Abstract
BACKGROUND:
Prospective studies on the incidence of VTE during severe sepsis and septic shock remain absent, hindering efficacy assessments regarding VTE prevention strategies in sepsis.
METHODS:
We prospectively studied 113 consecutively enrolled patients in the ICU with severe sepsis and septic shock at three hospitals. All patients provided informed consent. VTE thromboprophylaxis was recorded for all patients. Patients underwent ultrasonography and were followed for VTE prior to ICU discharge. All-cause 28-day mortality was recorded. Variables from univariate analyses that were associated with VTE (including central venous catheter [CVC] insertion, age, length of stay, and mechanical ventilation) were included in a multivariable logistic regression analysis using backward stepwise elimination to determine VTE predictors.
RESULTS:
Mean APACHE (Acute Physiology and Chronic Health Evaluation) II score was 18.2 ± 7.0, and age was 50 ± 18 years. Despite all patients receiving guideline-recommended thromboprophylaxis, the incidence of VTE was 37.2% (95% CI, 28.3-46.8). Most VTE events were clinically significant (defined as pulmonary embolism, proximal DVT, and/or symptomatic distal DVT) and associated with an increased length of stay (18.2 ± 9.9 days vs 13.4 ± 11.5 days, P < .05). Mortality was higher in patients with acute VTE but did not reach statistical significance. Insertion of a CVC and longer mechanical ventilation duration were significant VTE risk factors. VTE incidence did not differ by thromboprophylaxis type.
CONCLUSIONS:
To our knowledge this is the first multicenter prospective study to identify a high incidence of VTE in patients with severe sepsis and septic shock, despite the use of universal, guideline-recommended thromboprophylaxis. Our findings suggest that the systemic inflammatory milieu of sepsis may uniquely predispose patients with sepsis to VTE. More effective VTE prevention strategies are necessary in patients with sepsis.
TRIAL REGISTRY:
ClinicalTrials.gov; No.: NCT02353910; URL: www.clinicaltrials.gov
Sepsis, particularly when complicated by hypotension and shock, is considered a risk factor for VTE, including upper and lower extremity DVT and pulmonary embolism (PE).1‐4 The underlying pathogenesis of VTE in sepsis remains incompletely understood but is believed to be the result of multiple factors, including immobility, activation of thromboinflammatory pathways, disseminated intravascular coagulation, and venous stasis. VTE in patients with sepsis may also be challenging to recognize, leading to underdiagnosis and complications of hypotension, tachycardia, hypoxia, and lung injury.4‐6 As such, VTE in sepsis may contribute to increased length of stay and higher rates of adverse outcomes such as organ failure and death.
To date, there are no prospective studies investigating VTE incidence and risk factors specifically in patients with severe sepsis and septic shock. Prior, well-conducted studies were performed in more heterogeneous groups of critically ill patients that included surgical patients.1,7‐10 Sepsis is characterized by pathophysiologic processes distinct in many ways from patients in trauma, surgical, neurologic, and cardiology ICUs. This absence of data hinders assessments of the effectiveness of guideline-recommended VTE prophylaxis in severe sepsis and septic shock and limits advances in the prevention of VTE among these patients. Thus, identification of VTE incidence and risk factors in sepsis, especially in contemporary settings of universal prophylaxis, remains paramount. The purpose of this study was to prospectively determine the incidence of VTE among these patients and to identify independent risk factors for VTE.
