Abstract
Air pollution in China, especially in the Pearl River Delta (PRD) region, has drastically increased in recent years. We modelled annual mean ground-level PM2.5 concentrations based on worldwide satellite information and meteorological data from 40 cities outside the PRD. The model of PM2.5 concentration (R = 0.845) was best explained by aerosol optical thickness (43.8%). We validated the spatial–temporal dimensions of the model and estimated that the annual mean PM2.5 concentration in PRD ranged between 22 and 65 μg m−3. Then we used meta-analysis to obtain the pooled excess risks of mortality in China and assessed the health impacts. We found an inverse association between short-term excess risks of mortality and annual mean PM2.5 concentrations. Based on the above models and analyses, the associated excess deaths for all-cause and cardiopulmonary diseases were 3386 and 2639 respectively. The corresponding risk-standardized excess death rates were 2006 and 1069 per million people.
Introduction
Long-term exposure to fine particulate matter PM2.5 (aerodynamic diameter ≤ 2.5 μm) has been linearly associated with all-cause, cardiovascular and lung cancer mortality with detectable effects down to 8 μg m−3,1 which is very close to the World Health Organization (WHO) Air Quality Guidelines (AQG) for PM2.5 of 10 μg m−3.2 Urban air pollution in Asian countries contributed to two thirds of the global burden of disease due to poor air quality3 and the highest levels were often observed in Chinese cities.4 China's rapid economic growth relying on vast consumption of fossil fuels5 for power generation, transportation and manufacturing industries has drastically increased the emissions in recent decades.6 The Pearl River Delta (PRD) in south mainland China is one of the most polluted regions where PM2.5 monitoring is still at an initial stage.7
Recent epidemiological studies have used correlations between satellite data of aerosol optical thickness (AOT) and PM2.5 to estimate the spatial variations of exposure to particulate pollution4,8–11 and the associated adverse health impacts.12 We aimed to estimate the PM2.5 concentration in the PRD region based on worldwide satellite and meteorological data, to pool the excess risks of mortality from the worldwide literature, and to assess the associated excess mortality in the PRD population.
Materials and methods
PM2.5 data
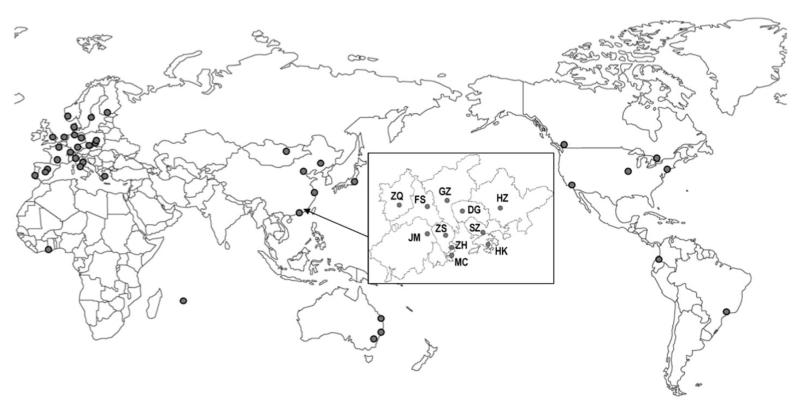
We collected PM2.5 annual mean concentration (μg m−3) for 40 cities in 25 countries (Fig. 1) corresponding to the years 2008 (n = 31) and 2009 (n = 9) from the World Health Organization (WHO) Urban Outdoor Air Pollution Database13 and from the Hong Kong SAR Government.14 The latter was the only city in the PRD with accessible data of PM2.5 recorded by a fixed-site monitoring network. We also obtained PM2.5 data from Beijing, Guangzhou, Shanghai and Tokyo by contacting the authors of relevant publications.15,16
Fig. 1.
Forty cities for modeling and eleven cities in the Pearl River Delta region in China for health impact assessment. Note: Large dots represent 40 cities in the world for modeling. Small dots inside the box represent 11 cities in the Pearl River Delta region in China for health impact assessment. ZQ = Zhaoqing, FS = Foshan, GZ = Guangzhou, DG = Dongguan, HZ = Huizhou, JM= Jiangmen, ZS = Zhongshan, SZ = Shenzhen, ZH = Zhuhai, MC = Macau, and HK = Hong Kong. 4 cities in China (Beijing, Shanghai, Shenyang, and Hong Kong) were part of the 40 cities in the world for modeling.
Satellite and meteorological data
We retrieved the databases from National Aeronautics and Space Administration (NASA)'s Moderate-resolution Imaging Spectroradiometer (MODIS) for monthly averages of AOT,17,18 cloud optical thickness (COT), carbon monoxide (CO) level (ppbv), land surface temperature (LST) (°C), and vegetation index (VI) in the 40 world cities as well as 11 Chinese cities in the PRD region (Fig. 1). We assessed the satellite information in 2–4 grids of fixed coordinate size (0.11 × 0.11) in the central area of each city (covering 272 to 547 km2). The annual mean value for air temperature (°C), dew point (°C), relative humidity (%), visibility (km), wind speed (km h−1), and cloud cover (okta) data of the base year were retrieved from a publicly accessible database.19 Missing data of monthly AOT (26%) were replaced by the data of the same month in the closest year (±1 to 3 years) multiplied by the year-to-year percentage changes of the available monthly data. The remaining missing data of AOT (13%) as well as some missing data of COT and CO (1.5% and 7.3%, respectively) were replaced by a multiple imputation method.20 AOT and visibility data from all cities were right-skewed and ln-transformed.
