Abstract
CAP2 has been suggested as a potential diagnostic biomarker for early hepatocellular carcinoma (HCC). However, its prognostic significance in HCC remains unclear. Here, we show that CAP2 expression is much higher in HCC tissues than that in paracarcinoma tissues, at both mRNA and protein levels. Data of immunohistochemistry (IHC) revealed that CAP2 was markedly up-regulated in 77.3% of HCC cases. High CAP2 expression, defined by the median score of IHC, was present in 53.3% of the patients. Kaplan-Meier analysis indicated that high CAP2 expression was associated with poor overall survival (P < .0001), disease-free survival (P = .013) and recurrence probability (P = .004) in a training cohort of 312 HCC patients. The prognostic implication of CAP2 in HCC was further confirmed in a validation cohort of 208 HCC patients and by stratified survival analysis. Multiple Cox regression analysis indicated CAP2 as an independent predictor for overall survival (hazard ratio (HR) = 1.615, 95% confidence interval: 1.345-1.938, P < .001). Collectively, we conclude that CAP2 is increased in HCC and is a novel unfavorable biomarker for prognostic prediction for patients with this deadly disease.
Introduction
The 5-year survival for patients with hepatocellular carcinoma (HCC) has been poorly improved worldwide last decades [1], despite the advances in surgical management and the clinical implementation of numerous therapeutic strategies. The mortality rate of HCC ranks the second most common cause of cancer-related death in men and the sixth in women [2]. The incidence of HCC has been increasing in economically developed regions, including Japan, Western Europe and the USA [3], [4]. In view of the poor outcome of patients with HCC, interests in developing novel strategies for HCC therapy have been accumulating. Discovery of biological markers useful for HCC prognostic prediction is one of the potential strategies to monitor the progress of this deadly disease in clinical management.
Cyclase-associated protein (CAP), consisting of 474 to 551 amino acid residues, is an evolutionary highly conserved protein between yeast and mammals. It was firstly identified in the budding yeast Saccharomyces cerevisiae [5]. CAP exerts functions towards the activations of adenylyl cyclase and the mediating the dynamics of actin polymerization by binding to G-actin [5], [6]. Two homologs, CAP1 and CAP2, are present in higher eukaryotes. CAP1 and CAP2 share about 76% similarity in rat [7]. CAP2 is rarely present in a few of tissues. It could co-localize with actin in skeletal muscle cells [8]. In rat, CAP2 transcripts were found in testes, lung and kidney, but not in liver and spleen [9]. During the development of mice embryos, CAP2 was detectable throughout cardiogenesis [10]. Loss of CAP2 led to cardiomyopathy, according to the data that CAP2 depletion caused dilated cardiomyopathy and various cardiac detects [11]. In human cancers, CAP2 was differently expressed. For example, CAP2 was highly up-regulated in thyroid, kidney and bladder cancers. On the contrary, CAP2 mRNA was found down-regulated in breast fibroadenoma [12]. In HCC, CAP2 was demonstrated to be overexpressed in several studies [8], [13], [14]. However, the relevant prognostic implication of CAP2 has not been understood and remains elusive.
In this study, the expression of CAP2 in HCC was examined. The relationship between CAP2 expression and clinicopathological features was investigated. The role of CAP2 in HCC prognosis was assessed. Our results reveal that CAP2 is noticeably up-regulated in HCC and significantly correlated with unfavorable prognosis.
Materials and Methods
Patients and Tissue Samples
HCC samples, along with the clinicopathological information, were obtained from 520 HCC patients underwent surgical resection at Sun Yat-sen University Cancer Center, Guangzhou, China, between January 2000 and December 2010. This cohort consists of 470 (90.4%) male and 50 (9.6%) female. The mean age is 49, ranging from 13.0 to 71.0. The mean follow-up time is 40.5 months. Another 32 paired fresh resection HCC tissues and the corresponding adjacent liver tissues were collected for quantitative real-time PCR and Western blot analysis. None of the patients had received adjuvant therapies before surgery. The use of tissues for this study has been approved by the Institute Research Medical Ethics Committee of Sun Yat-sen University Cancer Center.
Immunohistochemistry (IHC)
Tissue microarray containing 520 HCC samples was constructed as described in our previous study [15]. Formalin-fixed and paraffin-embedded HCC sections were dewaxed in xylene and graded alcohols, hydrated, and washed in PBS. After pretreatment in a microwave oven, endogenous peroxidase was inhibited by 3% hydrogen peroxide in methanol for 20 minutes, followed by avidin-biotin blocking using a biotin-blocking kit (DAKO, Germany). Slides were then incubated with CAP1 (Abcam, Cambridge, MA) and CAP2 antibody (Santa Cruz Biotechnology, Santa Cruz, CA) overnight at 4°C, washed in PBS, and incubated with biotinylated goat anti-rabbit/mouse antibodies (DAKO, Germany). Slides were developed with DAB and counterstained with hematoxylin.
