Abstract
The aim of the study
The aim of the study was to evaluate the spectrum of AIDS-defining malignancies (ADMs) and non-AIDS-defining malignancies (NADMs) in HIV-infected patients in Poland.
Material and methods
A retrospective observational study was conducted among HIV-infected adult patients who developed a malignancy between 1995 and 2012 in a Polish cohort. Malignancies were divided into ADMs and NADMs. Non-AIDS-defining malignancies were further categorised as virus-related (NADMs-VR) and unrelated (NADMs-VUR). Epidemiological data was analysed according to demographic data, medical history, and HIV-related information. Results were analysed by OR, EPITools package parameters and Fisher's exact test.
Results
In this study 288 malignancies were discovered. The mean age at diagnosis was 41.25 years (IQR20-81); for ADMs 38.05 years, and for NADMs-VURs 46.42 years; 72.22% were male, 40.28% were co-infected with HCV. The risk behaviours were: 37.85% IDU, 33.33% MSM, and 24.31% heterosexual. Mean CD4+ at the diagnosis was 282 cells/mm3 (for ADMs 232 and for NADMs-VUR 395). Average duration of HIV infection at diagnosis was 5.69 years. There were 159 (55.2%) ADMs and 129 (44.8%) NADMs, among whom 58 (44.96%) NADMs-VR and 71 (55.04%) NADMs-VUR. The most frequent malignancies were: NHL (n = 76; 26.39%), KS (n = 49; 17.01%), ICC (n = 34; 11.81%), HD (n = 23; 7.99%), lung cancer (n = 18; 6.25%) and HCC (n = 14; 4.86%). The amount of NADMs, NADMs-VURs in particular, is increasing at present. Male gender (OR = 1.889; 95% CI: 1.104–3.233; p = 0.024), advanced age: 50–60 years (OR = 3.022; 95% CI: 1.359–6.720; p = 0.01) and ≥ 60 years (OR = 15.111; 95% CI: 3.122–73.151; p < 0.001), longer duration of HIV-infection and successful HAART (OR = 2.769; 95% CI: 1.675–4.577; p = 0) were independent predictors of NADMs overall, respectively.
Conclusions
In a Polish cohort NHL was the most frequent malignancy among ADMs, whereas HD was the most frequent among NADMs. Increased incidence of NADMs appearing in elderly men with longer duration of HIV-infection and with better virological and immunological control was confirmed. As HIV-infected individuals live longer, better screening strategies, especially for NADMs-VUR, are needed. The spectrum of cancer diagnoses in Poland currently does not appear dissimilar to that observed in other European populations.
Keywords: HIV, AIDS-defining malignancies, non-AIDS-defining malignancies, PLHIV, cART, cancer
Introduction
The prevalence and spectrum of malignancies have continued to grow, resulting in high morbidity and mortality. It also concerns, with no exceptions, people living with human immunodeficiency virus (PLHIV) [1–3]. Experience has taught us that several malignancies, such as Acquired Immunodeficiency Syndrome-AIDS-defining malignancies (ADMs), including Kaposi sarcoma (KS), non-Hodgkin's lymphoma (NHL), and an invasive cervical cancer (ICC) are closely connected with human immunodeficiency virus (HIV) infection and are found more frequently in HIV-infected patients. Since the introduction of combination antiretroviral therapy (cART), the number of ADMs as a whole has decreased significantly. Nevertheless, it remains a significant problem and one of the major causes of death [4–6]. There also exist non-AIDS-defining malignancies (NADMs), the number of which seems still to be rising and the reasons for which may be completely different [7–13]. NADMs appear to have increased prevalence and higher malignancy-related mortality attributable to earlier onset, a more advanced malignancy stage, and a worse prognosis at malignancy diagnosis in HIV-infected patients than in the general population [9–10, 14–17]. Although the introduction of cART has considerably improved HIV positive patients’ prognosis and contributed to a significant decrease of opportunistic infections prevalence and mortality, NADMs have become responsible for a new challenge in HIV-positive patients’ care and cure. It is still unclear whether the number of NADMs has indeed increased or whether their prevalence is the result of both increased surveillance and longevity of HIV-positive patients [18–19]. Furthermore, there are many possible reasons and risk factors of NADMs prevalence in HIV-infected individuals. The rise in survival caused by cART may also result in an increased exposure of the population to oncogenes, including, among others, HIV chronic infection, prolonged immunosuppression, environmental factors, and potentially oncogenic drug activities [7–9, 15, 20–22]. We should also take into consideration the lifestyle of many PLHIV and the impact of an increased burden of traditional risk factors, such as, for example, smoking [18, 23]. Moreover, co-infections with other viruses and their treatment have also influenced the carcinogenesis in HIV-infected individuals with the loss of immune control. Thus, literature often tends to make a distinction between virus related (VR) NADMs and virus unrelated (VUR) NADMs [20, 24]. Some viruses have specific oncogenic properties. For instance, the relation between human papillomavirus (HPV), hepatitis B virus (HBV), hepatitis C virus (HCV), human herpesvirus-8 (HHV-8), Epstein-Barr virus (EBV), and malignancies has been confirmed [9, 24–26]. In addition, Immune Reconstitution Inflammatory Syndrome in successful antiretroviral treatment (ART) induces the activity of latent oncogenic viruses [27]. Much remains to be learned about the risk of malignancies onset, risk reduction, optimal treatment, and drug interactions in the HIV-infected population. The aim of this study was to evaluate the spectrum of malignancies in HIV-infected adult population (18 years and older) in Poland; to describe the trends in these illnesses over the past eighteen years; and to attempt to research the reasons for their hypothetically increased prevalence.
Material and methods
There is limited data of malignancies’ prevalence in HIV-infected patients in Poland. The very first retrospective, observational study was conducted among HIV-infected adult patients who developed a malignancy during the period 1995–2012 in the long-lasting Polish cohort approach. The present analysis is based upon the data collected from 1st January 1995 to the earliest diagnosis of a new malignancy, namely until 1st January 2013 (the cut-off date for the present dataset), adding the observational period of six months after the patient's last clinic visit. HIV-database includes most (8 out of 10) of AIDS clinical centres that also offer ART in Poland: Białystok, Bydgoszcz, Gdańsk, Kraków, Łódź, Poznań, Szczecin, and Warszawa. The malignancies were classified according to the current World Health Organisation (WHO), International Statistical Classification of Diseases and Related Health Problems, the tenth edition code classification system (ICD-10), including the WHO Classification of Tumours of Hematopoietic and Lymphoid Tissues for HIV-related lymphomas [28, 29]. Detailed data on all malignancies was collected on a specific and anonymous case report form (CRF). The CRFs have also included a definite histological confirmation or, exceptionally, through lack of other measures, a case description based upon an accurate clinical diagnosis and complementary examinations made by an experienced practitioner where the treatment had been initiated to support the description of an invasive malignancy, yet lacking supportive histopathological findings. A probable degree of certainty was excluded from the study. All patients diagnosed with malignancies were followed up by an oncologist. Malignancies were divided into ADMs and NADMs. Additionally, NADMs were further categorised as virus-related (NADMs-VR) and virus unrelated (NADMs-VUR). Epidemiological data was analysed according to demographic data, medical history, HIV-related information, ART, and malignancies’ outcome, and was collected from all patients at the time of malignancy diagnosis. The contact with HBV was defined as HBV surface antigen positive. The contact with HCV was defined as HCV core antibody positive at baseline or ever in the past. Baseline characteristics of the patients are summarised in Table 1, stratified by separate malignancy types. A standard descriptive analysis was performed, including frequency distributions for categorical data and calculation of medians alongside interquartile ranges (IQR) for continuous variables. The predictors of declining screening were explored using univariate and multivariate logistic regression. The parameters Odds Ratio (OR) and 95% confidence limits (95% Cl) were reported in the analysis of the association of chosen attributes in various types of cancers (ADMs vs. NADMs and NADMs-VR vs. NADMs-VUR). The system R and packet EPITools of the function Epitab were used for data calculation. The Fisher's exact test was used to calculate the p-value. Specific ethical approval for this study was not a requirement, in accordance with Polish national legislation.
