Abstract
AIM
To assess the safety and cosmetic efficacy of a new multiple noncontinuous transepithelial puncture technique for tattooing a decompensated cornea.
METHODS
It was a non-comparative clinical case series study. The study examines 33 eyes in 33 patients with total corneal opacity due to corneal decompensation, which developed following intraocular surgery. Corneal tattooing was performed using the multiple noncontinuous transepithelial puncture technique (i.e. pointage). The safety of this new surgical strategy was assessed by occurrence of adverse events for the follow-up period. The cosmetic efficacy was determined by the patient's cosmetic satisfaction and independent observer's opinion about patient appearance.
RESULTS
Seven women and 26 men were included in the study. The mean age was 46.4±17.5y (range: 7-67). In total, 30 of 33 patients (91%) reported cosmetic satisfaction within the follow-up period. Only 3 patients (9%) required additional tattooing due to cosmetic unsatisfaction. Cosmetic outcomes were analyzed and classified as excellent or good in 13 (39%) and 17 (52%) patients, respectively. No serious adverse events developed, except delayed epithelial healing in 3 cases.
CONCLUSION
The cosmetic outcomes of the multiple noncontinuous transepithelial puncture technique for corneal tattooing were good. The safety of this method is higher than conventional procedures. This new procedure also provides improved cost-effectiveness and safety over current corneal tattooing techniques.
Keywords: corneal tattooing, total corneal opacity, corneal decompensation
INTRODUCTION
Corneal decompensation can develops because of complications from ocular surgery, and total corneal edema and opacity tend to become permanent as part of the progression to irreversible corneal decompensation. Although corneal transplantation is the gold-standard treatment for corneal decompensation, various available treatment options include conjunctival flaps, anterior stromal puncture, amniotic membrane transplantation, phototherapeutic keratectomy, bandage contact lenses, hypertonic saline eye drops, and collagen cross-linking for symptomatic relief of corneal decompensation[1]. However, all these treatments cannot expect cosmetic improvement. Because of psychological stress, cosmetic management for corneal opacity is often considered, including iris-imprinted contact lenses and corneal tattooing with or without amniotic membrane transplantation[2]. Corneal tattooing has been considered for centuries not for visual improvement but for cosmetic improvement in decompensated eyes with poor visual potential[3]–[5]. It was recently reported that corneal tattooing can be used to reduce glare in defective irises and photopsia following peripheral iridotomy[6]–[8]. Classic corneal tattooing uses dyes that are applied to the anterior stroma following epithelial debridement or transepithelial needle puncture[3],[4]. Recently, numerous attempts to assess the efficacy of corneal tattooing have been made using mechanical microkeratome and femtosecond lasers[9]–[11]. For cosmetic purposes, physicians previously focused on homogeneously staining the cornea; therefore, numerous techniques have been introduced to stain the entire cornea. Infectious and granulomatous keratitis, persistent corneal epithelial defects, corneal ulceration, iridocyclitis, and toxic reactions have been reported following the application of corneal tattooing using conventional methods[3],[5],[12],[13]. Pointage technique, which was named after the painting technique originally created by Michel Eugene Chevreul; i.e. only black dots can be seen close-up, but the image can be observed when viewed from a distance.
In the present study, corneal tattooing was performed on patients with stable total corneal opacity due to corneal decompensation using the multiple noncontinuous transepithelial puncture (pointage) technique and the treated patients received follow-up examinations for 6y. Moreover, we assessed the safety and cosmetic efficacy of this new surgical strategy.
SUBJECTS AND METHODS
Subjects
Between June 2008 and July 2012, we performed tattooing on patients with stable total corneal opacity due to corneal decompensation. Patients who demonstrated no improvement in visual acuity or degree of corneal opacity for more than 1y were included. No affected eyes were able to detect hand motion at 30 cm. Nine eyes could detect hand motion, 5 eyes could perceive light, and 19 eyes could not perceive light. In all cases, iris-imprinted contact lenses were not tolerated. Patients were excluded if they did not demonstrate total corneal opacity. Only patients who received follow-up examinations for more than 1y following tattooing were included in this analysis. The study was approved by the Institutional Review Board of the Asan Medical Center at the University of Ulsan College of Medicine, Seoul, Republic of Korea. Informed consent was obtained before surgery and after the cosmetic purpose and possible complications were explained. The tenets of the Helsinki declaration were followed in this study.