Materials and Methods
ICU admission logs were screened for potentially eligible patients Monday through Friday (excluding weekday holidays) between 7:00 am and 5:00 pm. Consecutively identified consenting patients admitted to the ICU at one of three academic medical centers with a diagnosis of severe sepsis or septic shock were prospectively enrolled within 72 h of admission (Fig 1). The institutional review boards approved this study, and this study was registered on ClinicalTrials.gov (NCT02353910). Each patient or an authorized family member provided written, informed consent (institutional review board approval number 00028210). Sepsis was defined as systemic infection and two or more of the following: (1) temperature > 38°C or < 36°C; (2) heart rate > 90 beats/min; (3) respiratory rate > 20 breaths/min or Paco2 < 32 mm Hg; (4) WBC count > 12,000/μL, < 4,000/μL, or > 10% bands.11,12 Severe sepsis was defined as sepsis and one or more indexes of organ failure.11,12 Septic shock was defined as the presence of sepsis and the need for vasopressors to maintain systolic BP > 90 mm Hg or within 40 mm Hg of baseline, despite adequate fluid resuscitation.11,12
Figure 1 –
CONSORT diagram of the study procedures.
Exclusion criteria included an admission diagnosis of acute VTE, age < 13 years, pregnancy, severe chronic respiratory disease, severe chronic liver disease (Child-Pugh Score of 10-15), moribund patients not expected to survive 24 h, recent surgery, and acute myocardial infarction within 30 days. Severe chronic respiratory disease was defined as the following: chronic hypercapnia with Paco2 > 45 mm Hg, chronic hypoxemia with Pao2 < 55 mm Hg on Fio2 = 0.21, hospitalization within the last 6 months for respiratory failure (Paco2 > 50 mm Hg and/or Pao2 < 55 mm Hg on 0.21 Fio2), secondary polycythemia, severe pulmonary hypertension (mean PAP > 40 mm Hg), or chronic ventilator dependency.
After informed consent, demographic data, comorbid conditions, physiologic parameters, laboratory data, admission APACHE (Acute Physiology and Chronic Health Evaluation) II scores, and VTE prophylaxis regimens were recorded. Although the choice of VTE prophylaxis was left to the treating physicians, the receipt of VTE prophylaxis was recorded for all patients and then daily while they remained in the ICU. Standardized ICU protocols allowed for the use of either low-dose unfractionated heparin (UFH) administered bid or tid or low-molecular-weight heparin (LMWH) once daily as appropriate unless patients were on a vitamin K antagonist for another indication that was continued. If patients had a contraindication to pharmacologic-based VTE prophylaxis (eg, active bleeding or high risk of bleeding) knee-high sequential compression devices (SCDs) were used. Patients were evaluated for evidence of VTE during ICU care as detailed later. We also captured all-cause 28-day mortality.
Evaluation for Signs and Symptoms of DVT
Immediately prior to compression ultrasonography (CUS), trained clinical research staff evaluated patients for signs and symptoms consistent with DVT using a standardized assessment that was defined a priori. Specifically, each patient was assessed for the following: (1) localized tenderness, (2) swelling, (3) pitting edema, and/or (4) erythema in each lower extremity. If a central venous catheter (CVC) was present, the presence or absence of these symptoms was also assessed in the upper extremity. Patients with one or more of these were coded as having signs or symptoms consistent with DVT.
Compression Ultrasonography
Lower extremity CUS was performed by registered vascular technologists in standardized fashion.13 If an indwelling CVC had been placed, we also performed ultrasound examinations of the upper extremity where the CVC was placed. The deep veins of the thigh, calf, and arms, specifically the common femoral, femoral, popliteal, posterior tibial, gastrocnemius, soleal sinus, peroneal, internal jugular, subclavian, axillary, and brachial veins, were identified and compressed sequentially in 1- to 2-cm increments. Lack of venous compressibility with the ultrasound transducer held in a transverse position to the vein was interpreted as a positive study.
Per protocol, CUS was performed prior to ICU discharge in all patients. At any time during the study, the patient’s ICU team could also perform CUS if DVT was clinically suspected. These CUSs were performed in an identical manner and recorded as clinically indicated CUS. Patients who had a CUS ordered for clinical suspicion of DVT had a second, predischarge CUS if the first CUS was negative. All patients were also followed for the development of symptomatic PE or DVT until ICU discharge.
