Abstract
Children with obesity report musculoskeletal pain more than normal weight children; this may be linked with literature suggesting children with obesity have higher prevalence of pes planus (flatfoot). To further elucidate whether this relation occurs, we conducted a systematic literature review on the co-occurrence of pes planus and pediatric obesity. Empirical articles published through September 2013 were obtained through an electronic search of MEDLINE and SportDiscus; included articles examined the association between bodyweight and pes planus in children. Thirteen cross-sectional studies of varied designs were identified. Methods used to diagnose pes planus varied between studies: imaging modalities, anthropometric measurements, and clinical examination. Across all studies, pes planus prevalence among children with obesity ranged widely from 14 to 67%. Nearly all studies indicated increasing pes planus in children with increasing weight. No studies evaluated pain/complications related to pes planus. Our review suggests increased prevalence of pes planus among children with obesity or increasing weight status. Due to differing methodologies, lack of consensus regarding the pes planus definition, the dearth of investigation into pain/complications, and the few existing studies, more research is needed to determine a relation between children’s body weight, pes planus, and associated effects on pain and function.
Keywords: pes planus, flatfoot, obesity, pediatrics, children, pain
INTRODUCTION
Musculoskeletal problems are being recognized as a comorbidity of higher body weight among children1–3 and adults4. Children with overweight or obesity have an increased risk of skeletal fractures, musculoskeletal pain, inferior quality of life reported on the mobility scale, and abnormal dual-energy x-ray absorptiometry (DEXA) scan angles5. Carrying excess body weight affects the musculoskeletal system as a whole, and may lead to pain and decreased physical function through abnormal loading of bones and joints, and misalignment conditions such as slipped capital femoral epiphysis (SCFE), Blount’s disease, and genu valgum6. Reports of physical pain are common among children with obesity, and musculoskeletal pain has been recognized as a potential comorbidity of obesity7. Such musculoskeletal problems and associated pain experiences are likely limiting factors discouraging children from involvement in physical activity behaviors, which may, in turn, exacerbate obesity and hinder efforts to achieve a healthy weight.
Given that the foot is especially influenced by excess weight gain and that childhood and adolescence are periods of dramatic physical development8, children with overweight or obesity may be at an increased risk for musculoskeletal problems such as pes planus (flatfoot). Studies have shown that pes planus is more prevalent among children with overweight or obesity9–11 compared to normal weight children, as 9.3–12.4% and 2.4–3.8% of overweight or obese children have either mild or severe pes planus, respectively10. Other studies report prevalences of 4–28%11, 12, and support a positive association between prevalence of pes planus and child weight. Although pes planus is not considered a comorbidity of pediatric obesity, it is a common diagnosis among children who are overweight13. It is not known, however, if carrying excess weight may be a cause of pes planus in children; studies have questioned whether pes planus may occur as a result of a lowered medial longitudinal arch after full development13, or a thicker midfoot plantar fat pad14, 15. Foot pain severity and thickness of plantar fascia are related to the midfoot loading and foot arch angle16. In obese adults, it has been suggested that pain with weight bearing and exercise comes from this increased plantar pressure 17. Alteration of foot biomechanics such as with pes planus, may play a role in the development of lower extremity pain with exercise18. Pes planus is known to cause pain in the feet and lower legs16, especially so after long walks or intense exercise17, 18. Thus, it is probable that the condition of flat feet limits desire for and participation in effective physical activity that could facilitate weight management.
Butterworth et al. reviewed studies examining the association between body composition, foot structure and function in adults, finding a strong association between higher body mass index (BMI) and reports of foot pain19. Though pes planus appears to be a common complaint among obese children and is likely to impact functional ability to engage in physical activity, expert recommendations pertaining to the assessment and treatment of pediatric obesity do not include pes planus as a potential weight-related problem20. To date, there has not been a review of the literature exploring pes planus in children with obesity. Further, it is not known if pes planus and obesity lead to greater musculoskeletal pain complaints, or impact levels of physical activity in children. This review aims to identify and summarize the pertinent literature regarding pes planus and pediatric obesity, and to clarify if a connection exists between them.
METHODS
Study design
Utilizing the 2009 PRISMA guidelines21, we systematically reviewed studies to investigate the relation between pes planus and obesity in children ages 3–18 years. Foot maturity, specifically medial longitudinal arch development, occurs between 2–6 years of age and is considered to be complete by 6 years of age22–25. The age range of 3–18 years includes both the developing and mature pediatric foot.
