Abstract
Background:
Rural population in developing countries face water, sanitation, and hygiene-related health issues. To objectively highlight these issues, we studied the knowledge, attitude, and practices-related to drinking water and sanitation facilities among the rural population of Chennai, India.
Materials and Methods:
A cross-sectional study was designed involving individuals over 18 years of age living in Thandalam village, Chennai, India. Basic information about sociodemographic profile and existing drinking water and sanitation related knowledge, attitude, and practices was collected using a modified version of previously validated questionnaire and analyzed.
Results:
Forty-five percent of the participants were not following any methods of water treatment and among them half of the participants felt that water available to them was clean and did not require any additional treatment. Twenty-five percent of the participants surveyed did not have access to toilets inside their household.
Conclusion:
There is a need for intervention to educate individuals about drinking water treatment methods, sanitation, and hand washing practices.
Keywords: Attitude, drinking water, household members, hygiene, knowledge, practices, rural settings, sanitation
INTRODUCTION
The effects of poor sanitation seep into every aspect of life — health, nutrition, development, economy, dignity and empowerment.[1] With a little less than a year left to achieve the millennium development goals, 2.5 billion people are still devoid of improved sanitation facility.[2,3] The sanitation target 7C (target 7C: Halve, by 2015, the proportion of the population without sustainable access to safe drinking water and basic sanitation) to reach 75% of global coverage by 2015 from the present 63% is likely to be missed.[4] Globally, water and sanitation hygiene practice are responsible for 90% of diarrhea-related mortality, which is much higher than combined mortality from malaria and HIV/AIDS.[5,6,7] Although piped water facility in the rural regions almost doubled in past two decades, there are still 171 million people in rural regions who use surface water as the primary source of water.[8] Despite limited improvement in drinking water facilities in rural regions, the trend of the sanitation is still on a slow track, with 66% of the total rural population not having toilet facilities.[9]
Limited access to safe drinking water and poor sanitation can lead to under nutrition, water borne diseases, gastro-enteropathy along with diarrhea and dysentery. These problems are predominant among preschool children in the developing countries.[10,11] Although majority of water borne infections could be treated using antibiotics, the persisting burden of water borne infectious disease and increasing antibiotic resistance has created dual pressure on public health professionals, pharmaceutical industry and policy makers. Interventions for reducing the proportion of people with limited access to clean drinking water can lead to significant economic benefits,[11] which can help in achieving sustainable development.[12]
Although government agencies are providing the infrastructural support to improve sanitation condition in the developing countries, nevertheless there is a need for collateral personal hygiene and sanitary education to achieve improved outcomes.[2,3,13]
Many communicable diseases can be effectively managed by improving the sanitation, hygiene and water usage practices.[14,15,16,17,18] However, infrastructure development and policies alone are adequate to fill the existing gap of knowledge and practice of drinking water and sanitation. Nevertheless for effective reduction of effects from poor water and sanitation practices there is a need for understanding the present scenario and the affect of currently existing interventions in the rural settings. Hence, the objective of this study was to understand the knowledge, attitude, and practices related to drinking water and sanitation facilities among the rural population of Chennai, India.
MATERIALS AND METHODS
A cross-sectional study was designed during September 2013 in the rural setting, Chennai, India. Thandalam village, Chennai, India was selected as study site. 100 households were selected randomly and one member from each household was enrolled as participant. Efforts were made to contact head of the family and in case of his unavailability next immediate available resident was contacted for the interview. The participants had to be over 18 years of age and residing in rural areas. Participants were informed about the study objectives and those eligible and giving a written informed consent were enrolled in this study. Individuals who were mentally or physically challenged were excluded from participating in the study. The study protocol was approved by the Institutional Review Board (IRB) of the Foundation of Healthcare Technologies Society (FHTS), New Delhi (IRB#FHTS/006/2013). Confidentiality of all the participants was maintained by assigning unique code to each of the participants.
Data collection tools
A modified questionnaire was prepared from the existing validated tools. It consisted of following content.
