Abstract
Hypertension (HTN) is one among the fiery health problems of the present era. Since it does not cause symptoms usually for many years until a vital organ is damaged. The present study was carried out on 40 patients of essential HTN with Brahmyadi Churna and tablet Shilajatu for a period of 1 month with milk as Anupana. Observation was done before the treatment, 3 mid test assessments on 7th, 14th, and 21st day, posttest assessment was done on 30th day. Intervention revealed that 19 had marked improvement, 14 had moderate improvement, 5 had mild improvement, and no improvement was noticed in 2 individuals. Reduction in blood pressure was observed markedly with P < 0.000.
Keywords: Brahmyadi Churna, essential hypertension, postural changes
INTRODUCTION
Hypertension (HTN) being a chronic illness constitutes an important public health challenge because of its prevalence and concomitant increase in the risk of cardiovascular diseases. In India, 14% of people suffer from HTN[1] and majority of them have essential HTN. It is estimated that 1 billion people are affected worldwide.[2] As most of the patients suffering from abnormally elevated blood pressure (BP) are asymptomatic, diagnosis is either missed or delayed. HTN remains one of the most frequent risk factors for cardiovascular/cerebrovascular morbidity and mortality.[3]
Modern style of living might have given man all comforts that he has craven for, but in the meantime it has a darker side too, and one of them is the increase in the incidence of lifestyle disorders, to mention few are obesity, diabetes, and HTN.[4]
HTN is classified as either primary (essential) HTN or secondary HTN, about 90–95% of cases are categorized as “primary HTN” which means high BP (HBP) with no obvious underlying medical cause.[5] The remaining 5–10% of cases (secondary HTN) are caused by other conditions that affect the other system such as kidneys, arteries, heart, or endocrine system.
Though direct references regarding HTN are not available in the classical literature of Ayurveda, attempts are made to explain HTN according to the Dosha and Dhatu involvement. The lifelong and palliative treatment of HTN in western medicine induces many side effects. Therefore, to attain and to maintain good health, hypertensive patients are looking toward Ayurveda. In this study, an attempt is made to probe the possibility of managing HTN with drugs which have lesser side effects, especially considering the chronicity and lifelong nature of the disease.
Aim and objective
To evaluate the combined effect of Brahmyadi Churna (Brahmi, Shankhapushpi, Jyotishmati, Jatamansi, Vacha, Ashwagandha 1 Part each) and tablet Shilajatu in the management of essential HTN.
MATERIAL AND METHODS
Drug
Brahmyadi Churna (Brahmi, Shankhapushpi, Jatamansi, Jyotishmati, Vacha, Ashwagandha Churna 1 part each)
Shilajatu Vati.
Brahmyadi Churna
The ingredients of Brahmyadi compound were procured from Abdul Ravoof and son's Pansari Shop, Mysore. It was made into powder, mixed well in a container and used.
Shilajatu Vati
Shilajatu Vati was procured from SDP Pharmacy, Puttur.
The identification of the individual raw drugs was done by experts in the field.
Source of data
Patients of either sex diagnosed to be suffering from essential HTN were selected from the OPD, IPD of Alvas Ayurveda Medical College, Moodbidri.
Sampling
Totally, 40 cases of essential HTN were selected incidentally. The patients were registered for the present study with the help of proforma prepared for the study.
Diagnostic criteria
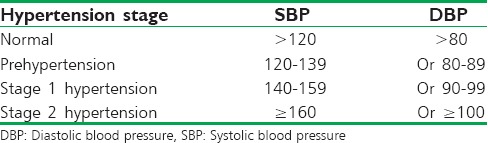
Primary criteria
The 7th Report of the Joint National committee on prevention, detection, evaluation, and intervention of HBP were considered as the standard for the diagnosis of HTN.[2]
Secondary criteria
Headache, palpitation, chest pain, insomnia, fatigue, and giddiness.
Inclusion criteria
Patients of either sex between the age group of 30–70 years either treated or freshly detected cases of essential HTN were selected
Patient with pre-HTN and HTN stage 1 with or without symptoms were included for the study.
Exclusion criteria
Patients suffering from any other systemic disorders which interfere with the course of the disease and intervention were excluded.
Statistical methods
Descriptive statistics, Chi-square test, contingency coefficient analysis, repeated measure ANOVA, paired samples t-test using SPSS program version 20.0 (Illinois, USA).
Investigations
Patients were subjected for routine investigations of blood, urine, etc., to exclude any other systemic disorders.
