Abstract
Importance
Detailed, nationally-representative data describing high-risk populations and circumstances involved in insulin-related hypoglycemia and errors (IHEs) can inform approaches to individualizing glycemic targets.
Objective
Describe U.S. burden, rates, and characteristics of emergency department (ED) visits and emergent hospitalizations for IHEs.
Design
Nationally-representative, public health surveillance of adverse drug events and a national, household survey of insulin use.
Setting
National Electronic Injury Surveillance System—Cooperative Adverse Drug Event Surveillance (NEISS-CADES), 2007–2011 and National Health Interview Survey (NHIS), 2007–2011.
Participants
Insulin-treated patients seeking ED care.
Main outcome(s) and Measures
Estimated annual numbers and estimated annual rates of ED visits and hospitalizations for IHEs among insulin-treated patients with diabetes.
Results
Based on 8,100 cases, an estimated 97,648 (95% confidence interval [CI], 64,410–130,887) ED visits for IHEs occurred annually; almost one-third (29.3% [CI, 21.8%–36.8%]) resulted in hospitalization. Severe neurologic sequelae were documented in an estimated 60.6% (CI, 51.3%–69.9%) of ED visits for IHEs, and glycemic levels ≤50 mg/dL were recorded in over one-half of cases (53.4%). Insulin-treated patients aged ≥80 years were more than twice as likely to visit the ED (rate ratio, 2.5; CI, 1.5–4.3) and nearly five times as likely to be subsequently hospitalized (rate ratio, 4.9; CI, 2.6–9.1) for IHEs than those aged 45–64 years. The most commonly-identified IHE precipitants were reduced food intake and administration of the wrong insulin product.
Conclusions and Relevance
Rates of ED visits and subsequent hospitalizations for IHEs were highest in patients aged ≥80 years; the risks of hypoglycemic sequelae in this age group should be considered in decisions to prescribe and intensify insulin. Meal-planning and insulin product mix-up misadventures are important targets for hypoglycemia prevention efforts.
Insulin is a cornerstone of Type 1 diabetes mellitus (T1DM) treatment and is increasingly introduced early in the treatment course for patients with Type 2 DM (T2DM), who account for 90% to 95% of new DM cases annually.1 Over the last decade, the number of U.S. patients with insulin-treated DM rose 50%; one-third of patients with diabetes currently use insulin,2 and in 2012, insulin was estimated to cost the U.S. healthcare system approximately $6 billion.3 Tight glycemic control with insulin has been associated with reductions in disease complications among patients with T1DM,4 but has been increasingly associated with harms among patients with T2DM.5–7 Insulin remains one of the most challenging and limiting aspects of DM medical management owing to complexities in dosing and administration, as well as need for routine monitoring of blood glucose (BG) and food intake to avoid potentially fatal hypoglycemia.8 The risk of insulin-related hypoglycemia is an important consideration when choosing among treatment options and individualizing glycemic targets, particularly in patients for whom benefits of intensive control may not be as likely realized.9, 10
We used recent, nationally-representative data to estimate the burden and rates of insulinrelated hypoglycemia and errors (IHEs) resulting in emergency department (ED) visits and subsequent hospitalizations, and identify high-risk groups and precipitating factors for IHEs.
METHODS
DATA SOURCES & COLLECTION METHODS
Numerator Data
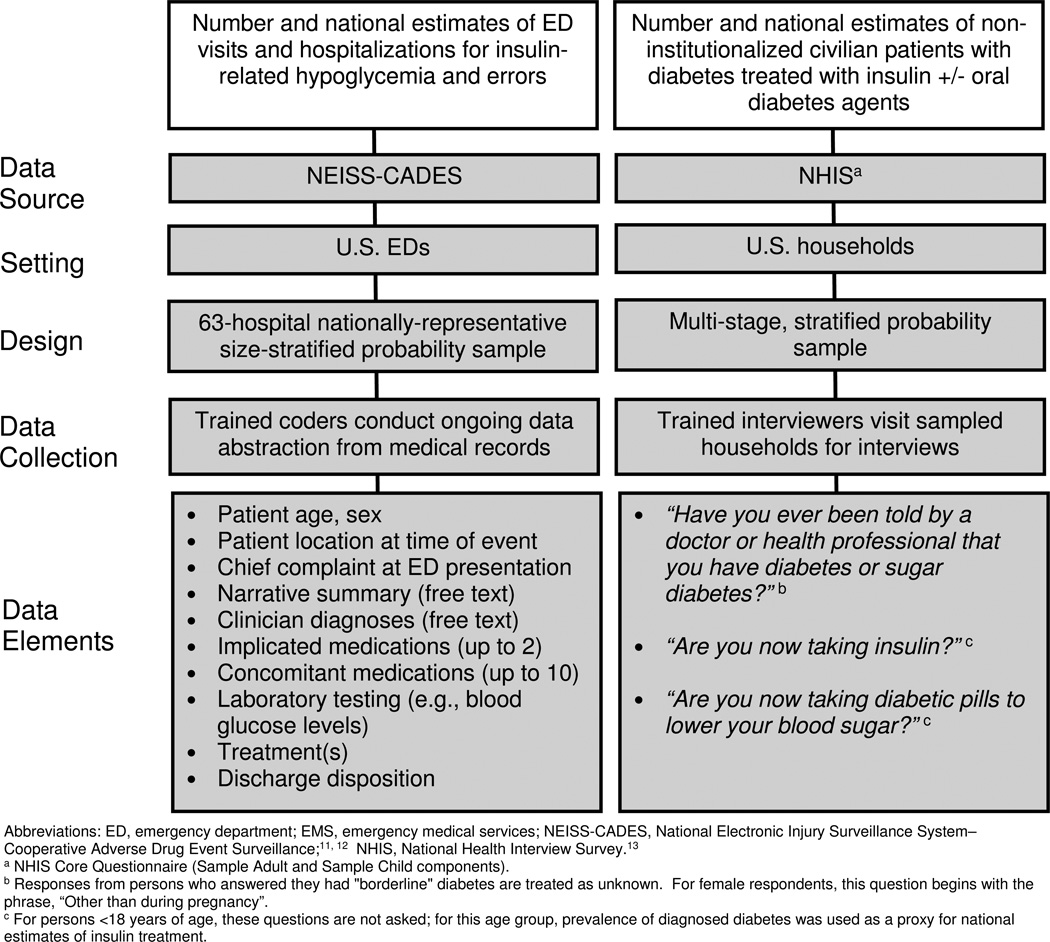
We estimated the numbers of U.S. ED visits and hospitalizations for IHEs based on data from the 63 hospitals participating in the National Electronic Injury Surveillance System–Cooperative Adverse Drug Event Surveillance (NEISS-CADES) project, a stable, nationally-representative, size-stratified probability sample of hospitals (excluding psychiatric and penal institutions) in the U.S. and its territories with a minimum of 6 beds and a 24-hour emergency department (Figure 1).11 As described elsewhere,12 trained coders at each hospital review clinical records of every ED visit to identify physician-diagnosed adverse drug events (ADEs), and report up to two medications implicated in the adverse event as well as any concomitant medications documented in the medical record. Coders also record narrative descriptions of the ADE, including preceding events, physician diagnosis, clinical and laboratory testing, treatment administered by emergency medical services (EMS) or ED staff, and discharge disposition.