Search strategy
We conducted sequential online electronic searches of MEDLINE (PubMed) and SportDiscus for all years available up to September 31, 2013. Databases were searched by crossing two search terms (Table 1). All studies identified by search terms combinations were compiled, and duplicates removed. One investigator (AC) screened titles and abstracts of all identified studies initially for relevance to the study aim. Two investigators (AC, MBI) reviewed full manuscripts for consideration of inclusion, with discrepancies resolved by a third investigator (JAS). References from each manuscript were evaluated for possible inclusion as well.
Table 1.
Search Terms for Literature Review
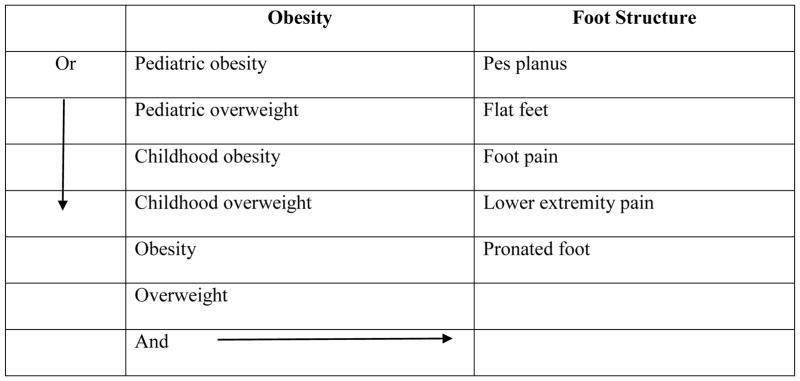
|
Inclusion and exclusion criteria
All studies included in this systematic review examined the association between weight and pes planus and other foot structure deformities and were obtained from English language peer-reviewed scientific journals. We focused on studies that identified children and adolescents as the main subjects (ages 3 to 18 years of age) and on weight as a factor that potentially influences the development or prevalence of pes planus, or is associated with pes planus. Studies that examined pes planus in adults, the influence of pes planus in adult locomotion, biological foot structures without regard to weight, or that focused solely on treatment options for pes planus were not included in the review. Studies focused on congenital pes planus, which typically were in children less than 3 years of age, were not included.
Data extraction
Three investigators (AC, MBI, JAS) extracted the following from each eligible study: objective, study design, study population characteristics including country of study, method or approach to foot measurement or evaluation, and study findings.
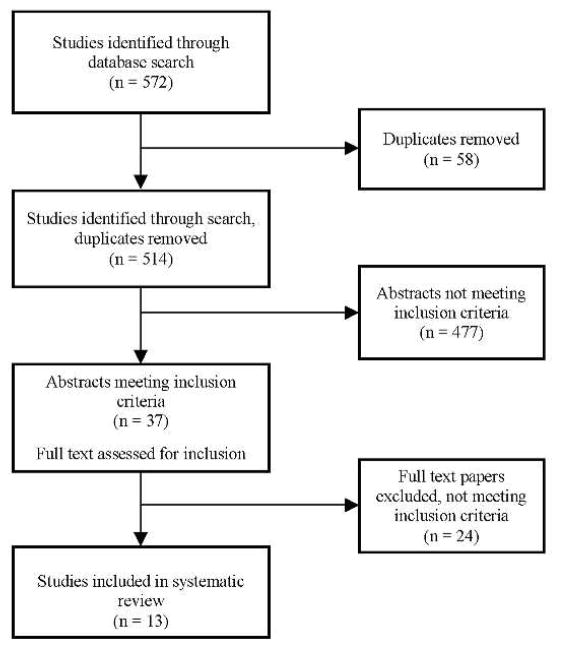
RESULTS
A total of 572 studies were identified through the electronic database searches. Fifty-eight duplicates were removed, and 514 studies were initially reviewed for potential inclusion. Of these, 477 abstracts did not meet inclusion criteria for the following reasons: 1) 447 studies were not pertinent to the objectives of pediatric obesity and pes planus, dealt primarily with foot deformities and structure, or studied adults only, 2) 25 studies were of the effects of pes planus on biomechanics of movement, and 3) 5 studies dealt with genetic differences and developmental problems linked to pes planus and obesity. Thirty-seven abstracts remained and their relevance to the objectives were further reviewed. Twenty four papers were excluded for the following reasons: 1) 12 did not explore the association between obesity and pes planus, 2) 6 did not include children (adults only in study), 3) 4 studied the effect of pes planus on walking and sitting mechanisms, and 4) 2 only discussed pes planus treatment options. Using these criteria, we identified 13 studies (Table 2) that focus on the feet of normal weight versus overweight and obese children and adolescents that met the criteria for inclusion in the systematic review. Figure 1 illustrates the selection process.
