Abstract
Background
Health promotion interventions often include multiple components and several patient contacts. The objective of this study was to examine how participation within a multi-component intervention (Project SHARE) is associated with changes in at-risk drinking among older adults.
Methods
Observational data analysis from a cluster-randomized trial of 31 primary care physicians and their patients aged ≥60 years, at a community-based practice with seven clinics. Recruitment occurred between 2005 and 2007. At-risk drinkers in a particular physician’s practice were randomly assigned as a group to usual care (n=640 patients) vs. intervention (n=546 patients). The intervention included personalized reports, educational materials, drinking diaries, in-person physician advice, and telephone counseling by health educators (HE). The primary outcome was at-risk drinking at follow-up, defined by scores on the Comorbidity Alcohol Risk Evaluation Tool (CARET). Predictors included whether a physician-patient alcohol risk discussion occurred, HE call occurred, drinking agreement with the HE was made, and patients self-reported keeping a drinking diary as suggested by the HE.
Results
At 6 months, there was no association of at-risk drinking with having had a physician-patient discussion. Compared to having had no HE call, the odds of at-risk drinking at 6 months were lower if an agreement was made OR patients reported keeping a diary (OR 0.58, 95% CI 0.37–0.90), or if an agreement was made AND patients reported keeping a diary (0.52, 0.28–0.97). At 12 months, a physician-patient discussion (0.61, 0.38–0.98) or an agreement AND reported use of a diary (0.45, 0.25–0.82) were associated with lower odds of at-risk drinking.
Conclusions
Within the Project SHARE intervention, discussing alcohol risk with a physician, making a drinking agreement and/or self-reporting the use of a drinking diary were associated with lower odds of at-risk drinking at follow-up. Future studies targeting at-risk drinking among older adults should consider incorporating both intervention components.
Keywords: Alcohol use, older adults, physician-patient discussion, drinking diary, drinking agreement
Approximately 30–40% of American adults aged 65 years and over drink alcohol regularly (Blazer & Wu 2011; Kirchner et al. 2007). While heavy drinking is less common with advancing age, light or moderate drinking has different risks and benefits for older adults compared to younger populations (Cooper et al. 2009; Chan et al. 2009; Reid et al. 2002). Several observational studies have found that older adults who drink moderately have better cognitive function, a reduction in cardiovascular disease, and decreased mortality compared to non-drinkers (Townsend et al. 2009; Reid et al. 2006;Lang et al. 2007a; Lang et al. 2007b; Karlamangle et al. 2009; Byles et al. 2006 ). Conversely, age-related physiologic changes in older adults elevate blood alcohol levels per amount of alcohol consumed and increase brain sensitivity to the effects of alcohol thereby increasing the potential risk of injury (Vestal et al. 1977; Gilbertson et al. 2009). Compared to younger persons, older adults also have more comorbid conditions and use more medications, including those that may increase risks with alcohol (e.g., nonsteroidal anti-inflammatories and warfarin) (Moore et al. 2007). Current practice guidelines recommend that adults be asked about their alcohol consumption as part of routine examinations as well as prior to prescribing medications that interact with alcohol (Department of Health & Human Services National Institute of Health National Institute on Alcohol Abuse and Alcoholism 2007).. However, physicians infrequently screen their existing patients for alcohol use and misuse, because they have limited time or because they simply may not remember to do so (McCormick et al. 2006; Friedmann et al. 2000; Aira et al. 2003; Johansson et al. 2005). As a result, there has been significant interest in developing effective interventions to reduce at-risk drinking in this population, and several intervention protocols have been implemented with varying degrees of success (Fink et al. 2005; Moore et al. 2011; Lin et al. 2010; Saitz et al. 2003; Whitlock et al. 2004; Jonas et al. 2012).
While the evidence suggests that multi-component interventions for at-risk adult drinkers are more successful than single brief interventions in reducing risky alcohol use (Whitlock et al. 2004; Jonas et al. 2012), there is significant heterogeneity in how these interventions have been designed. These interventions typically involve between 2 and 4 contacts with the patient over a period of several months, and often combine several different components such as personalized counseling, drinking diaries to quantify alcohol consumption, and goal-setting to reduce drinking to less harmful levels. However, some of these interventions are delivered entirely by primary care physicians while others include non-physicians, typically nurses or health educators. Some are limited to face-to-face patient contacts while others include telephone calls. These reports do not frequently describe whether specific, individual components of these interventions are each linked to reductions in at-risk drinking. Distinguishing whether different intervention components (e.g., patient-physician discussions, keeping a drinking diary, etc.) are linked to reductions in at-risk drinking may help to identify the essential intervention components for future efforts to translate clinical trials into practice.
We recently conducted a large cluster randomized clinical trial, designed to evaluate the effectiveness of a multi-component intervention designed to reduce at-risk drinking among older adults, defined by scores on the Comorbidity Alcohol Risk Evaluation Tool (CARET) (Moore et al. 2011). Project SHARE (Senior Health and Alcohol Risk Education) found a statistically significant decrease in at-risk drinking among older adults at 12 month follow-up (Ettner et al. 2014)..While the intervention included several different components, including a physician component that involved physician-patient discussions of alcohol-related risk, as well as a health educator component that involved health educator telephone calls and encouragement to keep a drinking diary and/or make an agreement to cut down on alcohol intake, the specific mechanism/s that resulted in reductions in at-risk drinking are not clear. Therefore, we conducted an analysis to investigate to what extent participation in the different intervention components may be associated with the observed behavior change.
