Abstract
Aim:
The aim of the present study was to determine the prevalence of carotid artery calcification (CAC) in postmenopausal females on panoramic radiographs and to study the correlation of CAC with possible risk factors such as hypertension, osteoporosis, and hypercholesterolemia, among others.
Materials and Methods:
Totally, 1214 panoramic radiographs of postmenopausal females attending the Department of Oral Medicine and Radiology were examined for the presence of CAC. The subjects were also assessed for the presence of various risk factors and the possible correlation to CAC. Statistical analysis was done using Chi-square test, and P < 0.05 was considered to be statistically significant.
Results:
Two hundred and seventy-eight postmenopausal females presented with CAC and a prevalence of 22.9%. These patients presented with a medical history that was laden with risk factors, of which hypertension (71.2%) was the most common risk factor. Hypertension, hypercholesterolemia, osteoporosis, and obesity were significantly (P < 0.05) related to the presence of CAC while age, diabetes, and smoking were not significantly (P > 0.05) related to CAC.
Conclusion:
The incidental finding of CAC on panoramic radiographs during the routine dental examination can provide life-saving information for the identification of postmenopausal females who are at a higher risk for stroke. Oral clinicians should, therefore, record a proper medical history of such patients to identify the atherogenic risk factors and refer such patients to the physician for careful evaluation and conformation of the disease.
Keywords: Carotid artery calcification, hypertension, panoramic radiography, postmenopausal females
INTRODUCTION
Menopause, by annotation is the time at which cyclic ovarian function, as illustrated by menstruation, ceases. It is a physiological state bequeathing rise to robust diversity at systemic and oral level. The term menopause literally means “without estrogen.” It is a physiological unfolding portrayed by the enduring cessation of menstruation and is often attributed by the term climacterium. However, menopause is not synonymous of climacterium.[1] Menopause, an array of physiological effects, seen in the fifth decade of a woman's life owed to the diminution in estrogen output secondary to a bereavement of follicular function. It has been implied by disparate studies that menopause initiates a host of physiologic changes.[2,3,4] It is well cited that calcified atheroma in the common carotid artery can be ascertained in panoramic radiograph and this can succor as an imperative tool for early detection of carotid artery calcification (CAC). Apperception of CAC by panoramic radiograph proclaimed to be ranging from 0.43% to 9.4%, depending on the age and lifestyle of the samples comprehended in the studies. The radiopaque masses disclosed on OPG as CAC were more commonly instituted in females, unilaterally or bilaterally.[5]
The physiological changes connected with menopause and different processes concord with aging result in women being at a disproportionately high risk of developing stroke, which has been accounted for to be the third driving motive behind death in most countries after cardiovascular diseases and cancer.[6] Components are prompting carotid artery atherosclerosis incorporate increasing age, systolic hypertension, hypercholesterolemia, diabetes mellitus, obesity, physical inactivity, coronary artery disease, and cigarette smoking more than 20 packs/year.[7] Postmenopause female are established to foster hypertension and carotid artery atherosclerosis as they customarily mellow an atherogenic blood lipid profile during menopause and because of increased hepatic lipase activity and decreased low-density lipoprotein, both related to reduced estrogen levels.[8] Friedlander and Lande initially reported the vicinity of CACs on panoramic radiographs.[9] Studies in literature affirmed an expanded danger of extracranial carotid calcifications in women after menopause and an increased incidence of arteriosclerosis in women between 45 and 60 years of age were also been reported.[10] The dental practitioners, therefore, ought to have the competency to recognize such findings and allude the patients to general physicians.
The aim of the present study was to determine the prevalence of CAC on panoramic radiographs of postmenopausal females and to study the correlation of CAC with conceivable risk factors such as hypertension, osteoporosis, and hypercholesterolemia, among others.
