Abstract
Objective:
We sought to determine the safety of IV thrombolysis (IVT) in acute ischemic stroke (AIS) patients harboring unruptured intracranial aneurysm (UIA) in a multicenter study and a comprehensive meta-analysis of available case series.
Methods:
We analyzed prospectively collected data from consecutive AIS patients treated with IVT during a 4-year period at 4 tertiary-care stroke centers. All patients routinely underwent CT or magnetic resonance angiography during hospitalization. The presence of UIA was documented on the basis of neuroradiology reports. Symptomatic intracranial hemorrhage (sICH) was defined as imaging evidence of ICH combined with an increase in NIH Stroke Scale score of ≥4 points. A systematic meta-analysis of case series reporting safety of IVT in AIS with concomitant UIA was conducted according to PRISMA recommendations.
Results:
Among 1,398 AIS patients treated with IVT, we identified 42 cases (3.0%) harboring a total of 48 UIAs. The rates of symptomatic and asymptomatic ICH were 2.4% (95% confidence interval [CI] by adjusted Wald method: 0%–12.6%) and 7.1% (95% CI: 1.8%–19.7%), respectively. A total of 5 case series met our inclusion criteria for meta-analysis, and the pooled rate of sICH among 120 IVT-treated AIS patients harboring UIA was 6.7% (95% CI: 3.1%–13.7%). In the overall analysis of 5 case-series studies, the risk ratio of sICH did not differ between AIS patients with and without UIA (risk ratio = 1.60; 95% CI: 0.54–4.77; p = 0.40) with no evidence of heterogeneity across included studies (I2 = 22% and p = 0.27 for Cochran Q test).
Conclusions:
Our prospectively collected multicenter data, coupled with the findings of the meta-analysis, indicate the potential safety of IVT in AIS patients with UIA.
The most feared complication of IV thrombolysis (IVT) for the treatment of acute ischemic stroke (AIS) is symptomatic intracranial hemorrhage (sICH), which is associated with substantial increase in mortality and morbidity.1,2 Incidental unruptured intracranial aneurysms (UIAs) are not uncommon in AIS patients (because of shared risk factors for aneurysm formation)3,4 and it has been postulated that these patients should be excluded from IVT in view of the theoretical risk of aneurysm rupture postthrombolysis. The former hypothesis was based on single case reports of AIS patients with concomitant undiagnosed UIA that developed sICH due to aneurysmal rupture as a complication of IVT.5–7 However, small retrospective case series collecting data from a single8–11 or 2 centers12 have reported that sICH risk is not increased in AIS patients with coexisting UIA in comparison to those with absent intracranial aneurysms or vascular malformations.
In view of former considerations, the aim of the present multicenter study was to determine the safety of IVT in AIS patients harboring UIAs. We also conducted a comprehensive meta-analysis of reported case series.
METHODS
Multicenter study.
We evaluated consecutive patients treated with IVT according to the American Heart Association recommendations13 from 4 tertiary-care stroke centers during the 4-year study period (2011–2014): Methodist University Hospital (Memphis, TN), National University Hospital (Singapore), Carl Gustav Carus University Hospital (Dresden, Germany), and Attikon University Hospital (Athens, Greece). Noncontrast head CT, pretreatment NIH Stroke Scale (NIHSS) score, and modified Rankin Scale score at discharge were obtained as standard of care as previously described.14,15 Pretreatment systolic and diastolic blood pressure levels were measured using automated or manual cuffs. Additional details regarding our international collaborative group that has been evaluating the safety and efficacy of acute reperfusion therapies in patients with AIS have been previously described.16,17
Vascular neuroimaging including magnetic resonance angiography (MRA), time-of-flight MRA, or CT angiography (CTA) was performed during hospitalization (before or after administration of IVT) as part of standard diagnostic workup in all cases. Neuroimaging reports were reviewed and information regarding the presence of incidental UIA was abstracted. Digital subtraction angiography was performed as a supplemental neuroimaging test in selected cases according to the treating physician's discretion. We also obtained additional data regarding type, location, and diameters of UIAs from formal neuroradiology reports. We defined sICH as imaging evidence of ICH on brain CT with NIHSS score increase of ≥4 points.14,15 Asymptomatic ICH was defined as imaging evidence of ICH (hemorrhagic transformation or parenchymal hematoma) on brain CT without clinical worsening.16 Finally, 2 certified stroke neurologists who were not involved with the management of cases in any center independently determined whether sICH was caused by aneurysmal rupture in AIS patients harboring UIA complicated by intracranial bleeding postthrombolysis. All cases with unavailable vascular neuroimaging data were excluded from the present analyses.
Comprehensive meta-analysis.
