Abstract
Background:
Reproductive tract infections (RTIs) have adverse implications on the health of the women. Community-based studies in India have shown a high prevalence of RTIs but here is a lack of sizeable literature from urban slums and resettlement areas.
Aims and Objectives:
The objective was to document the prevalence and determinants of RTIs in married women (15-49 years) residing in an urban slum in Delhi, India.
Materials and Methods:
The study was conducted in an urban resettlement colony of Gokulpuri in the North-East district of Delhi. Systematic random sampling method was adopted to choose the study subjects, that is, married and non-pregnant women in the reproductive age group (15-49 years) residing in the study area. Data were collected using a pretested semi-structured questionnaire, through the house to house visits. The diagnosis of RTIs was made as per the World Health Organization syndromic approach. Data were analyzed in SPSS version 16 (Chicago, IL, USA).
Results:
A total of 802 women were interviewed. The mean age of study subjects was 30.79 ± 7 years. A total of 352 (43.9%) women currently had symptoms of RTIs. The most frequently reported symptoms included abdominal pain (68.2%), back pain (69.6%), and vaginal discharge (59.3%). Older women (≥25 years) (odds ratio [OR] 2.2, 95% confidence interval [CI]; 1.4-3.5), those belonging to the lower socioeconomic status (OR 2.1, 95% CI; 1.5-2.9), those using cloth during menses (OR 2.6, 95% CI; 1.6-4.3), those having more than three pregnancies (OR 1.8, 95% CI; 1.2-2.6) and those using an intrauterine contraceptive device (OR 11.8, 95% CI; 4.3-32.0) had higher odds of having RTIs.
Conclusions:
A high case load was found based on the syndromic approach. Generating community awareness, ensuring proper menstrual hygiene, and improving the socioeconomic status would help in reducing the cases of RTI.
Keywords: Delhi, married women, reproductive tract infections, risk factors, sexually transmitted infections, urban slum
INTRODUCTION
Reproductive tract infections (RTIs) are a hidden epidemic leading to enormous health and economic consequence worldwide. They have huge repercussions on health mainly in the form of pelvic inflammatory disease, infertility (in both women and men), ectopic pregnancy, and adverse pregnancy outcomes such as miscarriage, stillbirth, preterm birth, and congenital infections.[1] Sexually transmitted infections (STIs)/RTIs are also known to increase the risk of HIV transmission.[2]
Globally, according to 2005 World Health Organization (WHO) estimates, 448 million new cases of curable STIs (syphilis, gonorrhea, chlamydia, and trichomoniasis) occur annually in adults aged 15-49 years.[3] In India, the annual incidence of STIs is estimated to be 5%.[4] The prevalence of self-reported morbidity varies in different regions in India.[5] Various community-based studies in India have shown the prevalence of RTIs to range from 39% to 84%.[6,7] It not only depends on the prevalence of RTIs/STIs in that area, but also on various other factors such as the inability of women to take decisions on their own, their impoverish status within the family, and their health seeking behavior.
Prior studies have reflected upon various factors influencing the occurrence of RTIs mainly socioeconomic status, poor hygiene, intra-uterine device (IUD) insertion, place of residence (urban/rural), male substance abuse, extra-marital sexual relations, and non-use of condoms.[8,9,10] Recognizing the risk factors and addressing them is required to combat the growing burden of RTIs. Although many studies have been conducted in various parts of the country with the aim to document the prevalence of STIs/RTIs and its risk factors, yet there is a lack of sizeable literature from urban slums and resettlement areas. The current study was undertaken to fill this existing lacunae.
MATERIALS AND METHODS
Study area and period
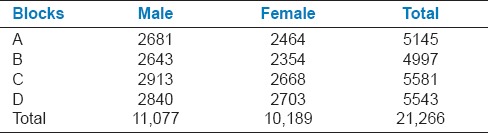
This study was conducted in an urban resettlement colony of Gokulpuri in the North-East district of Delhi. It is the field practice area of Department of Community Medicine, Maulana Azad Medical College, New Delhi, India. It represents well the situation of urban resettlement slums in Delhi and has been in existence for more than 20 years. According to the economic survey of Delhi, 2002 slums have been categorized typologically into eight types. Resettlement colonies were formed in Delhi under a scheme wherein the residents of slums were relocated in permanent colonies.[11] Gokulpuri is divided into four blocks with a total population was around 21,000 [Table 1]. Healthcare services are largely provided by the Urban Health Centre (UHC) Gokulpuri which is associated with the Department of Community Medicine at Maulana Azad Medical College, New Delhi. As per the yearly survey conducted by the UHC along with the Department of Community Medicine, Gokulpuri mostly comprises of the urban population belonging to the lower to lower middle socioeconomic class. There were nearly 3000 eligible couples in the study area during the year 2010. The study was conducted over a period of 1-year from November 2010 to December 2011.
