Summary
Background
Scrotal blunt trauma may result in injuries, such as testicular rupture, dislocation, torsion, hematoma, spermatic cord injury or contusion, and epididymal, scrotal, and urethral injuries. Ultrasonography (US) has a crucial role in the evaluation of those kinds of pathologies. Early diagnosis of testicular rupture may lead to the salvaging of the testicle by prompt surgical exploration within 72 h.
Case Report
A 21-year-old male with right scrotal swelling and pain complaints was admitted to another hospital one month ago. Epididymo-orchitis was diagnosed and the patient was given medical treatment. The patient was admitted to our emergency service with ongoing complaints. The patient stated that the pain and swelling suddenly developed after prolonged marching. On US, a large hematoma was detected between the leaves of the tunica vaginalis, and rupture from the lower pole was diagnosed. On color Doppler US, no vascularity was observed in the heterogeneous testicular parenchyma. Traumatic torsion was primarily suggested. Intraoperatively, an extratesticular hematoma, hematocele, and rupture were confirmed but torsion was not found. Because the hematoma entirely replaced the normal parenchyma, orchiectomy was performed.
Conclusions
Testicular rupture may occur even after moderate sportive action such as prolonged marching. If any delay occurs in diagnosis and/or operation, the coagulum may replace the entire parenchyma. We think that US and clinical findings may sometimes mislead the physicians and cause misdiagnoses, such as inflammation or torsion. In this paper, we present a complex delayed diagnosed example case of testicular rupture clinically mimicing epididymo-orchitis and radiologically mimicing traumatic testicular torsion.
MeSH Keywords: Hematocele; Spermatic Cord Torsion; Testicular Diseases; Ultrasonography; Ultrasonography, Doppler, Color
Background
Blunt trauma to the scrotum may result in testicular rupture, hematoma, or hematocele [1]. Ultrasonography (US) helps in assessing a trauma by confirming or excluding rupture and by differentiating hematoma from hematocele [1–3]. Gray-scale and especially color Doppler US are invaluable examinations to show the extent of the underlying injury. Early diagnosis of testicular rupture or ischemic compression due to large blood collection leads to prompt surgical exploration within 72 h and to the salvaging of the organ while preserving its function [1,4]. However, clinical and sonographic findings may sometimes misdirect physicians and make the diagnosis difficult, especially in delayed cases.
In this paper, we present a complex delayed diagnosed case with surgically proven large intra- and extratesticular hematoma, which occurred after a slight sportive activity, clinically mimicing epididymo-orchitis and radiologically mimicing traumatic testicular torsion.
Case Report
A 21-year-old male complaining of right scrotal swelling and pain was admitted to the urology department of another hospital one month ago. His laboratory data were within normal limits except for clear leucocytosis (24.000/mm3). The patient was diagnosed with epididymo-orchitis and given antibacterial and anti-inflammatory treatment. He was referred to the radiology department for US examination. The patient stated that he did not undergo the US examination because of a slight relief he felt after the treatment. The patient was admitted to our emergency service one month after his first visit and stated that the swelling did not disappear despite the treatment.
Upon physical examination that was conducted in our urology department, the right scrotum was diffusely swollen and tender but there was no color change or increase in heat. When the patient was asked carefully about the history of his complaints, the doctors learned that there was no history of a direct trauma. The patient stated that his pain and swelling suddenly developed after prolonged marching. Through serum chemistry, mild leucocytosis (12.400/mm3, 86% neutrophil dominance) was detected. Scrotal US examination was arranged for further evaluation.
