Abstract
AIM
To evaluate the clinical findings of toxic keratopathy associated with abuse of topical anesthetics and the treatment efficacy of amniotic membrane transplantation (AMT).
METHODS
Fifteen eyes of 10 patients with abuse of topical anesthetics were included in this study. The data collected included patients' demographic information, initial best corrected visual acuity (BCVA), clinical findings, time to AMT, duration of epithelization, additional treatments, posttreatment BCVA, and the results of psychiatric examination.
RESULTS
All patients were male, with the mean age of 37.9±5.4y. The patients had received 0.5% proparacaine hydrochloride due to pain resulting from foreign bodies, such as welding flash burns and car battery explosions, for a mean of 18.2±12.4d. The mean initial BCVA of the patients was 0.069±0.100. All patients had persistent epithelial defects, stromal infiltration, ring ulcer, and corneal edema. Initially, medical treatment was attempted in all cases. Because of severe pain, persistent epithelial defects and progressing stromal thinning did not improve with medical treatment, thus, the patients underwent AMT. The mean posttreatment BCVA of the patients was 0.33±0.27. All of them, except for two patients, showed improved visual acuity. One patient underwent evisceration for corneal melting and endophthalmitis in another center, and one patient underwent evisceration for severe pain of unknown origin. All 5 patients who consented to a psychiatric examination had depression, had personality disorder, and used tobacco.
CONCLUSION
AMT appears to be an effective method for pain relief, rapid epithelial and stromal healing; however, visual prognosis is still poor despite medical and surgical interventions.
Keywords: amniotic membrane transplantation, ring stromal infiltration, topical anesthetic abuse, toxic keratopathy
INTRODUCTION
Topical anesthetics represent one of the most widely used groups of drugs in clinical practice, ranging from outpatient examination to major surgeries, such as cataract surgery. Cocaine was the first topical anesthetic agent used in the eye, which was subsequently followed by more potent and less toxic synthetic topical anesthetics such as tetracaine, oxybuprocaine, and proparacaine. Though these new generations of topical anesthetic agents are safe, their chronic and uncontrolled use results in toxic reactions, particularly to the cornea and ocular surface, which has been well defined in the literature[1]. A wide clinical spectrum of toxic reactions has been reported, ranging from punctate keratopathy, persistent epithelial defect, ring shaped stromal infiltration, corneal edema, Descemet's membrane folding, endothelial cell loss to neurotrophic ulcer, stromal melting, secondary infectious keratitis, corneal scarring, and corneal perforation[2],[3]. Patients may present with symptoms ranging from mild redness and lacrimation to severe photophobia and severe pain inconsistent with the clinical pattern. The discontinuation of topical anesthetics and the use of preservative-free topical medication yield satisfactory outcomes in patients with early diagnosis whereas permanent changes in the cornea lead to decreased vision and keratoplasty or even enucleation in patients with late diagnosis[2],[4].
This study evaluated clinical patterns of patients with toxic keratopathy undergoing amniotic membrane transplantation (AMT) associated with abuse of topical anesthetics, the efficacy of AMT in treatment, and psychiatric status of patients were evaluated.
SUBJECTS AND METHODS
Fifteen eyes of 10 patients who were referred to the Ophthalmology Department of Süleyman Demirel University between January 2009 and 2013 and who underwent AMT with the diagnosis of toxic keratopathy associated with abuse of topical anesthetics were included in this retrospective study. Prior to the study, informed consent was obtained from all subjects and ethical approval was granted by the ethics committee of our university. The study was conducted in accordance with the principles of the Declaration of Helsinki. The data obtained from medical records included patients' demographic information (age, gender, occupation, how the patient obtained the drug and how long and how often the patient used it), initial best corrected visual acuity (BCVA), clinical findings, time from AMT to the completion of epithelization, additional treatments, posttreatment BCVA and results of psychiatric examination. The patients were asked to rate their pain intensity from 0 (no pain) to 10 (worst possible pain) upon admission and following the AMT. In the psychiatric evaluation, all patients were diagnosed using Structured Clinical Interview for the Diagnostic and statistical manual of mental disorders (SCID) I for Axis I disorders, SCID II and Minnesota Multiphasic Personality Inventory (MMPI) for personality structures, and Beck depression inventory for depressive symptoms.
Patients' visual acuity was evaluated according to the Snellen chart and converted to the decimal system for statistical analysis. The data analysis was performed using SPSS for Windows, version 15 (SPSS Inc., Chicago, IL, USA). The data were expressed as the mean±SD for continuous variables and for the number of patients and as the percentages for categorical variables. To quantify the change in the pain, the patients were analyzed using paired t-test.