Table 1.
Distribution of population in the four blocks in Gokulpuri
Sample size and sampling strategy
Sample size was calculated considering a prevalence of RTIs as 36.8%,[12] relative precision of 10%, and an alpha error of 0.05. Accounting for a non-response rate of 10%, the final sample size came out to be 756, and it was decided to include 800 participants in the study. Married and non-pregnant women in the reproductive age group (15-49 years) residing in the area were eligible to be included in the study. Systematic random sampling method was adopted to choose the study subjects. Based on the survey data of the study area there were 3305 eligible couples. Considering that the required sample size was 800, the sampling interval came out to be 4. To ensure a representative sample, 200 participants were included from each block. The first woman in a block was selected randomly, and then the rest of the women were included from every fourth consecutive couple till a sample size of 200 was reached. This procedure was repeated in all the blocks to get a total sample size of 800. When houses were found locked, a second visit was made before excluding them from the study. Furthermore, in cases where females denied participation in the study, the next eligible woman was approached and the original sequence was maintained thereafter.
Data collection
Data were collected using a pretested semi-structured interview schedule, which was divided into four parts-sociodemographic profile; knowledge, attitude, and practices regarding RTIs; History of RTIs; clinical examination. House to house visits were made. The questions in the interview schedule were asked in the local language, that is, Hindi. The questions were mostly open-ended and the probable responses were listed to facilitate recording and minimizing interview time. The diagnosis of RTIs was made as per the guidelines of WHO for the syndromic approach.[13]
The data were collected by a postgraduate student of Community Medicine (MB), as a part of the dissertation. The data collector was trained in research methodology and data collection techniques. Around 15% of the data collected was cross-checked by the senior investigator (PL) for completeness and accuracy of the information collected.
Statistical analysis
Data were entered in Microsoft Excel and analyzed in Statistical Package for Social Sciences (SPSS) designed by IBM, Chicago, Illinois, USA. Descriptive analysis was done with proportions reported with 95% confidence interval (CI), mean ± standard deviation (SD), and median (interquartile range). Chi-square and Fisher's test were applied to compare proportions. Logistic regression was performed to document the independent risk factors.
RESULTS
Sociodemographic profile of the participants
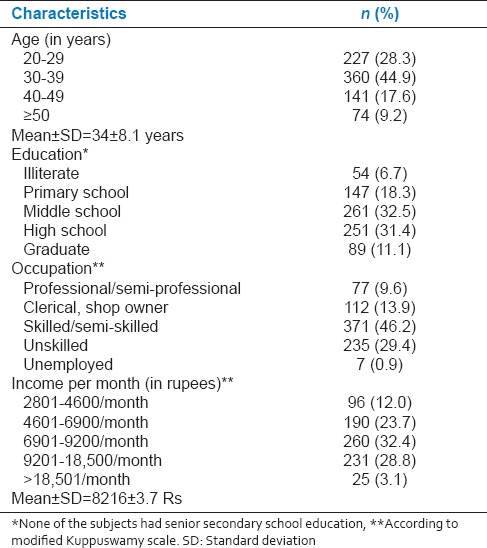
A total of 835 women were approached out of which 802 gave consent to participate in the study. The mean age of study subjects was observed to be 30.79 ± 7 years. Majority of the study subjects were Hindus (84.78%) [Table 2]. Approximately 27% of the study women were illiterate. Majority of the study subjects were housewives (89%). Most of the study subjects belonged to middle socioeconomic class (68%), followed by those who belonged to the lower socioeconomic class (32.2%) [Table 2]. The mean age of the spouses was observed to be 34 (±8.1) years [Table 3].
Table 2.