Sociodemographic characteristics
Information was gathered about age (years), gender, educational status (no formal education, primary [1-5th grade], middle [6-8th grade], high school [9-10th grade], intermediate [11-12th] or equivalent, graduate or postgraduate), marital status (single/married/divorce or separated/widow), annual household income, type of family (joint, nuclear, broken, extended), number of family members, and occupation status (professional, semi-profession, clerical, shop owner, farmer, skilled worker, semi-skilled worker, unskilled, unemployed).[19]
Water facility and related issues
Information was gathered about the various sources of drinking water, individuals that were responsible for fetching water in household, periods of water shortage, distance of water source from household, water supply timings and water storage practices.
Water treatment and storage practices
Information was gathered about participant's attitudes toward water treatment practices. Water safety, effects of unsafe drinking water on health, and the practices that were adopted to make water safe to drink related topics were included.
Sanitation and related health issues
Information was gathered about toilet facilities, hand washing, waste disposal facilities and quantity of water being used in the house for various purposes (drinking, cooking, and ablutions, washing clothes, house cleaning, and miscellaneous). Additional information was sought regarding any diarrheal episode has occurred in the family in past 3 months.
Additional information was gathered through open-ended questions about challenges faced by the participants to fetch water, their satisfaction toward existing water and sanitation facilities.
Statistical analysis
Descriptive analysis was performed using univariate statistics to report means and standard deviations (SDs) for the continuous variables and frequency distribution for the categorical variables. All analysis was performed using SPSS version 16 (SPSS Inc., Chicago, USA).
RESULTS
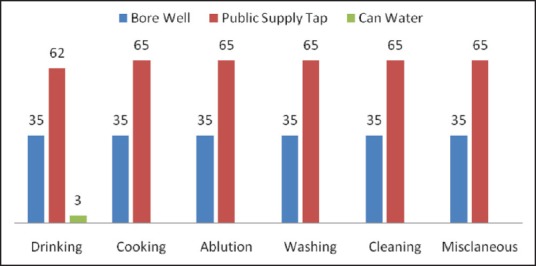
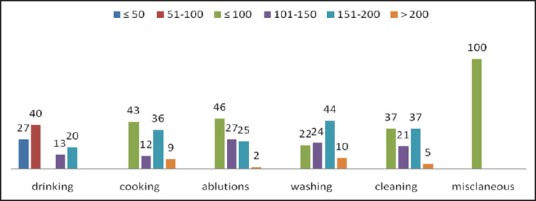
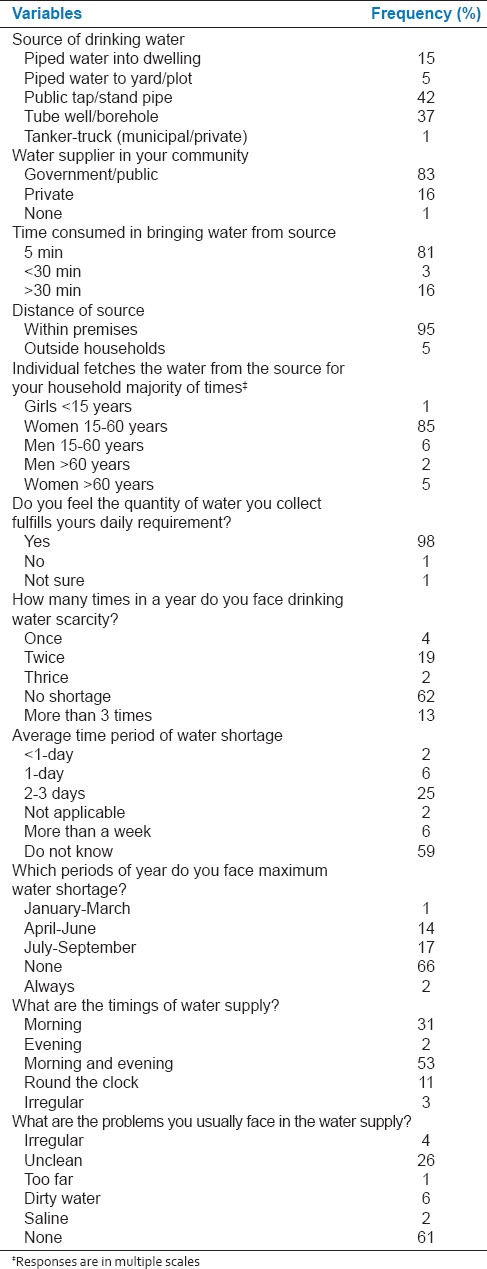
The average age of participants was 39 years (SD = 9.7), Majority of them were females (71%), 74% of them were married and 68% of them were living in nuclear families with average family size of 4 (SD = 2). Thirty-six percent of the participants had intermediate (12th grade) or above level of education. Half of the participants were unemployed with average annual household income of Indian National Rupee 89,175 (SD = 13,179) [Table 1]. The major sources of water procurement were public tap/stand pipe (42%) and tube well/borehole (37%). Sixteen percent of the participants were dependent on private water supply. Figure 1 presents the source of water utilized for different activities. Daily consumption of water for various activities varied considerably [Figure 2]. Ninety-five percent of the participant's