Preparation of Amniotic Membrane
Placenta was obtained under sterile conditions after elective caesarean delivery from pregnant women seronegative for hepatitis B, hepatitis C, syphilis, and HIV 1-2. The amniotic membrane (AM) was separated from the chorion via blunt dissection and was cleaned of blood clots with sterile saline solution. The AM separated from the chorion was kept in 1000 mL of sterile serum saline solution containing 800 000 IU of penicillin, 50 mg/mL of streptomycin, 500 mg/mL amicasin, and 2.5 mg/mL of amphotericin B. It was stored at +4°C for 24h and then flattened on sterile cellulose papers with the epithelial side up. The papers were then cut in pieces measuring 3×3-cm2 and stored at -80°C until their use.
Surgical Technique
After the loose corneal epithelium was scraped off with a cellulose sponge, the AM was placed the epithelial side up on the entire cornea and limbus and sutured continuously to the conjuctiva adjacent to the limbus using 10-0 nylon.
RESULTS
All patients were male, aged 30 to 43y (37.9±5.4y in average). All patients worked in auto assembly industry. The initiating event was the exposure to arc welding flash in 5 patients, metallic foreign body injury in 4 patients, and chemical injury by car battery explosion in 1 patient. All patients had been previously followed up with various diagnoses in various centers. One patient was referred to our clinic with the diagnosis of acanthamoeba keratitis, 2 with the diagnosis of bacterial keratitis, and others with the diagnosis of persistent epithelial defects. All patients reported having received Alcaine (0.5% proparacaine hydrochloride) (Alcon, Inc, Switzerland) with different intervals, ranging from once in every 10min to once in every one hour for 7-50d (mean, 18.2±12.4d). Regarding the way topical anesthetics were obtained, one patient reported that they their physician prescribed it while the others reported that they obtained it from pharmacy without prescription. Three patients had previously used the drug repeatedly for corneal foreign bodies. The most common complaints of patients were blurred vision, severe pain, photophobia, and lacrimation. The mean pain score of the patients upon admission was 9.1±8.8 (range 8-10). Pretreatment BCVA ranged from 0.008 to 0.400 (mean, 0.069±0.100). The patients had severe conjunctival injection, central or paracentral oval large epithelial defects, corneal edema, and complete or incomplete ring-shaped stromal infiltration and hypopyon. All patients were hospitalized. Corneal and conjuctival smears were obtained for microbiological examination. Patients stopped all medications, particularly topical anesthetic agents. They were treated with preservative-free artificial tears and 3rd or 4rd generation topical fluoroquinolone drops. Initial cultures revealed no growth. The patients were given systemic nonsteroidal anti-inflammatory agents for pain. One patient was discovered by hospital staff using Alcaine secretly on the 3rd day of hospitalization and one patient on the 4th day of hospitalization.
All patients underwent AMT for the absence of pain relief, corneal melting (in 3 patients), and non-healing epithelial defects (the remaining patients) after a mean of 6.7±0.8d (range 5-8d). The mean posttreatment pain score was 2.1±2.1 (range 1-8). The difference between pain scores on admission and in the posttreatment period was statistically significant (P<0.001, paired t-test).
AMT was performed twice in one eye of 2 patients and once in the remaining patients. All patients experienced relief in pain within one week after AMT. The mean time to complete epithelization after AMT was 17.7±3.9d (range 10-25d). Posttreatment BCVA ranged from 0 to 0.8 (0.33±0.27 in average). All patients, with the exception of two, showed improvement, though limited, in their visual acuity. One patient underwent evisceration for fungal keratitis and one for severe pain without origin on the non-functioning eye. The patients were followed up on an average of 6.8±2.5mo (range 3-11mo). Table 1 presents the summary of the findings.
Table 1. Clinical findings of patients.