This meta-analysis has adopted the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines for systematic reviews and meta-analyses18 and was written according to the MOOSE (Meta-analysis of Observational Studies in Epidemiology) proposal.19–21 Eligible observational studies reporting the use of IVT in AIS patients with coexisting incidental UIA were identified by searching MEDLINE and Scopus. The following combination of search strings was used in both database searches: “stroke,” “cerebral ischemia,” “thrombolysis,” “aneurysm,” “malformation,” “congenital abnormality,” and “alteplase.” No language or other restrictions were imposed. Last literature search was conducted on March 15, 2015. Reference lists of all articles that met the inclusion criteria and of relevant review articles were examined to identify studies that may have been missed by the database search. All retrieved studies and reference lists were scanned independently by 2 reviewers (N.G. and G.T.). There were no discrepancies between the 2 authors in the final presentation of the literature search results. Both prospective and retrospective study protocols were included in the present analysis. Case reports and case series with fewer than 5 patients were excluded from the final analysis. Data regarding location, type, maximal diameters of intracranial aneurysms, and rates of asymptomatic or symptomatic ICH were abstracted for all retrieved reports.
Standard protocol approvals, registrations, and patient consents.
The study was approved by the corresponding institutional ethical standards committees in each participating center and written informed consent was obtained from all patients or guardians before the administration of tissue plasminogen activator (tPA).
Statistical analyses.
Multicenter study.
Continuous variables are presented as mean ± SD (normal distribution) and as median with interquartile range (skewed distribution). Categorical variables are presented as percentages with their corresponding 95% confidence intervals (CIs). The adjusted Wald method, which provides the best coverage for binomial CI when samples are less than ≈150,22 was used for computation of 95% CI of asymptomatic and symptomatic ICH among patients with AIS and concomitant UIA. The Statistical Package for Social Science version 13.0 (SPSS Inc., Chicago, IL) for Windows was used for statistical analyses.
Meta-analysis.
For each study, the numbers of events in IVT-treated stroke patients with and without UIA were identified and a risk ratio (RR) was calculated. For studies with a zero cell, we used a continuity correction of 0.5, as appropriate. In cases of 2 or more zero cells, the assumption of continuity correction was not used and the corresponding point estimates were designated as “not estimable.”23 The overall RR for all pooled studies was computed using the random effects method (DerSimonian and Laird). Heterogeneity between studies was assessed using the Cochran Q and I2 statistic as previously described.20 Heterogeneity was considered as statistically significant when the p value derived from Cochran Q was <0.1. For the qualitative interpretation of heterogeneity, I2 values of at least 50% are usually considered to represent substantial heterogeneity, while values of at least 75% indicate considerable heterogeneity according to the Cochrane Handbook.24 Publication bias was assessed at the overall analysis graphically using a funnel plot and with the Egger test for funnel plot asymmetry.25,26
Statistical analyses were conducted using RevMan version 5.3 software (The Nordic Cochrane Centre, The Cochrane Collaboration, Copenhagen) and Comprehensive Meta-analysis version 2 software (Biostat, Englewood, NJ).
RESULTS
Multicenter study data.
Our multicenter study evaluated a total of 1,398 AIS patients treated with IVT with available neurovascular imaging data. The presence of concomitant UIAs was identified in 42 cases (3.0%; 95% CI by adjusted Wald method: 2.2%–4.1%) harboring a total of 48 intracranial aneurysms. Four of the 42 AIS patients (8%) had multiple aneurysms. Baseline characteristics of the study population (mean age 63 ± 13 years, 26%, median NIHSS score 9 points, interquartile range 6–14) are presented in table 1. Pretreatment with oral anticoagulants and single and dual antiplatelet therapy was prevalent in 2.4%, 42.9%, and 2.4% of the study population. Table e-1 on the Neurology® Web site at Neurology.org summarizes the anatomical features of the 48 incidental UIAs that were identified in our study population. The mean maximum diameter of UIAs was 4.3 ± 2.7 mm ranging between 2 and 15 mm. Nearly all UIAs were saccular (45/48, 94%) and the majority were located in the anterior circulation (29/48, 61%). The maximum diameter was ≥7 mm and ≥10 mm in 6 (12.5%) and 3 (6.3%) cases, respectively.
Table 1.
