Abstract
Background
A growing segment of the population—adults aged ≥65 years—is more susceptible than younger adults to certain enteric (including foodborne) infections and experience more severe disease.
Materials and Methods
Using data on laboratory-confirmed infections from the Foodborne Diseases Active Surveillance Network (FoodNet), we describe trends in the incidence of Campylobacter spp., Escherichia coli O157, Listeria monocytogenes, and nontyphoidal Salmonella infections in adults aged ≥65 years over time and by age group and sex. We used data from FoodNet and other sources to estimate the total number of illnesses, hospitalizations, and deaths in the United States caused by these infections each year using a statistical model to adjust for underdiagnosis (taking into account medical care-seeking, stool sample submission, laboratory practices, and test sensitivity).
Results
From 1996 to 2012, 4 pathogens caused 21,405 laboratory-confirmed infections among older adults residing in the FoodNet surveillance area; 49.3% were hospitalized, and 2.6% died. The average annual rate of infection was highest for Salmonella (12.8/100,000) and Campylobacter (12.1/100,000). Salmonella and Listeria led as causes of death. Among older adults, rates of laboratory-confirmed infection and the percentage of patients who were hospitalized and who died generally increased with age. A notable exception was the rate of Campylobacter infections, which decreased with increasing age. Adjusting for underdiagnosis, we estimated that these pathogens caused about 226,000 illnesses (~600/100,000) annually among U.S. adults aged ≥65 years, resulting in ~9700 hospitalizations and ~500 deaths.
Conclusion
Campylobacter, E. coli O157, Listeria, and Salmonella are major contributors to illness in older adults, highlighting the value of effective and targeted intervention.
Keywords: Campylobacter, E. coli O157, Listeria, Salmonella, elderly
INTRODUCTION
Adults aged ≥65 years are more susceptible than younger adults to certain enteric (including foodborne) infections such as listeriosis and Campylobacter and Salmonella bacteremia (Lund and O'Brien, 2011; Crim et al., 2014). Older adults are also more likely to die of enteric infections (Barton Behravesh et al., 2011). Several age-related factors may contribute to their increased susceptibility and disease severity, including weakening of the immune system, changes to the gastrointestinal tract, higher prevalence of other conditions, and more frequent use of antacids and immunosuppressants (Smith, 1998; Lund and O'Brien, 2011). Although laboratory-confirmed infections are a substantial health burden, diagnosed and reported illnesses represent but a fraction of total illnesses (Scallan et al., 2011).
Reducing the incidence of foodborne disease in older adults is a pressing public health challenge, especially because older adults are a rapidly growing segment of the population. The percentage of the U.S. population ≥65 years is expected to increase from 13% in 2010 to 19% by 2030 (U.S. Census Bureau, 2010). To better inform public policy and effectively target interventions, we need to know more about the incidence of and trends in infection from pathogens transmitted commonly through food. The aim of this study was to describe trends in the incidence of laboratory-confirmed infections caused Campylobacter, Escherichia coli O157, Listeria monocytogenes, and nontyphoidal Salmonella in adults aged ≥65 years and to estimate the total number of illnesses, hospitalizations, and deaths annually (both diagnosed and undiagnosed).
MATERIALS AND METHODS
Incidence of Laboratory-Confirmed Infections
We describe the incidence of laboratory-confirmed infections using data obtained from the Foodborne Diseases Active Surveillance Network (FoodNet), a collaborative program of the Centers for Disease Control and Prevention, 10 state health departments, the U.S. Department of Agriculture’s Food Safety and Inspection Service, and the U.S. Food and Drug Administration. FoodNet conducts active, population-based surveillance for laboratory-confirmed illnesses caused by pathogens transmitted commonly through food, including Campylobacter, E. coli O157, Listeria, and nontyphoidal Salmonella. When established in 1996, the FoodNet surveillance area included Minnesota, Oregon, and selected counties in California, Connecticut, and Georgia. During 1997–2004, the surveillance area expanded to 10 states (Connecticut, Georgia, Maryland, Minnesota, New Mexico, Oregon, and Tennessee, and select counties in California, Colorado and New York) and has been stable since then. In 2012, the FoodNet surveillance area accounted for 15% of the U.S. population (~48 million people).
FoodNet defines “case” as isolation of a pathogen by culture from a clinical specimen obtained from a resident of the surveillance area. FoodNet routinely contacts and audits ~650 clinical laboratories serving the surveillance area to learn about laboratory-confirmed infections. For Listeria, only invasive cases, defined as isolation of the pathogen from a normally sterile site (e.g., blood, cerebrospinal fluid) were counted. We considered nontyphoidal Salmonella (hereafter, Salmonella) to include all serotypes other than Typhi. For each patient, we sought information on age, sex, date of specimen collection, specimen source, hospitalization, outcome (alive or dead), and, for infections during 2004–2012, whether the illness was part of a recognized outbreak. We defined hospitalization as admission within 7 days of specimen collection date. Patient outcome was determined by interview or medical chart review and was recorded 7 days after specimen collection or at hospital discharge, whichever was later.
Data Analysis
We identified cases of infection during 1996–2012 in adults aged ≥65 years. We assumed patients with an unknown outcome were alive (Manikonda et al., 2012). Incidence rates per 100,000 were calculated using U.S. census population estimates for the corresponding years. When examining changes in incidence over time, we used a negative binomial regression model to account for the changing surveillance area and site-to-site variation in incidence (Henao et al., 2010). We compared incidence rates and percentage hospitalized/died among adults ≥65 years with children <5 years and people aged 5–64 years. Analyses were conducted using SAS version 9.3 (SAS Institute, Cary, NC).
