10). Thus, orthopedic surgeons prefer operative management due to early return to function and low compliance of the patients.
Although several techniques have been introduced for operative fixation of humeral shaft fractures, there is no consensus over the optimal technique. However, plate osteosynthesis remains the standard technique for fixation of humeral shaft fractures (11). Recently, minimally invasive plate osteosynthesis (MIPO) techniques showed encouraging results compared to open conventional techniques due to preservation of biological media of the fracture site (12, 13). However, close proximity of neurovascular structures to humeral bone have raised concerns about the appropriateness of MIPO techniques in this region. Thus, some surgeons recommend the use of anterior approach to the surface of the humerus to avoid neurovascular injuries.
2. Objectives
The current study aimed to compare the functional and clinical outcomes of conventional open reduction and internal fixation (ORIF) versus MIPO in treating two-third distal humeral shaft fractures.
3. Patients and Methods
This prospective study was performed on 68 patients with closed unstable mid-distal humeral shaft fractures referred to our referral center and underwent either ORIF or MIPO between November 2008 and December 2011. The fractures were classified based on the AO/ASIF (Arbeitsgemeinschaft fuer Osteosynthesefragen/ association for the study of internal fixation) classification system. All operations were performed by the same surgeon. Before the operation, a written informed consent was obtained from all patients. The patients with open fracture, fractures extended to shoulder and elbow joints, preoperative radial nerve injury and pathological fractures were excluded. Patients were randomly assigned to the MIPO or ORIF groups using the random number table.
In the MIPO technique, after positioning the patient in the supine or breech position, a pad was placed beneath the scapula to elevate the limb, and the arm was draped free to facilitate access to the shoulder and elbow. While the limb was supported on an arm board, the forearm positioned in supination and the elbow flexed 70°, a 3 - 4 cm incision was made 5 cm distal to the acromion along the anterior border of the deltoid muscle and palpable lateral border of the biceps brachii. Distally a 3 - 4cm incision was made on the anterior surface of the arm along the lateral border of the biceps, extending to within 5 cm proximal to the flexion crease. Then, the biceps muscle was retracted medially to expose the musculocutaneous nerve, between the biceps and the brachialis muscle. In the depth of the incision, the brachialis was exposed and splitted longitudinally to the bone, the medial half was retracted medially accompanying the musculocutaneous nerve and the lateral half was retracted laterally to protect the radial nerve. Then a sub-brachialis tunnel was created from each incision to the fracture site over the periosteum deep to the brachialis muscle. To minimize the risk of iatrogenic radial nerve injury, care was taken to pass the periosteal elevator anteriorly or anteromedially to avoid using lever retractors and to use gentle traction and manipulation for reduction. A 4.5-mm narrow dynamic compression plate (DCP) with 9 - 14 holes (depending on the length of the fracture) was gently inserted through the submuscular tunnel from proximal or distal incision (based on the location of the fracture). After reducing the fracture by applying gentle traction and abduction, a screw was inserted in the distal fragment, the quality of reduction was evaluated using an image intensifier. If the reduction was acceptable, a second screw was inserted in the proximal fragment. Then, one or two more screws were inserted on each side of the fracture to make the fixation more secure.
In the ORIF group, the plate was placed through either the conventional anterolateral or the posterior approach according to the fracture site. The patients were placed in supine and side-lying position for anterolateral and posterior approach, respectively. Four patients were operated on through the posterior approach. The other steps were similar to the MIPO technique.
In both groups, the time of surgery was recorded. After surgery, the arm was supported in a sling for 6 weeks. The patient started elbow and active shoulder exercises at the third postoperative day. Monthly clinical evaluations were performed until complete healing was achieved with the absence of pain at the fracture site and the presence of three bridging cortices on images in two orthogonal planes (Figures 1, 2, 3 and 4). Nonunion was defined as the absence of clinical and radiographic evidence of union up to 9 months.