Table 2.
Characteristics of included studies
| First Author (Country) (year) | Study design; study population | Sample Size | Foot measurements | Objective(s) | Findings |
|---|---|---|---|---|---|
| Adoración Villarroya (2008)(Spain)13 | Cross-sectional; children ages 9–16.5 years | 245 | Pedograph footprint | Analyze association between overweight/obesity and foot structure in children 9 years of age and older | Decrease of foot angle with increasing weight associated with a lower longitudinal medial arch. Significant correlation between BMI z-score and footprint parameters. |
| Chang (2010)(Taiwan)26 | Cross sectional; children ages 7–12 years | 2,083 | Harris-Beath mat footprint for flatfoot grading | Determine prevalence of flexible flatfoot in elementary school children and evaluate relationship between flatfoot and obesity, gender, and age. | Prevalence of flatfoot: 67% of males, 49% of females. Prevalence by weight status: 75%, 65%, 57%, and 48% of obese, overweight, normal weight, and underweight children, respectively. Preponderance of flatfoot observed in 8-year-olds. |
| Chen (2009)(Taiwan)11 | Cross sectional; children ages 5–13 years | 1,024 | 15 foot dimensions by 3D coordinate measurement system, digital tape, and physical therapist measurement of bony landmarks | Determine prevalence of flatfoot and foot dimensions, and evaluate change in foot size between weight and non-weight bearing conditions | Significant difference in prevalence of flatfoot between normal-weight (27%), overweight (31%), and obese (56%) children Obesity effect significant for most foot dimensions, except flatfoot only significant on foot height. |
| Chen (2011)(Taiwan)27 | Cross sectional: children ages 3–6 years | 1,598 | Clinical diagnosis of flat foot by exam | Determine influence of age, gender, obesity, joint laxity, and W-sitting on unilateral and bilateral flatfoot | Prevalence of bilateral flatfoot decreased significantly with increasing age: 54.5% of 3-year-olds, only 21% for 6-year-olds Risk increased with increasing weight, and was higher in boys than girls. Age and weight not significantly influential in the unilateral flatfoot group. |
| Mauch (2008)(Germany)8 | Cross sectional; children ages 2–14 years | 2887 | 12 foot dimensions by 3-Dimensional foot scanner | Investigate influence of body mass on development of child’s foot based on foot type classification | Prevalence of flatfoot 15% Five foot types identified: flat, robust, slender, short and long feet. Significant differences among foot types by children’s BMI. Flat and robust feet more common in overweight children. |
| Mickle (2006)(Australia)14 | Cross sectional; mean age 4.3 years | 38 | Clinical foot dimensions, pedograph footprint, midfoot plantar fat pad thickness by ultrasound | Determine if flat feet in young obese children is secondary to thicker midfoot plantar fat pad or lowering of longitudinal arch relative to non-overweight children | No significant between-group differences in thickness of midfoot plantar fat pad. Overweight/obese children had significantly lower plantar arch height |
| Mickle (2006)(Australia)15 | Case matched, cross-sectional: children ages 2.9–5.5 years | 34 | Pressure platform to measure plantar pressures | Determine effects of overweight and obesity on plantar pressures generated by pre-school children during gait. | Overweight/obese children had significantly larger contact areas and generated significantly larger forces on plantar surface of foot, heel, midfoot and forefoot compared to non-overweight children. Despite forces dispersed over larger contact areas, overweight/obese children had higher peak pressures, force-time integrals and pressure-time integrals in midfoot compared. |
| Pfeiffer (2006)(Austria)9 | Cross-sectional; children ages 3–6 years | 835 | Clinical diagnosis of flat foot by exam, laser surface scanner | Establish prevalence of flat foot in 3–6 year old children to evaluate cofactors such as age, weight, and gender, and estimate the number of unnecessary treatments | Flexible flat foot prevalence 44%; pathological flat foot < 1%. 10% of children were wearing arch supports. Prevalence decreases significantly with age, prevalence decreasing from 54% at 3 years to 24% by 6 years of age. Boys had greater tendency for flat foot than girls. Significant differences in prevalence of flat foot between overweight, obese, and normal-weight children were observed. 90% of treatments unnecessary. |
| Riddiford-Harland (2000)(Australia)30 | Case matched, cross sectional; mean age 8.5 years | 124 | Pedograph footprint | Investigate relationship between obesity and foot structure | Obese children changes indicative of structural foot changes associated with compromised function. |
