ABSTRACT
Objectives:
The aim of the study was to review published evidence and the opinion of practising clinicians on the prevalence and long-term health consequences of functional gastrointestinal symptoms in infants younger than 12 months.
Methods:
PubMed was searched from inception to November 2014 to find articles reporting the prevalence and long-term health outcomes of infantile colic, regurgitation, functional constipation, functional diarrhoea, and dyschezia in infants younger than <12 months. A questionnaire was sent to practising clinicians worldwide, and a group of 15 international experts met to discuss the likely frequency and longer-term consequences of these symptoms.
Results:
The literature search identified 30 studies reporting the prevalence of infantile colic (2%–73%), 13 that of regurgitation (3%–87%), 8 that of functional constipation (0.05%–39.3%), 2 that of functional diarrhoea (2%–4.1%), and 3 that of dyschezia (0.9%–5.6%). The studies varied in design, populations investigated, and definition of the symptoms. Questionnaires were received from 369 respondents. The experts agreed that the likely prevalences for colic, regurgitation, and functional constipation were 20%, 30%, and 15%, respectively. The limited data in the literature for functional diarrhoea and dyschezia suggest prevalences <10%. Infantile colic may be associated with future health problems in a subset of infants.
Conclusions:
Functional gastrointestinal symptoms appear to occur in a significant proportion of infants younger than 12 months and may have an impact on future health outcomes. Prospective collection of data according to agreed criteria is needed to obtain more accurate estimates of the prevalence and consequences of these symptoms.
Keywords: constipation, dyschezia, functional diarrhoea, functional gastrointestinal disorder, infant, infantile colic, regurgitation
Functional gastrointestinal (GI) symptoms are frequently observed in infancy (1), whether they are accompaniments to physiological development or arise from maladaptive behavioural responses to internal or external stimuli (2). Various definitions and classification or diagnostic criteria for these disorders have been developed, including the Rome III criteria published in 2006 (1). Practical algorithms for managing many of these symptoms have also been published (3). The real frequency of these symptoms among young infants, however, remains uncertain (4), as do their consequences for future health. The aim here was to review published evidence and the opinion of practising clinicians on the prevalence and long-term health consequences of functional GI symptoms in infants of age <12 months.
METHODS
PubMed was searched from inception to November 2014 to find articles reporting the prevalence in population-based studies of infantile colic (including crying and fussing), regurgitation, functional constipation, functional diarrhoea, and dyschezia in infants younger than 12 months, as well as the longer-term effects on children's health. Intervention studies were not included.
A questionnaire was sent to general paediatricians, paediatric gastroenterologists, and other health care professionals involved with the care of infants and their families worldwide, asking them what criteria they used to diagnose the conditions under consideration, what they considered the local prevalence to be, and whether they had any unpublished local data. The questions for the survey were constructed by the lead author (Y.V.) and discussed with the coauthors. When consensus was reached, the questionnaire was distributed to practising clinicians via the authors, national societies of paediatrics and paediatric gastroenterology, and the “bulletin board” (a worldwide electronic communication tool for paediatric gastroenterologists) using the online SurveyMonkey tool. The total number of questionnaires distributed is unknown. Publications suggested by respondents were added to the literature search findings. Finally, a group of 15 international experts in the field met to discuss the data and to reach a consensus on the likely prevalence and longer-term consequences of these frequent GI symptoms, and to identify areas where more data are needed.
PREVALENCE OF FUNCTIONAL GI SYMPTOMS AT 0 TO 12 MONTHS
The characteristics and findings of studies reporting the prevalence of functional GI symptoms in infants age <12 months are summarised in supplemental Tables S1–S5. Figure 1 provides a visual representation of the findings, and Table 1(5–9) summarises the prevalences from studies using Rome III criteria to define symptoms. Questionnaires were received from 369 respondents: 132 from the EU, 57 from Asia, 53 from Africa, 38 from North America, 28 from eastern Europe, 28 from the Middle East, 24 from South America, 4 from the Caribbean, 3 from Oceania, and 2 from Central America. Of these, 221 were paediatricians (other respondents included general physicians, nutritionists, and educators). Average estimated prevalences from the survey are indicated in Figure 1, and estimated prevalences by region are shown in supplemental Table S6.
FIGURE 1.
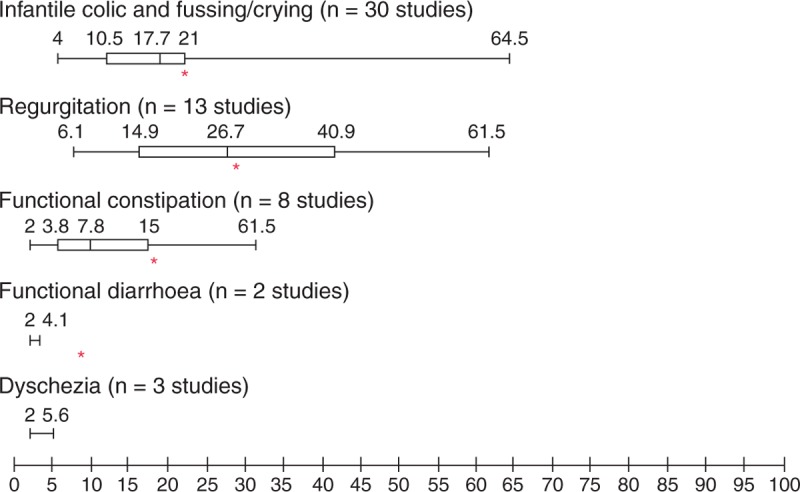
Estimated prevalence of functional gastrointestinal (GI) symptoms in infants younger than 12 months. Box shows 25th to 75th centile of literature values, with median marked; whiskers show full range. Study means were used wherein >1 value was reported. Asterisks show means from worldwide survey.