All CUSs were interpreted by board-certified vascular surgeons blinded to the patient’s clinical history. CUSs were coded as negative (DVT absent) if all imaged deep vein segments were fully compressible or as positive (DVT present) if a noncompressible segment was identified. Proximal DVT was defined as acute-appearing thrombosis involving the popliteal and/or more proximal lower extremity deep vein segments or any deep vein segment in the upper extremity. Distal DVT was defined as acute-appearing thrombosis in any deep vein segment distal to the popliteal vein. Superficial vein thrombosis and chronic-appearing thrombosis was coded as DVT absent. Clinically significant VTE was defined as PE, proximal symptomatic or asymptomatic DVT, and symptomatic distal DVT.9,14,15 Decisions on VTE treatment were left to the discretion of the patient’s primary team.
Statistical Analysis
Data were examined for normality using skewness and kurtosis tests. Groups were compared using the Student t test or Wilcoxon rank sum (for continuous variables) and using the χ2 or Fisher exact test (for categorical variables), as appropriate (STATA v11.0). Central tendency data are reported as the mean (± SD) or median (interquartile range) if the distribution was skewed. VTE prophylaxis rates are reported as percentages and 95% CI. To determine if baseline risk factors were associated with VTE, we conducted univariate and multivariable logistic regression analyses. Independent, prespecified variables included in these analyses were age, sex, weight, BMI, admission APACHE II score, the presence of shock requiring vasopressors upon admission, the presence of a CVC prior to VTE, mechanical ventilation, ventilator-free days, tobacco use, congestive heart failure, active malignancy, admission laboratory values (eg, platelet count, WBC count, creatinine, fibrinogen, C-reactive protein), and the type of prophylaxis (eg, UFH, LMWH, or mechanical devices). Variables from univariate analyses that were associated with VTE (P value < .1) were then included in a multivariable logistic regression analysis using backward stepwise elimination. ORs and 95% CIs were calculated for all significant predictors retained in the final analysis. A P value < .05 was considered statistically significant.
Results
We prospectively enrolled 113 consecutively identified patients in the ICU with severe sepsis or septic shock (Fig 1, Table 1). Upon study entry, the mean APACHE II score was 18.2, > 50% of patients had shock requiring vasopressors, and > 75% required mechanical ventilation (Table 1). Overall, 61.1% of patients (69 of 113) had a CVC placed as part of their ICU care. More than 50% of patients had obesity, a known risk factor for VTE (Table 1). All-cause 28-day mortality was 21.2% (95% CI, 14.1-30.0).
TABLE 1 ] .
Characteristics of Patients With Severe Sepsis and Septic Shock
| Characteristic | Critically Ill Patients With Sepsis (N = 113) |
| Age, y | 50 ± 18 |
| Male sex | 53 (47) |
| BMI, kg/m2 | 31.7 ± 9.8 |
| APACHE II score | 18.2 ± 7.0 |
| Shock requiring vasopressors | 61 (54) |
| Mechanical ventilation | 87 (77) |
| 28-d mortality | 24 (21.2) |
| ICU LOS, median (IQR), d | 14.8 (7, 21) |
| Comorbid risk factors | |
| Obesity (BMI ≥ 30 kg/m2) | 60 (53.1) |
| CHF | 5 (4.4) |
| Active cancer | 4 (3.5) |
| CVD | 13 (11.5) |
Data presented as No. (%) or mean ± SD unless otherwise specified. APACHE = Acute Physiology and Chronic Health Evaluation; CHF = congestive heart failure; CVD = cardiovascular disease; IQR = interquartile range; LOS = length of stay.