fetched water within premises and majority of them (81%) required <5 min for fetching water from the water outlet. Majority of the participants (85%) fetching water were women in the age group of 15-60 years. Majority of the participants (98%) reported meeting the daily need of water quantity. Nineteen percent of the participants reported water shortage twice in a year with average shortage period of 2-3 days (25%). Seventeen percent of the participants indicated July-September as water shortage months while 14% suggested April-June. Half of the participants (53%) reported morning and evening supply of water with uncleanliness (26%) as one of the predominant problem [Table 2].
Table 1.
Sociodemographic characteristics of the participants
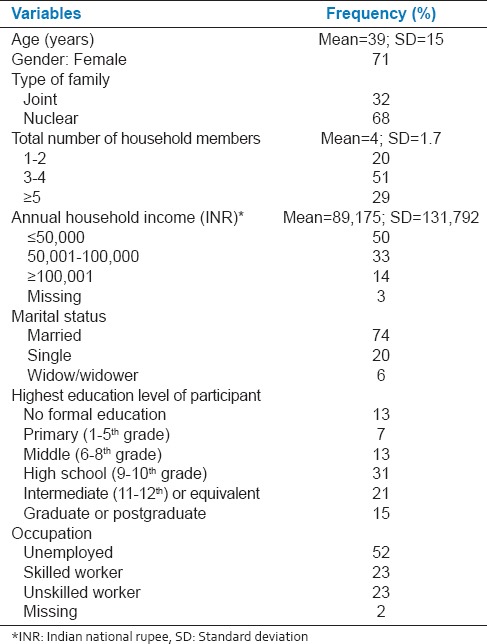
Figure 1.
Source of water used for different daily activities by individuals living in Thandalam village of Chennai, India
Figure 2.
Quantity of water (L) required for various activities by individuals living in Thandalam village of Chennai, India
Table 2.
Existing water facilities and associated issues in Thandalam village of Chennai, India as reported by the participants
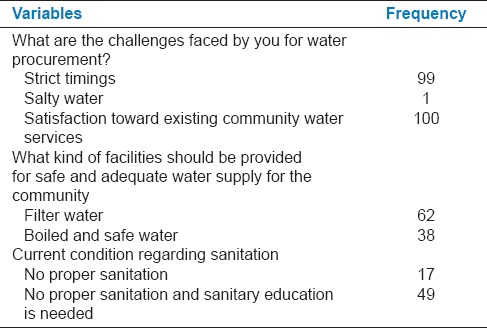
Majority of the participants (95%) perceived that the quality of water being used was safe, 71% of the participants agreed that quality of water can affect health status, 75% of them stored drinking water in wide mouth closed container and most of them cleaned water container daily (70%). Forty-five percent of the participants were not following any methods of water treatment and among them half of the participants felt that water was already clean and did not require any additional treatment. Half of the participants (51%) agreed that unsafe drinking water can cause general fever, whereas 22%, 18%, and 16% of the participants reported common cold, diarrhea, and vomiting respectively as potential consequence of drinking unsafe water. Water supply timing was the biggest challenge faced by the majority (94%) of the participants [Table 3]. Twenty-five percent of the participants did not have access to toilets inside the households. Seventy-nine percent of the participants had access to septic tank type of toilets. The majority of the participants agreed that hand should be washed before and after meals, while only 32% felt that hand should be washed after defecation. Results showed that 17% of the participants used plain water or water with ash to clean their hands while majority of the participants washed their hands to prevent infection (82%) or for hygiene maintenance (76%). Forty-seven percent of the participants reported that they discharge their waste in open drainage [Table 4]. Sixty-two percent of the participants desired for filter water and 38% of them desired for boiled and safe water facilities from the suppliers. Most of them had reported improper sanitary facilities and stressed on the need of sanitary education [Table 5].