Table 1.
Characteristics of the patients at the time of malignancies' diagnosis, for all malignancies in total and for each group: ADMs, NADMs, NADMs-VR, NADMs-VUR
| Characteristics (n = 288): |
Total (n = 288) n (%) |
ADMs (n = 159) n (%) |
NADMs (n = 129) n (%) |
NADMs-VR (n = 58) n (%) |
NADMs-VUR (n = 71) n (%) |
|---|---|---|---|---|---|
| Age at baseline | |||||
| median [IQR] (years) | 41 [20-81] | 38 [21-66] | 45 [20-81] | 44 [22-71] | 46 [20-81] |
| Gender | |||||
| male | 208 (72.2) | 106 (66.7) | 102 (79.1) | 50 (86.2) | 52 (73.2) |
| female | 80 (27.8) | 53 (33.3) | 27 (20.9) | 8 (13.8) | 19 (26.8) |
| Race | |||||
| Caucasian | 284 (98.6) | 156 (98.1) | 129 (100.0) | 58 (100.0) | 70 (98.6) |
| other | 4 (1.4) | 3 (1.9) | 0 (0.0) | 0 (0.0) | 1 (1.4) |
| Exposure group | |||||
| homosexual | 96 (33.3) | 61 (38.4) | 35 (27.1) | 17 (29.3) | 18 (25.4) |
| IDU | 109 (37.8) | 54 (34.0) | 55 (42.6) | 28 (48.3) | 27 (38.0) |
| Hetreosexual | 70 (24.3) | 38 (23.9) | 32 (24.8) | 11 (19.0) | 21 (29.6) |
| other | 13 (4.5) | 6 (3.8) | 7 (5.4) | 2 (3.4) | 5 (7.0) |
| Hepatitis B status | |||||
| negative | 182 (63.2) | 107 (67.3) | 75 (58.1) | 36 (62.1) | 39 (54.9) |
| positive | 105 (36.5) | 51 (32.1) | 54 (41.9) | 22 (37.9) | 32 (45.1) |
| unknown | 1 (0.3) | 1 (0.6) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Hepatitis C status | |||||
| negative | 167 (58.0) | 97 (61.0) | 70 (54.3) | 27 (46.6) | 43 (60.6) |
| positive | 116 (40.3) | 58 (36.5) | 58 (45.0) | 31 (53.4) | 27 (38.0) |
| unknown | 5 (1.7) | 4 (2.5) | 1 (0.8) | 0 (0.0) | 1 (1.4) |
| Ever smoked | |||||
| yes | 216 (75.0) | 114 (71.7) | 102 (79.1) | 46 (79.3) | 56 (78.9) |
| no | 72 (25.0) | 45 (28.3) | 27 (20.9) | 12 (20.7) | 15 (21.1) |
| Ever abused alcohol | |||||
| yes | 129 (44.8) | 74 (46.5) | 55 (42.6) | 31 (53.4) | 24 (33.8) |
| no | 159 (55.2) | 85 (53.5) | 74 (57.4) | 27 (46.6) | 47 (66.2) |
| Ever abused drugs | |||||
| yes | 112 (38.9) | 57 (35.8) | 55 (42.6) | 29 (50.0) | 26 (36.6) |
| no | 176 (61.1) | 102 (64.2) | 74 (57.4) | 29 (50.0) | 45 (63.4) |
| Duration of HIV-infection (years) | |||||
| < 1 | 90 (31.3) | 66 (41.5) | 24 (18.6) | 10 (17.2) | 14 (19.7) |
| 1-5 | 85 (29.5) | 46 (28.9) | 39 (30.2) | 16 (27.6) | 23 (32.4) |
| 6-10 | 46 (16.0) | 22 (13.8) | 24 (18.6) | 14 (24.1) | 10 (14.1) |
| > 10 | 67 (23.3) | 25 (15.7) | 42 (32.6) | 18 (31.0) | 24 (33.8) |
| Prior opportunistic infections | |||||
| yes | 127 (44.0) | 61 (38.4) | 66 (51.2) | 35 (60.3) | 31 (43.7) |
| no | 161 (55.9) | 98 (61.6) | 63 (48.8) | 23 (39.7) | 40 (56.3) |
| Nadir CD4 count | |||||
| median [IQR] (cells/mm3) | 145 [0-1265] | 135 [0-1265] | 157 [2-965] | 131 [2-426] | 179 [2-965] |
| CD4 count at baseline | |||||
| median [IQR] (cells/mm3) | 282 [8-1265] | 232 [3-1265] | 345 [8-1260] | 283 [8-1260] | 395 [18-1242] |
| VL suppression at baseline (< 50 copies/ml) | |||||
| yes | 89 (30.9) | 32 (20.1) | 57 (44.2) | 25 (43.1) | 31 (43.7) |
| no | 175 (60.8) | 109 (68.6) | 66 (51.2) | 28 (48.3) | 39 (54.9) |
| Unknown | 24 (8.3) | 18 (11.3) | 6 (4.7) | 5 (8.6) | 1 (1.4) |
| Ever started cART before Malignancies' diagnosis | |||||
| yes | 150 (52.1) | 70 (44.0) | 80 (62.0) | 33 (56.9) | 47 (66.2) |
| no | 138 (47.9) | 89 (56.0) | 49 (38.0) | 25 (43.1) | 24 (33.8) |
| cART at baseline | 139 (48.3) | 63 (39.6) | 76 (58.9) | 33 (56.9) | 43 (60.6) |
| yes | 149 (51.7) | 96 (60.4) | 53 (41.1) | 25 (43.1) | 28 (39.4) |
| no | |||||
| Duration of cART (years) none | 138 (47.9) | 89 (56.0) | 49 (38.0) | 25 (43.1) | 24 (33.8) |
| < 1 | 48 (16.7) | 33 (20.8) | 15 (11.6) | 6 (10.3) | 9 (12.7) |
| 1-2 | 33 (11.5) | 18 (11.3) | 15 (11.6) | 7 (12.1) | 8 (11.3) |
| 3-5 | 23 (8.0) | 8 (5.0) | 15 (11.6) | 6 (10.3) | 9 (12.7) |
| > 5 | 46 (16.0) | 11 (6.9) | 35 (27.1) | 14 (24.1) | 21 (29.6) |
| Death during study period | |||||
| yes | 130 (45.1) | 66 (41.5) | 64 (49.6) | 33 (56.9) | 31 (43.7) |
| no | 158 (54.9) | 93 (58.5) | 65 (50.4) | 25 (43.1) | 40 (56.3) |
| Overall survival after Malignancies' diagnosis (years) | |||||
| < 1 | 99 (34.4) | 55 (34.6) | 44 (34.1) | 27 (46.6) | 17 (23.9) |
| 1-2 | 66 (22.9) | 32 (20.1) | 34 (26.4) | 7 (12.1) | 27 (38.0) |
| 3-5 | 56 (19.4) | 27 (17.0) | 29 (22.5) | 11 (19.0) | 18 (25.4) |
| 6-10 | 46 (16.0) | 27 (17.0) | 19 (14.7) | 10 (17.2) | 9 (12.7) |
| > 10 | 21 (7.3) | 18 (11.3) | 3 (2.3) | 3 (5.2) | 0 (0.0) |
ADMs – AIDS-defining malignancies; NADMs – non-AIDS-defining malignancies; NADMs-VR – non-AIDS-defining malignancies virus related; NADMs-VUR – non-AIDS-defining malignancies virus unrelated
Results
In this study, between 1995 and 2012, a total of 288 malignancies were finally confirmed in 285 HIV-infected adult patients and were ultimately included in the analyses. One patient diagnosed with NADM was previously diagnosed with an ADM, and two patients were diagnosed with two malignancies from the same group; however, they occurred at different times. In the vast majority of the cases, the malignancies were confirmed by histological examination (n = 260; 90.3%) and the rest were defined as the probable degree of certainty as mentioned above (n = 28; 9.7%). Table 1 gives the main characteristics of patients included in the present study. The mean age at the malignancy diagnosis was 41 years [IQR, 20–81 years]; the youngest for ADMs was 38 years and the most advanced for NADMs-VURs was 46 years. Patients were mainly male (n = 208; 72.2%) and of white ethnic origin (n = 284; 98.6% Caucasian). Overall, the risk behaviours reported were as follows: 37.8% Injecting Drug Users (IDUs; n = 109), 33.3% Men who have Sex with Men (MSM; n = 96), and 24.3% heterosexual (n = 70), and they were broadly similar to each group of malignancies. Men who have Sex with Men dominated solely in the ADMs group (n = 61; 38.4%) where KS diagnosed patients constituted 75.5% (n = 37). HIV-infected patients diagnosed with malignancies had, in the majority, smoked tobacco at some time (n = 216; 75%) and they had high prevalence of co-infections with HBV (n = 105; median 36.5%) and HCV (n = 116; median 40.3%).