Gray scale and color Doppler US examination was performed (Philips HD6, Philips Ultrasound Systems, Bothell, WA, USA; gray scale parameters; transducer frequency: 12-3 MHz, mechanic index: 1.2, thermal index soft tissue: 0.5, gain: 70%, dynamic range: 232 dB, frame rate: 19 Hz, depth 6 cm; Color Doppler parameters; transducer frequency: 5 MHz, scale: ±10 cm/sec, mechanic index: 0.6, thermal index soft tissue: 1.1, gain: 75%, frame rate: 8 Hz, depth: 6 cm). According to US, the left testicle was normal. However, in the right scrotum, there was a well-circumscribed, large, heterogeneous lesion consistent with an organized hematoma. The hematoma had the anteroposterior diameter of 2 cm, and a complicated hydrocele appearance between the leaves of the tunica vaginalis (Figure 1A, 1B). The normal-sized right testicle was nearly in the transvers orientation. Its parenchyma was prominently heterogeneous on the gray-scale examination, and no vascularity was detected on color Doppler US (Figure 2). At the inferior pole of the testicle, discontinuity in the tunica albuginea was seen, and rupture was diagnosed (Figures 1, 3). Moreover, based on the sonographic and clinical findings, delayed traumatic testicular torsion was mainly considered, and surgery was arranged.
Figure 1.
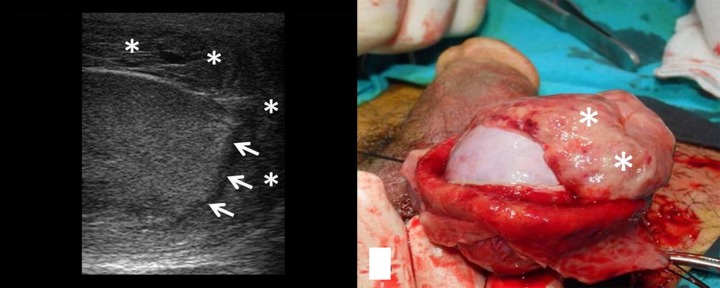
(A, B) The longitudinal gray-scale US image shows discontinuity in the tunica albuginea, which suggests rupture at the inferior pole of the testicle (arrows). A large, crescent-shaped, organized hematoma located between the leaves of the tunica vaginalis is readily seen in both US scan and corresponding intraoperative image (asterisks).
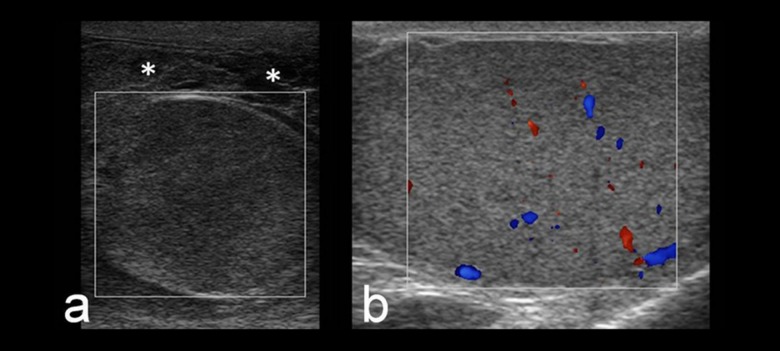
Figure 2.
The longitudinal color Doppler US image (A) shows no internal vascularity in the prominently heterogeneous–hypoechogeneic testicular parenchyma. On the other color Doppler US image (B), healthy left testicle with normal homogeneous parenchyma and internal vascularity is seen. The organized hematoma located between the leaves of the tunica vaginalis is also observed (asterisks).
Figure 3.
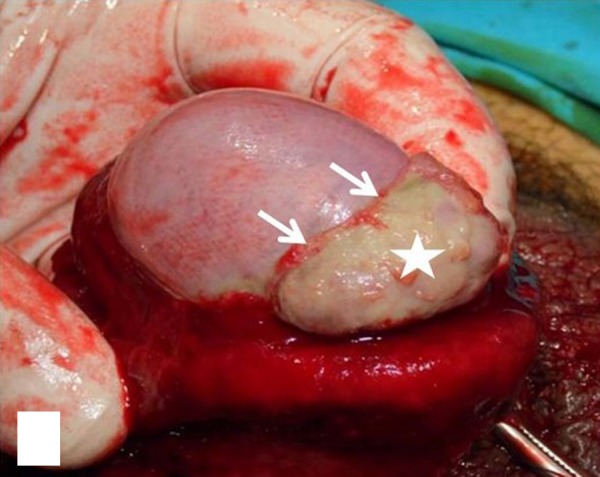
The rupture site (arrows) and the organized coagulum (pentagram) at the lower pole of the normal-colored testicle are observed in the corresponding intraoperative photo taken after cleaning the hematoma located between the leaves of the tunica vaginalis.