Estimates of Annual Illness, Hospitalizations, and Deaths
For an illness to be diagnosed, someone must seek medical care and submit a stool sample, and the clinical laboratory must confirm the cause. If these steps do not occur, the cause will not be laboratory confirmed (underdiagnosis). Therefore, to estimate total illnesses in adults aged ≥65 years, we used a statistical model that scaled counts of laboratory-confirmed illnesses up to an estimated number of total illnesses, adjusting for underdiagnosis. Because FoodNet conducts active surveillance, we assumed that all laboratory-confirmed illnesses were reported. A similar model has estimated illnesses in the general population (Scallan et al., 2011) and among children aged <5 years (Scallan et al., 2012). For comparability with these estimates, we used FoodNet data from 2005 to 2008, basing our estimates on the 2006 U.S. population. Because FoodNet is limited to 10 states, we estimated laboratory-confirmed illnesses by applying pathogen-specific incidence rates among adults aged ≥65 years from FoodNet to the 2006 U.S. population estimate for adults ≥65 years (37.2 million people).
To adjust for underdiagnosis for Campylobacter, E. coli O157, and Salmonella, we estimated how often adults aged ≥65 years with a diarrheal illness sought medical care and submitted stool samples. We used data from the surveys of the general FoodNet population in 2000–2001, 2002–2003 (Jones et al., 2007), and 2006–2007 (CDC, 2012), where diarrheal illness was defined as an illness with ≥3 loose stools in 24 h and a duration of >1 day or resulting in restricted daily activities. People with more severe diarrheal illness are likely to seek medical care (Scallan et al., 2005a), so we adjusted separately for medical care-seeking and stool sample submission among people with mild or severe illness. For E. coli O157, ”severe” was the percentage of laboratory-confirmed case–patients ≥65 years enrolled in FoodNet case-control studies who reported bloody diarrhea (Kassenborg et al., 2004; Voetsch et al., 2007) (Supplementary Appendix Table A1; Supplementary Data are available online at www.liebertpub.com/fpd). For Campylobacter and Salmonella, the percentage of laboratory-confirmed case–patients aged ≥65 years enrolled in FoodNet case-control studies who reported bloody diarrhea (15% and 22%, respectively) (Friedman et al., 2004; Hennessy et al., 2004; Kimura et al., 2004; Mermin et al., 2004; Marcus et al., 2007) was lower than that reported among all ages (45% and 45%, respectively) (Scallan et al., 2011) despite higher hospitalization rates among older adults (Table 1). Therefore, we concluded the percentage of older adults categorized “severe” with a laboratory-confirmed Campylobacter and Salmonella infection tracked with the general population (Supplementary Appendix Table A1). For Listeria, because only invasive illnesses were counted, we assumed high rates of medical care-seeking (90%) and specimen submission (80%), as done for similar analyses (Scallan et al., 2011). We adjusted for laboratory testing practices and test sensitivity using FoodNet surveys and other sources (Supplementary Appendix Table A1).
Table 1.
Average Annual Rate of Laboratory-Confirmed Infections, Hospitalizations, and Deaths by Pathogen, 1996–2012a
| Average Annual Rate of Infection, per 100000 population |
Hospitalized, % | Died, % | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Age Group, yearsa | |||||||||
| Pathogen | <5 | 5–64 | ≥65 | <5 | 5–64 | ≥65 | <5 | 5–64 | ≥65 |
| Salmonella | 64.7 | 11.2 | 12.8 | 22.0 | 25.2 | 54.5 | 0.1 | 0.3 | 2.4 |
| Campylobacter | 29.2 | 14.3 | 12.1 | 9.3 | 13.6 | 35.8 | 0.04 | 0.08 | 0.5 |
| Listeria | 0.5 | 0.1 | 1.4 | 98.3 | 91.3 | 95.4 | 5.4 | 11.1 | 21.9 |
| E. coli O157 | 5.5 | 1.2 | 1.1 | 33.5 | 39.8 | 69.4 | 0.7 | 0.1 | 4.2 |
| Total | 99.9 | 26.9 | 27.4 | 19.6 | 20.5 | 49.3 | 0.13 | 0.22 | 2.6 |
Data are from the Foodborne Diseases Active Surveillance Network (FoodNet).
To estimate total hospitalizations and deaths, we determined the pathogen-specific percentage of adults aged ≥65 years with a laboratory-confirmed illness who were hospitalized and died. Then we applied these percentages to the estimated number of laboratory-confirmed illnesses in the United States. Some people with undiagnosed illnesses would have been hospitalized and died. For this reason, we doubled the number of hospitalizations and deaths to account for underdiagnosis, similar to previous analyses (Scallan et al., 2011).
Uncertainty Analysis
We used probability distributions to describe a range of plausible values for model inputs and described the uncertainty in our estimates by generating a point estimate and upper and lower 5% limits for 90% credible intervals (CrI) (Supplementary Appendix Table A1). Analyses were conducted using SAS version 9.3 (SAS Institute, Cary, NC).
RESULTS
Incidence of Laboratory-Confirmed Infections
During 1996–2012, FoodNet identified 21,405 laboratory-confirmed infections among adults aged ≥65 years caused by Salmonella (10,413 infections; 48.7%), Campylobacter (9229; 43.1%), Listeria (1007; 4.7%), and E. coli O157 (756; 3.5%). Among infections with a known specimen source, 11.0% (1129/10,309) of Salmonella, 2.7% (248/9048) of Campylobacter, and 0.3% (2/753) of E. coli O157 infections were isolated from a normally sterile site. (All Listeria infections were invasive, by definition.) From 2004 to 2012, 3.9% (575/14,881) of infections with information available were identified as outbreak-associated: E. coli O157 (18.1%; 72/398), Salmonella (5.9%; 448/7554), Listeria (5.8%; 36/621), and Campylobacter (0.3%; 19/6308).