Figure 1. A, Preoperative X-Ray of a Patient With Severe Angulation Treated Using the Minimally Invasive Plate Osteosynthesis Technique; B, PostOperative Anteroposterior and Lateral Radiographic Views Showing Solid Union of the Fracture With a Proper Alignment.

Figure 2. A, Preoperative Anteroposterior X-Ray Showing Angulated Fracture in Humeral Diaphysis; B, The Patient Underwent Minimally Invasive Plate Osteosynthesis and the Fracture United Successfully.
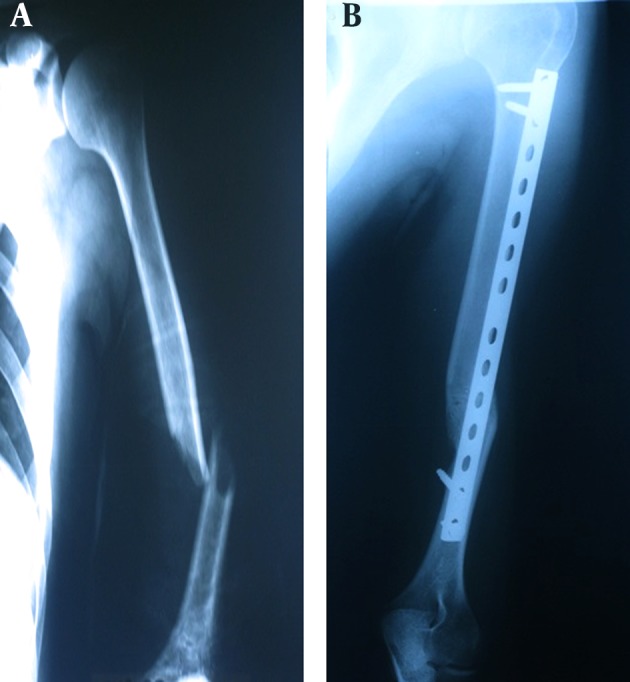
Figure 3. A, Preoperative Angulated Fracture in Humeral Diaphysis; B, Postoperative X-Rays (Arm is Rotated).
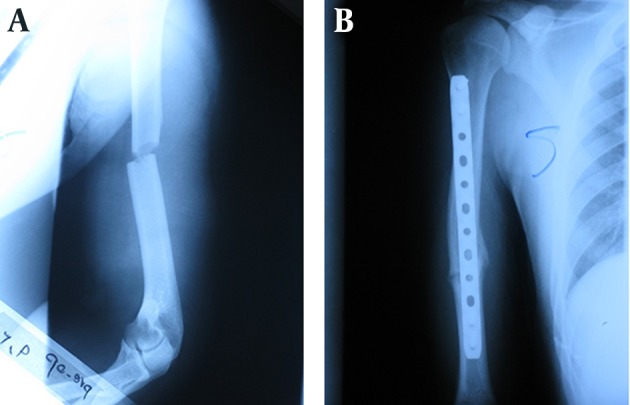
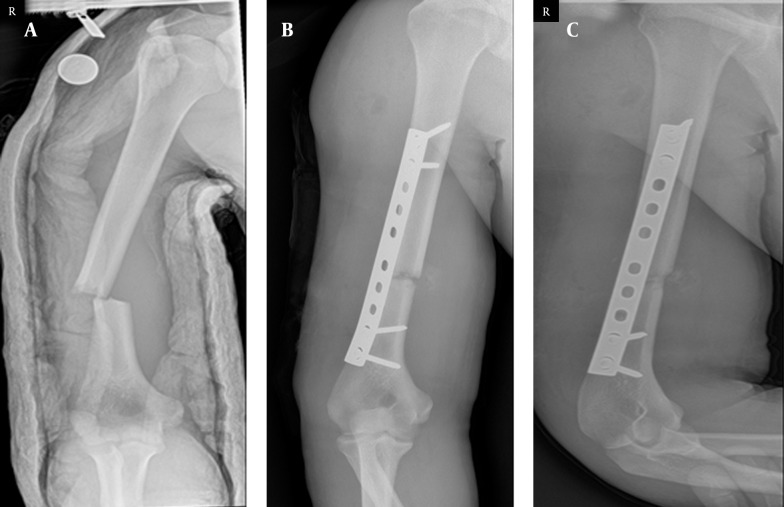
Figure 4. A, Preoperative; and B and C, Postoperative X-Rays.
