Abstract
Aims
Anticholinergic drug exposure is associated with adverse outcomes in older people. While a number of tools have been developed to measure anticholinergic drug exposure, there is limited information about the agreement and overlap between the various scales. The aim of this study was to investigate the agreement and overlap between different measures of anticholinergic drug exposure in a cohort of community-dwelling older men.
Methods
A cross-sectional study was used to compare anticholinergic drug exposure calculated using the Anticholinergic Risk Scale (ARS), the Anticholinergic Drug Scale (ADS), the Anticholinergic Cognitive Burden (ACB) and the Drug Burden Index anticholinergic subscale (DBI-ACH) in a cohort of community-dwelling men aged 70 years and older (n = 1696). Statistical agreement, expressed as Cohen's kappa (κ), between these measurements was calculated.
Results
Differences were found between the tools regarding the classification of anticholinergic drug exposure for individual participants. Thirteen percent of the population used a drug listed as anticholinergic on the ARS, 39% used a drug listed on the ADS and the ACB, and 18% of the population used one or more anticholinergic drugs listed on the DBI-ACH. While agreement was good between the ACB and ADS (κ = 0.628, 95% CI 0.593, 0.664), little agreement was found between remaining tools (κ = 0.091–0.264).
Conclusions
With the exception of the ACB and ADS, there was poor agreement regarding anticholinergic drug exposure among the four tools compared in this study. Great care should be taken when interpreting anticholinergic drug exposure using existing scales due to the wide variability between the different scales.
Keywords: anticholinergic burden, anticholinergic drug exposure, drug utilization, methodology, older people
What is Already Known about this Subject
The use of anticholinergic drugs is associated with an increased risk of adverse events, especially in older people.
Several tools have been developed to assess the impact of anticholinergic drug exposure on different clinical outcomes.
Differences between these tools are profound and knowledge regarding the relationship between different anticholinergic drug exposure scales is essential if these tools are to be clinically implemented.
What this Study Adds
There is poor agreement regarding anticholinergic drug exposure among existing tools.
Great care should be taken when interpreting and comparing anticholinergic drug exposure using these scales due to the wide variability of drugs included.
Introduction
There is increasing awareness of the risks of using medicines with anticholinergic effects in older people. Anticholinergic agents may be used therapeutically in the treatment of respiratory disease, urge incontinence and Parkinson's disease 1. However, in most cases, anticholinergic effects are unwanted and associated with considerable harm. Commonly reported anticholinergic adverse effects include constipation, urinary retention, heat intolerance, dry eyes, dry mouth, tachycardia, impaired cognition, agitation, paranoia and delirium, all of which may have a significant burden on the individual 2,3. This has led to increased interest in being able to estimate anticholinergic drug exposure for individual patients to predict the risk of adverse effects and guide treatment decisions.
A number of methods have been developed to quantify anticholinergic drug exposure for an individual 4–9. A 2013 review of tools for assessing anticholinergic drug exposure identified seven tools encompassing 225 therapeutic substances that were in use for measuring anticholinergic drug exposure 10. Looking at those scales used to assess anticholinergic drug exposure in the literature which have been associated with clinically important outcomes, four main scales should be considered. These are the Anticholinergic Risk Scale (ARS) 4, the Anticholinergic Drug scale (ADS) 6, the Anticholinergic Cognitive Burden scale (ACB) 7 and the anticholinergic subscale (DBI-ACH) from the Drug Burden Index (DBI) 8.
Each of the four scales identified above has been associated with significant clinical outcomes in older persons. Across the scales, increasing anticholinergic drug exposure has been found associated with falls 9, poorer cognitive function 7,8,11,12, increased adverse effects 6, functional decline 11,13,14, institutionalization 15 and increased mortality 16. However different associations have been reported for each scale. For example associations between increasing burden and mortality were reported for the ACB 16 and, increasing exposure measured by the DBI-ACH but not the ARS, was associated with poorer functional status 13. Yet similar studies showed no association between anticholinergic drug exposure and mortality measured via the ARS 11 or the DBI 8. Despite these indications that differences exist between the scales, there is limited information about the overlap and agreement between the different anticholinergic scales.