| Case | Age | Laterality | Ocular history | Time of anesthetic abuse (d) | Initial BCVA | Posttreatment BCVA | Admission-AMT interval (d) | Epitelization period (d) | Psychiatric disorder | Follow-up (mo) |
| 1 | 40 | Left | Battery explosion | 16 | 0.4 | - | 7 | - | 4 | |
| 2 | 42 | Bilateral | Welding flash | 25 | CF/CF | 0.16/- | 7 | 25/- | Major depression (Beck depression: 34), severe impulse control disorder, antisocial personality disorder, homicidal behaviors | 11 |
| 3 | 41 | Left | Corneal foreign body | 11 | CF | 0.4 | 7 | 22 | Mild depression (Beck depression: 5), impulse control disorder, narcissistic personality disorder, anxiety disorder, homicidal behaviors | 8 |
| 4 | 36 | Bilateral | Welding flash | 50 | CF/CF | 0.2/0.3 | 6 | 15/18 | Major depression (Beck depression: 16), anxiety disorder, impulse control disorder | 6 |
| 5 | 43 | Bilateral | Welding flash | 18 | CF/CF | 0.1/0.2 | 7 | 18/20 | 6 | |
| 6 | 30 | Bilateral | Welding flash | 20 | CF/CF | 0.2/0.1 | 7 | 15/18 | Major depression (Beck depression: 39), social phobia, alcohol abuse, impulse control disorder | 9 |
| 7 | 42 | Left | Corneal foreign body | 10 | 0.1 | 0.7 | 7 | 10 | Mild depression (Beck depression: 5), impulse control disorder, borderline personality disorder | 7 |
| 8 | 30 | Left | Corneal foreign body | 15 | 0.1 | 0.5 | 6 | 21 | 9 | |
| 9 | 32 | Bilateral | Welding flash | 7 | CF/CF | 0.6/0.7 | 8 | 16/18 | 5 | |
| 10 | 43 | Right | Corneal foreign body | 10 | 0.16 | 0.8 | 5 | 14 | 3 |
BCVA: Best corrected visual acuity; AMT: Amniotic membrane transplantation; CF: Counting finger.
Five patients who consented to a psychiatric examination had smoking addiction and depression, which was major in 3, and impulse control disorder. Two patients with homicidal behavior were involved in criminal activities and one of them was put into prison. One patient had alcohol abuse. All patients had personality disorder based on the results of MMPI. Patients entered the therapy though the psychiatry clinic. It was found that during ongoing therapeutic interviews, patients' depressive symptoms improved and their compliance with keratopathy treatment improved.
Case 1
A 40-year old male patient was referred to our clinic with pain, photophobia, and reduced sight in both eyes. The patient worked as an electrician in an auto assembly industry. He had half-a-pack a day smoking habit. He reported that his eye had been exposed to chemicals as a result of car battery explosion and had been followed up with the diagnosis of bilateral infectious keratitis in a different center. Based on the clinical findings, topical anesthetic abuse was suspected in the patient and with an insistent questioning of drug use history. He reported having used topical anesthetics that he had obtained from pharmacy every half an hour for 16d. Corneal and conjunctival samples were obtained from both eyes. His visual acuity was counting fingers at 2 m in the right eye and 0.4 in the left eye, according to the Snellen chart. On examination, the right eye showed an epithelial defect measuring 5×5-mm2 (Figure 1A) whereas the left eye showed an epithelial defect measuring 9×9-mm2 in center of cornea (Figure 1B). Both eyes showed ring-shaped stromal infiltration, edema, and hypopyon. He was treated with 4th generation cephalosporin drop every hour, preservative-free artificial tears every hour, and systemic nonsteroidal anti-inflammatory agents. The hypopyon of the right eye resolved in a few days. His culture showed no growth. After the epithelial defect was closed on day 15, the patient was given topical steroids three times a day. The patient's visual acuity reached 0.1; however, he reported a decreased vision since childhood and amblyopia in the right eye. Even though hypopyon in the left eye had regressed, the patient underwent AMT due to non-healing epithelial defect on day 7. AMT was performed again because the amniotic melt during week 1. The patient experienced pain relief after the second AMT at week 1 (Figure 2A). On day 44, the patient presented with severe pain, purulent discharge, and corneal melting in the left eye. This patient was diagnosed with nummular keratitis (Figure 2B) and treated with topical fortified ceftazidime and vancomycin. New samples were obtained from the patient. The culture grew Aspergillus ssp and coagulase negative Staphylococcus. Topical and oral voriconazole was added to the treatment. Since an improvement could not be observed, the patient was guided to a center where the tectonic penetrating keratoplasty could be performed. In this center, evisceration was done to the patient after 1mo because of the melting in the cornea and endophthalmitis development as a result of the progression of infection into the intraocular region.
Figure 1. Clinical images of both eyes.
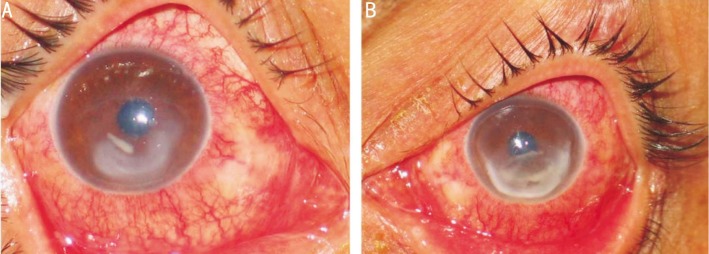
A: Conjunctival injection, large epithelial defect, stromal infiltrate in the right eye; B: Conjunctival injection, close to total large epithelial defect, stromal infiltrate, inferior corneal melting in the left eye.