MATERIALS AND METHODS
One thousand two hundred and fourteen postmenopausal females attending the Outpatient Department of the College of Dentistry for various routine dental complaints were incorporated in the study. All females aged 50 years or over, with a history of cessation of menstruation for 12 months were randomly selected for the study. A written informed consent was obtained from all patients prior to the study. Ethical Clearance was obtained from the Institutional Ethical Committee. All the study subjects required a panoramic radiograph for the evaluation of the associated dental problems. Hence, in accordance with the ethical considerations none of the patients were exposed to unwanted radiographic radiations only for the study to identify the CAC. All panoramic radiographs were taken with the Dentsply Gendex Orthoralix 9200 (Dentsply Asia, Milford, USA), and the magnification factor was 1.23. All reported measurements were adjusted according to this factor. The OPGs were evaluated for the presence or absence of CAC. The OPGs with low diagnostic qualities were excluded. The panoramic radiographs were examined on standard light boxes, under good lighting conditions, standardized screen brightness, and resolution to determine the dental anomalies. The radiopaque nodular mass which was adjacent to the cervical vertebrae, inside or below the C3-C4 intervertebral disk level, or to the retromandibular area, generally at an angle of 45° from the angle of the mandible, which was independent of the hyoid bone was considered as a CAC.[11] The CAC's were scored as present or absent.
The subjects were also assessed for the presence of various risk factors and were questioned about the time elapsed since the cessation of menses, history of hypertension, diabetes, high cholesterol levels, and smoking habits. One hundred and seventy-nine patients of the total 1214 patients were referred from the orthopedic department with a confirmed diagnosis of osteoporosis. The patients were thoroughly examined clinically and laboratory tests were requested for the confirmation of the underlying systemic disease. Patients who reported a systolic blood pressure of 140 mm of Hg and diastolic blood pressure of 90 mm of Hg and taking hypertensive drugs for the past 6 months were considered as hypertensive patients. Those patients who presented with a blood cholesterol level of >200 mg/dl and currently taking medications for the same for 6 months were regarded as hypercholesterolemic patients. Patients who reported with a fasting blood sugar level of >126 mg/dl over the past 6 months and taking medications for the same were regarded as diabetic. Patients with a body mass index of 27-29.9 were considered overweight and those with a body mass index of >30 were considered as obese.
The data were entered using computer software SPSS 12.0 (SPSS Inc., Chicago, USA) and analyzed using the Chi-square test, and P < 0.05 was considered to be statistically significant.
RESULTS
The study included 1214 postmenopausal females of age 50 years and above with a mean age of 62.47 ± 5.27 years. Totally, 617 patients were 50-60 years age group, 499 females were from 61 to 70 years age group and 98 females were of age ≥71 years. Two hundred and seventy-eight postmenopausal females presented with CAC with a prevalence of 22.9%. A total of 126 (45.3%) patients presented with calcifications on the left side [Figure 1], while 102 (36.7%) patients had calcifications on the right side and 50 (18%) patients showed bilateral calcifications. Of the patients from age group 50-60 years, 117 patients had CAC, 145 patients from the 61 to 70 years age group showed CAC and only 16 patients of age 71 and above presented with CAC. No significant (P > 0.05) difference was found between the age of the patient and the presence of CAC.
Figure 1.
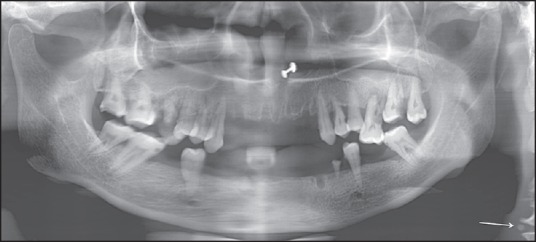
Panoramic radiograph showing carotid artery calcification
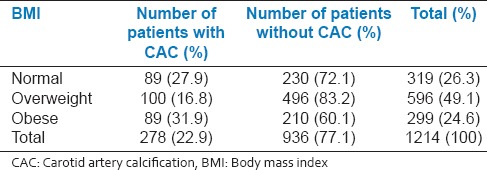
These patients presented with a medical history that was laden with risk factors, of which hypertension was the most common risk factor affecting 198 patients (71.2%) of the hypertensive patients [Table 1]. A total of 288 patients presented with hypercholesterolemia, of which 202 (70.1%) patients had CAC [Table 2]. Diabetes was present in 392 postmenopausal females, out of which 74 (18.1%) patients showed CAC on panoramic radiographs [Table 3]. Of the 179 patients with osteoporosis, 84 (46.9%) patients showed CAC [Table 4]. In the present study, a total of 319 patients normal, 596 overweight females and 299 females were obese [Table 5]. About 31.9% obese patients showed calcifications while 27.9% normal patients and 16.8% over weight females presented with CAC findings on panoramic radiographs. Statistically significant (P < 0.05) difference was observed between the correlation of hypertension, hypercholesterolemia, osteoporosis, and obesity to the presence of CAC. Only 16 patients had the habit of smoking, of which only 3 had CAC. There was no statistically significant (P > 0.05) difference between smoking and presence of CAC.
