Abstract
AIM
To determine the effectiveness of pharmacological and interventional treatment of hypotony and flat anterior chamber (FAC) resulting from glaucoma filtration surgery.
METHODS
We retrospectively examined the medical records of fifty-two trabeculectomy patients (52 eyes) who developed postoperative hypotony and FAC. The management and associated complications of hypotony, changing intraocular pressure (IOP) and best corrected visual acuity (BCVA) were evaluated.
RESULT
Of the 52 patients with hypotony, 29 (56%) had a grade 1 FAC, 21 (40%) had a grade 2 FAC, and only 2 had a grade 3 FAC. There was no significant difference between the mean preoperative IOP and the mean IOP at three and six months after surgery. Thirteen eyes (25%) required antiglaucomatous medication three months after surgery. The mean BCVA at 6mo after surgery was significantly reduced as compared with the mean preoperative BCVA.
CONCLUSION
Hypotonia and FAC following trabeculectomy are associated with troublesome complications that require pharmacological and/or surgical treatment. Thus, close follow-up is essential for affected patients.
Keywords: hypotony, flat anterior chamber, trabeculectomy
INTRODUCTION
Trabeculectomy is the most commonly performed and effective surgical method for treating medically uncontrolled glaucoma[1]–[3]. The complications of trabeculectomy include scarring, conjunctival leak, hypotony, choroidal detachments, infection, hyphema and malignant glaucoma[4]. Hypotony and flat anterior chamber (FAC) are frequent and significant complications that develop after trabeculectomy. In a study that included 1240 trabeculectomy patients, Edmunds et al[5] found that 23.9% of the patients had a FAC and 24.3% developed hypotony. A FAC usually but not always accompanies hypotony; it may also be associated with malignant glaucoma and choroidal effusion. Left untreated, hypotony and a FAC can lead to secondary complications, such as cataract formation, synechiae, persistent choroidal detachment or hypotony maculopathy[5],[6]. Hypotony and FAC have been treated with cycloplegic eye drops, a tightly applied eye patch and injection of sodium hyaluronate, air bubbles, perfluoropropane or sulfur hexafluoride gas into the anterior chamber[7],[8]. The aim of the present study was to compare the effectiveness of pharmacological and interventional treatment of hypotony and FAC after glaucoma filtration surgery.
SUBJECTS AND METHODS
We retrospectively analyzed the medical records of 352 trabeculectomy patients from the Okmeydani Education and Training Hospital. Fifty-two patients (52 eyes) who underwent an uneventful glaucoma filtration surgery without antifibrotic adjuvant and developed postoperative hypotony and FAC were included in the study. These patients had no leakage from the conjunctiva during the early postoperative period. Exclusion criteria included a postoperative follow-up period of less than 6mo, use of antifibrotic adjuvant during surgery, a combined trabeculectomy with phacoemulsification or had best corrected visual acuity (BCVA) of less than 1.0 as represented by the logarithm of the minimum angle of resolution (logMAR).
All of the surgeries were performed by the same surgeon, and all of the procedures conformed to the tenets of the Declaration of Helsinki. Of the 52 procedures, 38 of the trabeculectomies (73%) were performed under local anesthesia; the remaining operations (27%) were performed under general anesthesia. The fornix-based conjunctival flap approach followed by the creation of a rectangular scleral flap was used for all surgeries. All of the patients received the following postoperative treatments: topical prednisolone acetate every 2h for one week and then tapering over the next 4-6wk, antibiotics such as ofloxacin five times daily for two weeks or as needed and cyclopentolate twice daily for 1-2wk as needed. For patients with hypotony and FAC the topical prednisolone acetate application was decreased to four times daily. All antiglaucomatous medication was discontinued after surgery.
Preoperatively, all of the patients underwent a standard ophthalmic examination to determine BCVA, slit-lamp biomicroscopy to examine the anterior segment, optic nerve head and peripheral retina. Goldmann applanation tonometry was used to determine intraocular pressure (IOP). Patient follow-up occurred one day after surgery. The patients were not discharged until anterior chamber reformation and IOP recovery were achieved. All patients were examined at 1, 4wk and 3, 6mo after recovery. At each visit, the IOP was measured using Goldmann applanation tonometry, BCVA was determined, anterior and posterior segment examinations were performed. Hypotony was defined as having an IOP of less than 6 mm Hg. The severity of FAC was classified as follows: grade 1, just peripheral iridocorneal touch; grade 2, total iridocorneal touch but no lenticular touch and grade 3, corneal-lenticular touch[9].