Figure 2. Clinical images after AMT in the left eye.
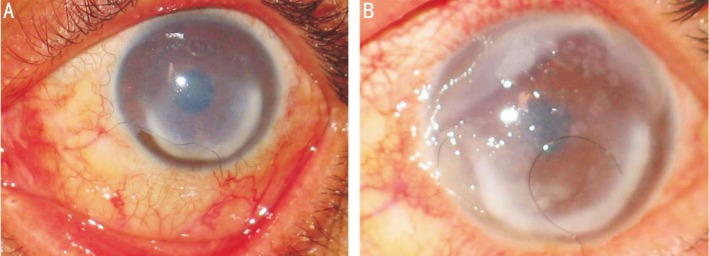
A: Clinical image of the left eye with AMT on the 28th day of treatment; B: Nummular keratitis condition on the 44th day of treatment.
Case 2
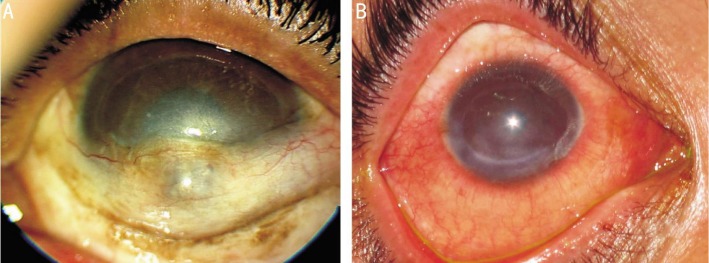
A 42-year old male patient was referred to our clinic with complaints of pain, blurred vision, lacrimation, photophobia, and blepharospasm as well as with the diagnosis of persistent epithelial defect. He reported to have been using Alcaine for severe pain after the exposure to welding flash, with intervals ranging from once in every 10min to once in every one hour for 25d. Samples were obtained from the patient. His visual acuity was counting fingers at 2m in the right eye and counting fingers at 1.5 m in the left eye. An examination showed conjunctival injection and large epithelial defects in both eyes (Figure 3). He was treated with 4th generation cephalosporin drops every 3h, preservative-free artificial tears per hour, and systemic nonsteroidal anti-inflamattory agents. Both eyes of the patient underwent AMT due to the absence of an improvement of the epithelial defect and severe pain on the 7th day of admission. The patient showed marked relief in pain and improvement in blepharospasm within the first week. Culture showed no growth. The AMs melt one month later. An examination revealed that the corneal epithelial defect improved bilaterally, however, bilateral ring shaped stromal infiltration persisted with widespread punctate epithelial staining. The patient underwent AMT on his left eye due to the onset of pain. The autologous serum eye drops were administered to the left eye. The AM melted 3wk later. The visual acuities were 0.1 in the right eye and counting fingers at 1 m in the left eye. The patient's complaints in the left eye were not alleviated. The patient did not re-attend repeat examinations for 3mo. Based on the results of biomicroscopic examination and information obtained from the patient, he had developed inferior corneal perforation of the left eye, and the hole in the cornea had been sealed up with a tissue adhesive and covered by the conjunctiva in a different center (Figure 4A). Right corneal leucoma was present (Figure 4B). The patient had intractable pain in the left eye. His visual acuities were 0.16 in the right eye with light perception in the left eye. Because of intractable pain, the patient insisted that his eye be removed. The patient's left eye was eviscerated. A psychiatric examination revealed severe major depression (Beck depression: 34) and severe impulse control disorder. The patient exhibited homicidal behaviors and became involved in criminal activities. A psychiatric examination and the results of the MMPI test revealed antisocial personality disorder.
Figure 3. Conjunctival injection and large epithelial defect at the right eye (A) and left eye (B).
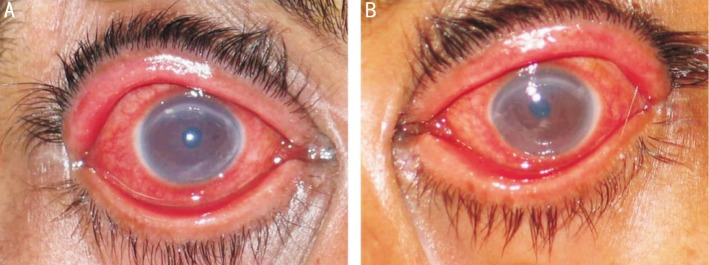
Figure 4. Clinical images of the left eye (A) and right eye (B) 6mo after the treatment.