Modeling
We used cluster analysis to select independent variables with low multicollinearity and then fitted multiple regression models to estimate PM2.5 annual mean concentrations for all combinations of these selected variables (Suppl 1†).21 We assessed models' temporal sensitivity by using years different from 2008 and 2009 in Hong Kong, Los Angeles, Rome, Shenyang and Sydney which were cities with non-missing data. We also assessed models' spatial sensitivity by using cities other than the 40 cities. We identified the best model as having the smallest average discrepancy in both temporal and spatial sensitivity for prediction of PM2.5 annual mean (Suppl 2†). We ranked influential predictors based on the percentage variance explained (partial eta square η2) by each variable in the model and then visually inspected the linear associations between PM2.5 and the influential predictors after adjusting for covariates (Suppl 2†).22
Systematic review
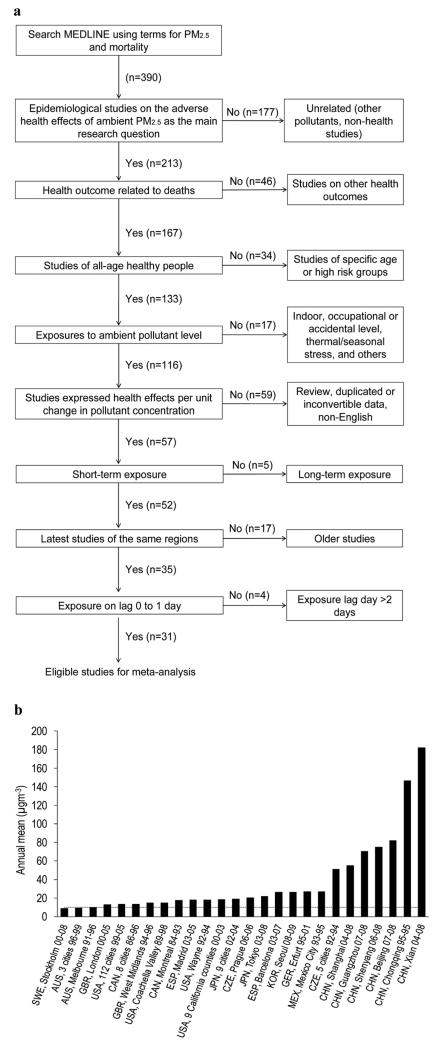
We searched the MEDLINE database using structured keyword terms, (“fine particulate”[tiab] or “fine particulates”[tiab] or “fine particle”[tiab] or “fine particles”[tiab] or “PM2.5”[tiab] or “PM(2.5)”[tiab]) and (“health”) and (mortality[tiab]), and retrieved 390 abstracts on 1st June 2012. We selected 35 literature articles using the following inclusion criteria (Fig. 2a): (i) all epidemiological studies on the adverse health effects of PM2.5 as the main research question; (ii) the health outcomes were related to deaths; (iii) the subjects were not high risk groups (e.g. patients or smokers) nor sensitive age subgroups (e.g. children or elders); (iv) exposures to ambient levels (not indoor, occupational or accidental exposures); (v) the health risk estimates were expressed in terms of unit change in pollutant mass concentration; and (vi) reported in English. We included non-duplicated publications on short-term effects only. We excluded the literature on long-term effects of mortality due to the insufficient number of studies that followed the abovementioned criteria (n = 5). We included studies on the single-pollutant model with lags ranging within day 0 and 1 since these findings were mostly reported. Finally, we selected the latest study only in each of the population to avoid over-representation by any single population (Fig. 2b).
Fig. 2.
(a) Literature selection. (b) Selected literature' records of PM2.5 concentrations. Note: Only the annual mean concentrations of the latest exposure year in each city are shown. Three-letter country codes: Australia (AUS), Canada (CAN), China (CHN), Czech Republic (CZE), Germany (GER), Japan (JPN), Korea (KOR), Mexico (MEX), Spain (ESP), Sweden (SWE), United Kingdom (GBR), and United States (USA). The dotted line represents the WHO annual AQG of 10 μg m−3 for PM2.5.
Meta-analysis
We used meta-analysis to pool risk estimates of PM2.5 on mortality for every 10 μg m−3 increase in pollutant concentration.23 We pooled excess risks (ER) in random effects if I2 statistics for heterogeneity was >25% or otherwise in a fixed effect. We used the influence plot of the conditional square root q2 statistics against square root w weight to diagnose the overall heterogeneity due to each study; and funnel plots with the Egger test on asymmetry at alpha level 0.1 to assess publication bias. We assumed the overall heterogeneity as statistically significant under normal distribution when the square root of q2 statistic lay outside −1.96 and 1.96.24,25
Meta-regression
Recent reviews of the health effects of PM2.5 in the American,26 European27 and Asian countries28 have consistently indicated evidence of increased deaths when exposure is elevated, but meta-analyses with meta-regression of these estimates across regions were rare. In this study, we pooled the short-term effect estimates of the excess risk of mortality from time-series studies on ambient PM2.5 in different global regions and conducted a meta-regression analysis of these estimates for improving our understanding of the differences in effect sizes across regions.
Health impact assessment
We obtained the annual total number of deaths (N) in 2008 from the Guangzhou Health Statistical Yearbook,29 Department of Health Statistical yearbook in Macau,30 and Hospital Authority clinical database in Hong Kong.31 The number of deaths in prefectures other than Guangzhou in PRD was not publicly available and we estimated by proportionality using the population ratios between these prefectures and Guangzhou (the capital city of Guangdong). We calculated the health impact by multiplying the pooled ER with N and the estimated annual mean concentrations of PM2.5. We assumed no threshold level for PM2.5 based on the hypothesis of both linear32–35 and nonlinear concentration response relationships.36,37 For comparison with the global health burden assessment study of excess deaths due to PM2.5,38 we calculated risk-standardized excess death rates, which was defined as the excess death rates per one million population multiplied by 10% (per 10 μg m−3 of PM2.5) as the fixed excess risk of death.
Results
Table 1 shows the selected best model (R = 0.85) that PM2.5 concentration was positively associated with ln-transformed aerosol optical thickness (β = 0.613 [95%CI: 0.367, 0.859]) but negatively associated with ln-transformed visibility (β = −0.987 [−1.587, −0.388]). These associations were consistent in other models. The largest variance of PM2.5 was explained by ln-transformed AOT (44%, p < 0.001) and multi-collinearity (variance inflation factors: 1.1 to 1.8) which were low for the rest of the covariates.
Table 1.