| Riddiford-Harland (2011)(Australia)29 | Case matched, cross-sectional; children 6.4–9.9 years | 150 | Clinical foot measurements; medial midfoot plantar fat pad thickness and internal arch height by ultrasound | Determine if flatter foot structure characteristic of obese primary school-aged children due to increased medial midfoot plantar fat pad thickness (fat feet) or structural lowering of the longitudinal arch (flat feet). | Obese children had significantly greater medial midfoot fat pad thickness compared to leaner children, while non-weight and weight bearing. Obese children had lowered medial longitudinal arch height compared to leaner children. |
| Riddiford-Harland (2011) (Australia)28 | Cross sectional; 6–9.9 years | 252 | Medial midfoot plantar fat pad thickness by ultrasound and dynamic plantar pressure distributions using pressure platform | Investigate relationship between dynamic plantar pressures generated beneath feet of school-aged children and their medial midfoot fat pad thickness | Medial midfoot plantar fat pad thickness and medial midfoot plantar pressure correlated with BMI. |
| Tenenbaum (2013)(Israel)10 | Cross sectional; 16–19 year olds | 825,964 | Clinical examination | Determine if flexible pes planus is associated with increased BMI, shorter body height, and more common in male than female adolescents | Prevalence of flexible pes planus 14.2%. Flexible pes planus significantly associated with increased BMI and shorter height. |
| Villarroya (2009)(Spain)31 | Case matched, cross sectional; children ages 9–16.5 years | 116 | Pedograph footprint, radiographs | Evaluate foot arch types of obese children and using indirect and direct measures | Morphological flatfoot in identified in obese children. |
BMI, body mass index; 3D, three-dimensional
Figure 1.
Systematic Review Flow Chart
Study Design and Participants
All studies were cross-sectional, with four employing a case-control design, matching obese or overweight with non-obese or non-overweight children, though non-matched studies tended to group participants by weight status. Sample sizes varied significantly depending on design: smaller matched cohorts (n=34)15 to larger databases (n=825,964)10. Studies mostly used convenience samples, such as schools8, 9, 11, 13–15, 26–30, outpatient clinics31, or military screenings10. Studies were conducted in Australia, Austria, Germany, Israel, Spain, and Taiwan. No studies were conducted in North America.
Methods of Measurement
Over half of the studies utilized means of imaging or measuring the foot to determine structural changes or describe foot morphology (Table 2). Imaging modalities included a “footprint” measurement termed a pedograph, radiographs, three-dimensional measurement systems or scanners, ultrasound (measurement of fat pad thickness and arch height), and laser surface scanner. Measurement modalities included clinical tape measurements of foot size or bony landmarks. Pressure exerted by the foot was measured by a pressure platform in two studies15, 28. Three studies diagnosed pes planus via clinical exam by a physician or experienced clinician using established guidelines9, 10, 27.
Prevalence of pes planus
As many of the studies drew from school populations, several studies reported overall prevalence of pes planus, though methods of determining and classifying flat feet varied. Prevalence from population studies varied to as high as 67% in males and 49% in females26 to as low as 14.2%10 and 15%8. Pfeiffer et al noted an overall prevalence of flexible pes planus of 44%, with <1% having pathological pes planus9.
Association with Weight and Age
All studies showed an increased prevalence of pes planus in obese or overweight children. Chang et al demonstrated a prevalence of 48% in normal weight children, up to 75% in obese children26. Studies by Chen et al11, 27, also in Taiwan, had lower prevalence measured by different imaging modalities, but also showed increases with increasing weight status. Three studies investigated associations with age, all finding that prevalence of pes planus decreases with increasing age9, 26, 27.
Foot Structure
Case-matched studies demonstrated differences in foot morphology between overweight or obese children versus normal weight children, specifically differences in overall foot structure30, fat pad thickness28, and contact area and pressures15. Morphologic aspects of the foot were featured in studies that obtained imaging or measurements of the foot8, 9, 11, 13–15, 28–30. In general, studies showed lower plantar arches and increased midfoot fat pad thickness in overweight or obese children, or found correlations with increasing body mass index (BMI). However, one study did not find a difference in fat pad thickness between weight groups14. Mauch et al’s study classified feet into 5 types, finding overweight children tended to have flat and robust feet8. Only one study designated differences between pathologic pes planus and flexible pes planus9, though Tennenbaum’s study noted to only be reporting prevalence of flexible pes planus10.