TABLE 1.
Prevalence of all symptoms using Rome III criteria
| Study, year (reference) | Country | Study design | No. in population (age range included in study, y) | Age group for symptom reported, mo | Prevalence, % |
| Infantile colic | |||||
| Chouraqui, 2011 (5) | France | Prospective population | 1211 (1–4) | 0–4 | 19 |
| van Tilburg, 2015 (6) | USA | Cross-sectional survey | 264 (0–3) | 0–4 | 6 |
| Regurgitation | |||||
| Chouraqui, 2011 (5) | France | Prospective population | 1211 (1–4) | 0–12 | 17.3 |
| van Tilburg 2015 (6) | USA | Cross-sectional survey | 264 (0–3) | 0–12 | 26 |
| Functional constipation | |||||
| Osatakul 2014 (8) | Thailand | Cross-sectional | 1749 | 0–12 | 0.05 |
| Turco 2014 (7) | Italy | Multicentre prospective cohort | 465 | 3 | 12 |
| 6 | 14 | ||||
| 12 | 11 | ||||
| van Tilburg 2015 (6) | USA | Cross-sectional survey | 264 (0–3) | 0–12 | 5 |
| Functional diarrhoea | |||||
| van Tilburg 2015 (6) | USA | Cross-sectional survey | 264 (0–3) | 0–12 | 2 |
| Dyschezia | |||||
| Chouraqui 2011 (5) | France | Prospective population | 1211 (1–4) | 0–6 | 5.6 |
| Kramer 2014 (9) | Netherlands | Prospective cohort | 1292 | 1 | 3.9 |
| 3 | 0.9 | ||||
| van Tilburg 2015 (6) | USA | Cross-sectional survey | 264 (0–3) | 0–12 | 2 |
Infantile Colic
Literature Search
Thirty studies were found, reporting a prevalence of infantile colic or crying/fussing problems of between 2% and 73% in infants younger than 12 months (4–6,10–36). Of these, 18 were prospective studies; the rest were cross-sectional or retrospective surveys (supplemental Table S1). Only 2 studies used the Rome III criteria of paroxysms of irritability, fussing, or crying that starts and stops without obvious cause, lasts ≥3 hours/day and occurs ≥3 days/week for ≥1 week, in infants from birth to 4 months (Table 1). One of these was prospective and reported a prevalence of infantile colic of 19% (5), whereas the other was cross-sectional and reported a prevalence of 6% (6). Another 6 studies used the Wessel criteria (crying for ≥3 hours/day, for ≥3 days/week, for ≥3 weeks), reporting prevalences between 9% and 22% (16,19,26–29). The other studies used a variety of definitions. One study reported prevalences ranging from 9% to 16% depending on the definition used (19). The study reporting the highest prevalence was based on parental report of paroxysmal irritability (30). Studies including only infants aged younger than 4 months reported prevalences ranging from 4% to 28%.
A systematic review from 2001 of 15 community-based surveys of the occurrence of infantile colic found occurrence rates in the first 3 months of life ranging from 3% to 28% in prospective studies and from 8% to 40% in retrospective studies (37).
Worldwide Survey and Expert Consensus
The overall average worldwide prevalence of infantile colic reported by the survey respondents (n = 227) was 21%, with most respondents using the Rome III criteria and a few the Wessel criteria. The prevalence of “colicky infants” who may not meet formal diagnostic criteria was slightly higher, with a worldwide average of 24%.
The expert group noted that according to Rome III criteria, infantile colic occurs only before the age of 4 months. The consensus was that the worldwide prevalence of infantile colic is uncertain, but is estimated to be approximately 20%; good quality data are lacking.
Regurgitation
Literature Search
Thirteen studies reported a wide range of prevalences of regurgitation (from 3% to 87%) in infants younger than 12 months (4,11,6,38–46). Of these, 8 were prospective studies and 5 were cross-sectional. The criteria used to define regurgitation varied widely. Two studies used the Rome III criteria of 2 or more episodes per day for at least 3 weeks (Table 1), reporting prevalences of 17.3% and 26% (5,6). Other studies used definitions ranging from at least one episode per day to at least 4 episodes per day. In studies reporting on infants at different ages, prevalence was highest in the first few months of life and declined after approximately 6 months (supplemental Table S2).
Worldwide Survey and Expert Consensus
The respondents to the survey (n = 210) reported an overall average worldwide prevalence of regurgitation of 29%. Diagnosis is mainly symptom based, with some respondents using Rome III criteria or the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition/European Society for Pediatric Gastroenterology, Hepatology, and Nutrition guidelines. The overall prevalence of infants with more than 4 episodes of regurgitation per day was 23%.
The expert consensus was that the worldwide prevalence of infant regurgitation according to Rome III criteria is uncertain, but is estimated to be approximately 30%; good-quality data are lacking.
Functional Constipation
Literature Search
Eight studies were found, reporting prevalences of functional constipation ranging from 0.05% to 39.3% in infants younger than 12 months (4,6–9,11,45–49) (supplemental Table S3). Only 2 of the studies were prospective, 5 were cross-sectional and 1 was retrospective. Three of the studies used the Rome III criteria of passage of large diameter stools at intervals of less than twice per week, with retentive posturing and avoiding defecation by purposefully contracting the pelvic floor (Table 1). Of these, 1 prospective study found that functional constipation was present in 12% of the 465 infants at 3 months, 14% at 6 months, and 11% at 12 months after birth (7). The other 2 studies were cross-sectional and reported prevalences of 0.05% and 5% (6,8).