Selected best model of annual mean PM2.5 concentration (μg m−3) for health impact assessmenta
| Model | Unit | β | 95% CI | p-values | VIF | η2 (%) |
|---|---|---|---|---|---|---|
| Constant | 8.097 | 6.427, 9.767 | <0.001 | |||
| ln A | 0–1 | 0.613 | 0.367, 0.859 | <0.001 | 1.5 | 43.8 |
| In V | km | −0.987 | −1.587, −0.388 | 0.002 | 1.3 | 25.4 |
| C | 0–50 | −0.048 | −0.095, −0.001 | 0.045 | 1.7 | 11.7 |
| W | km h−1 | −0.037 | −0.075, 0.002 | 0.063 | 1.1 | 10.1 |
| L | °C | −0.020 | −0.049, 0.009 | 0.165 | 1.8 | 5.7 |
| cc | okta | −0.068 | −0.233, 0.097 | 0.406 | 1.4 | 2.1 |
Note: A = aerosol optical thickness, V = visibility, C = cloud optical thickness, W = wind speed, L = land surface temperature, and cc = cloud cover. VIF = variance inflation factor, in which VIF less than 2.5 is indicative of non-collinearity. η2 = partial eta square, which indicates the percentage variance explained by the variable in the model. Model selection (see M8 in Suppl 2, ESI).
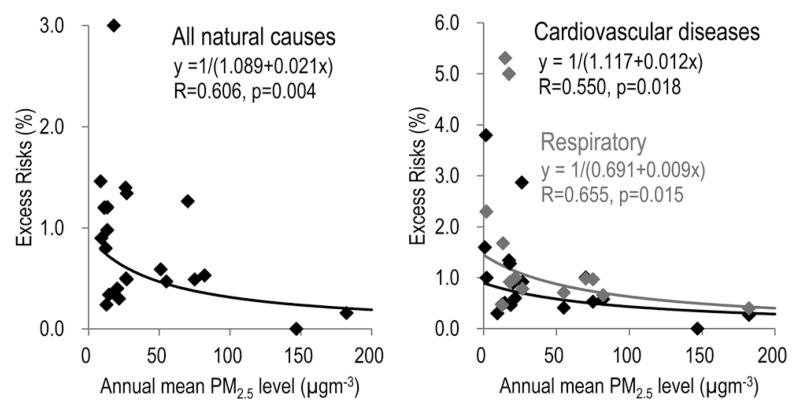
The pooled ER of mortality due to all-cause (ICD-10 A00-R99), cardiovascular (ICD-10 I00–I99) and respiratory (ICD-10 J00-J99) diseases for all the reviewed studies were 0.69% [0.45, 0.94], 0.60% [0.39, 0.80] and 0.83% [0.50, 1.17] respectively (Suppl 3 and 4†).63–93 The highest pooled ER by region in America (1.01% [0.79, 1.22]) followed by Europe 0.88% [0.34, 1.42] and Asia-Pacific 0.50% [0.19, 0.81] while the pooled ER for all of the six Chinese cities was 0.51% [0.14, 0.89] (Suppl 3†). Some publication bias was found (Egger test: p = 0.080) but it was not evident (Egger test: p = 0.460) after excluding influential studies defined by significant overall heterogeneity (Suppl 5†). Results of meta-regression analysis indicated that the ER of mortality in the literature were inversely related to the annual PM2.5 concentrations in a slightly decaying pattern (Fig. 3).
Fig. 3.
Meta-regression analysis of annual mean PM2.5 concentration and the non-negative excess risk (%) of mortality for all natural causes (n = 22) and for cardiovascular (n = 19) and respiratory causes (n = 13) in different studies.
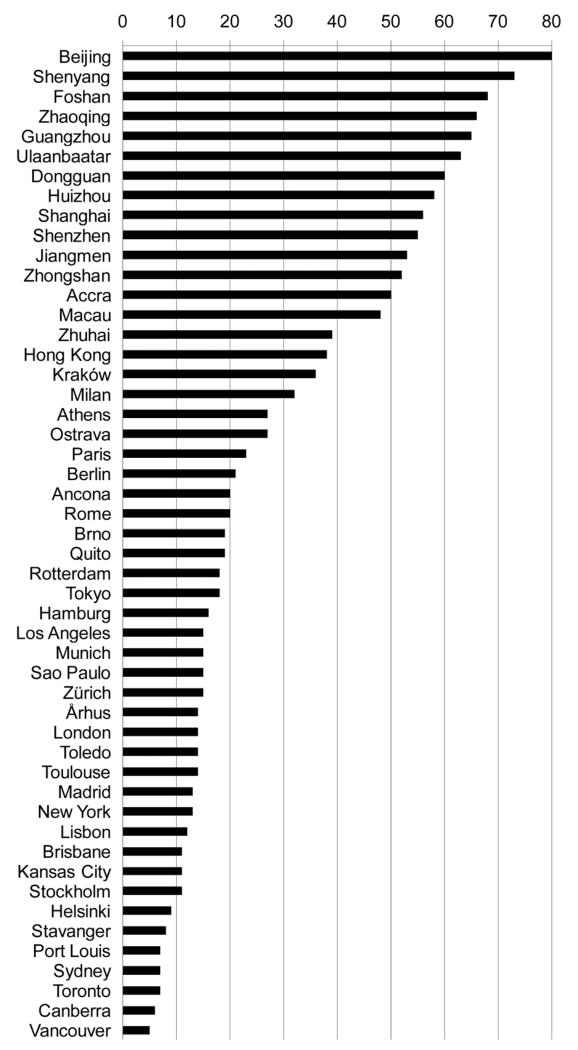
In PRD regions in 2008–2009, the model predicted annual mean PM2.5 concentrations were 45 μg m−3, which was 4.5 times of the WHOAQG of 10 μg m−3. The lowest predicted annual mean was in Zhuhai (22 μg m−3) and the highest one was in Foshan (65 μg m−3). In the region, the mean estimated PM2.5 annual concentration based on the ratio of PM2.5/PM10 was 50 μg m−3, with the lowest annual mean in Hong Kong (33 μg m−3) and the highest one in Foshan (81 μg m−3) (Table 2). The predicted values of the PM2.5 in PRD regions were relatively higher than the rest of the other cities in the world (Fig. 4).
Table 2.
