Abstract
Background
Fertility counseling and treatment can help women achieve their desired family size, however, disparities exist in the utilization of this care.
Methods
This study examines the persistence of a racial disparity in visiting a doctor for help getting pregnant by estimating the direct effect of this association using data from the FUCHSIA Women’s Study, a population-based cohort study. This cohort included 1073 reproductive age women (22-45 years) with 28% reporting infertility. We fit log binomial models to quantify the magnitude of the racial difference in reported care seeking after adjustment for hypothesized mediators using inverse probability weighting.
Results
Compared with white women, black women were less likely to visit a doctor in the total population [adjusted risk ratio (aRR) = 0.57, 95% confidence interval (CI): 0.41, 0.80] and in the subgroup of women with infertility [aRR = 0.75, 95% CI: 0.56, 0.99]. In addition, black women waited twice as long on average before seeking help compared with white women.
Conclusions
There were notable racial differences in visiting a doctor for help getting pregnant in this study although reports of infertility were similar by race. These differences may be mitigated through improved communication about the range of counseling and treatment options available.
Infertility and impaired fecundity affect millions of women in the United States. Estimates of the prevalence of infertility range from 6%-15% among women of reproductive age.1, 2 The burden of infertility and impaired fecundity affects women across demographic groups and exists unnoticed among women not actively trying to get pregnant.3, 4 This inability to conceive or carry a baby to term affects the quality of life of women. Infertility, however, is not just a quality of life issue, the American Society for Reproductive Medicine, World Health Organization, and International Committee for Monitoring Assisted Reproductive Technology classify infertility as a disease of the reproductive system.5, 6 National organizations have been established to provide support for those suffering from infertility and education to the public at large.7 Recently, focus has been directed towards addressing the causes of infertility from a broader societal perspective.8 The Centers for Disease Control and Prevention developed a National Action Plan to address the detection, prevention, and management of infertility at the population level.9
In the most recent cycle of the National Survey for Family Growth, 12% of female participants, representing 7.4 million women in the US, reported ever using medical services for infertility. These services ranged from advice, to provision of medications, to in vitro fertilization (IVF).10 Counseling provides information to optimize chances of natural conception, as well as guidance about more involved procedures. For example, controlled ovarian hyperstimulation with injectable gonadotropins with timed intercourse or intrauterine insemination are often successful in younger women, but are also associated with a higher risk of multiple gestations.11, 12 Whereas IVF is more invasive and expensive, with single embryo transfer, this procedure has a higher ongoing pregnancy rate and lower risk of multiple gestations compared with other less invasive treatments.13, 14 This information is essential to making informed decisions about medical care for getting pregnant.
Healthy People 2020 describes health disparities as not only differences in a health-related outcome, but differences that systematically and adversely affect disadvantaged populations.15 The social construct of race which represents a combination of factors including, appearance, culture, and social factors has been used as the basis for discrimination and perpetuating disadvantage.16 In the US, black race is associated with a history of unequal treatment, exposure to racism, deprived neighborhoods, and lack of socioeconomic opportunity. These exposures have led to racial disparities in health and health related outcomes.17, 18 According to the National Survey for Family Growth, among married women, black women are more likely to report infertility compared with white women. Further, racial disparities exist in the utilization of infertility treatments with non-Hispanic white women most likely to receive treatment.1, 10 As fertility counseling and treatment become more common and more successful in helping women become pregnant, a new area for disparity has emerged.19
Gaps remain in understanding disparities in the accessibility to and utilization of infertility counseling and treatment. The preponderance of the literature is in clinic-based studies and only provides information on the subgroup of help-seeking women with infertility. Even among women who do seek medical help to become pregnant, studies have found that black women wait longer to seek care after difficulty becoming pregnant compared with white women.20, 21 Infertility treatment may be cost prohibitive for some women, however, even in states where there are mandates that insurance coverage include infertility treatment, disparities by race and education persist.22, 23
The primary objective of this paper is to assess the persistence of racial disparities after accounting for known mediating pathways of the association between race and seeking medical help for becoming pregnant. We also explore differences by race in the length of time women wait from when they first experience infertility to the time they visit a doctor for help becoming pregnant.
METHODS
We used data from the Furthering Understanding of Cancer Health and Survivorship in Adult (FUCHSIA) Women’s Study. The FUCHSIA Women’s Study is a population-based cohort study examining how cancer treatment during the reproductive years affects future fertility. It compares the reproductive experiences of female cancer survivors to a group of comparison women who never had cancer treatment. Comparison women were frequency matched on 5 year age ranges and Georgia region of residence to the cancer survivors. Analyses for this paper utilize comparison women only because women who have been treated for cancer may have different motivations and access to medical care for help becoming pregnant compared with the general population, even if they did not receive treatment believed to impair fertility. Women were eligible to participate if they were 22-45 years old at recruitment, had a working telephone, and spoke English. Women were recruited to participate in the study independent of their fertility status, which allows us to examine infertility service use in the overall population and characterize participants who did and did not seek help for becoming pregnant. Women consented to participate and completed the study interview by telephone. The study was approved by the Emory University and Georgia Department of Public Health Institutional Review Boards.