Baseline characteristics and outcome variables in acute ischemic stroke patients with coexisting unruptured intracranial aneurysms (n = 42) treated with IV thrombolysis
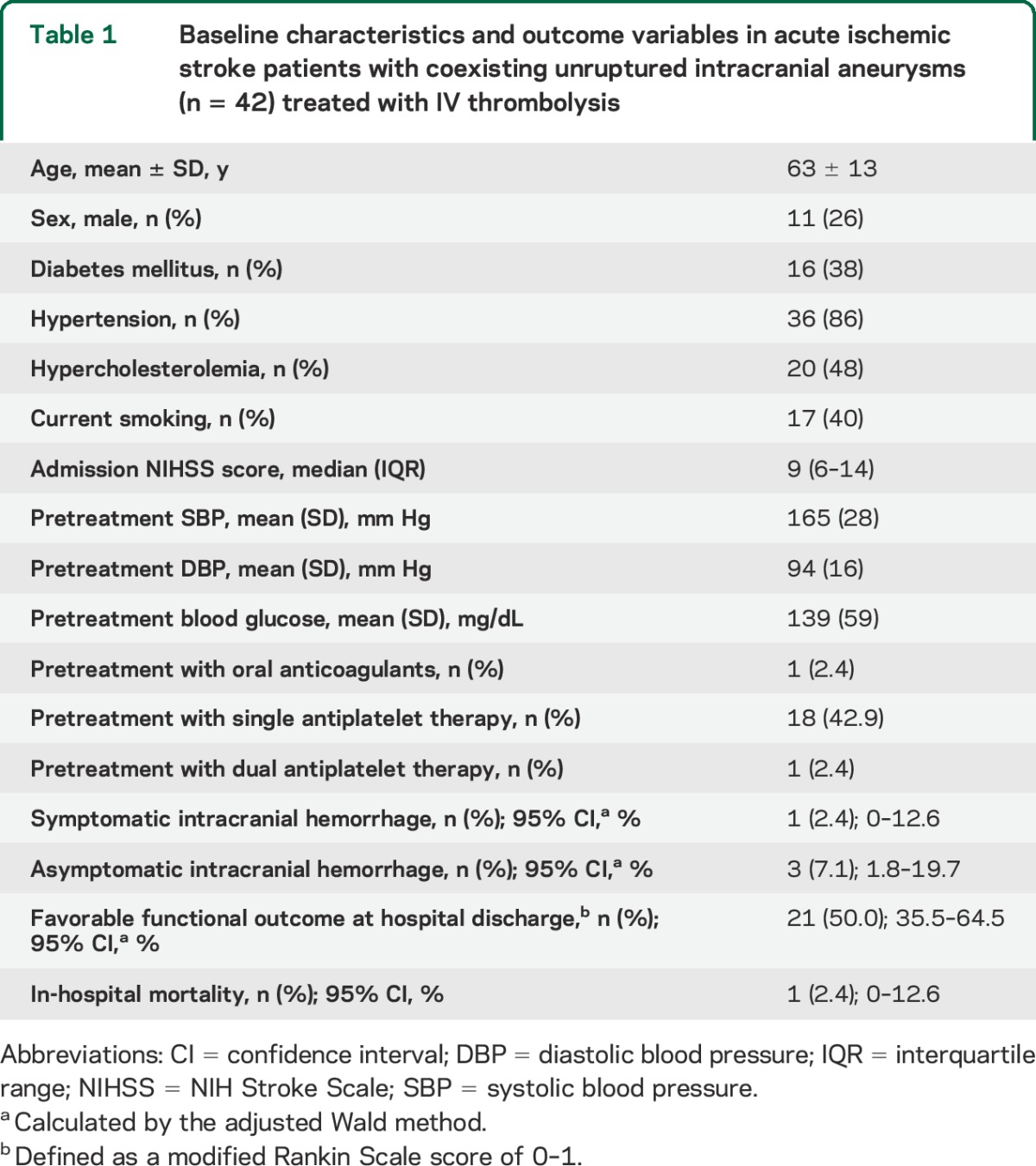
The rates of symptomatic and asymptomatic ICH were 2.4% (95% CI by adjusted Wald method: 0%–12.6%) and 7.1% (95% CI by adjusted Wald method: 1.8%–19.7%), respectively. The single sICH reported in our multicenter study was not caused by aneurysmal rupture, since the incidental aneurysm was located in the posterior communicating artery in the hemisphere that was contralateral to the sICH. Among the study population (1,398 AIS patients treated with IVT), there was no case of fatal sICH that did not undergo vascular imaging with CTA or MRA. The rates of in-hospital mortality and favorable functional outcome at hospital discharge (defined as modified Rankin Scale score of 0–1) were 2.4% (95% CI by adjusted Wald method: 0%–12.6%) and 50.0% (95% CI by adjusted Wald method: 35.5%–64.5%), respectively.
Meta-analysis of case series.