Overall, 80.5% (91 of 113) of patients had VTE chemoprophylaxis prescribed, mostly UFH (49 of 91, 53.8%), followed by LMWH (38 of 91, 41.8%). A small percentage of patients had their previously prescribed warfarin continued (three of 91, 2.7%). SCDs were prescribed for the remainder of patients (19.5%, 22 of 113) not given anticoagulant-based VTE prophylaxis because of a contraindication, such as bleeding or coagulopathy. All VTE prophylaxis was appropriate and consistent with current institutional and national guidelines.15
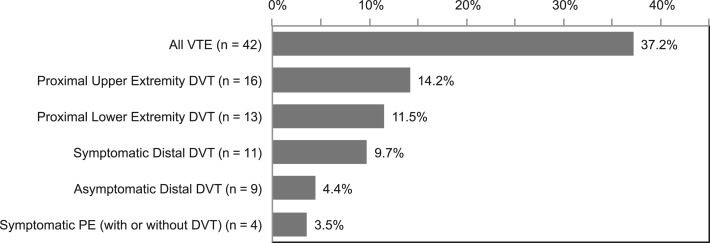
The primary outcome of acute VTE of any type (including upper and lower extremity DVT and symptomatic PE) occurred in 42 patients (37.2%; 95% CI, 28.3-46.8) (Fig 2). The majority of patients (76%, 32 of 42) had symptomatic DVT at the time CUS was performed. Among patients with a CVC, 23.2% (16 of 69) had CVC-associated upper extremity DVT. The majority of CUSs (110 of 113, 97.3%) were performed as a screening evaluation per the study protocol at the time of ICU discharge. Only three patients (2.7%) had a CUS performed at the request of their primary ICU team because of clinical suspicion of venous thrombosis and, in two of these three patients (66%), acute DVT was present. Clinically significant VTE occurred in 88.1% of patients (37 of 42). Isolated asymptomatic distal DVT, the clinical significance of which remains uncertain, occurred in 11.9% (five of 42) of patients.
Figure 2 –
The incidence of VTE among patients (N = 113) with severe sepsis or septic shock. Shown is the incidence of VTE of any type (All VTE) and the individual types of venous thromboembolic events, which include proximal DVT in the upper extremities, proximal DVT in the lower extremities, distal symptomatic DVT, distal asymptomatic DVT, and symptomatic PE. Patients with sepsis may have had one or more thromboses (eg DVT and PE). PE = pulmonary embolism.
Patients with sepsis with clinically significant VTE had a significantly longer ICU length of stay compared with patients without VTE (13.4 ± 11.5 days vs 18.2 ± 9.9 days, P < .05). ICU length of stay in patients with sepsis with isolated, asymptomatic distal DVT did not differ from patients without VTE (10.4 ± 3.3 vs 13.4 ± 11.5, P = .57). All-cause, 28-day mortality was numerically higher in patients with clinically significant VTE but did not reach statistical significance (28.6% vs 17.6%, P = .18)
The incidence of VTE did not differ between patients receiving LMWH compared with UFH (33.3% vs 41.3%, respectively; P = .43). Similarly, there was no difference in the incidence of VTE between patients receiving pharmacologic-based prophylaxis compared with SCDs (37.3% vs 36.3%, respectively; P = .93). When total chemoprophylaxis was determined (defined as the percentage of ICU days a patient received chemoprophylaxis), there was no difference between patients with or without VTE (Table 2). In addition, patients received either LMWH or UFH for chemoprophylaxis during > 90% of the time they were in the ICU (Table 2), demonstrating high use of VTE chemoprophylaxis in these patients with sepsis. The duration of prophylaxis did not differ between patients with proximal or distal DVT (P = .67).
TABLE 2 ] .
Percentage (95% CI) of Total ICU Days With Chemoprophylaxis
| Chemoprophylaxis | No VTE | VTE | P Value |
| LMWH | 96.3 (90.3-100) | 95.3 (86.1-100) | .84 |
| UFH | 91.9 (85.0-98.8) | 90.8 (80.0-100) | .85 |
For patients with ICU-acquired VTE, percentage was calculated based on d prior to VTE diagnosis. LMWH = low-molecular-weight heparin; UFH = unfractionated heparin.