Figure 1.
Data sources and Descriptions.
Abbreviations: ED, emergency department; EMS, emergency medical services; NEISS-CADES, National Electronic Injury Surveillance System–Cooperative Adverse Drug Event Surveillance;11, 12 NHIS, National Health Interview Survey.13
a NHIS Core Questionnaire (Sample Adult and Sample Child components).
b Responses from persons who answered they had "borderline" diabetes are treated as unknown. For female respondents, this question begins with the phrase, “Other than during pregnancy”.
c For persons <18 years of age, these questions are not asked; for this age group, prevalence of diagnosed diabetes was used as a proxy for national estimates of insulin treatment.
Denominator Data
We estimated the numbers of U.S. patients who reported having DM and using insulin or oral diabetes agents from the National Health Interview Survey (NHIS), a multistage cluster sample of non-institutionalized civilian households (Figure 1).13
Institutional Review Board Approval
NEISS-CADES data collection is considered a public health surveillance activity by federal human subjects oversight bodies and does not require human subject review or institutional review board (IRB) approval.14 NHIS data collection is approved by the IRB at the National Center for Health Statistics, Centers for Disease Control and Prevention, Hyattsville, MD. No approval is necessary for analyses of deidentified survey data.15
DEFINITIONS
ED visits for IHEs included visits to any NEISS-CADES ED from January 1, 2007 through December 31, 2011 in which there was clinician documentation of (1) insulin-related clinically relevant hypoglycemia (BG <70 mg/dL, diagnosis of “hypoglycemia”, or treatment for hypoglycemia), or (2) “insulin overdose” or “insulin reaction”, or (3) an error in insulin use (e.g., administration of the wrong insulin dose). ED visits for allergic reactions, local effects (e.g., injection site pain), non-hypoglycemic effects (e.g., “headache” alone) and accidental needlesticks were excluded. Definitions of other variables, including IHE location, clinical presentation, BG levels, hypoglycemia treatments, diabetes therapy, and precipitating factors are provided in eTable 1.
Prevalence of self-reported diabetes from January 1, 2007 through December 31, 2011 was estimated from the number of NHIS respondents who answered “Yes” to the question, “Have you ever been told by a doctor or health professional that you have diabetes or sugar diabetes?”.16–18 For those ≥ 18 years of age, prevalence of insulin-treated diabetes was estimated via the number of NHIS respondents who answered “Yes” to the question, “Are you now taking insulin?”. For those <18 years of age, this question is not asked; thus, prevalence of diagnosed diabetes was used as a proxy for insulin treatment. Insulin-treated patients were considered to be treated with both insulin and oral diabetes agent(s) if they also answered “Yes” to the question, “Are you now taking diabetic pills to lower your blood sugar?”.
STATISTICAL ANALYSIS
Each NEISS-CADES record is accompanied by a sample weight based on inverse probability of selection, adjusted for non-response and hospital non-participation, and post-stratified to account for changes in the number of U.S. ED visits each year. Each NHIS record is accompanied by a sample weight based on non-zero probability of selection, with design, ratio, non-response and post-stratification adjustments; post-stratification adjustment is made relative to census control totals for the number of U.S. civilian, non-institutionalized individuals.19
National estimates and proportions of ED visits and hospitalizations for IHEs and national estimates of patients with diabetes using insulin alone or in combination with oral diabetes agents, with corresponding 95% confidence intervals (CIs) were calculated using the SURVEYMEANS procedure in SAS (version 9.3, SAS Institute, Cary, NC) to account for the sample weights and complex sample designs. Estimates and their corresponding CIs derived from 2007–2011 NEISS-CADES and NHIS data were divided by 5 to obtain average annual estimates and CIs. Estimates based on small numbers of cases (<20) or with a coefficient of variation greater than 30% were considered statistically unstable and are noted in the tables. National estimates were calculated for variables with completed documentation (≥90% of cases); case-based analysis was used for remaining variables.
To estimate rates of ED visits and hospitalizations for IHEs in relation to insulin exposure, we divided (NEISS-CADES-derived) estimates of ED visits or hospitalizations for IHEs by (NHIS-derived) estimates of insulin-treated patients. A similar approach was used to estimate the rates of IHEs by age and sex. Accompanying CIs were calculated accounting for variability in both numerator and denominator estimates, and assuming statistical independence (as these components were derived from separate surveys).20 These rate estimates were then used to calculate rate ratios (RRs) of ED visits and hospitalizations for IHEs associated with different patient groups. Estimated CIs for RRs were calculated using an initial logarithmic transformation and incorporated the estimated variances of the numerators and denominators of both component rate estimates, which were assumed to be independent across patient populations.21
RESULTS
NUMBERS OF ED VISITS
Based on 8,100 NEISS-CADES surveillance cases, an estimated 97,648 (CI, 64,410–130,887) ED visits for IHEs occurred annually between 2007 and 2011 (Table 1), accounting for 9.2% (CI, 6.7%–11.8%) of ED visits for all ADEs during this period. Among the very elderly (≥80 years of age), ED visits for IHEs accounted for 12.4% (CI, 8.9%–16.0%) of ED visits for all ADEs. The estimated median age of patients who presented to EDs for IHEs was 60 years for patients treated with insulin alone and 67 years for patients treated with insulin and at least one oral diabetes agent. An estimated 50.4% (CI, 46.4%–54.3%) of ED visits for IHEs occurred among males. Among adults (≥18 years of age), at least one oral diabetes agent was documented in addition to insulin in an estimated 17.1% (CI, 13.3%–20.8%) of ED visits for IHEs (Table 2).
Table 1.