Health impact assessment – excess deaths due to PM2.5 in the PRD regionsa
| HK | MC | DG | FS | GZ | HZ | JM | SZ | ZH | ZQ | ZS | PRD | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Annual mean (μ gm−3) | Mean | |||||||||||
| Monitored PM2.5 | 33 | 45.2 | ||||||||||
| Modeled PM2.5 | 28 | 58 | 65 | 61 | 43 | 32 | 47 | 22 | 63 | 47 | ||
| Estimated PM2.5 (70% of monitored PM10, for validation purpose) | 33 | 39 | 56 | 81 | 50 | 55 | 48 | 38 | 39 | 62 | 49 | 50.0 |
| Total | ||||||||||||
| Population (million) | 7.0 | 0.5 | 1.7 | 3.6 | 7.8 | 3.2 | 3.9 | 2.3 | 1.0 | 4.1 | 1.5 | 36.7 |
| Death rate per 1000 | 6.00 | 3.20 | 4.54 | 5.49 | 5.55 | 4.90 | 7.49 | 0.98 | 2.79 | 5.25 | 6.01 | |
| No. of deaths (1000) | Total | |||||||||||
| All-cause | 39.8 | 1.8 | 7.9 | 20.0 | 43.5 | 15.6 | 28.9 | 2.3 | 2.8 | 21.5 | 8.8 | 192.9 |
| Cardiovascular | 11.4 | 0.5 | 2.8 | 7.1 | 15.5 | 5.6 | 10.3 | 0.8 | 1.0 | 7.7 | 3.1 | 65.9 |
| Respiratory | 8.2 | 0.2 | 1.4 | 3.6 | 7.9 | 2.8 | 5.3 | 0.4 | 0.5 | 3.9 | 1.6 | 36.0 |
| ER derived from meta-regressions | Mean | |||||||||||
| All-cause | 0.56 | 0.60 | 0.43 | 0.41 | 0.42 | 0.50 | 0.57 | 0.48 | 0.64 | 0.42 | 0.48 | 0.49 |
| Cardiovascular | 0.66 | 0.69 | 0.55 | 0.53 | 0.54 | 0.61 | 0.67 | 0.60 | 0.72 | 0.53 | 0.59 | 0.60 |
| Respiratory | 1.02 | 1.06 | 0.83 | 0.79 | 0.81 | 0.93 | 1.02 | 0.90 | 1.12 | 0.80 | 0.90 | 0.91 |
| ED | Total | |||||||||||
| All-cause | 505 | 19 | 165 | 447 | 937 | 259 | 362 | 40 | 22 | 472 | 157 | 3386 |
| Cardiovascular | 170 | 6 | 75 | 206 | 429 | 113 | 152 | 18 | 9 | 217 | 70 | 1463 |
| Respiratory | 187 | 4 | 57 | 157 | 326 | 87 | 119 | 14 | 7 | 165 | 53 | 1176 |
| ED rate (per million) | ||||||||||||
| All-cause | 72 | 34 | 94 | 123 | 120 | 81 | 94 | 17 | 22 | 115 | 108 | 92 |
| Cardiovascular | 24 | 11 | 43 | 57 | 55 | 35 | 39 | 8 | 9 | 53 | 47 | 40 |
| Respiratory | 27 | 8 | 33 | 43 | 42 | 27 | 31 | 6 | 7 | 40 | 37 | 32 |
| Risk-standardized ED rate (per million) | ||||||||||||
| All-cause | 1282 | 562 | 2175 | 3002 | 2835 | 1616 | 1658 | 359 | 339 | 2772 | 2238 | 2006 |
| Cardiovascular | 366 | 155 | 777 | 1072 | 1012 | 577 | 592 | 128 | 121 | 990 | 799 | 698 |
| Respiratory | 263 | 77 | 396 | 547 | 517 | 294 | 302 | 65 | 62 | 505 | 408 | 371 |
Note: PM2.5 in Hong Kong was the real data from the Hong Kong Environmental Protection Department. HK = Hong Kong, MC = Macau, DG = Dongguan, FS = Foshan, GZ = Guangzhou, HZ = Huizhou, JM = Jiangmen, SZ = Shenzhen, ZH = Zhuhai, ZQ = Zhaoqing, ZS = Zhongshan, and PRD = Pearl River Delta. ER = excess risks per 10 μg m−3 derived from meta-regression models (see Fig. 3). ED = excess deaths. The risk-standardized ED rate was calculated using 10% as the excess risks per 10 μg m−3 of PM2.5. The ratio of PM2.5 to PM10 annual mean has been very stable at 0.7 over the years in Hong Kong, which is the only city in PRD with a fixed site monitoring of PM2.5.
Fig. 4.
Modeled and monitored annual mean PM2.5 concentrations (μg m−3) in all cities from 2008–2009.
Based on model predicted PM2.5 levels, the annual total number of deaths due to all natural causes ranged from 1756 in Macau to 43 521 in Guangzhou, with a total of 192 911 deaths per year in the whole region (Table 2). The annual cardiovascular deaths were the lowest in Macau (485) and the highest in Guangzhou (15 543); but the highest respiratory deaths were observed in Hong Kong (8160).
The annual excess deaths due to model-predicted PM2.5 for all causes were the highest in Guangzhou (937) and the lowest in Macau (19). The same trends followed in excess deaths due to cardiovascular and respiratory diseases. The total excess deaths due to all-cause, cardiovascular and respiratory diseases were 3386, 1463, and 1176 respectively in the whole PRD region in 2008–2009. The corresponding risk-standardized excess death rates per one million people were 2006, 698 and 371 respectively (Table 2).
Discussion
Many studies have examined the relationship between ground-level monitored PM2.5 concentration and satellite AOT on a local or countrywide scale10,11,39–50 as well as on a global scale.4,51 We based our study on the established approach of predicting ground-level PM2.5 annual mean concentration in the PRD region where public accessibility to the monitoring data was not yet fully available.
Our model utilized both the vertical column aerosol, as measured by AOT, and the horizontal ground-level aerosol, as measured by visibility, together with cloud optical thickness and other satellite and meteorological information as co-predictors of the ground-level annual mean of PM2.5 concentration. Visibility is a well-known indicator of PM2.5.52,53 It is measured horizontally at a height that is relevant to the ground level monitoring of PM2.5 and provides information to explain the variance of PM2.5 in addition to that measured vertically by AOT. Besides, visibility data are readily obtainable in many cities for worldwide comparisons as they are standard measurements in airports as well as in weather observatories. Cloud optical thickness is a satellite measure of light extinction due to the amount and thickness of a cloud, which is related to humidity and pressure in the atmosphere. This variable together with cloud cover in our model shared the variance of relative humidity as a common covariate.10 Although the satellite detected carbon monoxide was identified as a covariate of AOT, it was not included in our selected model. Further studies on applying the carbon monoxide variable should be warranted since it is publicly available and is related to fossil fuel burning and traffic emissions, and we found the best predictive performance in the temporal sensitivity assessment.