Intraoperatively, testicular prominent color change was not seen, and torsion was not found. A large extratesticular organized hematoma and hematocele were observed similar to the US. When the coagulum was gently removed, discontinuity of the tunica albuginea was seen at the inferior pole. The organized coagulum protruded from the testicle parenchyma directly from the ruptured site (Figure 3). The organized hematoma entirely replaced the normal testicular parenchyma. The testicle was as soft as a balloon. The upper pole of the parenchyma was necrotic. Orchiectomy was applied because of the lack of vascularity and the replacement of the normal parenchyma with the organized coagulum. Histopathological examination confirmed the coagulum and intense inflammatory chances in the testicular parenchyma.
Discussion
In the current paper, we presented a complex case of a surgically confirmed intra- and extratesticular hematoma that mimics clinically epididymo-orchitis and radiologically traumatic torsion. We believed that the diagnosis was delayed even if the urologist called for a US examination because the patient did not undergo the US examination immediately after his first visit to hospital. We considered the tear at the lower pole of the testicle and the hematoma to have expanded during the time interval between the patient’s first and second visit. The fact that no increased heat on the scrotal skin and no increased body temperature were observed is a beneficial clue for the condition to be disregarded as epididymo-orchitis. However, the existence of leucocytosis complicated the case. Heterogeneous and low echogenicity of the parenchyma and no internal vascularization in color Doppler US supported the torsion diagnosis. However, because of discontinuity at the inferior pole of the tunica albuginea, the presence of extratesticular hematoma, and the complicated hydrocele, we mainly considered traumatic testicular torsion. With those findings, orchiectomy was arranged, and testicular rupture associated with intra- and extratesticular hematoma was confirmed. The compression of extratesticular hematoma and replacement of the entire testicular parenchyma with hematoma were the reasons for the absence of internal vascularization. We also considered the secondary infection of hematocele and extratesticular hematoma to be the causes of leucocytosis.
The mobile and elastic structure of the scrotal tissues due to cremasteric muscle contraction and the thick tunica albuginea protect the male genital system from most injuries. However, when intrascrotal structures are forcefully compressed against the pubic rami or struck with objects moving at high velocities, severe injuries may occur [1].
Blunt testicular trauma may result from various kinds of injuries, such as testicular rupture, dislocation, torsion, hematoma, spermatic cord injury or contusion, and epididymal, scrotal, and urethral injuries. The tear in the tunica albuginea causes the seminiferous tubules to extrude into the tunica vaginalis sac, and hematocele may form. Moreover, a pole of the testis or the complete testis may be disrupted or shattered [5]. Testicular rupture is typically seen in patients with traumatic hematocele and is frequently overlooked [1].
Various studies have shown that exploring and evacuating blood clots and hematomas in the tunica vaginalis and repairing testicular tears increase testis salvage rates, decrease disability, hospital stay, and morbidity, and cause faster return of patients to normal activity compared with patients managed conservatively. Moreover, among patients managed conservatively, increased secondary infection of the hematocele or an injured testis was found. Subsequently, necrosis could occur with secondary infection, and the pressure effect of a large hematocele could cause atrophy of the testis. Conservative management in cases of contusion or rupture of the testis results in 45% failure rate and 45% orchidectomy rate compared with 9% orchidectomy rate in patients with testicular trauma who underwent early exploration and repair [6].