Most of the patients showed advanced HIV disease. In almost one third of the patients (n = 90; 31.3%) HIV infection diagnosis was confirmed at the same time or less than a year before a malignancy diagnosis. As much as 41.5% (n = 66) of the patients diagnosed with ADM were late presenters. Moreover, most of them were previously diagnosed with AIDS – over two third of them (n = 219; 76.0%) had nadir CD4+ cell count < 200 cells/mm3 (Centres for Disease Control and Prevention (CDC) classification system-clinical categories 3) and/or almost half of the patients (n = 127; 44%) had experienced at least one of the opportunistic infections (not including ADMs) before the baseline (CDC classification system – clinical categories C). An average duration of HIV infection before the diagnosis was short, averaging 5.7 years. Attention shall be paid to a longer period of HIV infection among NADMs, particularly among the NADMs-VR. Mean nadir CD4+T cell count was 145 cells/mm3 (the lowest for NADMs-VR 131 cells/mm3 and the highest for NADMs-VUR 179 cells/mm3). The average duration of cART according to accurate Polish guidelines before malignancies’ diagnosis was also short and was equal to 1.9 years (the shortest for ADMs was 1.0 year and the longest for NADMs-VUR was 3.2 years). Mean CD4+T cell count at baseline was 282 cells/mm3 (the lowest for ADMs was 232 cells/mm3 and the highest for NADMs-VUR was 395 cells/mm3) and 60.8% (n = 175) patients at baseline had a detectable HIV-1 viral load (> 50 copies/ml). As much as 60.4% (n = 96) of the patients had not received any cART when ADM was diagnosed, unlike 58.9% (n = 76) of the patients who received such treatment when NADM was diagnosed, most of all at the NADM-VUR diagnosis (n = 43; 60.6%). The diagnosis of any malignancy was connected to a worse prognosis and poor treatment outcome with mean overall survival after malignancies’ diagnosis equal to 3.4 years – shortest for NADMs-VUR at 2.5 years. Although for 80.2% (n = 231) of the patients, oncological treatment was started, as much as 45.1% (n = 130) of them died during the observation period, while the highest mortality was registered for NADMs-VR (n = 33; 56.9%). For as much as 92.9% of the patients diagnosed with hepatocellular carcinoma (HCC) (n = 13/14) symptomatic treatment was introduced due to the advanced stage of the malignancy and the lack of any possibility to start curative treatment. Similarly, the palliative treatment was started for 55.6% (n = 5/9) of primary central nervous system lymphomas (PCNSLs) and 33.3% of lung cancers (n = 6/18).
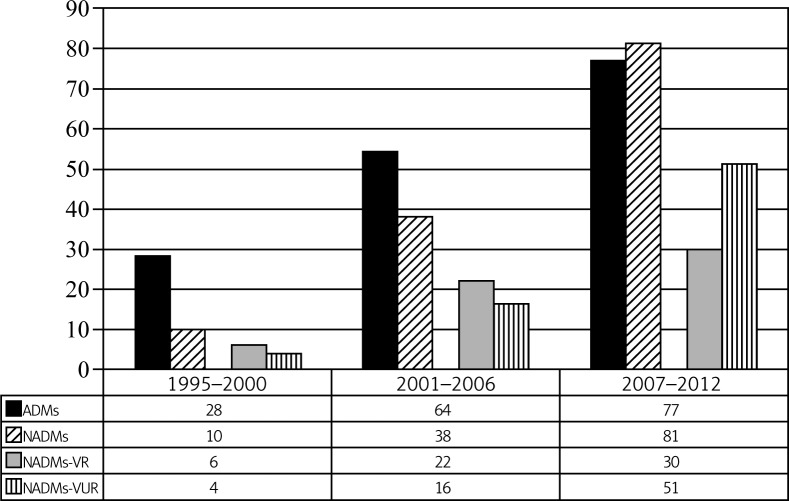
There were 159 (55.2%) ADMs and 129 (44.8%) NADMs diagnosed. Among NADMs 58 (45%; 20.1% of total malignancies) were VR and 71 (55%; 24.7% of total malignancies) were VUR. Figure 1 shows that the cumulative incidence of malignancies increased considerably in each of the three six-year periods from 1995 to 2012. However, it should also be emphasised that a progressive, substantial increase in the 6-year cumulative incidence was chiefly observed for NADMs. Furthermore, this figure demonstrates a rising trend in NADMs-VUR among NADMs over the study period.
Fig. 1.
Estimated prevalence of AIDS-defining malignancies (ADMs) and non-AIDS-defining malignancies (NADMs). The latter are divided into virus related (NADMs-VR) and virus unrelated (NADMs-VUR) over the presented periods of time
Most of the cases were as follows: non-Hodgkin lymphoma (NHL) (n = 76; 26.4%), Kaposi sarcoma (KS) (n = 49; 17.0%), invasive cervical cancer (ICC) (n = 34; 11.81%), Hodgkin's disease (HD) (n = 23; 8.0%), lung cancer (n = 18; 6.3%), and hepatocellular carcinoma (HCC) (n = 14; 4.9%). The most frequent malignancies classified by sex were as follows: NHL (n = 57; 27.4%), KS (n = 49; 23.6%), HD (n = 19; 9.1%), lung cancer (n = 17; 8.2%) for men and ICC (n = 34; 42.5%), NHL (n = 19; 23.8%), HD (n = 4; 5.0%), skin cancer (n = 4; 5.0%) for women. The spectrum of confirmed malignancies from each group is represented by a percentage against the total sum, and they were divided into sexes (Table 2). Taking into consideration the frequency of particular types of malignancies’ prevalence in certain periods of time, most of malignancies increased, especially among NADMs – lung, skin, and anal cancer as well as among HD and HCC. The only types of malignancies which showed a tendency to decrease were ICCs and PCNSLs.
Table 2.