Defining race and racial disparities in health are challenging.24 In this study, the exposure was designated as self-reported black race compared with self-reported white race. We used self-reported race to represent the composite of factors that make up the experience of being black in the US to estimate disparities attributable to this complex measure. The outcome was whether or not women accessed care for help getting pregnant regardless of whether they used treatment or not. It was determined by the question “Have you ever visited a doctor or health professional for help becoming pregnant?” We also collected information on periods of possible impaired fertility through the question “Has there ever been a period of time during which you had unprotected sex with a male partner for 6 months or longer but you did not get pregnant? Only count periods of time when you had sex at least 3 times per month.” Participants who answered ‘yes’ to this question were classified as sub-fertile. Follow-up questions captured the total number of months of impaired fertility, age when it happened, whether the woman was actively trying to get pregnant at the time, if spontaneous conception occurred, and any recurrences. We used the age and total months of impaired fertility to define infertility. Women reporting a period of time lasting 12 months or longer between the ages of 20-34 years or a period of 6 months or longer at age 35 years or older when they had unprotected intercourse but did not get pregnant were classified as infertile. These determinations correspond to the American Society for Reproductive Medicine definition of infertility, although their definition also includes that unprotected intercourse must be appropriately timed.25
Interviewers collected information from women on their general health and reproductive experiences, as well as demographic and lifestyle characteristics. We asked women for their race, current level of education, total household income in the previous 12 months, and address at the time of the interview. We asked participants how many children they had given birth to and how many children they desired. To gauge women’s feelings about invasive infertility procedures, women were asked about their comfort with intrauterine insemination and IVF using a 5 point Likert type scale. Women also answered questions about diagnosis with reproductive conditions including polycystic ovary syndrome, fibroids, or endometriosis and sexually transmitted infections (STIs) including chlamydia, gonorrhea, or pelvic inflammatory disease.
Many of the participant characteristics collected in the interview were considered mediators of the association between race and visiting a doctor for help getting pregnant in our conceptual framework. Our main objective was to quantify the racial disparity that remains if the distribution of these sociodemographic factors were balanced between black and white women. To do this, we controlled for measured variables on all indirect paths between the social construct of race and visiting a doctor for help getting pregnant in a weighted analysis. Weights were created using the inverse probability of the participants’ self-reported race based in their education, income, place of residence, comfort with assisted reproductive technology (ART) and history of reproductive conditions, and STIs. The weights created a pseudo-population where hypothesized mediators were balanced between black and white women. For analyses conducted in the subgroup of women who reported infertility, age at infertility and whether or not a woman was actively trying to get pregnant were also included as mediators in the estimation of the weights. Weights were scaled to represent the observed sample size. Values in the tails of the distribution (at the 5st and 95th percentile) were truncated to reduce the influence of extremely large or small weights in the analysis.26
We fit generalized linear models with a log binomial distribution to estimate the total and direct effect of the social construct of race on visiting a doctor for help getting pregnant. To compare the results from our weighted analysis to traditional multivariable methods we fit a modified Poisson model with robust variances, because the log binomial model did not converge.27 Assuming that our conceptual framework depicts the true causal relationships, differences in the coefficients from the models with versus without adjustment for mediating variables represents the proportion of the total effect mediated by the specified paths.28
To address possible differences by race in the time waited before visiting a doctor for help getting pregnant, we fit Cox proportional hazard models to estimate hazard ratios for visiting a doctor among women with infertility. The start time in these models was defined as the age at which women reported their first infertile period and the event time was the age at first doctor’s visit. Women who did not visit a doctor were censored at age of hysterectomy, menopause, spontaneous conception, or interview. Survival models were adjusted for the same set of mediators as models in the main analysis using multivariable and weighted models. SAS 9.3 was used for all statistical analyses.
RESULTS
The FUCHSIA Women’s Study comparison group included 1,073 women. Of these women, 309 were black (29%), 712 were white (66%) and 52 reported another race (5%). Our analyses were restricted to women who reported black or white race. Characteristics of the sample by race are presented in Table 1. Median age at interview was 38 years for both black and white women. Black women in the study population had comparable education levels to white women, but lower household incomes. Most study participants resided in a large metropolitan area, with more white women reporting rural residence. The prevalence of STIs was higher among black women compared with white women (25% vs 5%) as well as the prevalence of fibroids (30% vs. 9%), while other reproductive conditions were more similarly distributed. Childlessness differed between the groups with 73% of black women and 84% of white women giving birth to at least one child at the time of the interview. Meeting reproductive goals also differed by race with over half of black women reporting they currently had fewer children than they desired compared with 39% of white women. The characteristics among the subgroup of women who experienced infertility were similar to the full sample (data not shown).