IHC Evaluation
Semi-quantitative IHC detection was used to determine the CAP2 protein levels. For each case, 1000 cells were randomly selected and scored independently by two pathologists (Dr. JP Yun and Dr. M Li). The percentage of positively stained cells was scored as “0” (0%), “1” (1% to 25%), “2” (26% to 50%), “3” (51% to 75%), “4” (76% to 100%). Intensity was scored as “0” (negative staining), “1” (weak staining), “2” (moderate staining), and “3” (strong staining). The percentage score was multiplied by the staining intensity score. The median score of IHC staining was chosen as the cut-off value.
Quantitative Real-Time PCR (qRT-PCR) and Western Blot
qRT-PCR and western blot were performed as described in our previous study [15]. Primers were designed as follows: CAP1, forward: 5′- GCAGATTAATCAGGGGGAGAG-3′ and reverse: 5′- TTCCTGATTTTCCACTCTCCAC-3′; CAP2, forward: 5′-AGTACCAACAACCCCACGAG-3′ and reverse: 5′- TTCCACAATGCCCACCAC AT-3′; β-actin, forward: 5′-TGGCACCCAGCACAATGAA-3′ and reverse: 5′-CTAAGTCATAGTCCG CCTAGAAGCA-3′.
Statistical Analysis
Statistical analyses were performed using the SPSS 16.0 software (SPSS, Chicago, IL). Wilcoxon matched pairs test was used to determine the significant difference of CAP2 expression. χ2 test was performed to analyze the correlation between CAP2 expression and clinicopathological parameters. Kaplan-Meier analysed (log-rank test) was conducted for survival analysis and univariate analysis. Independent analyses were performed according to the selected population: overall population and different morphological and pathological subgroups. Cox proportional hazards regression model was used to identify the independent prognostic factors. Statistical significance was set at P < .05.
Results
Expression of CAP2 in HCC Tissue Samples by qRT-PCR and Western Blot
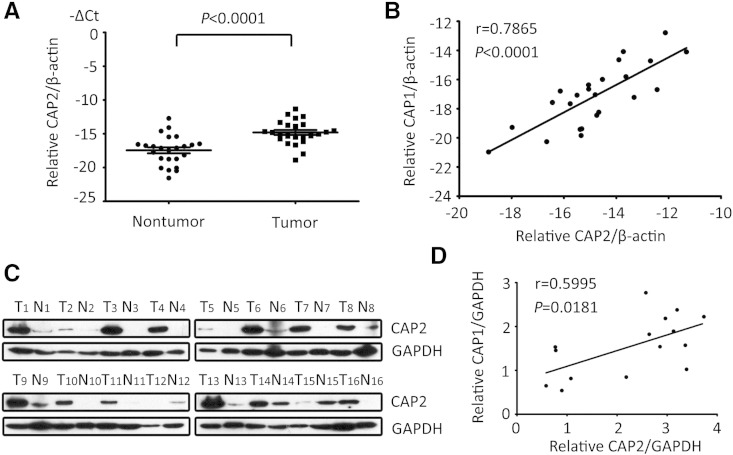
To determine the expression of CAP2 in HCC, 24 pairs of tumor samples and the corresponding adjacent nontumorous samples were collected. Results of qRT-PCR showed that CAP2 mRNA levels in HCC were markedly increased in 87.5% (21/24) of the cases, compared with the paracarcinoma tissues (Figure 1A). The mRNA expression of CAP2 was found to be positively connected with CAP1 mRNA expression (Figure 1B). Consistently, the protein levels of CAP2 in 87.5% (14/16) of HCC cases were noticeably up-regulated in HCC samples (Figure 1C). The significant correlation of CAP2 and CAP1 protein expression was also depicted (Figure 1D).
Figure 1.
CAP2 expression is increased in HCC samples by qRT-PCR and Western blot. (A) mRNA levels of CAP2 were determined by qRT-PCR in 24 paired fresh HCC tissues. (B) Wilcoxon matched paired test showed the relationship of CAP2 and CAP1 expression at mRNA level. (C) Protein levels of CAP2 in tumorous samples (T) and corresponding adjacent nontumorous samples (N) were examined in 16 pairs of HCC fresh tissues by western blot. (D) Correlation of protein expression normalized to GAPDH of CAP2 and CAP1 were calculated.