Table 1.
Correlation of CAC and a history of hypertension
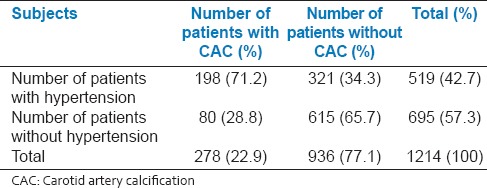
Table 2.
Correlation of CAC and a history of hypercholesterolemia
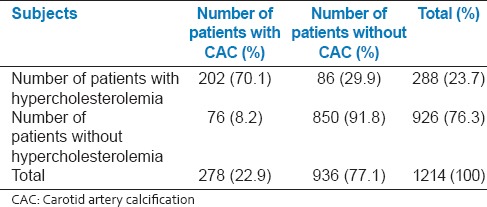
Table 3.
Correlation of CAC and a history of diabetes
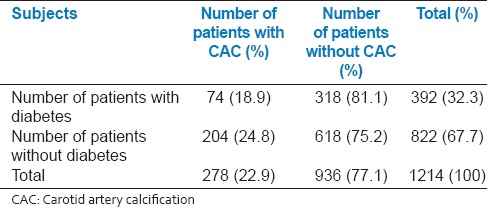
Table 4.
Correlation of CAC and a history of osteoporosis
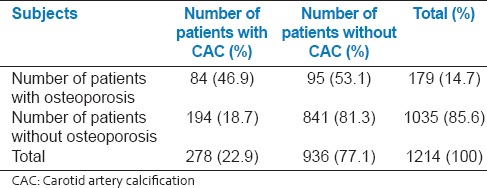
Table 5.
Correlation of CAC and BMI
DISCUSSION
Atherosclerosis is a radical inflammatory disorder that may prompt to peripheral artery disease, coronary artery disease or stroke. Atherosclerosis, leading to strokes and heart attacks are a noteworthy well-being issue. The prevalence of atherosclerosis associated with mortality and morbidity is very high in developed countries is on the ascent in developing countries.[12] Several components for the stroke can be assembled as modifiable and unmodifiable risk factors. The modifiable factors include hypertension, diabetes mellitus, hyperlipidemia, obesity, smoking, and carotid atherosclerotic disease, whereas the gender, age, ethnicity, and heredity are unmodifiable factors.[13] Early detection of these risk elements reduces the morbidity and mortality.[14] The physiological changes connected with menopause and other age-related procedures in females frames the danger of creating a stroke. Epidemiologic studies have shown that 16% women die of a stroke, when contrasted to only 8% of men who die of stroke.[10] Most of the strokes result from ischemic cerebral injury due to thrombus or emboli formation.