Number of Cases and Estimates of Emergency Department Visits for Insulin-related Hypoglycemia and Errors, by Patient Characteristics—United States, 2007–2011a
| Patient Characteristics | ED Visits for IHEs | Persons with Diabetes Mellitus Treated with Insulin +/− Oral Diabetes Agents |
ED Visits Per 1,000 Persons with Diabetes Mellitus Treated with Insulin +/− Oral Diabetes Agents |
||||
|---|---|---|---|---|---|---|---|
| Cases | Annual National Estimate | Annual National Estimate | Annual National Estimate |
95% Confidence Interval |
|||
| No. | No. | % | No. | % | |||
| Age | |||||||
| <18 yearsb | 265 | 2,088 | 2.1 | 152,555 | 2.8 | 13.7 | 4.9 – 22.5 |
| 18–44 years | 1,675 | 21,189 | 21.7 | 871,150 | 15.9 | 24.3 | 15.0 – 33.6 |
| 45–64 years | 2,817 | 34,173 | 35.0 | 2,492,704 | 45.5 | 13.7 | 9.1 – 18.3 |
| 65–79 years | 2,190 | 24,720 | 25.3 | 1,515,077 | 27.7 | 16.3 | 10.7 – 21.9 |
| ≥80 years | 1,153 | 15,479 | 15.9 | 443,497 | 8.1 | 34.9 | 20.5 – 49.3 |
| Sexc | |||||||
| Female | 4,080 | 48,458 | 49.6 | 2,740,352 | 50.1 | 17.7 | 11.9 – 23.5 |
| Male | 4,019 | 49,186 | 50.4 | 2,734,631 | 49.9 | 18.0 | 11.4 – 24.5 |
| Total | 8,100 | 97,648 | ~ | ~ | ~ | ~ | ~ |
Abbreviations: ED, emergency department; IHEs, insulin-related hypoglycemia and errors.
Case counts and estimates from the National Electronic Injury Surveillance System – Cooperative Adverse Drug Event Surveillance (NEISS-CADES) project, CDC. Diabetes prevalence estimates from the National Health Interview Survey (NHIS), CDC.
For persons <18 years of age, diabetes therapy is not reported by NHIS; for this age group, prevalence of diagnosed diabetes was used as a proxy for national estimates of insulin treatment.
Sex missing for one case.
Table 2.
Number of Cases and Estimates of Emergency Department Visits for Insulin-related Hypoglycemia and Errors, by Diabetes Therapy and Patient Age—United States, 2007–2011a
| Diabetes Therapy by Patient Age | ED Visits for IHEs | Persons with Diabetes Mellitus Treated with Insulin +/− Oral Diabetes Agents |
ED Visits Per 1,000 Persons with Diabetes Mellitus Treated with Insulin +/− Oral Diabetes Agents |
||||
|---|---|---|---|---|---|---|---|
| Cases | Annual National Estimate | Annual National Estimate | Annual National Estimate |
95% Confidence Interval |
|||
| No. | No. | % | No. | % | |||
| <18 yearsb | |||||||
| Insulin only | 261 | 2,051 | 98.2 | n/a | n/a | n/a | n/a |
| Insulin + oral agent | 4 | c | c | n/a | n/a | n/a | n/a |
| ≥18 years | |||||||
| Insulin only | 6,492 | 79,245 | 82.9 | 2,553,062 | 48 | 31.0 | 20.3 – 41.7 |
| Insulin + oral agent | 1,343 | 16,315 | 17.1 | 2,769,366 | 52 | 5.9 | 3.7 – 8.1 |
| 18–44 years | |||||||
| Insulin only | 1,580 | 20,190 | 95.3 | 579,860 | 66.6 | 34.8 | 21.1 – 48.5 |
| Insulin + oral agent | 95 | 999 | 4.7 | 291,290 | 33.4 | 3.4 | 1.8 – 5.1 |
| 45–64 years | |||||||
| Insulin only | 2,322 | 28,029 | 82.0 | 1,042,828 | 41.8 | 26.9 | 17.3 – 36.5 |
| Insulin + oral agent | 495 | 6,144 | 18.0 | 1,449,876 | 58.2 | 4.2 | 2.5 – 6.0 |
| 65–79 years | |||||||
| Insulin only | 1,672 | 18,836 | 76.2 | 688,371 | 45.4 | 27.4 | 17.5 – 37.2 |
| Insulin + oral agent | 518 | 5,884 | 23.8 | 826,706 | 54.6 | 7.1 | 4.2 – 10.0 |
| ≥80 years | |||||||
| Insulin only | 918 | 12,190 | 78.8 | 242,003 | 54.6 | 50.4 | 28.6 – 72.1 |
| Insulin + oral agent | 235 | 3,289 | 21.2 | 201,493 | 45.4 | 16.3 | 8.0 – 24.7 |
| Total | 8,100 | 97,648 | ~ | ~ | ~ | ~ | ~ |
Abbreviations: ED, emergency department; IHEs, insulin-related hypoglycemia and errors; n/a, not applicable.
Case counts and estimates from the National Electronic Injury Surveillance System – Cooperative Adverse Drug Event Surveillance (NEISS-CADES) project, CDC. Diabetes prevalence estimates from the National Health Interview Survey (NHIS), CDC. "Insulin only" refers to cases where only insulin was documented in the ED medical record and no concomitant oral diabetes agent was documented. "Insulin + oral agent" refers to cases where an oral diabetes agent was documented in addition to insulin in the ED medical record.
For persons <18 years of age, diabetes therapy is not reported by NHIS; treatment-specific rates were not calculated for this age group ("n/a").
Estimates based on fewer than 20 cases are not shown.
RATES OF ED VISITS AND HOSPITALIZATIONS
Patients ≥80 years of age had the highest estimated rate of ED visits for IHEs (34.9 per 1,000 insulin-treated patients with diabetes; CI, 20.5–49.3), followed by patients 18–44 years of age (24.3 per 1,000; CI, 15.0–33.6). When all patients ≥65 years of age are considered, the estimated rate was 20.5 per 1000 (CI, 13.2–27.8). Insulin-treated patients ≥80 years of age were more than twice as likely to seek ED evaluation for IHEs than those 65–79 years of age (RR, 2.1; CI, 1.3–3.7) and those 45–64 years of age (RR, 2.5; CI, 1.5–4.3) (Table 2). Patients ≥80 years of age were also almost five times as likely to be hospitalized for IHEs than those 45–64 years of age (RR, 4.9; CI, 2.6.–9.1). No significant differences in the rates of ED visits (RR, 1.0; CI, 0.6–1.6) or hospitalizations (RR, 1.2; CI, 0.6–2.1) for IHEs were identified between female and male patients. Overall, the rate of ED visits for IHEs among patients ≥18 years of age treated with insulin only was five times that of patients treated with insulin and at least one oral diabetes agent (RR, 5.3; CI, 3.2–8.8); the RR decreased as patient age increased (Table 2).
SPECIFIC INSULIN AND CONCOMITANT ORAL AGENTS
In an estimated 22.9% of ED visits for IHEs, more than one type of insulin product was documented in the medical record (Table 3). Long-acting (32.9%) and rapid-acting (26.4%) products were the most commonly-documented insulin product types (eTable 2). Metformin and sulfonylureas were the most commonly-documented concomitant oral diabetes agents, identified in 50.9% (CI, 47.6%–54.2%) and 39.2% (CI, 34.8%–43.6%) of estimated ED visits for IHEs where an oral diabetes agent was documented, respectively.
Table 3.