At the final visit, participants were referred to another orthopedic surgeon to assess the university of California-Los Angeles (UCLA) shoulder rating scale (35 points) and Mayo Elbow performance score (MEPS) (100 points).
The incidence of nonunion and malunion (in sagittal and coronal planes), the incidence of iatrogenic neurovascular injury, shoulder and elbow range of motion, the time of surgery and the UCLA and MEPS scores were compared.
Statistical analysis was performed using SPSS statistical software (version 15.0; SPSS, Chicago, Illinois, USA). Independent samples t-test or Mann-Whitney U test were used to compare the quantitative variables. The qualitative variables were compared using the chi-square test. P < 0.05 was considered statistically significant.
4. Results
One of the patients in the MIPO group and two patients in the ORIF group did not complete the study and were excluded. The characteristics of the remaining patients are presented and compared in Table 1. As is shown, there were no significant differences between the two groups in terms of age, sex, mechanism and type of fracture, and preoperative radial nerve injury.
Table 1. Comparison of Demographic and Underlying Characteristics of the Two Groups a.
| Parameters | Groups | P Value | |
|---|---|---|---|
| MIPO (N = 32) | ORIF (N = 33) | ||
| Age, y | 0.239 | ||
| Mean ± SD | 33.4 ± 10.6 | 34.6 ± 12.1 | |
| Range | 15 - 53 | 16 - 56 | |
| Gender b | 0.835 | ||
| Male | 24 (75) | 24 (72.7) | |
| Female | 8 (25) | 9 (27.3) | |
| Fracture type b | 0.825 | ||
| A | 10 (31.25) | 12 (36.4) | |
| B | 9 (28.1) | 10 (30.3) | |
| C | 13 (40.65) | 11 (33.3) | |
| Mechanisms of fracture b | 0.16 | ||
| Motor-vehicle accident | 11 (34.4) | 12 (36.4) | |
| Falling down | 5 (15.6) | 11 (33.3) | |
| Sport activity | 16 (50) | 10 (30.3) | |
a Abbreviations: MIPO, minimally invasive plate osteosynthesis; and ORIF, open reduction internal fixation.
b Data are presented as No. (%).
The time of surgery was shorter in the MIPO group; however, the difference was not statistically significant. Our results indicated that the median of union time was 4 months (range: 3-6 months) in the MIPO group and 5 months (range: 3 - 11 months) in the ORIF group. The functional outcomes according to UCLA and MEPS scores were not statistically different (Table 2). There were 6 (18.7%) and 2 (6%) patients with varus deformity more than 5° in the MIPO and ORIF groups, respectively (P = 0.12), while the varus angulation did not exceeded 7° in any of the patients. Also, varus deformity smaller than 5° was found in 3 (9%) and 7 (21.2%) patients in the MIPO and ORIF groups, respectively (P = 0.303). Although, the incidence of nonunion, infection, and iatrogenic radial nerve injuries were greater in the ORIF group, the difference was not statistically significant (Table 2). We found that the radial nerve was contused in all patients with preoperative radial nerve injuries and improved in the follow-up.