Methods
Surgical procedures
After administering retrobulbar anesthesia, the procedure was performed on all patients by the same surgeon (Kim JY). A black carbon particle suspension dye was used (Mukhyang; Buyoung, Inc., Yongin Si, Korea) after sterilization in an autoclave at 134°C for 6min before surgery. The dye contained 200 nm-sized carbon black pigments (Orion Engineered Carbons Co. Ltd., Frankfurt, Germany). Under an operating microscope, the dye was transepithelially injected into the anterior stroma (without removing the epithelia) by beveled-down tangential puncture using a 30-gauge needle and 1 mL disposable syringe. Gentle injection was performed with the diameter of each point about 1.5 to 2 mm. The distance between points was about 1 mm. After each puncture, proper location of needle tip and dye spread in the anterior stroma was confirmed by irrigation using balanced salt solutions. When a thick fibrotic scar tissue in the corneal stroma was met, the puncture and injection through the fibrotic scar tissue were avoided and the fibrotic scar tissue remained dye-free area. Although the number of punctures varied depending on the condition of the cornea, the number never exceeded 30. Careful attention was taken to avoid corneal perforation. After the procedure, a therapeutic contact lens was placed on the eye.
Postoperative management and follow-up examinations
Postoperative topical therapy included topical antibiotic/corticosteroid (tobramycin/dexamethasone; Tobradex, Alcon Laboratories, Inc., Fort Worth, TX, USA) that was administered 4× per day for 1mo. The therapeutic lens was removed 3-7d after surgery when the cornea had reepithelialized without pain. Patients were examined on the first postoperative day, and then 1wk; 1, 3, 6mo, and 1y after surgery by the same observer (Kim JY). At the 1mo follow-up examination, anterior segment and facial photographs were taken for comparison with the preoperative appearance. Main outcomes were determined, including the patient's cosmetic satisfaction and the independent observer's opinion about patient appearance. The patients was subjectively asked if they were satisfied or not with the cosmetic outcome and the independent observer objectively evaluated the patient appearance using anterior segment and facial photographs as excellent (excellent cosmetic aspect), good (acceptable cosmetic aspect), or poor (unacceptable cosmetic aspect).
RESULTS
Patient Characteristics
A total of 33 eyes in 33 patients (7 women and 26 men) were included in the study. The mean age of the patients was 46.4±17.5 year-old (range: 7-67). The most common type of intraocular surgery prior to corneal decompensation was prior pars plana vitrectomy (70%; 23 of 33 eyes), followed by penetrating keratoplasty (21%; 7 of 33 eyes) and Ahmed valve implantation (9%; 3 of 33 eyes). Prior to intraocular surgery, all patients (except one) had been diagnosed with underlying diseases. The most common underlying disease prior to corneal decompensation was ruptured globe (55%; 18 of 33 eyes), followed by proliferative diabetic retinopathy (21%; 7 of 33 eyes), neovascular glaucoma (9%; 3 of 33 eyes), rhegmatogenous retinal detachment (6%; 2 of 33 eyes), congenital glaucoma (3%; 1 of 33 eyes), and aniridia (3%; 1 of 33 eyes). The associated systemic diseases included diabetes mellitus in 6 patients (18%), hypertension in 4 patients (12%), chronic renal failure in 1 patient (3%), angina in 1 patient (3%), and no systemic disease of in 21 patients (64%).
Surgical Outcomes
Most patients (91%; 30 of 33 patients) were satisfied with their postoperative cosmetic results. Only 3 of 33 patients (9%) were unhappy with their cosmetic results, and these individuals underwent additional corneal tattooing procedures. The cosmetic results determined by the independent observer were classified as excellent (excellent cosmetic aspect) in 13 patients (39%), good (acceptable cosmetic aspect) in 17 patients (52%), and poor (unacceptable cosmetic aspect) in 3 patients (9%). During 1y follow-up period, no serious adverse events developed, but 3 patients (9%) developed delayed corneal epithelial healing.