We hypothesized that Project SHARE patients with greater participation in the physician intervention component would have lower odds of being classified as at-risk drinkers at 6 months and at 12 months of follow-up, as compared to patients who did not participate in this intervention component. We further hypothesized that patients who participated in the health educator component, specifically those who 1) received a call from the health educator but did not keep a drinking diary or make a drinking agreement, 2) either made an agreement OR self-reported that they kept a diary, and 3) both made an agreement AND self-reported that they kept a diary, would have lower odds of being classified as at-risk drinkers at 6 months and at 12 months of follow-up, as compared to patients who did not participate at all in the health educator intervention component.
METHODS
Study Design/Setting
The Project SHARE study population was drawn from primary care physicians and their patients aged 60 years and over at Sansum Clinic, a community-based group practice with seven clinics in and near Santa Barbara, California. The Project SHARE study was approved by the Institutional Review Board of the University of California, Los Angeles.
Sample - Primary Care Providers and their Patients
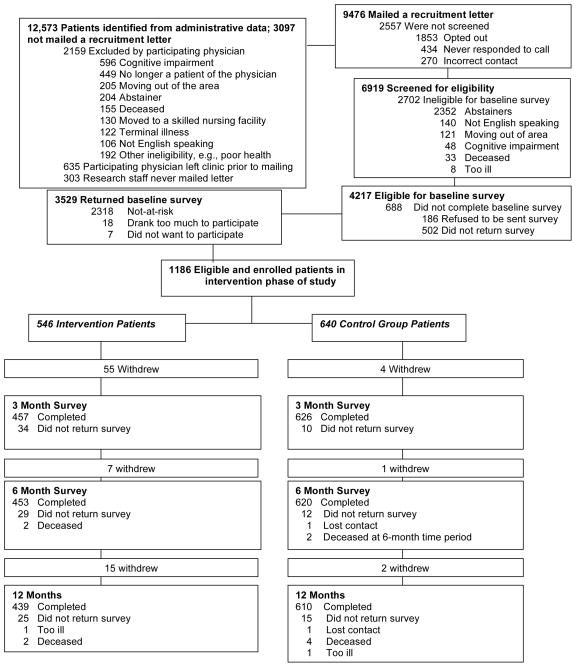
All 43 Sansum Clinic physicians were approached about the study, and 31 (72%) agreed to participate. As shown in Figure 1, Sansum Clinic staff then identified patients (n=12,573) of these 31 physicians who were aged 60 years and older. From these lists, providers indicated which patients should be excluded due to severe cognitive impairment, terminal illness, whether they were known to be moving out of the area within the next year, or inability to speak and understand English. Of the remaining patients not excluded by the physicians, 9,476 were mailed recruitment letters and 6,919 (73%) agreed to participate. They were then screened by telephone to verify the self-reported absence of these same exclusion criteria, and to confirm that they were current drinkers (consumed at least one drink in the prior three months).
Figure 1.
Participant Flow in Project SHARE
Potentially eligible patients then completed a written survey including demographic and clinical information as well as the Comorbidity Alcohol Risk Evaluation Tool (CARET). The CARET, an updated and revised version of the Alcohol-Related Problems Survey (Moore et al. 2011), identifies older adults at risk for harm from their alcohol consumption based on their responses to a set of questions about their clinical status, medication use, symptoms consistent with increased risk and drinking habits (Appendix 1). Patients who completed the baseline survey and were classified as at-risk drinkers (n=1,186) by the CARET were included in the Project SHARE intervention study, and were randomized at the level of the primary care physician into experimental and control groups (Figure 1). All patients, both control and experimental, were asked to complete follow-up surveys at 6 months and 12 months that included the CARET items. All surveys in the Project SHARE study were mailed to patients.
Appendix 1.
Comorbidity Alcohol Risk Evaluation Tool (CARET)
| Item | Amount of Drinking Considered At-Risk |
|---|---|
|
| |
| Alcohol use and behaviors in the last 12 months | |
| a. Number of drinks and frequency of drinking | a. ≥5/day at any frequency, 4/day at least 2 times/month, 3/day at least 4 times/week |
| b. Four or more drinks on one occasion (heavy episodic drinking) | b. At least 1 time/week |
| c. Driving within 2 hours of drinking 3 or more drinks | c. Any frequency |
| d. Someone concerned about participant’s alcohol use | d. Any amount |
| e. Someone concerned about participant’s alcohol use more than 12 months ago | e. ≥4/day at any frequency, 2–3/day at least 4 times/week |
|
| |
| Alcohol use and medications taken at least 3–4 times per week currently | |
| a. Medications that may cause bleeding, dizziness, sedation | a. ≥4/day at any frequency, 2–3/day at least 4 times/week |
| b. Medications used for gastroesophageal reflux, ulcer disease, depression | b. ≥4/day at any frequency, 2–3/day at least 4 times/week |
| c. Medications for hypertension | c. ≥5/day at any frequency, 4/day at least 2 times/week, 3/day at least 4 times/week |
|
| |
| Alcohol use and comorbidities in the past 12 months | |
| a. Liver disease, pancreatitis | a. Any amount |
| b. Gout, depression | b. ≥4/day at any frequency, 3/day at least 2 times/week, 2/day at least 4 times/week |
| c. High blood pressure, diabetes | c. 5/day at any frequency, 4/day at least 2 times/month, |
| d. Sometimes have problems with sleeping, falling | d. 3/day at least 4 times/week |
| e. Memory problems, heartburn, stomach pain, nausea, vomiting, or feel sad/blue | e. ≥5/day at any frequency, 4/day at least 2 times/month, 3/day at least 2 times/week |
| f. Often have problems with sleeping, falling, memory, heartburn, stomach pain, nausea, vomiting or feel sad/blue | f. ≥4/day at any frequency, 2–3/day at least 2 times/week |
Intervention
Experimental patients received a multi-component intervention that included individualized patient risk reports provided to patients and to their physicians, as well as telephone-based counseling from a health educator (Table 1). Both at baseline and at 6-month follow-up, CARET software was used to generate two risk reports with reasons for the classification as an at-risk drinker (e.g., taking blood thinning medications that could interact adversely with alcohol, symptoms of depression that may be exacerbated by alcohol, driving after drinking, etc.) and the potential harms that could result from the patient’s at-risk drinking practices. One report was designed for and mailed to patients. The other was designed for physicians, and was attached to the front of each experimental patient’s chart prior to each scheduled visit to an experimental physician.