It is interesting that the annual mean concentrations in the Chinese cities were relatively higher than all other studies, but the magnitude of pooled ER of all natural mortalitities for these six Chinese cities was only a half of that in the American region. The APHENA investigators have also tested whether the concentration–response curve was actually nonlinear and whether statistical methods were appropriate though conclusive evidence was not explicit.54 A distributed lag nonlinear model was also proposed to detect the nonlinear concentration–response curve and delayed effects.55 In meta-regression analysis we found some evidence of an inverse linear relationship between ER of mortality and the annual PM2.5 concentration. This pattern appears to be leveling off in the downward direction rather than purely linear.36 A similar pattern of inverse association has been observed in a cross-sectional study of lung function and exposure to indoor PM2.5 concentration.37 This inverse relationship could be related to a saturation mechanism occurring at lower exposure levels56 where both irreversible and reversible processes may simultaneously exist. This has been hypothesized that, as indicated by structural changes in airways,57,58 particulates that penetrate to the deepest part of the lung and cause alveolar epithelial injury are associated with both acute reversible inflammatory responses and cumulative irreversible pulmonary damage.37 An explanation by the saturation hypothesis for cardiovascular diseases is also warranted.36 Our findings suggest that there is a need for further study to assess the effects of longer-term exposure on the short-term mortality risks. In addition, difference in climate, population structures, gene susceptibility, health status, occupational exposures, long-term exposure history and composition in PM2.5 may play a role in explaining the potential differences in short-term effects by region. There were some reviews on the epidemiological studies on the impact of fine particulate air pollution on mortality,26,59,60 while reviews on the cause for specific mortality are rare. The present review provided a meta-regression between the short-term effects and the annual mean concentrations and is the first to report an inverse relationship with a slightly decaying pattern.
For health impact assessment in the PRD region, we reviewed six Chinese studies and pooled the excess risks of mortalities based on physician-diagnosis, which were once-in-a-lifetime clinical records and so could provide more reliable health effect information than physiological and bio-microscopic measurements. Our health impact assessment results were well supported by the latest global estimation of health burden due to PM2.5 concentration38 since our estimation of the risk-standardized excess death rate of 1069 per million people for cardiorespiratory causes was very close to that in Asia of 1104 per million per 10% excess risk (i.e. 2584 thousand × 1 million/1.8 billion × 10 excess risk%/13 reported excess risk%) in that report. Non-risk standardized estimates of disease burden varies between places and the type of study design. For instance, the short-term excess death rates calculated in the current study were smaller by an order of magnitude than those estimated in long-term studies.34,59 However when we standardized the excess risk to 10%, comparison with other studies was more meaningful.
There were several limitations in this study. First, the number of cities involved in modeling was based on availability of satellite AOT data and ground-level fixed site monitored records of PM2.5 concentrations as compiled by WHO.5 Also some cities might have been overlooked, but the approximate normal distributions of our collected data have indicated that the cities selected in our sample are representative of respective regions so that selection bias might have been minimum and therefore not affecting overall representativeness of the sample. Second, our assumption of PM2.5 concentration as 70% of PM10 concentration in the PRD region might have ignored the heterogeneity of PM2.5/PM10 ratio across the region. However a similar ratio derived from a recent study in Guangzhou has indicated that it is in good agreement with the ratio we used.61 Third, the generalization of our best model for prediction in cities outside China has not been assessed despite that our spatial validation was based on ten cities in the PRD region only. Nevertheless, our temporal validation that was based on cities in different continents has demonstrated to have good performance for prediction among the forty cities that were included in the modeling. Fourth, the variation in risks due to differences in anthropogenic versus natural dust components of PM was not addressed.62 Our results should be interpreted with caution especially for international comparison.
Conclusions
The exposure to particulate pollutants in the Pearl River Delta regions in China is much higher than many other cities in the world. This study shows that the variation in PM2.5 annual concentrations may be inversely related to magnitude of short-term effects on mortality across geographic regions. The rapid growth of the economy in the region undoubtedly has contributed to the impact of air pollution on the population which is estimated to be responsible for 1069 excess deaths per million people. Nowadays, satellite and meteorological information is readily accessible so that public health impacts due to particulate air pollution in locations lacking monitoring can also be assessed.
Supplementary Material
Environmental impact.
Particulate air pollution has surged over densely populated cities in China in recent years and has recently received international attention due to the toxicity of the fine portion of particulate matter and the associated adverse health consequences to local residents as well as to tourists and investors. The environmental impact could be assessed based on the community health burden attributable to exposure to the ambient concentration in the Pearl River Delta which represents Chinese regions with rapid economic growth where energy production mainly depends on fossil fuels with air pollution generated from power plants, motor vehicles and industrial emissions. Worldwide satellite and meteorological information could be applied for exposure assessment and model validation.
Acknowledgements
This work was supported by the Wellcome Trust [#094330/Z10/Z].