Intervention
Brahmyadi Churna 6 g tid after food with milk (Dried Panchanga of Brahmi and Shankhapushpi, Roots of Jatamansi and Ashwagandha, seeds of Jyotishmati, stem of Vacha, 1 part each were taken and made into Churna [powder form] and mixed well in a container)
-
Tablet Shilajatu 1 bid after food with milk
Duration: 30 days
Patients were advised for limiting the usage of salt, restricting the intake of fat rich food, quitting smoking and alcohol, and managing stress levels.
Assessment criteria
The assessment was done considering systolic BP (SBP), diastolic BP (DBP), and mean BP readings in all the three postures that is, supine, sitting, and standing at pretest that is, 0th day, 3 mid test assessments on 7th, 14th, 21st day, respectively and posttest on 30th day [Table A].
Table A.
Stages of hypertension
Overall assessment
The overall assessment of the intervention was interpreted as reduction in SBP and DBP in the range of:
Marked improvement - SBP 30–40 mm of Hg and DBP up to ≤15 mm of Hg
Moderate improvement - SBP 20–29 mm of Hg and DBP 11–14 mm of Hg
Mild improvement - SBP 10–19 mm of Hg and DBP 5–10 mm of Hg
No improvement - Reduction in SBP in the range of 0–9 mm of Hg and DBP in the range 0-4 mm of Hg.
The mean of both is taken and overall assessment is done.
OBSERVATION AND RESULTS
Pretest
Out of 40 patients, 19 fresh patients and 21 treated cases were noted. Fresh cases were observed with frequent measurement of BP and then intervention was started, in treated cases the earlier medication was withdrawn gradually and completely, after complete withdrawal of earlier treatment a flush out period of 7 days was allowed before the intervention was started. Out of 40 patients, 32 patients were symptomatic and majority of them that is, 19 patients (47.5%) had headache, followed by symptoms like insomnia in 17 patients (42.5%), fatigue 17 patients (42.5%). Fifteen patients (37.5%) with giddiness, palpitation was found in 9 patients (22.5%), and 2 patients (5%) had chest pain. Epistaxis was observed only in 2 patients (5%).
In the present study, familial predisposition was observed in 42% of the cases, excessive salt intake was observed in 50% of cases and the risk factors like smoking, obesity, alcohol was found only in 17% of cases.
Mid test
On 7th day
In the majority of patients, no much difference in BP was recorded in all the three postures. Though linear reduction in BP was observed in few cases, few cases showed a slight increase in BP when compared to previous reading.
14th day
Reduction in SBP to an average of 15 mm of Hg and DBP to an average of 10 mm of Hg was noted. Symptoms such as headache, giddiness reduced in few patients.
21st day
Reduction in SBP to an average of 20 mm of Hg and DBP to an average of 12 mm of Hg was observed. There was an improvement in the quality of sleep in individuals who complained of insomnia.
Posttest observation
After the intervention, there was a significant reduction in symptoms such as giddiness, headache, fatigue, insomnia though no much improvement in palpitation, and chest pain was observed.
Overall assessment of the intervention revealed that out of 40 patients, 19 (47.5%) had marked improvement, 14 (35%) had moderate improvement, 5 (12.5%) had mild improvement, and no improvement was noticed in 2 (5%) individuals. Overall, the study revealed that the selected drugs have a significant role to play in the management of Essential HTN. Reduction in BP was observed markedly with P value 0.000 [Tables 1-8 and Figures 1-9].
Table 1.
Descriptive statistics of SBP in supine posture
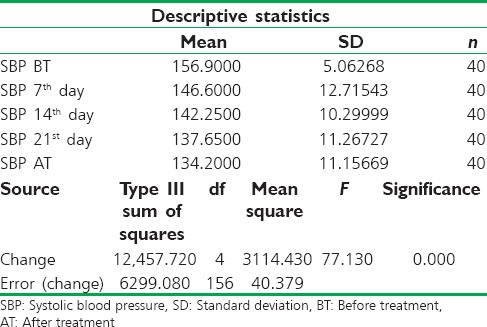
Table 8.
General linear mode of mean DBP
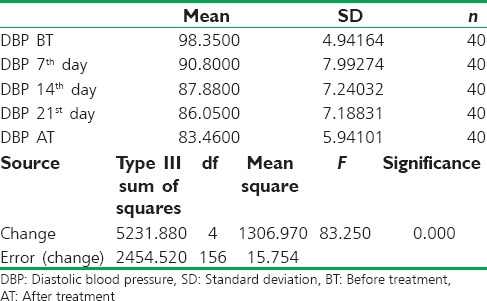
Figure 1.