Table 2. Comparison of Surgical Factors, Functional Outcomes and Complications a.
| Parameters | Groups | P Value | |
|---|---|---|---|
| MIPO (N = 32) | ORIF (N = 33) | ||
| Time Of surgery, min | 0.118 | ||
| Mean ± SD | 93.9 ± 23.9 | 106.5 ± 27.2 | |
| Range | 48 - 151 | 58 - 173 | |
| UCLA scale | 0.215 | ||
| Range | 33.1 ± 1.5 | 32.8 ± 1.1 | |
| Mean ± SD | 29 - 35 | 30 - 35 | |
| MEPS | 0.528 | ||
| Range | 96.6.1 ± 5.1 | 96.9 ± 6.8 | |
| Mean ± SD | 80 - 100 | 80 - 100 | |
| Complications b | 0.355 | ||
| Infection | 0 (0) | 2 (6) | |
| Nonunion | 1 (3) | 3 (9) | |
| Iatrogenic radial nerve injury | 1 (3) | 4 (12) | |
a Abbreviations: MEPS, Mayo elbow performance score; MIPO, minimally invasive plate osteosynthesis; ORIF, open reduction internal fixation; and UCLA, university of California-Los Angeles.
b Data are presented as No. (%).
5. Discussion
The most important finding of the current study was that the union time was shorter in the MIPO technique compared to that of the ORIF and these patients returned to their previous level of daily living activities more quickly. Statistical analyses revealed that the treatment of two-third distal humeral shaft fractures with either the ORIF or MIPO technique resulted in nearly the same functional outcomes.
An et al compared the results of treating mid-distal humeral shaft fractures with ORIF and MIPO in 33 patients. Iatrogenic radial nerve injury occurred in 31.3% of the patients in the ORIF group while none were found in the MIPO group. The mean union time was 15.29 weeks in the MIPO group and 21.25 weeks the ORIF groups; the difference was not statistically significant. Functional outcomes were satisfactory and similar in both groups. An et al. (13) concluded that because of the reduced incidence of iatrogenic nerve injury, accelerated union and similar functional outcomes, the MIPO technique is superior to ORIF in treating humeral shaft fractures. Recently, Oh et al. (14) in a similar prospective study found that the primary union rate (95.6% in the MIPO group and 90% in the ORIF group) and the functional outcomes were the same. The mean operation time was significantly shorter in the MIPO group (110 minutes versus 169 minutes). There were 5 patients in the ORIF group and no patient in the MIPO group that required bone grafting (14).
Even though humeral shaft fractures in most of the cases heal effectively when conservative treatment is applied (15, 16), in certain circumstances, surgical treatment is inevitable (17). Sarmiento et al. (10), in 2000 demonstrated that using functional bracing for treating closed fractures of the humeral diaphysis resulted in a high rate of union due to the hydraulic impacts of the soft tissues. However, considerable limitations in shoulder and elbow mobility and certain residual angular deformities have been reported with functional bracing (5, 9, 10) which makes returning to usual daily activities difficult.
Because of strength and load-sharing characteristics, minimal soft tissue dissection and lower risk of radial nerve damage, intramedullary (IM) nailing has yielded good results (18-22). However, this treatment also has its own limitations (23, 24). Moreover, the insertion of nails from humeral head or olecranon fossa can produce shoulder impingement or elbow fracture, (25-28). Humeral plating has been accepted as the standard technique for fixation of humeral shaft fractures (11, 13, 29). The technique has certain advantages such as lower reoperation rate, high union rate, anatomical reduction and less shoulder and elbow morbidities (30, 31). However, surgeons tend to use MIPO due to certain disadvantages with humeral plating such as extensive incision, increased risk of infection, cosmetic problems, high incidence of iatrogenic radial nerve injury, disruption of periosteal blood supply and violation of the fracture site hematoma (1, 3, 32-34). Minimally invasive plate osteosynthesis requires two small incisions which theoretically minimizes the soft tissue injury and subsequent infection and cosmetic problems. With the anterior approach and insertion of the plate far from the radial nerve, decreased neurovascular injury is expected. Also, the periosteum and fracture site hematoma remain intact which can promote union rate and speed up the union time. Moreover, MIPO requires fewer screws reducing the cost of treatment. These theoretical advantages of MIPO have been addressed by several recent studies (13, 35-39).