Table 1.
Demographic and Reproductive Characteristics of Participants in the FUCHSIA Women’s Study by Race
| Characteristic | Total women, no. n = 1,021 |
Black n = 309 |
White n = 712 |
P valuea |
|---|---|---|---|---|
| % | % | |||
| Age at interview (years) | ||||
| 22-29 | 64 | 7.1 | 5.9 | 0.74 |
| 30-39 | 552 | 53.1 | 54.5 | |
| 40-45 | 405 | 39.8 | 39.6 | |
| Education | ||||
| Less than high school/ high school grad | 50 | 6.5 | 4.2 | 0.06 |
| Some college or technical school | 238 | 24.3 | 22.9 | |
| College graduate | 381 | 31.7 | 39.8 | |
| Some graduate school/ graduate degree | 351 | 37.5 | 33.1 | |
| Missing | 1 | |||
| Income | ||||
| Less than or equal to $50k | 279 | 41.6 | 21.8 | <.01 |
| $50k - 100k | 386 | 40.0 | 37.8 | |
| $100k+ | 338 | 18.4 | 40.4 | |
| Missing | 4 | |||
| Place of residence | ||||
| Non-metro | 117 | 6.2 | 13.8 | <.01 |
| Small metro | 158 | 12.3 | 16.9 | |
| Large metro | 746 | 81.6 | 69.4 | |
| Married or cohabitating | ||||
| Yes | 886 | 73.5 | 92.6 | <0.01 |
| No | 135 | 26.5 | 7.4 | |
| Ever given birth | ||||
| Yes | 822 | 72.5 | 84.0 | <.01 |
| No | 199 | 27.5 | 16.0 | |
| Fewer children than desired at interviewb | ||||
| Yes | 431 | 51.2 | 38.8 | <.01 |
| No | 583 | 48.8 | 61.2 | |
| Missing | 7 | |||
| Comfortable with assisted reproductive technologyc |
||||
| Strongly agree | 101 | 6.9 | 11.3 | 0.09 |
| Agree | 229 | 20.0 | 23.8 | |
| Neither agree nor disagree | 113 | 11.5 | 11.0 | |
| Disagree | 289 | 32.1 | 27.0 | |
| Strongly disagree | 280 | 29.5 | 26.9 | |
| Missing | 9 | |||
| Polycystic ovary syndrome | ||||
| Yes | 80 | 5.5 | 8.9 | 0.07 |
| No | 937 | 94.5 | 91.1 | |
| Missing | 4 | |||
| Endometriosis | ||||
| Yes | 91 | 7.5 | 9.6 | 0.28 |
| No | 927 | 92.5 | 90.4 | |
| Missing | 3 | |||
| Fibroids | ||||
| Yes | 155 | 30.4 | 8.7 | <.01 |
| No | 861 | 69.6 | 91.3 | |
| Missing | 5 | |||
| Chlamydia | ||||
| Yes | 94 | 21.0 | 4.1 | <.01 |
| No | 927 | 79.0 | 95.9 | |
| Gonorrhea | ||||
| Yes | 27 | 5.5 | 1.4 | <.01 |
| No | 994 | 94.5 | 98.6 | |
| Pelvic inflammatory disease | ||||
| Yes | 25 | 4.9 | 1.4 | <.01 |
| No | 996 | 95.2 | 98.6 |
P-values were calculated using a chi square statistic.
Fewer children defined by subtracting the number of children a woman desired from the number of children she had at the time of the interview.
Based on the question: “I would be/would have been comfortable with the idea of using assisted reproductive technology, such as in vitro fertilization or artificial insemination, to help me get pregnant.”
Of the 978 women who answered the question about experiencing impaired fertility, 44% reported a sub-fertile period, with similar reporting by race (Table 2). When using the stricter definition of infertility, the percentage dropped to 30% for black women and 28% for white women. Among the infertile, 67% of black women and 76% of white women reported primary infertility, or infertility before ever giving birth. Although report of this more restrictive period of infertility was similar by race, there were large differences in who was actively trying to get pregnant among this group. Thirty-two percent of black women and 67% of white women reported they were trying to conceive at the time of infertility.
Table 2.