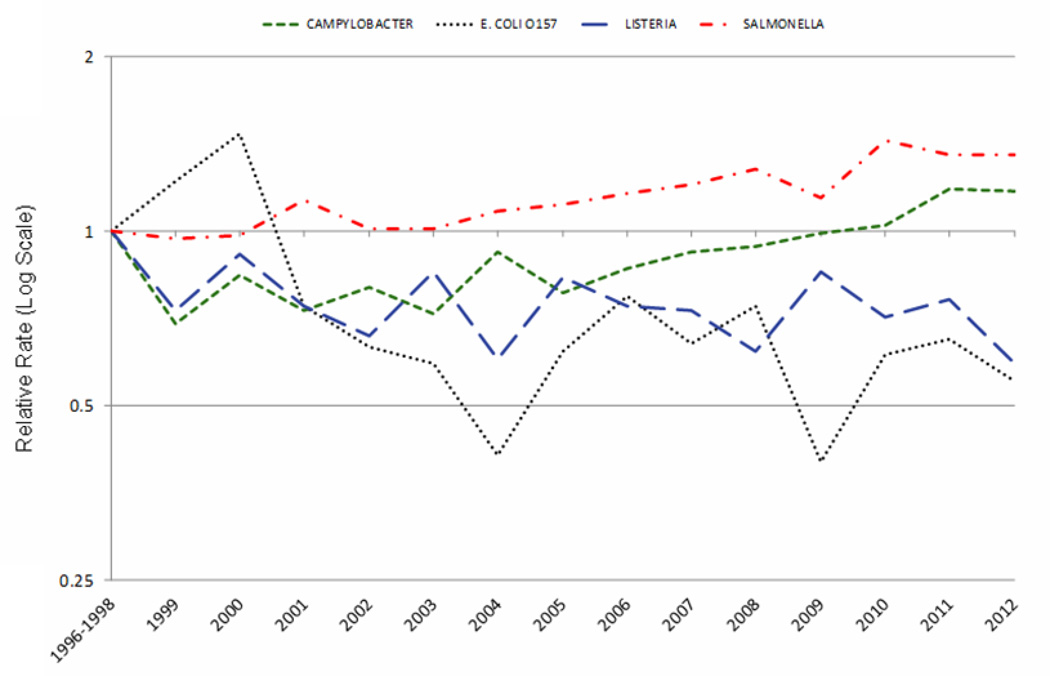
The average annual rate of infection was highest for Salmonella (12.8/100,000) and Campylobacter (12.1/100,000), followed by Listeria (1.4/100,000) and E. coli O157 (1.1/100,000). For Salmonella and Campylobacter, rates were significantly higher in 2012 than in 1996–1998 or 2006–2008: for Salmonella, 35% (95% CI, 18–56) and 12% higher (95% CI, 1–24), respectively; for Campylobacter, 17% (95% CI, 3–32) and 29% higher (95% CI, 17–43), respectively (Fig. 1). Rates in 2012 were significantly lower for E. coli O157 (45%; 95% CI, 20–62) and Listeria (41%; 95% CI, 18–58), compared with 1996–1998. Compared with children aged <5 years and people aged 5–64 years, adults aged ≥65 years had the highest average annual rate of Listeria infection, the lowest rates of Campylobacter and E. coli O157 infection, and the second highest rate of Salmonella infection (Table 1).
Figure 1.
Relative rates of laboratory-confirmed infections with Campylobacter, Escherichia coli O157, Listeria, and nontyphoidal Salmonella compared with 1996–1998 rates, by year, among adults aged ≥65 years, Foodborne Diseases Active Surveillance Network (FoodNet), 1996–2012
Among adults aged ≥65 years, the rate of infection increased with age for Listeria and Salmonella and decreased with age for Campylobacter (Fig. 2). Incidence of E. coli O157 infection was highest among adults aged 75–79 years. Average annual rates of Campylobacter and Listeria infection were higher among older men than older women, whereas the rate of Salmonella infection was higher in older women (Fig. 2). This disparity among cases of Salmonella infection was driven solely by the higher rate of urinary tract infections among older women. After excluding cases listing urine as the specimen source, the higher rate of infection in older women disappears. Conversely, the rate is slightly higher among males aged >70 years (data not shown). Overall, the rate of E. coli O157 infection was slightly higher among women than men. However, this varied by age group.
Figure 2.