Profound differences exist between different tools for determining anticholinergic drug exposure regarding the medicines included and assignment of anticholinergic scores to individual drugs. Studies comparing the different scales have highlighted this 17–19. A Spanish study comparing the results of the ADS, ARS and ACB in a small sample of 83 psychiatric inpatients aged 65 years and older found that overall agreement was poor among all three scales 17. A large Italian study reported difference between the ACB and ARS in terms of their relationships with functional outcomes 18. Similar results were also reported in a recent Canadian study which concluded that different methods for defining drug exposure will have a significant effect on the results of pharmacoepidemiological studies in terms of capturing drug exposure and impact on outcomes 19.
Given the impact of anticholinergic effects on older persons, knowledge regarding the relationship between different anticholinergic drug exposure scales is essential if these tools are to be clinically implemented. The lack of clarity between anticholinergic drug exposure scales makes it difficult for clinicians to measure and interpret changes in anticholinergic drug exposure in daily practice. The aim of this study was to investigate the agreement and overlap between different measures of anticholinergic drug exposure in a large group of community-dwelling older men.
Methods
Study population
Data from the Concord Health and Ageing in Men Project (CHAMP) study were used for this study. In the CHAMP study, community dwelling men aged 70 years and over living in a defined geographical region near a tertiary university teaching hospital in Sydney were recruited and were followed in a longitudinal cohort. Eligible participants were identified using compulsory electoral roll registration and were invited to participate in the CHAMP study. Details on the CHAMP cohort profile and study design have been published elsewhere 20. In this study, baseline data from 1696 participants with complete medication use data in 2005–2007 were used. The CHAMP study was approved by the Concord Hospital Human Research Ethics Committee. All participants gave written informed consent.
Medication use
CHAMP participants were instructed to bring all prescription and non-prescription medicines to each clinic visit. At the visit, they were also asked if they had taken any medicines, either prescribed by a doctor or obtained over-the-counter, during the past month. Medication information including name, dose, frequency and duration was collected. The Iowa Drug Information Service (IDIS) drug codes were used to classify the medication data and medicines were categorized on the most detailed level of classification 21. Participants were excluded from analyses if medication use data was unknown (n = 9).
Anticholinergic drug exposure scales
To determine the ARS experts ranked the anticholinergic effects of 500 commonly prescribed drugs from 0 (no or low anticholinergic potential) to 3 (high anticholinergic potential) 4. Using the ARS, each medication is scored according to its potential anticholinergic effect and like the ABS, the total anticholinergic drug exposure for an individual according to the ARS is the sum of scores for all medicines.
The ADS ranks the anticholinergic effects of medicines with a score between 0 and 3 6. A score of 0 is given to medicines with no known anticholinergic activity, medicines that have potential anticholinergic effects based on receptor binding studies score 1, medicines with reported anticholinergic adverse events, usually at excessive doses, score 2 and medicines with profound anticholinergic properties score 3. Again, each individuals' score is the sum of the individual medication rankings.
Using the ACB scale, medicines with possible anticholinergic effects, defined as those with serum anticholinergic activity or in vitro affinity for muscarinic receptors, but with no known clinically relevant adverse cognitive effects are given score 1 7. Score 2 or 3 is assigned to medicines with established and clinically relevant cognitive anticholinergic effects. Scores are summed per individual.
The DBI was developed to measure exposure to anticholinergic and sedative drugs taking into account the daily dose 8. The DBI comprises two subscales, the DBI-ACH measures anticholinergic effects while the DBI-S assesses sedative effects. Increases in DBI have been associated with poorer physical performance 8, increased functional decline 22 and falls 23. In this study we have used the DBI-ACH subscale since our primary aim was to compare scales measuring anticholinergic drug exposure 22. To calculate the DBI-ACH an anticholinergic activity value is assigned to each medication based on the Australian Approved Product Information.
For each participant, the DBI-ACH was calculated using the following formula:
where D is the dose of an anticholinergic medicine that a person is receiving and δ is the minimum recommended daily dose according to the Australian Approved Product Information 8. Where the drug dose was unknown for calculating the DBI-ACH for an individual the median value of all users within the study population was used.
Anticholinergic drug exposure
Anticholinergic drug exposure was calculated for each participant using each of the scales. Each scale was calculated according to published methods 4,6–8. For the ARS, ADS and ACB the lists of medicines with their specified anticholinergic activity specified in the relevant publications were used 4,6,7. The ARS included a total of 49 medicines, the ADS 117 and the ACB 79. In the CHAMP cohort 46 medicines were considered to have anticholinergic activity according to Australian Approved Product Information.
