Abstract
Background:
Oral diseases are common chronic diseases that are affected by human health behavior. One-way to promote health behaviors can be achieved through education. The present study aims to assess the effect of an oral health education program using motivational interviewing (MI) method on oral health status of preschool children.
Materials and Methods:
This study recruited 222 volunteer children and their parents from 10 elementary schools into a community trial. At baseline, plaque, gingival and decayed, missing, and filled teeth indexes were measured in the children. They were randomly allocated into test groups where they and their parents received oral health education using MI and the control group received traditional oral health education. The test group had recall and postal reminder during 6 months of the study, but there was no reminder for the control group. After 6 months, the same oral health indexes were measured. Data were analyzed using SPSS version 20 (SPSS Inc., Chicago, IL, USA) by t-test, Mann-Whitney and Wilcoxon signed ranks test. P < 0.05 was considered as significant.
Results:
The results showed that after both oral health education programs, differences of plaque index (PI) (P = 0.000) and gingival index (P = 0.000) were significant between the two groups. The number of children with healthy gingiva and low PI were more frequent in the test group after intervention.
Conclusion:
Considering the limitations of this study, oral health status of children after education of parents using MI was observed, and it should be considered in oral health education programs.
Keywords: Iran, motivational interviewing, oral education, education, preschool children
INTRODUCTION
Health promotion principles were founded on the notion that health is related to behavior, and changing behavior can lead to an improvement. Oral disease including oral cancer, gum disease, and tooth decay are related to lifestyle and personal behavior. If people have appropriate oral health behaviors, the risk of oral diseases will decrease significantly.[1]
Health education could result in behavior change and providing oral health education is the responsibility of dental professionals. In traditional health education methods, most of the clinicians are increasing their patients’ knowledge regardless of their intrinsic motivations. Additionally, it has been shown that education and professional recommendations are not sufficient for changing the behaviors.[2] Therefore, something more than knowledge and education is necessary to improve oral health. In the past decades, different models have been presented for the change in behaviors related to oral health. One of these models is a consultation technique called “motivational interviewing (MI).” MI is a patient-centered consultation which helps them change their behaviors with maximum intrinsic motivation and minimum resistance. This method was first introduced for patients who were addicts (alcohol or tobacco) and since then has been used for changes in lifestyle including diet, exercise and weight loss.[3] Several studies have suggested that MI is effective for changing health behaviors in different populations,[2] and it can also be used to change oral health behaviors.[4]
The MI method of health education is based on a preplanned interview protocol to explore factors which can encourage and persuade health behaviors and also the factors, which could act as a resistance to change. Afterward, an educational schedule will be set for each person according to discovered factors and necessary guidance to achieve educational health purposes. It is also suggested that desired educational notes should be reminded by postal card and reminder calls through a schedule.
Cultural and social context can affect the application of educational methods in different communities; hence, some researchers have suggested that more studies are needed on this issue in different populations.[5,6]
Researchers have studied this method in the field of oral health,[6,7,8] and this study was designed to evaluate the effectiveness of the MI educational method on the oral health status in an Iranian population.
MATERIALS AND METHODS
This study was a community trial which recruited a sample of 222 preschool children, with considering parameter: α = 5%, 1−β = 80% and drop out = 30% and design effect = 1.40 (Power Analysis and Sample Size (PASS), version 13, Number Cruncher Statistical System (NCSS), USA).
All elementary schools (160) were numbered, and 10 schools randomly selected and then allocated into test and control groups after matching for their sex. Figure 1 shows the flow chart of the study. After coordination with the school principals, a meeting was held in the schools for parents to explain the purpose of the study, and then volunteers signed consent forms. There were 250 volunteers from the schools. Children with a history of medical problem, medication and also those who were using a type of a removable appliance such as space maintainer or tongue guard were excluded from the study. Children who were not cooperating for dental examination also were excluded and substituted by another eligible consented child to reach the desirable sample size.
Figure 1.
