Abstract
Aims:
We aimed to validate Mannheim peritonitis index (MPI) for prediction of outcome in patients with perforation peritonitis.
Materials and Methods:
A prospective study involving 100 subjects operated for perforation peritonitis over the period of 2 years was designed. Postevaluation of predesigned performa, MPI score was calculated and analyzed for each patient with death being the main outcome measure. The MPI scores were divided into three categories; scores <15 (category 1), 16-25 (category 2), and >25 (category 3).
Results:
Our study consisted of 82 males and 18 females (male:female ratio 4.56:1), with the mean patients age of 37.96 ± 17.49 years. 47, 26, and 27 cases belonged to MPI score categories 1, 2, and 3, respectively. The most common origin of sepsis was ileal with small intestine dominating the source of perforation. When the individual parameters of MPI score were assessed against the mortality only, age >50 years (P = 0.015), organ failure (P = 0.0001), noncolonic origin of sepsis (P = 0.002), and generalized peritonitis (P = 0.0001) significantly associated with mortality. The sensitivity of MPI was 92% with a specificity of 78% in receiver operating characteristic curves.
Conclusion:
MPI is an effective tool for prediction of mortality in cases of perforation peritonitis.
Keywords: Mannheim peritonitis index, perforation peritonitis, receiver operating characteristic curve
INTRODUCTION
Peritonitis is inflammation of the peritoneum and/or peritoneal cavity due to localized or generalized infections. Most cases of peritonitis are consequence to the invasion of the peritoneal cavity by bacteria from the gut. Hence, early prognostic evaluation of abdominal sepsis is desirable to select high-risk patients for more aggressive therapeutic procedures and to provide an objective classification of the severity of the disease.[1,2,3] Treatment is primarily surgical and in case of doubt, early surgical intervention is always desired especially in previously healthy patients and those with postoperative peritonitis. Different scorings are used to predict the outcome in patients with peritonitis. These scoring systems can be a good tool to predict and hence to monitor the priority of treatment for better care in case of peritonitis.[4] Moreover, performing a risk analysis for cases by detecting the prognostic factors that affect morbidity and mortality may help prognosis prediction. Along with the predictive factors affecting the morbidity and mortality of cases, scoring systems have also been developed with parameters including demographic and clinical features.[5,6,7,8] Here, we assessed the utility of one such scoring system that is, Mannheim peritonitis index (MPI) score system[6,9] in predicting the outcome of patients with perforation peritonitis.
MATERIALS AND METHODS
This is a hospital-based prospective study designed to evaluate the validity of MPI in predicting prognosis in patients with perforation peritonitis. Total of 100 patients with secondary peritonitis admitted in the surgery department, who underwent exploratory laparotomy through a midline vertical incision were enrolled in the study. These 100 patients had confirmed diagnosis of perforation peritonitis. The study was approved from Institutional Ethical Committee. Necessary consents were taken before enrolling in the study. The study covered a period of 24 months from December, 2012 to December, 2014.
Inclusion criteria: Patients aged >15 years with perforation peritonitis were enrolled for the study following informed consent.
Following exclusion criteria were used in this study: Patients who would not be able to take full treatment (due to financial or other constraints)
Cases of primary peritonitis.
Cases that are ruled out after investigations.
Cases refused or unfit for surgery.
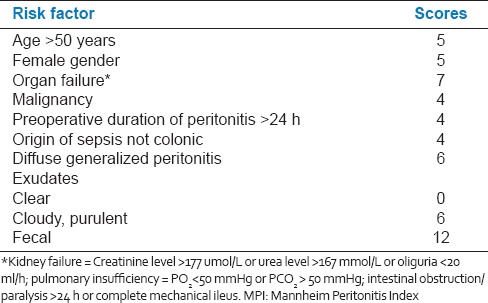
Following evaluation using a predesigned performa, MPI score was calculated for each patient and the patients were followed-up till death or discharge from the hospital [Table 1]. Death was the main outcome measure against which the MPI scores were analyzed. The MPI scores were divided under three categories; scores <15 (category 1), 16-25 (category 2), and >25 (category 3). The patient's data were analyzed statistically.
Table 1.