Worldwide Survey and Expert Consensus
The overall average worldwide prevalence of infant constipation reported by respondents (n = 198) was 18%. Approximately one-fifth of the respondents use the Rome III criteria, whereas the rest use specific symptoms such as frequency of defecation, consistency of stools, and pain experienced. The overall reported prevalence of constipation-like symptoms was 20%.
The expert consensus was that the worldwide prevalence of functional constipation in infants age younger than 12 months is uncertain, but is estimated to be approximately 15%, depending on the type of feeding; good quality data are lacking.
Functional Diarrhoea
Literature Search
The literature search found only 2 articles that specifically reported the prevalence of functional diarrhoea (4,6). An Italian prospective study reported a prevalence of diarrhoea (supplemental Table S4) of 4.1% at 0 to 12 months (4). In a US cross-sectional study, the prevalence of functional diarrhoea according to Rome III criteria (daily painless, recurrent passage of ≥3 large, unformed stools for ≥4 weeks starting after 6 months of age) was 2% among infants younger than 12 months (Table 1) (6).
Worldwide Survey and Expert Consensus
According to the respondents to the survey (n = 192), the overall average worldwide prevalence of functional diarrhoea (mainly diagnosed using Rome III criteria) was 9%.
The expert group noted that studies reporting the prevalence of functional, as distinct from acute, diarrhoea are scarce. They also noted that functional diarrhoea in children typically starts in the toddler age group and was often referred to in the past as “toddlers’ diarrhoea”; a diagnosis below the age of 2 years is not frequent. The consensus was that the worldwide prevalence of functional diarrhoea is unknown, because good quality data are missing.
Dyschezia
Literature Search
Only 3 studies reporting the prevalence of infant dyschezia were found (5,6,9) (supplemental Table S5). All 3 used the Rome III criteria of at least 10 minutes of straining and crying before successful passage of soft stools without other health problems in an infant younger than 6 months of age (Table 1). In a recent US cross-sectional study, the prevalence of dyschezia according to Rome III criteria was 2% among infants younger than 12 months (6). A French prospective study found a prevalence of 5.6% at 0 to 6 months (5). A recent prospective cohort study of 1292 infants in the Netherlands found that 3.9% fulfilled the Rome III criteria for dyschezia at 1 month and 0.9% at 3 months; however, parents of 17.3% and 6.5% of infants reported symptoms preceding defecation while not strictly fulfilling the Rome III criteria at these time points (9).
Worldwide Survey and Expert Consensus
Of the respondents to the survey (n = 205), 69% were aware of infant dyschezia; 36% classified it as part of the colic spectrum, and 44% classified it as functional constipation. The expert consensus was that infant dyschezia appears to be not well known and seems to be often classified as colic or constipation, which will therefore have an impact on the management. It appears that there is a possibility to improve the definition of this entity. Therefore, more awareness and education around the condition is required.
FUTURE HEALTH OUTCOMES OF FUNCTIONAL GI SYMPTOMS
Literature Search
Literature on the future health impact of functional GI symptoms before 12 months of age is scarce. A number of studies have looked at the longer-term impact of infantile colic, but few have looked at the other symptoms discussed in this article.
Infantile Colic
For infantile colic, associations with later GI problems, atopy, migraine, and behavioural/cognitive problems have been studied. One prospective study (n = 75) found that 28% of infants with colic developed functional GI problems by the age of 13 years, compared with 6% without (50). Another prospective study (n = 96) reported an association between colic at age 31 to 87 days and recurrent abdominal pain and allergic disorders in the next 10 years (51). One prospective study (n = 90) found no association between infantile colic and subsequent risk of developing asthma and/or atopy (22), whereas another (n = 116) found an association in high-risk infants (≥1 atopic relative) (52). A retrospective case-control study found that children and adolescents ages 6 to 18 years with migraine (n = 208) were more likely (odds ratio 6.61, 95% confidence interval [CI] 4.38–10.00) to have experienced infantile colic than controls (n = 471) (53). A prospective study found that infants with colic at 3 months (n = 338) had more sleeping problems and more frequent temper tantrums at 3 years than did those without colic (n = 866) (54). A survey of parents of 228 toddlers who had had infantile colic showed that those who had received chiropractic treatment were twice as likely not to experience long-term sequelae such as temper tantrums and frequent nocturnal waking (55). A comparison of 40 children ages 6 to 8 years found that those who had had infantile colic had maternal ratings suggestive of more difficulty with emotional regulation and displayed a more impulsive cognitive style (56), and another reported that ex-colicky 4-year-old children (n = 52) displayed more negative emotions than controls (n = 118) according to the temperament scale (mean score (1–5) 3.38 vs 2.88, P = 0.001) and had more reported stomach aches (57). A prospective study (n = 202) recently reported that the duration and frequency of crying bouts in infancy was correlated with Child Behavior Check List scores at 4 years (58).
Follow-up of a cohort of 75 school-age children who had been hospitalised for persistent crying in infancy found a significantly higher prevalence of mental health problems and mental disorders compared with community controls (26% vs 10%, risk ratio 2.56, 95% CI 1.72–3.80) (59), but another prospective study looking at children ages 2 to 4 years who had cried excessively at 6 to 8 weeks reported little impact on the children's later behavioural development (60). A prospective study in 117 very-low-birth-weight infants found that longer duration of fussing and crying in extremely early infancy (0–6 weeks), but not at 5 months, was associated with less optimal psychomotor development at 24 months (61). A prospective cohort study of 561 children found that those with prolonged crying at 6 to 13 weeks had lower intelligence quotient scores at 5 years than the control group (62). Another study found that children (n = 53) referred for persistent crying in infancy (mean 3.8 months) were at increased risk for hyperactivity problems and academic difficulties later in childhood (8–10 years) compared with classroom controls (n = 64) (63).