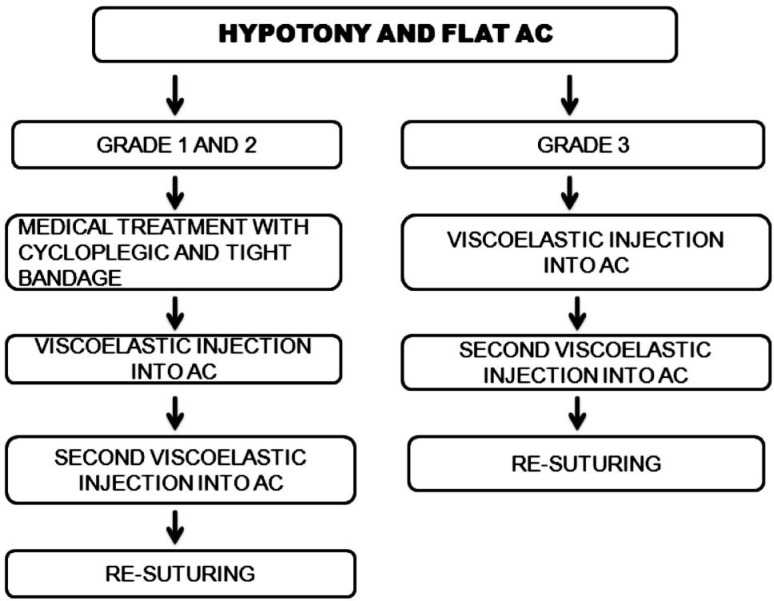
All of the patients with hypotony and FAC were managed based on our clinic's treatment algorithm which is shown in Figure 1.
Figure 1. Treatment algorithm.
All of the statistical analyses were performed using Statistical Package for of Social Sciences (SPSS, version 16). BCVA was converted to logMAR and analysis of variance (ANOVA) for repeated measurements was used to examine the changes in IOP and visual acuity. A P value of less than 0.05 was considered statistically significant.
RESULTS
The mean age of the patients with hypotony was 55±10.51y (range, 28-74). The participants included 28 female and 24 male patients. The mean follow-up time period after surgery was 34.3mo (range, 6-110mo). Of these 52 patients, 29 (56%) had a grade 1 FAC, 21 (40%) had a grade 2 FAC, and only 2 had a grade 3 FAC.
All of the patients received topical prednisolone acetate and ofloxacin: grade 1 patients also received topical cyclopentolate three times daily and a tight bandage was applied to their eyes. All of the patients with grade 1 FAC achieved normal IOP and their anterior chamber was formed in response to the reported treatment regimen. Only 3 of the 21 patients diagnosed with grade 2 FAC were effectively treated with medicine. For the patients in whom anterior chamber reformation was not achieved by topical treatment, viscoelastic injection was performed. Of these patients, eleven required a single injection of viscoelastic and six needed a second injection. One grade 2 patient who did not benefit from viscoelastic injection experienced rapid cataract formation and required phacoemulsification and secondary suturing. For one of the patients diagnosed with grade 3, 2 viscoelastic injections were sufficient to achieve anterior chamber reformation; the others underwent phacoemulsification and secondary suturing (Table 1).
Table 1. Treatment of hypotony according to grade of flat anterior chamber.
| Grade | Only medical therapy | Single injection of viscoelastic | Two injection of viscoelastic | Second surgery |
| Grade 1 (29) | 29 | 0 | 0 | 0 |
| Grade 2 (21) | 3 | 11 | 6 | 1 |
| Grade 3 (2) | 0 | 0 | 1 | 1 |
n
The mean preoperative IOP of the patients was 25.01±3.39 mm Hg (range, 20-37 mm Hg). In 30 of the patients, the preoperative IOP was between 20-24 mm Hg and 18 of these patients (60%) had a grade 1 FAC. In 22 patients the preoperative IOP was greater than 24 mm Hg and 11 of these patients (50%) had a grade 1 FAC. The mean IOP for all 52 patients was 3.82 mm Hg one day after surgery, 10.63±1.78 mm Hg (range, 7-14 mm Hg) 1mo postoperatively, 13.57±1.69 mm Hg (range, 10-19 mm Hg) 3mo postoperatively and 15.32±2.96 mm Hg 6mo postoperatively. There was a statistically significant difference between the mean preoperative IOP and the mean IOP one month postoperatively (P=0.023). However, there was no significant difference between the mean preoperative IOP and the mean IOP 3 or 6mo after surgery (P=0.203 and P=0.486, respectively).