Types of malignancies diagnosed among adult HIV-infected patients in a Poland cohort by total and by overall percentage with division into sexes
| Type of malignancies (288 evaluable data sets from 285 patients) | Total, n | Total, % | Men, n | Women, n |
|---|---|---|---|---|
| Grand total | 288 | 100.0 | 208 (72.22%) | 80 (27.78%) |
| AIDS-Defining Malignancies (ADMs) – subtotal: | 159 | 55.2 | 106 (66.7%) | 53 (33.3%) |
| Non-Hodgkin's Lymphoma (NHL) | 76 | 26.4 | 57 | 19 |
| Diffuse large B-cell lymphoma (DLBCL): | 55 | 19.1 | 40 | 15 |
| DLBCLs | 42 | 14.6 | 34 | 8 |
| Primary central nervous system lymphoma (PCNSL) | 9 | 3.1 | 3 | 6 |
| Centroblastic lymphoma | 4 | 1.4 | 3 | 1 |
| Burkitt lymphoma | 18 | 6.3 | 15 | 3 |
| Plasmablastic lymphoma (PBL) | 3 | 1.0 | 2 | 1 |
| Kaposi Sarcoma (KS) | 49 | 17.0 | 49 | 0 |
| Invasive Cervical Cancer (ICC) | 34 | 11.8 | 0 | 34 |
| Non-AIDS-Defining Malignancies (NADMs) – subtotal: | 129 | 44.8 | 102 (79.1%) | 27 (20.9%) |
| Non-AIDS-Defining Malignancies-Virus Related (NADMs-VR): | 58 | 20.1 | 50 (86.2%) | 8 (13.8%) |
| EBV-related: | 28 | 9.7 | 24 | 4 |
| Hodgkin's disease (HD) | 23 | 8.0 | 19 | 4 |
| T-cell non-Hodgkin's lymphoma | 3 | 1.0 | 3,0 | 0 |
| Not classified | 2 | 0.7 | 2,0 | 0 |
| HPV-related: | 16 | 5.6 | 13 | 3 |
| Anal | 9 | 3.1 | 8 | 1 |
| Larynx | 5 | 1.7 | 4 | 1 |
| Tonsil | 2 | 0.7 | 1 | 1 |
| HBV and HCV-related: | 14 | 4.9 | 13 | 1 |
| Hepatocellular carcinoma (HCC) | 14 | 4.9 | 13 | 1 |
| Non-AIDS-Defining Malignancies-Virus Unrelated (NADMs-VUR) | 71 | 24.7 | 52 (73.2%) | 19 (26.8%) |
| Lung | 18 | 6.3 | 17 | 1 |
| Skin cancer | 13 | 4.5 | 9 | 4 |
| Germ cell tumor | 7 | 2.4 | 7 | 0 |
| Colon | 5 | 1.7 | 3 | 2 |
| Prostate | 5 | 1.7 | 5 | 0 |
| Thyroid | 5 | 1.7 | 3 | 2 |
| Acute promyelocytic leukemia | 3 | 1.0 | 1 | 2 |
| Central nervous system | 3 | 1.0 | 2 | 1 |
| Ovary | 3 | 1.0 | 0 | 3 |
| Brest | 2 | 0.7 | 0 | 2 |
| Uterus | 2 | 0.7 | 0 | 2 |
| B-cell chronic lymphocytic leukemia | 1 | 0.3 | 1 | 0 |
| Gallbladder | 1 | 0.3 | 1 | 0 |
| Multiple myeloma | 1 | 0.3 | 1 | 0 |
| Stomach | 1 | 0.3 | 1 | 0 |
| Suprarenal gland | 1 | 0.3 | 1 | 0 |
On closer inspection of the ADMs and NADMs, multivariate statistical analysis eventually revealed that patients diagnosed with NADM were more often male (p = 0.024) and of advanced age: 50–60 years (p = 0.01) and ≥ 60 years (p < 0.001). Also, the probability of NADMs prevalence among patients who had been diagnosed with prior opportunistic infections other than ADM is statistically significant and is associated with an increased NADMs risk (p = 0.032). Besides, a longer history of HIV-infection (1–5 years: p = 0.009; 5–10 years: p = 0.004; > 10 years: p < 0.001) and successfully received cART currently (p = 0.003) alongside HIV-1 viral load suppression (p < 0.001) and with higher levels of CD4+T cell count (CD4+ > 501 cells/mm3 vs. ≤ 500 cells/mm3: p < 0.001) at baseline were independent predictors of NADMs, respectively. Comparing NADMs-VR and NADMs-VUR, fewer factors remained statistically significant, namely: nadir CD4+ count > 500 cells/mm3 (p = 0.03) and previous or current alcohol abuse (p = 0.032) were independent predictors of NADMs-VUR. Moreover, for patients diagnosed with NADM-VUR there is a statistical tendency to a shorter life expectancy over a 1-2 year-long period of time (p = 0.003) and 2–5 years (p = 0.004) after a malignancy diagnosis. All characteristics of the patients at the time of malignancies’ diagnosis as well as their statistical relations for ADMs vs. NADMs and for NADMs-VR vs. NADMAs-VUR are presented in Table 3 and 4.
Table 3.
Characteristics of the patients at the time of malignancies' diagnosis for AIDS-defining malignancies (ADMs) versus non-AIDS-defining malignancies (NADMs). Factors statistically associated with NADMs in bold
| Characteristic | ADMs | NADMs | OR | 95% CI | p value | |||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| n | % | n | % | |||||
| Sex | female | 53 | 33.3 | 27 | 20.9 | 1 | - | - |
| male | 106 | 66.7 | 102 | 79.1 | 1.889 | 1.104-3.233 | 0.024 | |
| Age at the malignancies' diagnosis (years) | [20; 30) | 34 | 21.4 | 18 | 14.0 | 1 | - | - |
| [30; 40) | 65 | 40.9 | 22 | 17.1 | 0.639 | 0.302-1.351 | 0.252 | |
| [40; 50) | 38 | 23.9 | 41 | 31.8 | 2.038 | 0.99-4.195 | 0.072 | |
| [50; 60) | 20 | 12.6 | 32 | 24.8 | 3.022 | 1.359-6.72 | 0.01 | |
| [60; 81] | 2 | 01.3 | 16 | 12.4 | 15.111 | 3.122-73.151 | 0 | |
| Mode of HIV exposure | bisexual | 6 | 03.8 | 7 | 05.4 | 1 | - | - |
| heterosexual | 38 | 23.9 | 32 | 24.8 | 0.722 | 0.22-2.367 | 0.764 | |
| IDU | 54 | 34.0 | 55 | 42.6 | 0.873 | 0.276-2.766 | 1 | |
| MSM | 61 | 38.4 | 35 | 27.1 | 0.492 | 0.153-1.58 | 0.241 | |
| Duration of HIV-infection at the malignancies' diagnosis (years) | [0; 1) | 66 | 41.5 | 24 | 18.6 | 1 | - | - |
| [1; 5) | 39 | 24.5 | 35 | 27.1 | 2.468 | 1.284-4.742 | 0.009 | |
| [5; 10) | 26 | 16.4 | 27 | 20.9 | 2.856 | 1.4-5.826 | 0.004 | |
| [10; 34] | 28 | 17.6 | 43 | 33.3 | 4.223 | 2.168-8.228 | 0 | |
| Opportunistic infections before malignancies' diagnosis | no | 98 | 61.6 | 63 | 48.8 | 1 | - | - |
| yes | 61 | 38.4 | 66 | 51.2 | 1.683 | 1.051-2.694 | 0.032 | |
| Nadir CD4 count (cells/mm3) | [0; 200) | 126 | 79.2 | 93 | 72.1 | 1 | - | - |
| [200; 350) | 21 | 13.2 | 24 | 18.6 | 1.548 | 0.813-2.948 | 0.191 | |
| [350; 500) | 8 | 05.0 | 6 | 04.7 | 1.016 | 0.341-3.028 | 1 | |
| [> 500] | 4 | 02.5 | 6 | 04.7 | 2.032 | 0.558-7.407 | 0.336 | |
| Smoking status | no | 45 | 28.3 | 27 | 20.9 | 1 | - | - |
| yes | 114 | 71.7 | 102 | 79.1 | 1.491 | 0.863-2.576 | 0.172 | |
| Alcohol status | no | 85 | 53.5 | 74 | 57.4 | 1 | - | - |
| yes | 74 | 46.5 | 55 | 42.6 | 0.854 | 0.535-1.363 | 0.552 | |
| Drugs status | no | 102 | 64.2 | 74 | 57.4 | 1 | - | - |
| yes | 57 | 35.8 | 55 | 42.6 | 1.33 | 0.826-2.141 | 0.274 | |
| Hepatitis C status | negative | 97 | 61.0 | 70 | 54.3 | 1 | - | - |
| positive | 58 | 36.5 | 58 | 45.0 | 1.386 | 0.861-2.231 | 0.184 | |
| unknown | 4 | 02.5 | 1 | 00.8 | 0.346 | 0.038-3.167 | 0.65 | |
| Hepatitis B status | negative | 107 | 67.3 | 75 | 58.1 | 1 | - | - |
