Background
Depression affects more people than any other mental disorder and is the leading cause of disability worldwide in terms of total years lost due to disability [1]. Major depression impacts daily quality of life and is the psychiatric diagnosis most commonly associated with suicide. The lifetime suicide risk among patients with untreated depressive disorder is nearly 20% [2].
Refugees are at risk for mental health problems due to forced migration from their home countries and other traumatic experiences. For example, Karenni refugees residing along the Burmese-Thai border had a higher prevalence of depression (41%) and anxiety (42%) in comparison to the rates in the US general population (7-10% respectively). Traumatic events related to harassment, lack of basic needs, and violence were associated with depression and anxiety [3]. Similarly, 82.6% of Cambodian respondents living in Thailand-Cambodia border camps self-reported depression, characterized as “a deep sadness inside oneself.” Based on Hopkins Symptoms Checklist-25 responses, 55% of respondents experienced symptoms of major depression, and 14.7 % experienced symptoms of post-traumatic stress disorder (PTSD) [4].
In addition to pre-existing stressors and traumatic experiences, refugees resettled to a third country may experience post-resettlement problems ranging from difficulty finding jobs and accessing services to cultural and linguistic isolation, all of which could increase risk for mental illness. In a systematic review of studies of major depression with 200 or more refugees who had resettled to western countries, about 5% were diagnosed with major depression [5].
In the early 1990s, over one hundred thousand ethnic Nepalis in Bhutan fled to Nepal after experiencing human rights violations, including violence, loss of property, and citizenship [6]. Refugee camps in Nepal accommodated the influx of refugees. Third-country resettlements from Nepal to the United States began in February 2008; over 56,000 Bhutanese refugees have resettled to date [7].
During 2010, in response to the high number of suicides and suicide attempts in Bhutanese refugee camps in Nepal, the International Organization for Migration (IOM) conducted an assessment of psychological needs and suicide risk factors of Bhutanese refugees in the camps [8]. The suicide rate in the camps was 20.8/100,000, almost twice the rate in the US general population (11.1/100,000) [8]. Over 20 suicides of Bhutanese refugees have been reported in the United States from 2009-2012, prompting concern about the high rate of suicide and the need to address mental health concerns, particularly depression, in this population. Despite documented high risk, mental health burdens in Bhutanese refugees have not been characterized in published literature. Understanding the burden of depression in the Bhutanese refugee population is essential for developing culturally appropriate resources and intervention programs to improve quality of life for resettled Bhutanese refugees and to prevent suicides.
In this study we document the prevalence of depression and other mental illness symptoms in Bhutanese refugees recently resettled to the United States and explore factors associated with depression. We apply these findings to developing recommendations for addressing depression in the Bhutanese refugee community.
Methods
We randomly selected 579 Bhutanese refugees 18 years or older who resettled during January 1, 2008, through November 17, 2011, in seven cities in four states: Georgia (Atlanta), New York (Buffalo, Syracuse), Arizona (Phoenix, Tucson), and Texas (Dallas/Fort Worth, Houston). These states were chosen because of their large Bhutanese refugee populations. Exclusion criteria included declining consent or not completing the interview due to physical or mental impairment. The survey was administered in Nepali or English by trained interviewers in the respondent’s home. This study was approved by the Centers for Disease Control and Prevention (CDC) Institutional Review Board.
Instruments
Questionnaire sections included demographics, mental health symptoms and history, difficulties post migration, social support and coping mechanisms. The demographic responses were used as independent variables in the analyses, including questions on education, ability to read/write Nepali, ability to read/write English, regular income, employment status, being a provider for family, and self-reported health. Questions and response options were derived from focus group discussions with members of the Bhutanese refugee community and interviews with key informants.
Post-migration challenges
This 22-item measure adapted from the Post-Migration Living Difficulties checklist [9]was based on focus group discussions with Bhutanese refugees. The items assessed stressors encountered by refugees resettled in the U.S. and asked participants to rate the degree they experienced these items on a 4-point Likert scale (“not at all” to “extremely”). Scores were collapsed into two categories (none/a little or a lot) for analyses.
Social support
Twelve items from the Perceived Social Support [10] measure were used to assess perceived social support related to everyday life and how the participant perceived the current social support level provided by his/her social network. Participants were asked to rate how true each item is for them at that moment on a 5-point Likert scale (“strongly disagree” to “strongly agree”). The social support score was the sum of all items and was categorized as low (0-39), medium (40-49) or high (50-60) perceived social support.
Coping
Coping was assessed using items from the Coping Strategies Indicator [11] comprising three items from each of the three original subscales: problem-solving coping, seeking-support coping, and avoidant coping. In addition, 9 items were created based on focus group discussions with Bhutanese refugees living in the US. Each item was scored using a Likert-type scale of 1 (a lot), 2 (a little), and 3 (not at all). Scores were collapsed into two categories (none/a little or a lot) for analyses.