Expression of CAP2 in HCC Tissue Samples by IHC
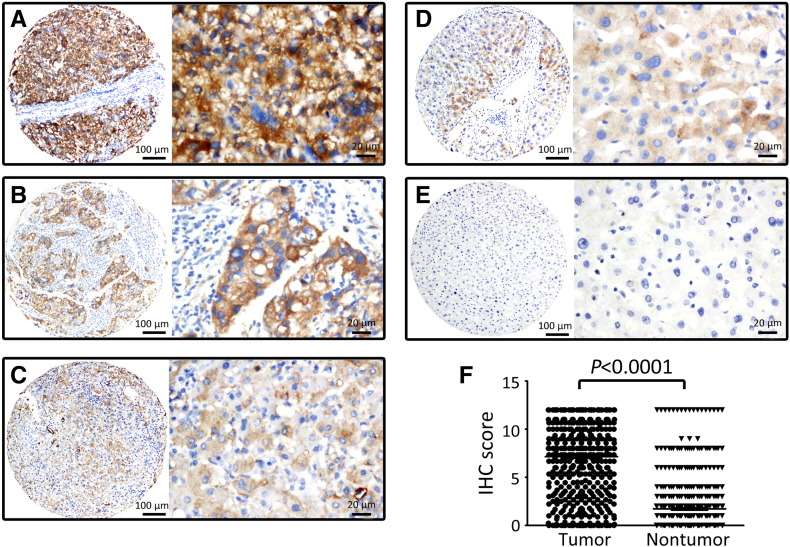
To further confirm the overexpression of CAP2 in HCC, 520 paraffin-embedded HCC samples were collected to construct tissue microarray. As shown by the results of IHC, positive staining of CAP2 was presented in 94.8% (493/520) of tumorous tissues, but only in 42.3% (220/520) of the nontumorous tissues. Furthermore, 77.3% (402/520) of patients with HCC expressed more CAP2 protein in tumorous tissue. CAP2 was mainly located in the cytoplasm of tumor cells (Figure 2,A–C). The representative images of CAP2 expression in nontumorous tissues were also recorded (Figure 2,D–E). According to the IHC score, CAP2 expression in HCC was remarkably higher than that in nontumorous tissues (Figure 2F).
Figure 2.
CAP2 expression is increased in HCC samples by IHC. Representative images of strong (A), moderate (B) and weak (C) immunoreactivities of CAP2 in HCC, as well as positive (D) and negative (E) staining of CAP2 in normal liver tissues were shown (Left panel: magnification × 100; Right panel: magnification × 400). F. Wilcoxon matched paired test revealed a significant increase of IHC score in HCC.
Association of CAP2 Expression and Clinical Outcome in HCC
To disclose the clinical value of CAP2 in HCC, the relationship between CAP2 expression and the clinical variables of HCC patients was analyzed. Based on the median score (7.33) of IHC staining of CAP2, patients were divided into two groups defined as low CAP2 expression and high CAP2 expression. High CAP2 expression was present in 53.3% of the patients. No significant associations were depicted in CAP2 expression with the clinicopathological parameters (Supplementary Table 1).
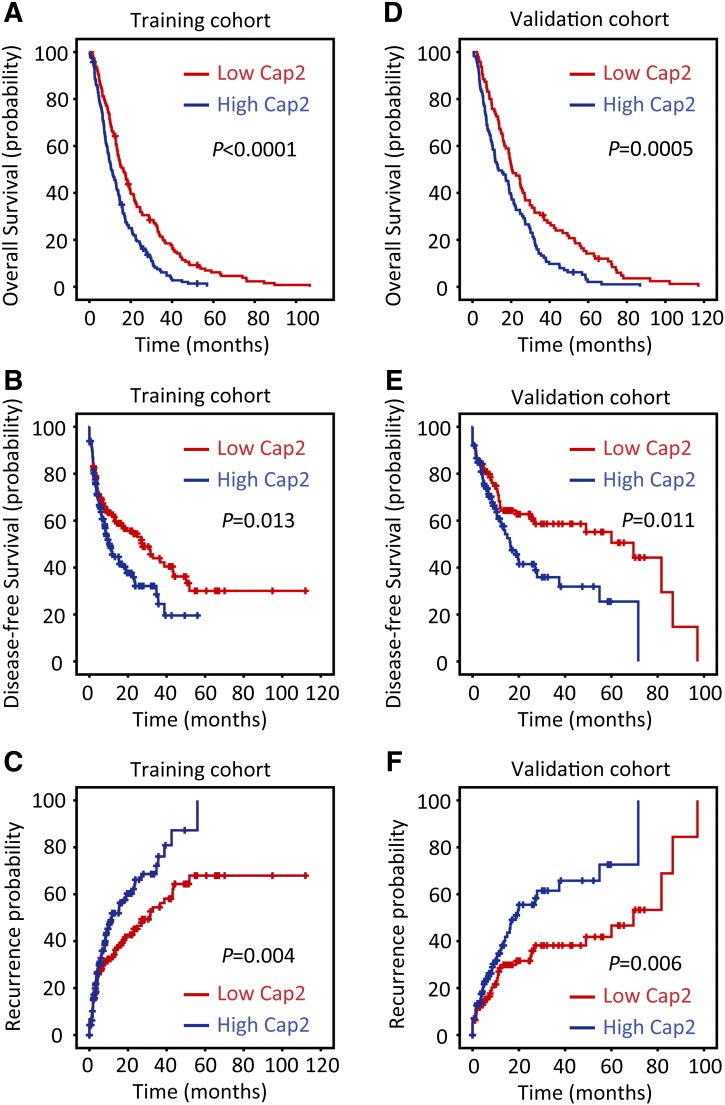
