Abstract
Association between sarcoidosis and antiphospholipid syndrome (APS) is rare with few reported cases. We sought to systematically review the published cases of APS with sarcoidosis to better characterize the demographics, clinical characteristics, treatment, and the outcome of this association. Systematic electronic search for case report, case series, and related articles published until May 2014 was carried out and relevant data were extracted and analyzed. Four cases of APS with sarcoidosis were identified exclusively in females. These cases were seen in the sixth decade of life. Pulmonary embolism and central retinal artery occlusion were the presenting thrombotic events. All the patients were treated with lifelong anticoagulation with warfarin. During the median follow-up period of 5.5 months, additional thrombotic events were not observed. Although rare, sarcoidosis may be associated with APS. Further reporting of the cases will help to better establish this association, elucidate pathogenesis, and define clinical characteristics and outcomes.
Keywords: Antiphospholipid syndrome, association, sarcoidosis, systematic review
Introduction
Sarcoidosis is a systemic inflammatory disorder of unknown cause that is characterized by the granulomatous inflammation of various organs.[1] Antiphospholipid syndrome (APS) is an autoimmune condition defined by persistently positive antiphospholipid antibodies as well as recurrent arterial or venous thromboses and pregnancy complications.[2] Diagnosis of APS is made according to the revised Sapporo criteria,[3] which requires at least one clinical (vascular thrombosis or pregnancy morbidity) and one laboratory criteria (presence of lupus anticoagulant, presence of immunoglobulin G [IgG], and/or immunoglobulin [IgM] anticardiolipin antibody [>40 U/ml, or >99th percentile], and/or presence of IgG and/or IgM anti-beta 2 glycoprotein antibody [>99th percentile]). All antibodies must be demonstrated on two or more occasions separated by at least 12 weeks. Both APS and sarcoidosis have been known to occur with autoimmune conditions[4,5] with genetic factors playing equally important roles.[6,7] Even though studies have found an association between antiphospholipid antibodies and sarcoidosis,[8] cases with concurrent sarcoidosis and APS are rare. In order to expand the current understanding of this association, we carried out a systematic review of all the published cases.
Search Strategy and Data Collection
We searched Medline (via PubMed) and Embase for case reports, case series, and related articles on the association between sarcoidosis and APS from inception to March 15, 2014. We used the search terms “antiphospholipid syndrome,” “sarcoidosis,” “pulmonary sarcoidosis,” and “lung sarcoidosis” in addition to the medical subject heading terms “sarcoidosis” and “antiphospholipid syndrome.” The search was limited to human subjects. We also performed hand search to identify additional publications. Eligibility criteria included the following requirements:
Concurrent sarcoidosis (confirmed by biopsy)[9] and APS and
The diagnosis of APS was confirmed according to the revised Sapporo criteria.
We excluded three cases with sarcoidosis, where APS was thought to be secondary to other causes such as systemic lupus erythematosus,[10] treatment with tumor necrosis factor inhibitor, or interferon alpha [Figure 1].[11,12] With this approach, we identified four eligible cases in English language. We studied their demographic variables, clinical presentation, treatment, and outcomes.
Figure 1.
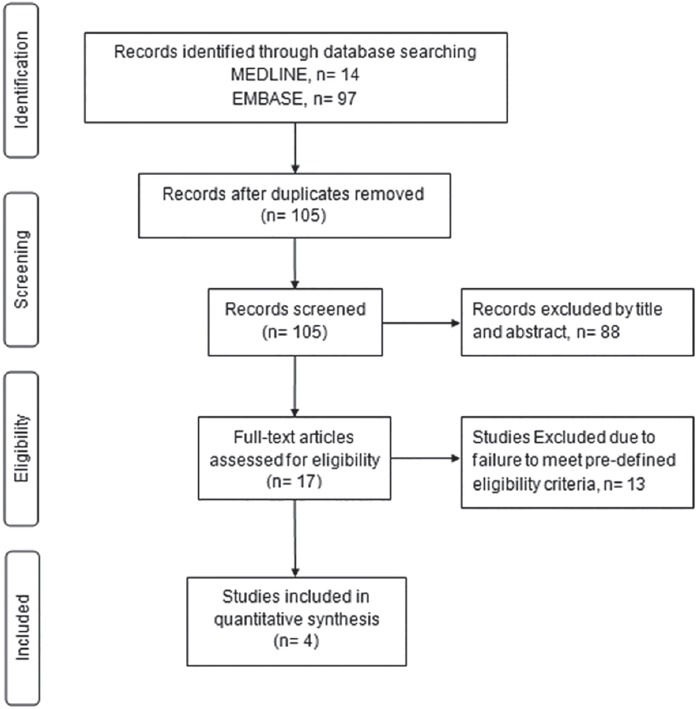
Systematic literature search and study selection process
Results
Demographic data and clinical presentation
All four cases included in the study met the revised Sapporo criteria and there were no obvious alternative causes for APS. Of the four cases of sarcoidosis with APS, all of them were females. The age ranged from 29 to 72 years, with a median (interquartile range) of 58 (50-62), and a mean of 54 years. Presenting thrombotic event varied from central retinal artery occlusion (n = 1) to pulmonary embolism (n = 1). Stroke was the most common arterial thrombosis (n = 2). A history of fetal loss was present in two cases. The duration of sarcoidosis was more than eight years in two cases and was not mentioned in the rest. APS was observed in early (n = 2) as well as late (n = 1) stages of sarcoidosis. Only one case had extra-thoracic involvement (ocular and skin sarcoidosis) [Table 1].