Sociodemographic characteristics of the study subjects (n = 802)
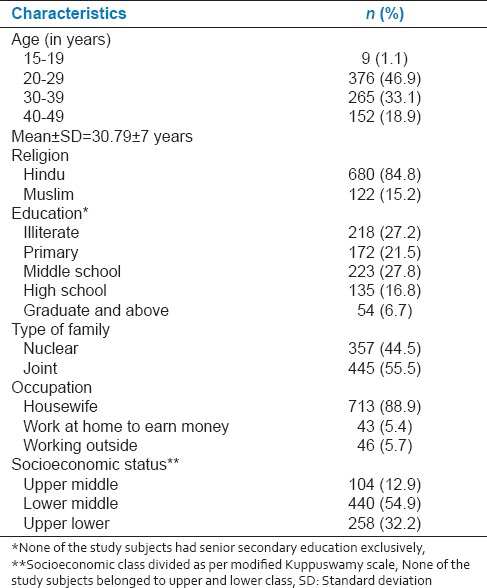
Table 3.
Sociodemographic profile of spouses of respondents (n = 802)
Obstetric history and contraceptive use among the study subjects
The mean age of marriage was 18 years (±3.7) years. Majority of the women (95.2%) consummated between the ages 16 and 25 years. The mean age of consummation was 19 years (±2.12) years. Mean number of pregnancies women went through was observed to be 2.78 ± 1.76 and majority of the women (77.8%) experienced multiple pregnancies. Mean number of children was observed to 2.17 (±1.2). Only 25.8% women were currently using contraceptive measures. Use of barrier methods, which are known to protect against RTIs, was observed only by 9.9% of the study women. Terminal methods had been opted 4.2% women.
Personal hygiene and menstrual practices
In this study, majority of the study subjects (87%) took a bath every day. Around 61.0% of the women washed their perineal area with soap and water every time they took a bath. Further, almost all (99%) study subjects had been washing hands with soap and water after using the toilet. Age at menarche of the study subjects ranged from 11 to 17 years. The mean (SD) age at menarche was observed to be 14.18 (1.3) years. Majority of the study women (69.9%) had no menstrual problems. Among menstrual problems, most commonly observed ones were dysmenorrhea (27.8%) and irregular menstrual cycles (10.7%). The most common material used by women to absorb menstrual blood flow was a piece of cloth (76.88%). Of these, 15% women reused the same cloth after washing. Sanitary napkins were used only by 23.3% of the women.
Self-reported reproductive tract infection symptoms and treatment seeking
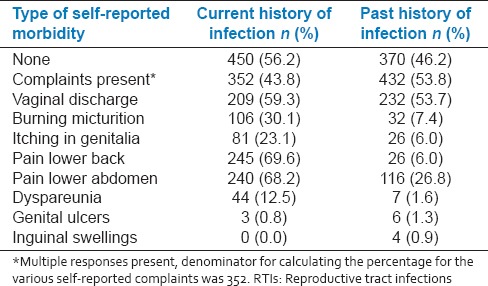
More than half of the study women (53.8%) had symptoms of RTI in the past. Approximately one-fourth (24%) women gave a history of RTI like symptoms within past 1-month, 38% within 6 months, and 11% 1-year. A total of 352 (43.9%) women were reported to have symptoms of RTIs on the day of visit. The most frequently reported symptoms included abdominal pain (68.2%), back pain (69.6%), and vaginal discharge (59.3%) [Table 4]. Dyspareunia was complained by 12.5% of the women. Overall, 26.8% women did not consult any healthcare facility for treatment of their illness. Of those who sought care, a total of 84.8% women visited allopathic doctors whereas 15.2% visited local traditional/faith healers.
Table 4.