Inflammation of the epididymis is the most common cause of acute scrotum in adults. It is rarely seen in the pre-pubertal age. Only 20% of cases have additional orchitis. Physical examination varies from slight scrotal swelling to prominent edema, intense pain, fever, and pyuria. Differential diagnosis with acute torsion is sometimes difficult and needs further diagnostic tests, such as gray-scale and color Doppler US. During the first visit to hospital, epididymo-orchitis was diagnosed without US examination [4]. On the basis of the US that was performed in our department, we disregarded the cause to be inflammatory or infective because parenchymal vascularity did not increase, and intra- and extratesticular hematoma was observed. Based on those findings, we became distant from an inflammatory/infective cause despite the presence of leucocytosis.
Traumatic testicular torsion is another pathology that can be considered in our case. This entity has been rarely reported in the medical literature. Trauma history may result in a delay of accurate diagnosis [7]. In the current case, traumatic testicular torsion was our primary pre-diagnosis because of the patient’s history and US findings (discontinuity at the lower pole of the tunica albuginea and no vascularity inside the testicle parenchyma).
US of the scrotum is an important tool in the management of blunt scrotal trauma. Parenchymal heterogeneity or loss of normal interface between the testis and the tunica albuginea is the most important sign of testicular trauma [8]. Intratesticular hypoechogeneities may represent hematomas, extruded testicular parenchyma, or fragmented testis. US may help in evaluating blunt testicular trauma by confirming or excluding rupture and torsion and by differentiating a soft-tissue hematoma from a hematocele. Doppler US is useful in investigating the vascular status of the testis. Normal blood flow to the testis indicates that the vascular pedicle is intact and excludes the torsion [3]. Physical examination, together with US, increases the rate of accurate diagnoses. It is especially valuable when swelling and distortion due to trauma make the examination difficult [1]. In contrast to this information, US findings led us to a misdiagnosis of our case.
Conclusions
In conclusion, testicular rupture may occur even after moderate physical activity or prolonged marching. If the diagnosis is delayed, as in our case, the coagulum may replace the whole normal parenchyma. In this situation, we think that US and clinical findings may mislead the physicians and mimic different diseases, such as inflammation or torsion.
References
- 1.Micallef M, Ahmad I, Ramesh N, et al. Ultrasound features of blunt testicular injury. Injury. 2001;32:23–26. doi: 10.1016/s0020-1383(00)00083-8. [DOI] [PubMed] [Google Scholar]
- 2.Dogra VS, Gottlieb RH, Oka M, Rubens DJ. Sonography of the scrotum. Radiology. 2003;227:18–36. doi: 10.1148/radiol.2271001744. [DOI] [PubMed] [Google Scholar]
- 3.Patil MG, Onuora VC. The value of ultrasound in the evaluation of patients with blunt scrotal trauma. Injury. 1994;25:177–78. doi: 10.1016/0020-1383(94)90157-0. [DOI] [PubMed] [Google Scholar]
- 4.Pavlica P, Barozzi L. Imaging of the acute scrotum. Eur Radiol. 2001;11:220–28. doi: 10.1007/s003300000604. [DOI] [PubMed] [Google Scholar]
- 5.MacDermott JP, Gray BK, Stewart PA. Traumatic rupture of the testis. Br Urol. 1988;62:179–81. doi: 10.1111/j.1464-410x.1988.tb04303.x. [DOI] [PubMed] [Google Scholar]
- 6.Cass AS. Testicular trauma. J Urol. 1983;129:299–300. doi: 10.1016/s0022-5347(17)52062-5. [DOI] [PubMed] [Google Scholar]
- 7.Seng YJ, Moissinac K. Trauma induced testicular torsion: a reminder for the unwary. J Accid Emerg Med. 2000;17:381–82. doi: 10.1136/emj.17.5.381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wessells H, McAninch JW. Testicular trauma. Urology. 1996;47:750. doi: 10.1016/s0090-4295(96)00020-9. [DOI] [PubMed] [Google Scholar]