Selected Case Summaries
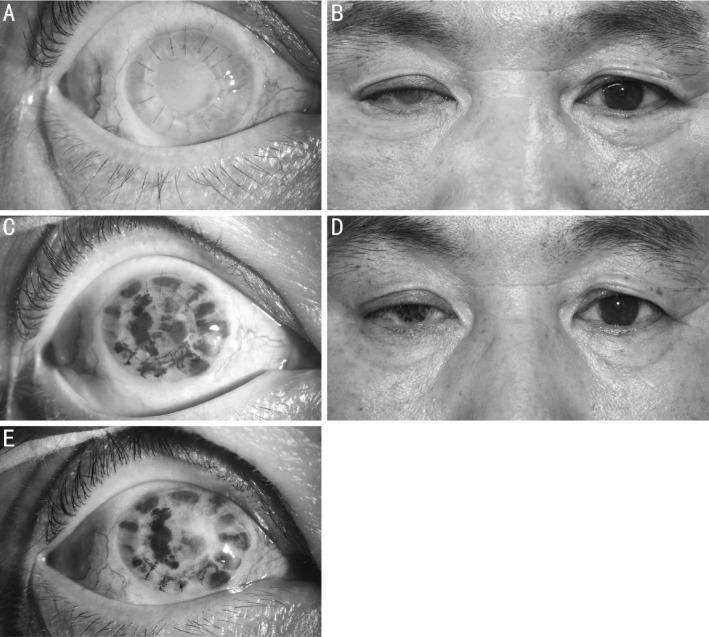
A 53 year-old male patient presented with a white opaque right eye on his first visit. He had undergone penetrating keratoplasty and pars plana vitrectomy with intravitreal silicone oil injection. Associated systemic diseases included diabetes mellitus and hypertension. Slit biomicroscopy demonstrated total corneal opacity due to corneal decompensation (Figure 1A, 1B). He was satisfied with his cosmetic appearance at 1mo (Figure 1C, 1D) and 1y postoperatively (Figure 1E), although the tattoing was slightly weakened at 1y postoperatively. No complications developed during the follow-up period.
Figure 1. Comparison between preoperative and postoperative slit-lamp biomicroscopic and facial photographs.
Preoperative slit-lamp biomicroscopic and facial photographs of selected patients with total corneal opacity (A, B). Postoperative slit-lamp biomicroscopy and facial photographs taken at 1mo postoperatively demonstrating excellent cosmetic improvement; however, the slit-lamp examinations demonstrated insufficient cosmetic improvement (C, D). At 12mo postoperatively, the slit-lamp biomicroscopy showed the tattooing was slightly weakened (E).
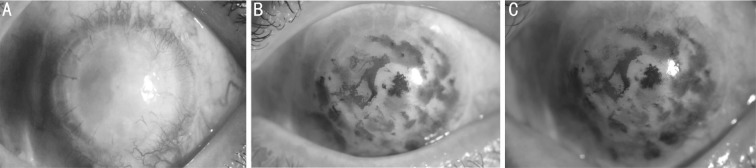
A 41-year-old male patient also presented with a totally white opaque right eye on his first visit. He had undergone penetrating keratopathy 14y ago, and wound repair and pars plana vitrectomy with intravitreal silicone oil injection due to ruptured globe after trauma 2y ago. Associated systemic disease included diabetes. The patient's right eye could not perceive light. Slit biomicroscopy demonstrated total corneal opacity due to corneal decompensation in his left eye (Figure 2A). After corneal tattooing using the multiple noncontinuous puncture, the patient was satisfied with his cosmetic appearance at 1mo (Figure 2B) and 6mo (Figure 2C) postoperatively. Adverse events never developed during the follow-up period.
Figure 2. Preoperative and postoperative slit lamp examinations.
Preoperative slit-lamp examination of selected patient. The total corneal opacity is shown (A). Postoperative slit-lamp examination of selected patient at 1mo (B) and 6mo (C) postoperatively. The slit-lamp examination demonstrated sufficient cosmetic improvements.