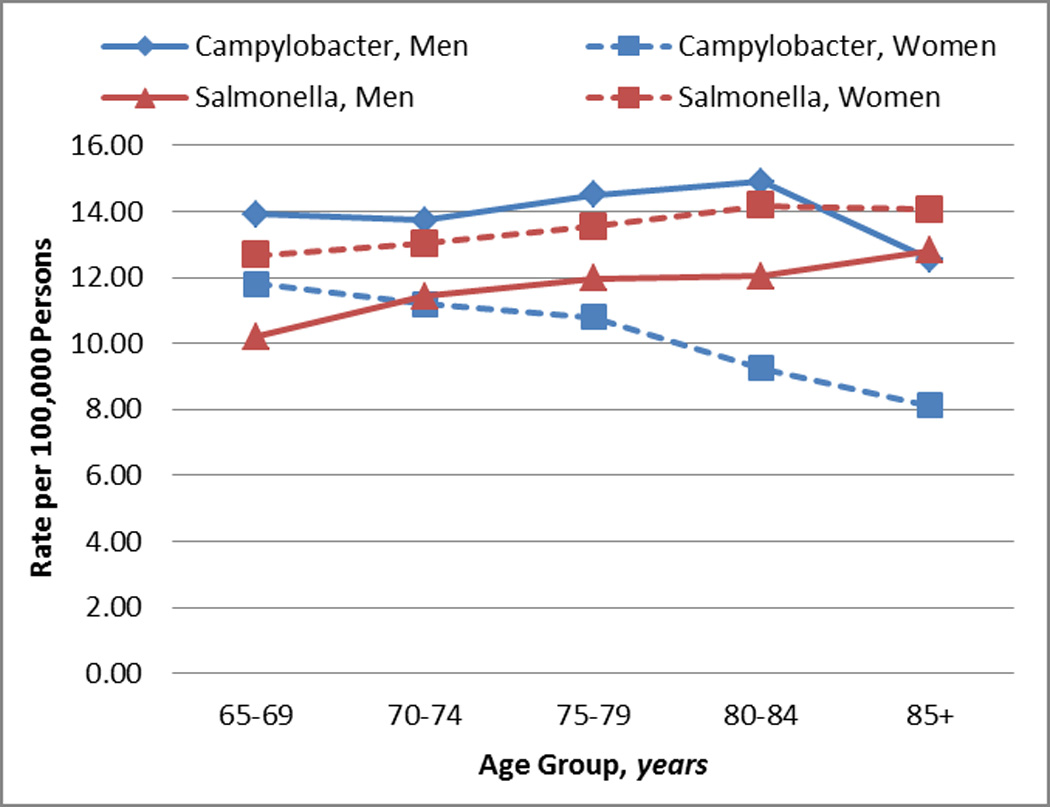
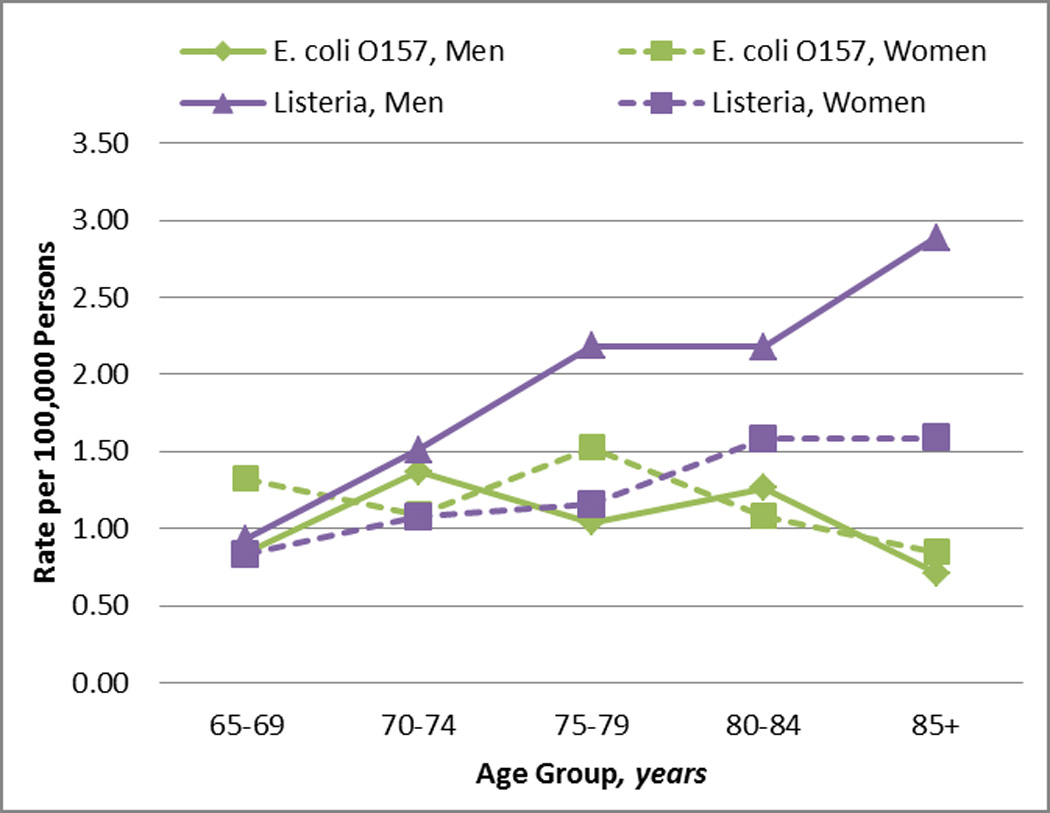
Incidence of laboratory-confirmed infections with Campylobacter and Salmonella (A) and E. coli O157 and Listeria (B) among adults aged ≥65 years by sex, Foodborne Diseases Active Surveillance Network (FoodNet), 1996–2012.
Overall, 49.3% of ill adults aged ≥65 years with available data were hospitalized (Table 2). Most hospitalizations were due to Salmonella infection, although the percentage of patients hospitalized was higher for Listeria and E. coli O157. Hospitalization rates increased with increasing age, except for Listeria, which had a high hospitalization rate in all age groups. At least 2.6% of adults aged ≥65 years died (Table 2). Salmonella and Listeria were the leading causes of death, though the percentage who died was almost 10-fold higher for Listeria. For all pathogens, the percentage who died was lowest among older adults in the youngest age group. The percentage hospitalized for Campylobacter, E. coli O157, and Salmonella and the percentage who died for each of the 4 pathogens was higher among adults aged ≥65 years than among children aged <5 years or people aged 5–64 years (Table 1).