DISCUSSION
The mechanisms through which topical anesthetic agents lead to toxic keratopathy remain unclear. One of the mechanisms suggests that topical anesthetics cause delayed healing of epithelial defects by exerting direct toxic effects on the epithelium, leading to delays in epithelial healing or non-healing of epithelial defects. An experimental and ultrastructural study designed to investigate the effects of topical anesthetics on the epithelium demonstrated that proparacaine at a concentration of 1.0 mmol/L caused abnormal morphology as well as abnormal distribution and orientation on cytoplasmic arrays of actin-rich stress fibers in epithelial cells, impairing epithelial cell migration and adhesion [5]. These effects were reversible at concentrations less than 0.01 mmol/L. The difference between single and repeated doses in the severity of toxicity was also significant. After a single dose of local anesthetic, the number of microvilli and microplicae decreased significantly. The intercellular spaces and the prominence of the cell nuclei with single dose application became disrupted whereas several applications resulted in greater toxicity, regular cell desquamation, and disruption to the plasma membrane and cytoplasm, an effect which also extends to deeper layers of the cornea [5]. Topical anesthetic agents produce a decrease in keratocyte viability by exerting direct cytotoxic effect [6]. The use of topical anesthetics impairs keratocyte and endothelial cell metabolisms such as glycolysis[7]. Na+/K+ pump in endothelial cells became impaired and osmotic pressure of the cornea increased, thus leading to stromal edema[7]. An examination of the corneal endothelium in a patient undergoing keratoplasty for topical anesthetic abuse by scanning laser microscopy revealed endothelial polymorphism, focal endothelial necrosis, and abnormalities in the intercellular junctions and apical attachment [8]. Specular microscopic examination of keratoplasty specimen from another case revealed a decreased cell count, presumably reflecting cell death and compensatory enlargement of surviving cells[9].
One of the assumptions put forward for toxicity is that topical anesthetic agents trigger the formation of antigen-antibody complex, resulting in ring shaped stromal infiltration[3]. Another assumption is that preservatives can cause toxic keratopathy or worsen the condition. Benzalkonium chloride, a preservative in Alcaine, exerts direct cell toxicity, damaging cytoplasmic membranes and cytoplasmic organelles and impeding metabolic cellular function. A concentration of 0.01% (the concentration used in Alcaine) benzalkonium chloride causes immediate cell retraction, cessation of normal cytokinesis and mitotic activity, and degeneration of human corneal epithelial cells within 2h. Benzalkonium chloride is toxic to all ocular tissues, including the corneal endothelium[10].
The use of topical anesthetic agents inhibits the conduction of corneal nerve impulses and loss of corneal sensation, resulting in decreased tear secretion, decreased blink reflex, and impaired tear film stability [11]. Excessive and prolonged use of anesthetic agents may damage the corneal nerves and lead to neurotrophic ulcers. The continued use of drugs promotes penetration of both anesthetic agents and preservatives into the anterior chamber and may cause toxic effect on intraocular tissues [7].
The prolonged use of topical anesthetics and persistent epithelial defect result in decay of corneal barrier function, facilitating the development of bacterial colonization and secondary infectious keratitis. In a study by Chern et al[12], cultures grew candida spp. in 3 patients and in a study by Kintner et al[13], cultures grew Streptococcus viridans in 2 patients. In the present study, culture grew Aspergillus spp. and coagulase negative Staphylococcus in one patient one month later.
Clinical pattern of anesthetic abuse keratopathy is quite confusing, unless the patient reports having used anesthetics. Pain and ring shaped stromal infiltration that are discordant with clinical state can be confused with acanthamoeba keratitis. Furthermore, fungal keratitis, varicella infection, properdin-mediated rings from bacteria (especially Pseudomonas and Escherichia coli), and recurrent corneal epithelial erosions may present a clinical picture similar to toxic keratopathy due to the abuse of Alcaine[14]. In this study, one patient was referred to our clinic with acanthamoeba keratitis and two patients with infectious keratitis.
A number of patients present with the symptoms of corneal, conjunctival foreign bodies, and ocular surface disorders. Why is drug-abuse not encountered in other patients? We believe the answer to this question lies in patients' personality traits. Psychiatric disturbances and psychoactive substance abuse are more common in topical anesthetic abusers[15]. In a report of 8 cases of toxic keratopathy by Yeniad et al[16], 4 patients had anxiety disorder and 1 had bipolar disease. Topical anesthetic abuse was reported in 2 patients with previous major depressive disorder[17]. A study by Katsimpris et al[4] reported two patients with suicide attempt. A report by Webber et al[9] reported that topical anesthetic abuse resulted in abuse of systemic opioids. It is noteworthy that 5 of all patients in our study who consented to undergo a psychiatric examination had moderate or severe psychiatric and personality disorders. Furthermore, the secret use of Alcaine during the treatment period in two of 10 patients supports severe addiction. It is probable that some other patients also received Alcaine secretly, resulting in the extension of treatment duration.