Number of Cases and Estimates of Emergency Department Visits for Insulin-related Hypoglycemia and Errors, by Case Characteristics—United States, 2007–2011a
| Case Characteristics | ED Visits for IHEs | ||
|---|---|---|---|
| Cases | Annual National Estimate | ||
| No. | % | 95% Confidence Interval |
|
| Number of Insulin Productsb | |||
| 1 | 6,149 | 77.1 | 71.3 – 83.0 |
| 2 | 1,892 | 22.3 | 16.5 – 28.0 |
| ≥3 | 59 | 0.6 | 0.3 – 0.9 |
| Other Diabetes Agentsc | |||
| Biguanide (metformin) | 705 | 8.5 | 6.7 – 10.4 |
| Sulfonylurea | 500 | 6.6 | 4.7 – 8.5 |
| Thiazolidinedione (glitazones) | 312 | 3.6 | 2.4 – 4.7 |
| Dipeptidyl peptidase-4 inhibitor (gliptins) | 82 | 1.3 | 0.6 – 2.0 |
| Other / unspecified oral agent | 73 | 0.9 | 0.5 – 1.4 |
| Exenatide, liraglutide, pramlintide | 21 | 0.2 | 0.1 – 0.4 |
| Clinical Presentation of Event | |||
| Hypoglycemia | 7,760 | 95.4 | 93.6 – 97.2 |
| With shock, loss of consciousness, or seizure | 1,846 | 23.2 | 15.5 – 31.0 |
| With fall or injury | 491 | 5.1 | 3.7 – 6.4 |
| With altered mental status | 2,535 | 32.3 | 20.6 – 44.0 |
| With other neurologic sequelae | 416 | 4.8 | 3.3 – 6.3 |
| With presyncope/syncope | 398 | 4.4 | 3.3 – 5.6 |
| With other sequelae | 439 | 5.6 | 3.8 – 7.4 |
| Without specific sequelae documented | 1,635 | 20.0 | 13.4 – 26.6 |
| No hypoglycemia documentedd | 340 | 4.6 | 2.8 – 6.4 |
| Discharge Dispositione | |||
| Admitted, transferred, or held for observation | 2,447 | 29.3 | 21.8 – 36.8 |
| Treated and released, or left against medical advice | 5,652 | 70.7 | 63.2 – 78.2 |
Abbreviations: ED, emergency department; IHEs, insulin-related hypoglycemia and errors.
Case counts and estimates from the National Electronic Injury Surveillance System - Cooperative Adverse Drug Event Surveillance (NEISS-CADES) project, CDC. Refer to eTable 1 for definitions of case characteristics.
All insulin products reported in the ED medical record, including those implicated in IHEs and those listed as concomitant medications.
Categories are not mutually exclusive; therefore, percentages may total more than 100%.
Clinician documentation of error in insulin use (n=323), “insulin overdose” (n=6), or “insulin reaction” (n=11) with no documentation of hypoglycemia.
Discharge disposition missing for one case.
IHE CHARACTERISTICS – NATIONAL ESTIMATES
Hypoglycemia was documented in an estimated 95.4% of ED visits for IHEs, and severe neurologic sequelae (i.e., hypoglycemia-associated shock, loss of consciousness, or seizure; hypoglycemia-associated injury or fall; or hypoglycemia-associated altered mental status) were documented in an estimated 60.6% (CI, 51.3%–69.9%) of ED visits (Table 3). Almost one-third (29.3%) of estimated ED visits for IHEs required admission, transfer to another facility, or observation admission; observation admissions comprised 2.1% (CI, 0.9%–3.3%) of estimated ED visits.
IHE CHARACTERISTICS – CASE-BASED ANALYSIS
In most cases (53.3%), IHEs occurred in a home setting (eTable 2). Use of an insulin pump was documented in 6.1% of cases. Over one-half (53.4%) of cases involved a BG level ≤50 mg/dL. Intravenous dextrose 50% was the most common EMS/ED treatment administered (50.8% of cases).
PRECIPITATING FACTORS
Precipitating factors for ED visits for IHEs were documented in an estimated 20.8% (CI, 14.8%–26.9%) of ED visits. When documented, almost one-half (45.9%) involved meal-related misadventures (e.g., neglecting to eat shortly after taking a rapid-acting insulin, not adjusting insulin regimen in the presence of reduced caloric intake) (Table 4). Taking the wrong insulin product was documented in an estimated 22.1% of ED visits for IHEs with documented precipitants, and taking the wrong dose or confusing dosing units was documented in an estimated 12.2% of ED visits with documented precipitants. Among ED visits for IHEs where taking the wrong insulin was documented, the most commonly reported error was mixing up long-acting and rapid-acting insulin products. In an estimated 52.3% (CI, 42.5%–62.0%) of these ED visits, patients reported an intent to take a long-acting insulin product (e.g., detemir, glargine), but took a rapid-acting one (e.g., aspart, lispro) instead. The proportion hospitalized did not differ among ED visits where an IHE precipitant was documented (20.7%; CI, 15.9%–25.4%) compared with ED visits without an IHE precipitant documented (31.6%; CI, 22.9%–40.2%).
Table 4.
Number of Cases and Estimates of Precipitating Factors Identified in Emergency Department Visits for Insulin-related Hypoglycemia and Errors—United States, 2007–2011a
| Precipitating Factors | ED Visits for IHEs | Illustrative Casesb | ||
|---|---|---|---|---|
| Cases, No. |
Annual National Estimate |
|||
| % | 95% Confidence Interval |
|||
| Meal-related misadventure | 952 | 45.9 | 38.2 – 53.6 |
|
| Unintentionally took wrong insulin product | 332 | 22.1 | 17.2 – 26.9 |
|
| Unintentionally took wrong dose / Confused units | 205 | 12.2 | 9.2 – 15.2 |
|
| Intentionally took "additional" dose | 113 | 6.0 | 4.4 – 7.6 |
|
| Pump-related misadventure | 38 | 1.5 | 0.7 – 2.2 |
|
| Other misadventurec | 211 | 13.4 | 10.4 – 16.4 |
|
Abbreviations: ED, emergency department; EMS, emergency medical services; IHEs, insulin-related hypoglycemia and errors.
Case counts and estimates from the National Electronic Injury Surveillance System - Cooperative Adverse Drug Event Surveillance (NEISS-CADES) project, CDC. Percentages are out of a total of 1,829 cases (20,346 estimated ED visits) where a precipitating factor was documented. Refer to eTable 1 for definitions of precipitating factors. Categories are not mutually exclusive; therefore, percentages may total more than 100%.
Case descriptions are verbatim excerpts as reported by medical coders based on review of ED medical record narrative (with spelling corrected and abbreviations spelled out).
"Other misadventure" includes: insulin administration at the incorrect time or without regard to checking blood glucose, administration of "too much insulin" not further described, or medication error with insulin not otherwise specified.