Mental Health
The survey included validated, standardized tools to assess mental health outcomes. The Hopkins Symptom Checklist-25 (HSCL25) comprised 10 statements measuring anxiety symptoms and 15 statements measuring depression symptoms [7]. An average score of 1.75 or higher out of 4 for the anxiety and depression items was considered positive for anxiety and depression symptoms, respectively. The depression score consistently correlates with clinical diagnosis of major depression, as defined by the DSM-IV in many cultures [12]. The Harvard Trauma Questionnaire (HTQ) [13] was used to evaluate symptoms of PTSD and traumatic experiences. We defined cases meeting PTSD symptom criteria according to a scoring algorithm proposed by the Harvard Refugee Trauma Group, on the basis of DSM-IV diagnostic criteria, which required at least 1 of 5 re-experiencing symptoms, at least 3 of 7 avoidance or numbing symptoms, and at least 2 of 5 arousal symptoms [4]. The HSCL-25 and HTQ indicate the presence of mental health condition symptoms but do not provide clinical diagnosis. Participants were also asked if they had ever expressed suicidal ideation, defined as ever having thought seriously about committing suicide in their lifetimes. Interviewers were trained to implement a distressed respondent protocol1 if a participant expressed suicidal thoughts during the interview.
Data Analysis
Data were analyzed using SAS 9.2 statistical software. Data were summarized and tested for statistical significance by sex, by using the chi-square test for categorical variables and the Wilcoxon rank sum test for difference in medians for continuous variables. To determine the association between depression and risks factors, we used conditional logistic regression by state of residence, adjusted by age and sex, to estimate the odds ratios and associated 95% confidence intervals (CI).
Principle component analysis (PCA) was used to evaluate sets of questions related to post migration difficulties and coping mechanisms. PCA reduces a set of observed variables into principle components due to the redundancy in variables, thereby minimizing collinearity from correlated variables measuring possibly the same construct [14]. Each principle component was standardized to a scale from 0 to 7 to facilitate interpretation, with increasing value representing an increasing difficulty with a particular type of migration difficulty or increasing reliance on a particular approach to coping.
Multivariate logistic regression was used to model the association between symptoms of depression and 1) demographics variables, 2) PCA indices for post migration difficulties, and 3) PCA indices for coping mechanisms. Variables were retained in the multivariate model as determined by backward selection, with a 0.1 significance level as the cut-off for removal from the model. Separate models were computed for men and women, and the state of residence and age variables were forced to remain in all multivariate models.
Results
Of 423 (73%) respondents who agreed to participate in the survey, 386 (91%) were included in the analysis. The remaining respondents were omitted due to missing major variables of interest or items on the HSCL-25.
Respondent demographics
Over half the respondents were men (53%; Table 1). The median age was 34 (range 18-83). The majority of participants were married (73%) and Hindu (73%). The median time in the United States post resettlement was 1.7 years (range = 0.2-5.0). Over one-third (34%) had no education, 27% were not able to read or write Nepali, and 40% were not able to read or write English. Two-thirds (65%) had a regular income, 52% were employed, and 48% considered themselves the provider for their family; 22% self-reported poor general health, compared with 38% who reported fair health and 40% who reported good to excellent heath.
Table I.
Demographic characteristics of Bhutanese refugees, Arizona, Georgia, New York, and Texas, 2012 (N=386)
| Variable | Male n (col%) (n=204) |
Female n (col%) (n=182) |
Total N (%) |
|
|---|---|---|---|---|
| Age | Median | 33 | 35 | 34 |
| Range | 18-82 | 18-83 | 18-83 | |
|
| ||||
| Marital Statusa | Married | 141 (70) | 139 (77) | 280 (73) |
| Single | 54 (27) | 29 (16) | 83 (22) | |
| Other | 6 (3) | 13 (7) | 19 (5) | |
|
| ||||
| Education (Ed)a | None | 52 (26) | 81 (45) | 133 (34) |
| Primary | 29 (14) | 22 (12) | 51 (13) | |
| Secondary | 86 (42) | 65 (36) | 151 (39) | |
| University or graduate work | 37 (18) | 14 (8) | 51 (13) | |
|
| ||||
| Englisha | Read and write | 137 (67) | 95 (52) | 232 (60) |
| No | 67 (33) | 87 (48) | 154 (40) | |
|
| ||||
| Nepalia | Read and write | 178 (87) | 105 (58) | 283 (73) |
| No | 26 (13) | 77 (42) | 103 (27) | |
|
| ||||
| Religionb | Hindu | 138 (68) | 142 (78) | 280 (73) |
| Buddhist | 27 (13) | 10 (6) | 37 (10) | |
| Christian | 37 (18) | 26 (14) | 63 (16) | |
| Other | 2 (1) | 4 (2) | 6 (1) | |
|
| ||||
| Caste | Bahun | 71 (35) | 73 (40) | 144 (37) |
| Chhetri | 48 (24) | 47 (26) | 95 (25) | |
| Dalit | 13 (6) | 17 (9) | 30 (8) | |
| Janajati | 64 (31) | 43 (24) | 107 (28) | |
| Other | 8 (4) | 2 (1) | 10 (5) | |
|
| ||||
| Health insurance | Yes | 134 (66) | 119 (65) | 253 (66) |
| No | 70 (34.) | 60 (33) | 130 (34) | |
|
| ||||
| Regular incomea | Yes | 159 (78) | 92 (51) | 251 (65) |
| No | 45 (22) | 89 (49) | 134 (35) | |
|
| ||||
| Employeda | Yes | 137 (68) | 63 (35) | 200 (52) |
| No | 65 (32) | 116 (65) | 181 (47) | |
|
| ||||
| Provider of Familya | Yes | 130 (64) | 57 (31) | 187 (48) |
| No | 74 (36) | 125 (69) | 199 (52) | |
|
| ||||
| General healtha | Good to excellent | 96 (47) | 58 (32) | 154 (40) |
| Fair | 73 (36) | 73 (40) | 146 (38) | |
| Poor | 35 (17) | 51 (28) | 86 (22) | |
|
| ||||
| Time in US (years)c | Median | 1.6 | 1.9 | 1.7 |
| Range | 0.2-5.0 | 0.2-3.9 | 0.2-5.0 | |
Chi-square p-value <0.05
Fisher’s exact test p-value <0.05
Days in the United States is an estimate derived from the date of the interview minus the 15th day of the month and year the immigrant reported arriving in the United States.