Table 1.
Demographic characteristics, clinical presentation, diagnostic evaluation, treatment, and follow-up of identified patients with sarcoidosis and APS
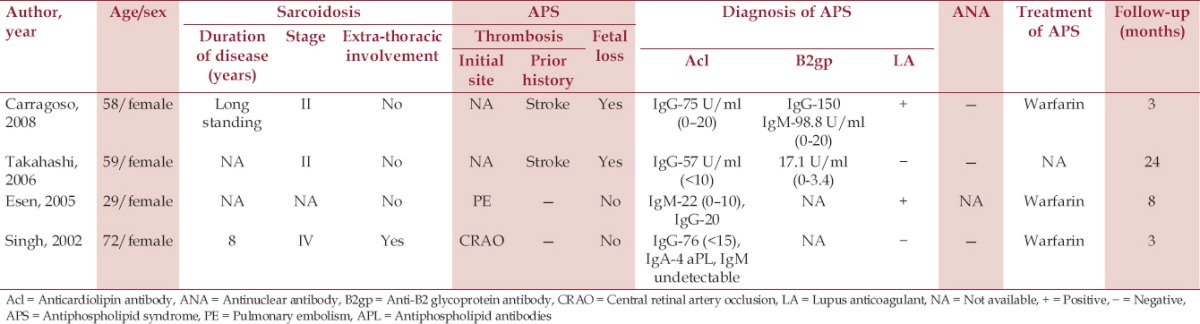
Laboratory investigation
Positive titers of anticardiolipin antibodies and anti-beta 2-glycoprotein antibodies were present in four and two cases, respectively. Lupus anticoagulant activity was positive in two cases and negative in the other two. Angiotensin converting enzyme (ACE) level was elevated in all the reported cases (n = 3, mean ACE level 95 U/L). Erythrocyte sedimentation rate was elevated in one reported case (50 mm/h).
Treatment and prognosis
Three cases with APS were treated with heparin acutely, followed by lifelong warfarin. Details of the treatment were not provided in one of the case. None of the cases reported further thrombotic events while on anticoagulation on follow-up (median duration 5.5 months).
Discussion
Only four definite cases of APS and sarcoidosis have been reported in the literature. Both APS and sarcoidosis share immune dysregulation and autoimmunity,[4,5] which might explain their co-occurrence.
In our study, an association of APS and sarcoidosis was exclusive to females, which is consistent with the female predominance of APS in general.[13,14] The mean age of patients with APS in sarcoidosis was higher than the average age of patients with APS alone (54 years vs. 42 years[13]). Although sarcoidosis is more common in the younger age group (20-40),[15] a second peak has been observed at about age 50, especially in women.[16] The higher mean age of APS in sarcoidosis may be due to the propensity of APS to develop in older sarcoidosis patients.
Common presenting thrombotic events were pulmonary embolism and central retinal artery occlusion. Interestingly, deep venous thrombosis, the most common thrombotic complication of APS in a large European cohort,[13] was not seen in the any of these patients. Stroke was the most common arterial thrombosis, which is consistent with the results of the European study.[13] Catastrophic APS, which is associated with more than 50% mortality,[4] has been found to be associated with various autoimmune disorders.[17] However, none of the patients in our review had the features of catastrophic APS.