Carotid artery calcification, particularly close to carotid bifurcation can result in a stroke.[14] Panoramic radiographs are routinely used as a part of the assessment of patients with dental problems and have discovered to be valuable in detecting the atherosclerosis. CAC may be seen in the standard panoramic radiograph adjacent to the cervical vertebrae at the level of the C3-C4 intervertebral intersection or to the retromandibular area, by and large at an angle of 45° from the angle of the mandible, independent of the hyoid bone. They may seem as either a radiopaque vertical line or nodular radiopaque mass inferior to the angle of the mandible.[11] The adequacy of panoramic radiography has been established by disparate studies done to assess their proficiency in the diagnosis of CACs in the patients without symptoms but with a high risk of stroke. The findings of these studies demonstrated that panoramic radiography is more commonly used, least expensive and easier when contrasted with the previous diagnostic methods and is considerably less invasive.[15] It must be noted that CAC must be located in the radiography field for it to be viewed on the radiograph, as lack of awareness of this may bring about erroneous selection of patients with or without the calcification.[6]
The present study evaluated the incidence of CACs in postmenopausal females aged 50 and older. The mean age of the patients in the present study was 62.47 ± 5.27 years. The present study revealed that 278 postmenopausal females presented with CAC with a prevalence of 22.9%. Cohen et al. studied 1879 panoramic radiographs of males >55 years of age and reported a prevalence of 3.8% for CAC.[16] Uthman and Al-Saffar showed a prevalence of 38.8% in patients with stroke-related diseases and 11.6% prevalence of CAC in patients without stroke-related diseases.[17] They showed an equal gender predilection for CAC. Taheri and Moshfeghi revealed a prevalence of 11.0% in 200 postmenopausal women, which were much lower than the findings of the present study.[6] Tanaka et al. evaluated 659 panoramic radiographs from 80 years old subjects and reported a prevalence of 4%.[18] The related prevalence among females was 6.2%, which was also much lower than the findings of the present study. Contrasts in the prevalence rates in various studies may be identified with differences in gender, race, the study span, and sample size.
In the present study, 45.3% patients presented with calcifications on the left side while 36.7% patients had right-sided calcifications and 18% patients showed bilateral calcifications. No statistically significant relation (P > 0.05) was found between the presence of CAC and the side of involvement, similar to the findings of Taheri and Moshfeghi.[6] They showed a prevalence of 40.9% of CAC on the right side, 31.8% on the left side, and 27.3% on both sides. Uthman and Al-Saffar also reported a nonsignificant relation of CAC and the side involved, however, they reported a higher incidence of bilateral calcification when compared to unilateral calcification.[17] Whereas, Ohba et al. reported calcification involvement to be 3 times more prevalent on the right side than on the left side in a Japanese population.[19] The distinction in the side involvement can be explained by the way that carotid bifurcation level contrasts in connection to the cervical vertebrae and also the right and left sides. In addition, bifurcation levels on the level of C5 may not be noticeable on the panoramic radiograph.
Cohen et al. reported that 86% of the observed CAC's are present in patients with at least one risk factor for cerebrovascular disease with significant differences between the two groups.[16] A statistically significant difference was observed between the presence of CAC and history of hypertension in the current study (P < 0.05), similar to the findings of Taheri and Moshfeghi and Uthman and Al-Saffar.[6,17] However, Tanaka et al. did not report any statistically significant correlation between the presence of CAC and high blood pressure. This could be credited to race and age differences of patients selected for the study.[18]