DISCUSSION
Insulin is an important component of diabetes treatment, but remains complex to manage and poses serious risk of hypoglycemia.22 These national data quantify the burden and severity of IHEs, identify patient groups at higher risk for these events, and describe precipitating factors that could be targeted by prevention efforts.
Nearly 100,000 ED visits and 30,000 hospitalizations annually for IHEs demonstrate the high frequency and significant health impact of these adverse events. Based on prior cost estimates of ED visits for hypoglycemia,23 ED visits for IHEs may have cost well over $600 million during the 5-year study period. Direct comparisons of our findings to those of previous studies are limited by differences in study methodologies. One study estimated 40,700 ED visits for insulin and other diabetes agent-related adverse events in 2010 using International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) diagnosis codes for poisoning (962.3) or adverse effects due to insulin or other diabetes agents (E932.3);24 however, cause-of-injury codes such as these have low sensitivity for identifying many ADEs.25 Another study estimated that 316,000 visits for hypoglycemia were made to U.S. EDs in 2007 based on reporting of hypoglycemia as the first-listed diagnosis and diabetes as a secondary diagnosis;26 however, this analysis lacked information on insulin use and could not exclude hypoglycemia episodes related to other factors (e.g., alcohol use, occult infection).
The IHEs we identified were serious events, with BG levels ≤50 mg/dL in over half of cases and severe neurologic manifestations in almost two-thirds of cases. We have previously found insulin to be one of the most commonly implicated drugs in adverse events treated in EDs.27 Based on the more recent data in this study, IHEs accounted for 1 out of every 8 estimated ED visits for ADEs among the very elderly (≥80 years of age), who sought ED evaluation and were hospitalized for IHEs at rates two and five times higher than those 45–64 years of age, respectively. Other studies have found that Medicare beneficiaries ≥85 years of age are twice as likely to experience a hypoglycemia-related hospitalization compared with those 65–74 years of age,28 and that re-hospitalizations and mortality are more frequent among older adults (≥66 years of age) with at least one episode of hospitalized hypoglycemia.29
Although there are notable exceptions,30–33 until very recently, most diabetes treatment guidelines, quality metrics, and pay-for-performance measures placed little emphasis on hypoglycemia risk factors such as advanced age, limited life expectancy, or frailty.34 The higher rates of ED visits and hospitalizations for IHEs among older insulin-treated patients with diabetes suggest that individualizing glycemic targets by balancing hypoglycemia risks with long-term benefits of glycemic control is appropriate.22, 35–37 Updated guidelines and treatment recommendations are now advising glycemic targets be relaxed for patients with advanced age, high risk of hypoglycemia or shorter life expectancy.22, 35, 38, 39 For example, the American Geriatrics Society has advocated for avoiding adding medications to achieve tight hemoglobin A1c control in most adults ≥65 years of age.40, 41 Tighter glycemic control may continue to be appropriate for functional and cognitively intact elderly patients with diabetes who have longer life expectancy and for whom intensive insulin therapy can be managed safely;22, 35 however, the high frequency and severity of ED visits for IHEs suggest careful consideration of hypoglycemic sequelae and a cautious approach when deciding whether to start or intensify insulin treatment among older adults, especially the very elderly.
Adoption of a patient-centered approach to setting glycemic targets9, 10, 42–44 also requires development of healthcare quality metrics which recognize targets based on individual patients’ clinical profiles and preferences.33 Although current National Quality Forum-endorsed quality metrics do not yet incorporate variation in A1c target levels based on hypoglycemia risk,45, 46 new quality measures might allow for considerations of hypoglycemia risks along with long-term benefits of glycemic control.47
Enhanced prevention efforts should target commonly-identified IHE precipitants.48 Although meal-planning is a well-recognized component of diabetes self-management education,49, 50 the most commonly-documented IHE precipitant in this study was meal-related misadventure, suggesting further emphasis on meal-planning in diabetes patient education efforts may be needed. Reducing the frequency of missed meals and improving patients’ competency in adjusting insulin regimens when food intake is reduced may require both content review (e.g., reviewing patients’ understanding of dietetic needs in relation to BG levels) and simulation (e.g., patients demonstrating how they would manage insulin with a missed meal or reduced food intake scenario).48, 51
Administration of the wrong insulin product (e.g., rapid-acting vs. long-acting agents) was the second most commonly-documented IHE precipitant. The number of U.S. poison control center calls for insulin-related unintentional therapeutic errors increased in the last decade, but the frequency of specific errors, such as using the wrong insulin product, has not been described.52, 53 Recently, insulin packaging has become more distinguishable;54 however, mix-ups continue55 and further product type distinctions (e.g., using packaging color or texture) might be explored for reducing medication errors. Also, diabetes self-management education might emphasize distinguishing insulin types, minimizing mix-ups (e.g., storing rapid-acting and long-acting agents in different locations), and correctly timing insulin administration.54, 56
This study’s findings should be interpreted in the context of the limitations of public health surveillance data. First, these data likely underestimate the total burden of hypoglycemic events as hypoglycemia, although a frequent cause of EMS calls,57–61 is most often cared for outside of the ED setting.62 Patients who have hypoglycemia unawareness63, 64 and whose episodes may not result in EMS or ED care are not counted. Patients who died en route to or in the ED are also not counted. Second, since information on past medical history is limited in the ED medical record, the contributions of risk factors for hypoglycemia such as DM type, intensity and duration of insulin therapy, glycemic control, concomitant medications, and comorbidities were not assessed. Third, the specific insulin brand, formulation, and delivery system were not always documented, which limited the ability to assess differences in ED visits and hospitalizations for IHEs across specific insulin products. Similarly, we did not make detailed comparisons between patients treated with insulin alone and those treated with insulin and oral diabetes agent(s) because documentation of concurrent oral diabetes therapy may have been incomplete. Nonetheless, it is notable that across all adult age groups the rate of estimated ED visits for IHEs was consistently lower among those treated with concurrent oral diabetes therapy, perhaps suggesting concurrent use of long-acting insulin products, with less risk for hypoglycemia.65 Fourth, BG levels were not specified in approximately one-third of cases; nevertheless, over half of cases still had documented BG ≤50 mg/dL. Other indicators of the seriousness of these events included almost 60,000 estimated ED visits for IHEs with severe neurologic sequelae and almost 30,000 estimated ED visits resulting in hospitalization.
Insulin-related hypoglycemia and errors are clinically significant causes of ED visits and hospitalizations for ADEs, particularly among very elderly patients with diabetes. Reducing ED visits for adverse events related to injectable diabetes agents has been recognized as a national priority for improving the health of Americans in a new Healthy People 2020 goal.66 Reaching this goal will likely require balancing glycemic risks in vulnerable older patient populations and augmenting prevention efforts targeted at key IHE precipitants, such as meal-related misadventures and insulin product mix-ups. Healthcare quality metrics should evolve based on the most current glycemic control guidelines, and the impact of changing guidelines, quality metrics, and prevention strategies should be evaluated via ongoing national surveillance.22, 35, 67–69
Supplementary Material
Acknowledgments
Financial Support: None to report.