A meta-analysis of 22 longitudinal studies found that children with previous regulatory problems of feeding/sleeping/crying had more behavioural problems than controls (weighted mean effect size 0.41, 95% CI 0.28–0.54) (64). Studies have reported that regulatory problems in the first year of life are associated with hyperkinetic symptoms throughout childhood (65), infections and behavioural problems at the age of 2 years (66), behavioural problems at 3.5 years (67), as well as deficits in preschool adaptive behaviour and social skills, and eating problems at 20 and 56 months (68). One study found that regulatory problems at 5 months in girls were directly predictive of lower cognition at 56 months, whereas in boys the influence on cognition at 56 months was mediated by delayed mental development at 20 months (69). The UK Avon Longitudinal Study of Parents and Children found that having multiple regulatory problems was strongly associated with dysregulated behaviours later in childhood (70).
Regurgitation
In an Australian prospective birth cohort (41), infants with spitting on 90 days or more during the first 2 years of life were more likely to have gastro-oesophageal reflux symptoms at 9 years of age (relative risk 2.3, 95% CI 1.3–4.0 vs those with no spitting). Another study of infants with gastro-oesophageal reflux diagnosed before age 11 months found that 70% were still affected after 1 year of conservative treatment; of the 28 children followed up in the longer term, pathological reflux persisted in 7 of them at age 4, 5 at age 5, and 3 beyond 5 years (71).
Functional Constipation
A follow-up study of 47 children who had functional constipation in the first year of life and were seen in a tertiary centre, 69% of whom had recovered after 6 months, found that a relapse had occurred in 15% within 3 years. A duration of <3 months before referral was significantly correlated with a better outcome, suggesting that early therapeutic intervention may beneficially contribute to the resolution of constipation (72). Another study reported long-term outcomes in 90 children with chronic constipation before the age of 4 years. Follow-up a mean of 6.9 years after initial evaluation found that 57 (63%) had recovered; the recovery rate was higher in those ages younger than 2 years at initial evaluation (73). A few studies have reported a history of GI symptoms in children with autistic spectrum disorder (74–76), whereas others have found no such association (77,78).
Expert Consensus
The experts noted that infantile colic (by definition) does not start after 4 months of age (and in most cases it has disappeared by 4 months), so only associations with other conditions (and not future occurrence of colic) are relevant. The consensus was that infantile colic may be associated with future health problems, as suggested by the available literature; however, the possibility that these health problems present initially as infantile colic cannot be ruled out. Prospective studies are required to confirm establish these relationships, although proving causality would be impossible.
Regarding regurgitation, the experts noted that failure to treat reflux disease properly has consequences, but it is not known whether this is also the case for infant regurgitation; however, it was felt that inappropriate management may have adverse effects. The consensus was that it is uncertain if infant regurgitation is associated with future health problems; there are associations occurring within the literature, but prospective studies are required to confirm this hypothesis.
The experts noted that while infantile colic and regurgitation will usually resolve without management, this is less likely for constipation. The consensus was that functional constipation in infants may be associated with future GI problems, but this is uncertain and prospective studies would be needed to confirm it; one study suggests a positive impact of early treatment.
For functional diarrhoea, the expert consensus was that functional diarrhoea before the age of 12 months appears to have no long-term consequences. As regard dyschezia, the consensus was that there is no evidence that infant dyschezia leads to later functional constipation or other GI symptoms.
DISCUSSION
Studies on the prevalence and long-term health outcomes of functional GI symptoms other than colic in infants younger than 12 months are scarce. For most of the symptoms, many of the prevalence studies were conducted several decades ago; the study designs, populations studied and definitions used make it difficult to compare studies and draw firm conclusions. The reported prevalences varied widely: from 2% to 73% (30 studies) for infantile colic, 3% to 87% (12 studies) for infant regurgitation, and 0.1% to 39% (8 studies) for functional constipation; few studies used the Rome III criteria for these symptoms (Table 1). The small number of studies found for functional diarrhoea and dyschezia reported prevalences <10%.
The findings from the survey among practising clinicians are largely consistent with the average incidence found in the literature. Interestingly, infantile colic and functional diarrhoea were the functional GI disorders that were according to the respondents mainly diagnosed by Rome III criteria. Constipation was diagnosed according to Rome III criteria by only approximately 20% of the respondents, and the biggest gap in usage of standardised diagnosis was for dyschezia, which was not perceived by approximately 80% of the respondents as a separate diagnostic entity. Examination of any regional differences revealed by the survey responses, and comparison with published regional data, may be considered as the next step in this project.
On the basis of the evidence available, the experts considered that the likely worldwide prevalences according to Rome III criteria are approximately 20% for infantile colic, 30% for regurgitation, and 15% for functional constipation. The limited data for functional diarrhoea and dyschezia suggest prevalences <10%, but the latter in particular is not well understood. In the future, collection of reliable data on all these symptoms according to agreed criteria is required, to obtain a more accurate estimate. Infantile colic appears to be associated with future health problems such as GI disorders, migraine, and behavioural/developmental problems. Evidence for future problems associated with the other symptoms is lacking, but it seems that early management of constipation may be important.