In the present study, 288 patients presented with hypercholesterolemia, of which 202 (70.1%) patients had CAC and this correlation was statistically significant (P < 0.05). The finding of the present study was similar to the findings of Taheri and Moshfeghi,[6] Uthman and Al-Saffar,[17] and Tanaka et al.[18] who also reported a statistically significant difference between the presence of CAC and high cholesterol levels. Totally, 27 patients of the 36 patients with hypercholesterolemia presented with CAC in their study on 200 postmenopausal women. The vicinity of CAC in hypercholesterolemic patients is legitimized by the way that the fat accumulation in atherosclerotic plaque is mainly of cholesterol and its esters.[6]
Cardiovascular disease and osteoporosis are common age-related conditions. There has been an increase in the biological and epidemiological proof to bolster the connection between the two diseases. Low bone mineral density has been related to increased cardiovascular mortality, morbidity, and subclinical measures of atherosclerosis in various epidemiologic studies.[20,21,22] Previously, it has been shown that low skeletal bone mineral density in postmenopausal females’ results in endothelial dysfunction which is the first phase of atherosclerosis.[23] Since calcification in the vascular walls is the last stage of atherosclerosis, it is plainly apparent that elderly males and females with such calcifications may have an expanded risk of osteoporosis or fractures. Friedlander et al. initially demonstrated a significant inverse association between CAC detected on panoramic images and femoral neck bone mineral density measured using dual X-ray absorptiometry in postmenopausal white females.[24] The findings of the present study also demonstrated a significant (P < 0.05) relation between osteoporosis and presence of CAC. It is troublesome in clinical practice to allude every postmenopausal women for bone mineral density testing when considering the cost-effectiveness, along with the limited facilities and scarcity of trained technicians. The incidental perception of CAC on dental panoramic radiographs recommends a high-risk of osteoporosis; however this has been utilized to identify elderly people with a high-risk of cardiovascular diseases and might be a useful indicator to identify asymptomatic individuals who should be referred to medical professionals for further examinations for osteoporosis.[16,25]
The correlation of diabetes mellitus with the presence of CAC was not statistically significant (P > 0.05) similar to the findings of Taheri and Moshfeghi.[6] However, Uthman and Al-Saffar, who assigned diabetic and hyperlipidemia patients to a metabolic group, showed significant differences regarding the increased incidence of CAC in patients with metabolic diseases.[17] Friedlander and Maeder when compared 49 diabetic patients aged 55 years old and higher with no previous history of any cerebrovascular event with 314 controls, reported CAC in 20.4% of diabetic patients.[26] The overall relative risk of stroke and recurrent stroke were reported to be greater in patients with diabetes mellitus.[27] Larger, multicenter studies with accurate tests of blood sugar levels and similar laboratory circumstances are needed to establish a precise relationship association between diabetes and CAC findings on panoramic radiographs.
Association of obesity with atheromas in the carotid artery was also significantly (P > 0.05) related, with 31.9% of obese patients with calcifications. Thus, obesity may be considered a potential risk factor for cerebrovascular events. Notwithstanding, Friedlander and Altman did not report any measurably noteworthy distinction between obesity and presence of atheromatic plaques in the carotid arteries.[9] Kumagai et al. found a relatively higher prevalence of CAC in smokers (14.1% males and 14.3% females) when compared with nonsmokers (4.8% males and 9.0% females) on panoramic radiographs.[28] The higher incidence of CAC in male smokers was fundamentally related while there was no factually noteworthy connection in females, similar to the findings of the current study. Taheri and Moshfeghi also reported no significant association between smoking and CAC.[6] However, it can be asserted that the combination of age and smoking status might influence the prevalence of CAC findings on panoramic radiographs.