Table 1.
Components of the Project SHARE Intervention
| Reports and Educational Materials for Patients | Materials mailed to patients:
|
| Telephone Health Educator Intervention | 5 activities took place during the Health Educator (HE) telephone calls:
|
| Brief Provider Intervention |
|
Physicians received a single two-hour training session from study investigators prior to patient recruitment, which provided guidance on how to interpret these reports and use them to initiate an alcohol risk discussion with the patient. The physicians were asked to discuss the baseline and/or 6 month reports with the patient during regularly scheduled visits during the 12 months post-baseline, focusing on the relationship between risky drinking behavior and medication use and/or health conditions. After the appointment, the physician filled out a visit log confirming that a risk-related discussion did or did not take place and either describing the content of the discussion if it did take place or explaining why it did not take place, for example due to lack of time.
The telephone-based health educator intervention was based on the same risk report. Health educators called each experimental patient three times: within two weeks after both the baseline and 6-month reports were mailed, as well as at the three-month time period. The baseline and 6-month calls included explanation of the contents of the report, as well as reinforcement of the potential health consequences of the patient’s drinking. The health educator intervention component was essentially independent of the physician intervention component, because health educators were not aware of whether patients had already discussed alcohol use with their physicians, and vice-versa. The health educator encouraged patients to keep a drinking diary detailing their daily alcohol intake and also encouraged them to make an agreement that they would cut down on their drinking to a specific negotiated goal. The health educator also focused on behavior modification, such as identifying high-risk situations in which drinking would likely occur, and familiarized the patient with coping techniques for managing these situations. The 3-month calls were designed to check on patients’ progress with their initial goals. After each call, the health educator completed a form documenting the length of each call and content discussed. This form also included information on whether or not a drinking agreement was actually made and whether or not the patient reported that they kept a drinking diary.
Analysis of Participation in Different Intervention Components
In order to assess changes in at-risk drinking among patients who participated in different intervention components, we created separate variables to measure the separate components. For the physician component, using the records from the physician visit logs we classified patients as either having had, or not had, an alcohol-related discussion with their physician at any time during the 12 month follow-up period. We created 4 categories to measure participation in the health educator component: 1) “no health educator intervention,” defined as not receiving any health educator calls, 2) receiving at least one health educator call but not making a drinking agreement or reporting that they kept a drinking diary, 3) either making a drinking agreement OR reporting that they kept a drinking diary, and 4) making a drinking agreement AND reporting that they kept a drinking diary. Notably, patients who were originally randomized to the experimental group in the Project SHARE study were classified in this analysis as having received no physician intervention if they did not have an alcohol related discussion with their physician, and as having received no health educator intervention if they did not receive any health educator calls. Because all Project SHARE patients received a personalized risk report of their at-risk drinking as well as educational materials discussing at-risk drinking, we did not include these intervention components as predictor variables.
Other Measures
The dependent variable for this analysis, whether or not a patient was an at-risk drinker, was determined at 6 and 12 months based on patient responses to the CARET survey items. Covariates were drawn from the baseline survey and included gender, race, ethnicity, marital status, education, income, home ownership, and whether or not alcohol counseling from any provider took place in the 12 months prior to Project SHARE.
Statistical Methods
We used chi-squared tests for unadjusted comparisons between groups. We then constructed separate logistic regressions that included random-effects for physicians, at 6 month follow-up and at 12 month follow-up. All analyses were completed using STATA Version 10.1 (Stata Corp). Adjusted odds ratios for at-risk drinking and 95% confidence intervals are presented in the tables; in addition, predicted probabilities associated with statistically significant findings are presented in the text. The predicted probabilities were calculated using the “predict” command in STATA, which sets the physician random effect equal to zero.
We also examined several sensitivity analyses, first assuming that all of the patients who dropped out of the study and therefore had missing outcome values were at-risk drinkers at 6 month follow-up and 12 month follow-up, and then assuming that none of these patients were at-risk drinkers at follow-up. These sensitivity analyses did not produce different results from the main, complete-case analyses, and therefore we only report results from the main analyses.
RESULTS
A total of 1,186 older adults met criteria for at-risk drinking, were enrolled in Project SHARE, and completed the baseline data collection survey. A subsample of 1,073 older adults remained in the study and completed the questionnaire at 6-month follow-up, and 1,049 remained in the study and completed the questionnaire at 12-month follow-up. Among the 419 patients in the intervention arm, 392 (94%), 315 (75%), and 364 (87%) received the baseline, 3-month, and 6-month health educator calls. Furthermore, 37 received one call from the health educator, 67 received two calls, and 300 received three calls, while 164 had one alcohol-related risk discussion with their physician, 65 had two, 51 had three and 20 had four or more. We had <5% missing data for covariates, and limited the multivariate analyses to the 997 patients for whom we had complete data at both follow-up time points.