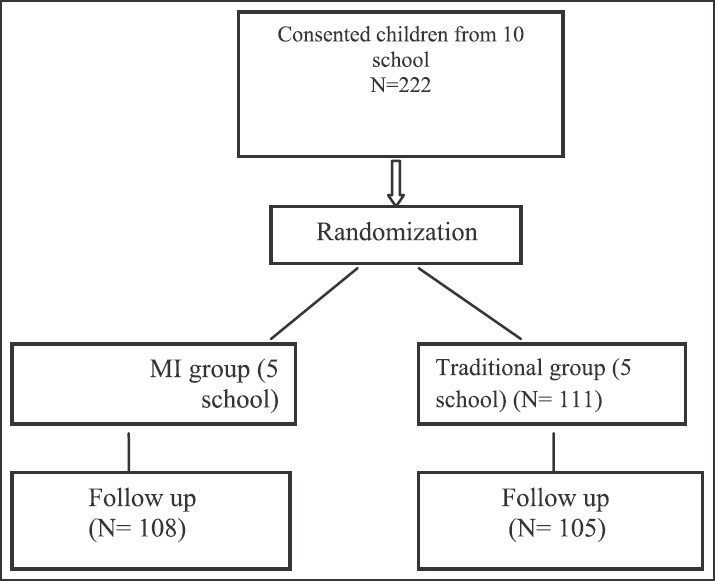
The study flow chart and stages.
The study was approved by Kerman University of Medical Sciences Research Ethics Committee (Code KA 90/265).
All children were examined at baseline by a trained dentist (intra-rater agreement 85%) who was unaware of the children's allocated groups, in school health room or one of the classes. The following oral health indexes were measured.
Rate of microbial plaque accumulation on the tooth surface was measured by standard oral hygiene’ Loe and Silness plaque index (PI).[9] Gingival health of children was measured by standard gingival inflammation index (GI).[10] Dental caries status was assessed using International Caries Detection and Assessment System (ICDAS). The ICDAS detection codes for coronal caries range from 0 to 6 depending on the severity of the lesion.[11]
Dental examination was done on a comfortable chair under a head light. A community periodontal index probe and dental mirror were used. First of all PI and then GI was recorded, after that the teeth surfaces were cleaned with gauzes and probe to record dental surface status codes.
After baseline dental examination, schools were randomly allocated to the test and control group. Children and their parents in the control group received a traditional oral health education program, and test group received the MI education program.
In the MI education program planning, a protocol of Professor Weinstain was used after getting permission and also cross-cultural validity checking through forward and backward translation and also cross-cultural adaptation.[12,13] Some parts were modified in an expert panel to be suitable for target group. The protocol included an interview with one of the child parents (who was more involved with child health issues) in the presence of their child in the school, and its duration was considered about 45 min. The Instruction for an interviewer (a member of the research team) was embedded in the main protocol. It was necessary to train an interviewer for this purpose to manage the time and interview process. The interview included some questions about oral health needs of participant child and other family members, parent wishes for their children oral health, their concern and also barriers to good oral health. The parents could also have a chance to talk about their dental concern, and the interviewer should note and acknowledged the concerns. At the end of the interview, a list of oral health information was shared with the parents.
Finally, a menu of oral health recommendations and goals for the child was prepared in writing and parents were asked to stick it somewhere on the fridge or freezer door by provided magnets. After interview, both the parent and the child watched an 11 min video about tooth eruption, oral health practices including tooth brushing, dental floss, fluoride, diet and regular dental visits. An oral health education lecture was also presented by one of the research assistants and she/he answered their questions if any.
The control group just watched the above-mentioned video and also same lecture by the assistant who was blinded to the group's allocation. Both groups received a package including a toothbrush (Royal child tooth brush, Germany), fluoridated toothpaste (Pooneh, Paksan, Iran) and a dental floss (Mina, Iran) and also an information sheet about oral health. The test group (MI) received reminders [Table 1], but the control group did not receive any reminder.
Table 1.
Timetable of reminder calls and postal cards after interview in MI group
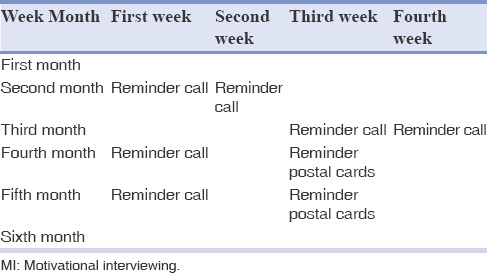
In postcards and call reminders the child special oral health menu was reviewed, and necessary comments were given to the parents.
In the follow-up survey, 6 months after the intervention, oral health indexes (PI, GI and decayed, missing, and filled teeth [dmft]) in both groups were measured by the same examiner and under the same circumstances.