Footnotes
Author Contributions: Dr Geller had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Budnitz, Shehab.
Acquisition of data: Budnitz, Shehab, Lovegrove, Weidenbach, Geller.
Analysis and interpretation of Data: Budnitz, Shehab, Kegler, Lovegrove, Weidenbach, Geller.
Drafting of the Manuscript: Geller.
Critical revision of the manuscript for important intellectual content: All authors.
Statistical analysis: Kegler, Shehab, Geller.
Administrative, technical, and material support: All authors.
Study supervision: Budnitz, Shehab.
Additional Contributions:
Kathleen Rose, BSN of Emergint Technologies (contractor to Centers for Disease Control and Prevention [CDC]), Lee M. Hampton, MD, MSc of CDC; and Cathy Irish, BS, and Joel Friedman, BA, from the U.S. Consumer Product Safety Commission assisted with data acquisition. No individuals named herein received compensation for their contributions.
Disclaimer: The findings and conclusions in this study are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Financial Disclosures: None to report.
References
- 1.Centers for Disease Control and Prevention. National diabetes fact sheet: national estimates and general information on diabetes and prediabetes in the United States. [Accessed December 31, 2012];2011 http://www.cdc.gov/diabetes/pubs/pdf/ndfs_2011.pdf.
- 2.Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion. Diabetes Medication Use Among Adults with Diabetes. [Accessed December 31, 2012];2012 Dec 7; http://www.cdc.gov/diabetes/statistics/treating_national.htm.
- 3.American Diabetes Association. Economic costs of diabetes in the U.S. in 2012. Diabetes Care. 2013 Apr;36(4):1033–1046. doi: 10.2337/dc12-2625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.The Diabetes Control and Complications Trial Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med. 1993 Sep 30;329(14):977–986. doi: 10.1056/NEJM199309303291401. [DOI] [PubMed] [Google Scholar]
- 5.Neugebauer R, Fireman B, Roy JA, O'Connor PJ. Impact of specific glucose-control strategies on microvascular and macrovascular outcomes in 58,000 adults with type 2 diabetes. Diabetes Care. 2013 Nov;36(11):3510–3516. doi: 10.2337/dc12-2675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Seaquist ER, Miller ME, Bonds DE, et al. The impact of frequent and unrecognized hypoglycemia on mortality in the ACCORD study. Diabetes Care. 2012 Feb;35(2):409–414. doi: 10.2337/dc11-0996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zoungas S, Patel A, Chalmers J, et al. Severe hypoglycemia and risks of vascular events and death. N Engl J Med. 2010 Oct 7;363(15):1410–1418. doi: 10.1056/NEJMoa1003795. [DOI] [PubMed] [Google Scholar]
- 8.Giordano C. Insulin therapy: unmet needs and new perspectives. Minerva Endocrinol. 2013 Mar;38(1):95–102. [PubMed] [Google Scholar]
- 9.Ismail-Beigi F, Moghissi E, Tiktin M, Hirsch IB, Inzucchi SE, Genuth S. Individualizing glycemic targets in type 2 diabetes mellitus: implications of recent clinical trials. Ann Intern Med. 2011 Apr 19;154(8):554–559. doi: 10.7326/0003-4819-154-8-201104190-00007. [DOI] [PubMed] [Google Scholar]
- 10.Laiteerapong N, John PM, Nathan AG, Huang ES. Public health implications of recommendations to individualize glycemic targets in adults with diabetes. Diabetes Care. 2013 Jan;36(1):84–89. doi: 10.2337/dc11-2344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schroeder T, Ault K. The NEISS sample (design and implementation) 1997 to present. June 1, 2001. [Accessed November 11, 2013]; http://www.cpsc.gov//PageFiles/106617/2001d011-6b6.pdf.
- 12.Jhung MA, Budnitz DS, Mendelsohn AB, Weidenbach KN, Nelson TD, Pollock DA. Evaluation and overview of the National Electronic Injury Surveillance System-Cooperative Adverse Drug Event Surveillance Project (NEISS-CADES) Med Care. 2007 Oct;45(10) Supl 2:S96–S102. doi: 10.1097/MLR.0b013e318041f737. [DOI] [PubMed] [Google Scholar]
- 13.Schiller JS, Lucas JW, Ward BW, Peregoy JA. Summary health statistics for U. S. adults: National Health Interview Survey, 2011. Vital Health Stat 10. 2012 Dec;(256):1–219. [PubMed] [Google Scholar]
- 14.Centers for Disease Control and Prevention. Distinguishing Public Health Research and Public Health Nonresearch. [Accessed August 5, 2013];2010 Jul 29; http://www.cdc.gov/od/science/integrity/docs/cdc-policy-distinguishing-public-health-research-nonresearch.pdf.
- 15.National Center for Health Statistics Research Data Center. Publishing Guidelines. [Accessed August 5, 2013];2012 Mar 15; http://www.cdc.gov/rdc/B6Pubeyond/Pub610.htm.
- 16.U.S. Census Bureau. National Health Interview Survey: CAPI manual for NHIS field representatives. [Accessed January 3, 2013];HIS—100—C. 2011 Jan 1; ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Survey_Questionnaires/NHIS/2011/frmanual.pdf.
- 17.National Center for Health Statistics. NHIS Sample Adult Questionnaire, National Health Interview Survey, 2011. [Accessed January 3, 2013];2012 May 30; ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Survey_Questionnaires/NHIS/2011/english/qadult.pdf.
- 18.National Center for Health Statistics. NHIS Sample Child Questionnaire, 2011. [Accessed January 3, 2013];2012 May 30; ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Survey_Questionnaires/NHIS/2011/english/qchild.pdf.
- 19.National Center for Health Statistics. NHIS Survey Description, 2011. [Accessed January 4, 2013];2012 Jun 1; ftp://ftp.cdc.gov/pub/health_statistics/nchs/dataset_documentation/nhis/2011/srvydesc.pdf.