For each scale we determined the number of anticholinergic drugs prescribed for participants of our study population as a percentage of the total number of anticholinergic drugs included in the scale. Drugs prescribed as pro re nata (prn) or as needed were excluded from the analysis and drugs not specifically included in a scale were assigned a score of 0 in the relevant calculation. Oral, inhaled and ocular anticholinergic medicines were all included in the DBI-ACH calculations but only oral medicines were included as having anticholinergic activity in the other scales 4,6–8.
Anticholinergic load is often classified categorically, and in this work anticholinergic exposure was classified into no, low and high burden using previously published cut-off points where possible 4,8,24. For the ACB and ARS individuals were categorized into no (score = 0), low (score = 1-2) and high (>3) categories 4,24. No published classification for the ACB was found so cut-off levels consistent to the ARS and ADS were used. For each drug, DBI-ACH ranges from 0–1, with 0.5 indicating that an individual is exposed to an anticholinergic medication at the minimum recommended daily dose. Using the DBI-ACH, high anticholinergic exposure was classified as ≥1 and a low anticholinergic exposure classified as <1 8,22.
Statistical analysis
As there is no gold standard for the measurement of anticholinergic drug exposure, agreement between categories on the different scales was determined using Cohen's kappa (κ). κ values less than 0.61 were considered to represent poor agreement between the scales, values between 0.61 and 0.80 good agreement and κ values over 0.80 very good agreement 25. Statistical analyses were performed with IBM SPSS® statistical software version 22.
Results
Study population
A total of 1696 men, aged between 70 to 97 years, were included in the study.
The mean age of participants at baseline was 76.9 (±5.5) years. Over 90% of participants (92.2%) in the study were using at least one medication on a regular basis and they used a mean of 4.9 regular medicines (±2.9). Participants were relatively robust, reflecting their community-dwelling status, with a mean of 2.5 (±1.8) comorbidities. Just under half the cohort (46.9%) were using at least one medication listed on any of the anticholinergic scales included in this analysis.
Comparison of anticholinergic drug exposure scales
While there was some overlap between the scales in terms of the medicines included, there were marked differences in the drugs defined as having anticholinergic action for each scale (Figure1). Ten medicines were included on all four scales (amitriptyline, atropine, cyproheptadine, imipramine, nortriptyline, olanzapine, oxybutynin, promethazine, thioridazine and trifluoperazine). Twenty-seven medicines were found on three of the anticholinergic scales, 46 on two scales while 78 medicines only appeared in a single anticholinergic scale.
Figure 1.
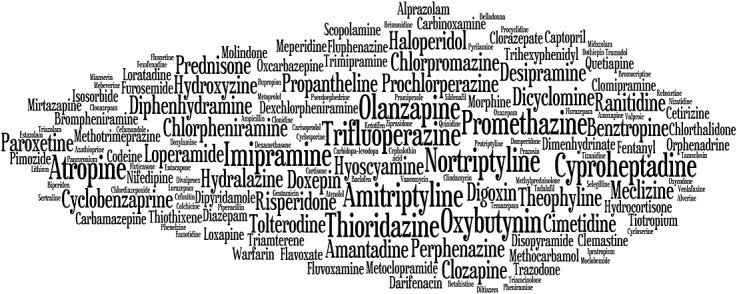
Overlap between medicines included in the different anticholinergic scales. The larger the generic name, the more scales that the medication appears on. (Figure created with wordle http://www.wordle.net/)
The ADS contains 117 drugs of which 57 were used in the CHAMP population, with 39% of men taking at least one of these drugs. The ARS contains 49 drugs of which 28 were used in the population. Thirteen percent of the population used a drug listed as anticholinergic on the ARS, 39% used a drug listed on the ADS and the ACB and 18% of the population used one or more anticholinergic medicines included in the DBI-ACH
Classification of anticholinergic drug exposure
Results differed between the scales. However, the majority of participants in the study were classified as having ‘no’ anticholinergic drug exposure. Differences were observed between the scales in the proportions of individuals classified at each level (Table1). Less than 50% of participants were classified to the same burden category by all scales (Table2). Looking at the agreement between pairs of scales, good agreement was observed between ACB and ADS (κ = 0.628, 95% CI 0.593, 0.664). However agreement between all other scales was poor (Table3).