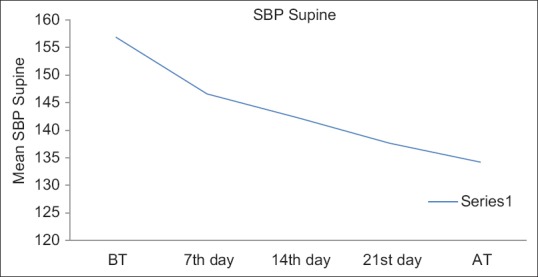
Descriptive statistics of systolic blood pressure in supine posture
Figure 9.
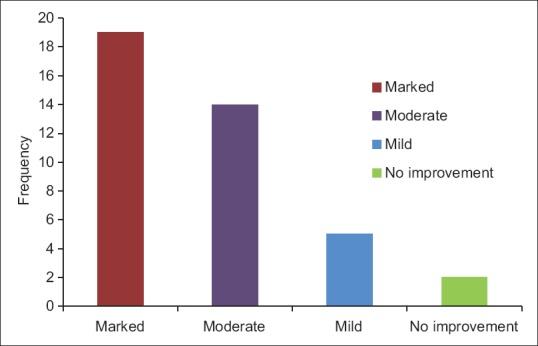
Overall assessment
Table 2.
Descriptive statistics of DBP in supine posture
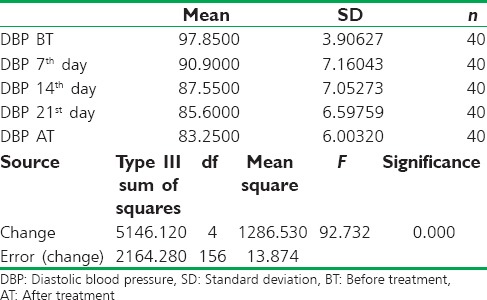
Table 3.
Descriptive statistics of SBP in sitting posture
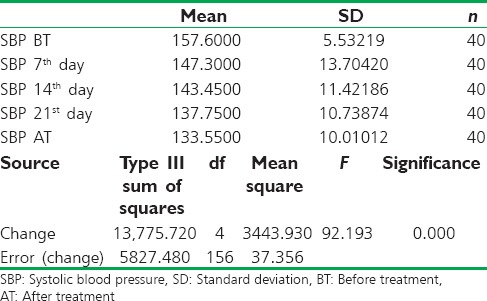
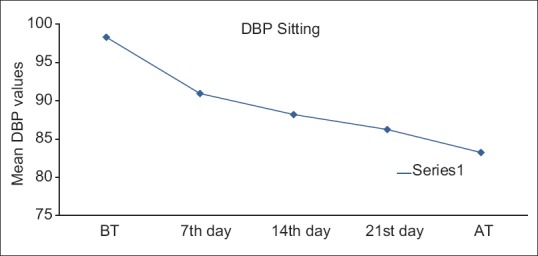
Table 4.
Descriptive statistics of DBP in sitting posture
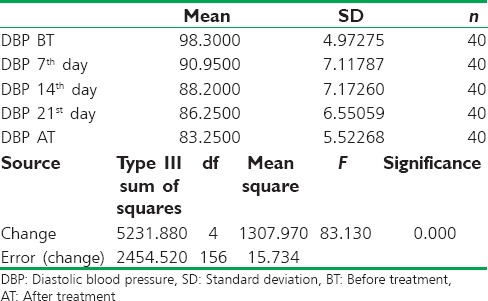
Table 5.
Descriptive statistics of SBP in standing posture
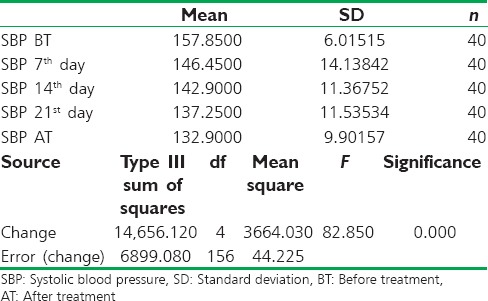
Table 6.
Descriptive statistics of DBP in standing posture
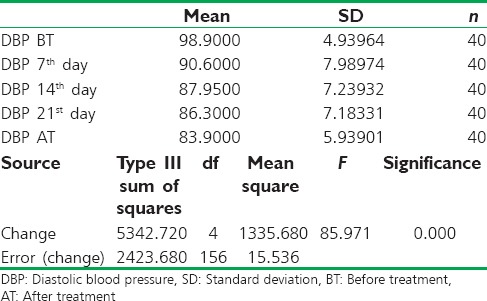
Table 7.