Footnotes
Electronic supplementary information (ESI) available: Supplementary I: cluster analysis for selection of independent variables in multiple regressions. Supplementary II: regression models of PM2.5 and sensitivity of the model predictions; visual inspection of the major independent variables: ln-transformed data of PM2.5 versus AOT and visibility in 40 cities. Supplementary III: literature review – detection of heterogeneity and publication bias. Supplementary IV: summary of excess risks of different causes of mortality in all age groups due to PM2.5. See DOI: 10.1039/c3em00357d
Notes and references
- 1.Lepeule J, Laden F, Dockery D, Schwartz J. Environ. Health Perspect. 2012;120:165–170. doi: 10.1289/ehp.1104660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization. Air Quality Guidelines Global Update . 2005: particulate matter, ozone, nitrogen dioxide and sulfur dioxide. WHO Regional Office for Europe; Copenhagen: 2006. [Google Scholar]
- 3.Krzyzanowski M, Cohen A. Air Qual., Atmos. Health. 2008;1:7–13. [Google Scholar]
- 4.van Donkelaar A, Martin RV, Brauer M, Kahn R, Levy R, Verduzco C, Villeneuve PJ. Environ. Health Perspect. 2010;118:847–855. doi: 10.1289/ehp.0901623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang JN, Lei Y, Yang JT, Yan G. Environ. Sci. Technol. 2012;46:4263–4264. doi: 10.1021/es301226n. [DOI] [PubMed] [Google Scholar]
- 6.Chen BH, Kan HD, Chen RJ, Jiang SH, Hong CJ. J. Air Waste Manage. Assoc. 2011;61:1292–1299. [Google Scholar]
- 7.Yuan Y, Liu SS, Castro R, Pan XB. Environ. Sci. Technol. 2012;46:3627–3628. doi: 10.1021/es300984j. [DOI] [PubMed] [Google Scholar]
- 8.Wang J, Christopher SA. Geophys. Res. Lett. 2003:30. [Google Scholar]
- 9.Engel-Cox JA, Hoff RM, Haymet ADJ. J. Air Waste Manage. Assoc. 2004;54:1360–1371. doi: 10.1080/10473289.2004.10471005. [DOI] [PubMed] [Google Scholar]
- 10.Liu Y, Sarnat JA, Kilaru A, Jacob DJ, Koutrakis P. Environ. Sci. Technol. 2005;39:3269–3278. doi: 10.1021/es049352m. [DOI] [PubMed] [Google Scholar]
- 11.Liu Y, Paciorek CJ, Koutrakis P. Environ Health Persp. 2009;117:886–892. doi: 10.1289/ehp.0800123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Crouse DL, Peters PA, van Donkelaar A, Goldberg MS, Villeneuve PJ, Brion O, Khan S, Atari DO, Jerrett M, Pope CA, Brauer M, Brook JR, Martin RV, Stieb D, Burnett RT. Environ. Health Perspect. 2012;120:708–714. doi: 10.1289/ehp.1104049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.World Health Organization . Urban Outdoor Air Pollution Database. WHO, Geneva: [Last accessed 13 June 2012]. 2011. http://www.who.int/phe/health_topics/outdoorair/databases/en/index.html. [Google Scholar]
- 14.Hong Kong Environmental Protection Department [Last accessed 21 May 2012];Past air monitoring station data, 2008–2009. http://epic.epd.gov.hk/ca/uid/airdata/p/1.
- 15.Chen R, Li Y, Ma Y, Pan G, Zeng G, Xu X, Chen B, Kan H. Sci. Total Environ. 2011;409:4934–4938. doi: 10.1016/j.scitotenv.2011.08.058. [DOI] [PubMed] [Google Scholar]
- 16.Yorifuji T, Kawachi I, Kaneda M, Takao S, Kashima S, Doi H. Sci. Total Environ. 2011;409:3620–3627. doi: 10.1016/j.scitotenv.2011.06.002. [DOI] [PubMed] [Google Scholar]
- 17.Lai HK, Ho SY, Wong CM, Mak KK, Lo WS, Lam TH. Int. J. Environ. Health Res. 2010;20:219–230. doi: 10.1080/09603120903511119. [DOI] [PubMed] [Google Scholar]
- 18.Liu Y, Franklin M, Kahn R, Koutrakis P. Remote Sensing of Environment. 2007;107:33–44. [Google Scholar]
- 19.Weather History for cities in 2008 and 2009. Weather Underground, Inc; [Last accessed 1 May 2012]. 2013. Weather underground. http://www.wunderground.com. [Google Scholar]
- 20.Schafer JL, Graham JW. Psychological Methods. 2002;7:147–177. [PubMed] [Google Scholar]
- 21.Lai HK, Bayer-Oglesby L, Colvile R, Gotschi T, Jantunen MJ, Künzli N, Kulinskaya E, Schweizer C, Nieuwenhuijsen MJ. Atmos. Environ. 2006;40:1299–1313. [Google Scholar]
- 22.Larsen WA, McCleary SJ. Technometrics. 1972;14:781–790. [Google Scholar]
- 23.Lai HK, Tsang H, Wong CM. BMC Public Health. 2013;13:360. doi: 10.1186/1471-2458-13-360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Woodward M. Epidemiology: study design and data analysis. 2nd edn Chapman & Hall/CRC, Boca Raton; Fla: 2005. Meta-analysis (Ch.12) [Google Scholar]
- 25.Egger M, Davey SG, Schneider MC. BMJ. 1997;315:629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Levy JI, Diez D, Dou Y, Barr CD, Dominici F. Am. J. Epidemiol. 2012;175:1091–1099. doi: 10.1093/aje/kwr457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Anderson HR, Atkinson RW, Peacock JL, Marston L, Konstantinou K. Meta-analysis of time-series studies and panel studies of particulate matter (PM) and ozone (O3): report of a WHO task group. World Health Organization; Copenhagen: 2004. [Google Scholar]
- 28.Jahn HJ, Schneider A, Breitner S, Eissner R, Wendisch M, Kramer A, et al. Int. J. Hyg. Environ. Health. 2011;214:281–295. doi: 10.1016/j.ijheh.2011.05.008. [DOI] [PubMed] [Google Scholar]
- 29.Bureau of Health of Guangzhou Municipality. 2010.
- 30. [Last accessed 2 February 2012];Macao Department of Health, Boletim Estatistico. 2008 http://www.ssm.gov.mo/design/statistic/e_statistic_fs.htm.
- 31.Hong Kong Hospital Authority [Last accessed 2 February 2012];Hospital Authority Statistical Report. 2009 http://www.ha.org.hk/upload/publication_15/281.pdf.