Dental practitioners ought to have the competence to diagnose CACs and be able to identify and distinguish them from various anatomical structures such as thyroid cartilage, cricoid cartilage, triticeous cartilage, submandibular lymph nodes, hyoid bone, styloid process, stylohyoid ligament, stylomandibular ligament and other pathological lesions observed in this region.[29] The morphology of CAC can be confused with the above structures by an inexperienced clinician and frequently cause ambiguity. Substantiation of CAC must be conducted with cervical spine radiographs, angiography or Doppler ultrasound analysis and imaging.[30]
The present study demonstrated a prevalence of 22.9% CAC in postmenopausal females, who were associated with one or more atherogenic risk factors. It is not only hormonal changes but also natural phenomena such as puberty, pregnancy, and menopause that incline women to many disease conditions. Along these lines, panoramic radiographs ought to be precisely analyzed in the area of the carotid artery in patients with systemic disease such as hypertension, osteoporosis, diabetes, etc., as well as those with absence of any symptoms. Further studies with larger sample size, in diverse population among various other high-risk groups are encouraged. The limitations of panoramic radiography ought to be considered when detecting CAC. Hence, factors such as obesity, high cholesterol levels, smoking, and hypertension may provide further information than CAC's among dental patients.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Chaveli López B, Sarrión Pérez MG, Jiménez Soriano Y. Dental considerations in pregnancy and menopause. J Clin Exp Dent. 2011;3:e135–44. [Google Scholar]
- 2.Krejci CB, Bissada NF. Women's health issues and their relationship to periodontitis. J Am Dent Assoc. 2002;133:323–9. doi: 10.14219/jada.archive.2002.0171. [DOI] [PubMed] [Google Scholar]
- 3.Grady D, Rubin SM, Petitti DB, Fox CS, Black D, Ettinger B, et al. Hormone therapy to prevent disease and prolong life in postmenopausal women. Ann Intern Med. 1992;117:1016–37. doi: 10.7326/0003-4819-117-12-1016. [DOI] [PubMed] [Google Scholar]
- 4.Speroff L. Menopause and hormone replacement therapy. Clin Geriatr Med. 1993;9:33–55. [PubMed] [Google Scholar]
- 5.Alves N, Deana NF, Garay I. Detection of common carotid artery calcifications on panoramic radiographs: Prevalence and reliability. Int J Clin Exp Med. 2014;7:1931–9. [PMC free article] [PubMed] [Google Scholar]
- 6.Taheri JB, Moshfeghi M. Prevalence of calcified carotid artery on panoramic radiographs in postmenopausal women. J Dent Res Dent Clin Dent Prospects. 2009;3:46–51. doi: 10.5681/joddd.2009.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Friedlander AH, Friedlander IK. Identification of stroke prone patients by panoramic radiography. Aust Dent J. 1998;43:51–4. doi: 10.1111/j.1834-7819.1998.tb00153.x. [DOI] [PubMed] [Google Scholar]
- 8.Usha VA, David MP. Prevalence of carotid artery atheromas in postmenopausal women: A digital panoramic radiographic study. J Indian Acad Oral Med Radiol. 2013;25:93–8. [Google Scholar]
- 9.Friedlander AH, Lande A. Panoramic radiographic identification of carotid arterial plaques. Oral Surg Oral Med Oral Pathol. 1981;52:102–4. doi: 10.1016/0030-4220(81)90181-x. [DOI] [PubMed] [Google Scholar]
- 10.Vengalath J, Puttabuddi JH, Rajkumar B, Shivakumar GC. Prevalence of soft tissue calcifications on digital panoramic radiographs: A retrospective study. J Indian Acad Oral Med Radiol. 2014;26:385–9. [Google Scholar]
- 11.Friedlander AH. Panoramic radiography: The differential diagnosis of carotid artery atheromas. Spec Care Dentist. 1995;15:223–7. doi: 10.1111/j.1754-4505.1995.tb00522.x. [DOI] [PubMed] [Google Scholar]
- 12.Ross R. Atherosclerosis - an inflammatory disease. N Engl J Med. 1999;340:115–26. doi: 10.1056/NEJM199901143400207. [DOI] [PubMed] [Google Scholar]
- 13.Sisman Y, Ertas ET, Gokce C, Menku A, Ulker M, Akgunlu F. The prevalence of carotid artery calcification on the panoramic radiographs in Cappadocia region population. Eur J Dent. 2007;1:132–8. [PMC free article] [PubMed] [Google Scholar]
- 14.Pornprasertsuk-Damrongsri S, Thanakun S. Carotid artery calcification detected on panoramic radiographs in a group of Thai population. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101:110–5. doi: 10.1016/j.tripleo.2005.04.002. [DOI] [PubMed] [Google Scholar]