The prognostic implication of CAP2 in HCC was next determined. Randomly, 520 patients with HCC were separated into two cohorts, named training and validation cohorts. Kaplan-Meier analysis indicated that, in the training cohort, HCC cases with high CAP2 expression were usually accompanied with significantly worse prognosis, in terms of overall survival (P < .001), disease-free survival (P = .013) and recurrence-free survival (P = .004) (log-rank test; Figure 3,A–C). Consistently, low CAP2 expression was positively correlated with favorable overall survival (P < .001), disease-free survival (P = .011) and recurrence-free survival (P = .006) in validation cohort (log-rank test; Figure 3,D–F).
Figure 3.
High CAP2 expression is correlated with unfavorable prognosis in training and validation cohorts. Kaplan-Meier analysis disclosed the significant differences in overall survival (A,D), disease-free survival (B,E) and recurrence probability (C,F) between postoperative patients with high and low CAP2 expression in HCC training (n = 312) and validation (n = 208) cohorts (log-rank test).
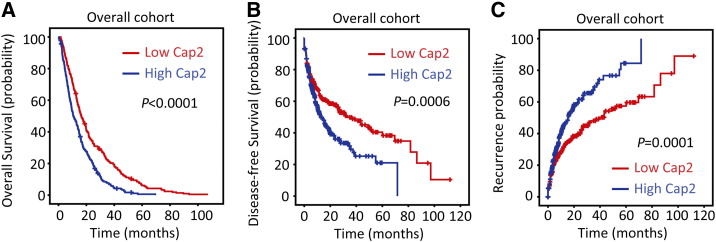
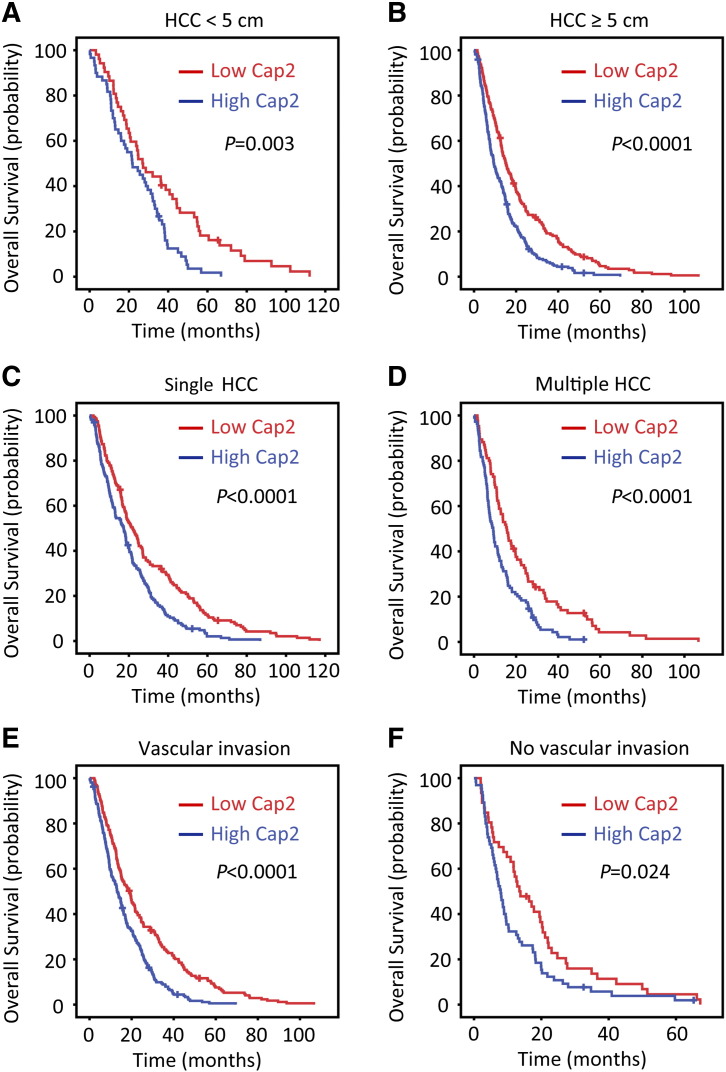
In line with the results of the individual cohort, patients with high CAP2 were likely to have shorter overall survival (P < .001), disease-free survival (P < .001) and recurrence-free survival (P < .001) in the overall cohort (log-rank test; Figure 4). The prognostic significance of CAP2 was further confirmed by stratified survival analyses, showing that CAP2 expression was connected with overall survival in small and large HCC (Figure 5,A–B), in unique and multinodular HCC (Figure 5,C–D), regardless of the presence or absence of microvascular invasion (Figure 5,E–F).