Data were analyzed by SPSS software version 20 (SPSS Inc., Chicago, IL, USA). Mean dmft index were calculated. Code 1 (First visual change in enamel) and code 2 (Distinct visual change in enamel) in ICDAS cods were analyzed separately and code 3 or more were considered as decayed teeth.
Dental health status of participants was compared between and within groups before and after the intervention using independent t-test. Mann-Whitney and Wilcoxon Signed Ranks were used to compare ordinal health variables between and within groups before and after intervention. P < 0.05 was considered as significant.
RESULTS
In total, 222 children and their parents participated in the study (response rate = 92%) with 54.5% (n = 120) girls and 95% (n = 213) of children were followed-up after 6 months. Nine children moved or left the school during the study period. The children age ranged from 4 to 6 years old. The mean dmft was 4.87 ± 4.14 and 4.79 ± 4.39 for all participant children at the baseline and follow-up respectively. Only 49 (22%) of children had healthy gingiva before the intervention. Frequency of poor oral hygiene scores was 62 (55.4%) in the test group before intervention which decreased to 13 (11.7%) after that, and it was 59 (53.2%) in control group before intervention and it decreased to 49 (44.1%) after education. Tables 2 and 3 show frequency distribution of GI and PI indexes among study subjects in both groups before and after intervention.
Table 2.
Gingival health status of children in all groups before and after oral health educations
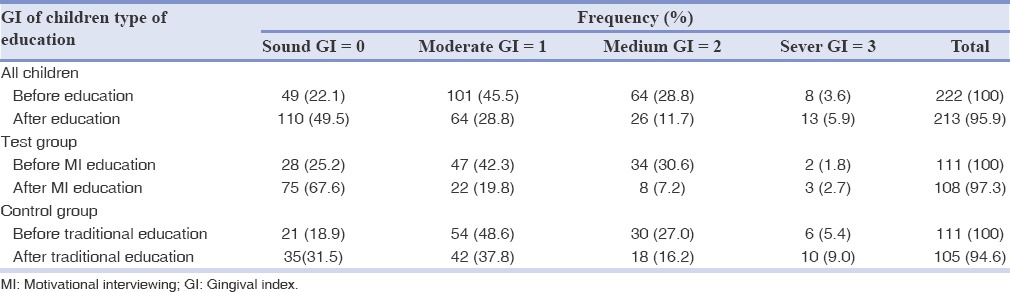
Table 3.
PI of children before and after educations in all groups
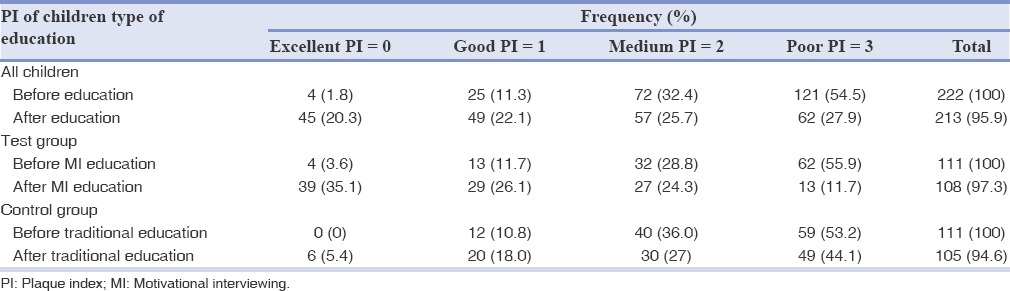
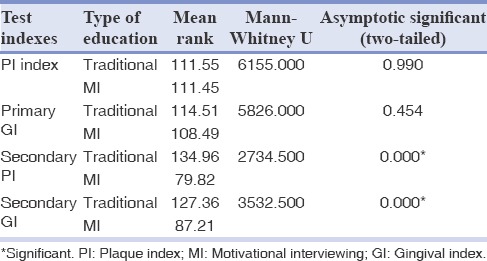
The results of Mann-Whitney test showed a difference of PI and GI were significant between MI and traditional groups after educations [Table 4].
Table 4.