Impulse control disorders, personality disorders, depression, and anxiety disorders are common in the presence of substance abuse and substance addiction[18]. However, chronic pain has been found to be associated with a higher prevalence of mental co-morbidity, especially for anxiety disorders and depressive disorders, which were found to have prevalence rates of 20.9% and 12.7%, respectively[19]. Varion epidemiologic studies showed that the combination of social anxiety disorder and chronic pain is common, as seen in the cases presented in this study[20]. In addition, previous findings have indicated that pain related sensitivity can be common and exaggerated and that individuals with anxiety and depressive disorder as well as various personality disorders can respond anxiously to somatic sensations[21],[22]. It is noteworthy that severe pain is accompanied by major depressive disorder, social anxiety disorder, antisocial and borderline personality disorders, and alcohol abuse in the cases presented here. Thus, a psychiatric therapeutic approach similar to that utilized among those with other substance abuse problems should be adopted in topical anesthetic abusers. We believe that, as in this study, the therapy administered to patients can improve patient compliance with the treatment and can be effective in the management of pain and the elimination of drug abuse.
The cessation of topical anesthetic use is the first step of the treatment of toxic keratopathy. Given that preservatives can increase toxicity, it is crucial to use preservative free agents in the treatment. In this study, AMT was performed during the first 8d to accelerate epithelial and stromal healing and to reduce pain. AM comprised an avascular, hypocellular stroma, and an overlying basement membrane with a single layer of epithelial cells. It has immunological inertness and anti-inflammatory, anti-bacterial, anti-scarring, stem cell proliferating, and epithelialization promoting effects on the ocular surface. AMT has been successfully used in patients with persistent corneal epithelial defects, chronic corneal ulcers, and ocular surface burns[23],[24]. In the presence of intact limbus, AM increases epithelial cell migration to the basal membrane, reinforces the adhesion of the basal epithelium, stimulates cellular differentiation, and inhibits apoptosis. The AM has been reported to bring in epidermal growth factor, hepatocyte growth factor, and keratinocyte growth factor. Increased activity of the proteases secreted by keratocytes as well as polymorfonucleer leukocytes and damaged epithelial cells contribute to stromal destruction. Protease inhibitors in the AM inhibit the effect of these proteinases[25]. Furthermore, AM prevents the new epithelium from being influenced by eyelid movements and protects the cornea from the damaging effects of inflammatory cells and proteins in tears by building a physical barrier and acting as a biological contact lens, thus reducing pain[26]. In a study by Altinok et al[27], nonpreserved AMT was performed on both eyes of a patient, with bilateral toxic keratopathy caused by topical anesthetic abuse. Despite the achievement of rapid pain relief, the patient was left with corneal perforation in one eye and residual corneal scarring in the other eye. Hence, the patient was referred to another center for keratoplasty. In another study, AMT was performed in 8 eyes of 7 proparacaine abusers within 1-5d after the diagnosis. The study reported that in the third month after the AMT, the visual acuities varied between hand motions and 0.9 and all patients had corneal stromal opacities with varying densities[28]. This study observed a dramatic relief in pain within the first week, epithelial improvement in all but two patients, and no vascularization of the cornea during the follow up period.
The prognosis in these patients varied according to how long and how often topical anesthetic agents have been used. Even though satisfactory outcomes have been reported with medical treatment in some patients in the literature[9], in some cases, keratoplasty was performed to preserve the integrity of the globe[13] or enucleation was performed because of treatment failure[15]. The severity of stromal scarring after healing is the most important cause of decreased vision. Two patients underwent evisceration in this study. Visual acuity due to stromal scarring was on an average 0.33±0.27 in the remaining patients.
Toxic keratopathy associated with the abuse of topical anesthetics should be kept in mind in terms of clinical picture in the differential diagnosis of ring-shaped stromal infiltrate and other pathologies causing ulcer. It is important for community health because of its potential to cause visual loss and because of being preventable. AMT promotes corneal epithelial healing, decreases stromal scarring, and produces rapid relief of pain. The resolution of pain, which appears to be the triggering factor in these patients, seems to be the most important factor in treatment. The application of AMT in the early period in patients with severe pain will promote treatment compliance and have a positive effect on the patient's confidence in the physician. The presence of severe psychiatric problems, such as depression, personality disorder, impulse control disorder, and substance and alcohol addiction, underlies the importance of psychiatric examination in these patients. Particularly the impaired impulse control may prompt these patients to continue using Alcaine, and it may impair their treatment compliance. Therefore, we consider that the addition of psychiatric evaluation to the treatment protocol in similar patient groups can contribute a great deal to the treatment in terms of prognosis.