Although this review has considered several functional GI symptoms separately in terms of prevalence and future health outcomes, there is overlap between the various symptoms in practice. For example, a recent study looking at the effects of a novel infant formula found that colic at 4 weeks of age was associated with flatulence, abdominal distension, constipation, diarrhoea, and regurgitation (79). In a survey about functional GI disorders performed among 273 paediatricians (80), 2747 infants ages between 0 and 6 months (mean age 6.9 weeks, exclusively formula fed) were studied. Only a single functional GI symptom was present in 602 infants (regurgitation in 63.8%, colic in 20.5%, constipation in 9.1%), but several symptoms were combined in 2145 infants. The most frequent associations seen in the infants were bloating and colic (36.2%), regurgitation and colic (22.4%), and bloating with regurgitation (9.7%). As assessed with a French quality of life scale (QUALIN), the infants were more uncomfortable when at least 2 symptoms were combined than when there was a single symptom (5.9 vs 6.5, P < 0.001) (80).
Another factor that needs to be taken into account is feeding—whether an infant is breast-fed or formula-fed, and which type of formula is used, will influence the development of functional GI symptoms. For example, a study in the Netherlands found that breast-fed infants had more frequent, softer stools in the first 3 months of life than did infants fed standard formula (81). Average daily defecation frequency decreased significantly during the first 3 months (from 3.65 to 1.88 times/day), whereas no significant changes were observed in infants fed standard formula or mixed feeding. Many of the studies discussed here date from before the introduction of infant formulas containing prebiotic and probiotic agents. New ingredients introduced in the past 10 years may have had an impact on the prevalence and outcome of some of the symptoms discussed. In colicky infants, trying a nonallergic diet for a short time followed by a challenge has been shown to be of benefit in some studies (82).
In conclusion, the functional GI symptoms considered here appear to occur in a significant proportion of infants younger than 12 months old (possibly up to 30%) and may have an impact on future health outcomes. Collection of reliable data in prospective studies and according to agreed criteria is needed to obtain more accurate estimates of the prevalence and consequences of these common symptoms.
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Footnotes
Financial support was received from Danone Nutricia Early Life Nutrition. The authors thank Nik Loveridge (Danone) for his support and Clare Griffith for assistance with the literature search and analysis.
All authors received honoraria from DanoneNutricia to attend the consensus meeting. Y.V. has participated as a clinical investigator, and/or advisory board member, and/or consultant, and/or speaker for Abbott Nutrition, Aspen, Biogaia, Biocodex, Danone, Hero, Nestle Nutrition Institute, Nutricia, Mead Johnson Nutrition, Merck, Orafti, Phacobel, Sari Husada, United Pharmaceuticals, Wyeth, and Yakult. T.H. is engaged by Danone Nutricia on an Ad Hoc basis to speak on ELN in Australia. C.L. is an advisory board member and/or consultant and/or speaker for Nestlé, Nestlé Nutrition Institute, Mead Johnson, Ipsen, and Sequoia. M.B.M. has participated as consultant and/or speaker for Danone Advanced Medical Nutrition, Danone Early Nutrition, Mead Johnson, Achê, Bago. R.S. has participated as a clinical investigator, advisory board member, or consultant or speaker for Abbott, Danone, Enzymotec, Ferrero, Nestlé Nutrition Institute, Nutricia, and Teva. A.S. has participated as a clinical investigator, and/or advisory board member, and/or consultant, and/or speaker for D.M.G, Valeas, Angelini, Miltè, Danone, Nestlé, Sucampo, and Menarini. H.S. has participated as a clinical investigator, and/or advisory board member, and/or consultant, and/or speaker for Arla, Biogaia, Biocodex, Danone, Dicofarm, Hipp, Nestle, Nestle Nutrition Institute, Nutricia, Mead Johnson, Merck, and Sequoia. N.T. has participated as a speaker and/or advisory board member for Danone, Nutricia, Shire Movetis and Sucampo. The other authors report no conflicts of interest.
REFERENCES
- 1.Drossman DA, Dumitrascu DI. Rome III: new standard for functional gastrointestinal disorders. J Gastrointestin Liver Dis 2006; 15:237–241. [PubMed] [Google Scholar]
- 2.Shamir R, St James-Roberts I, Di Lorenzo C, et al. Infant crying, colic, and gastrointestinal discomfort in early childhood: a review of the evidence and most plausible mechanisms. J Pediatr Gastroenterol Nutr 2013; 57 suppl 1:S1–S45. [DOI] [PubMed] [Google Scholar]
- 3.Vandenplas Y, Gutierrez-Castrellon P, Velasco-Benitez C, et al. Practical algorithms for managing common gastrointestinal symptoms in infants. Nutrition 2013; 29:184–194. [DOI] [PubMed] [Google Scholar]
- 4.Iacono G, Merolla R, D’Amico D, et al. Gastrointestinal symptoms in infancy: a population-based prospective study. Dig Liver Dis 2005; 37:432–438. [DOI] [PubMed] [Google Scholar]