- 32.Daniels MJ, Dominici F, Samet JM, Zeger SL. American journal of epidemiology. 2000;152:397–406. doi: 10.1093/aje/152.5.397. [DOI] [PubMed] [Google Scholar]
- 33.Samoli E, Analitis A, Touloumi G, Schwartz J, Anderson HR, Sunyer J, Bisanti L, Zmirou D, Vonk JM, Pekkanen J, Goodman P, Paldy A, Schindler C, Katsouyanni K. Environ. Health Perspect. 2005;113:88–95. doi: 10.1289/ehp.7387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pope CA, 3rd, Dockery DW. J. Air Waste Manage. Assoc. 2006;56:709–742. doi: 10.1080/10473289.2006.10464485. [DOI] [PubMed] [Google Scholar]
- 35.Wong CM, Vichit-Vadakan N, Kan H, Qian Z. Environ. Health Perspect. 2008;116:1195–1202. doi: 10.1289/ehp.11257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Smith KR, Peel JL. Environ Health Persp. 2010;118:1643–1645. doi: 10.1289/ehp.1002517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lai HK, Hedley AJ, Repace J, So C, Lu QY, McGhee SM, Fielding R, Wong CM. Thorax. 2011;66:615–623. doi: 10.1136/thx.2011.160291. [DOI] [PubMed] [Google Scholar]
- 38.Anenberg SC, Horowitz LW, Tong DQ, West JJ. Environ Health Persp. 2010;118:1189–1195. doi: 10.1289/ehp.0901220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.van Donkelaar A, Martin RV, Park RJ. J. Geophys. Res.: Atmos. 2006:111. [Google Scholar]
- 40.Kumar N, Chu A, Foster A. Atmos. Environ. 2007;41:4492–4503. doi: 10.1016/j.atmosenv.2007.01.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wang ZF, Chen LF, Tao JH, Zhang Y, Su L. Remote Sensing of Environment. 2010;114:50–63. [Google Scholar]
- 42.Glantz P, Kokhanovsky A, von Hoyningen-Huene W, Johansson C. Atmos. Environ. 2009;43:5838–5846. [Google Scholar]
- 43.Paciorek CJ, Liu Y. Environ. Health Perspect. 2009;117:904–909. doi: 10.1289/ehp.0800360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Liu Y, Koutrakis P, Kahn R. J. Air Waste Manage. Assoc. 2007;57:1351–1359. doi: 10.3155/1047-3289.57.11.1351. [DOI] [PubMed] [Google Scholar]
- 45.Liu Y, Koutrakis P, Kahn R, Turquety S, Yantosca RM. J. Air Waste Manage. Assoc. 2007;57:1360–1369. doi: 10.3155/1047-3289.57.11.1360. [DOI] [PubMed] [Google Scholar]
- 46.Paciorek CJ, Liu Y, Moreno-Macias H, Kondragunta S. Environ. Sci. Technol. 2008;42:5800–5806. doi: 10.1021/es703181j. [DOI] [PubMed] [Google Scholar]
- 47.Tian J, Chen DM. Remote Sensing of Environment. 2010;114:221–229. [Google Scholar]
- 48.Green M, Kondragunta S, Ciren P, Xu C. J. Air Waste Manage. Assoc. 2009;59:1082–1091. doi: 10.3155/1047-3289.59.9.1082. [DOI] [PubMed] [Google Scholar]
- 49.Li C, Hsu NC, Tsay SC. Atmos. Environ. 2011;45:3663–3675. [Google Scholar]
- 50.Di Nicolantonio W, Cacciari A. Ital. J. Remote Sens. 2011;43:97–109. [Google Scholar]
- 51.Gupta P, Christopher SA, Wang J, Gehrig R, Lee Y, Kumar N. Atmos. Environ. 2006;40:5880–5892. [Google Scholar]
- 52.Wang JL, Zhang YH, Shao M, Liu XL, Zeng LM, Cheng CL, Xu XF. J. Environ. Sci. 2006;18:475–481. [PubMed] [Google Scholar]
- 53.Abbey DE, Ostro BE, Fraser G, Vancuren T, Burchette RJ. J. Exposure Sci. Environ. Epidemiol. 1995;5:161–180. [PubMed] [Google Scholar]
- 54.Katsouyanni K, Samet JM, Anderson HR, Atkinson R, Le Tertre A, Medina S, et al. Res Rep Health Eff Inst. 2009:5–90. [PubMed] [Google Scholar]
- 55.Gasparrini A, Armstrong B, Kenward MG. Stat. Med. 2010;29:2224–2234. doi: 10.1002/sim.3940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Liistro G, Vanwelde C, Vincken W, Vandevoorde J, Verleden G, Buffels J. Chest. 2006;130:657–665. doi: 10.1378/chest.130.3.657. [DOI] [PubMed] [Google Scholar]
- 57.Dockery DW, Speizer FE, Ferris BG, Ware JH, Louis TA, Spiro A. Am. Rev. Respir. Dis. 1988;137:286–292. doi: 10.1164/ajrccm/137.2.286. [DOI] [PubMed] [Google Scholar]
- 58.Flouris AD, Metsios GS, Carrillo AE, Jamurtas AZ, Gourgoulianis K, Kiropoulos T, Tzatzarakis MN, Tsatsakis AM, Koutedakis Y. Am. J. Respir. Crit. Care Med. 2009;179:1029–1033. doi: 10.1164/rccm.200812-1920OC. [DOI] [PubMed] [Google Scholar]
- 59.Künzli N, Medina S, Kaiser R, Quenel P, Horak F, Jr, Studnicka M. Am. J. Epidemiol. 2001;153:1050–1055. doi: 10.1093/aje/153.11.1050. [DOI] [PubMed] [Google Scholar]
- 60.Bell ML, Samet JM, Dominici F. Annu. Rev. Public Health. 2004;25:247–328. doi: 10.1146/annurev.publhealth.25.102802.124329. [DOI] [PubMed] [Google Scholar]
- 61.Yang C, Peng X, Huang W, Chen R, Xu Z, Chen B, Kan H. Int Arch Occup Environ Health. 2012;85:579–585. doi: 10.1007/s00420-011-0707-7. [DOI] [PubMed] [Google Scholar]
- 62.Evans J, van Donkelaar A, Martin RV, Burnett R, Rainham DG, Birkett NJ, Krewski D. Environ. Res. 2013;120:33–42. doi: 10.1016/j.envres.2012.08.005. [DOI] [PubMed] [Google Scholar]
- 63.Burnett RT, Brook J, Dann T, Delocla C, Philips O, Cakmak S. Inhal Toxicol. 2000;12:15–39. doi: 10.1080/08958370050164851. [DOI] [PubMed] [Google Scholar]