Table 1.
Distribution of participants (n = 1696) according to degree of anticholinergic drug exposure for each scale
| Number of participants per anticholinergic drug exposure group (percentage of population) | |||
|---|---|---|---|
| No | Low | High | |
| Anticholinergic Risk Scale (ARS) | 1481 (87%) | 135 (8%) | 80 (5%) |
| Anticholinergic Drug Scale (ADS) | 1034 (61%) | 482 (28%) | 180 (11%) |
| Anticholinergic Cognitive Burden Scale (ACB) | 1033 (61%) | 532 (31%) | 131 (8%) |
| Drug Burden Index-Anticholinergic (DBI-ACH) | 1378 (81%) | 295 (17%) | 23 (1%) |
Table 2.
Percentage of participants (n = 1705) classified to the same level of anticholinergic drug exposure by the different scales
| Anticholinergic drug exposure scales# | Percentage of participants (n = 1705) |
|---|---|
| ACB + ARS + ADS + DBI-ACH | 47.5 |
| ACB + ARS + ADS | 7.3 |
| ACB + ARS + DBI-ACH | 5.6 |
| ACB + ADS + DBI-ACH | 3.7 |
| ARS + ADS + DBI-ACH | 7.0 |
| ACB + ARS | 6.2 |
| ACB + ADS | 17.2 |
| ACB + DBI-ACH | 2.0 |
| ARS + ADS | 1.6 |
| ARS + DBI-ACH | 18.4 |
| ADS + DBI-ACH | 1.2 |
#ACB Anticholinergic Cognitive Burden Scale, ARS Anticholinergic Risk Scale, ADS Anticholinergic Drug Scale, DBI-ACH Drug Burden Index-Anticholinergic.
Note Percentages cannot be totalled to 100% as there may be agreement between two different scale pairs for an individual participant.
Table 3.
Agreement between anticholinergic drug exposure scales (Cohen's κ, 95% confidence interval) in the classification of anticholinergic exposure
| Anticholinergic Risk Scale (ARS) | Anticholinergic Drug Scale (ADS) | AnticholinergicCognitive Burden Scale (ACB) | |
|---|---|---|---|
| Anticholinergic Risk Scale (ARS) | |||
| Anticholinergic Drug Scale (ADS) | 0.263 (0.226, 0.300) | ||
| Anticholinergic Cognitive Burden Scale (ACB) | 0.247 (0.208, 0.286) | 0.628 (0.593, 0.664) | |
| Drug Burden Index -Anticholinergic (DBI-ACH) | 0.237 (0.192, 0.282) | 0.119 (0.084, 0.154) | 0.091 (0.054, 0.128) |
Discussion
In general, the agreement between four scales measuring anticholinergic drug exposure in a group of community dwelling older men was poor. The only scales showing good agreement were the ADS and ACB, which may be explained by the similarity of methods used to determine anticholinergic activity. Both the ADS and ACB assign anticholinergic activity based on receptor binding studies and report clinically relevant anticholinergic adverse events, while the ARS was developed by an expert review of the 500 most prescribed drugs. The lack of agreement between different scales measuring anticholinergic drug exposure confirms earlier findings. The agreement between the ADS and ACB found in this study is in contrast to an earlier Spanish study, which reported poor agreement between these scales 17. However, the earlier study was conducted in a specialized psychiatric hospital rather than in the community setting, where medication use patterns may differ, especially around psychoactive medicines with high anticholinergic activity.
Our study confirms earlier work that the available lists are not interchangeable 17,18. Large differences in the classification of anticholinergic potential of different agents may be one underlying factor accounting for the lack of agreement between the scales. For example, olanzapine has a higher anticholinergic drug exposure score according to the ACB than the ADS. Haloperidol and quetiapine have anticholinergic properties according to the ACB but not according to the ADS. Another difference may be related to the ability to update scales to include newer anticholinergic medicines.