Proportion of Women in the FUCHSIA Women’s Study Reporting Subfertility and Infertilitya
| Characteristic | Total women, no. n = 978 |
Black n = 292 |
White n = 686 |
P valueb |
|---|---|---|---|---|
| % | % | |||
| Subfertilityc | ||||
| Yes | 432 | 45.6 | 43.6 | 0.57 |
| No | 546 | 54.5 | 56.4 | |
| Infertilityd | ||||
| Yes | 278 | 29.8 | 27.8 | 0.54 |
| No | 700 | 70.2 | 72.2 | |
| Actively tryinge | ||||
| Yes | 156 | 32.2 | 67.0 | <.01 |
| No | 122 | 67.8 | 33.0 |
Twenty-six white women and 17 black women had missing values for the question asking about impaired fertility.
P-values were calculated using a chi square statistic.
Subfertility: A period of time lasting at least 6 months when a women was having regular unprotected intercourse, but did not get pregnant.
Infertility: A period of time lasting at least 6 months at or after age 35 years or at least 12 months between the ages 20-34 years when a woman was having regular unprotected intercourse, but did not get pregnant.
Actively trying to get pregnant among those with infertility during the reported infertile period.
Estimates of the total effect of the social construct of race on visiting a doctor for help getting pregnant showed that black women were less likely to have a visit [risk ratio (RR) = 0.42, 95% confidence interval (CI): 0.28, 0.64] (Table 3). This association remained in the subset of women who experienced infertility [RR = 0.48, 95% CI: 0.32, 0.71]. Estimates of the direct effect in the full sample using the weighted model was RR = 0.57, 95% CI: 0.41, 0.80. Among the subgroup of women who reported infertility, the weighted RR was 0.75, 95% CI: 0.56, 0.99. In multivariable models including the full set of mediators, the results were similar. The difference in the coefficients from the unadjusted and adjusted models represents 35% of the total effect explained by mediating paths in the full sample and 61% in the subgroup of women with infertility.
Table 3.
Crude and Adjusted Risk Ratios of the Association Between Race and Visiting a Doctor for Help Getting Pregnant in the FUCHSIA Women’s Study
| Women visiting a doctor, no. |
Total women, no. |
Unadjusted | Adjusteda | Weightedb | ||||
|---|---|---|---|---|---|---|---|---|
| RR | 95% CI | RR | 95% CI | RR | 95% CI | |||
| All women | ||||||||
| White | 136 | 712 | 1.00 | reference | 1.00 | reference | 1.00 | reference |
| Black | 25 | 309 | 0.42 | 0.28, 0.64 | 0.54 | 0.35, 0.81 | 0.57 | 0.41, 0.80 |
| Infertile womenc | ||||||||
| White | 97 | 191 | 1.00 | reference | 1.00 | reference | 1.00 | reference |
| Black | 21 | 87 | 0.48 | 0.32, 0.71 | 0.76 | 0.52, 1.11 | 0.75 | 0.56, 0.99 |
Abbreviations: RR: risk ratio; 95% CI: 95% confidence interval
Adjusted: traditional adjustment for education (college graduate vs. no college degree), income (less than or equal to $50,000 vs. greater than $50,000), place of residence (non-metropolitan vs. metropolitan), comfort with ART (not comfortable with ART vs. comfortable with ART), fibroids, polycystic ovary syndrome, endometriosis, any sexually transmitted infections (chlamydia, gonorrhea, or pelvic inflammatory disease vs. no STIs), (models with the infertile group of women also included age at start of infertility and whether or not women were actively trying to get pregnant at the time they reported infertility); adjusted models use modified Poisson model because the log binomial model failed to converge
Weighted: data were weighted by the inverse probability of being exposed (black race); probabilities were calculated as a function of the mediators from the adjusted models
Infertile women: Women who reported a period of time lasting at least 6 months at or after age 35 years or at least 12 months between the ages 20-34 years when a woman was having regular unprotected intercourse, but did not get pregnant.