Greater than 95% of the sample was white, and most patients were men (Tables 2 and 3). More than half of the sample were college graduates and had annual household incomes exceeding $60,000. On average, the patients in the sample consumed 13.7 alcoholic drinks per week. Each of three relatively common risk factors for at-risk drinking (taking medications that increase risk, reporting symptoms consistent with risk, or engaging in behaviors that increase risk) was present in approximately 60% of the sample. Compared to patients who did not have a discussion of alcohol risk during the 12-month study window, those who had a discussion were more likely (p=0.005) to have already received some alcohol counseling in the past 12 months (24% vs. 15%) or over 12 months ago (17% vs. 16%); we controlled for these differences in the multivariate analyses. There were no other statistically significant differences between patients who had a risk discussion with their physician during the study window and those who did not (Table 2), or between patients by level of health educator intervention (Table 3).
Table 2.
Unadjusted Participant Characteristics, by Whether or Not Physician-Level Intervention (Alcohol-Related Risk Discussion) Occurred during Project SHARE (n=997)
| Risk Discussion Occurred During 12 Months Post-Baseline (n=300) | Risk Discussion Did Not Occur (n=697) | P value | |
|---|---|---|---|
| Female Gender | 36.0% | 33.9% | 0.51 |
| Latino Ethnicity | 5.7% | 5.3% | 0.82 |
| Age | 0.12 | ||
| 60–64 years | 18.0% | 24.1% | |
| 65–69 years | 30.0% | 28.1% | |
| 70–74 years | 17.7% | 19.7% | |
| 75–79 years | 17.3% | 14.9% | |
| 80 years or greater | 17.3% | 13.2% | |
| Race | 0.06 | ||
| White | 95.3% | 98.1% | |
| Black | 0.67% | 0.29% | |
| Asian | 2.33% | 0.57% | |
| American Indian | 1.7% | 1.7% | |
| Marital Status | 0.11 | ||
| Married | 78.5% | 71.3% | |
| Divorced or Separated | 8.9% | 12.3% | |
| Widowed | 13.3% | 10.3% | |
| Never Married | 3.0% | 2.3% | |
| Education Level | 0.62 | ||
| Less than High School | 2.7% | 3.2% | |
| High School or GED | 11.0% | 9.0% | |
| Some College | 28.3% | 25.5% | |
| Graduated College | 25.7% | 25.8% | |
| Professional or Graduate Degree | 32.3% | 36.4% | |
| Annual Household Income | 0.25 | ||
| <$30,000 | 12.7% | 8.9% | |
| $30,000–$40,000 | 10.0% | 7.9% | |
| $40,000–$60,000 | 17.7% | 17.4% | |
| $60,000–$80,000 | 16.7% | 16.4% | |
| $80,000–$100,000 | 13.3% | 18.4% | |
| $100,000–$200,000 | 21.7% | 21.5% | |
| >$200,000 | 8.0% | 9.6% | |
| Own Home | 87.0% | 89.2% | 0.31 |
| Patient Received Alcohol Counseling in the Past From Any Provider | 0.005 | ||
| Never | 50.7% | 60.4% | |
| During the last year | 24.0% | 15.1% | |
| More than 1 year ago | 17.3% | 16.6% | |
| Mean # of Alcoholic Drinks/Week (SD) | 13.5 (8.0) | 13.7 (7.9) | 0.67 |
| Categories of Alcohol-Related Risk | |||
| Taking Medications that Increase Risk | 62.3% | 59.7% | 0.43 |
| Symptoms Consistent with Risk | 63.0% | 60.8% | 0.52 |
| Behaviors that Increase Risk | 65.0% | 62.4% | 0.44 |
Table 3.
Adjusted Project SHARE Participant Characteristics, by Use of Components of the Health Educator-Level Intervention (n=997)
| No phone call from HE (classified as no HE intervention) (n=593) | Patient received a phone call from HE | ||||
|---|---|---|---|---|---|
| No drinking diary, no drinking agreement (n=124) | Drinking diary OR drinking agreement (n=184) | Drinking diary AND drinking agreement (n=96) | P value | ||
| Female Gender | 32.0% | 37.1% | 37.0% | 41.7% | 0.20 |
| Latino Ethnicity | 5.7% | 4.0% | 4.9% | 6.3% | 0.85 |
| Age | 0.05 | ||||
| 60–64 years | 23.8% | 25.0% | 16.3% | 20.8% | |
| 65–69 years | 27.5% | 35.5% | 28.8% | 26.0% | |
| 70–74 years | 20.9% | 11.3% | 16.3% | 22.9% | |
| 75–79 years | 14.2% | 16.1% | 18.5% | 18.8% | |
| 80 years or greater | 13.7% | 12.1% | 20.1% | 11.5% | |
| Race | 0.36 | ||||
| White | 97.8% | 97.6% | 95.1% | 97.9% | |
| Black | 0.3% | 0.0% | 1.1% | 0.0% | |
| Asian | 0.5% | 1.6% | 2.2% | 2.1% | |
| American Indian | 1.4% | 0.8% | 1.6% | 0.0% | |
| Marital Status | 0.005 | ||||
| Married | 79.9% | 73.4% | 67.4% | 75.0% | |
| Divorced or Separated | 8.1% | 16.1% | 12.0% | 9.4% | |
| Widowed | 9.4% | 7.3% | 18.5% | 13.5% | |
| Never Married | 2.5% | 3.2% | 2.2% | 2.1% | |
| Education Level | 0.79 | ||||
| Less than High School | 3.0% | 1.6% | 3.3% | 4.2% | |
| High School or GED | 9.8% | 7.3% | 10.3% | 10.4% | |
| Some College | 24.8% | 30.7% | 29.4% | 25.0% | |
| Graduated College | 25.1% | 29.8% | 23.4% | 29.2% | |
| Professional or Graduate Degree | 37.3% | 30.7% | 33.7% | 31.3% | |
| Annual Household Income | 0.14 | ||||
| <$30,000 | 8.6% | 11.3% | 13.6% | 10.4% | |
| $30,000–$40,000 | 7.6% | 8.1% | 12.5% | 7.3% | |
| $40,000–$60,000 | 18.0% | 16.9% | 17.4% | 14.6% | |
| $60,000–$80,000 | 15.2% | 20.2% | 12.5% | 27.1% | |
| $80,000–$100,000 | 18.0% | 18.6% | 15.2% | 10.4% | |
| $100,000–$200,000 | 22.4% | 18.6% | 20.7% | 21.9% | |