Figure 4.
High CAP2 expression is correlated with unfavorable prognosis in overall cohort. Kaplan-Meier analysis disclosed the significant differences in overall survival (A), disease-free survival (B) and recurrence probability (C) between postoperative patients with high and low CAP2 expression in overall (n = 520) cohort (log-rank test).
Figure 5.
CAP2 expression is associated with overall survival in subgroups of HCC patients. Stratified survival analyses showed that CAP2 expression was connected with overall survival in small and large HCC (A,B), in unique and multinodular HCC (C,D), regardless of the presence or absence of microvascular invasion (E,F) (log-rank test).
Univariate and Multivariate Analyses of Prognostic Variables in HCC
To evaluate the representative of our samples, univariate analyses were performed. In training cohort, CAP2, as well as tumor size, invonucrum, LNM, tumor differentiation and TNM, was responsible for the survival of HCC patients. After adjusted for the prognostic factors established in univariate analysis, a significant correlation of high CAP2 expression with worse overall survival (hazard ratio (HR) = 1.615, 95% confidence interval (95% CI): 1.271-2.051, P < .001) was indicated by multiple Cox regression analysis (Supplementary Table 2). This was further confirmed in validation cohort (HR = 1.889, 95% CI: 1.403-2.544, P < .001) (Supplementary Table 3).
In the overall cohort of 520 patients with HCC, CAP2, along with tumor size, tumor multiplicity, invonucrum, liver cirrhosis, serum level of AFP, LNM, tumor differentiation, and TNM, was identified as prognostic factor (Table 1). Multivariate analysis indicated CAP2 as an independent factor for overall survival (HR = 1.615, 95% CI: 1.345-1.938, P < .001) but not disease-free survival (Table 1 and data not shown).
Table 1.
Univariate and Multivariate Analysis of Clinicopathological and Cap2 for Overall Survival in Overall Cohort (n = 520)
| Variables | Univariate Analysis |
Multivariate Analysis |
||
|---|---|---|---|---|
| HR (95% CI) | P value | HR (95% CI) | P value | |
| Age (< 49 vs ≥ 49 years) | 0.868(0.728-1.035) | .114 | ||
| Gender (female vs male) | 1.021(0.758-1.376) | .891 | ||
| HBV (positive vs negative) | 1.092(0.857-1.391) | .478 | ||
| Tumor size (< 5 vs ≥ 5 cm) | 1.420(1.148-1.757) | .001 | ||
| Tumor multiplicity (single vs multiple) | 1.199(1.000-1.436) | .049 | 0.800(0.640-1.000) | .049 |
| Invonucrum (absent vs present) | 1.199(1.000-1.436) | .000 | 0.800(0.666-0.960) | .017 |
| Liver cirrhosis (yes vs no) | 0.744(0.588-0.941) | .013 | 0.866(0.679-1.104) | .244 |
| AFP (< 20 vs ≥ 20 ng/mL) | 1.407(1.145-1.728) | .001 | 1.174(0.948-1.455) | .142 |
| LNM (Yes vs no) | 1.568(1.100-2.235) | .013 | 1.338(0.931-1.921) | .115 |
| Tumor differentiation | 1.879(1.394-2.531) | .000 | 1.446(1.059-1.974) | .020 |
| TNM (I vs II-IV) | 1.740(1.444-2.095) | .000 | 1.765(1.398-2.229) | .000 |
| Cap2 expression (low vs high) | 1.693(1.412-2.030) | .000 | 1.615(1.345-1.938) | .000 |
HR, hazard ratio; CI, confident interval; LNM, lymph node metastasis.