General linear mode of mean SBP
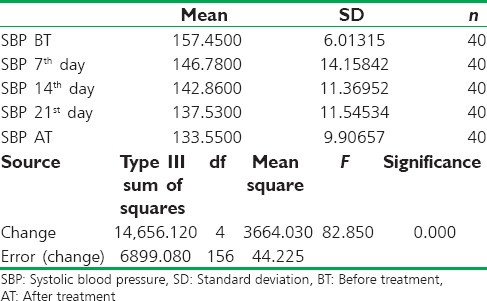
Figure 2.
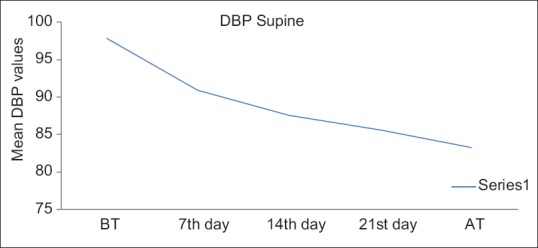
Descriptive statistics of diastolic blood pressure in supine posture
Figure 3.
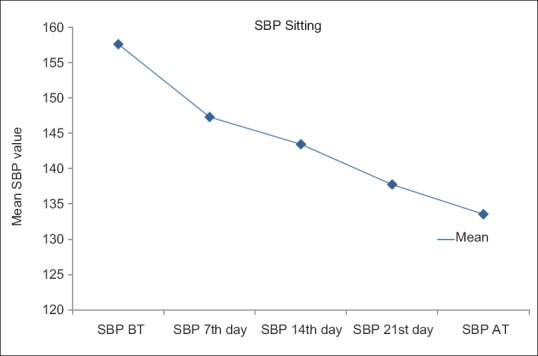
Statistics of systolic blood pressure in sitting posture
Figure 4.
The descriptive of systolic blood pressure inSBP Sitting position
Figure 5.
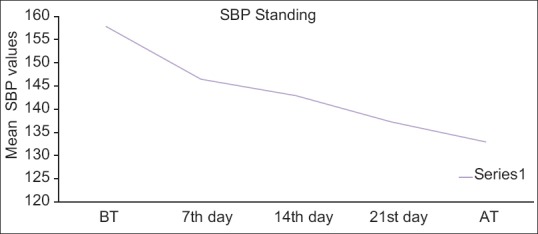
Descriptive statistics of systolic blood pressure in standing position
Figure 6.
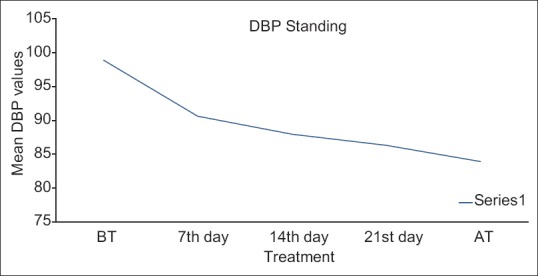
The descriptive analysis of diastolic blood pressure in standing position
Figure 7.
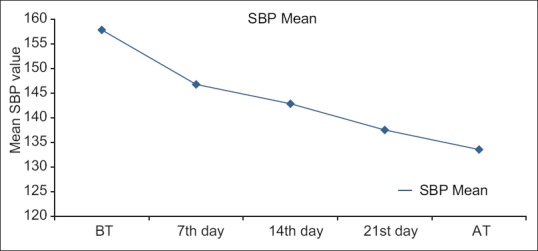
General linear mode of mean systolic blood pressure
Figure 8.
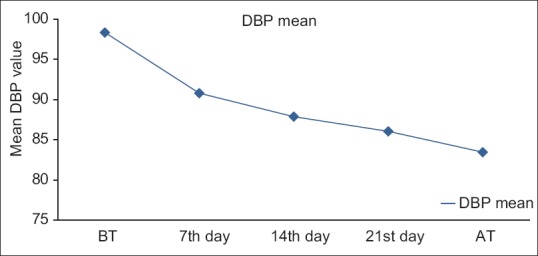
General linear mode of mean diastolic blood pressure
DISCUSSION ON RESULTS
The result of the study revealed that, a combination of Brahmyadi compound and Shilajatu Vati has a definite role in lowering BP, which also showed statistically highly significant results with P < 0.001.