Table 3.
Perceptions and practices-related to drinking water storage and safety among the study participants
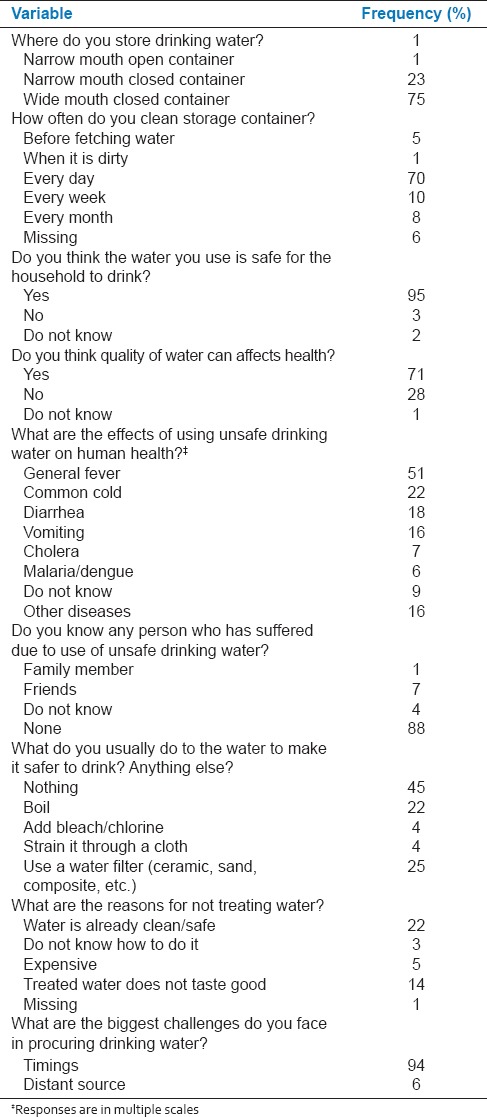
Table 4.
Existing sanitation facilities and related practices followed by the participants
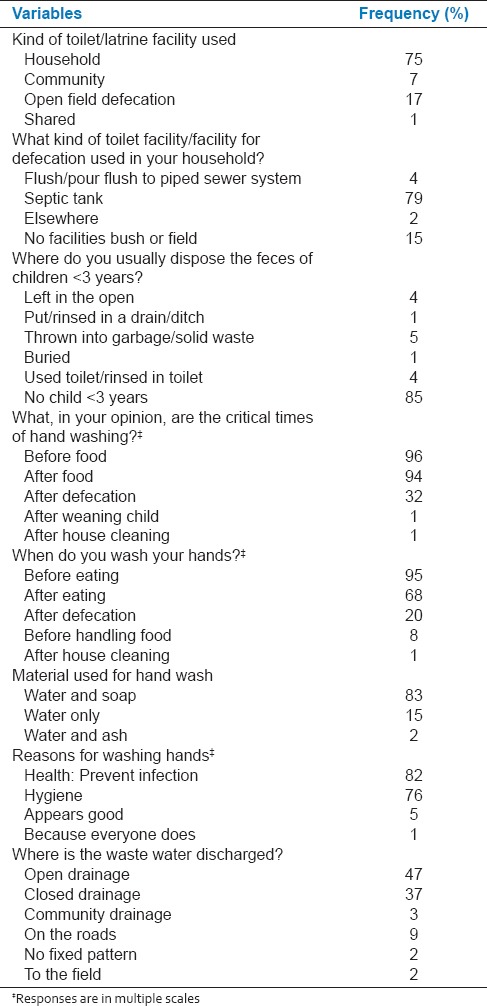
Table 5.