Pain
No studies identified in this search assessed pain or possible complications from flat feet.
DISCUSSION
Musculoskeletal problems are a known complication of pediatric obesity1–3, however, pes planus is not noted to be a concern in guidelines20, 32. From our systematic review of the literature, there does appear to be a relation between obesity and flat feet. While the studies are few in number, cross-sectional, and limited to six countries (none in North America), there is a clear association with increasing weight status and increasing prevalence of pes planus. However, there are also data that concludes that children with obesity may instead have larger, more robust feet. Despite all of these studies finding similar conclusions, a longitudinal, randomized control trial is necessary to declare a causal relation between a high BMI and pes planus. None of the studies identified included evaluation of pain or other complications that could result from flat feet; this does not imply there is no morbidity associated with flat feet, but that studies conducted to date did not investigate musculoskeletal pain. Overall, though, it is still clear that children’s feet are affected in some way by excess weight.
The clinical and functional relevance of pediatric flat feet is also still not clear. It can be postulated that children with pes planus have a more medial weight-bearing preference and subsequent changes to their lower extremity alignment during both static and dynamic gross motor activities. This could lead to deficits in balance, decreased gait speed, inefficiency of gait, or pain conditions throughout the lower extremity and spine33. A dose dependent effect of obesity has been reported by Selewski et al as children and adolescents with BMI ≥ 99th percentile report a higher burden of fatigue and mobility issues than those with BMI from the 85th to 99th percentiles34 and this could be related to the incidence of pes planus. Deficits in both static and dynamic balance could limit participation in walking, running, bicycling, dancing, and many other physical activities often prescribed as age appropriate exercise in the management of weight status.
Current literature in the evaluation of pes planus in pediatric obesity has several limitations. First, the evaluation of pain in conjunction with pediatric pes planus and obesity has not been explored to the extent that it deserves. In adults with plantar fasciitis, a painful foot condition, it has been suggested that their severity of pain and fascial thickness are related to both the regional loading and static shape of the arch of the foot16. However, this literature review did not bring out studies that have explored the connection of pes planus, obesity, and pain in children to be related to plantar fasciitis. Pes planus posturing in obese children may contribute to the development of plantar fasciitis and other gait deviations, but this has not been documented. In addition, imaging and measuring techniques, ranging from pedographs, radiographs, three-dimensional measurement systems/scanners, ultrasound, laser surface scanning, clinical tape measurements, and pressure platforms magnitudes along with clinical examinations, in this literature review demonstrate the vastly different observations of the foot arch and may contribute to the conflicting results reported. The quality of these imaging and measurement techniques are uniquely different and may not be readily available to the clinician evaluating pes planus in children. This review would warrant that a combination of imaging, measurement, and clinical examination would be recommended on each foot for a more robust evaluation of pes planus in pediatric obesity, but then also a clinically relevant and feasible technique accessible to all clinicians for diagnosis. Thirdly, standardization of foot position in both weight-bearing and non-weight-bearing positions is necessary as the medial longitudinal arch can often be flexible and dynamic with loading. Fourth, these studies have been conducted primarily in Europe and Asia in convenience samples. Future research should also examine North American samples (where pediatric obesity is highly prevalent).
Clinical practice guidelines have been established for diagnosis and treatment of pediatric pes planus by the American College of Foot and Ankle Surgeons35. The health care profession must make the distinction between the flexible pes planus and the rigid pes planus along with age of onset, family history, associated medical conditions, presence or absence of symptoms (pain, decreased endurance, and/or voluntary withdrawal from physical activities), trauma history, activity level, previous treatment, and a thorough review of systems35. Evaluation of appearance in both weight bearing and non-weight bearing positions along with range of motion, areas of tenderness, gait observations, and diagnostic studies (radiographs, CT, MRI, Bone Scan, and laboratory tests) should all be completed by the evaluator35. Seven corresponding pathways to specific diagnoses of pediatric pes planus (flexible type, rigid types, or other causes) can provide initial conservative treatment options, such as activity modifications, custom/over-the-counter orthoses to control excessive pronation, stretching exercises, NSAIDs, and reduction of comorbid conditions including weight status35. In the event that symptoms persist, surgical options including osteotomy, subtalar arthroereisis, fusions, and soft tissue procedures are presented35.