Mental Health Conditions
One-fourth (27%) of participants had symptoms of at least one mental health condition, with women having a significantly higher prevalence than men (p=0.0097). The prevalence of symptoms of depression was 21%, of PTSD was 4%, and of anxiety was 18%. Women had a significantly higher prevalence of symptoms of depression and anxiety than men (Table 2). Symptoms of mental health conditions showed a high degree of overlap in this population (Figure 1). Of refugees with symptoms of a mental health condition, almost half (45%) experienced symptoms of multiple conditions. All refugees with symptoms of PTSD also experienced symptoms of depression, anxiety, or both.
Table II.
Symptoms of depression, post-traumatic stress and anxiety in Bhutanese refugees, Arizona, Georgia, New York, and Texas, 2012
| Male n (col%) (n=204) |
Female n (col%) (n=182) |
Total N (%) |
||
|---|---|---|---|---|
| Any mental health conditiona | Yes | 45 (22) | 60 (33) | 105 (27) |
| No | 159 (78) | 122 (67) | 281 (73) | |
|
| ||||
| Depressiona | Yes | 32 (16) | 48 (26) | 80 (21) |
| No | 172 (84) | 134 (74) | 306 (79) | |
|
| ||||
| PTSD | Yes | 4 (2) | 10 (5) | 14 (4) |
| No | 200 (98) | 172 (95) | 372 (96) | |
|
| ||||
| Anxietya | Yes | 28 (14) | 41 (23) | 69 (18) |
| No | 176 (86) | 141 (77) | 317 (82) | |
Chi-square p-value <0.05
Figure 1.
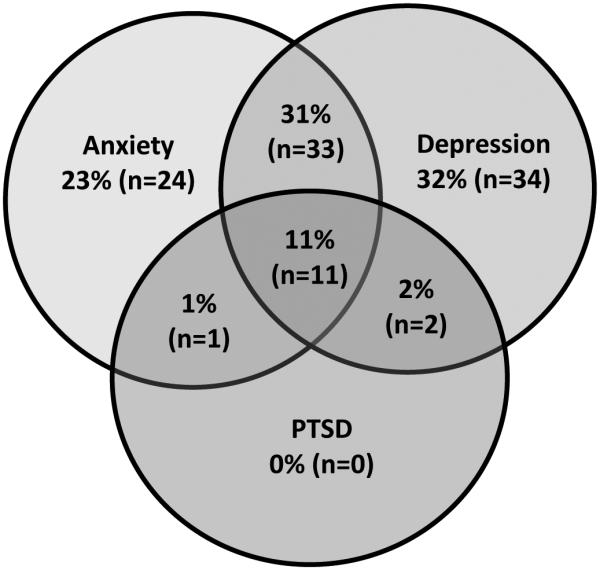
Overlapping symptoms of depression, anxiety, and post-traumatic stress in Bhutanese refugees, Arizona, Georgia, New York, and Texas, 2012 (n=105)
Symptoms of depression were significantly associated with symptoms of PTSD, anxiety, and suicidal ideation (Table 3). Refugees who had experienced more than 7 traumatic events or 4-7 traumatic events were at higher odds of symptoms of depression compared with those who had experienced 0-3 traumatic events (OR: 3.6, OR: 3.1, respectively). Refugees who perceived a low level of social support had higher odds of depression symptoms compared with those who perceived medium or high levels (Table 3).
Table III.