In univariate regression analyses, we identified several factors independently associated with VTE, including age, ICU length of stay, the need for mechanical ventilation upon admission, the presence of an indwelling CVC, and the duration of mechanical ventilation (Table 3). Active cancer was also significantly associated with VTE in univariate analyses (P = .008) but omitted from further multivariable analyses because of the small number of patients with cancer (n = 4) in our cohort. We explored other potential predictors, including illness severity (as determined by APACHE II scores), the presence of shock, BMI, age, sex, plasma fibrinogen levels, and platelet counts, but none of these was significantly associated with VTE in univariate analyses.
TABLE 3 ] .
Relationship Between VTE and Risk Factors
| Risk Factor | Univariate OR (95% CI) | P Value | Multivariable OR (95% CI) | P Value |
| Presence of CVC | 4.37 (1.77-10.74) | .001 | 2.82 (1.07-7.38) | .03 |
| ICU LOS, d | 1.03 (0.99-1.06) | .08 | … | … |
| Age, y | 1.01 (0.99-1.04) | .09 | … | … |
| Need for mechanical ventilation | 2.35 (0.85-6.44) | .09 | 3.55 (0.92-13.6) | .06 |
| Duration of mechanical ventilation, d | 1.07 (1.01-1.13) | .02 | 1.14 (1.00-1.29) | .04 |
Results presented as OR (95% CI). Relationships between VTE and several risk factors were first tested in stepwise fashion by univariate regression analyses. We identified two independent factors in subsequent multivariable regression analyses. CVC = central venous catheter. See Table 1 legend for expansion of other abbreviation.
In multivariable analyses, two factors remained as significant VTE risk factors: the presence of an indwelling CVC and the duration of mechanical ventilation (Table 3). The need for mechanical ventilation upon ICU admission was associated with a 3.5-fold higher risk for VTE in multivariable analyses but did not reach statistical significance (P = .06). In secondary multivariable analyses, where patients with upper extremity DVT were excluded, CVC use remained a significant risk factor for isolated lower extremity DVT and PE (OR, 2.62; 95% CI, 1.01-6.77).
Discussion
To our knowledge, this is the first prospective, multicenter study to investigate VTE incidence, outcomes, and risk factors in patients admitted to the ICU with severe sepsis and septic shock. We identified a high incidence of VTE (37.2%) in patients with sepsis despite the use of universal, guideline-recommended thromboprophylaxis. The majority of patients (88%) had clinically significant VTE (symptomatic PE, proximal DVT, or symptomatic distal DVT) that influenced clinical management and was also associated with a significantly longer ICU length of stay.
Our findings identify that critically ill patients with sepsis have a markedly higher incidence of VTE compared with published reports in patients in the ICU primarily without sepsis. For example, Cook and colleagues2 observed a VTE incidence of 5.4% among 93 patients in a medical-surgical ICU, where the majority (93.5%) of admissions were for noninfectious illnesses (eg, cardiovascular, respiratory, neurologic, or GI). Similarly, in a prospective study of 261 critically ill patients, the incidence of DVT was 9.6%, and the majority of patients (94.6%) had a primary admission diagnosis other than sepsis.10 Finally, in a retrospective review of 600 patients with critical illness, only 3.0% developed VTE during their ICU stay, with most events occurring in neurosurgical patients.16 Thus, our study builds on and extends the current literature by demonstrating that compared with patients admitted to the ICU for reasons other than sepsis, patients with sepsis have a markedly (approximately 3- to 10-fold higher) incidence of VTE. Moreover, the high incidence of VTE in our cohort occurred despite the universal use of guideline-recommended VTE prophylaxis.
As VTE chemoprophylaxis was prescribed > 90% of the days that patients with sepsis were in the ICU, the high incidence of VTE is unlikely to be attributable to suboptimal or inappropriate VTE thromboprophylaxis. Rather, since the incidence in patients with sepsis in our multicenter cohort was much higher than other well-conducted published studies in critical illness due to surgery, trauma, cardiovascular disease, neurologic disease, and other processes,2,10 our findings suggest that dysregulated hemostasis and coagulation in severe sepsis and septic shock differ from that of other, noninfectious critical illnesses. Although exact mechanisms remain incompletely understood, sepsis induces a marked proinflammatory and prothrombotic systemic milieu. These dysregulated responses include cellular activation responses, deposition of platelet-fibrin thrombi within the vasculature, and the development of disseminated intravascular coagulation.12,17‐22 These and other factors lead to hypercoagulability and may explain, in part, the high incidence of VTE in patients with sepsis identified in the current study.