MPI
Statistical analysis
An analysis was performed using SPSS software for Windows (version 11.0, 2001, SPSS Inc., Chicago, IL, USA). The statistical analysis was done by Pearsons Chi-square test for qualitative data, students t-test for quantitative data. The receiver operating characteristic (ROC) curves were plotted with sensitivity against 1-specificity.
RESULT
Of the 100 cases of perforation peritonitis over the period of 2 years in our institute, who underwent emergency laparotomy, 82 males and 18 females (male:female ratio 4.56:1). The mean patient age in our study was 37.96 ± 17.49 years. 47, 26, and 27 patients belonged to MPI score categories 1, 2, and 3, respectively.
The mean patient age was 33.52 ± 13.22 years, 37.15 ± 19.60 years and 37.15 ± 19.4 years in MPI score category 1, 2, and 3, respectively. The mean age of patients who survived and did not survive was similar (P = 0.22). Significantly greater numbers of female patients were in MPI category 3 compared to category 1 or 2. The most common origin of sepsis was ileal [Figure 1], with small intestine dominating the source of perforation. The gastric perforation was second to the small intestine in presenting as peritonitis.
Figure 1.
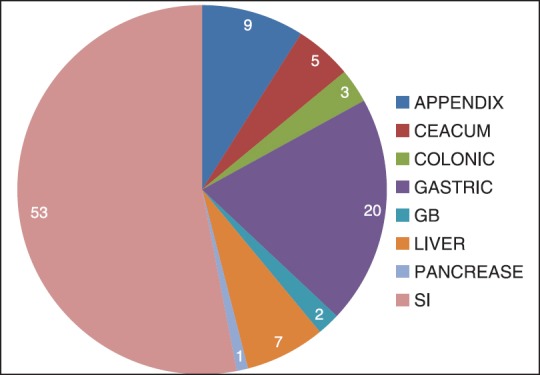
Distribution of origin of sepsis
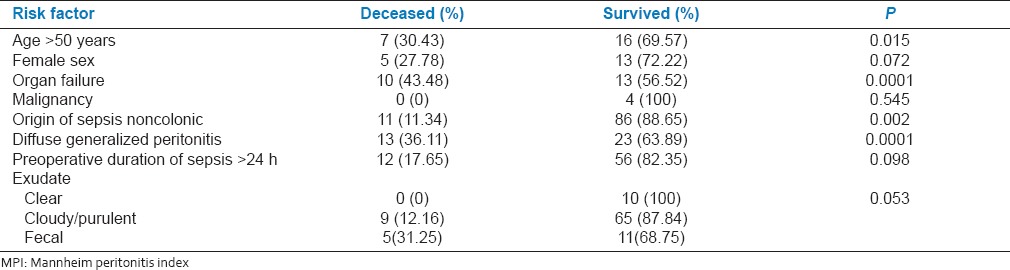
When the individual parameters of MPI score were assessed against the mortality only, age >50 years (P = 0.015), organ failure (P = 0.0001), noncolonic origin of sepsis (P = 0.002) and generalized peritonitis (P = 0.0001) were significantly associated with mortality [Table 2].
Table 2.
Individual mortality risk of components of MPI
The mortality rates observed were higher in category 3 of MPI. The difference in mortalities among MPI score categories was observed to be highly significant (P < 0.0001) [Table 3]. On plotting the ROC curve, the sensitivity was 92%, and specificity was 78% with area under curve (AUC) being 0.9 at a cut-off of 21 MPI score [Figure 2].
Table 3.
Survival within MPI score categories
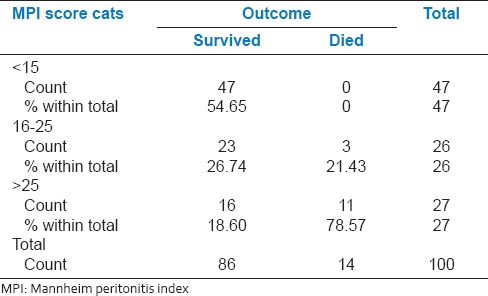
Figure 2.