Prevalence of self-reported morbidity of RTIs (n = 802)
Determinants of self-reported reproductive tract infections
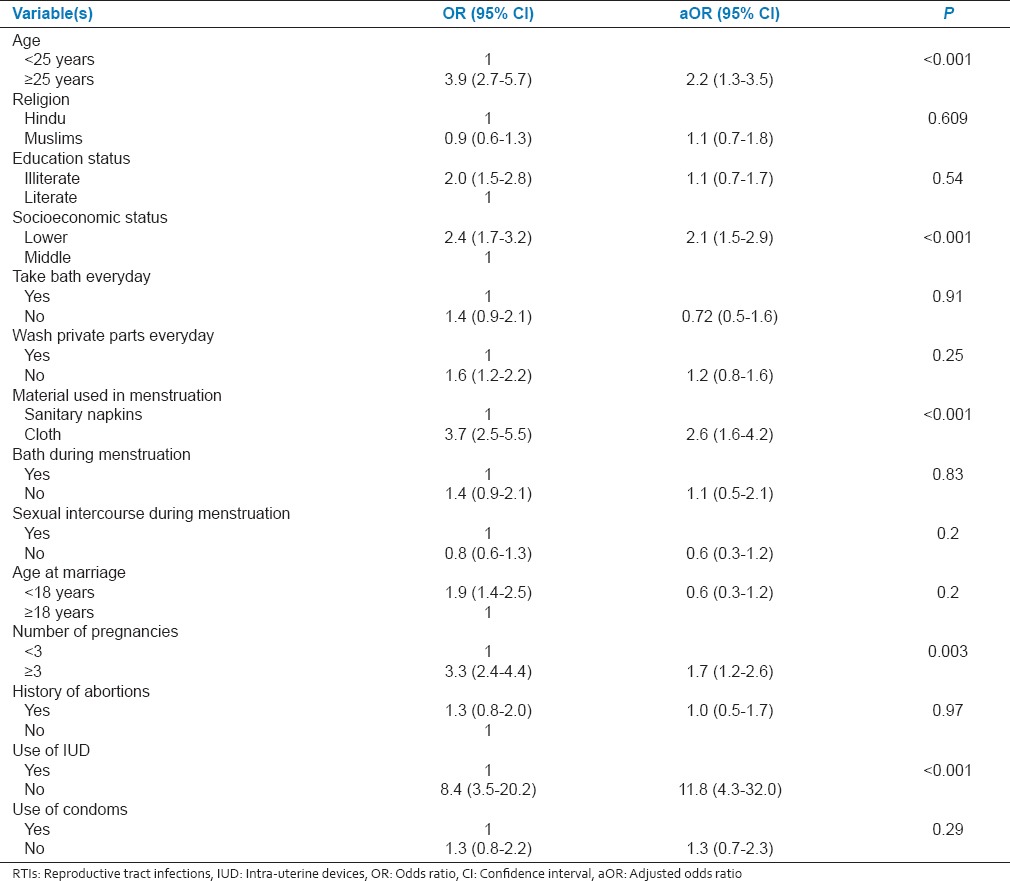
The prevalence of self-reported RTIs was observed to be higher among older women (≥25 years) (odds ratio [OR] 2.2, 95% CI; 1.4-3.5) as compared to young women <25 years of age [Table 5]. The odds of having RTI were more in women belonging to the lower socioeconomic status (OR 2.1, 95% CI; 1.5-2.9). Women who used cloth during menses (OR 2.6, 95% CI; 1.6-4.3), those having more than three pregnancies (OR 1.8, 95% CI; 1.2-2.6), those using an intrauterine contraceptive device (IUCD) (OR 11.8, 95% CI; 4.3-32.0) had higher odds of having RTIs [Table 5].
Table 5.
Determinants of RTIs obtained on multivariate logistic regression
DISCUSSION
The current study aimed to document the prevalence of self-reported RTIs among married females in urban slums of Delhi, India. All the women enrolled in the study were probed regarding reproductive morbidities namely, vaginal discharge, genital ulcers, inguinal swellings, pain lower abdomen, pain lower back, dyspareunia, burning micturition, and itching. In total, 43.9% women complained any or all of the above-mentioned symptoms during the data collection period, which is largely an issue of concern. The prevalence of symptoms suggestive of RTIs/STIs in the study population (43.9%) was higher as compared with what has been documented in other studies from India; 27% in urban women of Agra district of Uttar Pradesh; 35.6% in reproductive age women living in urban slums of Tirupati, Andhra Pradesh; 32% in urban women in Sundergarh district of Orissa; and 27.8% in Punjab.[14,15,16,17]
Prior literature has underscored the importance of using the laboratory diagnosis for RTI/STI and found that the syndromic approach reported higher results than laboratory diagnosis approach.[18,19] This over-reporting of RTI/STI based on syndromic approach cannot be ruled out in the present study. However, self-reporting of STI symptoms is a positive observation as it compels one to seek medical treatment early. Seeking prompt treatment for STI symptoms will increase women's chances of being diagnosed early and reduced complications.
In the present study, the majority of the women preferred to visit allopathic doctors in case of their reproductive morbidities. The possible reason this could be easy access to a healthcare facility as the UHC run by Department of Community Medicine; Maulana Azad Medical College, a tertiary level hospital, is within the locality and the treatment is provided free of cost. Reasons for not availing any kind of health care treatment, as seen in around 27% of the affected women in the present study and reasons for visits to traditional healers, as observed in around 15% of the women need to researched and appropriate measures to improve health care seeking behavior are required to be formulated.