The overall level of anticholinergic load and percentage of participants taking anticholinergic drugs in this study were low compared with other studies 25–27. A study from New Zealand reported 32% use of anticholinergic drugs according to the DBI-ACH and a 53% anticholinergic exposure according to the ADS in a population of older people 26. The difference is most likely due to the fact that medication use in the New Zealand study was determined by analyzing dispensed drugs in a period of 1 year, whereas in the CHAMP population drug use was based on information from a single clinical visit. A US study showed that 48% of the community-dwelling study population was exposed to high (≥3) anticholinergic exposure according to the ACB 27. Another North American study in an African American population reported 57% of participants used anticholinergics as determined by the ACB 25. In both North American studies, different methods of determining medication use is most likely the reason that a higher anticholinergic exposure was found in comparison with the current work.
It seems unlikely that cumulative exposure to anticholinergic drugs can be simplified into linear additive models such as those currently used to classify anticholinergic drug exposure. Anticholinergic effects are dose-dependent and anticholinergic activity is unlikely to be proportional to a 0: 1: 2: 3 ratio 10. Furthermore no relationship between serum anticholinergic concentrations and anticholinergic effects has been found, further supporting the complexity of this relationship 28–30.
This study had a number of limitations. Anticholinergic drug exposure was classified as no, low or high for each participant. Cut-offs in this work for the ADS, ARS 4,23 and DBI-ACH 8,21 were based on previously published studies. However, no published values were available for the ACB. More research is needed to find clinically valid cut-off points. We have compared various anticholinergic drug exposure scales in a large population of community-dwelling older men, but results may not be generalizable to other study populations, such as institutionalized individuals or community dwelling women. A major strength of the study was the collection of medication use information. Medication use in this cohort was determined by asking participants to bring all prescription and non-prescription drugs to the study centre, allowing capture of all medicines currently used by each participant.
In conclusion, this study found differences and generally poor agreement among four tools for measuring anticholinergic drug exposure. Marked variation in the drugs included in each scale as well as the anticholinergic potential of different drugs contributed greatly to the lack of agreement. Use of existing scales in clinical practice remains challenging due to complexity in both calculating anticholinergic exposure, ability to consistently update the scales as well as in relating differences in anticholinergic exposure to clinically significant outcomes such as adverse effects.
Conflict of Interests
All authors have completed the Unified Competing Interest form at www.icmje.org/coi_disclosure.pdf (available on request from the corresponding author) and declare no support from any organization for the submitted work, no financial relationships with any organizations that might have an interest in the submitted work in the previous 3 years and no other relationships or activities that could appear to have influenced the submitted work.
The CHAMP study is funded by the Australian National Health and Medical Research Council (NHMRC Project Grant No. 301916), Sydney Medical School Foundation and Aging and Alzheimer's Research Foundation. Danijela Gnjidic is supported by a National Health and Medical Research Early Career Fellowship. Andrew McLachlan is the Programme Director of the NHMRC Centre for Research Excellence on Medicines and Ageing.
Contributors
LP and JN contributed equally to this work.
All authors meet the criteria for authorship stated in the Uniform Requirements for Manuscripts Submitted to Biomedical Journals. LP, KT, JN, LC and AM contributed to the conception and design of the study. RC, LC, AM contributed to the acquisition of data. LP, JN and DG contributed to analysis of data. All authors contributed to the interpretation of data LP and JN drafted the manuscript and all authors contributed intellectual content in revising the article. All authors give final approval of the version to be submitted and any revised version.