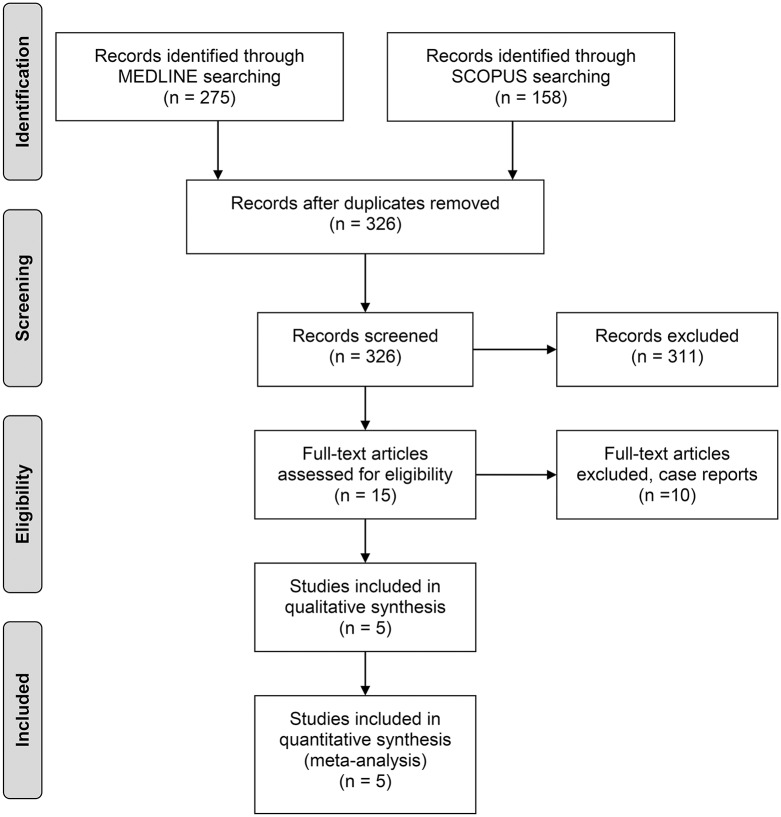
MEDLINE and Scopus database searches yielded 275 and 158 results, respectively. After removing duplicates, the titles and abstracts from the remaining 326 studies were screened and 15 potentially eligible studies for the meta-analysis were retained. After retrieving the full-text version of the aforementioned 15 studies, 10 studies were excluded because they reported case reports of single patients or they reported case series of fewer than 5 AIS patients with UIA treated with IVT.5–7,27–33 Characteristics of patients in excluded studies are available in table e-2. In the final presentation of the literature search results, there was no conflict or disagreement between the 2 reviewers, and the 5 studies that met the study protocol's inclusion criteria8–12 together with the data from the present study protocol were included both in the qualitative and quantitative synthesis (figure 1). The baseline characteristics and outcomes of the case series included in the present meta-analysis are summarized in table 2.
Figure 1. Flowchart diagram presenting the selection of eligible studies.
Table 2.
Baseline characteristics and outcomes of the case series included in the present meta-analysis (n = 6)
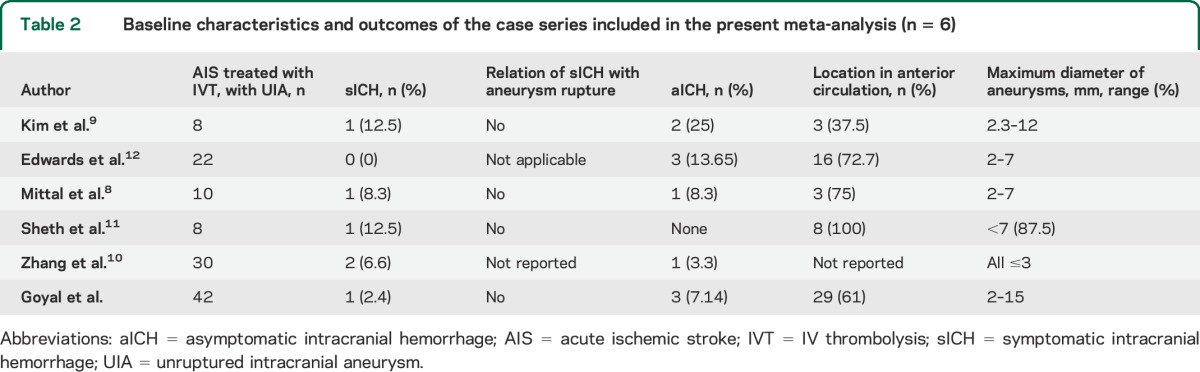
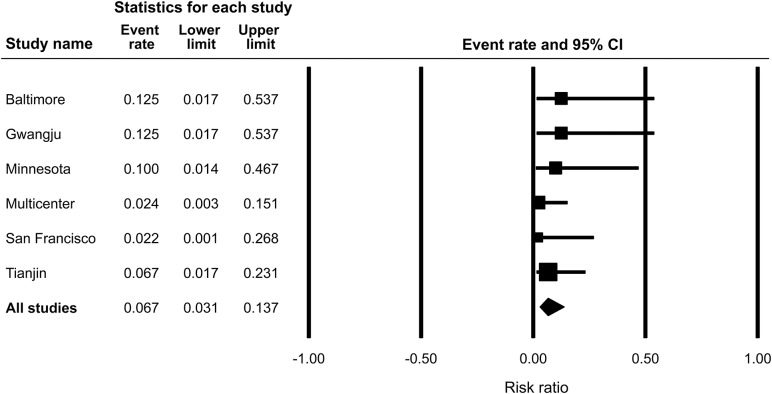
The pooled rate of sICH among 120 AIS patients harboring UIAs who were treated with IVT was 6.7% (95% CI: 3.1%–13.7%; figure 2). Publication bias was not evident in either the funnel plot inspection (figure e-1) or in the Egger statistical test for funnel plot asymmetry (p = 0.791). No heterogeneity (I2 = 0% and p = 0.729 for Cochran Q test) was identified between case series reporting rates of sICH among IVT-treated AIS patients with UIAs. In the overall analysis of 5 case series that reported sICH rates both in patients with and without incidental aneurysms, the RR of sICH did not differ between AIS patients with and without UIA (RR = 1.60; 95% CI: 0.54–4.77; p = 0.40) (figure 3) with no evidence of heterogeneity across included studies (I2 = 22% and p = 0.270 for Cochran Q test). After considering the data from the 11 patients who were reported in the studies that were excluded from the meta-analysis5–7,27–33 (131 total patients, harboring 132 total intracranial aneurysms), a total of 11 sICHs were identified (prevalence rate = 8.4%; 95% CI by the adjusted Wald method: 4.6%–14.5%).