Challenges and suggestions for water, sanitation and hygiene
DISCUSSION
Water is one of the precious natural resource and is essential element of our life. Clean water and optimum sanitation facilities can prevent the occurrence of various infectious diseases and help in curbing the associated morbidity and mortality. The current study was conducted in rural setting of India to understand the existing water and sanitation facilities, perceptions and practices. Majority of the participants used public tap/stand pipe for water procurement and most of them had water supply inside their household premises. Females of age between 15 and 60 years were the primary responsible person for fetching water, which is consistent with previous report.[20] Most of the participants were consuming 151-200 L of water daily for cleaning and washing and ≤100 L of water for drinking, cooking and ablutions. Most of the participants reported that their daily needs of water quantity were met by the current supply.
About one in five of the participants reported water shortage twice in a year with average shortage period of 2-3 days. A previous study on water quality of groundwater resources showed that the water quality index of bore well, dug well and hand pump declined in postmonsoon season[21] which may account for water shortage. In addition, impurity in supplied water was one of the predominant problems, reported by one-fourth of the participants while the majority of the participants felt that the quality of water being used was safe. Majority of the participants were aware of the effects on health due to quality of water and half of them agreed that the consumption of unsafe drinking water may lead to one or more infectious diseases. Despite the knowledge 45% of the participants were not following any methods of water treatment and among them half of the participants felt that water is already clean, hence no further treatment was necessary.
One-fourth of the total participants were devoid of toilets facilities inside their households; leaving them with the options of using community toilets, open defecation or sharing the toilets with other households which in turn promotes the increase in incidence of water-borne disease. Although, the majority of the participants knew and reported hand washing before and after meals only one in three participants felt that hand should be washed after defecation. It was also observed that few of the participants used plain water for hand washing after defecation. This is again consistent with the previous report.[22] This kind of practice may give rise to diseases of the feco-oral route and increase the financial burden in terms of hospital admissions and associated medical expenses. School attendance of children would be affected as their role changes from studying to care provider for an elderly sick person in the family; in addition to children falling ill due to similar hand washing practices.
On assessing the need of water, sanitation, and hygiene; most of the participants desired for filter water and 38% of them desired for boiled and safe water facilities form the suppliers. Most of the participants stressed on the need of sanitary education. Nevertheless, there are some limitations associated with our study. First it included smaller sample size and the study design was cross-sectional. Further the study was limited to one geographical location; hence, the results of the study should not be generalized. However, our study does identify the need for intervention program to educate the population regarding sanitation, water treatment methods, and hand washing practices. There is also a need for developing cost effective water testing devices to record seasonal variations in water quality in rural areas.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We would like to thank all our study participants for giving their valuable time out of their busy schedules to participate in the study and provided valuable information.
REFERENCES
- 1.New Delhi: UNICEF; 2012. [Last accessed on 2014 Aug 25]. UNICEF. Sanitation and Hygiene Advocacy and Communication Strategy Framework 2012-2017. Available from: http://www.tinyurl.com/nr6ynxq . [Google Scholar]
- 2.Water Aid, Unilever Domestos, Water Supply & Sanitation Collaborative Council; 2013. [Last accessed on 2014 Aug 25]. Water Aid, Unilever Domestos, Water Supply & Sanitation Collaborative Council. We Can’t Wait: A Report on Sanitation and Hygiene for Women and Girls. Available from: http://www.tinyurl.com/n2o4txo . [Google Scholar]