Discussion
In the recent years, searching for valuable biomarkers for HCC diagnosis and prognostic prediction has been attracting more and more interests. Numerous of factors, such as serum DKK1 [16] and microRNA panel [17], have been proposed as potential diagnostic biomarkers. On the other hand, abnormal expression of certain proteins, e.g., cyclin F [15] and CXCL5, [18], was considered to be of prognostic significance. In this study, we intended to determine the prognostic value of CAP2 in a large cohort of primary HCC patients who underwent curative surgery.
Current data suggest CAP2 is of diagnostic implication in early HCC, which is defined as a vaguely nodular well-differentiated tumor. Sakamoto et al. showed that CAP2 was expressed in 70% to 100% of early HCC to some extent, but only in 5% to 10% precancerous lesions [19]. Our data present a marked increase of CAP2 expression in HCC, compared with the nontumorous tissues. Consistent with our study, Shibata and colleagues offered evidence that CAP2 expression was increased in HCC, and that strong staining of CAP2 was more frequently presented in progressed HCC, compared to early HCC [13]. Similarly, Sakamoto et al. reported that CAP2 expression was generally increased from early to advanced stage of HCC [20]. However, in our study, the positive staining of CAP2 was also depicted in 42.3% of nontumorous tissues, which is much lower than that in HCC tissues. This may not meet the request of specificity for clinical diagnosis. On the other hand, it is worth the notice that CAP2 was somatically mutated in an early-stage primary myelofibrosis patient [21]. Whether the altered expression of CAP2 in human cancer is due to its mutation is unknown and requires further investigation. Undoubtedly, extensive studies should be done to confirm whether CAP2 could be used as a practical biomarker for the diagnosis of early HCC.
The prognostic value of CAP protein has been revealed in human cancers. Yu et al. showed that CAP1 was overexpressed in breast cancer and its knockdown inhibited cell proliferation and migration [22]. A later study showed that CAP1 overexpression in breast cancer was associated with unfavorable prognosis [23]. Xie et al. showed that CAP1 was up-regulated and predicted brain metastasis and poor survival in non-small cell lung cancer [24]. Hua et al. reported that CAP1 expression was induced, associated with Ki67 expression and poor outcome in epithelial ovarian cancer [25]. In HCC, high expression of CAP1 was correlated with unfavorable prognosis and promoted tumor metastasis [26]. However, to date, the prognostic implication of CAP2 in human cancer has not been understood. Our data showed that CAP2 expression in a large cohort of 520 patients with HCC was significantly associated with overall and disease-free survival. Further statistical analyses indicated CAP2 as an independent factor for prognostic prediction. Collectively, these data offer some suggestions to HCC clinical management that which patients should be under close surveillance for the tumor progression. Effendi et al. reported that CAP2 expression in 105 HCC cases was connected with tumor size, poor differentiation, portal vein invasion, and intrahepatic metastasis [8]. Oppositely, our data showed that CAP2 expression was not significantly correlated to the above malignant parameter. The difference between the two studies might be due to the cut-off value of IHC evaluation. In Effendi's study, definition of high or low CAP2 expression was decided by the positive control which was not provided, whereas in our study, IHC score was based on the CAP2 immunoreactivity in tumor cells. On the other hand, the sample size in our study (520 cases) was much bigger than that in Effendi's study (105 cases). We therefore considered our data was representative. Although our study could not provide information for the biological function of CAP2 in HCC development, literature showing that CAP2 is continually expressed throughout the development of cardiogenesis of mice embryos [10], and that CAP2 depletion resulted in delayed scratch closure probably due to the function of CAP2 on actin cytoskeleton [12], indicates that CAP2 might exert activities during cell differentiation and migration. The role of CAP2 in HCC, however, calls for further studies.
In summary, our data demonstrated that CAP2 expression was noticeably increased in HCC tissues, compared with the nontumorous tissues. High CAP2 expression was significantly correlated with poor overall and disease-free survival. The prognostic implication was also valid in several subgroups of HCC patients. Our study therefore suggests CAP2 as a promising biomarker for prognosis of patients with HCC.
Footnotes
Conflict of Interest: None.
Funding resource: The study was supported by grants from the National Natural Science Foundation of China (No. 81201717, 81372572).
Supplementary data to this article can be found online at http://dx.doi.org/10.1016/j.tranon.2015.08.003.