Figure 2. Forest plot of symptomatic intracranial hemorrhage rates across case series reporting the safety of IV thrombolysis in acute ischemic stroke patients harboring unruptured intracranial aneurysms.
CI = confidence interval.
Figure 3. Forest plots of the sICH risk ratios between acute ischemic stroke patients with and without UIAs with a continuity correction of 0.5 for studies with a zero cell (no sICH case in patients with UIAs).
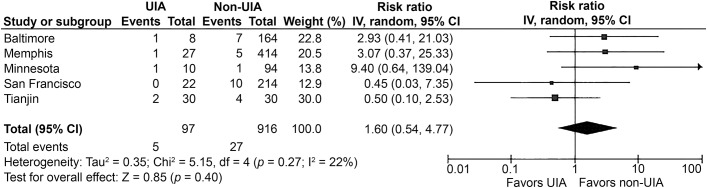
CI = confidence interval; sICH = symptomatic intracranial hemorrhage; UIA = unruptured intracranial aneurysm.
DISCUSSION
Our prospectively collected multicenter data, coupled with the findings of the comprehensive meta-analysis, underscore the safety of IVT in AIS harboring incidental UIA given the low rate of sICH that we documented in our international registry representing the largest to date case series (table 2). Moreover, the findings of our meta-analysis indicate that there is no increase in the risk of sICH between thrombolysis-treated AIS patients with and without incidental intracranial aneurysms. In addition, it should be noted that we detected no publication bias and no heterogeneity across the different case series included in the present meta-analysis. Consequently, our observations indicate that IVT does not adversely affect the natural history of UIA, while the treatment benefit from systemic thrombolysis may not be counterbalanced by the fear of potential aneurysmal rupture causing devastating sICH in AIS patients harboring UIA.
Of note, the one case of sICH that occurred in our series was not caused by aneurysmal rupture. This observation is similar to earlier studies that also failed to detect a causal association between incidental intracranial aneurysms and postthrombolysis sICH.8,9,11 Thus, the perceived fear of aneurysmal rupture following IVT in AIS harboring UIA is limited to evidence provided by case reports.5–7 However, it should be noted that in a case of left middle cerebral artery infarction due to a left carotid dissection with coexisting multiple intracranial aneurysms, which was complicated with a fatal subarachnoid hemorrhage following IVT, autopsy was not performed. Therefore, it is not clear whether the sICH was caused by intracranial extension of the dissection or by potential aneurysmal rupture.7 Finally, IVT has been reported to cause rupture of an anterior communicating aneurysm in a single patient, although important history suggestive of a sentinel bleed (3 days before presenting to the emergency department) was missed before the initiation of IVT, which in turn may have caused rebleeding in an aneurysm with a recent history of microrupture.5
The prevalence of UIAs in the general population is reported to range from 0.2% to 1.8% according to different studies.34 There are accruing data indicating that UIAs may have a higher prevalence in AIS patients in comparison to the general population. More specifically, a Japanese study demonstrated that incidental UIAs were found in 3.7% of stroke patients compared to 2.0% of healthy subjects.4 Another Korean study reported a prevalence of incidental UIAs in 6.6% of AIS.35 In addition, a recent meta-analysis indicates that the overall prevalence of intracranial aneurysms in patients with internal carotid artery stenosis (3.2%) is higher than the reported prevalence of UIAs in the general population.36 Moreover, a systematic review of autopsy and angiography studies suggests that atherosclerotic diseases appear to increase the risk of incidental cerebral aneurysm formation.37 Consequently, it may be postulated that the increased prevalence of UIAs in AIS can be explained by shared risk factors including hypertension, smoking, atherosclerosis, and potentially internal carotid stenosis.