Malhan et al. (2) in a prospective study investigated the outcomes of MIPO using a locking compression plate (LCP) in 42 patients and found that disabilities of arm, shoulder & hand score (DASH score) improved significantly after 1 year. The mean angulation was 4° and 7° in coronal and sagittal planes. Except two cases with delayed union, all fractures united after 14 weeks and one iatrogenic radial nerve palsy occurred (2). Also, Shin et al. (40) introduced a modified MIPO technique for humeral shaft fractures with no iatrogenic radial nerve injury and good clinical and functional outcomes. They concluded that although the MIPO technique for humeral shaft fractures is technically demanding, satisfactory clinical outcomes and shoulder and elbow function can be obtained.
In the current study, we found that the median of union time was shorter in the MIPO group (4 months versus 5 months) which has also been observed in the study by An et al. (13). Although we found no other significant differences between the two groups, the time of surgery was shorter (93.9 min versus 106.5 min) and the rate of infection (0% versus 6%) and iatrogenic radial nerve injury (3% versus 12%) were lower in the MIPO group. Functional outcomes and incidence of nonunion were the same in two groups. The incidence of varus deformity more than 5° was greater in the MIPO group; however, the difference was not significant.
Some surgeons are concerned with the MIPO technique as it can result in varus malunion. However, we found that considerable varus deformity did not occur in our patients. Furthermore, this mild varus angulation did not affect the functional outcome due to wide range of shoulder and elbow motion. Another concern is the potential risk of iatrogenic neurovascular injury which can be avoided by applying two technical tricks. In pronation, radial nerve moves closer to plate; so, the forearm must be positioned in supination (35). Also, the surgeons should consider that some authors caution against a danger zone which can reduce the risk of the iatrogenic neurovascular injury (38, 41). Apivatthakakul et al. (41) tried to find the safe location for screw insertion in the MIPO technique to decrease the risk of neurovascular injury in patients with humeral shaft fractures. They demonstrated that a danger zone for musculocutaneaous and radial nerves are located at 18.37% - 42.67% and 36.35% - 59.2% of the humeral length from the lateral epicondyle, respectively (41). Otherwise, radial nerve exploration through a small incision is technically difficult. So, in our opinion using MIPO technique in such cases is questionable.
The current study was limited by the small sample size and nonrandomized sampling. Also, we could not compare the outcomes in separated fracture types because of the limited number of the patients. In conclusion, the findings of the present study show that the MIPO technique is superior to ORIF due to the shorter union time, to some extent less complication rate and comparable functional and clinical results; thus, we conclude that the MIPO technique can be effective in treating mid-distal humeral shaft fracture when performed by an experienced surgeon.
Footnotes
Authors’ Contributions:Ali Akbar Esmailiejah: study concept and design, acquisition of data, critical revision of the manuscript for important intellectual content, and study supervision. Mohammad Reza Abbasian: acquisition of data, drafting of the manuscript, and administrative, technical, and material support. Farshad Safdari: acquisition of data, analysis and interpretation of data, drafting of the manuscript, and statistical analysis. Keyqobad Ashoori: acquisition of data, critical revision of the manuscript for important intellectual content, administrative, technical, and material support, and study supervision.