Table 2.
| Age Group, years | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 65–69 | 70–74 | 75–79 | 80–84 | 85+ | Overall | |||||||
| Hospitalizations | ||||||||||||
| Pathogen | N | % | N | % | N | % | N | % | N | % | N | % |
| Salmonellac | 1,219 | 46.5 | 1,191 | 52.4 | 1,072 | 55.6 | 935 | 63.6 | 837 | 62.1 | 5,254 | 54.5 |
| Campylobacter | 621 | 23.9 | 619 | 31.5 | 634 | 39.4 | 559 | 48.9 | 510 | 56.6 | 2,943 | 35.8 |
| Listeria | 179 | 95.2 | 183 | 92.0 | 202 | 96.2 | 181 | 97.3 | 195 | 96.5 | 940 | 95.4 |
| E. coli O157 | 130 | 62.8 | 111 | 60.3 | 128 | 75.3 | 84 | 79.2 | 61 | 82.4 | 514 | 69.4 |
| Total | 2,149 | 38.3 | 2,104 | 45.5 | 2,036 | 52.0 | 1,759 | 60.6 | 1,603 | 63.5 | 9,651 | 49.3 |
| Deaths | ||||||||||||
| Pathogen | N | % | N | % | N | % | N | % | N | % | N | % |
| Salmonellac | 43 | 1.5 | 50 | 2.0 | 39 | 1.9 | 55 | 3.5 | 63 | 4.3 | 250 | 2.4 |
| Campylobacter | 5 | 0.2 | 6 | 0.3 | 13 | 0.7 | 7 | 0.6 | 12 | 1.2 | 43 | 0.5 |
| Listeria | 28 | 14.7 | 46 | 22.4 | 49 | 22.3 | 45 | 23.6 | 52 | 25.2 | 220 | 21.9 |
| E. coli O157 | 4 | 1.9 | 5 | 2.7 | 13 | 7.4 | 3 | 2.8 | 7 | 9.3 | 32 | 4.2 |
| Total | 80 | 1.3 | 107 | 2.1 | 114 | 2.7 | 110 | 3.5 | 134 | 4.9 | 545 | 2.6 |
Among 17,586 (91%) of 19,311 laboratory-confirmed case-patients with known hospitalization status.
Data are from the Foodborne Diseases Active Surveillance Network (FoodNet).
Nontyphoidal; includes serotypes other than Typhi.
Estimated Illnesses, Hospitalizations, and Deaths
After adjusting for medical care-seeking, stool sample submission, laboratory practices, and test sensitivity, we estimated that each year Campylobacter caused 110,200 illnesses and Salmonella caused 110,100 among adults aged ≥65 years in the United States (296 illness per 100,000 older adults for each pathogen). Thus, for every laboratory-confirmed case of Campylobacter or Salmonella among adults aged ≥65 years, we estimated there were actually 24 and 23 illnesses, respectively. E. coli O157 caused an estimated 4700 illnesses and Listeria an estimated 990 illnesses annually.
Of the 4 pathogens, we estimated that Salmonella caused the most hospitalizations (5100) and deaths (220) among adults aged ≥65 years. Listeria was estimated to be the third leading cause of hospitalizations (890), after Campylobacter (3200), and the second leading cause of death (180) (Table 3).
Table 3.
Estimated Annual Illnesses of Campylobacter, Escherichia coli O157, Listeria, and Nontyphoidal Salmonella Among Adults Aged ≥65 Years, United Statesa
| Pathogen | Laboratory- Confirmed Illnessesb |
Multiplier | Total Illnessesc | Hospitalizations | Deaths | ||||
|---|---|---|---|---|---|---|---|---|---|
| Mean | 90% CrI | Mean | Mean | 90% CrI | Mean | 90% CrI | Mean | 90% CrI | |
| Campylobacter | 4700 | 1400–10,400 | 23.5 | 110,200 | 29,700–255,900 | 3200 | 1200–6600 | 60 | 0–270 |
| Salmonellad | 4900 | 3300–7900 | 22.6 | 110,100 | 51,800–213,800 | 5100 | 2500–9700 | 220 | 0–620 |
| Listeria | 480 | 150–910 | 2 | 990 | 290–1900 | 890 | 240–1800 | 180 | 0–570 |
| E. coli O157 | 340 | 0–870 | 13.8 | 4700 | 340–13,200 | 470 | 0–1200 | 20 | 0–130 |
Modal or mean value shown; numbers >1000 rounded to nearest hundred, numbers from 10 to 1000 rounded to nearest 10, numbers <10 not rounded.
Laboratory-confirmed cases were extrapolated from FoodNet surveillance data.
Adjusted for medical care sought, stool sample submitted, bacterial culture performed, laboratory testing for pathogen, and laboratory test sensitivity (Supplementary Appendix Table A1).
Nontyphoidal; includes serotypes other than Typhi.
CrI = credible interval.
Considering people of all ages, those aged ≥65 years accounted for 9% of estimated illnesses but 24% of estimated hospitalizations and 55% of estimated deaths caused by these enteric pathogens. Older adults accounted for 58% of estimated illnesses, 59% of hospitalizations, and 67% of deaths for Listeria. (Supplementary Appendix Table A2).
DISCUSSION
Campylobacter, E. coli O157, Listeria, and Salmonella infections disproportionately harm older adults, and as they age, that harm is more likely to result in hospital stays or death. After adjusting for underdiagnosis, we estimated that 4 pathogens caused about 226,000 illnesses, 9700 hospitalizations, and 480 deaths annually among older adults. Because these pathogens often spread through food, effective measures to improve food safety could go a long way toward improving the health of older adults.