Acknowledgments
Conflicts of interest: Tok OY, None; Tok L, None; Atay IM, None; Argun TC, None; Demirci N, None; Gunes A, None.
REFERENCES
- 1.Grant RL, Acosta D. Comparative toxicity of tetracaine, proparacaine and cocaine evaluated with primary cultures of rabbit corneal epithelial cells. Exp Eye Res. 1994;58(4):469–478. doi: 10.1006/exer.1994.1040. [DOI] [PubMed] [Google Scholar]
- 2.Yagci A, Bozkurt B, Egrilmez S, Palamar M, Ozturk BT, Pekel H. Topical anesthetic abuse keratopathy: a commonly overlooked health care problem. Cornea. 2011;30(5):571–575. doi: 10.1097/ico.0b013e3182000af9. [DOI] [PubMed] [Google Scholar]
- 3.Chen HT, Chen KH, Hsu WM. Toxic keratopathy associated with abuse of low dose anesthetic: a case report. Cornea. 2004;23(5):527–529. doi: 10.1097/01.ico.0000114127.63670.06. [DOI] [PubMed] [Google Scholar]
- 4.Katsimpris JM, Sarantoulakou M, Kordelou A, Petkou D, Petropoulos IK. Clinical findings in patients with topical anaesthetic abuse keratitis: a report of five cases. Klin Monbl Augenheilkd. 2007;224(4):303–308. doi: 10.1055/s-2007-962933. [DOI] [PubMed] [Google Scholar]
- 5.Dass BA, Soong HK, Lee B. Effects of proparacaine on actin cytoskeleton of corneal epithelium. J Ocul Pharmacol. 1988;4(3):187–194. doi: 10.1089/jop.1988.4.187. [DOI] [PubMed] [Google Scholar]
- 6.Moreira LB, Kasetsuwan N, Sanchez D, Shah SS, LaBree L, McDonnell PJ. Toxicity of topical anesthetic agents to human keratocytes in vivo. J Cataract Refract Surg. 1999;25(7):975–980. doi: 10.1016/s0886-3350(99)00075-9. [DOI] [PubMed] [Google Scholar]
- 7.Penna EP, Tabbara KF. Oxybuprocaine keratopathy: a preventable disease. Br J Ophthalmol. 1986;70(3):202–204. doi: 10.1136/bjo.70.3.202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Risco JM, Millar LC. Ultrastructural alterations in the endothelium in a patient with topical anesthetic abuse keratopathy. Ophthalmology. 1992;99(4):628–633. doi: 10.1016/s0161-6420(92)31926-8. [DOI] [PubMed] [Google Scholar]
- 9.Webber SK, Sutton GL, Lawless MA, Rogers CM. Ring keratitis from topical anaesthetic misuse. Aust N Z J Ophthalmol. 1999;27(6):440–442. doi: 10.1046/j.1440-1606.1999.00246.x. [DOI] [PubMed] [Google Scholar]
- 10.Eleftheriadis H, Cheong M, Sandeman S, Syam PP, Brittain P, Klintworth GK, Lloyd A, Liu C. Corneal toxicity secondary to inadvertent use of benzalkonium chloride preserved viscoelastic material in cataract surgery. Br J Ophthalmol. 2002;86(3):299–305. doi: 10.1136/bjo.86.3.299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rosenwasser GO. Complications of topical ocular anesthetics. Int Ophthalmol Clin. 1989;29(3):153–158. doi: 10.1097/00004397-198902930-00005. [DOI] [PubMed] [Google Scholar]
- 12.Chern KC, Meisler DM, Wilhelmus KR, Jones DB, Stern GA, Lowder CY. Corneal anesthetic abuse and Candida keratitis. Ophthalmology. 1996;103(1):37–40. doi: 10.1016/s0161-6420(96)30735-5. [DOI] [PubMed] [Google Scholar]
- 13.Kintner JC, Grossniklaus HE, Lass JH, Jacobs G. Infectious crystalline keratopathy associated with topical anesthetic abuse. Cornea. 1990;9(1):77–80. [PubMed] [Google Scholar]
- 14.Theodore FH, Jakobiec FA, Juechter KB, Ma P, Troutman RC, Pang PM, Iwamoto T. The diagnostic value of a ring infiltrate in acanthamoebic keratitis. Ophthalmology. 1985;92(11):1471–1479. doi: 10.1016/s0161-6420(85)33830-7. [DOI] [PubMed] [Google Scholar]
- 15.Rosenwasser GO, Holland S, Pflugfelder SC, Lugo M, Heidemann DG, Culbertson WW, Kattan H. Topical anesthetic abuse. Ophthalmology. 1990;97(8):967–972. doi: 10.1016/s0161-6420(90)32458-2. [DOI] [PubMed] [Google Scholar]