In conjunction with stretching and strengthening exercises for the foot and ankle, orthotics are the most common initial recommendation to improve foot alignment, decrease pain, and improve gross motor function. With these positive changes, it is hoped that the child with overweight or obesity will ultimately be able to increase participation in physical activity and exercise, begin to make changes in weight status, and improve quality of life. A Cochrane Review from 2010 suggests that there is not sufficient evidence from randomized controlled trials on the efficacy of foot orthoses or any other non-surgical intervention for asymptomatic pediatric pes planus33. Children with chronic juvenile arthritis do benefit from custom-made orthoses over prefabricated and newly supportive athletic shoes after three months of wear36, however, orthoses have very few side effects despite the ongoing questions of optimal choice of orthotics, weight capacity of orthotics, and long term wear of these devices.
In the case of a child with obesity, pes planus and foot pain, a trial of prefabricated orthoses is warranted in addition to good supportive shoewear during all mobility and physical activity participation. Custom orthoses can be pursued if pre-frabricated orthoses are not tolerated. Constant growth of the pediatric foot can limit the feasibility of custom made orthoses; however, custom made orthoses fabricated by an orthotist can directly impact the unique support necessary for the foot and potentially provide additional support over prefabricated options.
The epidemic of pediatric obesity has resulted in numerous comorbidities that impact a child’s health and quality of life, including musculoskeletal complaints. Pes planus has not previously been recognized as a concern in children with overweight and obesity as it has in adults. A thorough review of the literature has identified that increasing weight does appear to increase prevalence of pes planus, though due to differing populations, methodologies, and objectives, it is still not a clear association. Complications and comorbidities arising from pes planus in obese children, such as pain and limitations in activity, have also not been explored. Further investigation into these issues is needed, utilizing longitudinal designs and consistent diagnostic methodologies. However, clinicians can be aware of this association and the potential of flatfeet impacting a child’s mobility and well-being.
Acknowledgments
The authors would like to thank Karen Klein, MA (Research Support Core, Office of Research, Wake Forest School of Medicine) for her assistance in editing this manuscript.
Footnotes
CONFLICTS OF INTEREST:
Dr. Skelton was supported in part through NICHD/NIH Mentored Patient-Oriented Research Career Development Award (K23 HD061597). Dr. Skelton has served as a consultant for the Nestle Corporation, but they were not involved in any aspect of this manuscript.
- Promotion of Doctoral Studies (PODS) – Level I & II Scholarships from the Foundation for Physical Therapy, Inc.
- American Association of University Women American Dissertation Fellowship
- Rev. John P. Raynor, S.J. Fellowship from the President’s Council at Marquette University.
References
- 1.de Sa Pinto AL, de Barros Holanda PM, Radu AS, Villares SM, Lima FR. Musculoskeletal findings in obese children. J Paediatr Child Health. 2006;42:341–4. doi: 10.1111/j.1440-1754.2006.00869.x. [DOI] [PubMed] [Google Scholar]
- 2.Stovitz SD, Pardee PE, Vazquez G, Duval S, Schwimmer JB. Musculoskeletal pain in obese children and adolescents. Acta Paediatr. 2008;97:489–93. doi: 10.1111/j.1651-2227.2008.00724.x. [DOI] [PubMed] [Google Scholar]
- 3.Paulis WD, Silva S, Koes BW, van Middelkoop M. Overweight and obesity are associated with musculoskeletal complaints as early as childhood: a systematic review. Obes Rev. 2014;15:52–67. doi: 10.1111/obr.12067. [DOI] [PubMed] [Google Scholar]