The symptoms such as headache, insomnia, and giddiness were reduced after the intervention, while, other symptoms namely fatigue, chest pain, and palpitation showed no much response.
After observing the mean BP values, it is seen that SBP reduced up to 10 mm Hg while DBP reduced up to 6 mm Hg on 7th day. On 14th day, SBP reduced up to 14 mm Hg and DBP reduced upto10 mm Hg. On 21st day, SBP reduced up to 19 mm Hg and DBP reduced up to 12 mm Hg. After treatment, SBP reduced 22 mm Hg and DBP reduced 15 mm Hg.
Freshly detected and untreated cases responded well while treated cases of more than 2 years of history showed lesser improvement. The response was encouraging in majority of the patients where stress played an important role.
Sankhapuspi has been mentioned as a Rasayana in Charaka Samhita (Ca. Ci. 1/3), that it provides freedom from fatigue. Sankhapuspi is also a proven hypotensive drug (Chaturvedi et al., 1966) and this study also proved that Sankhapuspi also decreases BP and pulse rate due to its anti-stress effect.
Shankhapushpi (Convolvulus puricaulis) has been successfully used in the management of Chittodvega-Anxiety disorder.[6]
Shankhapushpi and Brahmi are the Medhya Rasayanas mentioned in Charaka Chikitsa 1st chapter.[7] Jyotishmati as Medhaa Prajna Buddhi Vivardhanam (improves cognitive and intellectual ability) is mentioned in Raja Nighantu.
Vacha has been described in Sushrutha Shareera 10th chapter as Medha Bala Buddhi Vivardhanah (improves intellect ability and strength). Vacha and Jatamansi are mentioned as sanjnasthapaka (to establish consciousness).[8] Considering the qualities of drugs, here an attempt is made to study the action of the drugs on HTN and is found effective.
CONCLUSION
In the present clinical trial, it was observed that there was a marked reduction in the levels of total BP. Symptoms such as headache, insomnia, and giddiness showed marked improvement while not much reduction was observed in other symptoms such as chest pain, fatigue, and palpitation.
Most of the patients in the study were symptomatic on the contrary to general notion that essential HTN is asymptomatic.
The most commonly observed symptoms in them were a headache, insomnia, fatigue, giddiness, respectively. Symptoms such as palpitation, chest pain were observed more in individuals who had chronic HTN and were already treated.
SBP reduced considerably than DBP. In the present trial with Brahmyadi Churna and Shilajatu Vati, reduction in BP was observed markedly with P < 0.000.
A small limitation of the study was that, the taste of the Churna was not palatable which was difficult for the patients to consume. Hence, extract of the same drug can be taken and made into capsule form or Churnas made into tablet form to make it more palatable and tried. Furthermore, controlled clinical trial with long-term follow-up is recommended.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Gupta R. Defining hypertension in the Indian population. Natl Med J India. 1997;10:139–43. [PubMed] [Google Scholar]
- 2.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr, et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: The JNC 7 Report. JAMA. 2003;289:2560–72. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 3.Whelton PK. Epidemiology of hypertension. Lancet. 1994;344:101–6. doi: 10.1016/s0140-6736(94)91285-8. [DOI] [PubMed] [Google Scholar]
- 4.Pappachan MJ. Increasing prevalence of lifestyle diseases: High time for action. Indian J Med Res. 2011;134:143–5. [PMC free article] [PubMed] [Google Scholar]
- 5.Carretero OA, Oparil S. Essential hypertension. Part I: Definition and etiology. Circulation. 2000;101:329–35. doi: 10.1161/01.cir.101.3.329. [DOI] [PubMed] [Google Scholar]
- 6.Parsania S. Jamnagar: Department of Kayachikitsa, IPGT and RA, Gujarat Ayurveda university; 2001. A clinical study on the role of Jaladhara and Shankhapushpi (Convolvulus pleuricaulis) in the management of Chittodvega (anxiety disorder) pp. 35–7. [Google Scholar]
- 7.Chikitsa. 1/103. 5th ed. Varanasi: Chaukhamba Surbharathi Prakashan; 2009. Vaidya Jadavaji Trikamaji Acharya. Charaka Samhita by Agnivesha, Revised by Charaka and Dridhabala with Ayurveda Deepika Commentary of Chakrapanidatta; p. 42. [Google Scholar]
- 8.Sharma PV. Vol. 2. Varanasi: Chaukhambha Bharati Academy; 1995. Dravyaguna-vijnana; pp. 4–17. In Hindi. [Google Scholar]