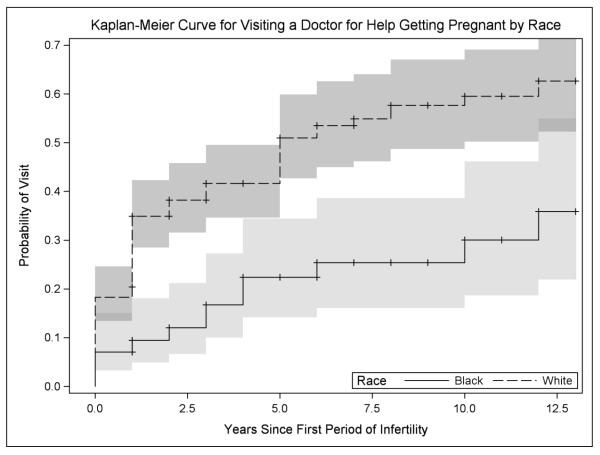
The distribution of ages at reported infertility cluster in the 20’s for both black and white women with an overall median age of 26 years [interquartile range (IQR): 23-30]. Age at visiting a doctor for help getting pregnant among women with infertility is shifted towards the 30’s with an overall median age of 29 years [IQR: 26-32]. Among women who visited a doctor after they reported infertility, white women waited a median of 1 year [IQR: 0-2] and black women waited 2 years [IQR: 0-4]. The unadjusted Kaplan-Meier plots show black women are less likely to have visited a doctor by the study interview (Figure 1). The maximum time women waited from first infertile period to visit was 12 years for both black and white women, however at this time 47% of white women and only 22% of black women had visited a doctor for help. The unadjusted hazard ratio (HR) for the association between race and visiting a doctor for help getting pregnant was 0.37, 95% CI: 0.22, 0.60 (Table 4). Adjusted models controlled for the same mediators as the main models restricted to infertile women. Using traditional adjustment, the estimated association moves towards the null [HR = 0.68, 95% CI: 0.39, 1.16], but the reduced likelihood of visiting a doctor remained. In the weighted model, the estimate was of a consistent magnitude as the fully adjusted model [HR = 0.70, 95% CI: 0.48, 1.03].
Figure 1.
Unadjusted Survival Curves for Visiting a Doctor for Help Getting Pregnant by Race in the FUCHSIA Women’s Study
Table 4.
Crude and Adjusted Hazard Ratios of the Association Between Race and Visiting a Doctor for Help Getting Pregnant in the FUCHSIA Women’s Study
| Women visiting a doctor, no. |
Total women, no. |
Unadjusted | Adjusteda | Weightedb | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| HR | 95% CI | HR | 95% CI | HR | 95% CI | ||||||
| Infertile womenc | |||||||||||
| White | 97 | 191 | 1.00 | reference | 1.00 | reference | 1.00 | reference | |||
| Black | 21 | 87 | 0.37 | 0.22 | 0.60 | 0.68 | 0.39 | 1.16 | 0.70 | 0.48 | 1.03 |
Abbreviations: HR: hazard ratio; 95% CI: 95% confidence interval
Adjusted: traditional adjustment for education (college graduate vs. no college degree), income (less than or equal to $50,000 vs. greater than $50,000), place of residence (non-metropolitan vs. metropolitan), comfort with ART (not comfortable with ART vs. comfortable with ART), fibroids, polycystic ovary syndrome, endometriosis, any sexually transmitted infections (chlamydia, gonorrhea, or pelvic inflammatory disease vs. no STIs), age at start of infertility, and whether or not women were actively trying to get pregnant at the time they reported infertility
Weighted: data were weighted by the inverse probability of being exposed (black race); probabilities were calculated as a function of the mediators from the adjusted models
Infertile women: Women who reported a period of time lasting at least 6 months at or after age 35 years or at least 12 months between the ages 20-34 years when a woman was having regular unprotected intercourse, but did not get pregnant.
COMMENTS
There were substantial racial differences in visiting a doctor for help getting pregnant in this study even though reports of impaired fertility were similar across race groups. To examine racial disparities in this paper, we used black race as the exposure in our analyses, recognizing that race is an amalgam of many different components. We were focused on aspects of the experience of black race in the context of the US as a result of cultural beliefs, experiences with discrimination, poor access to healthcare and economic opportunity among other factors. Our goal was to estimate the racial disparity that remained after accounting for a set of identified mediating paths from the social construct of race to visiting a doctor for help getting pregnant. We controlled for hypothesized mediators of this association, including sociocultural factors such as comfort with using assisted reproductive technologies, which other studies report differ by race.21, 29
In the main analysis, we included all women regardless of their infertility status to get a picture of the overall disparity in infertility service use. In our study, 9% of women who reported visiting a doctor for help getting pregnant never reported experiencing infertility. We addressed those most likely to need medical help for getting pregnant in the analyses restricted to infertile women. In mediator-adjusted models, hypothesized intermediate pathways were only able to partially explain the difference by race in visiting a doctor for help getting pregnant. Adjusted estimates from the survival analysis were consistent and showed that not only do black women visit the doctor for help getting pregnant less often than white women, they also wait longer after experiencing infertility. The fact that racial disparities persist despite control for mediating paths suggests that additional components that contribute to the social construct of race are influencing this association.