Association between symptoms of depression and other mental health conditions, perceived social support, and number of traumatic events experienced in Bhutanese refugees, Arizona, Georgia, New York, and Texas, 2012
| Depressed (n=80) |
Not Depressed (n=306) |
aORc
(95% CI) |
||
|---|---|---|---|---|
| PTSDa | No | 67 (84) | 305 (99.7) | Ref |
| Yes | 13 (16) | 1 (0.3) | 51.7 (6.4 – 414.7) | |
|
| ||||
| Anxietya | No | 36 (45) | 281 (92) | Ref |
| Yes | 44 (55) | 25 (8) | 11.0 (5.9 – 20.5) | |
|
| ||||
| Suicidal Ideationb, d | No | 72 (90) | 297 (97) | Ref |
| Yes | 8 (10) | 4 (1) | 10.6 (2.8 – 39.6) | |
|
| ||||
| Perceived Social Support | High | 21 (26) | 100 (33) | Ref |
| Medium | 35 (44) | 175 (57) | 1.1 (0.6 – 2.2) | |
| Low | 22 (28) | 24 (8) | 4.4 (1.9 – 10.3) | |
|
| ||||
| Traumatic events experienced | 0-3 events | 9 (11) | 102 (33) | Ref |
| 4-7 events | 37 (46) | 106 (35) | 3.1 (1.4 – 7.0) | |
| >7 events | 34 (43) | 98 (32) | 3.6 (1.5 – 8.6) | |
Chi-square p-value <0.05
Fisher’s exact test p-value <0.05
Adjusted for state of residence, age, and sex
Ever seriously thought about committing suicide
Demographic factors associated with depression
Men who considered themselves providers for their family had four times higher odds of reporting depression symptoms compared with males who were not providers (Table 4). Men who self-reported poor health had 39 time’s higher likelihood and women over seven times higher likelihood of symptoms of depression, than those with self-reported fair, good, or excellent health (Table 4). Inability to read and write Nepali increased the odds of symptoms of depression four times in men and two times in women versus those who could read and write Nepali (Table 4).
Table IV.
Demographic factors associated with symptoms of depression in Bhutanese refugees, Arizona, Georgia, New York, and Texas, 2012
|
Males (n=187)
|
Females (n=166)
|
||||||
|---|---|---|---|---|---|---|---|
| Demographic factor | Depressed | Not depressed | aOR (95%)a | Depressed | Not depressed | aOR (95%)b | |
| General Health | Good to excellent | 5 (16) | 91 (53) | Ref | 5 (16) | 53 (39) | Ref |
| Fair | 10 (31) | 63 (37) | 1.4 (0.4 – 5.3) | 17 (35) | 56 (42) | 2.8 (0.9 – 8.9) | |
| Poor | 17 (53) | 18 (10) | 39.7 (7.2 – 218.9) | 26 (54) | 25 (19) | 7.6 (2.1 – 27.3) | |
|
| |||||||
| Nepali | Read and write | 22 (69) | 156 (91) | Ref | 15 (31) | 90 (67) | Ref |
| No | 10 (31) | 16 (9) | 4.3 (1.1 – 16.5) | 33 (64) | 44 (33) | 2.6 (1.1 – 6.5) | |
|
| |||||||
| Provider for Family | No | 15 (47) | 113 (66) | Ref | - | - | - |
| Yes | 17 (53) | 59 (34) | 4.6 (1.1 – 19.6) | ||||
|
| |||||||
| Caste | Bahun | 13 (41) | 58 (340 | Ref | - | - | - |
| Chhetri | 13 (41) | 35 (20) | 2.6 (0.8 – 8.3) | ||||
| Dalit | 3 (9) | 10 (6) | 0.4 (0.1 – 2.4) | ||||
| Janajati | 3 (9) | 61 (35) | 0.1 (0.02 – 0.8) | ||||
| Other | 0 | 8 (5) | - | ||||
Adjusted for state of residence and age. All other demographic variables were not retained in the final model (Religion, N children, Health insurance, Education, English, Employed, N in household, Time in United States, and Marital Status)
Adjusted for state of residence, age and provider of family. All other demographic variables were not retained in the final model (Caste, Religion, N children, Health insurance, Education, English, Employed, N in household, Time in United States, and Marital Status)
Post migration difficulties associated with depression
Post migration difficulties were summarized into five principal components, i.e., indices: 1) general problems with resettlement to the United States, 2) family-related anxiety, 3) problems with religion and/or culture, 4) problems with accessing health resources, and 5) problems with obtaining aid and/or support.
General problems with resettlement in the United States and family-related anxiety were associated with symptoms of depression in both men and women (Table 5). Specific problems contributing to this index had a stronger association with depression, including the inability to pay living expenses (men OR=4.1, women OR=4.5) and a lack of choice over future (men OR=3.6, women OR=5.5). A higher score for family-related anxiety increased the odds for symptoms of depression for both sexes. Specifically, worrying about family back home was the index variable that had the strongest association with symptoms of depression.
Table V.