As only one patient in our study had extra-thoracic involvement, we were unable to clearly elucidate the relationship between the levels of antiphospholipid antibody and the extent of extra-thoracic involvement, as previously suggested by Ina et al.[8] Ina et al. had also demonstrated a significant correlation between antiphospholipid antibody level and chest X-ray abnormality, thus linking antiphospholipid antibody as a prognostic marker for sarcoidosis. In our study, we observed APS with both the early and late stages of sarcoidosis. However, due to small number of cases, we could not study if APS can also help prognosticate sarcoidosis.
Three cases in our study were initially treated with heparin and then with lifelong warfarin to decrease the risk of future thrombotic events. After the first thrombotic event, lifelong warfarin is recommended to achieve an international normalized ratio ranging from 2.0 to 3.0.[18] The treatment of thrombotic complications of APS is generally the same regardless of whether it is primary APS or secondary APS.[4] Studies have previously looked at the efficacy of hydroxychloroquine in preventing thrombosis in systemic lupus erythematosus patients, but data remain elusive.[19] By extension of this analogy, it is uncertain if future thrombotic events can be prevented in patients with APS and sarcoidosis with the treatment of underlying sarcoidosis. Further studies are needed to shed more light in this regard.
Patients who survive the initial thrombotic event remain at risk for recurrent events which may be as high as 7%, even with anticoagulation.[20] The risk of developing recurrent thrombotic events increases with the presence of anti-beta 2-glycoprotein antibodies, autoimmune hemolysis, or the involvement of more than one vascular bed.[21] Although two of the cases had positive anti-beta 2-glycoprotein antibodies, none of our patients were reported to have recurrent episodes of thrombotic events.
Small sample size precluded the use of statistical tests to determine the relationship between antiphospholipid antibody levels and the stage/extent of disease.
Conclusion
Although rare, APS associated with sarcoidosis may tend to occur in older age group than APS alone and may occur exclusively in females. It commonly presents with venous thrombotic events such as pulmonary embolism. Further reporting of cases will help to better define this association, determine if APS is a prognostic marker of sarcoidosis, and provide details on whether treating the underlying sarcoidosis may reduce the thrombotic risk in this subset of APS.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Fahim A, Mann JS. Pulmonary sarcoidosis: Diagnostic and treatment update. Expert Rev Respir Med. 2014;8:493–501. doi: 10.1586/17476348.2014.919225. [DOI] [PubMed] [Google Scholar]
- 2.Comarmond C, Cacoub P. Antiphospholipid syndrome: From pathogenesis to novel immunomodulatory therapies. Autoimmun Rev. 2013;12:752–7. doi: 10.1016/j.autrev.2012.12.006. [DOI] [PubMed] [Google Scholar]
- 3.Wilson WA, Gharavi AE, Koike T, Lockshin MD, Branch DW, Piette JC, et al. International consensus statement on preliminary classification criteria for definite antiphospholipid syndrome: Report of an international workshop. Arthritis Rheum. 1999;42:1309–11. doi: 10.1002/1529-0131(199907)42:7<1309::AID-ANR1>3.0.CO;2-F. [DOI] [PubMed] [Google Scholar]
- 4.Ruiz-Irastorza G, Crowther M, Branch W, Khamashta MA. Antiphospholipid syndrome. Lancet. 2010;376:1498–509. doi: 10.1016/S0140-6736(10)60709-X. [DOI] [PubMed] [Google Scholar]
- 5.Sharma OP. Sarcoidosis and other autoimmune disorders. Curr Opin Pulm Med. 2002;8:452–6. doi: 10.1097/00063198-200209000-00019. [DOI] [PubMed] [Google Scholar]