Sociocultural factors that were unmeasured in our study may explain some of the racial disparity we found. In our study we controlled for discomfort with ART, which only partially captures the stigmatization that may surround infertility for some women. In a fertility clinic-based study, compared with white women, black women were more likely to report that they were concerned about social stigmatization and disappointing a spouse because of their infertility.29 Furthermore, black women were more likely to report concern about friends and family finding out about treatment and to self-refer for care, suggesting a lack of support for care seeking for infertility in their social network. While black women were more likely to self-refer for fertility care compared with white women in this clinic-based study, we did not see this difference in our study. The remaining racial disparity we observed could also be the result of unmeasured confounding. We did not hypothesize any factors in our conceptual framework that would cause race and visiting a doctor for help getting pregnant. All of the covariates considered were mediators of this association. It is possible that there were factors that were not identified that confound the association between some of the mediators considered and the outcome, which could be distorting the estimate of disparities we found.
There are some data to support demographic differences in pregnancy planning. In a study of low income women recruited from a reproductive health clinic, they found that many women had unclear pregnancy intentions and so were not actively trying to get pregnant or using contraception.30 Another study found that black women were more likely to report an infertile period without the intent of getting pregnant.4 In our study, black women were less likely to be married or report they were trying to get pregnant during an infertile period compared with white women. However, women who are not married or cohabitating may still want to have a child and women not actively trying may want children in the future. The broad definition of infertility we used enabled us to capture potential fertility problems in all women. While every woman classified as having infertility in our study does not represent unmet need (e.g., women who do not desire children or have completed their family size) and some may be the result of mistimed intercourse, it is important to identify all women who are at possible risk of needing medical care for infertility. Regardless of women’s desire for children, infertility could represent an underlying reproductive condition or sexually transmitted infection that could be alleviated or treated with medical care.
Since fertility as well as the potential success of infertility treatments decline with age, there is also a benefit to discussing infertility treatment options with younger women.31, 32 For example, with IVF, the success rate of fresh non-donor cycles has been reported to be 40% in women 35 years and younger and only 1% in women 44 years and older.31 Despite our broad inclusion criteria, models restricting to women who reported primary infertility and wanting to have at least one child still showed a racial disparity.
The FUCHSIA Women’s Study was well suited to examine disparities by race. Women who participated in our study reflect the demographic composition of Georgia women of reproductive age (20-44 years), which is 34% black.33 Therefore, black women, a traditionally underrepresented group, had good representation in this study. Categories of education, place of residence, and household income were also well represented. In addition, women were recruited to participate in the study independently of their fertility status. This is in contrast to clinic-based studies that can only describe disparities among women who visit a fertility clinic for help getting pregnant, giving our study the advantage of being able to compare women who did and did not visit a doctor for help getting pregnant.
We recruited women using a purchased marketing list which may have lacked information on some women we wanted to participate in our study. This may have been a source of selection bias, but comparison women were similar to cancer survivors on many factors including race. Another potential limitation is that the data are restricted to self-reported information on fertility discussions with healthcare providers without verification of these visits with medical records. However, we expect women are able to remember a self-initiated visit to the doctor for help getting pregnant and found in our pilot studies that women are able to consistently report information about their fertility and infertility treatments received.34
Our study showed that even with control for an extensive list of hypothesized mediators a black/white racial disparity persisted. It is possible that stigma around infertility, which was unmeasured in our study, may be contributing to this disparity by limiting the sources of informal information and advice black women have access to in their social network. Better targeting of online resources, which have been suggested to be a preferred method of receiving information on stigmatized illnesses, could improve access to information on infertility and treatment.35 Accessing information online is associated with women feeling more comfortable discussing infertility issues with their healthcare provider.36 Initiation of conversations about available counseling and treatment options by a primary healthcare provider could also improve the exchange of information. This may decrease feelings of discomfort in visiting a specialist or using ART. Further, additional targeted outreach by organizations already in existence to fight stigma and improve knowledge about fertility problems, as well as support those suffering from infertility could be beneficial.7 Provision of information on the wide range of counseling and treatment options from different sources may decrease discomfort with infertility services, in turn reducing the disparity in their use, and help a greater number of women meet their reproductive goals.
Acknowledgements
Funding for this research was provided by The Eunice Kennedy Shriver National Institute of Child Health and Human Development Grant 1R01HD066059 and Reproductive, Perinatal, & Pediatric Training Grant T32HD052460, and the Health Resources and Service Administration Training Grant T03MC07651-06. The authors would like to thank Amy Fothergill for all data inquiries and support on the manuscript.