References
- Gerretsen P, Pollock BG. Drugs with anticholinergic properties: a current perspective on use and safety. Expert Opin Drug Saf. 2011;10:751–65. doi: 10.1517/14740338.2011.579899. [DOI] [PubMed] [Google Scholar]
- Peters NL. Snipping the thread of life: antimuscarinic side effects of medication in the elderly. Arch Intern Med. 1989;149:2414–20. [PubMed] [Google Scholar]
- Shiloh R, Stryjer R, Weizman A, Nutt DJ. Atlas of Psychiatric Pharmacotherapy. London: Martin Dunitz; 1999. [Google Scholar]
- Rudolph JL, Salow MJ, Angelini MC, McGlinchey RE. The anticholinergic risk scale and anticholinergic adverse effects in older persons. Arch Intern Med. 2008;168:508–13. doi: 10.1001/archinternmed.2007.106. [DOI] [PubMed] [Google Scholar]
- Han L, McCusker J, Cole M, Abrahamowicz M, Primeau F, Elie M. Use of medications with anticholinergic effect predicts clinical severity of delirium symptoms in older medical inpatients. Arch Intern Med. 2001;161:1099–105. doi: 10.1001/archinte.161.8.1099. [DOI] [PubMed] [Google Scholar]
- Carnahan RM, Lund BC, Perry PJ, Pollock BG, Culp KR. The anticholinergic drug scale as a measure of drug-related anticholinergic burden: Associations with serum anticholinergic activity. J Clin Pharmacol. 2006;46:1481–6. doi: 10.1177/0091270006292126. [DOI] [PubMed] [Google Scholar]
- Boustani M, Campbell N, Munger S, Maidment I, Fox C. Impact of anticholinergics on the aging brain: a review and practical application. Aging Health. 2008;4:311–20. [Google Scholar]
- Hilmer SN, Mager DE, Simonsick EM, Cao Y, Ling SM, Windham BG, Harris TB, Hanlon JT, Rubin SM, Shorr RI, Bauer DC, Abernethy DR. A Drug Burden Index to define the functional burden of medications in older people. Arch Intern Med. 2007;167:781–7. doi: 10.1001/archinte.167.8.781. [DOI] [PubMed] [Google Scholar]
- Aizenberg D, Sigler M, Weizman A, Barak Y. Anticholinergic burden and the risk of falls among elderly psychiatric inpatients: A 4-year case-control study. Int Psychogeriatr. 2002;14:307–10. doi: 10.1017/s1041610202008505. [DOI] [PubMed] [Google Scholar]
- Durán CE, Azermai M, Vander Stichele RH. Systematic review of anticholinergic risk scales in older adults. Eur J Clin Pharmacol. 2013;69:1485–96. doi: 10.1007/s00228-013-1499-3. [DOI] [PubMed] [Google Scholar]
- Kumpula EK, Bell JS, Soini H, Pitkala KH. Anticholinergic drug use and mortality among residents of long-term care facilities: a prospective cohort study. J Clin Pharmacol. 2011;51:256–63. doi: 10.1177/0091270010368410. [DOI] [PubMed] [Google Scholar]
- Bostock CV, Soiza RL, Mangoni AA. Associations between different measures of anticholinergic drug exposure and Barthel Index in older hospitalized patients. Ther Adv Drug Saf. 2013;4:235–45. doi: 10.1177/2042098613500689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koshoedo S, Soiza R, Mangoni A. Anticholinergic drugs and functional outcomes in older patients undergoing orthopedic rehabilitation. Am J Geriatr Pharmacother. 2012;10:251–7. doi: 10.1016/j.amjopharm.2012.06.003. [DOI] [PubMed] [Google Scholar]
- Cai X, Campbell N, Khan B, Callahan C, Boustani M. Long-term anticholinergic use and the aging brain. Alzheimers Dement. 2013;9:377–85. doi: 10.1016/j.jalz.2012.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lowry E, Woodman RJ, Soiza RL, Mangoini AA. Clinical and demographic factors associated with antimuscarinic medication use in older hospitalized patients. Hosp Pract. 2011;39:30–6. doi: 10.3810/hp.2011.02.371. [DOI] [PubMed] [Google Scholar]
- Fox C, Richardson K, Maidment MA, Savva GM, Matthews FE, Smithard D, Coulton S, Katona C, Boustani MA, Brayne C. Anticholinergic medication use and cognitive impairment in the older population: the Medical Research Council Cognitive Function and Ageing Study. J Am Geriatr Soc. 2011;59:1477–83. doi: 10.1111/j.1532-5415.2011.03491.x. [DOI] [PubMed] [Google Scholar]