DISCUSSION
Although corneal transplantation is the first choice for treating corneal decompensation, this procedure can be challenging because of its high cost, long-term required use of medication, and risk of corneal failure or rejection. In addition, some cases of corneal decompensation that develop following intraocular surgery demonstrate poor visual potential due to the condition of the retina and optic nerve. In this study, 18 of 33 eyes presented with a history of ruptured globe. Although the use of iris-imprinted cosmetic contact lenses is the second option, it can be poorly tolerated and expensive. Thus, corneal tattooing can be an attractive option for patients with corneal decompensation.
For conventional corneal tattooing, the dyes are first embedded in the de-epithelialized corneal stroma[3]. However, decompensated cornea usually demonstrates epithelial-healing problems, which causes persistent epithelial defects and recurrent corneal erosion[14]. Second, the dyes are embedded in the pocket after constructing a lamellar stromal pocket[13]–[16]. However, scar tissue prevents the construction of a pocket. Recently, mechanical microkeratome and femtosecond lasers have been used to create the lamellar stromal pocket for corneal tattooing[9]–[11],[16]–[18]. Although femtosecond laser-assisted corneal tattooing demonstrates good efficacy and safety, it is very expensive[10]. Third, the transepithelial needle puncture technique was performed for corneal tattooing, which requires the creation of multiple punctures in the corneal stoma through the epithelium[4],[19]. This technique is both inexpensive and cosmetically effective. However, it also demonstrates several drawbacks, including risk of perforation and technical difficulty. Because it requires multiple, relatively long punctures, especially in cases of total corneal opacity with corneal decompensation, this technique leads to recurrent corneal erosions secondary to multiple lacerations in the Bowman's layer, excision of the scar tissue itself, epithelial ingrowth, irregular tattooing borders, and stain distribution[4],[12],[13],[19],[20]. Furthermore, infectious and granulomatous keratitis, persistent corneal epithelial defects, corneal ulceration, iridocyclitis, and toxic reactions can occur following the use of conventional transepithelial puncture techniques[3],[5],[12],[13]. According to our empiric observations, the progression of corneal ulceration may be caused by the dyes disturbing the nutrient flow between anterior and posterior corneal stroma. Instead, our present results confirm the safety of this new surgical strategy.
On the other hand, the possibility that the cosmetic efficacy of this new strategy is poorer than conventional methods must be considered. However, an important finding in our current study was that most patients were satisfied with the cosmetic result following multiple noncontinuous tattooing techniques; even though slit-lamp microscopic images of the cornea were considered cosmetically insufficient, facial photographs were cosmetically acceptable. As shown in Figure 1, the observer's opinion based on slit-lamp microscopic examination was classified as good, however facial photographs were considered excellent and patients were satisfied with the cosmetic results. Only 3 of 33 patients were unhappy with their results and needed additional corneal tattooing procedures. Our cosmetic outcome was comparable to that of previous literatures. Alio et al[21] reported 3 of 40 patients unsatisfied with cosmetic outcomes of the procedure using mineral micronized pigments in disfiguring corneal opacities or severe leukoma and they would consider having the surgery again. Kim et al[10] reported corneal tattooing technique using femtosecond laser and tissue marking black pigment dye in which 3 patients with total corneal opacity were enrolled and no patients required repeated surgery. Kim et al[19] performed homogenous transepithelial corneal tattooing using tissue marking black pigment dye, showing that 12 of 147 eyes (85 eyes of total opacity) were required repeated surgery. However, these two studies did not show patient's satisfaction.
According to a previous long-term study on the conventional method, the main problem with corneal tattooing is fading color over time: 12 of 147 patients developed faded color or opaque eyes following tattooing[19]. Therefore, our results suggest that the long-term fade rate is similar to earlier studies on the conventional method. Because there is no officially approved dye, various kind of dyes have been used, including India ink (India Ink Reagent Dropper; Fisher Scientific International, Inc., Cedex, France)[22], tissue marking dye (Davison Marking system, Bradely Products, Inc., Bloomington, MN, USA; or Nigrosin water soluble, Sigma-Aldrich Co, St. Louis, MO, USA)[2],[10], black tattoo pigment (Spaulding Color Corp, Voorheesville, NY, USA)[11], drawing ink (Rotring GmbH; Hamburg, Germany)[4], and mineral micronized pigments (Salvador Cordoba SL; registration No DGFPS 84-PH, Spanish Ministry of Health, 2001)[16]–[18],[23]. The dye type does not seem to affect the cosmetic results or complication rate.