References
- 1.Chandra Anjani CCE, Hervey Stephen Elizabeth. Infertility and Impaired Fecundity in the United States, 1982–2010: Data From the National Survey of Family Growth. National Center for Health Statistics; Hyattsville, MD: [cited 2013]. 2013. Available from: http://www.cdc.gov/nchs/data/nhsr/nhsr067.pdf. [Google Scholar]
- 2.Thoma ME, McLain AC, Louis JF, King RB, Trumble AC, Sundaram R, et al. Prevalence of infertility in the United States as estimated by the current duration approach and a traditional constructed approach. Fertil Steril. 2013;99:1324–1331. e1321. doi: 10.1016/j.fertnstert.2012.11.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chandra A, Martinez GM, Mosher WD, Abma JC, Jones J. Fertility, family planning, and reproductive health of U.S. women: data from the 2002 National Survey of Family Growth. Vital Health Stat 23. 2005:1–160. [PubMed] [Google Scholar]
- 4.Greil AL, McQuillan J, Johnson K, Slauson-Blevins K, Shreffler KM. The hidden infertile: infertile women without pregnancy intent in the United States. Fertil Steril. 2010;93:2080–2083. doi: 10.1016/j.fertnstert.2009.08.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zegers-Hochschild F, Adamson GD, de Mouzon J, Ishihara O, Mansour R, Nygren K, et al. International Committee for Monitoring Assisted Reproductive Technology (ICMART) and the World Health Organization (WHO) revised glossary of ART terminology, 2009. Fertil Steril. 2009;92:1520–1524. doi: 10.1016/j.fertnstert.2009.09.009. [DOI] [PubMed] [Google Scholar]
- 6.American Society of Reproductive Medicine: Defining Infertility reproductivefacts.org. 2014 Available from: http://www.asrm.org/FACTSHEET_Defining_Infertility/
- 7.RESOLVE: The National Infertility Association [cited 2015 January 11];2015 Available from: http://www.resolve.org/
- 8.Farland LV, Missmer SA, Rich-Edwards J, Chavarro JE, Barbieri RL, Grodstein F. Use of fertility treatment modalities in a large United States cohort of professional women. Fertil Steril. 2014;101:1705–1710. doi: 10.1016/j.fertnstert.2014.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.National Public Health Action Plan for the Dectection, Prevention, and Management of Infertility. Centers for Disease Control and Prevention, Prevention CfDCa; Atlanta, GA: Jun, 2014. 2014. [Google Scholar]
- 10.Chandra A, Copen CE, Stephen EH. Infertility service use in the United States: data from the National Survey of Family Growth, 1982-2010. Natl Health Stat Report. 2014:1–21. [PubMed] [Google Scholar]
- 11.Valbuena D, Simon C, Romero JL, Remohi J, Pellicer A. Factors responsible for multiple pregnancies after ovarian stimulation and intrauterine insemination with gonadotropins. J Assist Reprod Genet. 1996;13:663–668. doi: 10.1007/BF02069646. [DOI] [PubMed] [Google Scholar]
- 12.Luke B, Brown MB, Morbeck DE, Hudson SB, Coddington CC, 3rd, Stern JE. Factors associated with ovarian hyperstimulation syndrome (OHSS) and its effect on assisted reproductive technology (ART) treatment and outcome. Fertil Steril. 2010;94:1399–1404. doi: 10.1016/j.fertnstert.2009.05.092. [DOI] [PubMed] [Google Scholar]
- 13.Kulkarni AD, Jamieson DJ, Jones HW, Jr., Kissin DM, Gallo MF, Macaluso M, et al. Fertility treatments and multiple births in the United States. N Engl J Med. 2013;369:2218–2225. doi: 10.1056/NEJMoa1301467. [DOI] [PubMed] [Google Scholar]
- 14.Kresowik JD, Stegmann BJ, Sparks AE, Ryan GL, van Voorhis BJ. Five-years of a mandatory single-embryo transfer (mSET) policy dramatically reduces twinning rate without lowering pregnancy rates. Fertil Steril. 2011;96:1367–1369. doi: 10.1016/j.fertnstert.2011.09.007. [DOI] [PubMed] [Google Scholar]
- 15.Healthy People 2020 . US Department of Health and Human Services. Office of Disease Prevention and Health Promotion; [cited 2013 March 5]. 2010. Available from: http://www.healthypeople.gov/2020/about/disparitiesAbout.aspx. [Google Scholar]
- 16.Lin SS, Kelsey JL. Use of race and ethnicity in epidemiologic research: concepts, methodological issues, and suggestions for research. Epidemiol Rev. 2000;22:187–202. doi: 10.1093/oxfordjournals.epirev.a018032. [DOI] [PubMed] [Google Scholar]
- 17.Kaufman JS, Cooper RS, McGee DL. Socioeconomic status and health in blacks and whites: the problem of residual confounding and the resiliency of race. Epidemiology. 1997;8:621–628. [PubMed] [Google Scholar]