In addition, our findings highlight that currently recommended VTE prophylaxis strategies may not be as effective in severe sepsis and septic shock compared with noninfectious critically ill populations. As such, clinical trials specifically studying thromboprophylaxis in patients with severe sepsis and septic shock are necessary to improve the prevention of VTE in septic syndromes.
Our findings also have several clinical implications for providers treating patients with severe sepsis or septic shock. First, since all patients received guideline-recommended thromboprophylaxis, the high incidence of VTE was not merely reflective of a failure to provide thromboprophylaxis. Rather, our study suggests that patients with sepsis frequently develop clinically significant VTE despite receiving guideline-recommended thromboprophylaxis. Thus, clinicians should maintain a high clinical suspicion for VTE in patients with severe sepsis or septic shock, even when appropriate VTE prophylaxis has been used. Additional studies investigating whether higher doses of heparinoids or combination prophylaxis with both heparinoids and mechanical devices may be more effective in patients with sepsis, particularly given the increasing incidence of obesity, are needed.
In addition, we identified that the presence of a CVC and the duration of mechanical ventilation were predictors of VTE. CVC use was associated with the greatest increased VTE risk (almost threefold higher risk), which builds on studies in patients without sepsis,2,5,23 and which we now identify as being a risk factor in severe sepsis and septic shock as well. We also report the novel finding that CVC use was significantly associated with isolated lower extremity DVT and PE, not just upper extremity DVT.
These findings highlight the importance of removing CVCs when no longer necessary; minimizing the size of CVCs, including peripherally inserted central catheters; and standardized approaches to mechanical ventilation weaning protocols and early physical therapy including ambulation of patients who are mechanically ventilated, as identified in other studies.2,23 Active cancer was also a strong, independent risk factor for VTE, consistent with published investigations of VTE and cancer in patients without sepsis, although the small number of patients with cancer in our cohort precludes firm conclusions.
The strengths of our study include its multicenter, prospective design; blinding of the vascular surgeons interpreting the CUS; comprehensive data collection; and our tracking of the type and duration of thromboprophylaxis. The majority of VTEs in our cohort were clinically significant and influenced medical management. Moreover, the development of VTE was associated with an approximately 5-day longer ICU length of stay, although our study was not designed to determine if this was causal. Mortality was higher in patients with VTE but did not reach statistical significance. These findings suggest that ICU-acquired VTE impacts clinical care and patient outcomes, although larger studies are needed to further evaluate the clinical impact of ICU-acquired VTE. Finally, although the majority of patients had signs or symptoms consistent with acute DVT at the time CUS was performed per study protocol, only three patients had CUS ordered by their primary team because of clinical suspicion for DVT. Recognizing VTE in patients with sepsis remains challenging, as the signs and symptoms of VTE may be mistaken for other processes.4‐6 Although routine screening for DVT in asymptomatic patients has not been recommended, clinicians should maintain a low threshold for evaluating the development of VTE in patients with severe sepsis and septic shock.
Limitations of our study include VTE risk factors such as thrombophilia and prior VTE that were not included in our model and the smaller sample size of a pilot study of this nature. Although our study was designed as a pilot study, the high incidence of VTE we identified in patients with sepsis warrants larger prospective studies in this high-risk population. In addition, since lower extremity symptoms of pain, swelling, and erythema in patients with sepsis may be due to DVT, immobility, fluid resuscitation, infection, or other causes, our findings support the prompt evaluation of patients with sepsis when VTE is suspected. Finally, we cannot completely exclude the possibility of VTE that occurred prior to ICU admission, although we attempted to mitigate this possibility by excluding patients with recent surgery, myocardial infarction, hospital admission, or severe chronic respiratory disease.