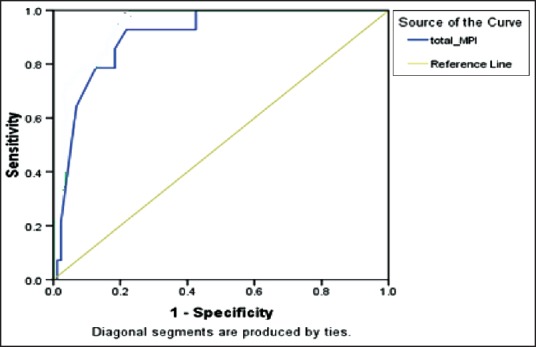
Receiver operating characteristic curve
DISCUSSION
Various studies have reported efficacy of MPI as an independent prognostic scoring system in predicting outcome in secondary peritonitis. We have compared our study findings with previously reported studies [Table 4]. In the present study, the sensitivity and specificity of MPI were 92% and 78%, respectively, at a cut-off of 21 MPI score. The area under ROC curve was 0.9. Our results are comparable to previous reports.[6,10,11,12,13,14] Although a minor higher sensitivity and lower specificity observed may be attributed to differences in sample sizes and setting of cut-off values.
Table 4.
Comparative validity assessment of MPI scores in predicting prognosis of peritonitis
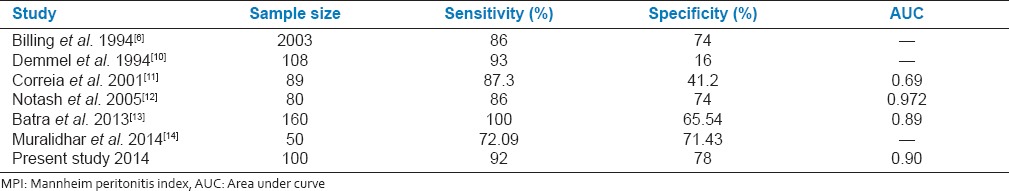
Correia et al.[11] retrospectively analyzed data of 89 cases with perforation peritonitis and found the mean MPI score to be 26.6 points (range: 5-47), with a sensitivity of 87.3%, and a specificity of 41.2%. The best accuracy (69.7%) was reached at a score of 21. Notash et al.[12] did a prospective study on 80 consecutive cases of perforation peritonitis and compared MPI with the multiple organ failure score. The AUC of ROC for MPI was 0.972. MPI of 21 had a sensitivity of 100% and specificity of 79%. With MPI of 29 the sensitivity was 79%, and specificity was 96%. These results were comparable to the findings of our study.
Batra et al.[13] calculated MPI score in a cross-sectional study of 160 patients of perforation peritonitis to evaluate MPI scoring system in defining the prognosis of the patients and to be able to deliver better patient care and furnish efficient management. The cut-off from ROC curve was 26. Sensitivity and specificity of MPI in predicting mortality were calculated to be 100% and 65.54%, respectively. The rate of mortality was 5.7%. This was a pioneering study in India where MPI scoring system was applied specifically for patients of perforation peritonitis in a hospital in the rural area. The results of our study were comparable, and the increase in mortality with the increment of MPI scores deduced that MPI score proved to be a useful tool to predict the mortality in patients of peritonitis. However, the validity results of MPI in the present study was not comparable to Demmel et al.,[10] Ohmann et al.[15] and Delibegovic et al.,[16,17] despite similar AUC of ROC curves, which may be due to variations in the sample sizes and cut-off values.