Post migration problems associated with symptoms of depression in Bhutanese refugees, Arizona, Georgia, New York, and Texas, 2012
|
Men (n=199)
|
Women (n=176)
|
||||||
|---|---|---|---|---|---|---|---|
| Post migration problem | Depressed | Not depressed | aOR (95%) | Depressed | Not depressed | aOR (95%) | |
| Resettlement to United States | Median | 4.40 | 2.65 | 1.8 (1.2 – 2.7)a | 4.41 | 2.82 | 1.8 (1.3 – 2.4)b |
| Range | 0.91-6.32 | 0-7.00 | 1.40-6.82 | 0.28-6.87 | |||
|
| |||||||
| Language barriers | A lot | - | - | - | 42 (88) | 81 (60) | 3.1 (1.1 – 8.6)c |
| No/A little | - | - | - | 6 (12) | 53 (40) | Ref | |
|
| |||||||
| Inability to pay living expenses | A lot | 16 (50) | 32 (19) | 4.1 (1.8 – 9.5)c | 23 (48) | 22 (16) | 4.5 (2.0 – 10.2)c |
| No/A little | 16 (50 | 140 (81) | Ref | 25 (52) | 112 (84) | Ref | |
|
| |||||||
| Lack of choice over future | A lot | 24 (75) | 66 (38) | 3.6 (1.5 – 8.8)c | 38 (79) | 51 (38) | 5.5 (2.4 – 12.4)c |
| No/A little | 8 (25) | 106 (62) | Ref | 10 (21) | 83 (62) | Ref | |
|
| |||||||
| Family-related anxiety | Median | 1.51 | 1.08 | 1.4 (1.1 – 2.0)a | 1.40 | 1.16 | 1.4 (1.1 – 1.8)b |
| Range | 0.21-7.00 | 0.27-6.72 | 0.30-6.76 | 0-6.92 | |||
|
| |||||||
| Worries about family back at home | A lot | 19 (59) | 47 (27) | 3.9 (1.7 – 9.1)c | 36 (75) | 49 (37) | 5.0 (2.3 – 11.0)c |
| No/A little | 13 (41) | 125 (73) | Ref | 12 (25) | 85 (63) | Ref | |
|
| |||||||
| Religion/culture | Median | 3.33 | 1.20 | 1.5 (1.1 – 2.1)a | - | - | - |
| Range | 0.38-7.00 | 0.10-6.63 | - | - | - | ||
|
| |||||||
|
Lack of community structures
for resolving family disputes |
A lot | 9 (28) | 7 (4) | 5.8 (1.8 – 18.5)c | - | - | - |
| No/A little | 23 (72) | 165 (96) | Ref | - | - | - | |
|
| |||||||
|
Difficulty maintaining cultural
and religious traditions |
A lot | 17 (53) | 31 (18) | 3.9 (1.6 – 9.1)c | - | - | - |
| No/A little | 15 (47) | 141 (82) | Ref | - | - | - | |
Only the indices that remained in the final model and significant individual variables are presented in the table
Adjusted for state of residence, age, provider for family, general health, caste and Nepali literacy.
Adjusted for state of residence, age, provider for family, general health and Nepali literacy.
Adjusted for state of residence and age
In men only, a higher score for problems with religion and/or culture increased the odds of experiencing symptoms of depression. Specific problems relating to the lack of community structures for resolving family disputes (OR=5.8) and difficulty maintaining cultural and religious traditions (OR=3.9) had the strongest association with symptoms of depression (Table 5).
Coping mechanisms associated with depression
Coping mechanisms were also summarized into five principal components, i.e., indices, including 1) withdrawal, 2) turning to friends or self-focused problem solving, 3) entertainment or leisure activities, 4) religion and/or culture, and 5) community support.
Of the five indices, use of withdrawal as a coping mechanism was associated with experiencing symptoms of depression for both sexes (Table 6). Of specific variables for withdrawal coping mechanisms, avoiding being with people had the strongest association with experiencing symptoms of depression in men (OR=2.6). In women, “wishing that people would just leave you alone” had the strongest association with experiencing symptoms of depression (OR=4.8).
Table VI. Coping mechanisms associated with symptoms of depression in Bhutanese refugees, Arizona, Georgia, New York, and Texas, 2012
|
Men (n=194)
|
Women (n=174)
|
||||||
|---|---|---|---|---|---|---|---|
| Coping mechanisma | Depressed | Not depressed | aOR (95%) | Depressed | Not depressed | aOR (95%) | |
| Withdrawal | Median | 2.48 | 2.21 | 1.4 (1.0 – 2.0)b | 2.65 | 1.57 | 1.4 (1.1 – 1.8)c |
| Range | 0.11 – 6.61 | 0.35 – 7.00 | 0.54 – 6.79 | 0.09 – 7.00 | |||
|
| |||||||
| Avoided being with people in general | No/A little | 26 (81) | 157 (91) | Ref | - | - | - |
| A lot | 6 (19) | 15 (9) | 2.6 (1.0 – 7.8)d | - | - | - | |
|
| |||||||
|
Wished that people would
just leave you alone |
No/A little | - | - | - | 41 (85) | 129 (96) | Ref |
| A lot | - | - | - | 7 (15) | 5 (4) | 4.8 (1.3 – 17.5)d | |
Only the indices that remained in the final model, and significant individual variables are presented in the table
Phrases regarding coping are derived from the Amirkahn coping scale [22]. Additional culture-specific coping questions were added based on the qualitative assessment during focus group
Adjusted for state of residence, age, provider for family, general health, ethnicity, and Nepali literacy
Adjusted for state of residence, age, provider for family, general health, and Nepali literacy
Adjusted for state of residence and age
Discussion
The prevalence of depression symptoms among resettled Bhutanese refugees (21%) was higher than the 5% reported in a meta-analysis of large studies of refugees resettled to western countries [5]. Prevalence of depression and anxiety was higher among women than men, which is consistent with previous studies in other refugee groups[15], new immigrants[16], and the general population [17]. A significant percentage of Bhutanese refugees had overlapping symptoms of mental health conditions, consistent with other studies shown high mental health comorbidities in the refugee population, with up to 71% of those diagnosed with depression also having a diagnosis of PTSD [5]. This finding is pertinent to the clinical diagnosis of mental health conditions, as those diagnosed with one mental health condition may be at risk for others. Additionally, depression with another mental health comorbidity increases the risk of suicide [18]. Only 4% of participants reported having been previously diagnosed with a mental health condition, though the investigation identified a much higher prevalence of potentially symptomatic persons, suggesting under-diagnosis in this population. Additionally, refugees with suicidal ideation had significantly higher odds of depression, which is expected, as a high percentage of suicides are directly associated with mental health conditions, especially depression [8] [18] [19]. Experiences prior to resettlement may affect the risk of depression in this population, as our study further supports the well-documented evidence showing a dose-effect relationship between cumulative trauma and psychiatric disorders [20] [21]. Further, experiencing more traumatic events is associated with an increase in nonspecific psychiatric disorders, a decrease in social functioning, and an increase in the prevalence of PTSD symptoms [22]. Previous literature has shown refugees with a PTSD diagnosis have a significantly higher rate of suicidal behavior and refugees with a PTSD diagnosis with comorbid depression report a higher frequency of suicidal thoughts [19]
Self-reported poor health was associated with depression, which could be evidence of somatization, defined as the expression of psychological or social distress through physical symptoms. Culture affects an individual’s tendency to somatize depression. In particular, people from nonwestern countries, where it is less culturally acceptable to express psychological distress verbally, often somatize depression [23]. Possible somatization of mental health conditions has been documented previously in the Bhutanese population [24]. However, self-reported poor health does not necessarily represent physical symptoms, and a cause-and-effect relationship is difficult to establish due to the methodology of this study, as the stress of poor health itself may lead to depression.