The mean BCVA of the patients was 0.75±0.25 preoperatively and 0.68±0.29 and 0.54±0.28 at 1 and 6mo after surgery, respectively. The decrease in the mean BCVA at 6mo after surgery compared with the mean preoperative BCVA was statistically significant (P<0.001).
The most common complication, which was observed in 30 eyes (57.6%), was choroidal detachment. Of these 30 eyes, 19 (63.3%) of them had a grade 2 or 3 FAC. Of the patients with choroidal detachment, eighteen had a preoperative IOP higher than 24 mm Hg. Choroidal detachment was more severe in patients with a preoperative IOP greater than 24 mm Hg. Eighteen eyes (34.6%) presented with hyphema; 15 of these cases resolved spontaneously. For the remaining 3 hyphema cases an anterior chamber lavage was performed. Cataract progression was observed in 8 eyes (15.3%). Two of these cases developed during hypotony and required phacoemulsification to reform the anterior chamber. Six eyes (11.5%) developed macular edema, which resolved spontaneously one week after surgery, subsequently increasing the IOP. Macular hypotony caused decreased visual acuity in three of these eyes. For 13 eyes (25%), the use of antiglaucomatous medications was initiated three months postoperatively; the target IOP was achieved in 7 eyes using timolol maleate, in 2 eyes using travoprost, and in 4 eyes using a fixed combination of dorzolamid and timolol (Table 2).
Table 2. Complications of hypotony.
| Grade | Choroidal detachment (30) | Hyphema (18) | Cataract (8) | Hypotony maculopathy (6) | Postoperative use of antiglaucomatous medication (13) |
| Grade 1 | 11 | 8 | 1 | 0 | 4 |
| Grade 2 | 17 | 9 | 5 | 4 | 8 |
| Grade 3 | 2 | 1 | 2 | 2 | 1 |
n
DISCUSSION
Despite the use of modified techniques such as releasable sutures, laser suture lysis and/or the adjunctive use of intraoperative viscoelastic, hypotony remains one of the most frequent complications of trabeculectomy[10]–[12]. In a case series of trabeculectomies performed on 277 eyes, Törnqvist and Drolsum[13] reported that hypotony and FAC occurred in 16% of the trabeculectomies. Ridgway[14] reported an incidence of hypotony of 14.5% in 203 patients. In our series, the original 352 trabeculectomy patients whose records were retrospectively analayzed, the incidence of hypotony and FAC was 14.6%. de Barros et al[6] compared three methods of managing FAC and demonstrated that watchful waiting can still be advised; moreover, this research group suggested that reformation with viscoelastic is more likely to result in a satisfactory postoperative IOP than the use of medications alone. Hyung and Jung[15] reported that conservative therapy that included the use of topical antibiotics, a firmly applied eye patch and aqueous suppressants, was generally unsuccessful in treating hypotony with only a 20% success rate. Their low success rate is likely due to their use of mitomycine C during trabeculectomy. In our study, 61.5% of hypotony and FAC cases were effectively treated with pharmaceutical therapy and a tight bandage, 34.6% required viscoelastic injection, and only 3.9% required additional surgery such as phacoemulsification and suturing. The anterior chamber of all grade 1 FAC patients reformed within one week with pharmaceutical therapy and a tight bandage. Thus, we suggest watchful waiting for patients with a grade 1 FAC. The same treatment can be used for patients with a grade 2 FAC, but such patients must be monitored closely. Because grade 2 flattening may persist for a long time, sometimes progressively worsening to grade 3, we recommend the use of viscoelastic injection if it continues longer than 3d. If reformation cannot be achieved with viscoelastic injection, secondary suturing is required. Grade 3 FAC is an emergency condition that requires immediate surgery because it can result in corneal endothelial loss, cataract formation and anterior synechia[16],[17].
To our knowledge, there is limited published data regarding changes in the postoperative IOP in patients who develop hypotony and a FAC following trabeculectomy. Reformation of the anterior chamber via drainage of the choroidal effsion has been suggested for higher long-term trabeculectomy success especially for grade 2 FAC[6]. Kim and Jung[18] reported that a FAC may be detrimental to the postoperative course of trabeculectomy. Based on a case series study of trabeculectomy patients with FACs, Hosoda et al[8] suggested that injection of viscoelastic may be an effective treatment for FAC. However, the long term success rate was relatively low. In our study, the difference between the mean preoperative IOP and the mean IOP six months after surgery was not significant. Furthermore, 25% of the patients required antiglaucomatous medication indicating that trabeculectomy was unsuccessful in these patients. Of the patients in our study, 69.2% had a grade 2 or 3 FAC. We believe that this is due to peripheral anterior synechia formation and excessive scarring after surgical revision of the sclera flaps. Thus, the quick administiration of pharmaceutical therapy and surgical intervention will increase the success rate of trabeculectomy in patients with a grade 2 or 3 FAC.