As one would suspect, rates of illness, hospitalization, and death generally increased with age among older adults, but we found the rate of laboratory-confirmed Campylobacter infection decreased with age. This is consistent with data from other industrialized countries that show campylobacteriosis peaks in childhood and, after a steep decline, peaks again in young adulthood before gradually declining. Some studies indicate that frequent exposure induces protective immunity to Campylobacter (Cawthraw et al., 2000). However, rates of hospitalization and death among older adults who become infected with Campylobacter continued to increase with age, similar to other enteric pathogens in this study. The percentage of outbreak-associated infections among older adults was similar to that of the general population except for Listeria, for which the outbreak-associated percentage was higher in older adults (Scallan et al., 2011). This difference was driven by a large outbreak of listeriosis that involved many older adults in 2011.
Not surprisingly, infections in older adults are more often invasive. In our study, 11% of Salmonella isolates were from blood, compared with just 5–6% for the overall population (Olsen et al., 2001; Jones et al., 2008). Campylobacter was also more likely to be isolated from blood in older adults (3% versus ≤1%) (Ailes et al., 2008; Nielsen et al., 2010). The increased risk of death in older adult patients hospitalized with Salmonella or Campylobacter infection may be partly due to the higher prevalence of comorbidities. This is one reason residents of long-term care facilities (LTCF), who are among the most frail elderly, are thought to experience a higher incidence of gastroenteritis and to be at higher risk for foodborne illness (Garibaldi, 1999).
The rate of laboratory-confirmed Campylobacter infections among older adults was higher for men than women, similar to findings in other age groups (Ailes et al., 2008). The rate of laboratory-confirmed Listeria infections was also higher among older men, suggesting sex-specific risk factors for these infections. In contrast, laboratory-confirmed Salmonella infections occurred more often in women, which is due to their higher rate of urinary tract infections. The higher rate of Salmonella urinary tract infections in older women is well documented (Sivapalasingam et al., 2004).
Our point estimates for every laboratory-confirmed case of Campylobacter, Salmonella, and E. coli O157 illness among adults aged ≥65 years were lower than for the general population (24 versus 30 for Campylobacter, 23 versus 29 for Salmonella, and 14 versus 26 for E. coli O157) but were higher than for children aged ≤5 years (14, 12, and 9, respectively) (Scallan et al., 2011, 2012). Our method assigned the same percentage of severe illnesses for older adults as that assigned to the general population for Campylobacter, Salmonella, and E. coli O157 infection. The lower rate of underdiagnosis among older adults compared with the general population was due mostly to their higher rate of medical care-seeking (56% versus 35% among those reporting severe [bloody] and 22% versus 18% among those reporting mild [non-bloody] diarrhea, respectively). These data are consistent with studies in other countries that have found slightly higher rates of medical care-seeking for gastrointestinal illnesses among older adults (Scallan et al., 2005b; Kirk et al., 2012).
Estimating the percentage of laboratory-confirmed Salmonella or Campylobacter infection to categorize as “severe illness” is a critical and challenging part of estimating the overall burden of disease and has considerable influence on the resulting estimates. In previous analyses, we used bloody diarrhea as an indicator of severe illness and estimated the proportion of laboratory-confirmed illnesses with bloody diarrhea using case series data from FoodNet case-control studies (Scallan et al., 2011, 2012). However, the proportion of older people with Salmonella and Campylobacter infections reporting bloody diarrhea in FoodNet case-control studies was low (15% and 22%, respectively) (Friedman et al., 2004; Hennessy et al., 2004; Kimura et al., 2004; Mermin et al., 2004; Marcus et al., 2007) for the percentage hospitalized. Therefore, when estimating total Campylobacter and Salmonella illnesses among older people, we assumed the percentage of severe illness was similar to that of the general population. Other choices would have resulted in different estimates for these pathogens. For example, using the percentage of case-patients hospitalized would have resulted in estimates similar to those we reported in the Results section for Campylobacter (121,080 versus 110,200) and Salmonella (99,800 versus 110,100). However, using the percentage of case-patients with bloody diarrhea as an indicator of the percentage of severe illness would have resulted in much higher estimates for Campylobacter (268,600) and Salmonella (285,600) (Supplementary Appendix Tables A3 and A4).
This analysis is subject to limitations beyond those already discussed. First, much of the data came from FoodNet sites, which were not selected to represent the U.S. population. However, a comparison of data from FoodNet and the 2005 U.S. census showed minimal demographic differences (Scallan, 2007). Second, FoodNet determines outcome at 7 days after the specimen collection date or at hospital discharge. When death occurs, however, FoodNet does not consider whether the reported infection contributed, and some reported deaths may not be related to the infection. Determining cause of death among older people is especially difficult because of comorbidities. Third, although FoodNet surveillance includes laboratory-confirmed cases of infection among residents of LTCF, FoodNet does not survey these residents when estimating how often they seek medical care. The incidence of foodborne pathogens and medical care-seeking practices may differ between older people living in LTCF and those living in the community. Also, the proportion of older adults living in LTCF varies by age. Fourth, estimates of the rates of medical care-seeking and stool sample submission from FoodNet population surveys increased each survey cycle, with the largest increase occurring between 2002 and 2003, and 2006 and 2007. The questionnaire used in 2006–2007 differed from earlier studies in the order and wording of questions, perhaps explaining at least some of this increase. Fifth, our adjustment for underdiagnosis by doubling the number of hospitalizations and deaths, although consistent with previous studies (Scallan et al., 2011), has not been validated. These sources of potential bias, along with the uncertainties reflected in our credible intervals, point to the need for additional studies to improve estimates of the total number of illnesses, hospitalization, and deaths. In our view, developing a more data-driven approach to adjusting for underdiagnosis for hospitalizations and deaths and being better able to classify severe illness in older adults are the most important questions to be addressed.