Depression and suicidal inclination have complex etiologies that in the case of refugees are compounded by a history of trauma and cultural disruption [18]. This makes identification of modifiable risk factors for suicide prevention in the Bhutanese refugee population very difficult. Principal component analysis revealed clusters of problems experienced during post-migration that in varying combinations can additively contribute to depression risk. Cultural isolation resulting from difficulty integrating into a new community after resettlement can affect the risk of depression in the Bhutanese refugee population. Language barriers, especially barriers relating to the ability to read and write Nepali, may led to a feelings of isolation, as they are not able to engage with other refugees in their native language. Difficulty maintaining cultural and religious practices can lead to isolation as refugees have no sense of community or lack the familiarity and personal identity that are associated with cultural and religious practices. Acculturation, where a minority culture assimilates to a majority culture, is common in refugee populations [25] and has been shown to increase risk of depression [26]. Adult refugees may feel as if they are losing their cultural identify post-migration and feel isolated from younger refugees who have assimilated to the resettled culture [25]. This sense of isolation may be compounded in individuals that use withdrawal as a coping mechanism during times of stress. Bhutanese refugees who reported using withdrawal as a coping mechanism, effectively isolating themselves from potential for connection to the resettlement community, were at significant risk for depression in the current study.
Financial responsibility and family obligations related to resettlement may impact the risk of depression in Bhutanese refugees. Men who considered themselves a provider for their household, regardless of their ability to provide through current employment, were more likely to report depression. Inversely, not being a provider of the family has been associated with suicidal ideation in members of the resettled Bhutanese community in the United States [27]. This finding perhaps indicates that those who are providers feel a responsibility towards their family; while this burden can lead to depression, it does not lead to suicidal ideation, potentially due to feelings of obligation and connection to family. Those who are not providers are more inclined to experience suicidal ideation, as they may feel their contributions are less valued or needed, and they are a burden upon their family.
Limitations
Mental health conditions are inherently difficult to research due to the sensitivity of the topic; therefore, symptoms and mental health conditions were likely underreported. Additionally, because we did not perform structured clinical interviews, the extent to which self-reported symptoms of depression would match clinical diagnosis is unclear. A cumulative depression score ≥1.75 is suggestive of the symptoms of depression, but health care provider must determine if the criteria for a clinical diagnosis of depression are met. However, the HSCL-25 is a widely used and validated screening tool for measuring symptoms of depression and anxiety in refugees [12].
Additionally, due to the cross-sectional methodology of this study, we cannot assume causal relationships with the risk factors for depression. The results of this investigation are not generalizable to other Bhutanese or refugee populations, but can be considered as descriptive factors that are associated with symptoms of depression in Bhutanese refugees in the four study states.
Clinical Implications
A combination of prior trauma and current stressors related to post-migration, in particular cultural isolation, financial stressors and disruption of family life lead to increased risk of depression and suicidal ideation in this population. These conclusions emphasize the need for a domestic mental health screening for refugees, using a tool specifically tailored for the refugee population. Currently, a mental health screening is recommended but not standard [28]. A mental health screening after resettlement could also be beneficial in this population, as a significant portion of refugees can have delayed onset of emotional distress [29].Onset of reportedly poor health or physical symptoms could be an indication for administering a mental health screening for refugees months or years after resettlement.