- Lertxundi U, Domingo-Echaburu S, Hernandex R, Peral J, Medrano J. Expert-based drug lists to measure anticholinergic burden: similar names, different results. Psychogeriatrics. 2013;13:17–24. doi: 10.1111/j.1479-8301.2012.00418.x. [DOI] [PubMed] [Google Scholar]
- Pasina L, Djade CD, Lucca U, Nobili A, Tettamanti M, Franchi C, Salerno F, Corrao S, Marengoni A, Iorio A, Marucci M, Violi F, Mannucci P. Association of anticholinergic burden with cognitive and functional status in a cohort of hospitalized elderly: Comparison of the Anticholinergic Cognitive Burden Scale and Anticholinergic Risk Scale: Results from the REPOSI study. Drugs Aging. 2013;30:103–12. doi: 10.1007/s40266-012-0044-x. [DOI] [PubMed] [Google Scholar]
- Kashyap M, Belleville S, Mulsant BH, Hilmer SN, Paquette A, Tu LM, Tannenbaum C. Methodological challenges in determining longitudinal associations between anticholinergic drug use and incident cognitive decline. J Am Geriatr Soc. 2014;62:336–41. doi: 10.1111/jgs.12632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cumming RG, Handelsman D, Seibel MJ, Creasey H, Sambrook P, Waite L, Naganathan V, Le Couter D, Litchfield M. Cohort profile: The Concord Health and Ageing in Men Project (CHAMP) Int J Epidemiol. 2009;38:374–8. doi: 10.1093/ije/dyn071. [DOI] [PubMed] [Google Scholar]
- Gnjidic D, Cumming RG, Le Couter DJ, Handelsman DJ, Naganathan V, Abernethy DR, Hilmer SN. Drug Burden Index and physical function in older Australian men. Br J Clin Pharmacol. 2009;68:97–105. doi: 10.1111/j.1365-2125.2009.03411.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson NM, Hilmer SN, March LM, Cameron ID, Lord SR, Seibel MJ, Sambrook PN. Associations between Drug Burden Index and falls in older people in residential aged care. J Am Geriatr Soc. 2011;59:875–80. doi: 10.1111/j.1532-5415.2011.03386.x. [DOI] [PubMed] [Google Scholar]
- Gouraud-Tanguy A, Berlioz-Thibal M, Brisseau JM, Ould Aoudia V, Beauchet O, Berrut G, De Decker L. Analysis of iatrogenic risk related to anticholinergic effects using two scales in an acute geriatric inpatient unit. Geriatr Psychol Neuropsychiatr Vieil. 2012;10:27–32. doi: 10.1684/pnv.2012.0337. [DOI] [PubMed] [Google Scholar]
- Altman DG. Practical Statistics for Medical Research. London: Chapman and Hall; 1999. [Google Scholar]
- Campbell NL, Boustani MA, Lane KA, Gao S, Hendrie H, Khan BA, Murrell JR, Unverzagt FW, Hake A, Smith-Gamble V, Hall K. Use of anticholinergics and the risk of cognitive impairment in an African American population. Neurology. 2010;75:152–9. doi: 10.1212/WNL.0b013e3181e7f2ab. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Narayan SW, Hilmer SN, Horsburgh S, Nishtala PS. Anticholinergic component of the Drug Burden Index and the Anticholinergic Drug scale as measures of anticholinergic exposure in older people in New Zealand: a population-level study. Drugs Aging. 2013;30:927–34. doi: 10.1007/s40266-013-0111-y. [DOI] [PubMed] [Google Scholar]
- West T, Pruchnicki MC, Porter K, Emptage R. Evaluation of anticholinergic burden of medications in older adults. J Am Pharm Assoc. 2013;53:496–504. doi: 10.1331/JAPhA.2013.12138. [DOI] [PubMed] [Google Scholar]
- Kersten H, Moilden E, Willumsen T, Engedal K, Wyller TB. Higher anticholinergic drug scale (ADS) scores are associated with peripheral but not cognitive markers of cholinergic blockade. Cross sectional data from 21 Norwegian nursing homes. Br J Clin Pharmacol. 2013;75:842–9. doi: 10.1111/j.1365-2125.2012.04411.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carnahan RM, Lund BC, Perry PJ, Culp KR, Pollock BG. The relationship of an anticholinergic rating scale with serum anticholinergic activity in elderly nursing home residents. Psychopharmacol Bull. 2002;36:14–9. [PubMed] [Google Scholar]
- Lampela P, Lavikainen P, Garcia-Horsman JA, Bell JS, Huupponen R, Hartikainen S. Anticholinergic drug use, serum anticholinergic activity, and adverse drug events among older people: a population-based study. Drugs Aging. 2013;30:321–30. doi: 10.1007/s40266-013-0063-2. [DOI] [PubMed] [Google Scholar]