- 3.Jenkins MW, Freeman MC, Routray P. Measuring the safety of excreta disposal behavior in India with the new Safe San Index: Reliability, validity and utility. Int J Environ Res Public Health. 2014;11:8319–46. doi: 10.3390/ijerph110808319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hulton G World Health Organization. Geneva: World Health Organization; 2012. [Last accessed on 2014 Aug 25]. Global costs and benefits of drinking-water supply and sanitation interventions to reach the MDG target and universal coverage. Available from: http://www.tinyurl.com/l4asj6z . [Google Scholar]
- 5.Geneva: UN Water; 2012. [Last accessed on 2014 Aug 25]. UN Water. Sanitation Drive to 2015 Planners’ Guide. Available from: http://www.tinyurl.com/msbtf8p . [Google Scholar]
- 6.Bethony J, Brooker S, Albonico M, Geiger SM, Loukas A, Diemert D, et al. Soil-transmitted helminth infections: Ascariasis, trichuriasis, and hookworm. Lancet. 2006;367:1521–32. doi: 10.1016/S0140-6736(06)68653-4. [DOI] [PubMed] [Google Scholar]
- 7.New York: United Nations; 2013. [Last accessed on 2013 Nov 2]. United Nations. The Millennium Development Goals Report 2013. Available from: http://www.tinyurl.com/njfqepm . [Google Scholar]
- 8.World Health Organization, UNICEF; 2013. [Last accessed on 2013 Nov 2]. World Health Organization, UNICEF. Progress on Sanitation and Drinking-Water-2013. Update: Joint Monitoring Programme for Water Supply and Sanitation. Available from: http://www.tinyurl.com/ozot7aq . [Google Scholar]
- 9.Geneva: World Health Organization; 2013. [Last accessed on 2013 Nov 2]. World Health Organization. World health statistics 2013: A wealth of information on global public health. Available from: http://www.who.int/gho . [Google Scholar]
- 10.Humphrey JH. Child undernutrition, tropical enteropathy, toilets, and handwashing. Lancet. 2009;374:1032–5. doi: 10.1016/S0140-6736(09)60950-8. [DOI] [PubMed] [Google Scholar]
- 11.Pruss-Ustun A, Bos R, Gore F, Bartram J. Geneva: World Health Organization; 2008. [Last accessed on 2013 Nov 2]. Safer water, better health: Costs, benefits and sustainability of interventions to protect and promote health. Available from: http://www.tinyurl.com/npyq5n3 . [Google Scholar]
- 12.Bartram J, Cairncross S. Hygiene, sanitation, and water: Forgotten foundations of health. PLoS Med. 2010;7:e1000367. doi: 10.1371/journal.pmed.1000367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mara D, Lane J, Scott B, Trouba D. Sanitation and health. PLoS Med. 2010;7:e1000363. doi: 10.1371/journal.pmed.1000363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Geneva: World Health Organization; 2013. [Last accessed on 2014 Aug 28]. World Health Organization. Water Quality and Health Strategy 2013-2020. Available from: http://www.tinyurl.com/q486xp5 . [Google Scholar]
- 15.Geneva: World Health Organization; 2011. [Last accessed on 2013 Nov 2]. World Health Organization. Cause-specific mortality: Regional estimates for 2008. Available from: http://www.tinyurl.com/7p2swfk . [Google Scholar]
- 16.Kolkata: National Institute of Cholera and Enteric Diseases (NICED); 2014. [Last accessed on 2015 May 19]. Department of Health Research. Surveillance: National and International Initiatives. Available from: http://www.dhr.gov.in/annual_report/2013-14/PDF/English%20pdf%20files/23.pdf . [Google Scholar]
- 17.Banerjee T, Shukla BN, Filgona J, Anupurba S, Sen MR. Trends of typhoid fever seropositivity over ten years in North India. Indian J Med Res. 2014;140:310–3. [PMC free article] [PubMed] [Google Scholar]
- 18.Van Minh H, Nguyen-Viet H. Economic aspects of sanitation in developing countries. Environ Health Insights. 2011;5:63–70. doi: 10.4137/EHI.S8199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sharma A, Gur R, Bhalla P. Kuppuswamy's socioeconomic scale: Updating income ranges for the year. Indian J Public Health. 2012;56:101–3. doi: 10.4103/0019-557X.96988. [DOI] [PubMed] [Google Scholar]
- 20.Nerkar SS, Tamhankar AJ, Johansson E, Lundborg CS. Improvement in health and empowerment of families as a result of watershed management in a tribal area in India. A qualitative study. BMC Int Health Hum Rights. 2013;13:42. doi: 10.1186/1472-698X-13-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rajankar PN, Gulhane SR, Tambekar DH, Ramteke DS, Wate SR. Water Quality Assessment of Groundwater Resources in Nagpur Region (India) Based on WQI. J Chem. 2009;6:905–8. [Google Scholar]
- 22.Ray SK, Zaman FA, Laskar NB. Hand washing practices in two communities of two states of Eastern India: An intervention study. Indian J Public Health. 2010;54:126–30. doi: 10.4103/0019-557X.75734. [DOI] [PubMed] [Google Scholar]