| positive | 51 | 32.1 | 54 | 41.9 | 1.511 | 0.932-2.449 | 0.109 | |
| unknown | 1 | 00.6 | 0 | 0.00 | 0 | 0-NaN | 1 | |
| CD4+ count at the malignancies' diagnosis (cells/mm3) | [3; 51) | 38 | 23.9 | 15 | 11.6 | 1 | - | - |
| [51; 501) | 102 | 64.2 | 81 | 62.8 | 2.012 | 1.035-3.912 | 0.04 | |
| [> 501] | 19 | 11.9 | 33 | 25.6 | 4.4 | 1.934-10.011 | 0 | |
| cART before malignancies' diagnosis | no | 89 | 56.0 | 49 | 38.0 | 1 | - | - |
| yes | 70 | 44.0 | 80 | 62.0 | 2.076 | 1.293-3.334 | 0.003 | |
| VL suppression at the malignancies' diagnosis | no | 121 | 76.1 | 69 | 53.5 | 1 | - | - |
| yes | 38 | 23.9 | 60 | 46.5 | 2.769 | 1.675-4.577 | 0 | |
| Death during study period | no | 93 | 58.5 | 65 | 50.4 | 1 | - | - |
| yes | 66 | 41.5 | 64 | 49.6 | 1.387 | 0.869-2.214 | 0.191 | |
| Overall survival after malignancies' diagnosis (years) | [0; 1) | 55 | 34.6 | 44 | 34.1 | 1 | - | - |
| [1; 2) | 13 | 08.2 | 20 | 15.5 | 1.923 | 0.862-4.293 | 0.114 | |
| [2; 5) | 42 | 26.4 | 38 | 29.5 | 1.131 | 0.626-2.043 | 0.763 | |
| [5; 10) | 27 | 17.0 | 23 | 17.8 | 1.065 | 0.538-2.108 | 0.863 | |
| [10; 17] | 22 | 13.8 | 4 | 03.1 | 0.227 | 0.073-0.708 | 0.007 | |
OR – odds ratio; 95% CI – 95% confidence limits; cART – combination antiretroviral therapy; VL – viral load
Table 4.
Characteristics of the patients at the time of malignancies' diagnosis for non-AIDS-defining malignancies virus related (NADMs-VR) versus non-AIDS-defining malignancies virus unrelated (NADMs-VUR). Factors statistically associated with NADMs-VUR in bold
| Characteristic | NADM-VR | NADM-VUR | OR | 95% CI | p | |||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| n | % | n | % | |||||
| Sex | female | 8 | 13.8 | 19 | 26.8 | 1 | - | - |
| male | 50 | 86.2 | 52 | 73.2 | 0.438 | 0.176-1.091 | 0.084 | |
| Age at the malignancies' diagnosis (years) | [20; 30) | 7 | 12.1 | 11 | 15.5 | 1 | - | - |
| [30; 40) | 11 | 19.0 | 11 | 15.5 | 0.636 | 0.18-2.251 | 0.537 | |
| [40; 50) | 21 | 36.2 | 20 | 28.2 | 0.606 | 0.196-1.873 | 0.412 | |
| [50; 60) | 15 | 25.9 | 17 | 23.9 | 0.721 | 0.223-2.335 | 0.768 | |
| [60; 81] | 4 | 06.9 | 12 | 16.9 | 1.909 | 0.436-8.353 | 0.477 | |
| Mode of HIV exposure | bisexual | 2 | 03.4 | 5 | 07.0 | 1 | - | - |
| heterosexual | 11 | 19.0 | 21 | 29.6 | 0.764 | 0.127-4.596 | 1 | |
| IDU | 28 | 48.3 | 27 | 38.0 | 0.386 | 0.069-2.16 | 0.427 | |
| MSM | 17 | 29.3 | 18 | 25.4 | 0.424 | 0.072-2.483 | 0.428 | |
| Duration of HIV-infection at the malignancies' diagnosis (years) | [0; 1) | 10 | 17.2 | 14 | 19.7 | 1 | - | - |
| [1; 5) | 15 | 25.9 | 20 | 28.2 | 0.952 | 0.333-2.7271 | 0.577 | |
| [5; 10) | 14 | 24.1 | 13 | 18.3 | 0.663 | 0.219-2.009 | 1 | |
| [10; 34] | 19 | 32.8 | 24 | 33.8 | 0.902 | 0.329-2.478 | ||
| Opportunistic infections before malignancies' diagnosis | no | 23 | 39.7 | 40 | 56.3 | 1 | - | - |
| yes | 35 | 60.3 | 31 | 43.7 | 0.509 | 0.252-1.031 | 0.077 | |
| Nadir CD4 count (cells/mm3) | [0; 200) | 45 | 77.6 | 48 | 67.6 | 1 | - | - |
| [200; 350) | 11 | 19.0 | 13 | 18.3 | 1.108 | 0.45-2.725 | 1 | |
| [350; 500) | 2 | 03.4 | 4 | 05.6 | 1.875 | 0.327-10.741 | 0.68 | |
| [> 500] | 0 | 0.00 | 6 | 08.5 | Inf | NaN-Inf | 0.03 | |
| Smoking status | no | 12 | 20.7 | 15 | 21.1 | 1 | - | - |
| yes | 46 | 79.3 | 56 | 78.9 | 0.974 | 0.415-2.286 | 1 | |
| Alcohol status | no | 27 | 46.6 | 47 | 66.2 | 1 | - | - |
| yes | 31 | 53.4 | 24 | 33.8 | 0.445 | 0.218-0.907 | 0.032 | |
| Drugs status | no | 29 | 50.0 | 45 | 63.4 | 1 | - | - |
| yes | 29 | 50.0 | 26 | 36.6 | 0.578 | 0.285-1.17 | 0.153 | |
| Hepatitis C status | negative | 27 | 46.6 | 43 | 60.6 | 1 | - | - |
| positive | 31 | 53.4 | 27 | 38.0 | 0.547 | 0.27-1.107 | 0.11 | |
| unknown | 0 | 0.00 | 1 | 01.4 | Inf | NaN-Inf | 1 | |
| Hepatitis B status | negative | 36 | 62.1 | 39 | 54.9 | 1 | - | - |
| positive | 22 | 37.9 | 32 | 45.1 | 1.343 | 0.662-2.723 | 0.475 | |
| unknown | 0 | 0.00 | 0 | 0.00 | NaN | NaN-NaN | 1 | |
| CD4+ count at the malignancies' diagnosis (cells/mm3) | [3; 51) | 8 | 13.8 | 7 | 09.9 | 1 | - | - |
| [51; 501) | 40 | 69.0 | 41 | 57.7 | 1.171 | 0.388-3.533 | 1 | |
| [> 501] | 10 | 17.2 | 23 | 32.4 | 2.629 | 0.748-9.239 | 0.198 | |
| cART before malignancies' diagnosis | no | 25 | 43.1 | 24 | 33.8 | 1 | - | - |
| yes | 33 | 56.9 | 47 | 66.2 | 1.484 | 0.725-3.034 | 0.362 | |
| VL suppression at the malignancies' diagnosis | no | 32 | 55.2 | 37 | 52.1 | 1 | - | - |
| yes | 26 | 44.8 | 34 | 47.9 | 1.131 | 0.564-2.269 | 0.859 | |
| Death during study period | no | 25 | 43.1 | 40 | 56.3 | 1 | - | - |
| yes | 33 | 56.9 | 31 | 43.7 | 0.587 | 0.292-1.182 | 0.158 | |
| Overall survival after malignancies' diagnosis (years) | [0; 1) | 27 | 46.6 | 17 | 23.9 | 1 | - | - |
| [1; 2) | 4 | 06.9 | 16 | 22.5 | 6.353 | 1.816-22.229 | 0.003 | |
| [2; 5) | 11 | 19.0 | 27 | 38.0 | 3.898 | 1.542-9.853 | 0.004 | |
| [5; 10) | 13 | 22.4 | 10 | 14.1 | 1.222 | 0.439-3.401 | 0.795 | |
| [10; 17] | 3 | 05.2 | 1 | 01.4 | 0.529 | 0.051-5.513 | 1 | |
OR – odds ratio; 95% CI – 95% confidence limits; cART – combination antiretroviral therapy; VL – viral load
Discussion
Between 1995 and 2012, more than 16,300 cases of HIV infections were registered in Poland (data from the National Institute of Public Health National Institute of Hygiene) [30]. In this retrospective, observational study, both the number of registered cases of HIV infections and the number of malignancies diagnosed in these patients have been rising over the given periods of time. Not much more than a half (n = 159/288; 55.2%) of the identified cases of malignancy were ADMs, among of which NHL was the most commonly reported and remains the commonest malignancy-related cause of death even in the cART era, as well as among men, while ICC was the commonest among women. Despite the introduction of cART in the mid-1990s, there has been a noticeable downward tendency in Poland over a period of time only applicable to two malignancies sets. The first, PCNSL, dominates in patients with marked immunosuppression and EBV co-infection, which may indirectly testify to partial improvement of earlier HIV diagnosis and of cART access [4, 5, 31, 32]. The second malignancy set, namely ICC, the result of several genital HPV types, has been identified as the carcinogenic precursor and necessary co-factor for ICC (not only in women with advanced immunosuppression), and it has been decreasing over the periods of time presented in this study, the reason for which may be easier access and more successful prophylactic programmes, HPV vaccines, early diagnosis, and ICC treatment in Poland (mostly yearly cervical Pap smear) similarly to other studies [4, 5, 19, 25, 33]. Like in other studies, KS occurs predominantly among men (n = 49/49; 100% of the cases in our study) in whom 81.6% (n = 40/49) reported male-to-male sex contact as the mode of HIV transmission, which was probably connected to the same way and prevalence of HHV-8 known to cause of KS [4, 5, 34, 35]. We believe that our findings may reflect a considerably changing epidemiological situation in Poland and may prove this means of HIV transmission to be currently predominant. It might be too early to observe a significant decrease in the prevalence of NHL and KS, and perhaps the HIV infections are still diagnosed too late and in a too advanced phase of infection. In patients unaware of their HIV status, the ADM is often the first opportunistic infection.
Apart from ADMs, the remaining malignancies were either NADMs, with a noticeable upward tendency exceeding the number of ADMs at the time. More recent data has shown several NADMs, most of all viruses being related to HIV-positive patients, to be increasing, similarly to the risk seen in transplantation recipients compared to the general population, suggesting a link between immune suppression proven in the present study [21]. According to the classification of malignancies established hereinbefore, 55% (n = 71/129) of them are NADMs-VR and 45% (n = 58/129) are NADMs-VUR, among which HD was the predominant one to be diagnosed in both sexes. It is known that EBV indicates its relation with HD, which can testify to a large number of co-infections with this virus in Poland [36]. Taken as a whole, the recent literature would suggest that HIV infection is currently an independent risk factor of lung cancer [17, 37]. In the present study, lung cancer has been a predominant malignancy among NADMs-VUR, most of which were diagnosed in men (n = 17/18; 94.4%), which suggests that HIV itself is a genuine risk factor of lung cancer, and its highest upward tendency among all NADMs proves a current epidemic of the malignancy in question [38, 39]. In addition, HIV-positive individuals who smoke tobacco are more predisposed to die of solid tumour than the general population [38, 40]. The association with smoking, on the other hand, may reflect the risk behaviour of the people who may engage in unprotected sex or drug use, which can also lead to viral co-infections [23, 40, 41]. In the study, the fact that as many as 75.8% (n = 216/285) of HIV-positive patients had at some time smoked tobacco and as many as 100% (n = = 18/18) of those with a lung cancer were heavy smokers accounts for the increasing risk. However, we did not find a statistically significant association of smoking status and NADMs-VUR. Among NADMs-VR, HCC is commonly reported (n = 14/58; 4.9% of all malignancies, second place after HD) and is likely to remain important in HIV-infected populations, particularly in the context of the high level of co-infections with HBV and HCV presented in the study and associated with higher serum hepatitis DNA/RNA viral levels, progression to cirrhosis, and more frequent HCC with more aggressive course and poorer survival time than HIV-negative patients [42–44]. In our study, all the cases of HCC were HBV and/or HCV co-infected (64.3%; n = 9/14 HBV and 92.9%; n = 13/14 HCV; one individual only HBV mono-co-infection), and 78.6% (n = 11/14) also suffered from cirrhosis. We did not find a statistically significant association of HBV or HCV co-infection and NADMs-VR either, which may be explained, as in lung cancer, by low numbers, but may also be due to the inclusion of other malignancies in this analysis, depending on co-infections with other viruses. HCC was diagnosed mostly in elderly men (median age 47.5 years), men (n = 13/14; 92.9%), IDUs mode of acquisition (n = 12/14; 85.7%), after many years of the lack of treatment, or inadequate treatment of HBV and/or HCV co-infection. Furthermore, HCC was usually diagnosed too late, which resulted in poor prognosis. It may indirectly testify to the fact that HCC natural history progression takes from years to decades to occur owing to the former major way of HIV transmission in Poland, being intravenous drug injection. Attention should be drawn to a relatively increasing number of skin cancers over periods of time mostly in women (it should be mentioned that Caucasians are more predisposed to have skin cancer [7]), and few cases of breast cancer in women (n = 2/288; only 2.5% of all malignancies in women, n = 2/80) and no such cases in men. There was also no case of leiomyosarcoma in both sexes. Comparing the malignancies’ prevalence between the countries located in the same region in Europe, strikingly few anal cancers have been diagnosed [45, 46]. Anal cancer was found mostly in men (88.9%; n = 8/9) and homosexuals (77.8%; n = 7/9). It was also diagnosed in further stages, showing the general tendency to increase in recent years. Similarly, a few cases of colorectal carcinoma (only n = 5/288; 1.7%) were diagnosed in surprisingly young people (median age 37.4 years), no matter the sex, the way of HIV transmission, the immune status, and ART or prostate cancer (only n = 5/288; 1.7%, median age 70 years) [4, 45, 47, 48]. There is a necessity of oncological supervision, mostly in the group of patients in question, as well as the necessity to introduce successful methods of prevention and early treatment.
In our study, we have also found several predictors of NADMs and less of VR vs. VUR subgroup. The results presented in the final part of the study confirm the findings from previous studies [7–9, 11–13, 15, 24].