Appendix A. Supplementary data
Correlation of Clinicopathological Parameters and Cap2 Expression in Overall Cohort
Supplementary Table 2. Univariate and Multivariate Analysis of Clinicopathological and Cap2 for Overall Survival in the Training Cohort (n = 312)
Supplementary Table 3. Univariate and Multivariate Analysis of Clinicopathological and Cap2 for Overall Survival in the Validation Cohort (n = 208)
References
- 1.Allemani C, Weir HK, Carreira H, Harewood R, Spika D, Wang XS, Bannon F, Ahn JV, Johnson CJ, Bonaventure A. Global surveillance of cancer survival 1995–2009: analysis of individual data for 25,676,887 patients from 279 population-based registries in 67 countries (CONCORD-2) Lancet. 2015;385(9972):977–1010. doi: 10.1016/S0140-6736(14)62038-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A. Global cancer statistics, 2012. CA Cancer J Clin. 2015;65(2):87–108. doi: 10.3322/caac.21262. [DOI] [PubMed] [Google Scholar]
- 3.Li XP, Cao GW, Sun Q, Yang C, Yan B, Zhang MY, Fu YF, Yang LM. Cancer incidence and patient survival rates among the residents in the Pudong New Area of Shanghai between 2002 and 2006. Chin J Cancer. 2013;32(9):512–519. doi: 10.5732/cjc.012.10200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Altekruse SF, Henley SJ, Cucinelli JE, McGlynn KA. Changing hepatocellular carcinoma incidence and liver cancer mortality rates in the United States. Am J Gastroenterol. 2014;109(4):542–553. doi: 10.1038/ajg.2014.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Field J, Vojtek A, Ballester R, Bolger G, Colicelli J, Ferguson K, Gerst J, Kataoka T, Michaeli T, Powers S. Cloning and characterization of CAP, the S. cerevisiae gene encoding the 70 kd adenylyl cyclase-associated protein. Cell. 1990;61(2):319–327. doi: 10.1016/0092-8674(90)90812-s. [DOI] [PubMed] [Google Scholar]
- 6.Gerst JE, Ferguson K, Vojtek A, Wigler M, Field J. CAP is a bifunctional component of the Saccharomyces cerevisiae adenylyl cyclase complex. Mol Cell Biol. 1991;11(3):1248–1257. doi: 10.1128/mcb.11.3.1248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zelicof A, Gatica J, Gerst JE. Molecular cloning and characterization of a rat homolog of CAP, the adenylyl cyclase-associated protein from Saccharomyces cerevisiae. J Biol Chem. 1993;268(18):13448–13453. [PubMed] [Google Scholar]
- 8.Effendi K, Yamazaki K, Mori T, Masugi Y, Makino S, Sakamoto M. Involvement of hepatocellular carcinoma biomarker, cyclase-associated protein 2 in zebrafish body development and cancer progression. Exp Cell Res. 2013;319(1):35–44. doi: 10.1016/j.yexcr.2012.09.013. [DOI] [PubMed] [Google Scholar]
- 9.Swiston J, Hubberstey A, Yu G, Young D. Differential expression of CAP and CAP2 in adult rat tissues. Gene. 1995;165(2):273–277. doi: 10.1016/0378-1119(95)00522-8. [DOI] [PubMed] [Google Scholar]
- 10.Christoforou N, Miller RA, Hill CM, Jie CC, McCallion AS, Gearhart JD. Mouse ES cell-derived cardiac precursor cells are multipotent and facilitate identification of novel cardiac genes. J Clin Invest. 2008;118(3):894–903. doi: 10.1172/JCI33942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Peche VS, Holak TA, Burgute BD, Kosmas K, Kale SP, Wunderlich FT, Elhamine F, Stehle R, Pfitzer G, Nohroudi K. Ablation of cyclase-associated protein 2 (CAP2) leads to cardiomyopathy. Cell Mol Life Sci. 2013;70(3):527–543. doi: 10.1007/s00018-012-1142-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Peche V, Shekar S, Leichter M, Korte H, Schroder R, Schleicher M, Holak TA, Clemen CS, Ramanath YB, Pfitzer G. CAP2, cyclase-associated protein 2, is a dual compartment protein. Cell Mol Life Sci. 2007;64(19–20):2702–2715. doi: 10.1007/s00018-007-7316-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shibata R, Mori T, Du W, Chuma M, Gotoh M, Shimazu M, Ueda M, Hirohashi S, Sakamoto M. Overexpression of cyclase-associated protein 2 in multistage hepatocarcinogenesis. Clin Cancer Res. 2006;12(18):5363–5368. doi: 10.1158/1078-0432.CCR-05-2245. [DOI] [PubMed] [Google Scholar]