- 18.Krieger N. Does racism harm health? Did child abuse exist before 1962? On explicit questions, critical science, and current controversies: an ecosocial perspective. Am J Public Health. 2008;98:S20–25. doi: 10.2105/ajph.98.supplement_1.s20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Seifer DB, Zackula R, Grainger DA. Trends of racial disparities in assisted reproductive technology outcomes in black women compared with white women: Society for Assisted Reproductive Technology 1999 and 2000 vs. 2004-2006. Fertil Steril. 2010;93:626–635. doi: 10.1016/j.fertnstert.2009.02.084. [DOI] [PubMed] [Google Scholar]
- 20.Seifer DB, Frazier LM, Grainger DA. Disparity in assisted reproductive technologies outcomes in black women compared with white women. Fertil Steril. 2008;90:1701–1710. doi: 10.1016/j.fertnstert.2007.08.024. [DOI] [PubMed] [Google Scholar]
- 21.Jain T. Socioeconomic and racial disparities among infertility patients seeking care. Fertil Steril. 2006;85:876–881. doi: 10.1016/j.fertnstert.2005.07.1338. [DOI] [PubMed] [Google Scholar]
- 22.Bitler M, Schmidt L. Health disparities and infertility: impacts of state-level insurance mandates. Fertil Steril. 2006;85:858–865. doi: 10.1016/j.fertnstert.2005.11.038. [DOI] [PubMed] [Google Scholar]
- 23.Jain T, Hornstein MD. Disparities in access to infertility services in a state with mandated insurance coverage. Fertil Steril. 2005;84:221–223. doi: 10.1016/j.fertnstert.2005.01.118. [DOI] [PubMed] [Google Scholar]
- 24.Kaufman JS, Cooper RS. Commentary: considerations for use of racial/ethnic classification in etiologic research. Am J Epidemiol. 2001;154:291–298. doi: 10.1093/aje/154.4.291. [DOI] [PubMed] [Google Scholar]
- 25.Definitions of infertility and recurrent pregnancy loss: a committee opinion. Fertil Steril. 2013;99:63. doi: 10.1016/j.fertnstert.2012.09.023. [DOI] [PubMed] [Google Scholar]
- 26.Cole SR, Hernan MA. Constructing inverse probability weights for marginal structural models. Am J Epidemiol. 2008;168:656–664. doi: 10.1093/aje/kwn164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Spiegelman D, Hertzmark E. Easy SAS calculations for risk or prevalence ratios and differences. Am J Epidemiol. 2005;162:199–200. doi: 10.1093/aje/kwi188. [DOI] [PubMed] [Google Scholar]
- 28.VanderWeele TJ, Robinson WR. On the causal interpretation of race in regressions adjusting for confounding and mediating variables. Epidemiology. 2014;25:473–484. doi: 10.1097/EDE.0000000000000105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Missmer SA, Seifer DB, Jain T. Cultural factors contributing to health care disparities among patients with infertility in Midwestern United States. Fertil Steril. 2011;95:1943–1949. doi: 10.1016/j.fertnstert.2011.02.039. [DOI] [PubMed] [Google Scholar]
- 30.Borrero S, Nikolajski C, Steinberg JR, Freedman L, Akers AY, Ibrahim S, et al. “It just happens”: a qualitative study exploring low-income women’s perspectives on pregnancy intention and planning. Contraception. 2015;91:150–156. doi: 10.1016/j.contraception.2014.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Centers for Disease Control and Prevention ASfRM, Society for Assisted Reproductive Technology . 2012 Assisted Reproductive Technology Fertility Clinic Success Rates Report. Atlanta, GA: 2014. [Google Scholar]
- 32.Benzies K, Tough S, Tofflemire K, Frick C, Faber A, Newburn-Cook C. Factors influencing women’s decisions about timing of motherhood. J Obstet Gynecol Neonatal Nurs. 2006;35:625–633. doi: 10.1111/j.1552-6909.2006.00079.x. [DOI] [PubMed] [Google Scholar]
- 33.2010 Census Summary File for Georgia [cited 2015 February 11];US Census. 2010 Available from: http://factfinder.census.gov/faces/tableservices/jsf/pages/productview.xhtml?pid=DEC_10_SF1_P12B&prodType=table.
- 34.Chin HB, Johnson CY, Kim KH, Knight JH, Mertens AC, Mink PJ, et al. Piloting a computer assisted telephone interview: the FUCHSIA Women inverted question marks Study. BMC Womens Health. 2014;14:149. doi: 10.1186/s12905-014-0149-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Berger M, Wagner TH, Baker LC. Internet use and stigmatized illness. Soc Sci Med. 2005;61:1821–1827. doi: 10.1016/j.socscimed.2005.03.025. [DOI] [PubMed] [Google Scholar]
- 36.Kahlor L, Mackert M. Perceptions of infertility information and support sources among female patients who access the Internet. Fertil Steril. 2009;91:83–90. doi: 10.1016/j.fertnstert.2007.11.005. [DOI] [PubMed] [Google Scholar]