Conclusions
In conclusion, patients with severe sepsis and septic shock have a high incidence of VTE, despite the use of universal, guideline-recommended thromboprophylaxis. More effective VTE prevention strategies are necessary in patients with sepsis, and future research in this population is urgently needed. Among these high-risk patients, removing CVCs when no longer necessary, minimizing the size of CVCs or avoiding their use when feasible, and strategies for early extubation may reduce the incidence of VTE in sepsis.
Acknowledgments
Author contributions: M. T. R. had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis, including and especially any adverse effects. D. K. contributed to data analysis, critical writing, and intellectual content; T. C. C. contributed to statistical analysis and intellectual content; C. G. E., S. M., and R. C. P. contributed to critical writing and intellectual content; L. W. K., A. S. W., C. K. G., G. A. Z., and M. T. R. contributed to study design, critical writing, and intellectual content. All authors have approved the final version of the manuscript.
Conflict of interest: C. G. E. has been a paid consultant for Janssen Research and Development, LLC in the design and conduct of a study to reduce venous thromboembolic risk. C. K. G. receives grant support for research on sepsis from the National Institutes of Health and from the Intermountain Research and Medical Foundation. G. A. Z. is a recipient of grants from the National Institutes of Health. None declared (D. K., T. C. C., S. M., R. C. P., L. W. K., A. S. W., M. T. R.).
Role of sponsors: The sponsors had no role in the design of the study, the collection and analysis of the data, or the preparation of the manuscript.
Other contributions: We thank Diana Lim, MS, for figure and table preparation and Alex Greer, BS, for her editorial assistance. We also thank all the patients who participated in this study.
ABBREVIATIONS
- APACHE
Acute Physiology and Chronic Health Evaluation
- CUS
compression ultrasonography
- CVC
central venous catheter
- LMWH
low-molecular-weight heparin
- PE
pulmonary embolism
- SCD
sequential compression device
- UFH
unfractionated heparin
Footnotes
FUNDING/SUPPORT: This work was supported by the National Institutes of Health [Grants HL092161 to M. T. R. and HL112311 to A. S. W.) and the National Institute on Aging [Grants AG040631 and AG048022 to M. T. R.]. This work was also supported by the University of Utah Study Design and Biostatistics Center, with funding in part from the National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health [Grant 8UL1TR000105 (formerly UL1RR025764)].
Reproduction of this article is prohibited without written permission from the American College of Chest Physicians. See online for more details.
References
- 1.Attia J, Ray JG, Cook DJ, Douketis J, Ginsberg JS, Geerts WH. Deep vein thrombosis and its prevention in critically ill adults. Arch Intern Med. 2001;161(10):1268-1279. [DOI] [PubMed] [Google Scholar]
- 2.Cook D, Attia J, Weaver B, McDonald E, Meade M, Crowther M. Venous thromboembolic disease: an observational study in medical-surgical intensive care unit patients. J Crit Care. 2000;15(4):127-132. [DOI] [PubMed] [Google Scholar]
- 3.Ribic C, Lim W, Cook D, Crowther M. Low-molecular-weight heparin thromboprophylaxis in medical-surgical critically ill patients: a systematic review. J Crit Care. 2009;24(2):197-205. [DOI] [PubMed] [Google Scholar]
- 4.Marik PE, Andrews L, Maini B. The incidence of deep venous thrombosis in ICU patients. Chest. 1997;111(3):661-664. [DOI] [PubMed] [Google Scholar]
- 5.Hirsch DR, Ingenito EP, Goldhaber SZ. Prevalence of deep venous thrombosis among patients in medical intensive care. JAMA. 1995;274(4):335-337. [PubMed] [Google Scholar]