- 5.Chouraqui JP, Brancato S, Rubio A, et al. Prevalence of functional intestinal disorders in infants and young children. Poster presented at European Society for Paediatric Gastroenterology, Hepatology, and Nutrition meeting; Sorrento, Italy; May 25–28, 2011. [Google Scholar]
- 6.van Tilburg MA, Hyman PE, Walker L, et al. Prevalence of functional gastrointestinal disorders in infants and toddlers. J Pediatr 2015; 166:684–689. [DOI] [PubMed] [Google Scholar]
- 7.Turco R, Miele E, Russo M, et al. Early-life factors associated with pediatric functional constipation. J Pediatr Gastroenterol Nutr 2014; 58:307–312. [DOI] [PubMed] [Google Scholar]
- 8.Osatakul S, Puetpaiboon A. Use of Rome II versus Rome III criteria for diagnosis of functional constipation in young children. Pediatr Int 2014; 56:83–88. [DOI] [PubMed] [Google Scholar]
- 9.Kramer EA, den Hertog-Kuijl JH, van den Broek LM, et al. Defecation patterns in infants: a prospective cohort study. Arch Dis Child 2015; 100:533–536. [DOI] [PubMed] [Google Scholar]
- 10.Stagnara J, Blanc JP, Danjou G, et al. Clinical data on the diagnosis of colic in infants. Survey in 2,773 infants aged 15-119 days. Arch Pediatr 1997; 4:959–966. [DOI] [PubMed] [Google Scholar]
- 11.Infante Pina D, Badia Llach X, Ariño-Armengol B, et al. Prevalence and dietetic management of mild gastrointestinal disorders in milk-fed infants. World J Gastroenterol 2008; 14:248–254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Crowcroft NS, Strachan DP. The social origins of infantile colic: questionnaire study covering 76,747 infants. BMJ 1997; 314:1325–1328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rubin SP, Prendergast M. Infantile colic: incidence and treatment in a Norfolk community. Child Care Health Dev 1984; 10:219–226. [DOI] [PubMed] [Google Scholar]
- 14.Rautava P, Helenius H, Lehtonen L. Psychosocial predisposing factors for infantile colic. BMJ 1993; 307:600–604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ståhlberg MR. Infantile colic: occurrence and risk factors. Eur J Pediatr 1984; 143:108–111. [DOI] [PubMed] [Google Scholar]
- 16.Lehtonen L, Korvenranta H. Infantile colic. Seasonal incidence and crying profiles. Arch Pediatr Adolesc Med 1995; 149:533–536. [DOI] [PubMed] [Google Scholar]
- 17.Hide DW, Guyer BM. Prevalence of infant colic. Arch Dis Child 1982; 57:559–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Canivet C, Ostergren PO, Jakobsson I, et al. Higher risk of colic in infants of nonmanual employee mothers with a demanding work situation in pregnancy. Int J Behav Med 2004; 11:37–47. [DOI] [PubMed] [Google Scholar]
- 19.Canivet C, Hagander B, Jakobsson I, et al. Infantile colic—less common than previously estimated? Acta Paediatr 1996; 85:454–458. [DOI] [PubMed] [Google Scholar]
- 20.Lothe L, Ivarsson SA, Ekman R, et al. Motilin and infantile colic. A prospective study. Acta Paediatr Scand 1990; 79:410–416. [DOI] [PubMed] [Google Scholar]
- 21.Høgdall CK, Vestermark V, Birch M, et al. The significance of pregnancy, delivery and postpartum factors for the development of infantile colic. J Perinat Med 1991; 19:251–257. [PubMed] [Google Scholar]
- 22.Castro-Rodriguez JA, Stern DA, Halonen M, et al. Relation between infantile colic and asthma/atopy: a prospective study in an unselected population. Pediatrics 2001; 108:878–882. [DOI] [PubMed] [Google Scholar]
- 23.Thomas DW, McGilligan K, Eisenberg LD, et al. Infantile colic and type of milk feeding. Am J Dis Child 1987; 141:451–453. [DOI] [PubMed] [Google Scholar]
- 24.Clifford TJ, Campbell MK, Speechley KN, et al. Infant colic: empirical evidence of the absence of an association with source of early infant nutrition. Arch Pediatr Adolesc Med 2002; 156:1123–1128. [DOI] [PubMed] [Google Scholar]
- 25.Howard CR, Lanphear N, Lanphear BP, et al. Parental responses to infant crying and colic: the effect on breastfeeding duration. Breastfeed Med 2006; 1:146–155. [DOI] [PubMed] [Google Scholar]
- 26.Saavedra MA, da Costa JS, Garcias G, et al. Infantile colic incidence and associated risk factors: a cohort study. J Pediatr (Rio J) 2003; 79:115–122. [PubMed] [Google Scholar]
- 27.Fazil M. Prevalence and risk factors for infantile colic in District Mansehra. J Ayub Med Coll Abbottabad 2011; 23:115–117. [PubMed] [Google Scholar]
- 28.Talachian E, Bidari A, Rezaie MH. Incidence and risk factors for infantile colic in Iranian infants. World J Gastroenterol 2008; 14:4662–4666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Akman I, Kusçu K, Ozdemir N, et al. Mothers’ postpartum psychological adjustment and infantile colic. Arch Dis Child 2006; 91:417–419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cohen Engler A, Hadash A, Shehadeh N, et al. Breastfeeding may improve nocturnal sleep and reduce infantile colic: potential role of breast milk melatonin. Eur J Pediatr 2012; 171:729–732. [DOI] [PubMed] [Google Scholar]
- 31.Tasche MJ, Bruijnzeels MA, van der Poel BN, et al. Infants who cry a lot: incidence and management of this problem in family practice. Ned Tijdschr Geneeskd 1993; 137:1927–1930. [PubMed] [Google Scholar]