Our multicenter study provides novel information in several aspects. More specifically, previous studies evaluating the safety of IVT in AIS patients with UIA had limited information regarding the potential risk of intracranial bleeding in cases with large (>7 mm) or posterior circulation aneurysms (table 2), which are known to carry a higher risk of rupture.38 Notably, we observed that tPA infusion did not result in any ICH complications in these specific high-risk subgroups that were represented in our cohort (6 cases of large aneurysms and 12 cases of posterior circulation aneurysms).
Certain limitations of the present study need to be acknowledged. Even though the complication rates in this analysis are reassuring, they are still subject to bias or underestimation because of the small numbers of samples and the nonrandomized manner of collection of patients reported in series and used in the meta-analysis. Finally, it should be noted that in our multicenter study, the majority of UIAs were detected with CTA or time-of-flight MRA since this is the standard of care across participating centers, and in specific cases, further diagnostic workup was performed using digital subtraction angiography. Consequently, some small aneurysms (<3 mm) may have been missed and the present study may actually underestimate the prevalence of UIAs among AIS patients treated with IVT. Although we acknowledge the lack of a standardized neuroimaging protocol, we emphasize that our observations reflect real-world experience in everyday clinical practice settings where alternative neuroimaging modalities may be used for diagnosis of UIA. Furthermore, the potential association of sICH with aneurysmal rupture was assessed centrally by 2 stroke neurologists who were not involved in the management of AIS patients in any center.
Our findings provide reassurance that the risk of sICH is not increased in AIS patients harboring UIA and the theoretical danger of aneurysmal rupture may not be substantiated in clinical practice settings. Consequently, the presence of an incidental and asymptomatic intracranial aneurysm in vascular neuroimaging studies of AIS patients who are otherwise eligible candidates for IVT should not preclude the administration of IV tPA on the basis of safety concerns.
Supplementary Material
GLOSSARY
- AIS
acute ischemic stroke
- CI
confidence interval
- CTA
CT angiography
- ICH
intracranial hemorrhage
- IVT
IV thrombolysis
- MRA
magnetic resonance angiography
- NIHSS
NIH Stroke Scale
- RR
risk ratio
- sICH
symptomatic intracranial hemorrhage
- tPA
tissue plasminogen activator
- UIA
unruptured intracranial aneurysm
Footnotes
Supplemental data at Neurology.org
AUTHOR CONTRIBUTIONS
Nitin Goyal: drafting/revising the manuscript, study concept or design, accepts responsibility for conduct of research and will give final approval, acquisition of data, study supervision. Georgios Tsivgoulis: drafting/revising the manuscript, study concept or design, analysis or interpretation of data, accepts responsibility for conduct of research and will give final approval, statistical analysis. Ramin Zand: drafting/revising the manuscript, study concept or design, accepts responsibility for conduct of research and will give final approval, acquisition of data. Vijay K. Sharma: drafting/revising the manuscript, analysis or interpretation of data, accepts responsibility for conduct of research and will give final approval, acquisition of data, study supervision. Kristian Barlinn: drafting/revising the manuscript, analysis or interpretation of data, accepts responsibility for conduct of research and will give final approval, acquisition of data. Shailesh Male: drafting/revising the manuscript, study concept or design, analysis or interpretation of data, accepts responsibility for conduct of research and will give final approval, acquisition of data, study supervision. Aristeidis H. Katsanos: drafting/revising the manuscript, analysis or interpretation of data, accepts responsibility for conduct of research and will give final approval, statistical analysis. Ulf Bodechtel: drafting/revising the manuscript, accepts responsibility for conduct of research and will give final approval, acquisition of data. Sulaiman Iftikhar: drafting/revising the manuscript, study concept or design, accepts responsibility for conduct of research and will give final approval, acquisition of data. Adam Arthur: drafting/revising the manuscript, analysis or interpretation of data, accepts responsibility for conduct of research and will give final approval. Lucas Elijovich: drafting/revising the manuscript, study concept or design, accepts responsibility for conduct of research and will give final approval, study supervision. Anne W. Alexandrov: drafting/revising the manuscript, study concept or design, accepts responsibility for conduct of research and will give final approval, acquisition of data. Andrei V. Alexandrov: drafting/revising the manuscript, study concept or design, analysis or interpretation of data, accepts responsibility for conduct of research and will give final approval, study supervision.
STUDY FUNDING
Dr. Georgios Tsivgoulis has been supported by the European Regional Development Fund, project FNUSA-ICRC (no. CZ.1.05/1.1.00/02.0123).
DISCLOSURE
The authors report no disclosures relevant to the manuscript. Go to Neurology.org for full disclosures.