- 6.Twigg SJ, McCrirrick A, Sanderson PM. A comparison of post mortem findings with post hoc estimated clinical diagnoses of patients who die in a United Kingdom intensive care unit. Intensive Care Med. 2001;27(4):706-710. [DOI] [PubMed] [Google Scholar]
- 7.Cook D, McMullin J, Hodder R, et al. ; Canadian ICU Directors Group. Prevention and diagnosis of venous thromboembolism in critically ill patients: a Canadian survey. Crit Care. 2001;5(6):336-342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lacherade JC, Cook D, Heyland D, Chrusch C, Brochard L, Brun-Buisson C; French and Canadian ICU Directors Groups. Prevention of venous thromboembolism in critically ill medical patients: a Franco-Canadian cross-sectional study. J Crit Care. 2003;18(4):228-237. [DOI] [PubMed] [Google Scholar]
- 9.Cook D, Meade M, Guyatt G, et al. ; Canadian Critical Care Trials Group. Clinically important deep vein thrombosis in the intensive care unit: a survey of intensivists. Crit Care. 2004;8(3):R145-R152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cook D, Crowther M, Meade M, et al. Deep venous thrombosis in medical-surgical critically ill patients: prevalence, incidence, and risk factors. Crit Care Med. 2005;33(7):1565-1571. [DOI] [PubMed] [Google Scholar]
- 11.American College of Chest Physicians/Society of Critical Care Medicine Consensus Conference: definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. Crit Care Med. 1992;20(6):864-874. [PubMed] [Google Scholar]
- 12.Dellinger RP, Levy MM, Rhodes A, et al. ; Surviving Sepsis Campaign Guidelines Committee including the Pediatric Subgroup. Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock: 2012. Crit Care Med. 2013;41(2):580-637. [DOI] [PubMed] [Google Scholar]
- 13.Talbot SR. B-mode evaluation of peripheral veins. Semin Ultrasound CT MR. 1988;9(4):295-319. [PubMed] [Google Scholar]
- 14.Kahn SR, Lim W, Dunn AS, et al. Prevention of VTE in nonsurgical patients: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2012;141(2_suppl):e195S-e226S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kearon C, Akl EA, Comerota AJ, et al. Antithrombotic therapy for VTE disease: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2012;141(2_suppl):e419S-e494S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Muscedere JG, Heyland DK, Cook D. Venous thromboembolism in critical illness in a community intensive care unit. J Crit Care. 2007;22(4):285-289. [DOI] [PubMed] [Google Scholar]
- 17.Rondina MT, Fraughton T, et al. Platelet-monocyte aggregate formation and mortality risk in older patients with severe sepsis and septic shock. J Gerontol A Biol Sci Med Sci. 2015;70(2):225-231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rondina MT, Weyrich AS, Zimmerman GA. Platelets as cellular effectors of inflammation in vascular diseases. Circ Res. 2013;112(11):1506-1519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rondina MT, Brewster B, Grissom CK, et al. In vivo platelet activation in critically ill patients with primary 2009 influenza A(H1N1). Chest. 2012;141(6):1490-1495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rondina MT, Schwertz H, Harris ES, et al. The septic milieu triggers expression of spliced tissue factor mRNA in human platelets. J Thromb Haemost. 2011;9(4):748-758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Harris ES, Rondina MT, Schwertz H, Weyrich AS, Zimmerman GA. Pathogenesis of sepsis and sepsis-induced acute lung injury. In: Choi AMK, ed. Acute Respiratory Distress Syndrome. New York, NY: Informa Healthcare; 2010:369-419. [Google Scholar]
- 22.Levi M. The coagulant response in sepsis and inflammation. Hamostaseologie. 2010;30(1):10-12, 14-16. [PubMed] [Google Scholar]
- 23.Evans RS, Sharp JH, Linford LH, et al. Risk of symptomatic DVT associated with peripherally inserted central catheters. Chest. 2010;138(4):803-810. [DOI] [PubMed] [Google Scholar]