- 4.Anandacoomarasamy A, Caterson I, Sambrook P, Fransen M, March L. The impact of obesity on the musculoskeletal system. Int J Obes (Lond) 2008;32:211–22. doi: 10.1038/sj.ijo.0803715. [DOI] [PubMed] [Google Scholar]
- 5.Taylor ED, Theim KR, Mirch MC, Ghorbani S, Tanofsky-Kraff M, Adler-Wailes DC, et al. Orthopedic complications of overweight in children and adolescents. Pediatrics. 2006;117:2167–74. doi: 10.1542/peds.2005-1832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chan G, Chen CT. Musculoskeletal effects of obesity. Curr Opin Pediatr. 2009;21:65–70. doi: 10.1097/MOP.0b013e328320a914. [DOI] [PubMed] [Google Scholar]
- 7.Hainsworth KR, Miller LA, Stolzman SC, Fidlin B, Davies WH, Weisman SJ, et al. Pain as a Comorbidity of Pediatric Obesity. ICAN: Infant, Child, & Adolescent Nutrition. 2012;4:315–20. doi: 10.1177/1941406412458315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mauch M, Grau S, Krauss I, Maiwald C, Horstmann T. Foot morphology of normal, underweight and overweight children. Int J Obes (Lond) 2008;32:1068–75. doi: 10.1038/ijo.2008.52. [DOI] [PubMed] [Google Scholar]
- 9.Pfeiffer M, Kotz R, Ledl T, Hauser G, Sluga M. Prevalence of flat foot in preschool-aged children. Pediatrics. 2006;118:634–9. doi: 10.1542/peds.2005-2126. [DOI] [PubMed] [Google Scholar]
- 10.Tenenbaum S, Hershkovich O, Gordon B, Bruck N, Thein R, Derazne E, et al. Flexible pes planus in adolescents: body mass index, body height, and gender--an epidemiological study. Foot & ankle international/American Orthopaedic Foot and Ankle Society [and] Swiss Foot and Ankle Society. 2013;34:811–7. doi: 10.1177/1071100712472327. [DOI] [PubMed] [Google Scholar]
- 11.Chen JP, Chung MJ, Wang MJ. Flatfoot prevalence and foot dimensions of 5- to 13-year-old children in Taiwan. Foot & ankle international/American Orthopaedic Foot and Ankle Society [and] Swiss Foot and Ankle Society. 2009;30:326–32. doi: 10.3113/FAI.2009.0326. [DOI] [PubMed] [Google Scholar]
- 12.Halabchi F, Mazaheri R, Mirshahi M, Abbasian L. Pediatric flexible flatfoot; clinical aspects and algorithmic approach. Iranian journal of pediatrics. 2013;23:247–60. [PMC free article] [PubMed] [Google Scholar]
- 13.Adoracion Villarroya M, Manuel Esquivel J, Tomas C, Buenafe A, Moreno L. Foot structure in overweight and obese children. Int J Pediatr Obes. 2008;3:39–45. doi: 10.1080/17477160701520298. [DOI] [PubMed] [Google Scholar]
- 14.Mickle KJ, Steele JR, Munro BJ. The feet of overweight and obese young children: are they flat or fat? Obesity (Silver Spring) 2006;14:1949–53. doi: 10.1038/oby.2006.227. [DOI] [PubMed] [Google Scholar]
- 15.Mickle KJ, Steele JR, Munro BJ. Does excess mass affect plantar pressure in young children? Int J Pediatr Obes. 2006;1:183–8. doi: 10.1080/17477160600881734. [DOI] [PubMed] [Google Scholar]
- 16.Wearing SC, Smeathers JE, Sullivan PM, Yates B, Urry SR, Dubois P. Plantar fasciitis: are pain and fascial thickness associated with arch shape and loading? Physical therapy. 2007;87:1002–8. doi: 10.2522/ptj.20060136. [DOI] [PubMed] [Google Scholar]
- 17.Hills AP, Hennig EM, McDonald M, Bar-Or O. Plantar pressure differences between obese and non-obese adults: a biomechanical analysis. Int J Obes Relat Metab Disord. 2001;25:1674–9. doi: 10.1038/sj.ijo.0801785. [DOI] [PubMed] [Google Scholar]
- 18.Willems TM, De Clercq D, Delbaere K, Vanderstraeten G, De Cock A, Witvrouw E. A prospective study of gait related risk factors for exercise-related lower leg pain. Gait & posture. 2006;23:91–8. doi: 10.1016/j.gaitpost.2004.12.004. [DOI] [PubMed] [Google Scholar]
- 19.Butterworth PA, Landorf KB, Gilleard W, Urquhart DM, Menz HB. The association between body composition and foot structure and function: a systematic review. Obes Rev. 2013 doi: 10.1111/obr.12130. [DOI] [PubMed] [Google Scholar]