| >$200,000 | 10.1% | 6.5% | 8.2% | 8.3% | |
| Own Home | 87.9% | 91.9% | 88.0% | 89.6% | 0.61 |
| Patient Received Alcohol Counseling in the Past | 0.13 | ||||
| Never | 58.9% | 54.8% | 56.0% | 55.2% | |
| During the last year | 15.2% | 17.7% | 24.5% | 20.8% | |
| More than 1 year ago | 17.2% | 21.0% | 12.0% | 18.8% | |
| Unknown | 8.8% | 6.5% | 7.6% | 5.2% | |
| Categories of Alcohol-Related Risk | |||||
| Taking Medications that Increase Risk | 60.2% | 54.8% | 64.1% | 62.5% | 0.41 |
| Symptoms Consistent with Risk | 61.7% | 63.0% | 61.5% | 64.6% | 0.88 |
| Behaviors that Increase Risk | 65.1% | 61.3% | 57.6% | 64.6% | 0.30 |
In adjusted multivariate analyses, the odds of being an at-risk drinker at 6 months did not vary significantly by whether or not a patient-physician alcohol risk discussion took place (Table 4). Compared to patients who did not receive a health educator intervention, those who either made a drinking agreement OR reported that they kept a drinking diary had a lower probability of being an at-risk drinker at 6 months [OR = 0.58, 95% CI 0.37–0.90; number needed to treat (NNT) of 10]. Patients who made a drinking agreement AND reported that they kept a drinking diary also had a lower odds of being an at-risk drinker at 6 months (OR = 0.52, 95% CI 0.28–0.97; NNT of 9). The predicted probability of at-risk drinking at 6 months would be reduced from 71% if patients did not receive a health educator intervention to 60% if patients kept a drinking diary OR made a drinking agreement, and would be further reduced to 58% if patients did both.
Table 4.
Adjusted Odds of At-Risk Drinking among Project SHARE Participants, at 6 and 12 months (n=997)
| 6 month follow-up | Odds Ratio (95% CI) | P-value for difference |
|---|---|---|
| Physician-Level Intervention | ||
| Physician-Patient Alcohol Risk Discussion Did Not Occur (REFERENCE) | 1.0 | |
| Physician-Patient Alcohol Risk Discussion Occurred | 0.81 (0.52–1.25) | 0.34 |
| Health Educator-Level Intervention | ||
| No HE Intervention (REFERENCE) | 1.0 | |
| Patient received HE phone calls ONLY | 0.72 (0.44–1.18) | 0.19 |
| Patient kept a drinking diary OR made a drinking agreement | 0.58 (0.37–0.90) | 0.02 |
| Patient kept a drinking diary AND made a drinking agreement | 0.52 (0.28–0.97) | 0.04 |
| 12 month follow-up | ||
| Physician-Level Intervention | ||
| Physician-Patient Alcohol Risk Discussion Did Not Occur (REFERENCE) | 1.0 | |
| Physician-Patient Alcohol Risk Discussion Occurred | 0.61 (0.38–0.98) | 0.04 |
| Health Educator-Level Intervention | ||
| No HE Intervention (REFERENCE) | 1.0 | |
| Patient received HE phone calls ONLY | 1.15 (0.67–1.99) | 0.60 |
| Patient kept a drinking diary OR made a drinking agreement | 0.75 (0.45–1.27) | 0.29 |
| Patient kept a drinking diary AND made a drinking agreement | 0.45 (0.25–0.82) | 0.01 |
Results are derived from logistic regression analyses.
Adjusted for gender, race, ethnicity, marital status, education, income, home ownership, whether or not alcohol counseling took place prior to Project SHARE, use of medications that increase alcohol risk, presence of symptoms that increase alcohol risk, behaviors that increase alcohol risk
As shown in Table 4, compared with patients who did not have a discussion, patients who had an alcohol-related risk discussion with their physician had lower odds of being an at-risk drinker at 12 months (OR 0.61, 95% 0.38–0.98, NNT of 10). The predicted probability of at-risk drinking at 12 months would be reduced from 67% if patients did not have an alcohol-related discussion with their physician to 54% if they did have such a discussion. No difference was seen in the probability of being an at-risk drinker at 12 months between patients with no health educator calls and those who either only received a health educator call without making a drinking agreement or reporting that they kept a drinking diary, or those who either made an agreement OR reported that they kept a diary. However, patients who both made a drinking agreement AND reported that they kept a drinking diary had lower odds of being an at-risk drinker at 12 months (OR 0.45, 95% CI 0.25–0.82, NNT of 7) compared to patients who did not receive a health educator intervention. The predicted probability of at-risk drinking at 12 months would be reduced from 68% if patients did not receive a health educator intervention to 49% if they kept a drinking diary AND made a drinking agreement.
DISCUSSION
This study examining data from Project SHARE supported our hypothesis that both the occurrence of a patient-physician risk discussion, and making a drinking agreement and/or self-report of keeping a drinking diary, were associated with lower rates of at-risk drinking at study follow-up. This suggests that both aspects of the intervention are important in reducing at-risk drinking and that efforts to reduce drinking in primary care settings should include both physicians and health educators.