Evidence of a dose-effect relationship between cumulative trauma events and depression, emphasizes the need for mental health services and interventions that are tailored to specific refugee populations based on their experiences prior to resettlement. Utilization of social support from both the refugee and local community [30]and through social media networks [31] are effective coping strategies for mitigating mental health impacts in resettled refugee populations. Notably, while the current study did not ask about social media use as a coping strategy, researchers anecdotally reported a high connectivity in resettled Bhutanese communities across the United States through social media. Such connectivity can be an effective coping mechanism, but it was also observed to aid in the rapid spread of news of recent suicides, increasing the potential for a contagion effect that could pose a risk for suicidal behavior in other high risk refugees [32]. Thus priority should be placed on successful integration of refugees into the community through a variety of social connections and not just social media. Providing opportunities for education and employment may boost community integration, and may also reduce the burden of depression, as Bhutanese who felt they lacked choices for their future were also at risk for depression.
Engagement in religious practices or traditional ceremonies have been shown to reduce anxiety and lessen depression symptoms [33] as have efforts to implement biculturalism [25], so efforts to encourage these practices within newly resettled refugee community are important. In general, when addressing post-migration concerns, evidence demonstrates that interventions that address suites of concerns, not just single factors, might be more effective for reaching diverse community members who may be struggling with different problems that lead to the same outcome of isolation and development of associated mental health concerns.
Clinicians should be aware of persons within the Bhutanese refugee community with the risk factors outlined above, as well as the high burden of mental health co-morbidities in this population. In particular, physicians treating physical ailments in this population should be aware of the potential for somatization of mental health symptoms and may wish to consider the possibility of depression or other mental health concerns in persons with chronic physical symptoms that have been difficult to diagnose or alleviate. Concomitantly, more resources need to be invested in this area, as current programs have limited capacity to provide the necessary culturally appropriate mental health services.
New Contribution to the Literature
Depression is prevalent among Bhutanese refugees in the United States and is associated with general problems with resettlement, such as providing for a family and finding work, family-related anxiety, and using withdrawal as a coping mechanism. Health care providers should be aware of mental health concerns and risk factors in Bhutanese refugees and should work to link those at higher risk to resources for mental health evaluation and appropriate care.
Supplementary Material
Acknowledgments
This study was partially supported in part by an appointment to the Applied Epidemiology Fellowship Program administered by the Council of State and Territorial Epidemiologists (CSTE) and funded by the Centers for Disease Control and Prevention (CDC) Cooperative Agreement U60/CCU007277. We want to express sincere appreciation to the Bhutanese refugee community, community leaders, interviewers and the resettlement agencies and refugee health programs in the cities of the investigation for their vital assistance with this project. Additionally, we would like to acknowledge the following individuals from the US Centers for Disease Control and Prevention for their assistance with this project: Dr. Eboni Taylor, Curtis Blanton and Teri Sivilli.
Footnotes
Authors report no conflicts of interest.
All authors have reviewed the submitted manuscript and approve the manuscript for submission.
Disclaimer: The findings and conclusions in this report are those of the author(s) and do not necessarily represent the views of the Centers for Disease Control and Prevention.
Adapted from a standard protocol developed by the Injury and Prevention Branch, CDC
References
- 1.Marcus M, et al. Depression: A Global Public Health Concern. WHO; 2012. [Google Scholar]
- 2.Gotlib IH, Hammen CL, editors. Handbook of Depression. Second The Guilford Press; 2010. [Google Scholar]
- 3.Lopes Cardozo B, et al. Karenni refugees living in Thai-Burmese border camps: traumatic experiences, mental health outcomes, and social functioning. Elsevier. 2004;58:2637–2644. doi: 10.1016/j.socscimed.2003.09.024. [DOI] [PubMed] [Google Scholar]
- 4.Mollica RF, et al. The Effect of Trauma and Confinement on Functional Health and Mental Health Status of Cambodians Living in Thailand0Cambodia Border Camps. JAMA. 1993;270(5):581–586. [PubMed] [Google Scholar]
- 5.Fazel M, Wheeler J, Danesh J. Prevalence of serious mental disorder in 7000 refugees resettled in western countries: a systematic review. Lancet. 2005;365:1309–1314. doi: 10.1016/S0140-6736(05)61027-6. [DOI] [PubMed] [Google Scholar]
- 6.WRITENET The Exodus of Ethnic Nepalis from Southern Bhutan. 1995 Apr 1; [Google Scholar]
- 7.Worldwide Refugee Admission Processing System (WRAPS) [Google Scholar]
- 8.IOM Who Am I? Assessment of Psychological Needs and Suicide Risk Factors among Bhutanese Refugees in Nepal and after Third Country Resettlement. 2011.
- 9.Laban CJ, et al. Postmigration living problems and common psychiatric disorders in Iraqi asylum seekers in the Netherlands. The Journal of Nervous and Mental Disease. 2005;193(12):825–832. doi: 10.1097/01.nmd.0000188977.44657.1d. [DOI] [PubMed] [Google Scholar]
- 10.Cutrona C. Ratings of social support by adolescents and adult informants: degree of correspondence and prediction of depressive symptoms. Journal of Personality and Social Psychology. 1989;57(4):723–730. doi: 10.1037//0022-3514.57.4.723. [DOI] [PubMed] [Google Scholar]
- 11.Amirkhan JH. A factor analytically derived measure of coping: The Coping Strategy Indicator. Journal of Personality and Social Psychology. 1990;59(5):1066–1074. [Google Scholar]
- 12.Mollica R, et al. Indochinese versions of the Hopkins Symptom Checklist-25: A screening instrument for psychiatric care of refugees. American Journal of Psychiatry. 1987;144(4):497–500. doi: 10.1176/ajp.144.4.497. [DOI] [PubMed] [Google Scholar]
- 13.Mollica RF, et al. The Harvard Trauma Questionnaire. Validating a cross-cultural instrument for measuring torture, trauma, and posttraumatic stress disorder in Indochinese refugees. J Nerv Ment Dis. 1992;180(2):111–6. [PubMed] [Google Scholar]
- 14.Principle Component Analysis. SAS/IML (R) Studio 12.3 User's Guide. Available from: http://support.sas.com/publishing/pubcat/chaps/55129.pdf.