- 20.Kish L. Survey Sampling. New York, NY: John Wiley & Sons; 1995. [Google Scholar]
- 21.Kegler SR. Applying the compound Poisson process model to the reporting of injury-related mortality rates. Epidemiol Perspect Innov. 2007;4:1. doi: 10.1186/1742-5573-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.American Diabetes Association. Standards of medical care in diabetes--2013. Diabetes Care. 2013 Jan;36(Suppl 1):S11–S66. doi: 10.2337/dc13-S011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Quilliam BJ, Simeone JC, Ozbay AB, Kogut SJ. The incidence and costs of hypoglycemia in type 2 diabetes. Am J Manag Care. 2011 Oct;17(10):673–680. [PubMed] [Google Scholar]
- 24.Lucado J, Paez K, Elixhauser A. Medication-Related Adverse Outcomes in U.S. Hospitals and Emergency Departments, 2008: Statistical Brief #109. Healthcare Cost and Utilization Project Statistical Briefs. 2011 [PubMed] [Google Scholar]
- 25.Leonard CE, Haynes K, Localio AR, et al. Diagnostic E-codes for commonly used, narrow therapeutic index medications poorly predict adverse drug events. J Clin Epidemiol. 2008 Jun;61(6):561–571. doi: 10.1016/j.jclinepi.2007.08.003. [DOI] [PubMed] [Google Scholar]
- 26.Division of Diabetes Translation, National Center for Chronic Disease Prevention and Health Promotion, Centers for Disease Control and Prevention. Diabetes Data & Trends: Data from the National Emergency Department Samples, Agency for Healthcare Research and Quality. [Accessed June 3, 2013];2012 Sep 11; http://www.cdc.gov/diabetes/statistics/emergency_national.htm.
- 27.Budnitz DS, Pollock DA, Weidenbach KN, Mendelsohn AB, Schroeder TJ, Annest JL. National surveillance of emergency department visits for outpatient adverse drug events. JAMA. 2006 Oct 18;296(15):1858–1866. doi: 10.1001/jama.296.15.1858. [DOI] [PubMed] [Google Scholar]
- 28.Lipska KJ, Wang Y, Ross JS, et al. National Trends in Hospital Admissions for Hyperglycemia and Hypoglycemia among Medicare Beneficiaries, 1999–2010. Presented at the 73rd Scientific Sessions of the American Diabetes Association; Chicago, IL. 24 June 2013. [Google Scholar]
- 29.Majumdar SR, Hemmelgarn BR, Lin M, McBrien K, Manns BJ, Tonelli M. Hypoglycemia Associated With Hospitalization and Adverse Events in Older People: Population-based cohort study. Diabetes Care. 2013 Nov;36(11):3585–3590. doi: 10.2337/dc13-0523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.The VA/DoD Diabetes Mellitus Working Group. VA/DoD Clinical practice guideline for the management of diabetes mellitus. [Accessed August 4, 2013];2010 Aug 1; http://www.healthquality.va.gov/diabetes/DM2010_FUL-v4e.pdf.
- 31.Brown AF, Mangione CM, Saliba D, Sarkisian CA. Guidelines for improving the care of the older person with diabetes mellitus. J Am Geriatr Soc. 2003 May;51:S265–S280. doi: 10.1046/j.1532-5415.51.5s.1.x. (5 Suppl Guidelines) [DOI] [PubMed] [Google Scholar]
- 32.Qaseem A, Vijan S, Snow V, et al. Glycemic control and type 2 diabetes mellitus: the optimal hemoglobin A1c targets. A guidance statement from the American College of Physicians. Ann Intern Med. 2007 Sep 18;147(6):417–422. doi: 10.7326/0003-4819-147-6-200709180-00012. [DOI] [PubMed] [Google Scholar]
- 33.Aron D, Conlin PR, Hobbs C, Vigersky RA, Pogach L. Individualizing glycemic targets in type 2 diabetes mellitus. Ann Intern Med. 2011 Sep 6;155(5):340–341. doi: 10.7326/0003-4819-155-5-201109060-00025. [DOI] [PubMed] [Google Scholar]
- 34.Berkowitz SA, Aragon K, Hines J, Seligman H, Lee S, Sarkar U. Do clinical standards for diabetes care address excess risk for hypoglycemia in vulnerable patients? A systematic review. Health Serv Res. 2013 Aug;48(4):1299–1310. doi: 10.1111/1475-6773.12048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Garber AJ, Abrahamson MJ, Barzilay JI, et al. AACE comprehensive diabetes management algorithm 2013. Endocr Pract. 2013 Mar-Apr;19(2):327–336. doi: 10.4158/endp.19.2.a38267720403k242. [DOI] [PubMed] [Google Scholar]
- 36.Seaquist ER, Anderson J, Childs B, et al. Hypoglycemia and diabetes: a report of a workgroup of the American Diabetes Association and the Endocrine Society. Diabetes Care. 2013 May;36(5):1384–1395. doi: 10.2337/dc12-2480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Qaseem A, Chou R, Humphrey LL, Shekelle P for the Clinical Guidelines Committee of the American College of Physicians. Inpatient Glycemic Control: Best Practice Advice From the Clinical Guidelines Committee of the American College of Physicians. Am J Med Qual. 2013 Jun 7; doi: 10.1177/1062860613489339. [DOI] [PubMed] [Google Scholar]
- 38.Raz I, Riddle MC, Rosenstock J, et al. Personalized management of hyperglycemia in type 2 diabetes: reflections from a diabetes care editors' expert forum. Diabetes Care. 2013 Jun;36(6):1779–1788. doi: 10.2337/dc13-0512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Inzucchi SE, Bergenstal RM, Buse JB, et al. Management of hyperglycemia in type 2 diabetes: a patient-centered approach: position statement of the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD) Diabetes Care. 2012 Jun;35(6):1364–1379. doi: 10.2337/dc12-0413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.ABIM Foundation Choosing Wisely Initiative. American Geriatrics Society Item 3: Avoid using medications to achieve hemoglobin A1c<7.5% in most adults age 65 and older moderate control is generally better. [Accessed August 26, 2013];2013 http://www.americangeriatrics.org/health_care_professionals/clinical_practice/clinical_guidelines_recommendations/choosingwisely. [Google Scholar]
- 41.Cassel CK, Guest JA. Choosing wisely: helping physicians and patients make smart decisions about their care. JAMA. 2012 May 2;307(17):1801–1802. doi: 10.1001/jama.2012.476. [DOI] [PubMed] [Google Scholar]
- 42.Lipska KJ, Montori VM. Glucose control in older adults with diabetes mellitus-more harm than good? JAMA Intern Med. 2013 Jul 22;173(14):1306–1307. doi: 10.1001/jamainternmed.2013.6189. [DOI] [PubMed] [Google Scholar]
- 43.Bailey CJ, Aschner P, Del Prato S, et al. Individualized glycaemic targets and pharmacotherapy in type 2 diabetes. Diab Vasc Dis Res. 2013 May 27; doi: 10.1177/1479164113490765. [DOI] [PubMed] [Google Scholar]