References
- 1.Paris H, Tropiano P, Clouet D'orval B, Chaudet H, Poitout DG. [Fractures of the shaft of the humerus: systematic plate fixation. Anatomic and functional results in 156 cases and a review of the literature]. Rev Chir Orthop Reparatrice Appar Mot. 2000;86(4):346–59. [PubMed] [Google Scholar]
- 2.Malhan S, Thomas S, Srivastav S, Agarwal S, Mittal V, Nadkarni B, et al. Minimally invasive plate osteosynthesis using a locking compression plate for diaphyseal humeral fractures. J Orthop Surg (Hong Kong). 2012;20(3):292–6. doi: 10.1177/230949901202000305. [DOI] [PubMed] [Google Scholar]
- 3.Cole PA, Wijdicks CA. The operative treatment of diaphyseal humeral shaft fractures. Hand Clin. 2007;23(4):437–48. doi: 10.1016/j.hcl.2007.11.004. [DOI] [PubMed] [Google Scholar]
- 4.Ekholm R, Adami J, Tidermark J, Hansson K, Tornkvist H, Ponzer S. Fractures of the shaft of the humerus. An epidemiological study of 401 fractures. J Bone Joint Surg Br. 2006;88(11):1469–73. doi: 10.1302/0301-620X.88B11.17634. [DOI] [PubMed] [Google Scholar]
- 5.Kapil Mani KC, Gopal Sagar DC, Rijal L, Govinda KC, Shrestha BL. Study on outcome of fracture shaft of the humerus treated non-operatively with a functional brace. Eur J Orthop Surg Traumatol. 2013;23(3):323–8. doi: 10.1007/s00590-012-0982-3. [DOI] [PubMed] [Google Scholar]
- 6.Mahabier KC, Vogels LM, Punt BJ, Roukema GR, Patka P, Van Lieshout EM. Humeral shaft fractures: retrospective results of non-operative and operative treatment of 186 patients. Injury. 2013;44(4):427–30. doi: 10.1016/j.injury.2012.08.003. [DOI] [PubMed] [Google Scholar]
- 7.Liu GY, Zhang CY, Wu HW. Comparison of initial nonoperative and operative management of radial nerve palsy associated with acute humeral shaft fractures. Orthopedics. 2012;35(8):702–8. doi: 10.3928/01477447-20120725-10. [DOI] [PubMed] [Google Scholar]
- 8.Gosler MW, Testroote M, Morrenhof JW, Janzing HM. Surgical versus non-surgical interventions for treating humeral shaft fractures in adults. Cochrane Database Syst Rev. 2012;1:CD008832. doi: 10.1002/14651858.CD008832.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Papasoulis E, Drosos GI, Ververidis AN, Verettas DA. Functional bracing of humeral shaft fractures. A review of clinical studies. Injury. 2010;41(7):e21–7. doi: 10.1016/j.injury.2009.05.004. [DOI] [PubMed] [Google Scholar]
- 10.Sarmiento A, Zagorski JB, Zych GA, Latta LL, Capps CA. Functional bracing for the treatment of fractures of the humeral diaphysis. J Bone Joint Surg Am. 2000;82(4):478–86. doi: 10.2106/00004623-200004000-00003. [DOI] [PubMed] [Google Scholar]
- 11.McKee MD, Larsson S. Humeral shaft Fractures. Rockwood and Green's fractures in adults. Phildelphia: Lippincott Williams & Wilkins; 2010. [Google Scholar]
- 12.Siegel J, Tornetta P3, Borrelli JJ, Kregor P, Ricci WM. Locked and minimally invasive plating. Instr Course Lect. 2007;56:353–68. [PubMed] [Google Scholar]
- 13.An Z, Zeng B, He X, Chen Q, Hu S. Plating osteosynthesis of mid-distal humeral shaft fractures: minimally invasive versus conventional open reduction technique. Int Orthop. 2010;34(1):131–5. doi: 10.1007/s00264-009-0753-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Oh CW, Byun YS, Oh JK, Kim JJ, Jeon IH, Lee JH, et al. Plating of humeral shaft fractures: comparison of standard conventional plating versus minimally invasive plating. Orthop Traumatol Surg Res. 2012;98(1):54–60. doi: 10.1016/j.otsr.2011.09.016. [DOI] [PubMed] [Google Scholar]