- 15.Sabin M, et al. Factors associated with poor mental health among Guatemalan refugees living in Mexico 20 years after civil conflict. JAMA. 2003;290(5):635–642. doi: 10.1001/jama.290.5.635. [DOI] [PubMed] [Google Scholar]
- 16.Wong E, Miles JV. Prevalence and Correlates of Depression Among New U.S. Immigrants. Journal of Immigrant and Minority Health. 2013:1–7. doi: 10.1007/s10903-013-9781-0. [DOI] [PubMed] [Google Scholar]
- 17.Desai H, Jann M. Major Depression in Women: A Review of the Literature. Journal of the American Pharmacists Association. 2000;40(4) [PubMed] [Google Scholar]
- 18.Vijayakumar L, Jotheeswaran AT. Mental Health of Refugees and Asylum Seekers. Oxford University Press; New York: 2010. Suicide in refugees and asylum seekers; pp. 195–2011. [Google Scholar]
- 19.Ferrada-Noli M, et al. Suicidal behavior after severe trauma. Part 1: PTSD diagnoses, psychiatric comorbidity, and assessments of suicidal behavior. Journal of Traumatic Stress. 1998;11(1):103–112. doi: 10.1023/A:1024461216994. [DOI] [PubMed] [Google Scholar]
- 20.Husain F, et al. Prevalence of War-Related Mental Health Conditions and Association With Displacement Status in Postwar Jaffna District, Sri Lanka. JAMA. 2011;306(5):522–531. doi: 10.1001/jama.2011.1052. [DOI] [PubMed] [Google Scholar]
- 21.Mollica R, et al. The Dose-Effect Relationships between Torture and Psychiatric Symptoms in Vietnamese Ex-Political Detainees and a Comparison Group. The Journal of Nervous and Mental Disease. 1998;186(9):543–553. doi: 10.1097/00005053-199809000-00005. [DOI] [PubMed] [Google Scholar]
- 22.Cardozo B, et al. Mental health, social functioning, and attitudes of kosovar albanians following the war in kosovo. JAMA. 2000;284(5):569–577. doi: 10.1001/jama.284.5.569. [DOI] [PubMed] [Google Scholar]
- 23.Katon W, Kleinman A, Rosen G. Depression and Somatization: a review. The American Journal of Medicine. 1982;72(1):127–135. doi: 10.1016/0002-9343(82)90599-x. [DOI] [PubMed] [Google Scholar]
- 24.Ommeren MV, et al. Trauma and loss as determinants of medically unexplained epidemic illness in a Bhutanese refugee camp. Psychological Medicine. 2001;31:1259–1267. doi: 10.1017/s0033291701004470. [DOI] [PubMed] [Google Scholar]
- 25.Pumariega A, Rothe E, Pumariega J. Mental Health of Immigrants and Refugees. Community Mental Health Journal. 2005;41(5):581–597. doi: 10.1007/s10597-005-6363-1. [DOI] [PubMed] [Google Scholar]
- 26.Bhugra D. Migration and depression. Acta Psychiatrica Scandinavica. 2003;108(s418):67–72. doi: 10.1034/j.1600-0447.108.s418.14.x. [DOI] [PubMed] [Google Scholar]
- 27.Ao T. Suicide and Suicide Ideation Among Bhutanese Refugees - United States, 2009-2012. MMWR. 2013;62(26):533–536. [PMC free article] [PubMed] [Google Scholar]
- 28.CDC Immigrant and Refugee Health Branch Guidelines for Mental Health Screening during the Domestic Medical Examination for Newly Arrived Refugees. 2012 Mar 29; [Google Scholar]
- 29.Pathways to Wellness The Refugee Health Screener-15 (RHS-15) Packet. 2011 http://refugeehealthta.org/webinars/mental-health-screening-and-care/tools-and-strategies-for-refugee-mental-health-screening-introducing-the-rhs-15-2/
- 30.Muhwezi WW, Sam DL. Adaptation of urban refugees in Uganda: a study of their socio-cultural and psychological well being in Kampala City. Journal of Psychology in Africa. 2004;14(1):37–46. [Google Scholar]
- 31.Willems R. Coping with displacement: Social networking among urban refugees in an east African context. 2005. status: published.
- 32.Ao T, et al. An Investigation into Suicides among Bhutanese Refugees in the US 2009-2012. 2012. [DOI] [PMC free article] [PubMed]
- 33.Cardozo B, et al. Mental health, social functioning, and disability in postwar Afghanistan. JAMA. 2004;292(5):575–584. doi: 10.1001/jama.292.5.575. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