In a prospective study of 108 cases of severe intraabdominal infections managed by open treatment, Demmel et al.[13] compared MPI and Acute Physiology and Chronic Health Evaluation II (APACHE II) scores. Statistical validation showed a sensitivity of 93% and a specificity of 16% for MPI. The Peritonitis study group[15] performed a multicentric study and compared APACHE II, MPI and peritonitis index altona scores in 271 cases of laparotomies for perforation peritonitis. The sensitivity and specificity of MPI were 60% and 80%, respectively. The AUC of ROC for a cut-off point of 26 was 0.79. We conclude that MPI scoring is a reliable predictor of death in perforation peritonitis patients and can be helpful in planning and evaluating future treatments with great ease. We would like to recommend its use in the prognostic evaluation of secondary peritonitis cases.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Bohnen J, Boulanger M, Meakins JL, McLean AP. Prognosis in generalized peritonitis. Relation to cause and risk factors. Arch Surg. 1983;118:285–90. doi: 10.1001/archsurg.1983.01390030017003. [DOI] [PubMed] [Google Scholar]
- 2.Farthmann EH, Schöffel U. Principles and limitations of operative management of intraabdominal infections. World J Surg. 1990;14:210–7. doi: 10.1007/BF01664875. [DOI] [PubMed] [Google Scholar]
- 3.Giessling U, Petersen S, Freitag M, Kleine-Kraneburg H, Ludwig K. Surgical management of severe peritonitis. Zentralbl Chir. 2002;127:594–7. doi: 10.1055/s-2002-32839. [DOI] [PubMed] [Google Scholar]
- 4.Knaus WA, Drapper EA, Wagner DP, Zimmerman JE. APACHE severity of disease classification system. Crit Care Med. 1985;13:818–29. [PubMed] [Google Scholar]
- 5.Rix TE, Bates T. Pre-operative risk scores for the prediction of outcome in elderly people who require emergency surgery. World J Emerg Surg. 2007;2:16. doi: 10.1186/1749-7922-2-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Billing A, Fröhlich D, Schildberg FW. Prediction of outcome using the Mannheim peritonitis index in 2003 patients. Peritonitis Study Group. Br J Surg. 1994;81:209–13. doi: 10.1002/bjs.1800810217. [DOI] [PubMed] [Google Scholar]
- 7.Koç M, Yoldas O, Kiliç YA, Göçmen E, Ertan T, Dizen H, et al. Comparison and validation of scoring systems in a cohort of patients treated for perforated peptic ulcer. Langenbecks Arch Surg. 2007;392:581–5. doi: 10.1007/s00423-007-0156-7. [DOI] [PubMed] [Google Scholar]
- 8.Lee FY, Leung KL, Lai BS, Ng SS, Dexter S, Lau WY. Predicting mortality and morbidity of patients operated on for perforated peptic ulcers. Arch Surg. 2001;136:90–4. doi: 10.1001/archsurg.136.1.90. [DOI] [PubMed] [Google Scholar]
- 9.Wacha H, Linder MM, Feldman U, Wesch G, Gundlach E, Steifensand RA. Mannheim peritonitis index-prediction of risk of death from peritonitis: Construction of a statistical and validation of an empirically based index. Theor Surg. 1987;1:169–77. [Google Scholar]
- 10.Demmel N, Muth G, Maag K, Osterholzer G. Prognostic scores in peritonitis: The Mannheim peritonitis index or APACHE II? Langenbecks Arch Chir. 1994;379:347–52. doi: 10.1007/BF00191581. [DOI] [PubMed] [Google Scholar]
- 11.Correia MM, Thuler LC, Velasco E, Vidal EM, Schanaider A. Prediction of death using the Mannheim peritonitis index in oncologic patients. Rev Bras Cancerologia. 2001;47:63–8. [Google Scholar]
- 12.Notash AY, Salimi J, Rahimian H, Fesharaki Ms, Abbasi A. Evaluation of Mannheim peritonitis index and multiple organ failure score in patients with peritonitis. Indian J Gastroenterol. 2005;24:197–200. [PubMed] [Google Scholar]
- 13.Batra P, Gupta D, Batra R, Kothari R, Deshmukh PR. Mannheim peritonitis index as an evaluative tool in predicting mortality in patients of perforation peritonitis. CIBTech J Surg. 2013;2:30–6. [Google Scholar]
- 14.Muralidhar VA, Madhu CP, Sudhir S, Srinivasarangam M. Efficacy of Mannheim peritonitis index (MPI) score in patients with secondary peritonitis. J Clin Diagn Res. 2014;8:NC01–3. doi: 10.7860/JCDR/2014/8609.5229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ohmann C, Wittmann DH, Wacha H. Prospective evaluation of prognostic scoring systems in peritonitis. Peritonitis Study Group. Eur J Surg. 1993;159:267–74. [PubMed] [Google Scholar]
- 16.Delibegović S, Nuhanovic A. Artificial neural network in prediction of the outcome of critically ill patients with perforative peritonitis. Acta Med Acad. 2008;37:106–12. [Google Scholar]
- 17.Delibegovic S, Markovic D, Hodzic S. APACHE II scoring system is superior in the prediction of the outcome in critically ill patients with perforative peritonitis. Med Arh. 2011;65:82–5. [PubMed] [Google Scholar]