- 15.Ekholm R, Tidermark J, Tornkvist H, Adami J, Ponzer S. Outcome after closed functional treatment of humeral shaft fractures. J Orthop Trauma. 2006;20(9):591–6. doi: 10.1097/01.bot.0000246466.01287.04. [DOI] [PubMed] [Google Scholar]
- 16.Toivanen JA, Nieminen J, Laine HJ, Honkonen SE, Jarvinen MJ. Functional treatment of closed humeral shaft fractures. Int Orthop. 2005;29(1):10–3. doi: 10.1007/s00264-004-0612-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Green A, Reid JP, DuWayne AC. Fractures of the humerus. Orthopeadic knowledge update: trauma 3.. Rosenmont: American Academy of Orthopedic Surgeons; 2000. [Google Scholar]
- 18.Habernek H, Orthner E. A locking nail for fractures of the humerus. J Bone Joint Surg Br. 1991;73(4):651–3. doi: 10.1302/0301-620X.73B4.2071653. [DOI] [PubMed] [Google Scholar]
- 19.Foster RJ, Dixon GJ, Bach AW, Appleyard RW, Green TM. Internal fixation of fractures and non-unions of the humeral shaft. Indications and results in a multi-center study. J Bone Joint Surg Am. 1985;67(6):857–64. [PubMed] [Google Scholar]
- 20.Bell MJ, Beauchamp CG, Kellam JK, McMurtry RY. The results of plating humeral shaft fractures in patients with multiple injuries. The Sunnybrook experience. J Bone Joint Surg Br. 1985;67(2):293–6. doi: 10.1302/0301-620X.67B2.3980544. [DOI] [PubMed] [Google Scholar]
- 21.Vander Griend R, Tomasin J, Ward EF. Open reduction and internal fixation of humeral shaft fractures. Results using AO plating techniques. J Bone Joint Surg Am. 1986;68(3):430–3. [PubMed] [Google Scholar]
- 22.Putti AB, Uppin RB, Putti BB. Locked intramedullary nailing versus dynamic compression plating for humeral shaft fractures. J Orthop Surg (Hong Kong). 2009;17(2):139–41. doi: 10.1177/230949900901700202. [DOI] [PubMed] [Google Scholar]
- 23.McCormack RG, Brien D, Buckley RE, McKee MD, Powell J, Schemitsch EH. Fixation of fractures of the shaft of the humerus by dynamic compression plate or intramedullary nail. A prospective, randomised trial. J Bone Joint Surg Br. 2000;82(3):336–9. doi: 10.1302/0301-620x.82b3.9675. [DOI] [PubMed] [Google Scholar]
- 24.Chapman JR, Henley MB, Agel J, Benca PJ. Randomized prospective study of humeral shaft fracture fixation: intramedullary nails versus plates. J Orthop Trauma. 2000;14(3):162–6. doi: 10.1097/00005131-200003000-00002. [DOI] [PubMed] [Google Scholar]
- 25.Riemer BL, D'Ambrosia R, Kellam JF, Butterfield SL, Burke C3. The anterior acromial approach for antegrade intramedullary nailing of the humeral diaphysis. Orthopedics. 1993;16(11):1219–23. doi: 10.3928/0147-7447-19931101-08. [DOI] [PubMed] [Google Scholar]
- 26.Port AM, Nanu AM, Cross AT. Windows for humeral interlocking nails-an anatomical study. J Bone Joint Surg Br. 1997;79(suppl 1):102. [Google Scholar]
- 27.Lin J, Inoue N, Valdevit A, Hang YS, Hou SM, Chao EY. Biomechanical comparison of antegrade and retrograde nailing of humeral shaft fracture. Clin Orthop Relat Res. 1998;(351):203–13. [PubMed] [Google Scholar]