In the present study, older women (>25 years) and those with ≥3 pregnancies were observed to be at higher risk of developing RTIs. This association might be due to longer periods of unprotected sex as couples seek to conceive and this increases their risks of infection. Early sexual activity and increasing number of pregnancies may have detrimental effects on a woman's health and also lengthen the time span for which she remains susceptible to reproductive tract morbidities. The low socioeconomic status of the women was observed to be a risk factor of developing RTI among women in the present study. Adequate menstrual hygiene is crucial for the health of the women. There is imminent need to provide low-cost quality sanitary pads in the community to address the problem of RTIs among women especially in slum dwellers. As seen in the present study, the majority of the women (76.7%) in were using cloth during menstruation. The risk of having RTI in these women was more than double in comparison to women who were using sanitary napkins. This finding in conformity with that reported by Bhawna Pant and Dasgupta A in their study.[20,21]
In the present study, RTIs were found to be significantly associated with the insertion of IUDs. The increased prevalence in women using IUDs could be due to the improper insertion techniques, including care to ensure sterile conditions, and poor follow-up care after insertion. Sharma and Gupta in West Bengal, Rathore et al. in rural Rajasthan, and Kumar et al. in the Dharmapuri district of Tamil Nadu have reported similar findings.[22,23,24]
A major limitation of our study is that laboratory investigations were not used to confirm the diagnosis of RTIs/STIs. However, our study has the advantage of being community-based. Symptomatic diagnosis of RTIs/STIs based on a syndromic approach has also been supported by WHO and Center for Disease Control and Prevention as an effective and inexpensive approach for diagnosis of RTIs/STIs in low-resource settings.
CONCLUSIONS
In this study, a high case load has been found based on the syndromic approach. More than half of the study women had symptoms of RTI in the past and of them, one-fourth gave a history of RTI like symptoms within past 1-month. The prevalence of self-reported RTIs was observed to be higher among older women (≥25 years), belonging to the lower socioeconomic status, those who used cloth during menses, those having more than three pregnancies and among those using an IUCD.
Appropriate steps should be taken for adequate management of these cases. There is also a need to conduct further studies to assess various behavioral and sociodemographic factors, predisposing women to the risk of RTIs and STDs. Health services should be improved and made more accessible so that women feel comfortable in seeking treatment and are not deterred by concerns over privacy and confidentiality. Measures such as generating community awareness, ensuring use of sanitary napkins, proper menstrual hygiene, improving the socioeconomic status, ascertaining sterile insertion of IUD, and follow-up thereafter would help in reducing the cases of RTI. Early treatment seeking from qualified health care personnel will further reduce the complications.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Rowley J, Berkley S. Sexually transmitted diseases. In: Murray CJ, Lopez AD, editors. Health Dimensions of Sex and Reproduction. The Global Burden of Sexually Transmitted Diseases, HIV, Maternal Conditions, Perinatal Disorders, and Congenital Anomalies. Massachusetts, USA: The Harvard School of Public Health, on behalf of WHO and World Bank, Harvard University Press; 1998. pp. 19–110. [Google Scholar]
- 2.van de Wijgert JH, Morrison CS, Brown J, Kwok C, Van Der Pol B, Chipato T, et al. Disentangling contributions of reproductive tract infections to HIV acquisition in African Women. Sex Transm Dis. 2009;36:357–64. doi: 10.1097/OLQ.0b013e3181a4f695. [DOI] [PubMed] [Google Scholar]
- 3.WHO. Sexually Transmitted Diseases. Fact Sheet No. 110; Auguest. 2011 [Google Scholar]
- 4.New Delhi: National AIDS Control Organisation; 2007. Government of India, Ministry of Health and Family Welfare. National Guidelines on Prevention, Management and Control of Reproductive tract Infections Including Sexually Transmitted Diseases. [Google Scholar]
- 5.Geneva: World Health Organization; 2001. WHO. Global prevalence and incidence of curable sexually transmitted infections overview and estimates. [Google Scholar]