- 32.van der Wal MF, van den Boom DC, Pauw-Plomp H, et al. Mothers’ reports of infant crying and soothing in a multicultural population. Arch Dis Child 1998; 79:312–317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Reijneveld SA, Lanting CI, Crone MR, et al. Exposure to tobacco smoke and infant crying. Acta Paediatr 2005; 94:217–221. [DOI] [PubMed] [Google Scholar]
- 34.Wurmser H, Lanting CI, Crone MR, et al. Excessive infant crying: often not confined to the first 3 months of age. Early Hum Dev 2001; 64:1–6. [DOI] [PubMed] [Google Scholar]
- 35.Forsyth BW, Leventhal JM, McCarthy PL. Mothers’ perceptions of problems of feeding and crying behaviors: a prospective study. Am J Dis Child 1985; 139:269–272. [DOI] [PubMed] [Google Scholar]
- 36.Wake M, Morton-Allen E, Poulakis Z, et al. Prevalence, stability, and outcomes of cry-fuss and sleep problems in the first 2 years of life: prospective community-based study. Pediatrics 2006; 117:836–842. [DOI] [PubMed] [Google Scholar]
- 37.Lucassen PL, Assendelft WJ, van Eijk JT, et al. Systematic review of the occurrence of infantile colic in the community. Arch Dis Child 2001; 84:398–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Miele E, Simeone D, Marino A, et al. Functional gastrointestinal disorders in children: an Italian prospective survey. Pediatrics 2004; 114:73–78. [DOI] [PubMed] [Google Scholar]
- 39.Nelson SP, Chen EH, Syniar GM, et al. Prevalence of symptoms of gastroesophageal reflux during infancy. A pediatric practice-based survey. Arch Pediatr Adolesc Med 1997; 151:569–572. [DOI] [PubMed] [Google Scholar]
- 40.Van Howe RS, Storms MR. Gastroesophageal reflux symptoms in infants in a rural population: longitudinal data over the first six months. BMC Pediatr 2010; 10:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Martin AJ, Pratt N, Kennedy JD, et al. Natural history and familial relationships of infant spilling to 9 years of age. Pediatrics 2002; 109:1061–1067. [DOI] [PubMed] [Google Scholar]
- 42.Hegar B, Boediarso A, Firmansyah A, et al. Investigation of regurgitation and other symptoms of gastroesophageal reflux in Indonesian infants. World J Gastroenterol 2004; 10:1795–1797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hegar B, Dewanti NR, Kadim M, et al. Natural evolution of regurgitation in healthy infants. Acta Paediatr 2009; 98:1189–1193. [DOI] [PubMed] [Google Scholar]
- 44.Miyazawa R, Tomomasa T, Kaneko H, et al. Prevalence of gastro-esophageal reflux-related symptoms in Japanese infants. Pediatr Int 2002; 44:513–516. [DOI] [PubMed] [Google Scholar]
- 45.Osatakul S, Sriplung H, Puetpaiboon A, et al. Prevalence and natural course of gastroesophageal reflux symptoms: a 1-year cohort study in Thai infants. J Pediatr Gastroenterol Nutr 2002; 34:63–67. [DOI] [PubMed] [Google Scholar]
- 46.Campanozzi A, Boccia G, Pensabene L, et al. Prevalence and natural history of gastroesophageal reflux: pediatric prospective survey. Pediatrics 2009; 123:779–783. [DOI] [PubMed] [Google Scholar]
- 47.Kocaay P, Eğrıtaş O, Dalgiç B. Normal defecation pattern, frequency of constipation and factors related to constipation in Turkish children 0-6 years old. Turk J Gastroenterol 2011; 22:369–375. [DOI] [PubMed] [Google Scholar]
- 48.Tunc VT, Camurdan AD, Ilhan MN, et al. Factors associated with defecation patterns in 0-24-month-old children. Eur J Pediatr 2008; 167:1357–1362. [DOI] [PubMed] [Google Scholar]
- 49.Loening-Baucke V. Prevalence, symptoms and outcome of constipation in infants and toddlers. J Pediatr 2005; 146:359–363. [DOI] [PubMed] [Google Scholar]
- 50.Partty A, Kalliomaki M, Salminen S, et al. Infant distress and development of functional gastrointestinal disorders in childhood: is there a connection? JAMA Pediatr 2013; 167:977–978. [DOI] [PubMed] [Google Scholar]
- 51.Savino F, Castagno E, Bretto R, et al. A prospective 10-year study on children who had severe infantile colic. Acta Paediatr Suppl 2005; 94:129–132. [DOI] [PubMed] [Google Scholar]
- 52.Kalliomäki M, Laippala P, Korvenranta H, et al. Extent of fussing and colic type crying preceding atopic disease. Arch Dis Child 2001; 84:349–350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Romanello S, Spiri D, Marcuzzi E, et al. Association between childhood migraine and history of infantile colic. JAMA 2013; 309:1607–1612. [DOI] [PubMed] [Google Scholar]
- 54.Rautava P, Lehtonen L, Helenius H, et al. Infantile colic: child and family three years later. Pediatrics 1995; 96:43–47. [PubMed] [Google Scholar]
- 55.Miller JE, Phillips HL. Long-term effects of infant colic: a survey comparison of chiropractic treatment and nontreatment groups. J Manipulative Physiol Ther 2009; 32:635–638. [DOI] [PubMed] [Google Scholar]
- 56.Neu M, Robinson J. Infants with colic: their childhood characteristics. J Pediatr Nurs 2003; 18:12–20. [DOI] [PubMed] [Google Scholar]
- 57.Canivet C, Jakobsson I, Hagander B. Infantile colic. Follow-up at four years of age: still more “emotional”. Acta Paediatr 2000; 89:13–17. [DOI] [PubMed] [Google Scholar]
- 58.Korja R, Huhtala M, Maunu J, et al. Preterm infant's early crying associated with child's behavioral problems and parents’ stress. Pediatrics 2014; 133:e339–e345. [DOI] [PubMed] [Google Scholar]