- 14.Sakamoto M, Effendi K, Masugi Y. Molecular diagnosis of multistage hepatocarcinogenesis. Jpn J Clin Oncol. 2010;40(9):891–896. doi: 10.1093/jjco/hyq099. [DOI] [PubMed] [Google Scholar]
- 15.Fu J, Qiu H, Cai M, Pan Y, Cao Y, Liu L, Yun J, Zhang CZ. Low cyclin F expression in hepatocellular carcinoma associates with poor differentiation and unfavorable prognosis. Cancer Sci. 2013;104(4):508–515. doi: 10.1111/cas.12100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shen Q, Fan J, Yang XR, Tan Y, Zhao W, Xu Y, Wang N, Niu Y, Wu Z, Zhou J. Serum DKK1 as a protein biomarker for the diagnosis of hepatocellular carcinoma: a large-scale, multicentre study. Lancet Oncol. 2012;13(8):817–826. doi: 10.1016/S1470-2045(12)70233-4. [DOI] [PubMed] [Google Scholar]
- 17.Zhou J, Yu L, Gao X, Hu J, Wang J, Dai Z, Wang JF, Zhang Z, Lu S, Huang X. Plasma microRNA panel to diagnose hepatitis B virus-related hepatocellular carcinoma. J Clin Oncol. 2011;29(36):4781–4788. doi: 10.1200/JCO.2011.38.2697. [DOI] [PubMed] [Google Scholar]
- 18.Zhou SL, Dai Z, Zhou ZJ, Wang XY, Yang GH, Wang Z, Huang XW, Fan J, Zhou J. Overexpression of CXCL5 mediates neutrophil infiltration and indicates poor prognosis for hepatocellular carcinoma. Hepatology. 2012;56(6):2242–2254. doi: 10.1002/hep.25907. [DOI] [PubMed] [Google Scholar]
- 19.Sakamoto M. Early HCC: diagnosis and molecular markers. J Gastroenterol. 2009;44(Suppl. 19):108–111. doi: 10.1007/s00535-008-2245-y. [DOI] [PubMed] [Google Scholar]
- 20.Sakamoto M, Mori T, Masugi Y, Effendi K, Rie I, Du W. Candidate molecular markers for histological diagnosis of early hepatocellular carcinoma. Intervirology. 2008;51(Suppl. 1):42–45. doi: 10.1159/000122603. [DOI] [PubMed] [Google Scholar]
- 21.Merker JD, Roskin KM, Ng D, Pan C, Fisk DG, King JJ, Hoh R, Stadler M, Okumoto LM, Abidi P. Comprehensive whole-genome sequencing of an early-stage primary myelofibrosis patient defines low mutational burden and non-recurrent candidate genes. Haematologica. 2013;98(11):1689–1696. doi: 10.3324/haematol.2013.092379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yu XF, Ni QC, Chen JP, Xu JF, Jiang Y, Yang SY, Ma J, Gu XL, Wang H, Wang YY. Knocking down the expression of adenylate cyclase-associated protein 1 inhibits the proliferation and migration of breast cancer cells. Exp Mol Pathol. 2014;96(2):188–194. doi: 10.1016/j.yexmp.2014.02.002. [DOI] [PubMed] [Google Scholar]
- 23.Liu X, Yao N, Qian J, Huang H. High expression and prognostic role of CAP1 and CtBP2 in breast carcinoma: associated with E-cadherin and cell proliferation. Med Oncol. 2014;31(3):878. doi: 10.1007/s12032-014-0878-7. [DOI] [PubMed] [Google Scholar]
- 24.Xie SS, Tan M, Lin HY, Xu L, Shen CX, Yuan Q, Song XL, Wang CH. Overexpression of adenylate cyclase-associated protein 1 may predict brain metastasis in non-small cell lung cancer. Oncol Rep. 2015;33(1):363–371. doi: 10.3892/or.2014.3577. [DOI] [PubMed] [Google Scholar]
- 25.Hua M, Yan S, Deng Y, Xi Q, Liu R, Yang S, Liu J, Tang C, Wang Y, Zhong J. CAP1 is overexpressed in human epithelial ovarian cancer and promotes cell proliferation. Int J Mol Med. 2015;35(4):941–949. doi: 10.3892/ijmm.2015.2089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Liu Y, Cui X, Hu B, Lu C, Huang X, Cai J, He S, Lv L, Cong X, Liu G. Upregulated expression of CAP1 is associated with tumor migration and metastasis in hepatocellular carcinoma. Pathol Res Pract. 2014;210(3):169–175. doi: 10.1016/j.prp.2013.11.011. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Correlation of Clinicopathological Parameters and Cap2 Expression in Overall Cohort
Supplementary Table 2. Univariate and Multivariate Analysis of Clinicopathological and Cap2 for Overall Survival in the Training Cohort (n = 312)
Supplementary Table 3. Univariate and Multivariate Analysis of Clinicopathological and Cap2 for Overall Survival in the Validation Cohort (n = 208)