REFERENCES
- 1.Tissue plasminogen activator for acute ischemic stroke. The National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group. N Engl J Med 1995;333:1581–1587. [DOI] [PubMed] [Google Scholar]
- 2.Emberson J, Lees KR, Lyden P, et al. ; Stroke Thrombolysis Trialists' Collaborative Group. Effect of treatment delay, age, and stroke severity on the effects of intravenous thrombolysis with alteplase for acute ischaemic stroke: a meta-analysis of individual patient data from randomised trials. Lancet 2014;384:1929–1935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Oh YS, Shon YM, Kim BS, Cho AH. Long-term follow-up of incidental intracranial aneurysms in patients with acute ischemic stroke. J Stroke Cerebrovasc Dis 2013;22:329–333. [DOI] [PubMed] [Google Scholar]
- 4.Ishikawa Y, Hirayama T, Nakamura Y, Ikeda K. Incidental cerebral aneurysms in acute stroke patients: comparison of asymptomatic healthy controls. J Neurol Sci 2010;298:42–45. [DOI] [PubMed] [Google Scholar]
- 5.Rammos SK, Neils DM, Fraser K, Klopfenstein JD. Anterior communicating artery aneurysm rupture after intravenous thrombolysis for acute middle cerebral artery thromboembolism: case report. Neurosurgery 2012;70:e1603–e1607. [DOI] [PubMed] [Google Scholar]
- 6.Zaldivar-Jolissaint JF, Messerer M, Bervini D, Mosimann PJ, Levivier M, Daniel RT. Rupture of a concealed aneurysm after intravenous thrombolysis of a thrombus in the parent middle cerebral artery. J Stroke Cerebrovasc Dis 2015;24:e63–e65. [DOI] [PubMed] [Google Scholar]
- 7.Haji F, van Adel B, Avery M, Megyesi J, Young GB. Intracranial aneurysm rupture following intravenous thrombolysis for stroke. Can J Neurol Sci 2014;41:95–98. [DOI] [PubMed] [Google Scholar]
- 8.Mittal MK, Seet RC, Zhang Y, Brown RD, Jr, Rabinstein AA. Safety of intravenous thrombolysis in acute ischemic stroke patients with saccular intracranial aneurysms. J Stroke Cerebrovasc Dis 2013;22:639–643. [DOI] [PubMed] [Google Scholar]
- 9.Kim JT, Park MS, Yoon W, Cho KH. Detection and significance of incidental unruptured cerebral aneurysms in patients undergoing intravenous thrombolysis for acute ischemic stroke. J Neuroimaging 2012;22:197–200. [DOI] [PubMed] [Google Scholar]
- 10.Zhang CH, Li C, Wang YX, et al. Efficacy and safety of intravenous thrombolysis for the treatment of acute ischemic stroke patients with saccular intracranial aneurysms of ≤3 mm. Cell Biochem Biophys Epub 2015 Feb 26. [DOI] [PubMed]
- 11.Sheth KN, Shah N, Morovati T, Hermann LD, Cronin CA. Intravenous rt-PA is not associated with increased risk of hemorrhage in patients with intracranial aneurysms. Neurocrit Care 2012;17:199–203. [DOI] [PubMed] [Google Scholar]
- 12.Edwards NJ, Kamel H, Josephson SA. The safety of intravenous thrombolysis for ischemic stroke in patients with pre-existing cerebral aneurysms: a case series and review of the literature. Stroke 2012;43:412–416. [DOI] [PubMed] [Google Scholar]
- 13.Jauch EC, Saver JL, Adams HP, Jr, et al. ; American Heart Association Stroke Council; Council on Cardiovascular Nursing; Council on Peripheral Vascular Disease; Council on Clinical Cardiology. Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2013;44:870–947. [DOI] [PubMed] [Google Scholar]
- 14.Tsivgoulis G, Alexandrov AV, Chang J, et al. Safety and outcomes of intravenous thrombolysis in stroke mimics: a 6-year, single-care center study and a pooled analysis of reported series. Stroke 2011;42:1771–1774. [DOI] [PubMed] [Google Scholar]
- 15.Tsivgoulis G, Frey JL, Flaster M, et al. Pre-tissue plasminogen activator blood pressure levels and risk of symptomatic intracerebral hemorrhage. Stroke 2009;40:3631–3634. [DOI] [PubMed] [Google Scholar]
- 16.Tsivgoulis G, Sharma VK, Mikulik R, et al. Intravenous thrombolysis for acute ischemic stroke occurring during hospitalization for transient ischemic attack. Int J Stroke 2014;9:413–418. [DOI] [PubMed] [Google Scholar]
- 17.Tsivgoulis G, Ribo M, Rubiera M, et al. Real-time validation of transcranial Doppler criteria in assessing recanalization during intra-arterial procedures for acute ischemic stroke: an international, multicenter study. Stroke 2013;44:394–400. [DOI] [PubMed] [Google Scholar]
- 18.Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol 2009;62:e1–e34. [DOI] [PubMed] [Google Scholar]