There are some limitations to this study. First, this is a retrospective, observational research on any type of malignancy in HIV-positive adult patients in Poland, without a control group. As with all cohort studies, we can only refer to the data that we have collected. Our study population might not reflect the exact distributions of malignancies occurring all over the country with a noticeable predominance of CRFs from the capital of Poland, being the largest HIV care and cure centre. Furthermore, there may be variations between the level of malignancy, screening mostly in earlier periods when there were no functional population-based malignancy registries. The registration of all the cases of malignancies in HIV-infected population was not accurate enough as the centres are located exclusively in urban areas. Also, our distribution between NADMs-VR and NADMs-VUR may be debateable. Not all of NADMs-VR types are dependent on co-infections with certain viruses in the same way. Finally, we did not analyse the types of malignancies individually, but in selected groups, which might have masked specific data.
In conclusion, the prevalence of malignancies in an ageing and growing HIV-infected adult Polish cohort continued to grow over the period between 1995 and 2012, concerning, in particular, non-AIDS-defining virus unrelated (NADMs-VUR) malignancies. Non-Hodgkin lymphoma (NHL) was the most frequent malignancy among ADMs, and Hodgkin's disease (HD) was the most frequent malignancy among NADMs-VR, whereas lung cancer was the most frequent malignancy among NADMs-VUR. It is possible that, with assertive prevention strategies, earlier diagnosis of HIV-infection in Poland, and starting cART adequately early among patients with a confirmed HIV diagnosis, the incidence of ADMs and NADMs-VR will decrease. An increased incidence of NADMs was confirmed in elderly men with longer duration of HIV-infection, with better virological and immunological control and prior AIDS diagnosis (defined as prior opportunistic infections, excluding ADMs). Effective primary prevention and screening strategies especially for NADMs-VUR as well as early detection and treatment of co-infections ought to be included in the routine long-term follow-up of the HIV-infected population. Further effort to resolve the direct and indirect effects of HIV itself on NADMs and prospective data to assess the impact of cART on all malignancies management and treatment outcomes are urgently needed. Nowadays, the spectrum of cancer diagnoses in the adult HIV Poland cohort does not appear dissimilar to those noted in other Western European populations.
The authors declare no conflict of interest.
Sincere thanks to all the participants who have contributed to this study as well as to the Research Development Foundation in the Hospital for Infectious Diseases in Warsaw. This study has been supported by a Polish AIDS Society grant.
References
- 1.Lewden C, May T, Rosenthal E, et al. ANRS EN19Mortalité Study Group and Mortavic1 Changes in causes of death among adults infected by HIV between 2000 and 2005: The “Mortalité 2000 and 2005” surveys (ANRS EN19 and Mortavic) J Acquir Immune Defic Syndr. 2008;48:590–8. doi: 10.1097/QAI.0b013e31817efb54. [DOI] [PubMed] [Google Scholar]
- 2.Barbaro G, Barbarini G. HIV infection and cancer in the era of highly active antiretroviral therapy. Oncol Rep. 2007;17:1121–6. [PubMed] [Google Scholar]
- 3.Simard EP, Pfeiffer RM, Engels EA. Cumulative incidence of cancer among individuals with acquired immunodeficiency syndrome in the United States. Cancer. 2011;117:1089–96. doi: 10.1002/cncr.25547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Engels EA, Pfeiffer RM, Goedert JJ, et al. HIV/AIDS Cancer Match Study Trends in cancer risk among people with AIDS in the United States 1980-2002. AIDS. 2006;20:1645–54. doi: 10.1097/01.aids.0000238411.75324.59. [DOI] [PubMed] [Google Scholar]
- 5.Nutankalva L, Wutoh AK, McNeil J, Frederick WR, Reddy RB, Daftary M, Gentles A, Addae-Afoakwa K. Malignancies in HIV: pre- and post-highly active antiretroviral therapy. J Natl Med Assoc. 2008;100:817–20. doi: 10.1016/s0027-9684(15)31375-4. [DOI] [PubMed] [Google Scholar]
- 6.Mocroft A, Ledergerber B, Katlama C, et al. EuroSIDA study group Decline in the AIDS and death rates in the EuroSIDA study: an observational study. Lancet. 2003;362:22–9. doi: 10.1016/s0140-6736(03)13802-0. [DOI] [PubMed] [Google Scholar]
- 7.Pantanowitz L, Schlecht HP, Dezube BJ. The growing problem of non-AIDS-defining malignancies in HIV. Curr Opin Oncol. 2006;18:469–78. doi: 10.1097/01.cco.0000239886.13537.ed. [DOI] [PubMed] [Google Scholar]
- 8.Mitsuyasu RT. Non-AIDS-defining malignancies in HIV. Top HIV Med. 2008;16:117–21. [PubMed] [Google Scholar]
- 9.Bedimo R. Non-AIDS-defining malignancies among HIV-infected patients in the highly active antiretroviral therapy era. Curr HIV/AIDS Rep. 2008;5:140–9. doi: 10.1007/s11904-008-0022-4. [DOI] [PubMed] [Google Scholar]
- 10.Patel P, Hanson DL, Sullivan PS, Novak RM, Moorman AC, Tong TC, Holmberg SD, Brooks JT, Adult and Adolescent Spectrum of DiseaseProject and HIV Outpatient Study Investigators Incidence of types of cancer among HIV-infected persons compared with the general population in the United States, 1992-2003. Adult and Adolescent Spectrum of Disease Project and HIV Outpatient Study Investigators. Ann Intern Med. 2008;148:728–36. doi: 10.7326/0003-4819-148-10-200805200-00005. [DOI] [PubMed] [Google Scholar]
- 11.Powles T, Robinson D, Stebbing J, et al. Highly active antiretroviral therapy and the incidence of non-AIDS-defining cancers in people with HIV infection. J Clin Oncol. 2009;27:884–90. doi: 10.1200/JCO.2008.19.6626. [DOI] [PubMed] [Google Scholar]
- 12.Hessol NA, Pipkin S, Schwarcz S, Cress RD, Bacchetti P, Scheer S. The impact of highly active antiretroviral therapy on non-AIDS-defining cancers among adults with AIDS. Am J Epidemiol. 2007;165:1143–53. doi: 10.1093/aje/kwm017. [DOI] [PubMed] [Google Scholar]
- 13.Worm SW, Bower M, Reiss P, et al. D:A:D Study Group Non-AIDS defining cancers in the D:A:D Study-time trends and predictors of survival: a cohort study. BMC Infect Dis. 2013;13:471. doi: 10.1186/1471-2334-13-471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bonnet F, Burty C, Lewden C, et al. Agence Nationale de Recherches sur le Sida et les Hépatites Virales EN19 Mortalité Study Group. Mortavic Study Group Changes in cancer mortality among HIV-infected patients: the Mortalité 2005 Survey. Clin Infect Dis. 2009;48:633–9. doi: 10.1086/596766. [DOI] [PubMed] [Google Scholar]
- 15.Pantanowitz L, Dezube BJ. Evolving spectrum and incidence of non-AIDS-defining malignancies. Curr Opin HIV AIDS. 2009;4:27–34. doi: 10.1097/COH.0b013e32831a7259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Achenbach CJ, Cole SR, Kitahata MM, Casper C, Willig JH, Mugavero MJ, Saag MS. Mortality after cancer diagnosis in HIV-infected individuals treated with antiretroviral therapy. AIDS. 2011;25:691–700. doi: 10.1097/QAD.0b013e3283437f77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shiels MS, Cole SR, Kirk GD, Poole C. A meta-analysis of the incidence of non-AIDS cancers in HIV-infected individuals. J Acquir Immune Defic Syndr. 2009;52:611–22. doi: 10.1097/QAI.0b013e3181b327ca. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hasse B, Ledergerber B, Furrer H, et al. Swiss HIV Cohort Study Morbidity and aging in HIV-infected persons: the Swiss HIV cohort study. Clin Infect Dis. 2011;53:1130–9. doi: 10.1093/cid/cir626. [DOI] [PubMed] [Google Scholar]