Comparing plaque and GI before and after interventions between two groups
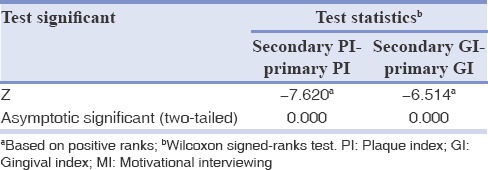
Plaque index and GI showed a significant difference within control and test groups before and after interventions by Wilcoxon test. Tables 5 and 6 show paired test for plaque and GI.
Table 5.
Comparison between PI and GI before and after traditional oral health education
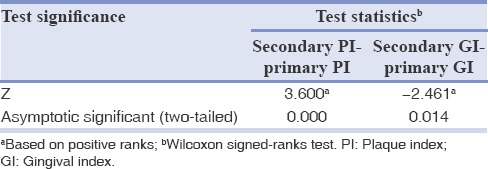
Table 6.
Comparison between PI and GI before and after MI oral health education
Dentition status (mean dmft) did not show a significant difference between and within groups during the study period (P = 0.36).
DISCUSSION
Measuring the outcome of oral health education programs could show the effectiveness of such plans and could help to implement the plan in a wider community. Many models and theories have been used in oral health education, and MI is one of these methods.[7,8,6]
This study sought to explore the difference between the effectiveness of two oral health education programs using MI and traditional methods during a 6 months period. Both programs were effective in promoting oral health status. However, the results showed that oral health education program using MI was more effective than oral health education by the traditional method in improving some oral health indexes such as PI and GI.
According to results, PI and GI did not have a significant difference between two groups at the baseline of the study, while Mann-Whitney test showed significant improvement in PI and GI after interventions. Some previous studies have shown improvement in plaque accumulation and gingival status in both types of education which is similar to the present study.[14,15]
These results confirmed the effectiveness of MI as an educational model. This involved parents actively participating in the program, which is similar to a study that showed individuals receiving MI had a significant improvement in their plaque level compared to people receiving oral health education alone.[16] Gingival health improvement following MI oral health education has also been addressed in other studies.[7]
Some studies have tested the effectiveness of MI on various aspects of oral health.[8,6,17] A review of literature with possible application of MI on improving oral hygiene behavior in periodontics was done in 2010.[7] It concluded that MI enhances self-efficacy about oral hygiene behaviors. A systematic review by Rubak et al. assessed the effectiveness of MI, and it concluded that some behavioral problems and diseases outcome improved in comparison with traditional education. However, it is not possible to judge the robustness of the authors’ conclusions, owing to the limited reporting of review methods and the lack of adequate information on individual studies.[18]
Application of MI into behavior change research should be continued because it is not clear yet how MI has its effect and what elements of MI are essential for the changes.[19] Further research also needs to establish the process of MI and its key components in oral health promotion.
As results showed, dmft scores were not different significantly before and after the intervention in the study. However, other studies have shown that MI is a promising approach that may decrease the risk of new caries.[16] The insignificant difference might be related to the duration of the reported study, which is too short to show an effect on dental caries process. This study used the new ICDAS system for caries assessment, but even detected initial caries had no changes and it may confirm that oral health education programs should be accompanied by preventive approaches such as fluoride application to be effective on early detected caries.
The results of the current study confirmed the effectiveness of MI on improvement of oral health indexes; however, generalization of the findings is limited because the study is cross-sectional, and the sample size is not very large. This method of education should be studied in different ages, and at different economic and social levels. Cost effectiveness and the time expenditure of the method in clinics should be investigated in future studies.
CONCLUSION
Oral health education programs dealing with parents can promote oral health indexes of children such as PI and GI; however, using MI as an oral health education model was significantly more effective than the traditional model. Therefore, new approaches and models should be considered for educating public by dental professionals, and it is necessary to include the relevant knowledge and skills in dental education curriculum.
Financial support and sponsorship
Nil.
Conflicts of interest
The authors of this manuscript declare that they have no conflicts of interest, real or perceived, financial or non-financial in this article.
ACKNOWLEDGMENTS
Authors wish to thank Professor Abbas Bahrampour for his statistical advice and also Dr. Fereshteh Emrani for her help in data collection. Many thanks to Professor Weinstein, who kindly provided original MI protocol to the research team. Our sincere thanks also go to all parents and school managers who were cooperative during the study. Many thanks to Mrs. Shiva Sheikholeslam for her contribution to the study. This report has been extracted from a PhD thesis (n = 66 T) in Kerman Dental School, which was supported financially by Vice Chancellor of Research at Kerman University of Medical Sciences.