We found that use of intervention components associated with the health educator (drinking agreement, self-report of keeping a drinking diary) was associated with lower rates of at-risk drinking as compared to patients who did not receive any health educator calls, at both study endpoints. A prior analysis reported a benefit of receiving health educator calls within a larger intervention study, specifically a reduction in the rates of at-risk drinking at 3 months if 3 calls were received within that time period (Maisto et al. 2001). These investigators did not find an effect of receiving health educator calls at 12 month follow-up. They were unable to specifically examine the association between at-risk drinking and having completed a drinking agreement during these phone calls, because few patients had completed a drinking agreement. Our results indicate that completion of a drinking agreement, as well as self-reported use of a drinking diary, may be important in achieving larger decreases in at-risk drinking that are sustained over a longer period. However, we did not assess outcomes beyond 12 months, and the literature indicates that extended interventions or repeated “booster” sessions may be required to maintain these effects, and may in fact be cost-effective over the long term (McKay 2005; Stout et al. 1999; Lash et al. 2011 ).
We found that having had a physician discussion about alcohol risk was associated with lower rates of at-risk drinking at 12 months but the association was not significant at the intermediate 6-month point. Many earlier intervention studies have focused on the 12-month endpoint, although the significant intervention effect is generally observed by 6 months (Fink et al. 2005; Richmond et al. 1995; Maisto et al. 2001; Curry et al. 2003; Fleming et al. 1997; Lin et al. 2010). The specific explanation for the lack of a significant effect at 6 months in our study is not entirely clear. However, because physicians were asked to engage in alcohol risk discussions with intervention patients at each visit during the 12-month followup period, only 62% of the alcohol risk discussions occurred in the first 6 months. The other 38% occurred in the second 6 months, and it is possible that the specific patients who had their initial discussion (or a follow-up discussion building on a prior discussion) between months 6 and 12 were more likely to change their behavior.
Studies of alcohol risk reduction have largely focused on describing the success of multi-component interventions, with less attention paid to the specific components within the intervention that may be most important. A recent study asked 17 primary care physicians who frequently deliver alcohol reduction interventions for young adults to rate the most effective approaches they include (Grossberg et al. 2010). Of 24 possible intervention components, 5 were identified as the most useful, specifically summarizing the patient’s drinking level, making a drinking agreement, keeping a drinking diary, discussing drinking likes and dislikes, and discussing life goals. While the target population is different in terms of age, the results of our study support these clinical observations. The ultimate goal of this line of research is to support the translation of effective interventions into widespread use in non-research situations. However, translated interventions are often modified or abbreviated to fit the capacity of different “real-world” delivery settings (Carlvlho et al. 2013; Napoles et al. 2013). Additional studies investigating which specific components of alcohol risk reduction interventions are critical to include in translation, and by whom the intervention can be delivered, will help to advance the field.
This study has several limitations, including the possibility that unmeasured differences in patient motivation or self-efficacy may lead to selection bias and different levels of intervention uptake. For example, patients who perceived their alcohol use as a more significant problem may have been more likely to engage with the health educators. However, in results not shown here, we examined the relationship between use of different intervention components and several baseline survey items that address patient self-efficacy, including confidence in being able to cut down on drinking if it was worsening one’s health and confidence in being able to ask physicians or other health care personnel for information about alcohol. The distribution of these survey items did not vary across patients who kept a drinking diary, made a drinking agreement, did both, or did neither, suggesting that unmeasured differences between patients were probably not the primary reason for the results of our main analyses. Also, due to limited statistical power we were unable to examine interactions between patient participation in the physician intervention and each of the different aspects of the health educator intervention. Other limitations include that fact that risk factors used in the CARET, such as drinking frequency and quantity, were self-reported. However, evidence from the literature suggests that patient self-reported alcohol consumption tends to be reliable and valid (Del Boca and Darkes 2003). We also relied on patient self-report that they kept a drinking diary and did not require patients to show the diary to the health educators. Finally, this study included primarily white, well-educated patients in a relatively affluent area and may not be generalizable to other settings.
In summary, we found that use of several components of the Project SHARE intervention, including the physician-delivered as well as the health educator-delivered approaches, were associated with lower rates of at-risk drinking at follow-up. This suggests that both components are important in achieving the desired effect, and future studies targeting at-risk drinking among older adults should consider incorporating both elements of the intervention.
Acknowledgments
This project was funded by National Institute on Alcohol Abuse and Alcoholism (NIAAA) Grant 1RO1AA013990 (Principal investigator: Susan L. Ettner). Alison A. Moore’s time was additionally supported by NIAAA Grants R01 AA15957 and K24 AA15957 (Principal investigator: Alison A. Moore). O. Kenrik Duru’s time was supported by National Institute on Aging Grants 5P30AG021684-12 and 5K08AG033630-05. The authors thank the following: the leadership, research staff, and information technology staff of Sansum Clinic, in particular Mr. Paul Jaconette, Ms. Chris McNamara, Ms. Linda Chapman, and Mr. Tom Colbert; Ms. Deborah Marshall and the University of California at Los Angeles research staff; the Project SHARE (Senior Health and Alcohol Risk Education) health educators; and the members of our research advisory board. Finally, we are indebted to the Sansum Clinic patients and physicians who participated in Project SHARE, without whom the study could not have been conducted.