The limitations of this study include the possibility of bias in the cosmetic results due to patient selection and subjective satisfaction ratings. Second, the new multiple noncontinuous puncture technique was not compared with the conventional corneal tattooing technique as a control group. Third, some aspects of our technique are not objective, because various modification can be followed according to the surgeon's preference and patient's cosmetic needs. Fourth, there is a need for a future prospective case-control study that compares the long-term safety and efficacy of conventional corneal tattooing and our new method.
In conclusion, our new corneal tattooing strategy, which uses the multiple noncontinuous puncture technique to treat total corneal opacity due to corneal decompensation, provides good cosmetic outcomes and excellent long-term safety.
Acknowledgments
Foundations: Supported by the Basic Science Research Program through the National Research Foundation of Korea (NRF) and funded by the Ministry of Education, Science, and Technology (MEST) (NRF-2010-0025662); the Asan Institute for Life Sciences, Seoul, Korea (2014-464).
Conflicts of Interest: Park JH, None; Um T, None; Kim MJ, None; Tchah H, None; Kim JY, None.
REFERENCES
- 1.Siu GD, Young AL, Jhanji V. Alternatives to corneal transplantation for the management of bullous keratopathy. Curr Opin Ophthalmol. 2014;25(4):347–352. doi: 10.1097/ICU.0000000000000062. [DOI] [PubMed] [Google Scholar]
- 2.Kim YK, Han YK, Wee WR, Lee JH, Kwon JW. 7 Cases of Combined Corneal Tattooing and Amniotic Membrane Transplantation in Bullous Keratopathy. J Korean Ophthalmol Soc. 2008;49(3):503–508. [Google Scholar]
- 3.Mannis MJ, Eghbali K, Schwab IR. Keratopigmentation: a review of corneal tattooing. Cornea. 1999;18(6):633–637. [PubMed] [Google Scholar]
- 4.Pitz S, Jahn R, Frisch L, Duis A, Pfeiffer N. Corneal tattooing: an alternative treatment for disfiguring corneal scars. Br J Ophthalmol. 2002;86(4):397–399. doi: 10.1136/bjo.86.4.397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.van der Velden/Samderubun EM, Kok JH. Dermatography as a modern treatment for coloring leucoma corneae. Cornea. 1994;13(4):349–353. doi: 10.1097/00003226-199407000-00011. [DOI] [PubMed] [Google Scholar]
- 6.Khan AO, Meyer D. Corneal tattooing for the treatment of debilitating glare in a child with traumatic iris loss. Am J Ophthalmol. 2005;139(5):920–921. doi: 10.1016/j.ajo.2004.10.048. [DOI] [PubMed] [Google Scholar]
- 7.Beekhuis WH, Drost BH, van der Velden/Samderubun EM. A new treatment for photophobia in posttraumatic aniridia: a case report. Cornea. 1998;17(3):338–341. [PubMed] [Google Scholar]
- 8.Gupta D, Broadway D. Cost-effective tattooing: the use of sterile ink for corneal tattooing after complicated peripheral iridotomies: an alternative to expensive salts. J Glaucoma. 2010;19(8):566–567. doi: 10.1097/IJG.0b013e3181ca771e. [DOI] [PubMed] [Google Scholar]
- 9.Fogla R, Gupta A, Indumathy TR. Microkeratome-assisted corneal tattooing: a case report. Cornea. 2010;29(4):446–448. doi: 10.1097/ICO.0b013e3181ae2560. [DOI] [PubMed] [Google Scholar]