- 6.Biggioggero M, Meroni PL. The geoepidemiology of the antiphospholipid antibody syndrome. Autoimmun Rev. 2010;9:A299–304. doi: 10.1016/j.autrev.2009.11.013. [DOI] [PubMed] [Google Scholar]
- 7.Morgenthau AS, Iannuzzi MC. Recent advances in sarcoidosis. Chest. 2011;139:174–82. doi: 10.1378/chest.10-0188. [DOI] [PubMed] [Google Scholar]
- 8.Ina Y, Takada K, Yamamoto M, Sato T, Ito S, Sato S. Antiphospholipid antibodies. A prognostic factor in sarcoidosis? Chest. 1994;105:1179–83. doi: 10.1378/chest.105.4.1179. [DOI] [PubMed] [Google Scholar]
- 9.Heinle R, Chang C. Diagnostic criteria for sarcoidosis. Autoimmun Rev. 2014;13:383–7. doi: 10.1016/j.autrev.2014.01.035. [DOI] [PubMed] [Google Scholar]
- 10.Wesemann DR, Costenbader KH, Coblyn JS. Co-existing sarcoidosis, systemic lupus erythematosus and the antiphospholipid antibody syndrome: Case reports and discussion from the Brigham and Women's Hospital Lupus Center. Lupus. 2009;18:202–5. doi: 10.1177/0961203308100483. [DOI] [PubMed] [Google Scholar]
- 11.Shinohara MM, Davis C, Olerud J. Concurrent antiphospholipid syndrome and cutaneous [corrected] sarcoidosis due to interferon alfa and ribavirin treatment for hepatitis C. J Drugs Dermatol. 2009;8:870–2. [PubMed] [Google Scholar]
- 12.Yee AM, Pochapin MB. Treatment of complicated sarcoidosis with infliximab anti-tumor necrosis factor-alpha therapy. Ann Intern Med. 2001;135:27–31. doi: 10.7326/0003-4819-135-1-200107030-00010. [DOI] [PubMed] [Google Scholar]
- 13.Cervera R, Piette JC, Font J, Khamashta MA, Shoenfeld Y, Camps MT, et al. Antiphospholipid syndrome: Clinical and immunologic manifestations and patterns of disease expression in a cohort of 1,000 patients. Arthritis Rheum. 2002;46:1019–27. doi: 10.1002/art.10187. [DOI] [PubMed] [Google Scholar]
- 14.Bertero MT, Bazzan M, Carignola R, Montaruli B, Silvestro E, Sciascia S, et al. Antiphospholipid syndrome in northwest Italy (APS Piedmont Cohort): Demographic features, risk factors, clinical and laboratory profile. Lupus. 2012;21:806–9. doi: 10.1177/0961203312446974. [DOI] [PubMed] [Google Scholar]
- 15.O’Regan A, Berman JS. Sarcoidosis. Ann Intern Med. 2012;156:ITC5. doi: 10.7326/0003-4819-156-9-201205010-01005. [DOI] [PubMed] [Google Scholar]
- 16.Hillerdal G, Nöu E, Osterman K, Schmekel B. Sarcoidosis: Epidemiology and prognosis. A 15-year European study. Am Rev Respir Dis. 1984;130:29–32. doi: 10.1164/arrd.1984.130.1.29. [DOI] [PubMed] [Google Scholar]
- 17.Nayer A, Ortega LM. Catastrophic antiphospholipid syndrome: A clinical review. J Nephropathol. 2014;3:9–17. doi: 10.12860/jnp.2014.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ruiz-Irastorza G, Cuadrado MJ, Ruiz-Arruza I, Brey R, Crowther M, Derksen R, et al. Evidence-based recommendations for the prevention and long-term management of thrombosis in antiphospholipid antibody-positive patients: Report of a task force at the 13th International Congress on antiphospholipid antibodies. Lupus. 2011;20:206–18. doi: 10.1177/0961203310395803. [DOI] [PubMed] [Google Scholar]
- 19.Barbhaiya M, Erkan D. Primary thrombosis prophylaxis in antiphospholipid antibody-positive patients: Where do we stand? Curr Rheumatol Rep. 2011;13:59–69. doi: 10.1007/s11926-010-0149-3. [DOI] [PubMed] [Google Scholar]
- 20.Crowther MA, Ginsberg JS, Julian J, Denburg J, Hirsh J, Douketis J, et al. A comparison of two intensities of warfarin for the prevention of recurrent thrombosis in patients with the antiphospholipid antibody syndrome. N Engl J Med. 2003;349:1133–8. doi: 10.1056/NEJMoa035241. [DOI] [PubMed] [Google Scholar]
- 21.Tektonidou MG, Ioannidis JP, Boki KA, Vlachoyiannopoulos PG, Moutsopoulos HM. Prognostic factors and clustering of serious clinical outcomes in antiphospholipid syndrome. QJM. 2000;93:523–30. doi: 10.1093/qjmed/93.8.523. [DOI] [PubMed] [Google Scholar]