References
- Aira M, Kauhanen J, Larivaara P, Rautio P. Factors influencing inquiry about patients’ alcohol consumption by primary health care physicians: Qualitative semi-structured interview study. Fam Pract. 2003;20:270–275. doi: 10.1093/fampra/cmg307. [DOI] [PubMed] [Google Scholar]
- Blazer DG, Wu LT. The epidemiology of alcohol use disorders and subthreshold dependence in a middle-aged and elderly community sample. Am J Geriatr Psychiatry. 2011;19:685–694. doi: 10.1097/JGP.0b013e3182006a96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Byles J, Young A, Furuya H, Parkinson L. A drink to healthy aging: The association between older women’s use of alcohol and their health-related quality of life. J Am Geriatr Soc. 2006;54:1341–1347. doi: 10.1111/j.1532-5415.2006.00837.x. [DOI] [PubMed] [Google Scholar]
- Carvalho ML, Honeycutt S, Escoffery C, Glanz K, Sabbs D, Kegler MC. Balancing fidelity and adaptation: implementing evidence-based chronic disease prevention programs. J Public Health Manag Pract. 2013;4:348–356. doi: 10.1097/PHH.0b013e31826d80eb. [DOI] [PubMed] [Google Scholar]
- Chan AM, von Muhlen D, Kritz-Silverstein D, Barrett-Connor E. Regular alcohol consumption is associated with increasing quality of life and mood in older men and women: The rancho bernardo study. Maturitas. 2009;62:294–300. doi: 10.1016/j.maturitas.2009.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper C, Bebbington P, Meltzer H, Jenkins R, Brugha T, Lindesay JE, Livingston G. Alcohol in moderation, premorbid intelligence and cognition in older adults: Results from the psychiatric morbidity survey. J Neurol Neurosurg Psychiatry. 2009;80:1236–1239. doi: 10.1136/jnnp.2008.163964. [DOI] [PubMed] [Google Scholar]
- Curry SJ, Ludman EJ, Grothaus LC, Donovan D, Kim E. A randomized trial of a brief primary-care-based intervention for reducing at-risk drinking practices. Health Psychol. 2003;22:156–165. [PubMed] [Google Scholar]
- Del Boca FK, Darkes J. The validity of self-reports of alcohol consumption: state of the science and challenges for research. Addiction. 2003;98(Suppl 2):1–12. doi: 10.1046/j.1359-6357.2003.00586.x. [DOI] [PubMed] [Google Scholar]
- Ettner SL, Xu H, Duru OK, Ang A, Tseng CH, Tallen L, Barnes A, Mirkin M, Ransohoff K, Moore AA. The effect of an educational intervention on alcohol consumption, at-risk drinking, and health care utilization in older adults: The Project SHARE study. J Stud Alcohol Drugs. 2014;75:447–457. doi: 10.15288/jsad.2014.75.447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fink A, Elliott MN, Tsai M, Beck JC. An evaluation of an intervention to assist primary care physicians in screening and educating older patients who use alcohol. J Am Geriatr Soc. 2005;53:1937–1943. doi: 10.1111/j.1532-5415.2005.00476.x. [DOI] [PubMed] [Google Scholar]
- Fleming MF, Barry KL, Manwell LB, Johnson K, London R. Brief physician advice for problem alcohol drinkers. A randomized controlled trial in community-based primary care practices. JAMA. 1997;277:1039–1045. [PubMed] [Google Scholar]
- Friedmann PD, McCullough D, Chin MH, Saitz R. Screening and intervention for alcohol problems. A national survey of primary care physicians and psychiatrists. J Gen Intern Med. 2000;15:84–91. doi: 10.1046/j.1525-1497.2000.03379.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilbertson R, Ceballos NA, Prather R, Nixon SJ. Effects of acute alcohol consumption in older and younger adults: Perceived impairment versus psychomotor performance. J Stud Alcohol Drugs. 2009;70:242–252. doi: 10.15288/jsad.2009.70.242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grossberg P, Halperin A, Mackenzie S, Gisslow M, Brown D, Fleming M. Inside the physician’s black bag: Critical ingredients of brief alcohol interventions. Subst Abus. 2010;31:240–250. doi: 10.1080/08897077.2010.514242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johansson K, Bendtsen P, Akerlind I. Factors influencing gps’ decisions regarding screening for high alcohol consumption: A focus group study in swedish primary care. Public Health. 2005;119:781–788. doi: 10.1016/j.puhe.2004.12.006. [DOI] [PubMed] [Google Scholar]
- Jonas DE, Garbutt JC, Amick HR, Brown JM, Brownley KA, Council CL, Viera AJ, Wilkins TM, Schwartz CJ, Richmond EM, Yeatts J, Evans TS, Wood SD, Harris RP. Behavioral counseling after screening for alcohol misuse in primary care: A systematic review and meta-analysis for the US Preventive Services Task Force. Ann Intern Med. 2012;157:645–654. doi: 10.7326/0003-4819-157-9-201211060-00544. [DOI] [PubMed] [Google Scholar]
- Karlamangla AS, Sarkisian CA, Kado DM, Dedes H, Liao DH, Kim S, Reuben DB, Greendale GA, Moore AA. Light to moderate alcohol consumption and disability: Variable benefits by health status. Am J Epidemiol. 2009;169:96–104. doi: 10.1093/aje/kwn294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirchner JE, Zubritsky C, Cody M, Coakley E, Chen H, Ware JH, Oslin DW, Sanchez HA, Durai UN, Miles KM, Llorente MD, Costantino G, Levkoff S. Alcohol consumption among older adults in primary care. J Gen Intern Med. 2007;22:92–97. doi: 10.1007/s11606-006-0017-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lang I, Guralnik J, Wallace RB, Melzer D. What level of alcohol consumption is hazardous for older people? Functioning and mortality in u.S. And english national cohorts. J Am Geriatr Soc. 2007;55:49–57. doi: 10.1111/j.1532-5415.2006.01007.x. [DOI] [PubMed] [Google Scholar]