- 19.Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis of Observational Studies in Epidemiology (MOOSE) Group. JAMA 2000;283:2008–2012. [DOI] [PubMed] [Google Scholar]
- 20.Khan NR, Tsivgoulis G, Lee SL, et al. Fibrinolysis for intraventricular hemorrhage: an updated meta-analysis and systematic review of the literature. Stroke 2014;45:2662–2669. [DOI] [PubMed] [Google Scholar]
- 21.Katsanos AH, Spence JD, Bogiatzi C, et al. Recurrent stroke and patent foramen ovale: a systematic review and meta-analysis. Stroke 2014;45:3352–3359. [DOI] [PubMed] [Google Scholar]
- 22.Lewis JR, Sauro J. When 100% really isn't 100%: improving the accuracy of small-sample estimates of completion rates. J Usability Stud 2006;1:136–150. [Google Scholar]
- 23.Sweeting MJ, Sutton AJ, Lambert PC. What to add to nothing? Use and avoidance of continuity corrections in meta-analysis of sparse data. Stat Med 2004;23:1351–1375. [DOI] [PubMed] [Google Scholar]
- 24.Deeks JJ, Higgins JPT, Altman DG, editors. Chapter 9: analysing data and undertaking meta-analyses. In: Cochrane Handbook for Systematic Reviews of Interventions [online]. Available at: http://handbook.cochrane.org/chapter_9/9_analysing_data_and_undertaking_meta_analyses.htm. Accessed February 4, 2015. [Google Scholar]
- 25.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997;315:629–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tsivgoulis G, Katsanos AH, Butcher KS, et al. Intensive blood pressure reduction in acute intracerebral hemorrhage: a meta-analysis. Neurology 2014;83:1523–1529. [DOI] [PubMed] [Google Scholar]
- 27.Briosa EG, Almeida A, Monteiro N, et al. Successful thrombolysis despite having an incidental unruptured cerebral aneurysm. Case Rep Neurol Med 2014;2014:323049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.D'Olhaberriague L, Joshi N, Chaturvedi S, et al. Tissue plasminogen activator for acute ischemic stroke in patients with unruptured cerebral aneurysms. J Stroke Cerebrovasc Dis 2000;9:181–184. [DOI] [PubMed] [Google Scholar]
- 29.Desai JA, Jin AY, Melanson M. IV thrombolysis in stroke from a cavernous carotid aneurysm to artery embolus. Can J Neurol Sci 2011;38:352–353. [DOI] [PubMed] [Google Scholar]
- 30.Matsuzaki T, Yoshino A, Sakatani K, Katayama Y. Recanalization of middle cerebral artery and intracranial aneurysm in the same ischemic territory with intravenous administration of recombinant tissue plasminogen activator: case report. J Stroke Cerebrovasc Dis 2011;20:269–272. [DOI] [PubMed] [Google Scholar]
- 31.Yoneda Y, Yamamoto S, Hara Y, Yamashita H. Unruptured cerebral aneurysm detected after intravenous tissue plasminogen activator for stroke. Case Rep Neurol 2009;1:20–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ganesalingam J, Redwood R, Jenkins I. Thrombolysis of an acute stroke presentation with an incidental unruptured aneurysm. JRSM Cardiovasc Dis 2013;2:2048004013478808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Xu M, Yan SQ, Cao J, Lou M. No hemorrhagic transformation after intravenous thrombolysis in a pontine infarction patient with basilar aneurysm. CNS Neurosci Ther 2014;20:473–475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Vernooij MW, Ikram MA, Tanghe HL, et al. Incidental findings on brain MRI in the general population. N Engl J Med 2007;357:1821. [DOI] [PubMed] [Google Scholar]
- 35.Oh YS, Lee SJ, Shon YM, Yang DW, Kim BS, Cho AH. Incidental unruptured intracranial aneurysms in patients with acute ischemic stroke. Cerebrovasc Dis 2008;26:650–653. [DOI] [PubMed] [Google Scholar]
- 36.Héman LM, Jongen LM, van der Worp HB, Rinkel GJ, Hendrikse J. Incidental intracranial aneurysms in patients with internal carotid artery stenosis: a CT angiography study and a metaanalysis. Stroke 2009;40:1341–1346. [DOI] [PubMed] [Google Scholar]
- 37.Griffiths PD, Worthy S, Gholkar A. Incidental intracranial vascular pathology in patients investigated for carotid stenosis. Neuroradiology 1996;38:25–30. [DOI] [PubMed] [Google Scholar]
- 38.Juvela S, Porras M, Poussa K. Natural history of unruptured intracranial aneurysms: probability of and risk factors for aneurysm rupture. J Neurosurg 2008;108:1052–1060. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.