- 28.Rommens PM, Verbruggen J, Broos PL. Retrograde locked nailing of humeral shaft fractures. A review of 39 patients. J Bone Joint Surg Br. 1995;77(1):84–9. [PubMed] [Google Scholar]
- 29.Spiguel AR, Steffner RJ. Humeral shaft fractures. Curr Rev Musculoskelet Med. 2012;5(3):177–83. doi: 10.1007/s12178-012-9125-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bhandari M, Devereaux PJ, McKee MD, Schemitsch EH. Compression plating versus intramedullary nailing of humeral shaft fractures--a meta-analysis. Acta Orthop. 2006;77(2):279–84. doi: 10.1080/17453670610046037. [DOI] [PubMed] [Google Scholar]
- 31.Niall DM, O'Mahony J, McElwain JP. Plating of humeral shaft fractures--has the pendulum swung back? Injury. 2004;35(6):580–6. doi: 10.1016/j.injury.2003.10.021. [DOI] [PubMed] [Google Scholar]
- 32.Walker M, Palumbo B, Badman B, Brooks J, Van Gelderen J, Mighell M. Humeral shaft fractures: a review. J Shoulder Elbow Surg. 2011;20(5):833–44. doi: 10.1016/j.jse.2010.11.030. [DOI] [PubMed] [Google Scholar]
- 33.Lim KE, Yap CK, Ong SC, Aminuddin. Plate osteosynthesis of the humerus shaft fracture an its association with radial nerve injury--a retrospective study in Melaka General Hospital. Med J Malaysia. 2001;56 Suppl C:8–12. [PubMed] [Google Scholar]
- 34.Jawa A, McCarty P, Doornberg J, Harris M, Ring D. Extra-articular distal-third diaphyseal fractures of the humerus. A comparison of functional bracing and plate fixation. J Bone Joint Surg Am. 2006;88(11):2343–7. doi: 10.2106/JBJS.F.00334. [DOI] [PubMed] [Google Scholar]
- 35.Apivatthakakul T, Arpornchayanon O, Bavornratanavech S. Minimally invasive plate osteosynthesis (MIPO) of the humeral shaft fracture. Is it possible? A cadaveric study and preliminary report. Injury. 2005;36(4):530–8. doi: 10.1016/j.injury.2004.05.036. [DOI] [PubMed] [Google Scholar]
- 36.Pospula W, Abu Noor T. Percutaneous fixation of comminuted fractures of the humerus: initial experience at Al Razi hospital, Kuwait. Med Princ Pract. 2006;15(6):423–6. doi: 10.1159/000095487. [DOI] [PubMed] [Google Scholar]
- 37.Yang T, Liu S, Liu Y. [Minimally-invasive locking compression plate to treat complex humeral shaft fracture]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2007;21(8):817–9. [PubMed] [Google Scholar]
- 38.Livani B, Belangero W, Andrade K, Zuiani G, Pratali R. Is MIPO in humeral shaft fractures really safe? Postoperative ultrasonographic evaluation. Int Orthop. 2009;33(6):1719–23. doi: 10.1007/s00264-008-0616-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.An Z, He X, Zeng B. [A comparative study on open reduction and plating osteosynthesis and minimal invasive plating osteosynthesis in treating mid-distal humeral shaft fractures]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2009;23(1):41–4. [PubMed] [Google Scholar]
- 40.Shin SJ, Sohn HS, Do NH. Minimally invasive plate osteosynthesis of humeral shaft fractures: a technique to aid fracture reduction and minimize complications. J Orthop Trauma. 2012;26(10):585–9. doi: 10.1097/BOT.0b013e318254895f. [DOI] [PubMed] [Google Scholar]
- 41.Apivatthakakul T, Patiyasikan S, Luevitoonvechkit S. Danger zone for locking screw placement in minimally invasive plate osteosynthesis (MIPO) of humeral shaft fractures: a cadaveric study. Injury. 2010;41(2):169–72. doi: 10.1016/j.injury.2009.08.002. [DOI] [PubMed] [Google Scholar]