- 59.Brown M, Heine RG, Jordan B. Health and well-being in school-age children following persistent crying in infancy. J Paediatr Child Health 2009; 45:254–262. [DOI] [PubMed] [Google Scholar]
- 60.Elliott MR, Pedersen EL, Mogan J. Early infant crying: child and family follow-up at three years. Can J Nurs Res 1997; 29:47–67. [PubMed] [Google Scholar]
- 61.Munck P, Maunu J, Kirjavainen J, et al. Crying behaviour in early infancy is associated with developmental outcome at two years of age in very low birth weight infants. Acta Paediatr 2008; 97:332–336. [DOI] [PubMed] [Google Scholar]
- 62.Rao MR, Brenner RA, Schisterman EF, et al. Long term cognitive development in children with prolonged crying. Arch Dis Child 2004; 89:989–992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Wolke D, Rizzo P, Woods S. Persistent infant crying and hyperactivity problems in middle childhood. Pediatrics 2002; 109:1054–1060. [DOI] [PubMed] [Google Scholar]
- 64.Hemmi MH, Wolke D, Schneider S. Associations between problems with crying, sleeping and/or feeding in infancy and long-term behavioural outcomes in childhood: a meta-analysis. Arch Dis Child 2011; 96:622–629. [DOI] [PubMed] [Google Scholar]
- 65.Becker K, Holtmann M, Laucht M, et al. Are regulatory problems in infancy precursors of later hyperkinetic symptoms? Acta Paediatr 2004; 93:1463–1469. [DOI] [PubMed] [Google Scholar]
- 66.Dahl M. Early feeding problems in an affluent society. III. Follow-up at two years: natural course, health, behaviour and development. Acta Paediatr Scand 1987; 76:872–880. [DOI] [PubMed] [Google Scholar]
- 67.Forsyth BW, Canny PF. Perceptions of vulnerability 3 1/2 years after problems of feeding and crying behavior in early infancy. Pediatrics 1991; 88:757–763. [PubMed] [Google Scholar]
- 68.Schmid G, Schreier A, Meyer R, et al. A prospective study on the persistence of infant crying, sleeping and feeding problems and preschool behaviour. Acta Paediatr 2010; 99:286–290. [DOI] [PubMed] [Google Scholar]
- 69.Wolke D, Schmid G, Schreier A, et al. Crying and feeding problems in infancy and cognitive outcome in preschool children born at risk: a prospective population study. J Dev Behav Pediatr 2009; 30:226–238. [DOI] [PubMed] [Google Scholar]
- 70.Winsper C, Wolke D. Infant and toddler crying, sleeping and feeding problems and trajectories of dysregulated behavior across childhood. J Abnorm Psychol 2014; 42:831–843. [DOI] [PubMed] [Google Scholar]
- 71.Semeniuk J, Kaczmarski M, Sidor K, et al. Long-term clinical observation of infants with gastroesophageal reflux. Pol Merkur Lekarski 2004; 16:208–212. [PubMed] [Google Scholar]
- 72.van den Berg MM, van Rossum CH, de Lorijn F, et al. Functional constipation in infants: a follow-up study. J Pediatr 2005; 147:700–704. [DOI] [PubMed] [Google Scholar]
- 73.Loening-Baucke V. Constipation in early childhood: patient characteristics, treatment, and longterm follow up. Gut 1993; 34:1400–1404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Molloy CA, Manning-Courtney P. Prevalence of chronic gastrointestinal symptoms in children with autism and autistic spectrum disorders. Autism 2003; 7:165–171. [DOI] [PubMed] [Google Scholar]
- 75.Niehus R, Lord C. Early medical history of children with autism spectrum disorders. J Dev Behav Pediatr 2006; 27 (2 suppl):S120–S127. [DOI] [PubMed] [Google Scholar]
- 76.Valicenti-McDermott M, McVicar K, Rapin I, et al. Frequency of gastrointestinal symptoms in children with autistic spectrum disorders and association with family history of autoimmune disease. J Dev Behav Pediatr 2006; 27 (2 suppl):S128–S136. [DOI] [PubMed] [Google Scholar]
- 77.Adams JB, Johansen LJ, Powell LD, et al. Gastrointestinal flora and gastrointestinal status in children with autism—comparisons to typical children and correlation with autism severity. BMC Gastroenterol 2011; 11:22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Black C, Kaye JA, Jick H. Relation of childhood gastrointestinal disorders to autism: nested case-control study using data from the UK General Practice Research Database. BMJ 2002; 325:419–421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Vandenplas Y, Ludwig T, Bouritius H, et al. The combination of scGOS/lcFOS with fermented infant formula reduces the incidence of colic in 4 week old infants. Arch Dis Child 2014; 99 suppl 2:A91.abstract O-174. [Google Scholar]
- 80.Bellaiche M, Barberot V. Approche de première intention des troubles digestifs bénins associés du nourrisson de moins de six mois: résultats de l’observatoire ADAN. Médecine Enfance 2014; 34 (7 suppl):1–12. [Google Scholar]
- 81.den Hertog J, van Leengoed E, Kolk F, et al. The defecation pattern of healthy term infants up to the age of 3 months. Arch Dis Child 2012; 97:F465–F470. [DOI] [PubMed] [Google Scholar]
- 82.Vandenplas Y, Broekaert I, Falconer J, et al. A consensus report on the management of frequent gastro-intestinal symptoms in <12 months old infants: regurgitation, colic, constipation, diarrhoea and cow's milk protein allergy: a position paper of the ESPGHAN Gastroenterology Committee and additional experts. In press. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