Some changes in visual acuity can occur after glaucoma surgery. In a series of 301 eyes Francis et al[19] found that 170 eyes (56.5%) experienced transient vision loss and 24 eyes (8.0%) developed permanent vision loss. de Barros et al[6] reported that 45% of the patients in their study (15/33) lost two or more lines of visual acuity, and most of these patients required surgical intervention. In their study of hypotony treatments, Lee and Hyung[20] found that the difference between the mean preoperative and final follow-up visual acuity was not significant; however, three eyes (in two patients; 16.7%) experienced no restoration of preoperative BCVA. In our study, a significant difference was found between the mean preoperative BCVA and the mean BCVA 6mo after surgery. We believe this result is due to the vision-threatening complications of hypotony and FAC such as cataracts and maculopathy. Prolonged hypotony can cause irreversible chorioretinal folds due to fibrosis within the retina, choroids or sclera.
Glaucoma filtration surgery can result in serious complications, such as suprachoroidal hemorrhage or choroidal detachment, if hypotony develops[4],[21]. Kim and Jung[18] demonstrated that the incidences of cataract progression and choroidal detachment were higher in eyes with an FAC than in patient with a formed anterior chamber (50% versus 22.7% for cataract progression and 21.7% versus 4.2% for choroidal detachment). Hyung and Jung[15] reported that the incidence of hypotonic maculopathy was 9.4%. To prevent visual loss due to hypotonic maculopathy some reports in the literature have recommended immediate surgical intervention such as transconjunctival suturing of the scleral flap[22],[23].
In our study, the incidences of significant complications are as follows: choroidal detachment 57.6%, hyphema 34.6%, cataract progression 15.3% and maculopathy 11.5%. Hypotony can result in serious vision-threatening complications; therefore, prevention of hypotony is the preferred approach as compared to treating hypotony. Most patients who experienced complications in our study had a grade 2 or 3 FAC. Thus, in such patients, we do not recommend waiting to see if pharmaceutical therapy is effective; immediate surgical intervention is recommended.
The main limitations of our study include the retrospective design and lack of a control group. Further prospective and comparative studies are required to fully understand the effects of hypotony and its management.
In conclusion, hypotony and FAC are frequent and troubling complications of trabeculectomy. The majority of these cases can be treated pharmaceutically; however, surgery is inevitable for some patients. For such patients, close follow-up and timely intervention are essential.
Acknowledgments
Conflicts of Interest: Tunç Y, None; Tetikoglu M, None; Kara N, None; Sagdık HM, None; Özarpacı S, None; Elçioglu MN, None.
REFERENCES
- 1.Cairns JE. Trabeculectomy. Preliminary report of a new method. Am J Ophthalmol. 1968;66(4):673–679. [PubMed] [Google Scholar]
- 2.Hussain R, Clarke JC, Seah SK, Khaw PT. A review of trabeculectomy in East Asian people-the influence of race. Eye(Lond) 2005;19(3):243–252. doi: 10.1038/sj.eye.6701477. [DOI] [PubMed] [Google Scholar]
- 3.Heng Hah M, Norliza Raja Omar R, Jalaluddin J, Fadzillah Abd Jalil N, Selvathurai A. Outcome of trabeculectomy in hospital Melaka, Malaysia. Int J Ophthalmol. 2012;5(3):384–388. doi: 10.3980/j.issn.2222-3959.2012.03.26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Murdoch I. Post-operative management of trabeculectomy in the first three months. Community Eye Health. 2012;25(79–80):73–75. [PMC free article] [PubMed] [Google Scholar]
- 5.Edmunds B, Thompson JR, Salmon JF, Wormald RP. The National Survey of Trabeculectomy. III. Early and late complications. Eye(Lond) 2002;16(3):297–303. doi: 10.1038/sj.eye.6700148. [DOI] [PubMed] [Google Scholar]