The burden of bacterial enteric infection among adults ≥65 years of age is high. Moreover, older adults are at an increased risk for severe outcomes. Because these four bacterial pathogens are transmitted commonly through food, this study highlights the need for effective food safety interventions that target older adults, especially given anticipated increases in the population of people over 65 years of age.
Supplementary Material
Acknowledgments
This article was supported in part by the Association of Public Health Laboratories and Cooperative Agreement Number #1U60HM000803 from Centers for Disease Control and Prevention (CDC). The contents are solely the responsibility of the authors and do not necessarily represent the official views of the Centers for Disease Control and Prevention.
Footnotes
Disclosures: None
References
- Ailes E, Demma L, Hurd S, Hatch J, Jones TF, Vugia D, Cronquist A, Tobin-D'Angelo M, Larson K, Laine E, Edge K, Zansky S, Scallan E. Continued decline in the incidence of Campylobacter infections, FoodNet 1996–2006. Foodborne Pathog Dis. 2008;5:329–337. doi: 10.1089/fpd.2008.0090. [DOI] [PubMed] [Google Scholar]
- Barton Behravesh C, Jones TF, Vugia DJ, Long C, Marcus R, Smith K, Thomas S, Zansky S, Fullerton KE, Henao OL, Scallan E FoodNet Working G. Deaths associated with bacterial pathogens transmitted commonly through food: foodborne diseases active surveillance network (FoodNet), 1996–2005. J Infect Dis. 2011;204:263–267. doi: 10.1093/infdis/jir263. [DOI] [PubMed] [Google Scholar]
- Cawthraw SA, Lind L, Kaijser B, Newell DG. Antibodies, directed towards Campylobacter jejuni antigens, in sera from poultry abattoir workers. Clin Exp Immunol. 2000;122:55–60. doi: 10.1046/j.1365-2249.2000.01349.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. •FoodNet Population Survey•. [Retrieved October 2013]; from http://www.cdc.gov/foodnet/studies/population-surveys.html.
- Crim SM, Iwamoto M, Huang JY, Griffin PM, Gilliss D, Cronquist AB, Cartter M, Tobin-D'Angelo M, Blythe D, Smith K, Lathrop S, Zansky S, Cieslak PR, Dunn J, Holt KG, Lance S, Tauxe R, Henao OL Centers for Disease C and Prevention. Incidence and trends of infection with pathogens transmitted commonly through food--Foodborne Diseases Active Surveillance Network, 10 U.S. sites, 2006–2013. MMWR Morb Mortal Wkly Rep. 2014;63:328–332. [PMC free article] [PubMed] [Google Scholar]
- Friedman CR, Hoekstra RM, Samuel M, Marcus R, Bender J, Shiferaw B, Reddy S, Ahuja SD, Helfrick DL, Hardnett F, Carter M, Anderson B, Tauxe RV. Risk factors for sporadic Campylobacter infection in the United States: A case-control study in FoodNet sites. Clin Infect Dis. 2004;38(Suppl 3):S285–S296. doi: 10.1086/381598. [DOI] [PubMed] [Google Scholar]
- Garibaldi RA. Residential care and the elderly: the burden of infection. J Hosp Infect. 1999;43(Suppl):S9–S18. doi: 10.1016/s0195-6701(99)90061-0. [DOI] [PubMed] [Google Scholar]
- Henao OL, Scallan E, Mahon B, Hoekstra RM. Methods for monitoring trends in the incidence of foodborne diseases: Foodborne Diseases Active Surveillance Network 1996–2008. Foodborne Pathog Dis. 2010;7:1421–1426. doi: 10.1089/fpd.2010.0629. [DOI] [PubMed] [Google Scholar]
- Hennessy TW, Cheng LH, Kassenborg H, Ahuja SD, Mohle-Boetani J, Marcus R, Shiferaw B, Angulo FJ. Egg consumption is the principal risk factor for sporadic Salmonella serotype Heidelberg infections: a case-control study in FoodNet sites. Clin Infect Dis. 2004;38(Suppl 3):S237–S243. doi: 10.1086/381593. [DOI] [PubMed] [Google Scholar]
- Jones TF, Ingram LA, Cieslak PR, Vugia DJ, Tobin-D'Angelo M, Hurd S, Medus C, Cronquist A, Angulo FJ. Salmonellosis outcomes differ substantially by serotype. J Infect Dis. 2008;198:109–114. doi: 10.1086/588823. [DOI] [PubMed] [Google Scholar]
- Jones TF, McMillian MB, Scallan E, Frenzen PD, Cronquist AB, Thomas S, Angulo FJ. A population-based estimate of the substantial burden of diarrhoeal disease in the United States; FoodNet, 1996–2003. Epidemiol Infect. 2007;135:293–301. doi: 10.1017/S0950268806006765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kassenborg HD, Hedberg CW, Hoekstra M, Evans MC, Chin AE, Marcus R, Vugia DJ, Smith K, Ahuja SD, Slutsker L, Griffin PM. Farm visits and undercooked hamburgers as major risk factors for sporadic Escherichia coli O157:H7 infection: data from a case-control study in 5 FoodNet sites. Clin Infect Dis. 2004;38(Suppl 3):S271–S278. doi: 10.1086/381596. [DOI] [PubMed] [Google Scholar]
- Kimura AC, Reddy V, Marcus R, Cieslak PR, Mohle-Boetani JC, Kassenborg HD, Segler SD, Hardnett FP, Barrett T, Swerdlow DL. Chicken consumption is a newly identified risk factor for sporadic Salmonella enterica serotype Enteritidis infections in the United States: a case-control study in FoodNet sites. Clin Infect Dis. 2004;38(Suppl 3):S244–S252. doi: 10.1086/381576. [DOI] [PubMed] [Google Scholar]