- 20.Krebs NF, Himes JH, Jacobson D, Nicklas TA, Guilday P, Styne D. Assessment of child and adolescent overweight and obesity. Pediatrics. 2007;120(Suppl 4):S193–228. doi: 10.1542/peds.2007-2329D. [DOI] [PubMed] [Google Scholar]
- 21.Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. doi: 10.1136/bmj.b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Leung AK, Cheng JC, Mak AF. A cross-sectional study on the development of foot arch function of 2715 Chinese children. Prosthetics and orthotics international. 2005;29:241–53. doi: 10.1080/03093640500199695. [DOI] [PubMed] [Google Scholar]
- 23.Volpon JB. Footprint analysis during the growth period. Journal of pediatric orthopedics. 1994;14:83–5. doi: 10.1097/01241398-199401000-00017. [DOI] [PubMed] [Google Scholar]
- 24.Clarke HH. An objective method of measuring the height of the longitudinal arch in foot examinations. Research Quarterly. 1993;4:99–107. [Google Scholar]
- 25.Hennig EM, Staats A, Rosenbaum D. Plantar pressure distribution patterns of young school children in comparison to adults. Foot & ankle international/American Orthopaedic Foot and Ankle Society [and] Swiss Foot and Ankle Society. 1994;15:35–40. doi: 10.1177/107110079401500107. [DOI] [PubMed] [Google Scholar]
- 26.Chang JH, Wang SH, Kuo CL, Shen HC, Hong YW, Lin LC. Prevalence of flexible flatfoot in Taiwanese school-aged children in relation to obesity, gender, and age. Eur J Pediatr. 2010;169:447–52. doi: 10.1007/s00431-009-1050-9. [DOI] [PubMed] [Google Scholar]
- 27.Chen KC, Yeh CJ, Tung LC, Yang JF, Yang SF, Wang CH. Relevant factors influencing flatfoot in preschool-aged children. Eur J Pediatr. 2011;170:931–6. doi: 10.1007/s00431-010-1380-7. [DOI] [PubMed] [Google Scholar]
- 28.Riddiford-Harland DL, Steele JR, Baur LA. Medial midfoot fat pad thickness and plantar pressures: are these related in children? Int J Pediatr Obes. 2011;6:261–6. doi: 10.3109/17477166.2011.579974. [DOI] [PubMed] [Google Scholar]
- 29.Riddiford-Harland DL, Steele JR, Baur LA. Are the feet of obese children fat or flat? Revisiting the debate. Int J Obes (Lond) 2011;35:115–20. doi: 10.1038/ijo.2010.119. [DOI] [PubMed] [Google Scholar]
- 30.Riddiford-Harland DL, Steele JR, Storlien LH. Does obesity influence foot structure in prepubescent children? Int J Obes Relat Metab Disord. 2000;24:541–4. doi: 10.1038/sj.ijo.0801192. [DOI] [PubMed] [Google Scholar]
- 31.Villarroya MA, Esquivel JM, Tomas C, Moreno LA, Buenafe A, Bueno G. Assessment of the medial longitudinal arch in children and adolescents with obesity: footprints and radiographic study. Eur J Pediatr. 2009;168:559–67. doi: 10.1007/s00431-008-0789-8. [DOI] [PubMed] [Google Scholar]
- 32.Barlow SE. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics. 2007;120(Suppl 4):S164–92. doi: 10.1542/peds.2007-2329C. [DOI] [PubMed] [Google Scholar]
- 33.Rome K, Ashford RL, Evans A. Non-surgical interventions for paediatric pes planus. Cochrane Database Syst Rev. 2010:CD006311. doi: 10.1002/14651858.CD006311.pub2. [DOI] [PubMed] [Google Scholar]
- 34.Selewski DT, Collier DN, MacHardy J, Gross HE, Pickens EM, Cooper AW, et al. Promising insights into the health related quality of life for children with severe obesity. Health and quality of life outcomes. 2013;11:29. doi: 10.1186/1477-7525-11-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Harris EJ, Vanore JV, Thomas JL, Kravitz SR, Mendelson SA, Mendicino RW, et al. Diagnosis and treatment of pediatric flatfoot. The Journal of foot and ankle surgery: official publication of the American College of Foot and Ankle Surgeons. 2004;43:341–73. doi: 10.1053/j.jfas.2004.09.013. [DOI] [PubMed] [Google Scholar]
- 36.Powell M, Seid M, Szer IS. Efficacy of custom foot orthotics in improving pain and functional status in children with juvenile idiopathic arthritis: a randomized trial. The Journal of rheumatology. 2005;32:943–50. [PubMed] [Google Scholar]