- 6.de Barros DS, Navarro JB, Mantravadi AV, Siam GA, Gheith ME, Tittler EH, Baez KA, Martinez SM, Spaeth GL. The early flat anterior chamber after trabeculectomy: a randomized, prospective study of 3 methods of management. J Glaucoma. 2009;18(1):13–20. doi: 10.1097/IJG.0b013e31816f7647. [DOI] [PubMed] [Google Scholar]
- 7.Hoffman RS, Fine IH, Packer M. Stabilization of flat anterior chamber after trabeculectomy with Healon5. J Cataract Refract Surg. 2002;28(4):712–714. doi: 10.1016/s0886-3350(01)01092-6. [DOI] [PubMed] [Google Scholar]
- 8.Hosoda S, Yuki K, Ono T, Tsubota K. Ophthalmic viscoelastic device injection for the treatment of flat anterior chamber after trabeculectomy: a case series study. Clin Ophthalmol. 2013;7:1781–1785. doi: 10.2147/OPTH.S51165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Spaeth G. Glaucoma surgery. In: Saunders W, editor. Ophthalmic Surgery: Principles and Practice. 2nd ed. Philadelphia: 1990. p. 370. [Google Scholar]
- 10.Agarwal HC, Anuradha VK, Titiyal JS, Gupta V. Effect of intraoperative intracameral 2% hydroxypropyl methylcellulose viscoelastic during trabeculectomy. Ophthalmic Surg Lasers Imaging. 2005;36(4):280–285. [PubMed] [Google Scholar]
- 11.Aykan U, Bilge AH, Akin T, Certel I, Bayer A. Laser suture lysis or releasable sutures after trabeculectomy. J Glaucoma. 2007;16(2):240–245. doi: 10.1097/IJG.0b013e31802d6ded. [DOI] [PubMed] [Google Scholar]
- 12.Hornova J, Novakova D. Immediate and late intraocular pressure levels after trabeculectomy with releasable sutures. Cesk Slov Oftalmol. 2001;57(6):403–407. [PubMed] [Google Scholar]
- 13.Törnqvist G, Drolsum LK. Trabeculectomies. A long term study. Acta Ophthalmol (Copenh) 1991;69(4):450–454. doi: 10.1111/j.1755-3768.1991.tb02021.x. [DOI] [PubMed] [Google Scholar]
- 14.Ridgway AE. Trabeculectomy. A follow-up study. Br J Ophthalmol. 1974;58(7):680–686. doi: 10.1136/bjo.58.7.680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hyung SM, Jung MS. Management of hypotony after trabeculectomy with mitomycine. Korean J Ophthalmol. 2003;17(2):114–121. doi: 10.3341/kjo.2003.17.2.114. [DOI] [PubMed] [Google Scholar]
- 16.Smith DL, Skuta GL, Lindenmuth KA, Musch DC, Bergstrom TJ. The effect glaucoma filtering surgery on corneal endothelial cell density. Ophthalmic Surg. 1991;22(5):251–255. [PubMed] [Google Scholar]
- 17.Philips CT, Clar CV, Levy AM. Posterior synechiae after glaucoma operations: aggravation by shallow anterior chamber and pilocarpine. Br J Ophthalmol. 1987;71(6):428–432. doi: 10.1136/bjo.71.6.428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kim YY, Jung HR. The effect of flat anterior chamber on the success of trabeculectomy. Acta Ophthalmol Scand. 1995;73(3):268–272. doi: 10.1111/j.1600-0420.1995.tb00283.x. [DOI] [PubMed] [Google Scholar]
- 19.Francis BA, Hong B, Winarko J, Kawji S, Dustin L, Chopra V. Vision loss and recovery after trabeculectomy: risk and associated risk factors. Arch Ophthalmol. 2011;129(8):1011–1017. doi: 10.1001/archophthalmol.2011.182. [DOI] [PubMed] [Google Scholar]
- 20.Lee K, Hyung S. Effect of excision of avascular bleb and advancement of adjacent conjunctiva for treatment of hypotony. Korean J Ophthalmol. 2009;23(4):281–285. doi: 10.3341/kjo.2009.23.4.281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rahman A, Mendonca M, Simmons RB, Simmons RJ. Hypotony after glaucoma filtration surgery. Int Ophthalmol Clin. 2000;40(1):127–136. doi: 10.1097/00004397-200001000-00013. [DOI] [PubMed] [Google Scholar]
- 22.Letartre L, Basheikh A, Anctil JL, Des Marchais B, Goyette A, Kasner OP, Lajoie C. Transconjunctival suturing of the scleral flap for overfiltration with hypotony maculopathy after trabeculectomy. Can J Ophthalmol. 2009;44(5):567–570. doi: 10.3129/i09-123. [DOI] [PubMed] [Google Scholar]
- 23.Eha J, Hoffmann EM, Pfeiffer N. Long-term result after transconjunctival resulting of the scleral flap in hypotony following trabeculectomy. Am J Ophthalmol. 2013;155(5):864–869. doi: 10.1016/j.ajo.2012.12.004. [DOI] [PubMed] [Google Scholar]