- Lang I, Wallace RB, Huppert FA, Melzer D. Moderate alcohol consumption in older adults is associated with better cognition and well-being than abstinence. Age Ageing. 2007;36:256–261. doi: 10.1093/ageing/afm001. [DOI] [PubMed] [Google Scholar]
- Lash SJ, Timko C, Curran GM, McKay JR, Burden JL. Psychol Addict Behav. 2011;25:238–251. doi: 10.1037/a0022608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin JC, Karno MP, Barry KL, Blow FC, Davis JW, Tang L, Moore AA. Determinants of early reductions in drinking in older at-risk drinkers participating in the intervention arm of a trial to reduce at-risk drinking in primary care. J Am Geriatr Soc. 2010;58:227–233. doi: 10.1111/j.1532-5415.2009.02676.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin JC, Karno MP, Tang L, Barry KL, Blow FC, Davis JW, Ramirez KD, Welgreen S, Hoffing M, Moore AA. Do health educator telephone calls reduce at-risk drinking among older adults in primary care? J Gen Intern Med. 2010;25:334–339. doi: 10.1007/s11606-009-1223-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maisto SA, Conigliaro J, McNeil M, Kraemer K, Conigliaro RL, Kelley ME. Effects of two types of brief intervention and readiness to change on alcohol use in hazardous drinkers. J Stud Alcohol. 2001;62:605–614. doi: 10.15288/jsa.2001.62.605. [DOI] [PubMed] [Google Scholar]
- McCormick KA, Cochran NE, Back AL, Merrill JO, Williams EC, Bradley KA. How primary care providers talk to patients about alcohol: A qualitative study. J Gen Intern Med. 2006;21:966–972. doi: 10.1111/j.1525-1497.2006.00490.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKay JR. Is there a case for extended interventions for alcohol and drug use disorders? Addiction. 2005;100:1594–1610. doi: 10.1111/j.1360-0443.2005.01208.x. [DOI] [PubMed] [Google Scholar]
- Moore AA, Blow FC, Hoffing M, Welgreen S, Davis JW, Lin JC, Ramirez KD, Liao DH, Tang L, Gould R, Gill M, Chen O, Barry KL. Primary care-based intervention to reduce at-risk drinking in older adults: A randomized controlled trial. Addiction. 2011;106:111–120. doi: 10.1111/j.1360-0443.2010.03229.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore AA, Whiteman EJ, Ward KT. Risks of combined alcohol/medication use in older adults. Am J Geriatr Pharmacother. 2007;5:64–74. doi: 10.1016/j.amjopharm.2007.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Napoles AM, Santoyo-Olsson J, Stewart AL. Methods for translating evidence-based behavioral interventions into health disparity communities. Prev Chronic Dis. 2013;10:E193. doi: 10.5888/pcd10.130133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reid MC, Boutros NN, O’Connor PG, Cadariu A, Concato J. The health-related effects of alcohol use in older persons: A systematic review. Subst Abus. 2002;23:149–164. doi: 10.1080/08897070209511485. [DOI] [PubMed] [Google Scholar]
- Reid MC, Van Ness PH, Hawkins KA, Towle V, Concato J, Guo Z. Light to moderate alcohol consumption is associated with better cognitive function among older male veterans receiving primary care. J Geriatr Psychiatry Neurol. 2006;19:98–105. doi: 10.1177/0891988706286513. [DOI] [PubMed] [Google Scholar]
- Richmond R, Heather N, Wodak A, Kehoe L, Webster I. Controlled evaluation of a general practice-based brief intervention for excessive drinking. Addiction. 1995;90:119–132. doi: 10.1046/j.1360-0443.1995.90111915.x. [DOI] [PubMed] [Google Scholar]
- Saitz R, Horton NJ, Sullivan LM, Moskowitz MA, Samet JH. Addressing alcohol problems in primary care: A cluster randomized, controlled trial of a systems intervention. The screening and intervention in primary care (sip) study. Ann Intern Med. 2003;138:372–382. doi: 10.7326/0003-4819-138-5-200303040-00006. [DOI] [PubMed] [Google Scholar]
- Stout RL, Rubin A, Zwick W, Zywiak W, Bellino L. Optimizing the cost-effectiveness of alcohol treatment: a rationale for extended case monitoring. Addict Behav. 1999;24:17–35. doi: 10.1016/s0306-4603(98)00029-x. [DOI] [PubMed] [Google Scholar]
- Townsend MK, Devore E, Kang JH, Grodstein F. The relation between moderate alcohol consumption and cognitive function in older women with type 2 diabetes. Diabetes Res Clin Pract. 2009;85:322–327. doi: 10.1016/j.diabres.2009.06.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Health & Human Services National Institute of Health National Institute on Alcohol Abuse and Alcoholism. [Accessed January 12, 2015];Helping patients with alcohol problems: A health practioner’s guide. [Online] Available from: http://pubs.niaaa.nih.gov/publications/Practitioner/CliniciansGuide2005/guide.pdf.
- Vestal RE, McGuire EA, Tobin JD. Aging and ethanol metabolism in man. Clin Pharmacol Ther. 1977;21:343–345. doi: 10.1002/cpt1977213343. [DOI] [PubMed] [Google Scholar]
- Whitlock EP, Polen MR, Green CA, Orleans T, Klein J. Behavioral counseling interventions in primary care to reduce risky/harmful alcohol use by adults: A summary of the evidence for the U.S. Preventive services task force. Ann Intern Med. 2004;140:557–568. doi: 10.7326/0003-4819-140-7-200404060-00017. [DOI] [PubMed] [Google Scholar]