REFERENCES
- 1.Schou L, Blinkhorn AS. Oxford, UK: Oxford University Press; 1993. Oral Health Promotion. [Google Scholar]
- 2.Williams KB. Motivational interviewing: Application to oral health behaviors. J Dent Hyg. 2010;84:6–10. [Google Scholar]
- 3.Mostofsky D, Forgione AG, Giddon DB. IOWA, USA: Blackwell Munksgaard; 2006. Behavioral Dentistry. [Google Scholar]
- 4.Emmons KM, Rollnick S. Motivational interviewing in health care settings. Opportunities and limitations. Am J Prev Med. 2001;20:68–74. doi: 10.1016/s0749-3797(00)00254-3. [DOI] [PubMed] [Google Scholar]
- 5.Freudenthal JJ. Motivational interviewing (MI) as an intervention for early childhood caries risk-related behaviors. J Dent Hyg. 2008;82:67–71. [PubMed] [Google Scholar]
- 6.Martins RK, McNeil DW. Review of motivational interviewing in promoting health behaviors. Clin Psychol Rev. 2009;29:283–93. doi: 10.1016/j.cpr.2009.02.001. [DOI] [PubMed] [Google Scholar]
- 7.Nalini HE, Punithavathy R. Motivational interviewing in improving oral hygiene behaviora review of literature with possible application in periodontics. J Indian Acad Dent Spec. 2010;1:12–5. [Google Scholar]
- 8.Campbell MK, Carr C, Devellis B, Switzer B, Biddle A, Amamoo MA, et al. A randomized trial of tailoring and motivational interviewing to promote fruit and vegetable consumption for cancer prevention and control. Ann Behav Med. 2009;38:71–85. doi: 10.1007/s12160-009-9140-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Loe H, Silness J. Periodontal disease in pregnancy. I. Prevalence and severity. Acta Odontol Scand. 1963;21:533–51. doi: 10.3109/00016356309011240. [DOI] [PubMed] [Google Scholar]
- 10.Lobene RR, Weatherford T, Ross NM, Lamm RA, Menaker L. A modified gingival index for use in clinical trials. Clin Prev Dent. 1986;8:3–6. [PubMed] [Google Scholar]
- 11.Malek Mohammadi T, Hajizamani A. A review on traditional caries diagnostic systems and introducing new international caries detection and assessment system (ICDAS) Shiraz Dent Sch J. 2011;12:67–83. [Google Scholar]
- 12.Harrison R, Benton T, Everson-Stewart S, Weinstein P. Effect of motivational interviewing on rates of early childhood caries: A randomized trial. Pediatr Dent. 2007;29:16–22. [PubMed] [Google Scholar]
- 13.Weinstein P, Harrison R, Benton T. Motivating parents to prevent caries in their young children: One-year findings. J Am Dent Assoc. 2004;135:731–8. doi: 10.14219/jada.archive.2004.0299. [DOI] [PubMed] [Google Scholar]
- 14.Sgan-Cohen HD. Oral hygiene improvement: A pragmatic approach based upon risk and motivation levels. BMC Oral Health. 2008;8:31. doi: 10.1186/1472-6831-8-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.White LL, Gazewood JD, Mounsey AL. Teaching students behavior change skills: Description and assessment of a new Motivational interviewing curriculum. Med Teach. 2007;29:e67–71. doi: 10.1080/01421590601032443. [DOI] [PubMed] [Google Scholar]
- 16.Freudenthal JJ. Motivational interviewing (MI) as an intervention for early childhood caries risk-related behaviors. J Dent Hyg. 2008;82:67. [PubMed] [Google Scholar]
- 17.Yeung CA. Motivational interviewing in an oral health promotion programme. Evid Based Dent. 2010;11:14–5. doi: 10.1038/sj.ebd.6400703. [DOI] [PubMed] [Google Scholar]
- 18.Rubak S, Sandbaek A, Lauritzen T, Christensen B. Motivational interviewing: A systematic review and meta-analysis. Br J Gen Pract. 2005;55:305–12. [PMC free article] [PubMed] [Google Scholar]
- 19.Britt E, Hudson SM, Blampied NM. Motivational interviewing in health settings: A review. Patient Educ Couns. 2004;53:147–55. doi: 10.1016/S0738-3991(03)00141-1. [DOI] [PubMed] [Google Scholar]