- Kirk MD, Hall GV, Becker N. Gastroenteritis in older people living in the community: results of two Australian surveys. Epidemiol Infect. 2012;140:2028–2036. doi: 10.1017/S0950268811002834. [DOI] [PubMed] [Google Scholar]
- Lund BM, O'Brien SJ. The occurrence and prevention of foodborne disease in vulnerable people. Foodborne Pathog Dis. 2011;8:961–973. doi: 10.1089/fpd.2011.0860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manikonda K, Palmer A, Wymore K, McMillian M, Nicholson C, Hurd S, Hoefer D, Tobin-D'Angelo M, Cosgrove S, Lyons C, Lathrop S, Hedican E, Patrick M. Validating deaths reported in the Foodborne Diseases Active Surveillance Network (FoodNet): are all deaths being captured? Clin Infect Dis. 2012;54(Suppl 5):S421–S423. doi: 10.1093/cid/cis266. [DOI] [PubMed] [Google Scholar]
- Marcus R, Varma JK, Medus C, Boothe EJ, Anderson BJ, Crume T, Fullerton KE, Moore MR, White PL, Lyszkowicz E, Voetsch AC, Angulo FJ. Re-assessment of risk factors for sporadic Salmonella serotype Enteritidis infections: a case-control study in five FoodNet Sites, 2002–2003. Epidemiol Infect. 2007;135:84–92. doi: 10.1017/S0950268806006558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mermin J, Hutwagner L, Vugia D, Shallow S, Daily P, Bender J, Koehler J, Marcus R, Angulo FJ. Reptiles, amphibians, and human Salmonella infection: a population-based, case-control study. Clin Infect Dis. 2004;38(Suppl 3):S253–S261. doi: 10.1086/381594. [DOI] [PubMed] [Google Scholar]
- Nielsen H, Hansen KK, Gradel KO, Kristensen B, Ejlertsen T, Ostergaard C, Schonheyder HC. Bacteraemia as a result of Campylobacter species: a population-based study of epidemiology and clinical risk factors. Clin Microbiol Infect. 2010;16:57–61. doi: 10.1111/j.1469-0691.2009.02900.x. [DOI] [PubMed] [Google Scholar]
- Olsen SJ, Bishop R, Brenner FW, Roels TH, Bean N, Tauxe RV, Slutsker L. The changing epidemiology of salmonella: trends in serotypes isolated from humans in the United States, 1987–1997. J. Infect. Dis. 2001;183:753–761. doi: 10.1086/318832. [DOI] [PubMed] [Google Scholar]
- Scallan E. Activities, achievements, and lessons learned during the first 10 years of the Foodborne Diseases Active Surveillance Network: 1996–2005. Clin Infect Dis. 2007;44:718–725. doi: 10.1086/511648. [DOI] [PubMed] [Google Scholar]
- Scallan E, Fitzgerald M, Cormican M, Smyth B, Devine M, Daly L, Reilly P, Crowley D, O'Sullivan MB, Collins C, Harkins V, McKeown P, Tohani V. The investigation of acute gastroenteritis in general practice: a survey of general practitioners in Northern Ireland and Republic of Ireland. Eur J Gen Pract. 2005a;11:136–138. doi: 10.3109/13814780509178257. [DOI] [PubMed] [Google Scholar]
- Scallan E, Hoekstra RM, Angulo FJ, Tauxe RV, Widdowson MA, Roy SL, Jones JL, Griffin PM. Foodborne illness acquired in the United States--major pathogens. Emerg Infect Dis. 2011;17:7–15. doi: 10.3201/eid1701.P11101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scallan E, Mahon BE, Hoekstra RM, Griffin PM. Estimates of Illnesses, Hospitalizations, and Deaths Caused By Major Bacterial Enteric Pathogens in Young Children in the United States. Pediatr Infect Dis J. 2013;32:217–221. doi: 10.1097/INF.0b013e31827ca763. [DOI] [PubMed] [Google Scholar]
- Scallan E, Majowicz SE, Hall G, Banerjee A, Bowman CL, Daly L, Jones T, Kirk MD, Fitzgerald M, Angulo FJ. Prevalence of diarrhoea in the Community in Australia, Canada, Ireland, and the United States. Int J Epidemiol. 2005b;34:454–460. doi: 10.1093/ije/dyh413. [DOI] [PubMed] [Google Scholar]
- Sivapalasingam S, Hoekstra RM, McQuiston JR, Fields PI, Tauxe RV. Salmonella bacteriuria: an increasing entity in elderly women in the United States. Epidemiol Infect. 2004;132:897–902. doi: 10.1017/s0950268804002717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith JL. Foodborne illness in the elderly. J Food Prot. 1998;61:1229–1239. doi: 10.4315/0362-028x-61.9.1229. [DOI] [PubMed] [Google Scholar]
- U.S. Census Bureau. The Next Four Decades, The Older Population in the United States: 2010 to 2050. Current Population Reports. 2010 May;:P25–P1138. [Google Scholar]
- Voetsch AC, Kennedy MH, Keene WE, Smith KE, Rabatsky-Ehr T, Zansky S, Thomas SM, Mohle-Boetani J, Sparling PH, McGavern MB, Mead PS. Risk factors for sporadic Shiga toxin-producing Escherichia coli O157 infections in FoodNet sites, 1999–2000. Epidemiol Infect. 2007;135:993–1000. doi: 10.1017/S0950268806007564. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.