- 10.Kim JH, Lee D, Hahn TW, Choi SK. New surgical strategy for corneal tattooing using a femtosecond laser. Cornea. 2009;28(1):80–84. doi: 10.1097/ICO.0b013e318181a83c. [DOI] [PubMed] [Google Scholar]
- 11.Kymionis GD, Ide T, Galor A, Yoo SH. Femtosecond-assisted anterior lamellar corneal staining-tattooing in a blind eye with leukocoria. Cornea. 2009;28(2):211–213. doi: 10.1097/ICO.0b013e3181859fbb. [DOI] [PubMed] [Google Scholar]
- 12.Sharma A, Gupta P, Dogra MR, Hidayat AA, Gupta A. Granulomatous keratitis following corneal tattooing. Indian J Ophthalmol. 2003;51(3):265–267. [PubMed] [Google Scholar]
- 13.Panda A, Mohan M, Chawdhary S. Corneal tattooing-experiences with “lamellar pocket procedure”. Indian J Ophthalmol. 1984;32(5):408–411. [PubMed] [Google Scholar]
- 14.Burris TE, Holmes-Higgin DK, Silvestrini TA. Lamellar intrastromal corneal tattoo for treating iris defects (artificial iris) Cornea. 1998;17(2):169–173. doi: 10.1097/00003226-199803000-00009. [DOI] [PubMed] [Google Scholar]
- 15.Remky A, Redbrake C, Wenzel M. Intrastromal corneal tattooing for iris defects. J Cataract Refract Surg. 1998;24(10):1285–1287. doi: 10.1016/s0886-3350(98)80215-0. [DOI] [PubMed] [Google Scholar]
- 16.Alio JL, Rodriguez AE, Toffaha BT. Keratopigmentation (corneal tattooing) for the management of visual disabilities of the eye related to iris defects. Br J Ophthalmol. 2011;95(10):1397–1401. doi: 10.1136/bjophthalmol-2011-300170. [DOI] [PubMed] [Google Scholar]
- 17.Alio JL, Rodriguez AE, Toffaha BT, El Aswad A. Femtosecond-assisted keratopigmentation double tunnel technique in the management of a case of Urrets-Zavalia syndrome. Cornea. 2012;31(9):1071–1074. doi: 10.1097/ICO.0b013e318243f6b1. [DOI] [PubMed] [Google Scholar]
- 18.Alio JL, Rodriguez AE, Toffaha BT, Pinero DP, Moreno LJ. Femtosecond-assisted keratopigmentation for functional and cosmetic restoration in essential iris atrophy. J Cataract Refract Surg. 2011;37(10):1744–1747. doi: 10.1016/j.jcrs.2011.08.003. [DOI] [PubMed] [Google Scholar]
- 19.Kim C, Kim KH, Han YK, Wee WR, Lee JH, Kwon JW. Five-year results of corneal tattooing for cosmetic repair in disfigured eyes. Cornea. 2011;30(10):1135–1139. doi: 10.1097/ICO.0b013e3181f2391a. [DOI] [PubMed] [Google Scholar]
- 20.Cronin KM, Meyer JC, Walter KA. Phototherapeutic keratectomy for treatment of long-term dye migration after corneal tattooing. Arch Ophthalmol. 2012;130(5):655–656. doi: 10.1001/archophthalmol.2011.1887. [DOI] [PubMed] [Google Scholar]
- 21.Alio JL, Sirerol B, Walewska-Szafran A, Miranda M. Corneal tattooing (keratopigmentation) with new mineral micronised pigments to restore cosmetic appearance in severely impaired eyes. Br J Ophthalmol. 2010;94(2):245–249. doi: 10.1136/bjo.2008.149435. [DOI] [PubMed] [Google Scholar]
- 22.Larrea X, De Courten C, Feingold V, Burger J, Buchler P. Oxygen and glucose distribution after intracorneal lens implantation. Optom Vis Sci. 2007;84(12):1074–1081. doi: 10.1097/OPX.0b013e31815b9dd6. [DOI] [PubMed] [Google Scholar]
- 23.Lee JE, Jun JB, Choi HY, Oum BS, Lee JS. Corneal tattooing to mask subsequent opacification after amniotic membrane grafting for stromal corneal ulcer. Acta Ophthalmol Scand. 2006;84(5):696–698. doi: 10.1111/j.1600-0420.2006.00680.x. [DOI] [PubMed] [Google Scholar]