- 16.Yeniad B, Canturk S, Esin Ozdemir F, Alparslan N, Akarcay K. Toxic keratopathy due to abuse of topical anesthetic drugs. Cutan Ocul Toxicol. 2010;29(2):105–109. doi: 10.3109/15569521003631752. [DOI] [PubMed] [Google Scholar]
- 17.Ansari H, Garibaldi DC, Jun AS. Anaesthetic abuse keratopathy as a manifestation of ocular Munchausen's syndrome. Clin Experiment Ophthalmol. 2006;34(1):81–83. doi: 10.1111/j.1442-9071.2006.01152.x. [DOI] [PubMed] [Google Scholar]
- 18.Wu LT, Gersing K, Burchett B, Woody GE, Blazer DG. Substance use disorders and comorbid Axis I and II psychiatric disorders among young psychiatric patients: findings from a large electronic health records database. J Psychiatr Res. 2011;45(11):1453–1462. doi: 10.1016/j.jpsychires.2011.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gerhardt A, Hartmann M, Schuller-Roma B, Blumenstiel K, Bieber C, Eich W, Steffen S. The prevalence and type of Axis-I and Axis-II mental disorders in subjects with non-specific chronic back pain: results from a population-based study. Pain Med. 2011;12(8):1231–1240. doi: 10.1111/j.1526-4637.2011.01190.x. [DOI] [PubMed] [Google Scholar]
- 20.Kroenke K, Outcalt S, Krebs E, Bair MJ, Wu J, Chumbler N, Yu Z. Association between anxiety, health-related quality of life and functional impairment in primary care patients with chronic pain. Gen Hosp Psychiatry. 2013;35(4):359–365. doi: 10.1016/j.genhosppsych.2013.03.020. [DOI] [PubMed] [Google Scholar]
- 21.Carleton RN, Abrams MP, Asmundson GJ, Antony MM, McCabe RE. Pain-related anxiety and anxiety sensitivity across anxiety and depressive disorders. J Anxiety Disord. 2009;23(6):791–798. doi: 10.1016/j.janxdis.2009.03.003. [DOI] [PubMed] [Google Scholar]
- 22.Thibodeau MA, Welch PG, Katz J, Asmundson GJ. Pain-related anxiety influences pain perception differently in men and women: a quantitative sensory test across thermal pain modalities. Pain. 2013;154(3):419–426. doi: 10.1016/j.pain.2012.12.001. [DOI] [PubMed] [Google Scholar]
- 23.Arora R, Mehta D, Jain V. Amniotic membrane transplantation in acute chemical burns. Eye (Lond) 2005;19(3):273–278. doi: 10.1038/sj.eye.6701490. [DOI] [PubMed] [Google Scholar]
- 24.Nubile M, Dua HS, Lanzini TE, Carpineto P, Ciancaglini M, Toto L, Mastropasqua L. Amniotic membrane transplantation for the management of corneal epithelial defects: an in vivo confocal microscopic study. Br J Ophthalmol. 2008;92(1):54–60. doi: 10.1136/bjo.2007.123026. [DOI] [PubMed] [Google Scholar]
- 25.Sippel KC, Ma JJ, Foster CS. Amniotic membrane surgery. Curr Opin Ophthalmol. 2001;12(4):269–281. doi: 10.1097/00055735-200108000-00006. [DOI] [PubMed] [Google Scholar]
- 26.Kruse FE, Rohrschneider K, Völeker HE. Multilayer amniotic membrane transplantation for reconstruction of deep corneal ulcers. Ophthalmology. 1999;106(8):1504–1511. doi: 10.1016/S0161-6420(99)90444-X. [DOI] [PubMed] [Google Scholar]
- 27.Altinok AA, Balikoglu M, Sen E, Serdar K. Nonpreserved amniotic membrane transplantation for bilateral toxic keratopathy caused by topical anesthetic abuse: a case report. J Med Case Rep. 2010;4:262. doi: 10.1186/1752-1947-4-262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Burcu A, Dogan E, Yalniz-Akkaya Z, Ornek F. Early amniotic membrane transplantation for toxic keratopathy secondary to topical proparacaine abuse: a report of seven cases. Cutan Ocul Toxicol. 2013;32(3):241–247. doi: 10.3109/15569527.2012.759959. [DOI] [PubMed] [Google Scholar]