- 6.Bang RA, Bang AT, Baitule M, Choudhary Y, Sarmukaddam S, Tale O. High prevalence of gynaecological diseases in rural Indian women. Lancet. 1989;1:85–8. doi: 10.1016/s0140-6736(89)91438-4. [DOI] [PubMed] [Google Scholar]
- 7.Latha K, Kanani SJ, Maitra N, Bhattacharya RV. Prevalence of clinically detectable gynaecological morbidity in India: Results of four community based studies. Fam Welf. 1997;43:8–16. [Google Scholar]
- 8.Weinhardt LS, Carey MP. Does alcohol lead to sexual risk behavior? Findings from event-level research. Annu Rev Sex Res. 2000;11:125–57. [PMC free article] [PubMed] [Google Scholar]
- 9.Bhatia JC, Cleland J. Self-reported symptoms of gynecological morbidity and their treatment in South India. Stud Fam Plann. 1995;26:203–16. [PubMed] [Google Scholar]
- 10.Oomman NM. Poverty and Pathology: Comparing Rural Rajasthani Women's Ethnomedical Models with Biomedical Models of Reproductive Behaviour. Ph.D. Thesis Johns Hopkins University. 1996 [Google Scholar]
- 11.Vol. 2. New Delhi: Govt. of India; 2002. [Last accessed on 2015 Feb 17]. Planning Commission. Nutrition and Social Safety Net, Eleventh Five Year Plan; pp. 341–6. Available from: http://www.planningcommission.nic.in . [Google Scholar]
- 12.Ray K, Bala M, Bhattacharya M, Muralidhar S, Kumari M, Salhan S. Prevalence of RTI/STI agents and HIV infection in symptomatic and asymptomatic women attending peripheral health set-ups in Delhi, India. Epidemiol Infect. 2008;136:1432–40. doi: 10.1017/S0950268807000088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Geneva, Swtizerland: WHO; 2003. WHO. Guidelines for the Management of Sexually Transmitted Diseases. [Google Scholar]
- 14.Nandan D, Misra SK, Sharma A, Jain M. Estimation of prevalence of RTI's/STD's among women of reproductive age group in district Agra. Indian J Community Med. 2002;27:110–3. [Google Scholar]
- 15.Devi BS, Swarnalatha N. Prevalence of RTI/STI among reproductive age women (15-49 years) in urban slums of Tirupati Town, Andhra Pradesh. Health Popul Perspect Issues. 2007;30:56–70. [Google Scholar]
- 16.Panda SC, Sarangi L, Bebartta D, Parida S, Panigrahi OP. Prevalence of RTI/STI among women of reproductive age in district Sundergarh (Orissa) Indian J Pract Doct. 2007. [Last accessed on 2014 Jun 21]. p. 4. Available from: http://www.indmedica.com/journals.php?journalid=3&issueid=94&articleid=1276&action=article .
- 17.Bhawsar RD, Singh JP, Khanna A. Determinants of RTIs/STIs among women in Punjab and their health seeking behaviour. Indian J Fam Welf. 2005;51:24–34. [Google Scholar]
- 18.Ray K, Muralidhar S, Bala M, Kumari M, Salhan S, Gupta SM, et al. Comparative study of syndromic and etiological diagnosis of reproductive tract infections/sexually transmitted infections in women in Delhi. Int J Infect Dis. 2009;13:e352–9. doi: 10.1016/j.ijid.2008.11.021. [DOI] [PubMed] [Google Scholar]
- 19.Prabha ML, Sasikala G, Bala S. Comparison of syndromic diagnosis of reproductive tract infections with laboratory diagnosis among rural married women in Medak district, Andhra Pradesh. Indian J Sex Transm Dis. 2012;33:112–5. doi: 10.4103/2589-0557.102121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pant B, Singh J, Bhatnagar M, Garg S, Chopra H, Bajpai S. Social Correlates in Reproductive Tract Infections among Married Women in Rural Area of Meerut. Indian J Community Med. 2008;33:52–3. doi: 10.4103/0970-0218.39246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dasgupta A, Sarkar M. Menstrual hygiene: How hygienic is the adolescent girl? Indian J Community Med. 2008;33:77–80. doi: 10.4103/0970-0218.40872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sharma S, Gupta B. The prevalence of reproductive tract infections and sexually transmitted diseases among married women in the reproductive age group in a rural area. Indian J Community Med. 2009;34:62–4. doi: 10.4103/0970-0218.45376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rathore M, Swami SS, Gupta BL, Sen V, Vyas BL, Bhargav A, et al. Community-based study of self reported morbidity of reproductive tract among women of reproductive age in rural areas of Rajasthan. Indian J Community Med. 2003;28:117–21. [Google Scholar]
- 24.Kumar S, Gupta SD, Kumar D, Singh JP, Bhawsar R. Reproductive tract infections and their associated risk factors among the women in Bundi District of Rajasthan. J Hum Ecol. 2002;13:307–10. [Google Scholar]