- 64.Borja-Aburto VH, Castillejos M, Gold DR, Bierzwinski S, Loomis D. Environ. Health Perspect. 1998;106:849–855. doi: 10.1289/ehp.106-1533229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Zanobetti A, Schwartz J. Environ. Health Perspect. 2009;117:898–903. doi: 10.1289/ehp.0800108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Ostro BD, Broadwin R, Lipsett MJ. J. Exposure Anal. Environ. Epidemiol. 2000;10:412–419. doi: 10.1038/sj.jea.7500094. [DOI] [PubMed] [Google Scholar]
- 67.Schwartz J, Dockery DW, Neas LM. J. Air Waste Manage. Assoc. 1996;46:927–939. [PubMed] [Google Scholar]
- 68.Peters A, Skorkovsky J, Kotesovec F, Brynda J, Spix C, Wichmann HE, et al. Environ. Health Perspect. 2000;108:283–287. doi: 10.1289/ehp.00108283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Branis M, Vyskovska J, Maly M, Hovorka J. Inhalation Toxicol. 2010;22(2):21–28. doi: 10.3109/08958378.2010.504758. [DOI] [PubMed] [Google Scholar]
- 70.Peters A, Breitner S, Cyrys J, Stolzel M, Pitz M, Wolke G, et al. Res Rep Health Eff Inst. 2009;5–77:79–90. discussion. [PubMed] [Google Scholar]
- 71.Ostro B, Tobias A, Querol X, Alastuey A, Amato F, Pey J, et al. Environ. Health Perspect. 2011;119:1781–1787. doi: 10.1289/ehp.1103618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Tobias A, Perez L, Diaz J, Linares C, Pey J, Alastruey A, et al. Sci. Total Environ. 2011;412-413:386–389. doi: 10.1016/j.scitotenv.2011.10.027. [DOI] [PubMed] [Google Scholar]
- 73.Meister K, Johansson C, Forsberg B. Environ. Health Perspect. 2012;120:431–436. doi: 10.1289/ehp.1103995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Atkinson RW, Fuller GW, Anderson HR, Harrison RM, Armstrong B. Epidemiology. 2010;21:501–511. doi: 10.1097/EDE.0b013e3181debc88. [DOI] [PubMed] [Google Scholar]
- 75.Anderson HR, Bremner SA, Atkinson RW, Harrison RM, Walters S. ccup. Environ. Med. 2001;58:504–510. doi: 10.1136/oem.58.8.504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Simpson R, Williams G, Petroeschevsky A, Best T, Morgan G, Denison L, et al. Aust N Z J Public Health. 2005;29:205–212. [PubMed] [Google Scholar]
- 77.Chen R, Li Y, Ma Y, Pan G, Zeng G, Xu X, Chen B, Kan H. Sci. Total Environ. 2011;409:4934–4938. doi: 10.1016/j.scitotenv.2011.08.058. [DOI] [PubMed] [Google Scholar]
- 78.Venners SA, Wang B, Xu Z, Schlatter Y, Wang L, Xu X. Environ. Health Perspect. 2003;111:562–567. doi: 10.1289/ehp.5664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Chen BH, Kan HD, Chen RJ, Jiang SH, Hong CJ. J. Air Waste Manage. Assoc. 2011;61:1292–1299. [Google Scholar]
- 80.Ma Y, Chen R, Pan G, Xu X, Song W, Chen B, et al. Sci. Total Environ. 2011;409:2473–2477. doi: 10.1016/j.scitotenv.2011.03.017. [DOI] [PubMed] [Google Scholar]
- 81.Cao J, Xu H, Xu Q, Chen B, Kan H. Environ. Health Perspect. 2012;120:373–378. doi: 10.1289/ehp.1103671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Son JY, Lee JT, Kim KH, Jung K, Bell ML. Environ. Health Perspect. 2012;120:872–878. doi: 10.1289/ehp.1104316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Simpson R, Denison L, Petroeschevsky A, Thalib L, Williams G. J. Exposure Anal. Environ. Epidemiol. 2000;10:488–496. doi: 10.1038/sj.jea.7500137. [DOI] [PubMed] [Google Scholar]
- 84.Morgan GE, Corbett S, Wlodarczyk J, Lewis P. Am. J. Public Health. 1998;88:759–764. doi: 10.2105/ajph.88.5.759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Goldberg MS, Burnett RT, Bailar JC, Brook J, Bonvalot Y, Tamblyn R, et al. Environ. Res. 2001;86:26–36. doi: 10.1006/enrs.2001.4243. [DOI] [PubMed] [Google Scholar]
- 86.Ostro B, Feng WY, Broadwin R, Green S, Lipsett M. Environ. Health Perspect. 2007;115:13–19. doi: 10.1289/ehp.9281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Wilson WE, Mar TF, Koenig JQ. J. Exposure Anal. Environ. Epidemiol. 2007;17(2):S11–S19. doi: 10.1038/sj.jes.7500620. [DOI] [PubMed] [Google Scholar]
- 88.Slaughter JC, Kim E, Sheppard L, Sullivan JH, Larson TV, Claiborn C. J. Exposure Anal. Environ. Epidemiol. 2005;15:153–159. doi: 10.1038/sj.jea.7500382. [DOI] [PubMed] [Google Scholar]
- 89.Lippmann M, Ito K, Nadas A, Burnett RT. Res Rep Health Eff Inst. 2000;5–72:73–82. discussion. [PubMed] [Google Scholar]
- 90.Goldberg MS, Bailar JC, Burnett RT, Brook JR, Tamblyn R, Bonvalot Y, et al. Res Rep Health Eff Inst. 2000;7–113:115–120. discussion. [PubMed] [Google Scholar]
- 91.Ostro B, Broadwin R, Green S, Feng WY, Lipsett M. Environ. Health Perspect. 2006;114:29–33. doi: 10.1289/ehp.8335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Ueda K, Nitta H, Ono M. Circulation. 2009;73:1248–1254. doi: 10.1253/circj.cj-08-1149. [DOI] [PubMed] [Google Scholar]
- 93.Stolzel M, Breitner S, Cyrys J, Pitz M, Wolke G, Kreyling W, et al. J. Exposure Anal. Environ. Epidemiol. 2007;17:458–467. doi: 10.1038/sj.jes.7500538. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.