- 15.Roldán-Chicano R, Oñate-Sánchez RE, López-Castaño F, Cabrerizo-Merino MC, Martínez-López F. Panoramic radiograph as a method for detecting calcified atheroma plaques. Review of literature. Med Oral Patol Oral Cir Bucal. 2006;11:E261–6. [PubMed] [Google Scholar]
- 16.Cohen SN, Friedlander AH, Jolly DA, Date L. Carotid calcification on panoramic radiographs: An important marker for vascular risk. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002;94:510–4. doi: 10.1067/moe.2002.125580. [DOI] [PubMed] [Google Scholar]
- 17.Uthman AT, Al-Saffar AB. Prevalence in digital panoramic radiographs of carotid area calcification among Iraqi individuals with stroke-related disease. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;105:e68–73. doi: 10.1016/j.tripleo.2007.11.009. [DOI] [PubMed] [Google Scholar]
- 18.Tanaka T, Morimoto Y, Ansai T, Okabe S, Yamada K, Taguchi A, et al. Can the presence of carotid artery calcification on panoramic radiographs predict the risk of vascular diseases among 80-year-olds? Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101:777–83. doi: 10.1016/j.tripleo.2005.10.035. [DOI] [PubMed] [Google Scholar]
- 19.Ohba T, Takata Y, Ansai T, Morimoto Y, Tanaka T, Kito S, et al. Evaluation of calcified carotid artery atheromas detected by panoramic radiograph among 80-year-olds. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;96:647–50. doi: 10.1016/j.tripleo.2003.07.001. [DOI] [PubMed] [Google Scholar]
- 20.Gerber Y, Melton LJ, 3rd, Weston SA, Roger VL. Osteoporotic fractures and heart failure in the community. Am J Med. 2011;124:418–25. doi: 10.1016/j.amjmed.2010.11.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chiang CH, Liu CJ, Chen PJ, Huang CC, Hsu CY, Chen ZY, et al. Hip fracture and risk of acute myocardial infarction: A nationwide study. J Bone Miner Res. 2013;28:404–11. doi: 10.1002/jbmr.1714. [DOI] [PubMed] [Google Scholar]
- 22.Farhat GN, Cauley JA. The link between osteoporosis and cardiovascular disease. Clin Cases Miner Bone Metab. 2008;5:19–34. [PMC free article] [PubMed] [Google Scholar]
- 23.Sanada M, Taguchi A, Higashi Y, Tsuda M, Kodama I, Yoshizumi M, et al. Forearm endothelial function and bone mineral loss in postmenopausal women. Atherosclerosis. 2004;176:387–92. doi: 10.1016/j.atherosclerosis.2004.05.021. [DOI] [PubMed] [Google Scholar]
- 24.Friedlander AH, Chang TI, Aghazadehsanai N, Berenji GR, Harada ND, Garrett NR. Panoramic images of white and black post-menopausal females evidencing carotid calcifications are at high risk of comorbid osteopenia of the femoral neck. Dentomaxillofac Radiol. 2013;42:20120195. doi: 10.1259/dmfr.20120195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Alman AC, Johnson LR, Calverley DC, Grunwald GK, Lezotte DC, Hokanson JE. Validation of a method for quantifying carotid artery calcification from panoramic radiographs. Oral Surg Oral Med Oral Pathol Oral Radiol. 2013;116:518–24. doi: 10.1016/j.oooo.2013.06.026. [DOI] [PubMed] [Google Scholar]
- 26.Friedlander AH, Maeder LA. The prevalence of calcified carotid artery atheromas on the panoramic radiographs of patients with type 2 diabetes mellitus. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;89:420–4. doi: 10.1016/s1079-2104(00)70122-3. [DOI] [PubMed] [Google Scholar]
- 27.Hankey GJ, Jamrozik K, Broadhurst RJ, Forbes S, Burvill PW, Anderson CS, et al. Long-term risk of first recurrent stroke in the Perth Community Stroke Study. Stroke. 1998;29:2491–500. doi: 10.1161/01.str.29.12.2491. [DOI] [PubMed] [Google Scholar]
- 28.Kumagai M, Yamagishi T, Fukui N, Chiba M. Long-term cigarette smoking increases the prevalence of carotid artery calcification seen on panoramic dental radiographs in male patients. Tohoku J Exp Med. 2007;212:21–5. doi: 10.1620/tjem.212.21. [DOI] [PubMed] [Google Scholar]
- 29.Kamikawa RS, Pereira MF, Fernandes A, Meurer MI. Study of the localization of radiopacities similar to calcified carotid atheroma by means of panoramic radiography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101:374–8. doi: 10.1016/j.tripleo.2005.03.030. [DOI] [PubMed] [Google Scholar]
- 30.Friedlander AH, Friedlander IK. Panoramic dental radiography: An aid in detecting individuals prone to stroke. Br Dent J. 1996;181:23–6. doi: 10.1038/sj.bdj.4809143. [DOI] [PubMed] [Google Scholar]