- 44.Helmer DA, Sambamoorthi U, Rajan M, Tseng CL, Pogach LM. Individualized, non-age-based glycemic control in elderly veterans with diabetes. Diabetes Care. 2008 Apr;31(4):728–731. doi: 10.2337/dc07-1431. [DOI] [PubMed] [Google Scholar]
- 45.National Committee for Quality Assurance. NQF #0731, Comprehensive Diabetes Care: Hemoglobin A1c (HbA1c) Control (<8.0%) [Accessed September 9, 2013];2009 Dec 4; http://www.qualityforum.org/QPS/0575. [Google Scholar]
- 46.Pogach L, Aron D. The other side of quality improvement in diabetes for seniors: a proposal for an overtreatment glycemic measure. Arch Intern Med. 2012 Oct 22;172(19):1510–1512. doi: 10.1001/archinternmed.2012.4392. [DOI] [PubMed] [Google Scholar]
- 47.Ali MK, Bullard KM, Saaddine JB, Cowie CC, Imperatore G, Gregg EW. Achievement of goals in U.S. diabetes care, 1999–2010. N Engl J Med. 2013 Apr 25;368(17):1613–1624. doi: 10.1056/NEJMsa1213829. [DOI] [PubMed] [Google Scholar]
- 48.American Association of Diabetes Educators. AADE7 Self-Care Behaviors. Diabetes Educ. 2008 May-Jun;34(3):445–449. [Google Scholar]
- 49.Shrivastava SR, Shrivastava PS, Ramasamy J. Role of self-care in management of diabetes mellitus. J Diabetes Metab Disord. 2013;12(1):14. doi: 10.1186/2251-6581-12-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Moghissi E, Ismail-Beigi F, Devine RC. Hypoglycemia: minimizing its impact in type 2 diabetes. Endocr Pract. 2013 May-Jun;19(3):526–535. doi: 10.4158/EP13005.RA. [DOI] [PubMed] [Google Scholar]
- 51.Haas L, Maryniuk M, Beck J, et al. National standards for diabetes self-management education and support. Diabetes Care. 2012 Nov;35(11):2393–2401. doi: 10.2337/dc12-1707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Glogan D, Levitan RD, Brooks DE, Gerkin RD. Unintentional Use of Mistaken Insulin Products: A Retrospective Review of Poison Center Data. J Emerg Med. 2013 May 14; doi: 10.1016/j.jemermed.2013.01.032. [DOI] [PubMed] [Google Scholar]
- 53.Spiller HA, Borys DJ, Ryan ML, Sawyer TS, Wilson BL. Unintentional therapeutic errors involving insulin in the ambulatory setting reported to poison centers. Ann Pharmacother. 2011 Jan;45(1):17–22. doi: 10.1345/aph.1P517. [DOI] [PubMed] [Google Scholar]
- 54.Grissinger M. Avoiding Medication Errors with Insulin Therapy. [Accessed August 22, 2013];2010 http://www.schererclin.com/documents/scherer_avoiding_med_errors.pdf. [Google Scholar]
- 55.Institute for Safe Medication Practices. A clinical reminder about the safe use of insulin vials. ISMP Med Saf Alert. 2013;18(3):1–2. [Google Scholar]
- 56.Cryer PE American Diabetes Association. Hypoglycemia in diabetes : pathophysiology, prevalence, and prevention. 2nd ed. Alexandria, VA: American Diabetes Association; 2013. [Google Scholar]
- 57.Frier BM. Hypoglycaemia in the diabetic adult. Baillieres Clin Endocrinol Metab. 1993 Jul;7(3):757–777. doi: 10.1016/s0950-351x(05)80218-6. [DOI] [PubMed] [Google Scholar]
- 58.Khunti K, Fisher H, Paul S, Iqbal M, Davies MJ, Siriwardena AN. Severe hypoglycaemia requiring emergency medical assistance by ambulance services in the East Midlands: A retrospective study. Prim Care Diabetes. 2013 Jul;7(2):159–165. doi: 10.1016/j.pcd.2013.01.001. [DOI] [PubMed] [Google Scholar]
- 59.Krnacova V, Kubena A, Macek K, Bezdek M, Smahelova A, Vlcek J. Severe hypoglycaemia requiring the assistance of emergency medical services--frequency, causes and symptoms. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 2012 Sep;156(3):271–277. doi: 10.5507/bp.2012.037. [DOI] [PubMed] [Google Scholar]
- 60.Parsaik AK, Carter RE, Myers LA, et al. Population-based study of hypoglycemia in patients with type 1 diabetes mellitus requiring emergency medical services. Endocr Pract. 2012 Nov-Dec;18(6):834–841. doi: 10.4158/EP12094.OR. [DOI] [PubMed] [Google Scholar]
- 61.Farmer AJ, Brockbank KJ, Keech ML, England EJ, Deakin CD. Incidence and costs of severe hypoglycaemia requiring attendance by the emergency medical services in South Central England. Diabet Med. 2012 Nov;29(11):1447–1450. doi: 10.1111/j.1464-5491.2012.03657.x. [DOI] [PubMed] [Google Scholar]
- 62.Beuhler MC, Spiller HA, Aleguas A. Demographics and outcome of unintentional insulin overdoses managed by three poison centers. Clin Toxicol (Phila) 2013 Aug 22; doi: 10.3109/15563650.2013.829236. [DOI] [PubMed] [Google Scholar]
- 63.Cryer PE. Hypoglycemia: still the limiting factor in the glycemic management of diabetes. Endocr Pract. 2008 Sep;14(6):750–756. doi: 10.4158/EP.14.6.750. [DOI] [PubMed] [Google Scholar]
- 64.Gold AE, MacLeod KM, Frier BM. Frequency of severe hypoglycemia in patients with type I diabetes with impaired awareness of hypoglycemia. Diabetes Care. 1994 Jul;17(7):697–703. doi: 10.2337/diacare.17.7.697. [DOI] [PubMed] [Google Scholar]
- 65.Cornell S, Dorsey VJ. Diabetes pharmacotherapy in 2012: considerations in medication selection. Postgrad Med. 2012 Jul;124(4):84–94. doi: 10.3810/pgm.2012.07.2571. [DOI] [PubMed] [Google Scholar]
- 66.U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion. Healthy People 2020 Objective MPS-5: Reduce emergency department (ED) visits for common, preventable adverse events from medications. [Accessed August 23, 2013]; http://www.healthypeople.gov/2020/topicsobjectives2020/objectiveslist.aspx?topicId=27#123156.
- 67.Kern LM, Malhotra S, Barron Y, et al. Accuracy of electronically reported "meaningful use" clinical quality measures: a cross-sectional study. Ann Intern Med. 2013 Jan 15;158(2):77–83. doi: 10.7326/0003-4819-158-2-201301150-00001. [DOI] [PubMed] [Google Scholar]
- 68.Pogach L, Aron DC. Sudden acceleration of diabetes quality measures. JAMA. 2011 Feb 16;305(7):709–710. doi: 10.1001/jama.2011.153. [DOI] [PubMed] [Google Scholar]
- 69.Aron D, Rajan M, Pogach LM. Summary measures of quality of diabetes care: comparison of continuous weighted performance measurement and dichotomous thresholds. Int J Qual Health Care. 2007 Feb;19(1):29–36. doi: 10.1093/intqhc/mzl064. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.