- 19.Shiels MS, Pfeiffer RM, Gail MH, et al. Cancer burden in the HIV-infected population in the United States. J Natl Cancer Inst. 2011;103:753–62. doi: 10.1093/jnci/djr076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Petoumenos K, Hui E, Kumarasamy N, et al. TREAT Asia HIV Observational Database Cancers in the TREAT Asia HIV Observational Database (TAHOD): a retrospective analysis of risk factors. J Int AIDS Soc. 2010;13:51. doi: 10.1186/1758-2652-13-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Grulich AE, van Leeuwen MT, Falster MO, Vajdic CM. Incidence of cancers in people with HIV/AIDS compared with immunosuppressed transplant recipients: a meta-analysis. Lancet. 2007;370:59–67. doi: 10.1016/S0140-6736(07)61050-2. [DOI] [PubMed] [Google Scholar]
- 22.Lowsky R, Lipton J, Fyles G, et al. Secondary malignancies after bone marrow transplantation in adults. J Clin Oncol. 1994;12:2187–92. doi: 10.1200/JCO.1994.12.10.2187. [DOI] [PubMed] [Google Scholar]
- 23.Clifford GM, Polesel J, Rickenbach M, et al. Cancer risk in the Swiss HIV Cohort Study: associations with immunodeficiency, smoking, and highly active antiretroviral therapy. J Natl Cancer Inst. 2005;97:425–32. doi: 10.1093/jnci/dji072. [DOI] [PubMed] [Google Scholar]
- 24.Reekie J, Kosa C, Engsig F, et al. EuroSIDA Study Group Relationship between current level of immunodeficiency and non-acquired immunodeficiency syndrome-defining malignancies. Cancer. 2010;116:5306–15. doi: 10.1002/cncr.25311. [DOI] [PubMed] [Google Scholar]
- 25.Bouvard V, Baan R, Straif K, et al. WHO International Agency for Research on Cancer Monograph Working Group A review of human carcinogens-Part B: biological agents. Lancet Oncol. 2009;10:321–2. doi: 10.1016/s1470-2045(09)70096-8. [DOI] [PubMed] [Google Scholar]
- 26.Michelow P, Wright C, Pantanowitz L. A review of the cytomorphology of Epstein-Barr virus-associated malignancies. Acta Cytol. 2012;56:1–14. doi: 10.1159/000334235. [DOI] [PubMed] [Google Scholar]
- 27.Engels EA. Non-AIDS-defining malignancies in HIV-infected persons: etiologic puzzles, epidemiologic perils, prevention opportunities. AIDS. 2009;23:875–85. doi: 10.1097/QAD.0b013e328329216a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. http://www.who.int/classifications/icd/en/.
- 29.Swerdlow SH, et al. Vol. 2. Lyon, France: IARC Press; 2008. World Health Organization Classification of Tumours of Haematopoietic and Lymphoid Tissues. [Google Scholar]
- 30. http://www.pzh.gov.pl/.
- 31.Gerstner ER, Batchelor TT. Primary central nervous system lymphoma. Arch Neurol. 2010;67:291–7. doi: 10.1001/archneurol.2010.3. [DOI] [PubMed] [Google Scholar]
- 32.Diamond C, Taylor TH, Aboumrad T, Anton-Culver H. Changes in acquired immunodeficiency syndrome-related non-Hodgkin lymphoma in the era of highly active antiretroviral therapy: incidence, presentation, treatment, and survival. Cancer. 2006;106:128–35. doi: 10.1002/cncr.21562. [DOI] [PubMed] [Google Scholar]
- 33.Vol. 90. Lyon: WHO International Agency for Research on Cancer; 2007. IARC Monographs on the Evaluation of Carcinogenic Risks to Humans. Human Papillomaviruses. [PMC free article] [PubMed] [Google Scholar]
- 34.Mesri EA, Cesarman E, Boshoff C. Kaposi's sarcoma and its associated herpesvirus. Nat Rev Cancer. 2010;10:707–19. doi: 10.1038/nrc2888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.El Amari EB, Toutous-Trellu L, Gayet-Ageron A, et al. Swiss HIV Cohort Study Predicting the evolution of Kaposi sarcoma, in the highly active antiretroviral therapy era. AIDS. 2008;22:1019–28. doi: 10.1097/QAD.0b013e3282fc9c03. [DOI] [PubMed] [Google Scholar]
- 36.Guidoboni M, Ponzoni M, Caggiari L, et al. Latent membrane protein 1 deletion mutants accumulate in reed-sternberg cells of human immunodeficiency virus-related Hodgkin's lymphoma. J Virol. 2005;79:2643–9. doi: 10.1128/JVI.79.4.2643-2649.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sigel K, Wisnivesky J, Gordon K, et al. HIV as an independent risk factor for incident lung cancer. AIDS. 2012;26:1017–25. doi: 10.1097/QAD.0b013e328352d1ad. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Giordano TP, Kramer JR. Does HIV infection independently increase the incidence of lung cancer? Clin Infect Dis. 2005;40:490–1. doi: 10.1086/427028. [DOI] [PubMed] [Google Scholar]
- 39.Winstone TA, Man SF, Hull M, Montaner JS, Sin DD. Epidemic of lung cancer in patients with HIV infection. Chest. 2013;143:305–14. doi: 10.1378/chest.12-1699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Tesoriero JM, Gieryic SM, Carrascal A, Lavigne HE. Smoking among HIV positive New Yorkers: prevalence, frequency, and opportunities for cessation. AIDS Behav. 2010;14:824–35. doi: 10.1007/s10461-008-9449-2. [DOI] [PubMed] [Google Scholar]
- 41.Demopoulos BP, Vamvakas E, Ehrlich JE, Demopoulos R. Non-acquired immunodeficiency syndrome-defining malignancies in patients infected with human immunodeficiency virus. Arch Pathol Lab Med. 2003;127:589–92. doi: 10.5858/2003-127-0589-NISMIP. [DOI] [PubMed] [Google Scholar]
- 42.Sterling RK, Sulkowski MS. Hepatitis C virus in the setting of HIV or hepatitis B virus coinfection. Semin Liver Dis. 2004;24:61–8. doi: 10.1055/s-2004-832930. [DOI] [PubMed] [Google Scholar]
- 43.Bruno R, Sacchi P, Filice C, Puoti M, Filice G. Hepatocellular carcinoma in HIV-infected patients with chronic hepatitis: an emerging issue. J Acquir Immune Defic Syndr. 2002;30:535–6. doi: 10.1097/00126334-200208150-00011. [DOI] [PubMed] [Google Scholar]
- 44.Berretta M, Garlassi E, Cacopardo B, et al. Hepatocellular carcinoma in HIV-infected patients: check early, treat hard. Oncologist. 2011;16:1258–69. doi: 10.1634/theoncologist.2010-0400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hensel M, Goetzenich A, Lutz T, et al. HIV and cancer in Germany. Dtsch Arztebl Int. 2011;108:117–22. doi: 10.3238/arztebl.2010.0117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.de Pokomandy A, Rouleau D, Ghattas G, et al. HAART and progression to high-grade anal intraepithelial neoplasia in men who have sex with men and are infected with HIV. Clin Infect Dis. 2011;52:1174–81. doi: 10.1093/cid/cir064. [DOI] [PubMed] [Google Scholar]
- 47.Yegüez JF, Martinez SA, Sands DR, Sands LR, Hellinger MD. Colorectal malignancies in HIV-positive patients. Am Surg. 2003;69:981–7. [PubMed] [Google Scholar]
- 48.Chapman C, Aboulafia DM, Dezube BJ, Pantanowitz L. Human immunodeficiency virus-associated adenocarcinoma of the colon: clinicopathologic findings and outcome. Clin Colorectal Cancer. 2009;8:215–9. doi: 10.3816/CCC.2009.n.036. [DOI] [PubMed] [Google Scholar]